Professional Documents
Culture Documents
Combination of Spinal Anesthesia and Obturator Nerve Block Intransurethral Resection of Bladder Tumor Comparison Between Nerve Sti
Combination of Spinal Anesthesia and Obturator Nerve Block Intransurethral Resection of Bladder Tumor Comparison Between Nerve Sti
Uploaded by
alfindyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Combination of Spinal Anesthesia and Obturator Nerve Block Intransurethral Resection of Bladder Tumor Comparison Between Nerve Sti
Combination of Spinal Anesthesia and Obturator Nerve Block Intransurethral Resection of Bladder Tumor Comparison Between Nerve Sti
Uploaded by
alfindyCopyright:
Available Formats
al and Me
nic
Journal of Clinical and Medical Teymourian et al., J Clin Med Sci 2018, 2:1
di
rnal of Cli
cal
Scienc Sciences
ou
e
J s
Research Article Open Access
Combination of Spinal Anesthesia and Obturator Nerve Block in
Transurethral Resection of Bladder Tumor, Comparison between Nerve
Stimulator and Ultrasonography
Houman Teymourian1*, Shayesteh Khorasanizadeh1, Mohammad Reza Razzaghi2 and Yasmin Khazaie3
1Department of Anesthesiology and Critical Care, Shohada-e-Tajrish Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran
2Department of Urology, Shohada-e-Tajrish Hospital, Shahid Beheshti University of Medical Sciences,Tehran, Iran
3Department of Anesthesiology and Critical Care, Eghbal Hospital, Tehran, Iran
Received: September 02, 2018; Accepted: September 16, 2018; Published: September 20, 2018
*Corresponding author: Houman Teymourian, Associate Professor, Department of Anesthesiology and Critical Care, Shohada-e-Tajrish Hospital, Shahid Beheshti
University of Medical Sciences, Tehran, Iran, Tel: +98-9121156198, E-mail: houman72625@yahoo.com
Copyright: © 2018 Teymourian H, et al. This is an open-access article distributed under the terms of the creative commons attribution license, which permits unrestricted
use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Genitourinary system mostly develops cancers with bladder origin which can be treated in several
ways. One of the most prevalent these ways are through the urethra (TURP). For anesthesia, general anesthesia or
neuraxial methods can be used but the most common procedure is spinal anesthesia. The level of sensory block
should reach to T10. Obturator nerves which are part of lumbar plexus innervate adductor muscles. The nerve in its
route passes close to the ladder wall. Sometimes during cauterization of the tumor this nerve is stimulated, causing
reflex adductor (Jump organs) despite the spinal anesthesia. Intraoperative complications of TURP include bleeding
(sometimes too much). In some cases, adductor reflex can cause rupture of the bladder due to the movement of the
patient. One of the useful measures to prevent this incident is to block the Obturator nerve separately.
Methods: 124 eligible subjects were assigned to two groups randomly. Ultrasound-guided Obturator nerve blocks
in one group and the other with nerve locator, both received 10 cc of Lidocaine 1.5% with Epinephrine 1/200000.
After spinal block with Bupivacaine 3 cc of 0.5% to obtain sensory level to 10, surgery is done. Presence or absence
of adductor reflexes were recorded by the surgeon. Bladder perforation and bleeding during and after surgery were
also recorded. The presence or absence of sensory or motor block residual was recorded in the next day.
Results: The incidence of adductor reflex (Jerking limbs during cauterization of the tumor) was significantly low in
the ultrasound group than nerve location. The amount of bleeding and ruptured bladder in ultrasound group was
significantly lower than in nerve locator. Any remaining blocks in any group after 24 hours were not present.
Conclusion: Based on the current study results, ultrasound-guided nerve block is more suitable than nerve
locator for obturator block.
