Professional Documents
Culture Documents
Predicting Retinal Tears in Posterior Vitreous Detachment
Uploaded by
Zarella Ramírez BorreroOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Predicting Retinal Tears in Posterior Vitreous Detachment
Uploaded by
Zarella Ramírez BorreroCopyright:
Available Formats
Predicting retinal tears in posterior vitreous detachment
Kelly D. Schweitzer, MD*, Amaka A. Eneh, MD*, Jonathan Hurst, BS, MD*, Mark D. Bona, MD*,
Karim J. Rahim, MSc*, Sanjay Sharma, BSc, MD, FRCS, MS (Epid), MBA*
ABSTRACT ● RÉSUMÉ
Objective: The purpose of this study is to determine whether patients with acute posterior vitreous detachment (PVD) who develop
delayed retinal tears within the first 6 weeks after initial presentation have predictive characteristics.
Design: Prospective cohort study.
Participants: All patients presenting to the Hotel Dieu Hospital Emergency Eye Clinic between September 2008 and July 2009
diagnosed with acute PVD were offered enrollment.
Methods: At the initial visit, patients were given the previously validated Queen’s University Posterior Vitreous Detachment Patient Diary to
record their daily symptoms for 6 weeks. Two or 6 weeks later, patients were reexamined in detail, and their diaries were collected and
analyzed. Exact logistic regression was used to establish characteristics predictive of delayed retinal tears.
Results: In our study population of 99 patients, 2 developed delayed retinal tears. One had retinal hemorrhages and the other had a
cloud-like floater at initial presentation. Vitreal or retinal hemorrhage, large number of floaters at initial presentation, and high floater
frequency at initial presentation indicated a high risk of delayed retinal tear formation, yielding a median unbiased estimated odds ratio
of 36.18 with p value 0.009. No other presenting risk factors or symptomatology followed daily over the first 6 weeks after acute PVD
were predictive of delayed retinal tear formation.
Conclusions: PVD patients with retinal or vitreal hemorrhage, a significant number of floaters or a cloud like appearance to the floaters,
or high floater frequency are at higher risk of developing delayed retinal tears.
Objet : Déterminer si les patients atteints d’un décollement postérieur aigu du vitré (DPV), qui développent une déchirure de la rétine
à retardement dans les six premières semaines suivant la présentation, ont des caractéristiques prédictives.
Nature : Étude prospective de cohorte.
Participants : Tous les patients qui s’étaient présentés à la clinique d’urgence oculaire de l’Hôpital Hôtel-Dieu dans les mois de
septembre 2008 à juillet 2009 et avaient reçu un diagnostic de DPV aigu, ont été invités à participer.
Méthodes : À la première visite, les patients recevaient de l’Université Queen’s le Carnet de suivi du patient sur le décollement
postérieur du vitré pour y noter quotidiennement leurs symptômes pendant six semaines. Après deux ou six semaines, les patients
subissaient un nouvel examen approfondi et l’on recueillait et analysait les carnets. La régression logistique exacte servait à établir
les caractéristiques prédictives du retard des déchirures de la rétine.
Résultats : Parmi les 99 patients de notre étude, 2 avaient développé une déchirure rétinienne à retardement; l’un avait une hémorragie
rétinienne et l’autre, une apparence de corps flottants nuageux, à la première présentation. L’hémorragie du vitré ou de la rétine ainsi
que le grand nombre et la fréquence des corps flottants à la première présentation indiquaient un risque élevé de formation des
déchirures rétiniennes à retardement, donnant une probabilité moyenne estimée à 36,18 avec une valeur p de 0,009. Aucun autre
facteur de risque ou symptôme apparent dans les suivis quotidiens des 6 premières semaines suivant le DPV aigu n’a prédit la
formation des déchirures rétiniennes à retardement.
Conclusions : Les patients ayant un DPV avec hémorragie de la rétine ou du vitré, un nombre important de corps flottants ou de corps
flottants ayant l’apparence de nuages ou encore une forte fréquence de corps flottants courent davantage de risque de déchirures
de la rétine à retardement.
