Professional Documents
Culture Documents
Medical Records Young Brave Female Traditional Chinese Medicine (TCM) Doctor Fighting COVID-19
Uploaded by
Fernanda BrenteganiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Medical Records Young Brave Female Traditional Chinese Medicine (TCM) Doctor Fighting COVID-19
Uploaded by
Fernanda BrenteganiCopyright:
Available Formats
恐惧来自无知,英雄来自中医 一位智勇双全的青年女中医医生抗击新冠肺炎纪实
Fear Comes from Ignorance, Redemption Comes from Chinese Medicine.
Medical Records from a Young
and Brave Female Traditional
Chinese Medicine (TCM)
doctor on Fighting the COVID-19
by Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang
Compiled and Translated by John K. Chen, Pharm.D., PhD., OMD, LAc
Editors: Debra Nash-Galpern, L.Ac., DiplOM, Robert Chu, L.Ac.,OME,
Lorraine Wilcox, L.A.c, Rina Sasmita, Donna Chow, L.Ac., DiplOM
Today, I want to share my experience treating 30 COVID-19 patients from the beginning
to the end with you. I treated every single patient from admission to discharge, and I
hope my experience can provide some insights for you.
One of the similarities of these 30 patients is that the time of onset of their illness
is relatively close. Admission date for all of these patients was February 4, 2020,
except for a few patients who were admitted on February 5, 2020. Through my
observations of the course of their illness, I hope to provide a small clinical group
study.
When I first started treating COVID-19 patients, my approach was multifaceted since
I had read and considered the excellent presentations by many of my teachers. Luckily,
Dr. Zhang Ying Liang and Dr. Zhang Chang were able to give me specific guidance and
assurance that I believe made a significant difference.
©2020 Lotus Institute of Integrative Medicine eLotus.org
Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang • Medical Records from a Young and Brave Female Traditional Chinese Medicine (TCM) doctor on Fighting the COVID-19 2
I specialize in difficult-to-treat conditions. Hence, when I first started seeing COVID-19
patients, naturally I was prepared to consider many different factors, including individual
patient constitution, the state of their Qi and blood, 8 principles, and Zang Fu differential
diagnosis. Yet, more than usual, these patients seemed to share similar presentations to
one another, therefore I was able to generally determine a common treatment plan.
THE PRINCIPLE SIMILARITY AMONGST THE THIRTY PATIENTS
What I noticed is that virtually all of these patients had a fever, and those who did
not, had chills. Furthermore, most patients presented with cold extremities; while
some had perspiration, others did not have any perspiration. Additionally, patients
experienced headache, nausea, a bitter taste in the mouth, and dry throat. The most
common symptom they all shared was a dry cough. Of these 30 patients, only a few
could expectorate phlegm.
I observed an intriguing detail in most cases. Their tongue coatings were thick, white,
and greasy, while my teacher from Changsha, a different geographical region located
300 kilos away, detected a different tongue coating. The question arose as to whether
tongue coatings were different due to geography and weather, or because most of my
teacher’s patients received more treatment prior to admission than my patients.
Please see the photos below of my patients’ tongues. These pictures were taken on the
first or second day of their admission to the hospital.
© 2020 Lotus Institute of Integrative Medicine eLotus.org
Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang • Medical Records from a Young and Brave Female Traditional Chinese Medicine (TCM) doctor on Fighting the COVID-19 3
To track their tongues over time, I set up a WeChat group for each patient and asked
them to send a picture of their tongue each morning. Along with their tongue photo, I
asked them to report their symptoms, energy level, sleep, appetite, urination, defecation,
aversion to cold, cold sensation in the extremities or the back, perspiration, including
whether they had hot or cold sweat, and if the amount of perspiration was profuse,
scanty, or oily. I also asked them to report their facial complexion and what medications
they were using, and if they were having any positive or negative reactions to those
medications.
© 2020 Lotus Institute of Integrative Medicine eLotus.org
Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang • Medical Records from a Young and Brave Female Traditional Chinese Medicine (TCM) doctor on Fighting the COVID-19 4
As “necessity is the mother of invention”, this WeChat format actually became
our method of intake for these patients. This has become the method that we now
communicate with all our patients. My colleagues and I compiled and analyzed all this
information, including daily photos, and we came to the conclusion that the majority
of these 30 patients had the diagnosis of Cold-Damp Invading the Lungs.
© 2020 Lotus Institute of Integrative Medicine eLotus.org
Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang • Medical Records from a Young and Brave Female Traditional Chinese Medicine (TCM) doctor on Fighting the COVID-19 5
TYPES OF WESTERN MEDICATIONS AND HERBS USED DURING TREATMENT
PERIOD
As this is an Integrative TCM and Western medicine hospital, our approach to the
COVID-19 virus, was to utilize both types of medicine. The Western medicine route
offered oral antiviral drugs such as Oseltamivir and Abidol. The critically ill patients
were given supportive therapy. IV fluids were strictly monitored. If they were still able to
eat, we generally did not administer fluids, as we felt they were getting enough. From the
Chinese medical perspective, we had to make a differential diagnosis before prescribing
herbs. Integrative therapy seemed like it would provide better results. Furthermore, this
provided the rare opportunity to fully embrace the essence of the Shang Han Lun. I
knew then that my understanding of COVID-19 was deepening, and that it would leave
a lasting impression on me.
As most patients had the diagnosis of Cold-Damp in the Lungs, they primarily
received the oral antiviral medications, Oseltamivir and Abidol. We observed
that some patients required IV fluids. The primary Chinese medicine formulas
used with these medications were:
• Xiao Chai Hu Tang (Minor Bupleurum Decoction)
• Chai Hu Gui Zhi Tang (Bupleurum and Cinnamon Twig Decoction)
• Ma Huang Fu Zi Xi Xin Tang (Ephedra, Asarum, and Prepared Aconite
Decoction)
• Gua Lou Xie Bai Ban Xia Tang (Trichosanthes Fruit, Chinese Chive, and Pinellia
Decoction)
© 2020 Lotus Institute of Integrative Medicine eLotus.org
Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang • Medical Records from a Young and Brave Female Traditional Chinese Medicine (TCM) doctor on Fighting the COVID-19 6
Almost All Patients Required Ma Huang (Herba Ephedrae)
Throughout the entire treatment process, regardless of which formula was used,
Ma Huang (Herba Ephedrae) was found to be an essential adjunct to treatment.