Keywords: Transurethral resection of bladder tumor (TURBT); TURBT is usually done under spinal anesthesia, but it does not
Obturator nerve; Reflexes adductor prevent the obturator jerk reflex leading to some problems for surgeons
and many complications such as bladder perforation, bleeding or
Introduction incompletely resection of tumor which could be prevented by ONB in
TURBT [8-11]. Many recent findings in different studies suggest that
Peripheral nerve blocks are still a well-accepted procedure in ONB can make it possible to eradicate tumors located on the lateral
comprehensive anesthetic care. Benefits of peripheral nerve block are wall of the bladder by immobilizing the surgical field.
better analgesia, less need for opioids and other pain medications
administration, decreased recovery room duration and/or hospital Objectives
stay, improved mobility and functional recovery post operation, and
increased patient satisfaction [1]. Obturator Nerve Block (ONB) is The degree of success of blocking the obturator nerve is between 65
usually performed to avoid sudden and harmful thigh adduction to 90 percent when we do the block blindly without use of sonographic
during TURBT [2,3]. approach. While the selective blockage of this nerve is partly safe, there
is a risk of neurological or other neighboring parts damage [12]. So
Labat et al., [4] first described selective ONB in 1922. Since then,
ultrasonography guide is a hopeful option. In this research, we
several ONB techniques using surface landmarks to localize the nerve
compared using ultrasonography or nerve stimulator for obturator
have been reported by different studies [5-7]. Obturator nerve (ON)
nerve block in TURBT [13].
passes through proximal to the inferolateral bladder wall, bladder neck,
and prostatic urethra. Hence, TURBT on the lateral side of the bladder
under spinal anesthesia may arouse an obturator reflex, adductor
muscle activation and so leg to jerk [8].
J Clin Med Sci, an open access journal Volume 2 • Issue 1 • 1000106
Citation: Teymourian H, Khorasanizadeh S, Razzaghi MR, Khazaie Y (2018) Combination of Spinal Anesthesia and Obturator Nerve Block in
Transurethral Resection of Bladder Tumor, Comparison between Nerve Stimulator and Ultrasonography. J Clin Med Sci 2: 106.
Page 2 of 5
Materials and Methods adductor muscle and when receiving to the posterior-medial side of
the thigh. Nerve stimulation by 2-3 mA decreased to 0.5 mA before
Patients with TURBT were enrolled in the current randomized local anesthesia. After needle insertion, 5 ml of local anesthetic was
clinical trial after signing the informed consent form. infiltrated.
Inclusion and exclusion criteria In the sonography-guided group, sonography confirmed injection
site. The proposition of LA was done slowly (10 ml/minute). Presence
Inclusion criteria: No addiction, no sensory or motor disorder, ASA of obturator reflex was reported by surgeon. In order to estimate
Class I/II, no diabetes mellitus, no coagulopathy, no infection on hemorrhage accurately, the bladder should be evacuated completely
injection site, no hyper/hypotension, consent in spinal anesthesia and before the procedure and the volume of the used liquid was accurately
no electrolyte imbalance. calculated. The amount of bleeding was evaluated low, very low (less
than MABL), Moderate (To the extent MABL: Without the need for
Exclusion criteria: Surgery duration above 2 hours, need for general
blood prescription and compensation by Serum) and Severe (to the
anesthesia, and electrolyte imbalance.
extent MABL and more and need for blood prescription).
Spinal anesthesia was done by 3 ml of 0.5% Bupivacaine after
blocking the obtoratur nerve in either ways. In both group after ���� �������� ��������� ����� ����
standard fluid therapy and monitoring, the sedation was achieved by
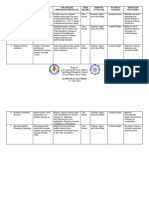
Midazolam 0.02 mg/kg (Table 1). ����ℎ� ������� ��� − ������� ���
= ������� + ��� ���
130 patients 2
Sonography (65 persons) Nervelocator (65 persons) During the operation, the patient was monitored for bladder
perforation symptoms and at the end of the surgery, the surgeon
1 1 persons 1 62 persons 1 persons 2 62 persons evaluated bladder for perforation. Eventually, the presence or absence
person person person
s s s
of sensory and motor symptoms was recorded on the day after surgery.