Posterior vitreous detachments (PVD) are a common tiple eye examinations. Thus, the management of PVDs
age-related condition among patients aged 45 years or consumes significant amounts of resources.4
older. The pathophysiology of PVD involves the separa- There is considerable interest in identifying symptoms
tion of the vitreous cortex from the internal limiting lam- that can predict the later development of retinal detach-
ina of the retina.1 This typically causes the patient to see ments or breaks so that follow-up visits can be reserved for
flashing lights and floaters at varying amounts of severity patients with serious risk factors. A recent study by van
and frequency.2 The main complications associated with Overdam et al.5 suggested that among patients with iso-
PVDs are retinal detachments or breaks either at initial lated PVDs, only those with more than 10 floaters, a cur-
presentation or at a later date.2,3 Therefore, all patients tain or cloud, vitreous hemorrhages, or retinal hemor-
presenting with flashes or floaters are typically examined rhages at initial presentation need to be rescheduled for a
using slit lamp biomicroscopy, indirect ophthalmoscopy, follow-up visit. All other patients can be instructed to re-
and scleral indentation both at initial presentation and turn if the number of floaters increases.
during a 6-week follow-up visit. PVDs have a high inci- The purpose of this study is to determine if our patients
dence in the general population and they necessitate mul- who present with acute PVD and later develop retinal tears
From the *Department of Ophthalmology, Queen’s University, Kingston, Can J Ophthalmol 2011;46:481– 485
Ont. 0008-4182/11/$-see front matter © 2011 Canadian Ophthalmological Society.
Published by Elsevier Inc. All rights reserved.
Originally received Feb. 26, 2011 Final revision Jun. 24, 2011 Accepted doi:10.1016/j.jcjo.2011.09.010
Jul. 28, 2011
Correspondence to Amaka Eneh, Hotel Dieu Hospital, Department of
Ophthalmology, 166 Brock Street, Kingston, ON K7L 5G2; 7aae1@
queensu.ca
CAN J OPHTHALMOL—VOL. 46, NO. 6, DECEMBER 2011 481
Predicting retinal tears in PVD—Schweitzer et al.
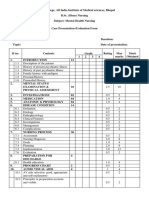
Fig. 1—Instructions sheet outlining the procedure for recording symptoms of posterior vitreous detachment in the Queen’s
University Posterior Vitreous Detachment Patient Diary. Floater shapes are represented in the lower left corner of the page. Groups
A, B, and C represent 1-3 floaters, 3-10 floaters, and >10 floaters respectively. Group D represents a curtain or cloud.
display these predictive characteristics, and to look for ad- as well as an attending staff physician, vitreoretinal fellow,
ditional predicting factors. or vitreoretinal surgeon.
On completion of the examination and a thorough ex-
METHODS planation of the nature of the diagnosis, enrollment and
consent was obtained. Each patient then received a
Study population Queen’s University Posterior Vitreous Detachment Pa-
All patients presenting to the Hotel Dieu Hospital Ur- tient Diary. The diary included an instructions sheet
gent Eye clinic diagnosed with acute PVD were offered (Fig. 1). The bulk of the diary centered around the main
enrollment in the study. The Urgent Eye clinic is a tertiary symptoms of PVD including the frequency and quality of
care centre accepting urgent referrals from ophthalmolo- photopsias and floaters. There was also room for any other
gists, optometrists, and medical doctors in Kingston and symptoms the patient wished to record (Fig. 2). At the
surrounding areas of southeastern Ontario. Exclusion cri- initial presentation, patient demographic information, vi-
teria of the study included retinal breaks or detachments at sual acuity, and risk factors for retinal tears were recorded
initial presentation, prior diagnosis of ocular disease, pa- in the diary. Risk factors included subjective vision loss,
tients under the age of 40 years or who had symptoms for family history of retinal detachment, myopia ⬎6D, pseu-
⬎1 month, or an identified history of blunt trauma to the dophakia, lattice degeneration, vitreous hemorrhage, reti-
eye. Patients with any history of ocular surgery except un- nal hemorrhage, and tobacco dust. Symptoms from the
complicated phacoemulsification cataract extraction with first day were recorded by the examining physician with
in the bag IOL insertion without posterior capsular rup- the patient’s input to ensure proper understanding. Four
ture or vitreous loss were also excluded. symptoms were recorded and they included floater fre-
All patients were asked about risk factors for retinal tears quency, floater group (A through D), flash frequency, and
and underwent a full ophthalmologic examination includ- flash intensity (1-10). The images of the various floater
ing slitlamp biomicroscopy, indirect ophthalmoscopy, and groups (Fig. 2) were adapted from van Overdam et al.4
scleral indentation. Goldmann 3-mirror examination was Groups A, B, and C represent 1-3 floaters, 3-10 floaters,
used as required based on clinical examination. All patients and ⬎10 floaters respectively. Group D represents a cur-
were seen by a Queen’s University ophthalmology resident tain or cloud (Fig. 1 and Fig. 2).4
482 CAN J OPHTHALMOL—VOL. 46, NO. 6, DECEMBER 2011
Predicting retinal tears in PVD—Schweitzer et al.