Initially, there was a great deal of dispute regarding the use of Ma Huang (Herba
Ephedrae), but those debates were quickly put to rest when we saw how effective it was.
When COVID-19 started around mid-January, 2020, I began to receive many calls daily
from patients. While my colleagues and I analyzed their x-rays, we did not pay too much
attention to the gravity of the illness, until we were actively working with patients.
What I noticed was that while many patients were experiencing symptomatic relief, their
CT scans were showing the progression of the disease. It showed the worsening of lung
conditions as the white area in the scan continued to show expansion. Surprisingly, the
© 2020 Lotus Institute of Integrative Medicine eLotus.org
Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang • Medical Records from a Young and Brave Female Traditional Chinese Medicine (TCM) doctor on Fighting the COVID-19 7
patient’s sleep, appetite, energy level, etc. were, by and large, improving. At first, I was
baffled and tried to explore possible explanations for this phenomenon. Hence, I asked
my senior colleague whether he thought it was possible that phlegm was unsuspectingly
lodging in the lungs of patients.
What my patients reported was that once they expectorated the sputum, their respiration
felt much more open. This was especially the case for patients with a dry cough, for the
30 patients I was overseeing. They all experienced the same thing: difficult inhalation,
but normal exhalation. So, with that in mind, I insisted on using Ma Huang (Herba
Ephedrae) for all my patients from that time forward.
Throughout the entire treatment period from February 4, 2020 through February 20,
2020, most of the critically ill patients became mild cases and most mild cases
were released out of the hospital with this integrative approach to care. From
this, we learned that Ma Huang (Herba Ephedrae) was pivotal in achieving exceptional
results for these 30 patients.
Following this experience, I now highly recommend the use of Chinese herbs to
treat COVID-19, in all of its stages. Though the use of herbs is non-invasive with
relatively mild side effects, it is not only effective to treat mild and mid-stages of
this illness, it can also help prevent patients from moving into the more critical
stages of this disease. However, I cannot stress the importance of achieving
accurate diagnosis and regularly updated herbal prescriptions for the particular
stage of illness. Below, please find a few case studies, with explanations for each one.
CASE 1
A female patient in Bed #4, was admitted to the hospital on 2/4/20, with a high fever
of approximately 41°C (105.8°F), nucleic acid detection (+). She also exhibited severe
chest pain, dyspnea, respiratory difficulty, and her blood oxygen saturation level was
97%. Furthermore, she was unable to get out of bed, had insomnia due to chest pain,
with an inability to eat. She was served one bowl of porridge and she could not even
finish that. This patient was barely able to talk, and when she did, she had a very feeble
© 2020 Lotus Institute of Integrative Medicine eLotus.org
Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang • Medical Records from a Young and Brave Female Traditional Chinese Medicine (TCM) doctor on Fighting the COVID-19 8
voice. I noticed that each time she tried to speak, her words were shortened due
to the need to inhale mid-sentence. However, it did not seem that her exhalation
was affected. The patient also could not sleep due to the pain, and she expressed that
she felt all her ribs were going to break. She did not feel that she had COVID-19,
rather, she felt her ribs were broken. She was emotional, understandably, and very fragile.
Modified Ma Huang Xia Zhu Tang and Gua Lou Xie Bai Ban Xia Tang (Trichosanthes Fruit,
Chinese Chive, and Pinellia Decoction) were prescribed. On 2/7/20 her temperature
was under control and chest pain, and dyspnea improved. On 2/20/20 the patient
© 2020 Lotus Institute of Integrative Medicine eLotus.org
Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang • Medical Records from a Young and Brave Female Traditional Chinese Medicine (TCM) doctor on Fighting the COVID-19 9
had only a moderate cough with phlegm and no other symptoms. Nucleic acid test (-).
Tongue is shown here for comparison.
The Western medicines, Ofloxacin and Ribavirin, were prescribed. I insisted on not
giving her steroids because of the large area of ground-glass opacity (GGO). Steroids
would cause further spreading of the infection and make recovery more difficult.
Therefore, she was only given Chinese herbs.
By 2/7/20, her temperature was under control and her chest pain and dyspnea were
somewhat better. However, what worried me was that her cough was worse. I was a bit
nervous especially since I am a Western Medical doctor who learned Chinese medicine
on my own, so my intuition to avoid the use of steroids raised a lot of questions
amongst my peers. When the patient said her cough worsened after taking the herbs, I
asked her, “Do you feel worse, or do you feel that your chest is tight after you cough?”
She said, “No, after I cough, I feel better, especially if I can cough out some sputum. I
feel the chest is more open.” After hearing that, I was very confident I was on the right
path. After her temperature was normal, we did not give her any more Ma Huang Fu
Zi Xi Xin Tang (Ephedra, Asarum, and Prepared Aconite Decoction). Instead, I used a
modified version of Gua Lou Xie Bai Ban Xia Tang (Trichosanthes Fruit, Chinese Chive,
and Pinellia Decoction) and added a large amount of Zi Su Zi (Fructus Perillae), Jiang
Can (Bombyx Batryticatus), Di Long (Pheretima), Fu Ling (Poria), and more. The key
was to open her congested chest and help her expectorate the phlegm.
After taking 3 more doses, following 9 days of herbs, her situation improved
dramatically. Previously, she was only able to lie down and was not able to get
out of bed. Sometimes, the nurse had to help feed her meals. But on 2/13/20,
her voice was robust and she was able to get out of bed. However, she said she still
felt a little bit of pain in her chest when she coughed or moved.
After that, the subsequent formulas were relatively easy to discern. I used Gua Lou Xie
Bai Ban Xia Tang (Trichosanthes Fruit, Chinese Chive, and Pinellia Decoction).
© 2020 Lotus Institute of Integrative Medicine eLotus.org
Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang • Medical Records from a Young and Brave Female Traditional Chinese Medicine (TCM) doctor on Fighting the COVID-19 10
Below, please find her CT scans over time.