Study variables were age, gender, lower extremity jerking, bladder
Open Surgery Failed Participatio Surgery Failed Participatio hemorrhage, perforation, etc.
surger Prolongatio Spinal n in the Prolongatio Spinal n in the
y n study n study 124 patients’ information including 62 persons under selective
obturator nerve block with nerve stimulator as well as 62 control
Table 1: The result of the reviews of 130 patients. subjects selected based on ultrasonographic guide was analyzed with
SPSS version 21.0. Chi-Square and Exact-Fisher tests were used
After aseptic techniques were done, 85 mm (Visicon) needle for (p<0.05).
performing block and ultrasonography (for guidance were used. Nerve
stimulator guided block was done selectively for the obtoratur nerves Results
at the inguinal level and little more distal. The adductor longus tendon
and the femoral artery is marked. to identify tendon, achievement of 130 patients were evaluated (65 in each group) and 6 patients (3 in
extreme leg abduction is required (Figure 1). Pubis tubercle as the each) were excluded from study (3 because of not achieving the
surface anatomic guide is important. considered level, 2 because of surgery duration more than 2 hours and
1 because of change of surgical plan to open surgery). The mean age of
patients in with/without ultrasonographic-guide groups were 62.11 ±
9.59 and 63.21 ± 9.71 years respectively (p>0.05) and 12 (19.4%) and
16 (25.8%) subjects were female in each group, respectively (p>0.05).
both groups had the same operation time (p>0.05, 88.6+19.4 versus
92.1+20.3 minutes).
Based on Table 2, however no significant difference was reported
between the without guide the guided groups in the onset time
(6.2+2.3 min vs. 5.8+2.2 min), while, the time needed for blocking
nerve (4.5+1.2 min versus 1.6+0.9 min) was shorter significantly
(p=0.001) in sonographic-guided group.
A B p-value
N 62 62
Gender
Female 16 (25.8%) 12 (19.4%)
Figure 1: Nervelocator. 0.39
Male 46 (74.2%) 50 (80.6%)
The needle was inserted one inch lateral and one inch inferior from Age 63.21 ± 9.71 62.11 ± 9.59 0.528
the pubis tubercle. Then, the needle was inserted deeper (2 cm) over
Bleeding
the short adductor muscle laterally until responding the major
J Clin Med Sci, an open access journal Volume 2 • Issue 1 • 1000106
Citation: Teymourian H, Khorasanizadeh S, Razzaghi MR, Khazaie Y (2018) Combination of Spinal Anesthesia and Obturator Nerve Block in
Transurethral Resection of Bladder Tumor, Comparison between Nerve Stimulator and Ultrasonography. J Clin Med Sci 2: 106.
Page 3 of 5
Low 13 (21.0%) 24 (38.7%) Jerking was seen in 22.6% and 8.1% of two groups respectively (p-
value: 0.025) and perforation was seen in 8 (12.9%) in first group and
Moderate 23 (37.1%) 27 (43.5%) 0.003 only 1 (1.6%) in second group (p-value: 0.032). Residual effect of nerve
block was seen in none of the patients in two groups.
Severe 26 (41.9%) 11 (17.7%)
Jerk 14 (22.6%) 5 (8.1%) 0.025 Discussion
Perforation 8 (12.9%) 1 (1.6%) 0.032 TURBT is a surgical technique extensively used to diagnose and
treat bladder cancer which often performed under spinal anesthesia.
Residual effects of block 0( 0%) 0 (0%) Non-significant
Peripheral nerve blocks are inexpensive anesthetic methods used to
Duration of operation 92.1+20.3 88.6+19.4 <0.05 induce anesthesia while avoiding induction of general anesthesia and
its complications or even neuroaxial 23 anesthesia. So, now-a-days
Onset time 6.2+2.3 min 5.8+2.2 min 0.001 demand for regional methods is growing increasingly because of
patients satisfaction, its cost-effectiveness, its usefulness and better
Table 2: The result of the reviews. postoperative recovery in different experiences [5,8,11,14].
Based on Graph 1, the success rate in block was relatively more in Obturator nerve block combined with spinal anesthesia is a suitable
patients underwent ultrasonography (92% versus 78%, p-value: 0.05). method in TURBT. There are different modalities described in
literature to block obturator nerve. One of them is nerve stimulation
technique which was reported by Prentiss et al., [15] and then Parks
and Kennedy [16] with a success rate of 83.8% to 85.7%.
Min et al., and Bolat et al., [17,18] in their study using nerve
stimulator to do ONB reported an overall success rate of 95.4% and
88.6% respectively. Recent studies reported more success rate of 97.2%
for nerve stimulation in combination with sonography [19,20]. In our
study success rate in group ONB+ nerve locator was about 78% and in
group ONB+ ultrasonography was about 92%.