Fig. 2—Daily recording pages for PVD symptoms. These pages were duplicated to provide enough daily records to record
symptoms for 6 weeks after the initial visit. The floater groups adapted from van Overdam et al4 are in the top right hand corner.
Floater shapes are represented in the upper right corner of the page. Groups A, B, and C represent 1-3 floaters, 3-10 floaters, and
>10 floaters respectively. Group D represents a curtain or cloud.
All patients were examined at 6 weeks. If additional risk University Posterior Vitreous Detachment Patient Diary.
factors such as retinal or vitreal hemorrhage, or pigment Three patients were lost to follow-up. Nine patients were
visualized in the anterior vitreous were present on the ini- given 2-week follow-up appointments. In total, we analyzed
tial exam, patients had another exam 2 weeks after initial 99 diaries. Of these, 2 people developed retinal tears within 6
presentation. A full examination was repeated at each visit. weeks. One of these patients had both vitreous and retinal
At every visit, the patient was reminded to return to clinic hemorrhages and had been seen at a 2-week follow-up ap-
immediately if they noticed increasing photopsias, an in- pointment. The other patient reported a curtain or cloud pat-
creased number of floaters, or a visual field defect. All dia- tern of floaters at presentation (group D floaters).4
ries were collected at the 6-week visit. In our study, the first patient presenting with a delayed
Study design was approved by the Queen’s University retinal tear had group D floaters but also presented with
Research Ethics Review Board. the highest floater frequency possible, and did not indicate
any change in floater frequency. In terms of flashes, this
Data analysis
patient only reported flashes on a total of six days during
Longitudinal data from the diary was recorded on Mi-
crosoft Excel (Microsoft, Seattle, Wash) and statistical analysis the 6-week study period. The intensity ranged from 2 of 10
was done using version 9.2 of the SAS System for Windows to 5 of 10 and the flash frequency, when flashes occurred,
(SAS Institute, Cary, NC). Retinal or vitreous hemorrhage, was once every 18 h. The second patient presenting with a
and multiple floaters at presentation (group C or D) were delayed retinal tear had retinal hemorrhages at presenta-
tested with exact logistic regression.5-7 In addition, any longi- tion. This patient had group A floaters throughout the
tudinal changes in the 4 symptoms recorded in the diary that study period and demonstrated no changes in flash fre-
may predict a retinal tear were explored. quency or intensity. However, this patient did report a
decrease in floater frequency from once every minute to
RESULTS once every hour on day 3. On day 28, there was another
decrease in floater frequency to once every 6 h. Regardless
Over the course of the study, 2 patients offered enrollment of the decrease noted in floater frequency, this patient
declined participation due to an inability to keep the 6-week would still have been scheduled for follow-up because he/
follow-up visit. A total of 102 patients were given a Queen’s she had a retinal hemorrhage at presentation.
CAN J OPHTHALMOL—VOL. 46, NO. 6, DECEMBER 2011 483
Predicting retinal tears in PVD—Schweitzer et al.