In this CT scan, it is clear that her infection is very severe. A quarter of her lungs
were covered with ground-glass opacity (GGO). Her initial clinical manifestation
corresponded precisely with the CT result.
© 2020 Lotus Institute of Integrative Medicine eLotus.org
Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang • Medical Records from a Young and Brave Female Traditional Chinese Medicine (TCM) doctor on Fighting the COVID-19 11
On 2/19/20, her CT showed that much of GGC had dissipated. Furthermore, both of
her nucleotide tests were negative. Yet, as regulations are strict from our headquarters,
we were not yet allowed to discharge the patient.
The main herbal formulas I used for this patient throughout the treatment were Ma
Huang Jia Zhu Tang (Ephedra Decoction plus Atractylodes) and Gua Lou Xie Bai Ban
Xia Tang (Trichosanthes Fruit, Chinese Chive, and Pinellia Decoction).
© 2020 Lotus Institute of Integrative Medicine eLotus.org
Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang • Medical Records from a Young and Brave Female Traditional Chinese Medicine (TCM) doctor on Fighting the COVID-19 12
CASE 2
The next case is regarding a male patient in Bed #14. This patient is 57 years old and
contracted the COVID-19 virus at home through a family gathering. Along with most
of his relatives, they are all in the hospital and experiencing severe symptoms. This
patient had a cough and fever 9 days prior to being admitted to the hospital. His fever
was not so high, so he took some over-the-counter drugs at home first. When he was a
confirmed case and admitted to our hospital on 2/4/20, his fever was as high as 39°C
(102.2°F). His presentation was more severe than the previous patient. For this patient,
we decided to put him on the steroid, Methylprednisolone. Previously, I felt steroids
would be inappropriate, but didn’t fully realize the side effects in COVID-19 patients,
until this patient. His CT clearly displayed slowed absorption. In other words, he would
need to stay in the hospital much longer than others.
© 2020 Lotus Institute of Integrative Medicine eLotus.org
Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang • Medical Records from a Young and Brave Female Traditional Chinese Medicine (TCM) doctor on Fighting the COVID-19 13
The difference I noticed with this patient is that, unlike others who were relatively
comfortable speaking, he didn’t want to talk to anyone and his spirits were very
low. He said he felt chest congestion and did not wish to get out of bed. I asked him
if he had dry mouth and he said that he did not, but that he had aversion to cold.
Reportedly, he felt cold everywhere in the body but had no perspiration. His
neutrophils, amyloid, and calcitonin levels were all abnormal. His transaminase level
was abnormal and his urine protein was 1+. At the time, his blood oxygen saturation
was only 93%, so I thought the test results and his mental condition and symptoms
were consistent.
This patient had aversion to cold, chills, preference to continuous sleep, poor spirits,
and a low energy level. As he reported an absence of thirst, I gave him Ma Huang Fu
Zi Xi Xin Tang (Ephedra, Asarum, and Prepared Aconite Decoction) with a little bit of
Ren Shen (Radix et Rhizoma Ginseng). Furthermore, given his high temperature and his
low energy, 80 mg of Methylprednisolone, a steroid, was administered, by the attending
physician that evening. The next day, his temperature normalized, but his blood oxygen
levels remained at 93%.
On 2/9/20, the patient still had chest congestion, dry cough, and no desire to move.
I had initially thought it was because he was more petite and weak, but his son-in-law
told me that the patient does physical work and was usually very healthy and strong. So,
I tried to convince my supervisor to stop using the steroids.
I was against administrating gamma globulin. I could not understand why it was necessary
to use it in this case. So on 2/9/20, I insisted we stop the steroids and my supervisor
agreed. We also took out the gamma globulin. By then, the patient’s temperature had
already returned to normal with the steroid use.
© 2020 Lotus Institute of Integrative Medicine eLotus.org
Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang • Medical Records from a Young and Brave Female Traditional Chinese Medicine (TCM) doctor on Fighting the COVID-19 14
2/9/20 I prescribed Ma Huang Fu Zi Xi Xin Tang (Ephedra, Asarum, and Prepared
Aconite Decoction) and added Dang Shen (Radix Codonopsis) and Sheng Sai Shen (dried
ginseng). I also added Zi Su Zi (Fructus Perillae), Jiang Can (Bombyx Batryticatus), Cang
Zhu (Rhizoma Atractylodis), Fu Ling (Poria). Please note that all the herbs I used this
time were extracted granules. I found that both extract granules and decoctions
yielded similar results.
After the patient took the formula for a few days, on 2/12/20, we astonishingly found
that he was able to get out of bed. Not only did he get out of bed, but he was
talking to others and eating normally without help! Between 2/4/20 and 2/9/20
he could only eat porridge and nothing else because he said he did not feel hungry and
he could barely swallow the porridge.
On 2/12/20, he wanted to order a box lunch from the set menu, and I was ecstatic. The
patient expressed through WeChat that his chest congestion was better, but that he was
still coughing severely, and the white phlegm could easily be expectorated. He no longer
felt his chest was congested with phlegm because it had loosened up. Given his overall
recovery, I modified the formula and gave him Ma Huang Fu Zi Xi Xin Tang (Ephedra,
Asarum, and Prepared Aconite Decoction) with San Ren Tang (Three-Nut Decoction).
© 2020 Lotus Institute of Integrative Medicine eLotus.org
Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang • Medical Records from a Young and Brave Female Traditional Chinese Medicine (TCM) doctor on Fighting the COVID-19 15
Below, please find his CT result.
This was the first scan when he was administered on 2/5/20. You can see his lungs were
severely damaged. It was my opinion, the alveoli were severely compromised.
© 2020 Lotus Institute of Integrative Medicine eLotus.org
Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang • Medical Records from a Young and Brave Female Traditional Chinese Medicine (TCM) doctor on Fighting the COVID-19 16
As you can see from the following CT result, on 2/9/20, there is an improvement.
Correspondingly, this is when he stated that his symptoms were improving as well.
© 2020 Lotus Institute of Integrative Medicine eLotus.org
Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang • Medical Records from a Young and Brave Female Traditional Chinese Medicine (TCM) doctor on Fighting the COVID-19 17
On 2/24/20, the medical team on the entire floor was very happy for him and his
family because his CT scan showed that the lungs were obviously clearing significantly.