In a study by Augspurger and Donohue [21] obturator jerk was
abolished 83.8% with blind anatomic approach which is lower to nerve
stimulation and sonographic-guided techniques described previously.
As the effectiveness rise from 89.4% to 100% in Gasparich et al., and
Kobayashi et al., [22,23] studies. In our study obturator jerk was seen
in 8.1% using ultrasound in compare with 22.6% in nerve stimulation
without sonographic guide.
Graph 1: Comparison of success rate in two groups.
Dick et al., [24] in a study evaluated the occurrence of hemorrhage
was 13% while Collado et al., [25] have reported 3.4% of patients
needed blood transfusion. Malik et al., [26] reported 25% of patients in
their study required transfusion after TURBT. In our study sever
bleeding was seen in 17.7% of ultrasound-guided ONB in compare
with 41.9% in control group.
Literature search revealed bladder perforation incidence between
0.9% to 5%, while in this study it was 1.6% and 12.9% in sonography-
guided ONB and control group respectively [27]. Yamauchi et al., [28]
evaluated the effect of peri articular infiltration analgesia (PIA) and
sciatic nerve block (SNB) for posterior knee pain. They reported lower
score of VAS in PIA group than in SNB group 12-24 hours, most of
patients didn’t experience posterior knee pain. So they included that
post-TKA application of FNB plus PIA is suitable periarticular
infiltration method and could be used instead of SNB providing
sufficient analgesia.
Helayel et al., [29] surveyed a new ultrasound-guided technique to
localize the obturator nerve. In 91% of cases, this nerve is properly
Graph 2: Comparison of bleeding rate in two groups. identified on the first attempt within 30 ± 23 seconds. Adductor
strength decreased in all patients and they had various sensory
territories, although 32% of them had no cutaneous distribution. 14%
Bleeding was mild, moderate and sever in 21%, 37.1% and 41.9% in of the patients received low-dose opioid and no one received general
group without sonographic guidance and 38.7%, 43.5% and 17.7% in anesthesia to complete the surgery.
sonographic guide nerve block group respectively (p-value: 0.003 and
Graph 2).
J Clin Med Sci, an open access journal Volume 2 • Issue 1 • 1000106
Citation: Teymourian H, Khorasanizadeh S, Razzaghi MR, Khazaie Y (2018) Combination of Spinal Anesthesia and Obturator Nerve Block in
Transurethral Resection of Bladder Tumor, Comparison between Nerve Stimulator and Ultrasonography. J Clin Med Sci 2: 106.
Page 4 of 5
In Manassero et al., [30] study 50 patients who were candidate for 4. Labat, Gaston, Mayo, William J (1922) Regional anesthesia: Its technic
spinal anesthesia randomly divided into two groups of 5 ml 2% and clinical application. Boston Med Surg J 188: 115.
Lidocaine, ultrasound-guided injection into the interfascial plane 5. Choquet O, Capdevila X, Bennourine K, Feugeas JL, Bringuier-
between adductor longus and adductor brevis as well as adductor Branchereau S, et al. (2005) A new inguinal approach for the obturator
nerve block: Anatomical and randomized clinical studies. Anesthesiology
brevis and magnus muscles (US group), and of 5 ml of 2% Lidocaine
103: 1238-1245.
accompanied by nerve stimulation after identification of the divisions
of the obturator nerve (USENS group). The blocking nerve was found 6. Baba M, Nishihara L, Tomi K (2007) Pubic tubercle side approach to the
obturator nerve block, Masui. Jpn J Anesth 56: 1174-1178.
by ultrasound-guided obturator after division of the nerve, induction
7. Khorrami MH, Javid A, Saryazdi H, Javid M (2010) Transvesical blockade
of local anesthetic between the planes of the adductor muscles as the of the obturator nerve to prevent adductor contraction in transurethral
nerve stimulation analogue. bladder surgery. J Endourol 24: 1651-1654.