Table 1—Sensitivity, specificity, positive likelihood ratios, and positive and negative predictive values of the criteria for
re-examination for delayed retinal tears among acute PVD patients proposed by van Overdam et al.5 and the effects of
including 1 additional criterion (high flash frequency at presentation)
Predictor Sensitivity (%) Specificity (%) Positive Positive Predictive Negative Predictive
Likelihood Ratio Value (%) Value (%)
Hemorrhage or floaters in group C or D 100 84.5 6.45 11.8 100
Hemorrhage or floaters in group C or D combined with
initial floater frequency of once every 6 h or higher 100 87.6 8.06 14.3 100
Hemorrhage or floaters in group C or D combined with
initial floater frequency of once every hour or higher 100 88.7 8.85 18.2 100
Hemorrhage or floaters in group C or D and initial floater
frequency once every minute 100 94.8 19.2 40.0 100
In total, 15 of 99 patients in our study fulfilled the within the above group should be asked to return for reex-
criteria for scheduling a follow-up visit, namely, vitreal or amination only if they experience an increase in the num-
retinal hemorrhage and group C or D floaters. Because ber of floaters.5 Our prospective cohort study on patients
these criteria captured our 2 patients who developed de- presenting with delayed retinal tears is supportive of this
layed retinal tears, they displayed 100% sensitivity for our basic predictive pattern that only patients with either large
study population. The specificity, positive predictive value, or numerous floaters, or retinal or vitreal hemorrhages
and likelihood ratios were 84.5%, 11.8%, and 6.45 respec- need to be scheduled for a follow-up visit after experienc-
tively (Table 1). The median unbiased estimated odds ratio ing acute PVD.5 One important caveat is that based on our
(OR) was 12.244 (p ⫽ 0.0561) (Table 2). In addition, our data, we are unable to support or refute the common
data suggested that stronger predictors can be explored by dogma that increasing floaters are predictive of delayed
considering the floater frequency at presentation. As both retinal tears. This is because both our patients who experi-
patients presenting had the highest floater frequency, we enced delayed retinal tears presented initially with floaters
attempted models that included high floater frequency at at the maximum frequency. In fact, one of them indicated
presentation. We found that when using hemorrhage, a decrease in floater frequency. However, this is insignifi-
group C or D floaters, and the highest floater frequency at cant as the patient who described a decrease in floaters
presentation, the estimated the OR was 36.18 (p ⫽ 0.009) would have been scheduled for a follow-up appointment
(Table 2). The sensitivity remained 100%, and the speci- based on the other factors suggested for follow-up, e.g.,
ficity increased to 94.8%. The likelihood ratio increased to numerous or cloud-like floaters at presentation.
19.2, and the positive predictive value increased to 40.0% Our data also indicates that follow-up criteria can be
(Table 1). Again, we used exact logistic regression to com- further refined by exploring floater frequency at presenta-
pensate for the small sample size. tion. By including the highest floater frequency in the
We did not detect any changes in floater frequency, aforementioned criteria, we found that as the specificity of
floater type, flash frequency, or flash intensity over the the criteria increased, so did the estimated OR.
6-week period that were predictive of delayed retinal tears. Because some patients were assessed by an attending
Nor were the other risk factors recorded at presentation staff physician or vitreoretinal fellow rather than by a
predictive of delayed retinal tears. vitreoretinal attending physician, it is theoretically pos-
sible that some retinal tears were not detected at the
DISCUSSION initial presentation. However, all patients received de-
tailed scleral depression indirect and 3-mirror gonio-
It has been suggested that patients with floater group C scopic retinal examination.
or D or vitreal or retinal hemorrhages at presentation The main limitation of this study is the small number of
should be scheduled for reexamination.5 Patients not delayed retinal tears, despite that we were able to confirm
Table 2—Estimated OR of the criteria for reexamination for delayed retinal tears among acute PVD patients proposed by van
Overdam et al.5 and the effects of including 1 additional criterion (high flash frequency at presentation)
Predictor Predicted Observed Exact OR P
Tears (n) Tears (n) Value
Hemorrhage or floaters in group C or D 15 2 12.2 0.056
Hemorrhage or floaters in group C or D combined with initial floater frequency of once every
6 h or higher 12 2 15.6 0.0375
Hemorrhage or floaters in group C or D combined with initial floater frequency of once every
hour or higher 11 2 17.1 0.0322
Hemorrhage or floaters in group C or D and initial floater frequency once every minute 5 2 36.2 0.0087
Note: OR, odds ratio.