As members of his family were all healing in the same unit, it would have been tragic,
and may have potentially affected their healing, if he had worsened and not improved.
© 2020 Lotus Institute of Integrative Medicine eLotus.org
Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang • Medical Records from a Young and Brave Female Traditional Chinese Medicine (TCM) doctor on Fighting the COVID-19 18
On 2/20/20, the patient felt generally great and had very little to no symptoms. He had
an occasional mild cough, but no sputum. We recommended that the patient remain in
the hospital for a few more days before going home.
© 2020 Lotus Institute of Integrative Medicine eLotus.org
Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang • Medical Records from a Young and Brave Female Traditional Chinese Medicine (TCM) doctor on Fighting the COVID-19 19
MY CONCLUSION AFTER REVIEWING PATIENT’S CT RESULTS
Through my observation of CT scans thus far, I concluded the following:
If the CT of the recovered patients showed very clear dark spots, I would ask the
patient “How was your body constitution prior to contracting the COVID-19?” Most
would answer very good. I would then ask, “Did you feel you were easily tired or would
perspire easily?” Most would say no.
However, if the markings in the lungs looked thicker than the rest and the dark area is
not as bright and clear, these patients would tell you that they had difficulty breathing
prior to contracting COVID-19 and exhibited frequent fatigue and easy perspiration.
So, with this in mind, I discussed with my colleagues the concept of whether or not
we could diagnose Lung Qi deficiency through CT results. As this is just a hypothesis,
I am uncertain if it is accurate, however, in reviewing the patient in bed #14 it is clear
to see that in a matter of 15 days from the initial CT to the last CT, there were great
improvements.
All Patients Discharged No Longer Had a Thick, White, Greasy Tongue Coating
Below, please find pictures of Case #2 both on 2/4/20 and on 2/20/20. Please note
the immense difference in the images. At first, I questioned whether it was a scan of the
same person, or if the camera was defective because there was such a dramatic change.
To be certain, I requested the photo be taken again (see below).
© 2020 Lotus Institute of Integrative Medicine eLotus.org
Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang • Medical Records from a Young and Brave Female Traditional Chinese Medicine (TCM) doctor on Fighting the COVID-19 20
After compiling all information about these 30 patients, including the recordings of
how their tongues had changed, they were ready to be discharged.
© 2020 Lotus Institute of Integrative Medicine eLotus.org
Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang • Medical Records from a Young and Brave Female Traditional Chinese Medicine (TCM) doctor on Fighting the COVID-19 21
The following is a compilation of all the tongue photos, and it is clear that none of the
patients had the thick, white, greasy tongue coating anymore. I cannot say they
are all normal tongue coatings but the patients told me that the state of their current
tongue after my treatments was the same as what it looked like prior to contracting the
COVID-19 virus.
Continue Phlegm Eliminating Herbs Throughout the Course of Treatment
I also recognized a similar pattern among all my patients. All the patients had a worsening
of symptoms around 1/31/20, the last one being 2/2/20. Most patients had their CT
scans on 2/2/20 or 2/3/20. What I discovered was that on 2/8/20, the CT results all
appeared to be more severe.
• However, despite CT results being more severe on 2/8/20, the patient’s
subjective symptoms were all improving
• 3/2/20-3/12 or 13, all patient’s CT results showed absorption
• I concluded that the peak of COVID-19 is roughly at days 7-8, which coincides
with the presentation of other types of viral pneumonia.
I asked many experts about why patients improve before their CT scans show
improvement. Many of them agree that the CT results seem to improve after the
patients’ subjective feeling is better. Hence, I conclude that the CT results lag behind
patient presentation.
My personal feeling is that even though the patient experiences relief from cough, fever,
nausea, etc, the retained phlegm in the lungs has not been addressed. Most patients
present with high fever so most doctors would focus on reducing the fever without
addressing the phlegm.
Furthermore, my ward primarily used TCM treatment, whereas others may strictly
use Western medicine. I noticed that some patients, when admitted, had very few
symptoms. However, after 3-4 days, they would start to develop dyspnea and respiratory
© 2020 Lotus Institute of Integrative Medicine eLotus.org
Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang • Medical Records from a Young and Brave Female Traditional Chinese Medicine (TCM) doctor on Fighting the COVID-19 22
obstruction. After discovering this pattern, I urged my colleagues to start using phlegm
eliminating herbs EVEN before the patient starts to show symptoms. Five of the herbs
that I used the most were Zi Su Zi (Fructus Perillae), Jie Zi (Semen Sinapis), Jiang Can
(Bombyx Batryticatus), Cang Zhu (Rhizoma Atractylodis) and finally Ma Huang (Herba
Ephedrae). Ma Huang (Herba Ephedrae) was something that I used throughout
the entire course of the treatment. It’s a key herb that must NOT be left out.
Most of our patients were using Ma Huang (Herba Ephedrae) from February 8, 2020 -
February 20, 2020.
This group of patients, especially the 15 who were released on 2/25/20 showed
complete absorption without leaving a trace. So, I suppose this theory is accurate.
On 2/18/20, I read a pathology report about COVID-19, and one doctor pointed
out that fibrosis develops in the lung, mucus secretions, pulmonary edema, hyaline
membrane formation, and more. My understanding is that there is a presence of these
secretion or mucus, and it is what we consider to be damp-phlegm in Chinese medicine.
So, what we learned is that it is vital for recovery to dispel this phlegm in order to avoid
further complications and burden on the lungs.
MY OBSERVATION OF THE CHARACTERISTICS OF COVID-19
The most noticeable characteristics of COVID-19 are:
FIRST: The patient enters peak severity in terms of symptoms, at approximately 1-week
into the virus. Whether it is cough, mucus, or any other complaints, approximately 7 days
from the onset of infection is when the patient will exhibit the most serious symptoms.
1. Within 1-week, the symptoms peak in severity
2. Excessive use of rectal antipyretic medications, heat-clearing detoxifying
herbs, or IV fluids will lead to afternoon fever or spike of fever at night, but
not during the day.
3. After the fever subsides, the cough worsens. The patient’s condition improves
© 2020 Lotus Institute of Integrative Medicine eLotus.org
Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang • Medical Records from a Young and Brave Female Traditional Chinese Medicine (TCM) doctor on Fighting the COVID-19 23
if the patient is able to expectorate sputum, with the help of Chinese herbs.