Based on the findings of a study, risk of intraneural injection and 8. Kuo JY (2008) Prevention of obturator jerk during transurethral resection
neurological postoperative complications can be reduced by of bladder tumor. JTUA 19: 27-31.
ultrasound guidance. An observational study was conducted on 257 9. Mydlo JH, Weinstein R, Shah S, Solliday M, Macchia RJ (1999) Long-
term consequences from bladder perforation and/or violation in the
patients underwent a pre-operative neurological examination before
presence of transitional cell carcinoma: Results of a small series and a
arthroscopy with sedation and ultrasound-guided interscalene or review of the literature. J Urol 161: 1128-1132.
supraclavicular block. The ultrasound video of the block offline was
10. Tatlisen A, Sofikerim M (2007) Obturator nerve block and transurethral
also displayed for two anesthesiologists who were blind to the study. 42 surgery for bladder cancer. Minerva Urol Nefrol 59: 137-141.
patients received Intraneural injection. No patient had postoperative 11. Akata T, Murakami J, Yoshinaga A (1999) Life-threatening haemorrhage
neurological complications at follow-up [31]. following obturator artery injury during transurethral bladder surgery: A
sequel of an unsuccessful obturator nerve block. Acta Anaesthesiol Scand
Conclusion 43: 784-788.
12. Fombon FN, Thompson JP (2006) Anesthesia for the adult patients with
Based on our current study results, ultrasound-guided nerve block rheumatoid arthritis. Contin Educ Anesth Crit Care Pain 6: 235-239.
is more suitable than nerve locator and has less morbidity for 13. Imagama S, Oishi Y, Miura Y, Kanayam Y, Ito Z, et al. (2010) Predictors of
Obturator block. But in my opinion every procedure needs practice aggravation of cervical spine instability in rheumatoid arthritis patients:
and one can be very skillful than others in a special method that is not The large joint index. J Orthop Sci 15: 540-546.
known as ‘choise’. 14. Moore DC (1980) Traditional or supraclavicular technique. Reg Anesth 5:
3-5.
Ethical Considerations 15. Prentiss RJ, Harvey GW, Bethard WF, Boatwright DE, Pennington RD
(1965) Massive adductor muscle contraction in transurethral surgery:
The objectives and procedure of the study was explained to all the Cause and prevention, development of electrical circuitry. J Urol 93:
263-271.
selected subjects and they were asked to sign the written informed
consent form. In addition the study protocol was approved by the 16. Parks CR, Kennedy WF (1967) Obturator nerve block: A simplified
approach. Anesthesiology 28: 775–778.
Ethics Committee of the local university.
17. Min HG, Cheon MY, Choi KT (2006) Use of nerve stimulator for the
The therapist undertook to avoid any disruption to the patient's obturator nerve block. Korean J Anesthesiol 50: 650-654.
treatment process and to maintain ethical issues throughout and after 18. Bolat D, Aydogdu O, Tekgul ZT, Polat S, Yonguc T, et al. (2015) Impact of
the operation. Eventually none of the patients experienced nerve stimulator-guided obturator nerve block on the short-term
complications from anesthetic procedures. outcomes and complications of transurethral resection of bladder
tumour: A prospective randomized controlled study. Can Urol Assoc J 9:
780-784.
Acknowledgments 19. Lee SH, Jeong CW, Lee HJ, Yoon MH, Kim WM (2011) Ultrasound
guided obturator nerve block: A single interfascial injection technique. J
Our other colleagues in the present study were: Houman
Anesth 25: 923-926.
Teymourian for designing the experiment, writing the manuscript and
providing significant advice; Yasmin Khazaie for collecting data and 20. Akkaya T, Ozturk E, Comert A, Ates Y, Gumus H, et al. (2009)
Ultrasound-guided obturator nerve block: A sonoanatomic study of a
consultation; Shayesteh Khorasanizadeh for analyzing the data and new methodologic approach. Anesth Analg 108: 1037-1041.
consultation; Mohammadreza Razaghi for providing significant advice 21. Augspurger RR, Donohue RE (1980) Prevention of obturator nerve
and consultation. stimulation during transurethral surgery. J Urol 123: 170-172.
22. Gasparich JP, Mason JT, Berger RE (1984) Use of nerve stimulator for
References simple and accurate obturator nerve block before transurethral resection.
J Urol 132: 291-293.