484 CAN J OPHTHALMOL—VOL. 46, NO. 6, DECEMBER 2011
Predicting retinal tears in PVD—Schweitzer et al.
the predictive value of the previously suggested acute PVD REFERENCES
follow-up criteria. We suggest floater frequency at presen-
tation as a possible addition to these criteria. The small 1. Hogan MJ. The vitreous: its structure in relation to the ciliary body and
retina. Invest Ophthalmol. 1963;2:418.
number of delayed retinal tears may also contribute to our 2. Hollands H, Johnson D, Brox AC, Almeida D, Simel DL, Sharma S.
inability to detect any changes in daily symptoms that Acute-onset floaters and flashes: is this patient at risk for retinal detach-
might also have been predictive of delayed retinal tears. ment? JAMA. 2009;302:2243-9.
3. Novak MA, Welch RB. Complications of acute symptomatic posterior
Nonetheless, given that the follow-up of patients with vitreous detachment. Am J Ophthalmol. 1984;97:308-14.
PVD requires a considerable amount of resources, it is 4. van Overdam KA, Bettink-Remeijer MW, Mulder PG, van Meurs JC.
worthwhile to confirm the findings of this study by ex- Symptoms predictive for the later development of retinal breaks. Arch
Ophthal. 2001;119:1483-6.
panding it to include more centers, longer follow-up inter- 5. van Overdam KA, Bettink-Remeijer MW, Klaver CC, Mulder PG, Moll
vals, and a larger sample size. AC, van Meurs JC. Symptoms and findings predictive for the develop-
ment of new retinal breaks. Arch Ophthal. 2005;123:479-84.
6. Cox DR, Snell EJ. Boca Raton (FL): Analysis of Binary Data. Chapman &
Hall/CRC, 1989.
Disclosures: The authors have no proprietary or commercial inter- 7. Hirji KF, Tang ML. A comparison of tests for trend. Commun Stat Theory
est in any materials discussed in this article. Methods. 1998;27:943-63.
CAN J OPHTHALMOL—VOL. 46, NO. 6, DECEMBER 2011 485
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- 12 Astrology Houses & Planets in HousesDocument22 pages12 Astrology Houses & Planets in HousesSreerangam Narasimharao100% (4)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- 2010 Handbook On Discovery Practice, Trial Lawyers Section of The Florida Bar & Conferences of The Circuit and County Courts JudgesDocument124 pages2010 Handbook On Discovery Practice, Trial Lawyers Section of The Florida Bar & Conferences of The Circuit and County Courts JudgesFloridaLegalBlog100% (3)
- EmotionalIntelligence TestDocument65 pagesEmotionalIntelligence Testjogutierrez100% (2)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Lord of The Rings Real HistoryDocument2 pagesThe Lord of The Rings Real HistoryDUNCAN0420No ratings yet
- MBT Basic Trainig Clinical Slides NEW OCT 2017 No Video 002Document171 pagesMBT Basic Trainig Clinical Slides NEW OCT 2017 No Video 002Naeem KhanNo ratings yet
- Kripal, Debating The Mystical As The Ethical: An Indological Map, in Crossing Boundaries: Essays On The Ethical Status of Mysticism (2002) : 15-69Document28 pagesKripal, Debating The Mystical As The Ethical: An Indological Map, in Crossing Boundaries: Essays On The Ethical Status of Mysticism (2002) : 15-69Keren MiceNo ratings yet
- Suspension Cable BridgesDocument29 pagesSuspension Cable Bridgesrameshbabu_197967% (3)