SECOND: I noticed that all patients had a fever, and were reflexively given Lopinavir
and Lian Hua Qing Wen capsules (herbs) for 3 days. I noticed that these patients then
developed nausea and absence of appetite, and diarrhea. Two-thirds of these
patients went on to develop liver dysfunction. I am unsure whether these symptoms
are part of the COVID-19 infection, or if they were side effects from the Lopinavir or
Lian Hua Qing Wen capsules. Both are considered cold in nature.
Another observation is that out of the 20 patients admitted on 2/4/20, if the patient
was repeatedly given antipyretic medication rectally to treat their high temperature, the
fever came down, but repeatedly spiked back up again. It seems to take around 3-5 days
for the temperature to stabilize.
If antipyretic medications were avoided in favor of herbs to reduce the fever,
the duration of fever seemed to shorten to 0.5-2 days. As this may have been
unconventional, we had to explain to the patients that they should remain calm
and not worry about high fever worsening their conditions, that it would, in fact,
shorten the duration of fever. This in turn, can help the patient sleep well and get much
needed rest for recovery.
My supervisor and I decided that IV fluids would only be used when absolutely necessary
and that we would limit it to 2 different types.
Ma Huang (Herba Ephedrae) DOSAGE AND FORMULAS
Some of you may ask what dose of Ma Huang (Herba Ephedrae) is most appropriate.
To be honest, I was not very confident about the dosing at first. My colleague suggested
using around 10 grams of Ma Huang (Herba Ephedrae), 15-20 grams of Gui Zhi
(Ramulus Cinnamomi), 15-20 grams of Ku Xing Ren (Semen Armeniacae Amarum) and
10 grams of Gan Cao (Radix et Rhizoma Glycyrrhizae).
© 2020 Lotus Institute of Integrative Medicine eLotus.org
Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang • Medical Records from a Young and Brave Female Traditional Chinese Medicine (TCM) doctor on Fighting the COVID-19 24
Why Do All Patients Need Ma Huang Fu Zi Xi Xin Tang (Ephedra, Asarum, and
Prepared Aconite Decoction)?
When national TCM experts came to our hospital, they asked why I was using Ma
Huang Fu Zi Xi Xin Tang (Ephedra, Asarum, and Prepared Aconite Decoction) for
all the patients and I explained my rationale to them this way. Along with Dr. Zhang
Chang and Zhang Ying Dong, we learned from an old man who is an expert in Five
Elements and Wu Yun Liu Qi (Five Movements and Six Climates) that 2019 is a year
that is deficient in the Earth Element. That means it is not a good year to do anything
that would hurt the digestive system, namely the Spleen and the Stomach. So, during the
spring of 2019, when I treated kids with sudden onset of fever due to a cold, I would
use his recommendation of Fu Zi Li Zhong Wan (Prepared Aconite Pill to Regulate
the Middle). It worked exceptionally well each time.
Furthermore, in the summer of 2019, I told all my Spleen Qi deficient patients to avoid
or minimize the consumption of raw fruits and vegetables, and to avoid cold water.
This is especially important for the children. I asked the parents to always give their
kids warm or hot drinks even during the summer. I know it was difficult for some of
them, but most parents were compliant. Also, in October of 2019, I intentionally
added 10-15 g of Fu Zi (Radix Aconiti Lateralis Praeparata) to all my patient’s
formulas. And what I was surprised to learn was that my patients, who followed my
dietary guidelines, were not infected with COVID-19. I have about 3600 patients and
60% of them worked in Wuhan and they were not infected!
My conclusion is that the patients who were admitted on 2/4/20 with high fever did
not “preserve” themselves enough in the winter. It is hard to explain Huang Di Nei
Jing (Yellow Emperor’s Inner Classic) to Western doctors or to patients, but the results
seemed to show that if someone did not take care of their body in the wintertime,
Springtime diseases can easily develop. What I did in the winter for my patients was
to tonify and “preserve” their Yang and then in the Spring, I had them use ventilating
herbs, such as Ma Huang (Herba Ephedrae) and Xi Xin (Radix et Rhizoma Asari), to
treat any exterior invasions.
© 2020 Lotus Institute of Integrative Medicine eLotus.org
Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang • Medical Records from a Young and Brave Female Traditional Chinese Medicine (TCM) doctor on Fighting the COVID-19 25
Before prescribing Ma Huang Tang (Ephedra Decoction) and Ma Huang Fu Zi Xi
Xin Tang (Ephedra, Asarum, and Prepared Aconite Decoction) to the patients, we
doctors drank these formulas for 3 full days first.
What I noticed is that even though these formulas normally dispel the exterior by
inducing sweating, neither I nor my colleagues had any sweating after we drank the
formula. We used up to 30g of Ma Huang (Herba Ephedrae) and 45g of Gui Zhi
(Ramulus Cinnamomi). The three of us did not experience any sweating nor did we
notice any discomfort or side effects. Therefore, we decided to use the same formulas
on our patients.
After giving the patients the herbs, I noticed that only a small amount of perspiration
occurred with patients with high fever. Furthermore, their fever would subside
after sweating occurred. Later after the fever has passed, when I administered any
formula with Ma Huang (Herba Ephedrae), I did not notice any sweating.
I asked my teacher, Dr. Zhang Ying Dong, about the rationale for the absence of
sweat. He recommended two very valuable research articles to me, which answered
many of my questions. I noticed that I only remembered Ma Huang (Herba Ephedrae)
as a diaphoretic herb to expel the exterior and induce sweating, yet I forgot about the
rest of its functions. I suddenly remembered that in my teacher Dr. Huang Shi Pei’s
lecture, Ma Huang (Herba Ephedrae) can even be used for an elderly patient who had
unconsciousness due to the usage of Diazepam.
THE SIGNIFICANCE OF Ma Huang (Herba Ephedrae) IN TREATING THIS EPIDEMIC
In my opinion, the two greatest benefits of Ma Huang (Herba Ephedrae) for treatment
of this epidemic are: FIRST - it opens the ENTIRE chest cavity; SECOND - it
opens the water passageway up above the lungs, by increasing urine output, leading
to the dissipating accumulated fluids and dampness from the Lungs. Case after case,
I saw patients increase urine output, without experiencing thirst. Furthermore, they
expressed feeling lighter and more energetic. Hence, I gained much more confidence in
prescribing Ma Huang (Herba Ephedrae) as time went on.