1. Swenson JD, Bay N, Loose E, Bankhead B, Davis J, et al. (2006)
23. Kobayashi M, Takeyoshi S, Takiyama R, Seki E, Tsuno S, et al. (1991) A
Outpatient management of continuous peripheral nerve catheters placed report of 107 cases of obturator nerve block. Jpn J Anesth 40: 1138-1143.
using ultrasound guidance: An experience in 620 patients. Anesth Analg
103: 1436-1443. 24. Dick A, Barnes R, Hadley H, Bergman RT, Ninan CA (1980)
Complications of transurethral resection of bladder tumors: Prevention,
2. Venkatramani V, Panda A, Manojkumar R, Kekre NS (2014) Monopolar recognition and treatment. J Urol 124: 810-811.
versus bipolar transurethral resection of bladder tumors: A single center,
parallel arm, randomized, controlled trial. J Urol 191: 1703–1707. 25. Collado A, Chéchile GE, Salvador J, Vicente J (2000) Early complications
of endoscopic treatment for superficial bladder tumors. J Urol 164:
3. Tekgül ZT, Divrik RT, Turan M, Konyalioglu E, Simsek E, et al. (2014) 1529-1532.
Impact of obturator nerve block on the short-term recurrence of
superficial bladder tumors on the lateral wall. Urol J 11: 1248–1252. 26. Malik MA, Nawaz S, Khalid M, Ahmad A, Ahmad M, et al. ( 2013)
Obturator Nerve Block (ONB) in transurethral resection of bladder
tumor (TURBT). JUMDC 4: 16-21.
J Clin Med Sci, an open access journal Volume 2 • Issue 1 • 1000106
Citation: Teymourian H, Khorasanizadeh S, Razzaghi MR, Khazaie Y (2018) Combination of Spinal Anesthesia and Obturator Nerve Block in
Transurethral Resection of Bladder Tumor, Comparison between Nerve Stimulator and Ultrasonography. J Clin Med Sci 2: 106.
Page 5 of 5
27. Traxer O, Pasqui F, Gattegno B, Pearle MS (2004) Technique and 30. Manassero A, Bossolasco M, Ugues S, Palmisano S, De Bonis U, et al.
complications of transurethral surgery for bladder tumours. BJU Int 94: (2012) Ultrasound-guided obturator nerve block: Interfascial injection
492-496. versus a neurostimulation-assisted technique. Regional Anesthesia and
28. Gi E, Yamauchi M, Yamakage M, Kikuchi C, Shimizu H, et al. (2014) Pain Medicine 37: 67-71.
Effects of local infiltration analgesia for posterior knee pain after total 31. Liu SS, Ya Deau JT, Shaw PM, Wilfred S, Shetty T, et al. (2011) Incidence
knee arthroplasty: Comparison with sciatic nerve block. J Anesthesia 28: of unintentional intraneural injection and postoperative neurological
696–701. complications with ultrasound-guided interscalene and supraclavicular
29. Helayel PE, Da Conceição DB, Pavei P, Knaesel JA, De Oliveira Filho GR nerve blocks. Anesthesia 68: 168-174.
(2007) Ultrasound-guided obturator nerve block: A preliminary report of
a case series. Regional Anesthesia and Pain Medicine 32: 221–226.