- Pastor. The History of The Popes, From The Close of The Middle Ages. 1891. Vol. 31Document540 pagesPastor. The History of The Popes, From The Close of The Middle Ages. 1891. Vol. 31Patrologia Latina, Graeca et Orientalis100% (1)
- Microbiology ExamDocument10 pagesMicrobiology ExamRustom Jose RojoNo ratings yet
- Pink Panther - Diabetes Management - Chapter 2Document6 pagesPink Panther - Diabetes Management - Chapter 2jennmoyerNo ratings yet
- Assessment of Critical Success Factors For Construction Projects in PakistanDocument13 pagesAssessment of Critical Success Factors For Construction Projects in PakistanAbdul Qayoom Memon100% (1)
- Demo DexDocument15 pagesDemo DexZarella Ramírez BorreroNo ratings yet
- Largo PlazoDocument6 pagesLargo PlazoZarella Ramírez BorreroNo ratings yet
- Limpia DorDocument7 pagesLimpia DorZarella Ramírez BorreroNo ratings yet
- COMPLETODocument9 pagesCOMPLETOZarella Ramírez BorreroNo ratings yet
- Oct y Eco VitreoDocument6 pagesOct y Eco VitreoZarella Ramírez BorreroNo ratings yet
- Ultrasound in Emergency Medicine: Use of Ocular Ultrasound For The Evaluation of Retinal DetachmentDocument5 pagesUltrasound in Emergency Medicine: Use of Ocular Ultrasound For The Evaluation of Retinal DetachmentZarella Ramírez BorreroNo ratings yet
- Effect of Audit Findings and Audit RecommendationDocument25 pagesEffect of Audit Findings and Audit RecommendationDwi Puspita SariNo ratings yet
- VariationDocument3 pagesVariationavantika5100% (1)
- Core Values WorkbookDocument16 pagesCore Values WorkbooktokabondaNo ratings yet
- Snow White and Seven Dwarf'sDocument2 pagesSnow White and Seven Dwarf'snur aidhaNo ratings yet
- Leif Eriksson-Annotated BibDocument7 pagesLeif Eriksson-Annotated Bibapi-308958050No ratings yet
- Role-Play #1: Saving Energy: WellDocument4 pagesRole-Play #1: Saving Energy: WellDaniel VasquezNo ratings yet
- 6QQMN969 Module OutlineDocument4 pages6QQMN969 Module OutlineyuvrajwilsonNo ratings yet
- 2G Feature ListDocument135 pages2G Feature ListPraveen DubeyNo ratings yet
- Unit 5 Student EditionDocument30 pagesUnit 5 Student Editionapi-233507392No ratings yet
- Daftar PustakaDocument11 pagesDaftar PustakaHilyaNo ratings yet
- O'Grady Cap 1Document12 pagesO'Grady Cap 1BarbaPardaNo ratings yet
- Hsyallx: Tutorial Letter 301/3/2023Document32 pagesHsyallx: Tutorial Letter 301/3/2023Lebohang MalauNo ratings yet
- Evaluation Form MSCDocument5 pagesEvaluation Form MSCvikash kumarNo ratings yet
- 11126-574002-EAT342 Hydraulically Powered Block Lifter INT MODERATED PDFDocument8 pages11126-574002-EAT342 Hydraulically Powered Block Lifter INT MODERATED PDFsaqibNo ratings yet
- 3 Disability ModelsDocument28 pages3 Disability ModelszainbNo ratings yet
- Presentations 2023Document6 pagesPresentations 2023Tawanda MatongeraNo ratings yet
- Design Research On Traffic Congestion in BangaloreDocument29 pagesDesign Research On Traffic Congestion in BangaloreBhagvanji Sonagra100% (2)
- Adjuvant Icotinib Versus Observation in Patients WDocument11 pagesAdjuvant Icotinib Versus Observation in Patients WVanilson BorgesNo ratings yet
- NP and Computational Intractability: Slides by Kevin Wayne. All Rights ReservedDocument52 pagesNP and Computational Intractability: Slides by Kevin Wayne. All Rights ReservedpreethiNo ratings yet