© 2020 Lotus Institute of Integrative Medicine eLotus.org
Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang • Medical Records from a Young and Brave Female Traditional Chinese Medicine (TCM) doctor on Fighting the COVID-19 26
THE RELATIONSHIP BETWEEN BODY CONSTITUTION BEFORE AND AFTER
INFECTION
Since I specialize in treating mixed or difficult-to-treat conditions, it is imperative
to balance the patient’s body constitution by treating conditions that have not yet
manifested. This means I have to not only consider the symptom but the root cause of
it. In this way, we can correct the imbalance of the body before they present as health
concerns.
However, after admitting so many patients to the hospital with COVID-19 infection, I
suddenly wondered if this epidemic is just one big accident? If so, does it really matter
if the patient is strong or weak, young or old? If it is something that comes on quickly,
when are we able to eradicate this “accident,” wouldn’t everything be back to normal?
What we found is that if the duration of the disease did not drag on for too long
or if the patient’s Zheng (upright) Qi remained intact because he or she had not
been too damaged by the virus or the medications, we were able to arrest it very
quickly. Therefore, theoretically, there may be no deficiency after the patient
recovers.
Out of the 30 patients, only 4 were elderly and critically ill. For those who averaged over
60 years of age, I would add some Dang Shen (Radix Codonopsis) and Huang Qi (Radix
Astragali) to their formula. For the rest of the patients, I didn’t add tonics. All patients
seemed to respond well to the Ma Huang (Herba Ephedrae) based formulas.
I also observed that, upon being admitted to the hospital, 7 of the patients could only
eat porridge for the first five days. They could not eat bread, rice, or anything else.
Up until yesterday, between the 30 patients, they ordered 40 lunch boxes per day. Why?
Some of the patients were young men and they were still hungry after finishing one
lunch box! I saw this as a very good sign that their health was returning.
In conclusion, when the appetite returns in a patient, this means the Spleen and Stomach
functions have returned to normal and that they are at the end of the misery they
endured.
Thank you for reading about my thoughts, observations, and process in regard to these
30 COVID-19 patients.
© 2020 Lotus Institute of Integrative Medicine eLotus.org
Chen Juan, Huang Di, Wang Shi Qi, Cai Xiang • Medical Records from a Young and Brave Female Traditional Chinese Medicine (TCM) doctor on Fighting the COVID-19 27
Disclaimer: This article is compiled and translated by John Chen from references below
to inform the readers how COVID-19, the 2019 novel coronavirus, is currently treated
in China. For readers who may have such an infection, contact and consult your primary
physician, go to the nearest emergency room or the hospital immediately. For additional
information, please contact the World Health Organization (WHO), the Center of
Disease Control (CDC) and the Food and Drug Administration (FDA).
Reference 1 :http://www.nhc.gov.cn/yzygj/s7653p/202002/8334a8326dd94d329df351d7da8aefc2/files/
b218cfeb1bc54639af227f922bf6b817.pdf
Reference 2 : https://mp.weixin.qq.com/s/lmnJnfJYoQ3dW5kG9XJ9nQ
Reference 3 : The following is the Guidance for Corona Virus Disease 2019 from the People’s Medical Publishing House
(6th version in English): https://mp.weixin.qq.com/s/nOAmosQ4YqkXHKdJbBE9GA
© 2020 Lotus Institute of Integrative Medicine eLotus.org
You might also like
- Pleural EffusionDocument38 pagesPleural EffusionMela VincoNo ratings yet
- COVID1981 Ebook PDFDocument105 pagesCOVID1981 Ebook PDFMexico English100% (2)
- I Do Not Consent: My Fight Against Medical Cancel CultureFrom EverandI Do Not Consent: My Fight Against Medical Cancel CultureRating: 4 out of 5 stars4/5 (10)
- CCPS Monograph Reflections From Global Process Safety LeadersDocument29 pagesCCPS Monograph Reflections From Global Process Safety LeadersKiranNo ratings yet
- 4TH Summative Test in English 10 Final PDFDocument3 pages4TH Summative Test in English 10 Final PDFKenneth Del Rosario100% (3)
- Covid-19 Bio-Warfare and The 21ST Century PandemicDocument9 pagesCovid-19 Bio-Warfare and The 21ST Century PandemicjavenacostaNo ratings yet
- Typhoid FeverDocument20 pagesTyphoid FeverKylie GolindangNo ratings yet
- ESRD Secondary To Diabetic Nephropathy CASE STUDYDocument42 pagesESRD Secondary To Diabetic Nephropathy CASE STUDYRalph Pelegrino75% (4)
- The Long Covid Self-Help Guide: Practical Ways to Manage SymptomsFrom EverandThe Long Covid Self-Help Guide: Practical Ways to Manage SymptomsNo ratings yet
- Case Presentation On Urinary Tract InfectionDocument56 pagesCase Presentation On Urinary Tract InfectionJohn Alvin Yoro92% (24)
- Beyond the Yeast Connection: A How-To Guide to Curing Candida and Other Yeast-Related ConditionsFrom EverandBeyond the Yeast Connection: A How-To Guide to Curing Candida and Other Yeast-Related ConditionsRating: 4.5 out of 5 stars4.5/5 (2)