J Clin Med Sci, an open access journal Volume 2 • Issue 1 • 1000106
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Vdoc - Pub Performance Improvement in Hospitals and Health Systems Managing Analytics and Quality in Healthcare 2nd EditionDocument251 pagesVdoc - Pub Performance Improvement in Hospitals and Health Systems Managing Analytics and Quality in Healthcare 2nd EditionShalva BichiashviliNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Narcissist-Masochist Character by Arnold CooperDocument7 pagesNarcissist-Masochist Character by Arnold Coopercamarneiro21580No ratings yet
- Proyecto de Ayuda para Personas Con Discapacidad Auditiva "ESOB Tipo Collar"Document6 pagesProyecto de Ayuda para Personas Con Discapacidad Auditiva "ESOB Tipo Collar"César Fabián CHÁVEZ LINARESNo ratings yet
- Surgical Report - MRMDocument4 pagesSurgical Report - MRMapi-551638506No ratings yet
- REIS A. 2023. - Some Myths in Dentin Bonding - An Evidence-Based PerspectiveDocument8 pagesREIS A. 2023. - Some Myths in Dentin Bonding - An Evidence-Based PerspectiveNicolás SotoNo ratings yet
- P.E 12Document21 pagesP.E 12Gourisankar SNo ratings yet
- 2023 LoGFA TECHNOTESDocument13 pages2023 LoGFA TECHNOTESHedjarah MulokNo ratings yet
- Psychoanalytic Contributions of Karl Abraham To The Freudian LegacyDocument5 pagesPsychoanalytic Contributions of Karl Abraham To The Freudian LegacyPsychologydavidNo ratings yet
- Entry Level Dental Assistant Cover Letter SampleDocument8 pagesEntry Level Dental Assistant Cover Letter Samplezagybofun0v2100% (2)
- Sira 02ATEX4216X Iss3 ProtectedDocument4 pagesSira 02ATEX4216X Iss3 ProtectedfggsaNo ratings yet
- Sophia Sophia: St. Catherine University St. Catherine UniversityDocument25 pagesSophia Sophia: St. Catherine University St. Catherine UniversityEmmanuel Andrew Dela CruzNo ratings yet
- Office of The Information and Privacy Commissioner of Alberta - Public Inquiry 005994, University of Alberta Freedom of Information RequestDocument60 pagesOffice of The Information and Privacy Commissioner of Alberta - Public Inquiry 005994, University of Alberta Freedom of Information RequestWilliam Makis100% (3)
- Government College University, Faisalabad: Max Marks 32 (20+12)Document2 pagesGovernment College University, Faisalabad: Max Marks 32 (20+12)Arslan Muhammad EjazNo ratings yet
- Arnis ClubDocument6 pagesArnis ClubJohn Rico MalasagaNo ratings yet
- Intro To Critical Care NursingDocument4 pagesIntro To Critical Care NursingHain YoloNo ratings yet
- ACTION PLAN IN CanteenDocument2 pagesACTION PLAN IN CanteenMaria Eloisa MabborangNo ratings yet
- Dysphagia NotesDocument5 pagesDysphagia Notesapi-31372205650% (2)
- Why Do You Need A Healthcare App Development Company Like Moon TechnolabsDocument11 pagesWhy Do You Need A Healthcare App Development Company Like Moon TechnolabsJessicaNo ratings yet
- Baby Book Template Free PrintablesDocument22 pagesBaby Book Template Free Printablesapi-537172848No ratings yet
- Chemegic Job Interview QuestionnaireDocument5 pagesChemegic Job Interview QuestionnaireLuisa FernandaNo ratings yet
- Mindfulness Is Not Enough: Why Equanimity Holds The Key To CompassionDocument10 pagesMindfulness Is Not Enough: Why Equanimity Holds The Key To CompassionGabriela LópezNo ratings yet
- ValidityDocument2 pagesValidityAnonymous CgefymGwvNo ratings yet
- Abyip and Cbydp Quinabigan AbyipDocument23 pagesAbyip and Cbydp Quinabigan AbyipMark KevinNo ratings yet
- Certificate 2Document1 pageCertificate 2api-339742296No ratings yet
- Dsa Cerebral AngiographyDocument20 pagesDsa Cerebral AngiographyLalaine De JesusNo ratings yet
- Roles and Responsibilities of Contracting Parties Scope and ObjectivesDocument40 pagesRoles and Responsibilities of Contracting Parties Scope and ObjectivesSUBODH100% (1)
- Natural Medicine!: Let'S "Talk" AboutDocument35 pagesNatural Medicine!: Let'S "Talk" AboutPascal OGOUDIKPENo ratings yet
- 2023 ADVERT For ST Johns Institute of Health, Mulanje & Holy Family Colleges EditedDocument4 pages2023 ADVERT For ST Johns Institute of Health, Mulanje & Holy Family Colleges EditedGerald Tisewerenaye ChiloraNo ratings yet
- Republic of The Philippines Position Description Form DBM-CSC Form No. 1Document2 pagesRepublic of The Philippines Position Description Form DBM-CSC Form No. 1RomathoNo ratings yet
- Organic Food Product RMDocument17 pagesOrganic Food Product RMPranai MehtaNo ratings yet