- Covid 19 Highly Treatable PDFDocument8 pagesCovid 19 Highly Treatable PDFbluefalkenNo ratings yet
- Fire Your Doctor!: How to Be Independently HealthyFrom EverandFire Your Doctor!: How to Be Independently HealthyRating: 5 out of 5 stars5/5 (11)
- Driving Amidst PandemicDocument15 pagesDriving Amidst PandemicJohn Andrie Sumatra AlbentoNo ratings yet
- Adherence To Long-Term Therapies Evidence of Action 1Document16 pagesAdherence To Long-Term Therapies Evidence of Action 1Anonymous so6ZnlKywNo ratings yet
- ESRD Secondary To Diabetic Nephropathy CASE STUDY Docx 2Document42 pagesESRD Secondary To Diabetic Nephropathy CASE STUDY Docx 2Eyerusalem100% (1)
- HES 032 Case Analysis Week 3Document4 pagesHES 032 Case Analysis Week 3Arsie CalvoNo ratings yet
- Theory ApplicationDocument38 pagesTheory ApplicationAnusha VergheseNo ratings yet
- Upper Respiratory Tract InfectionDocument26 pagesUpper Respiratory Tract InfectionKylie Golindang67% (3)
- Motion For Telephonic Appearance - Abogado Jose - Wendy Karina RAMIREZ MENDEZ - 10-23-2020Document5 pagesMotion For Telephonic Appearance - Abogado Jose - Wendy Karina RAMIREZ MENDEZ - 10-23-2020TuttiUribeNo ratings yet
- CHEN - ARTIGO - 2020 - How COVID-19 (2019-nCoV) Is Currently Treated in China With TCMDocument13 pagesCHEN - ARTIGO - 2020 - How COVID-19 (2019-nCoV) Is Currently Treated in China With TCMDiego Ken OsoegawaNo ratings yet
- Novel Corona Virus - TCM Treatment From The PPRC PDFDocument13 pagesNovel Corona Virus - TCM Treatment From The PPRC PDFexcalidorNo ratings yet
- Prevention and TX FormulasDocument17 pagesPrevention and TX FormulasBellpine WindbowNo ratings yet
- How the Pandemic Is Affecting You and Your HealthcareFrom EverandHow the Pandemic Is Affecting You and Your HealthcareNo ratings yet
- DCCN 40 156Document8 pagesDCCN 40 156liyana SyatirahNo ratings yet
- Universal Healthcare in AmericaDocument10 pagesUniversal Healthcare in AmericaJaie NikkNo ratings yet
- Group 6 - Social Studies-Health - IPBADocument3 pagesGroup 6 - Social Studies-Health - IPBARanen Darren P. BenitoNo ratings yet
- Maria Odette A. Carpio, COVID Confirmed With Moderate PneumoniaDocument18 pagesMaria Odette A. Carpio, COVID Confirmed With Moderate PneumoniaKeanuNo ratings yet
- DC PlanningDocument5 pagesDC Planningapi-379546477No ratings yet
- Lecture 2 China's Fight Against COVID-19 Wisdom of The Integration of Traditional Chinese Medicine and Western MedicineDocument61 pagesLecture 2 China's Fight Against COVID-19 Wisdom of The Integration of Traditional Chinese Medicine and Western MedicineKinfe MehariNo ratings yet
- Arunima Pingali Asl PortfolioDocument20 pagesArunima Pingali Asl PortfolioRitish KumarNo ratings yet
- FNPDocument93 pagesFNPAko si MNo ratings yet
- ANJUUDocument7 pagesANJUUSimon lundaNo ratings yet
- Head and Neck Cancer Care in a Pandemic: Prioritizing Safe CareFrom EverandHead and Neck Cancer Care in a Pandemic: Prioritizing Safe CareNo ratings yet
- Case Study On Pulmonary Tuberculosis: January 2017Document3 pagesCase Study On Pulmonary Tuberculosis: January 2017Nova DenisaNo ratings yet
- ProjectDocument4 pagesProjectrakeshsharma11794120% (1)
- Technical Report Writing AssignmentDocument9 pagesTechnical Report Writing AssignmentMuhammad AwaisNo ratings yet
- 2 07 2023 Reed Affidavit SignedDocument23 pages2 07 2023 Reed Affidavit SignedAlyc KaiNo ratings yet
- Coronavirus - Can Traditional Chinese Medicine Help Fight The Disease - Asia - An In-Depth Look at News From Across The Continent - DW - 11.02.2020Document4 pagesCoronavirus - Can Traditional Chinese Medicine Help Fight The Disease - Asia - An In-Depth Look at News From Across The Continent - DW - 11.02.2020albar ismuNo ratings yet
- Coronavirus - Can Traditional Chinese Medicine Help Fight The Disease - Asia - An In-Depth Look at News From Across The Continent - DW - 11.02.2020Document4 pagesCoronavirus - Can Traditional Chinese Medicine Help Fight The Disease - Asia - An In-Depth Look at News From Across The Continent - DW - 11.02.2020albar ismuNo ratings yet
- PTB Case StudyDocument51 pagesPTB Case Studykatrin anne f. carpenaNo ratings yet
- C Ovid Patient Treatment GuideDocument29 pagesC Ovid Patient Treatment Guidemmms25No ratings yet
- The Use of Prophylaxis April 2020Document15 pagesThe Use of Prophylaxis April 2020TarikNo ratings yet
- Beating the Flu: The Natural Prescription for Surviving Pandemic Influenza and Bird FluFrom EverandBeating the Flu: The Natural Prescription for Surviving Pandemic Influenza and Bird FluNo ratings yet
- Care of Pediatric Patients During COVID-19 Pandemic-04042020Document60 pagesCare of Pediatric Patients During COVID-19 Pandemic-04042020Florin StanciuNo ratings yet
- Nipah Jo Co Clin Trials 11NOV2021Document22 pagesNipah Jo Co Clin Trials 11NOV2021mojarramanNo ratings yet
- SOPIEDocument16 pagesSOPIEshing_1987No ratings yet
- Accepted ManuscriptDocument22 pagesAccepted ManuscriptYuliet SusantoNo ratings yet
- CovidPatientTreatmentGuide TFH 7-31-2021Document20 pagesCovidPatientTreatmentGuide TFH 7-31-2021Mark LaceyNo ratings yet
- Sepsis Debriefing QuestionsDocument5 pagesSepsis Debriefing Questionsapi-631170779No ratings yet
- Uti Rle Case StudyDocument29 pagesUti Rle Case StudyEvora, Sichem D.No ratings yet
- Drop Out Pengobatan Hiv Pada Ibu Berdasarkan Faktor Predisposisi Di Kabupaten Banyumas Tahun 2016Document10 pagesDrop Out Pengobatan Hiv Pada Ibu Berdasarkan Faktor Predisposisi Di Kabupaten Banyumas Tahun 2016Isva Nasari IshakNo ratings yet
- Ebook Icu Quick Drug Guide PDF Full Chapter PDFDocument67 pagesEbook Icu Quick Drug Guide PDF Full Chapter PDFdonald.hughes297100% (26)
- AwarenessDocument2 pagesAwarenessLema MideksaNo ratings yet
- Icu Quick Drug Guide Jennifer Pai Lee Full ChapterDocument60 pagesIcu Quick Drug Guide Jennifer Pai Lee Full Chaptersusan.long892100% (10)
- Case PresentationDocument8 pagesCase Presentation。No ratings yet
- Consent To TreatmentDocument37 pagesConsent To TreatmentinriantoNo ratings yet
- Self Healthcare-Some InsightsDocument7 pagesSelf Healthcare-Some Insightsapi-15379927No ratings yet
- Intro To PERIOPERATIVE II.Document15 pagesIntro To PERIOPERATIVE II.Samantha Bernardo UndaNo ratings yet
- Micro para Laboratory Activity 4 - Case Study 2Document5 pagesMicro para Laboratory Activity 4 - Case Study 2Vannesa TarifaNo ratings yet
- Case Study Cap 2016Document31 pagesCase Study Cap 2016NadeshikoNo ratings yet
- Sebuah Studi Kasus Pasien Dengan Tuberkulosis Yang Resistan Terhadap Beberapa Obat .Document7 pagesSebuah Studi Kasus Pasien Dengan Tuberkulosis Yang Resistan Terhadap Beberapa Obat .DhiyaKurniadyNo ratings yet
- The Theory of Ep Idemic Febrile Diseases (Warm Diseases) : Nanjing University of Chinese MedicneDocument31 pagesThe Theory of Ep Idemic Febrile Diseases (Warm Diseases) : Nanjing University of Chinese MedicneMansoor Iqbal ChishtiNo ratings yet
- India Today PDFDocument78 pagesIndia Today PDFSANTOSH KUMARNo ratings yet
- Meril COVID-19 One-Step RT-PCR KitDocument2 pagesMeril COVID-19 One-Step RT-PCR KitAnkit RanaNo ratings yet
- BoTS - Digital Eye StrainDocument2 pagesBoTS - Digital Eye StrainFranchesca ValerioNo ratings yet
- AIDS in Pre-AIDS EraDocument7 pagesAIDS in Pre-AIDS EraObginNo ratings yet
- Four More Test Positive For COVID-19: VNIT Team Develops Novel Device To Ease Glaucoma ScreeningDocument8 pagesFour More Test Positive For COVID-19: VNIT Team Develops Novel Device To Ease Glaucoma Screeningshrikant bobadeNo ratings yet
- 03 23 2020 EO 53 Temporary Restrictions Due To Novel Coronavirus (COVID 19)Document4 pages03 23 2020 EO 53 Temporary Restrictions Due To Novel Coronavirus (COVID 19)Virginia Department of Emergency ManagementNo ratings yet
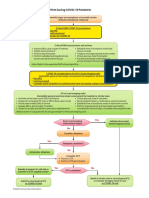
- Adult Suspected Stroke Algorithm During COVID-19 Pandemic: Yes NoDocument1 pageAdult Suspected Stroke Algorithm During COVID-19 Pandemic: Yes NoAnabel VinuezaNo ratings yet
- International Immunopharmacology: Hyun Jee Han, Chinekwu Nwagwu, Obumneme Anyim, Chinedu Ekweremadu, San KimDocument11 pagesInternational Immunopharmacology: Hyun Jee Han, Chinekwu Nwagwu, Obumneme Anyim, Chinedu Ekweremadu, San KimyoshefarieNo ratings yet
- Addendum 11 To Executive Order 01-20Document5 pagesAddendum 11 To Executive Order 01-20StephanieRyanNo ratings yet
- Managing COVID-19 in Low-And Middle-Income Countries: The Public Health ResponseDocument2 pagesManaging COVID-19 in Low-And Middle-Income Countries: The Public Health ResponseNuzlaNo ratings yet
- ESC - Prevention of CVDDocument78 pagesESC - Prevention of CVDIrsalina Nur ShabrinaNo ratings yet
- Letter of MD Support To RNs - FinalDocument4 pagesLetter of MD Support To RNs - FinalElishaDacey0% (1)
- Department of Biotechnology: Biotechnology Eligibility Test (BET) 2020Document2 pagesDepartment of Biotechnology: Biotechnology Eligibility Test (BET) 2020BabuHalderNo ratings yet
- Deeks Et Al-2020-Cochrane Database of Systematic ReviewsDocument311 pagesDeeks Et Al-2020-Cochrane Database of Systematic ReviewsSilvia Emy RarasNo ratings yet
- Consent Form For Students and Parents/Guardians: Sharda UniversityDocument2 pagesConsent Form For Students and Parents/Guardians: Sharda UniversitySANANo ratings yet
- Color - Results 2 PDFDocument3 pagesColor - Results 2 PDFCeleste CarabajalNo ratings yet
- COVID19 Vaccine OG111 Chapter 16Document148 pagesCOVID19 Vaccine OG111 Chapter 16Sri Chandra DudduNo ratings yet
- German Panic Paper 4 - Necessary Measures For Germany To Contain The COVID-19 Pandemic and To Avoid Social Collateral Damage (English)Document9 pagesGerman Panic Paper 4 - Necessary Measures For Germany To Contain The COVID-19 Pandemic and To Avoid Social Collateral Damage (English)MichaelNo ratings yet
- Amended Bond Conditions For Johnston TaylorDocument3 pagesAmended Bond Conditions For Johnston TaylorPlainsman EditorNo ratings yet
- Related Literature: Cameras-Can-Help-Prevent-The-Spread-Of-Covid-19 PDFDocument3 pagesRelated Literature: Cameras-Can-Help-Prevent-The-Spread-Of-Covid-19 PDFRyan DagsilNo ratings yet
- MAY 12, 2020 - FINAL Dashboard CovidDocument38 pagesMAY 12, 2020 - FINAL Dashboard CovidIrish Mae JovitaNo ratings yet
- Tennessee PledgeDocument7 pagesTennessee PledgeNewsChannel 9 StaffNo ratings yet
- COVID-19 Patient Screening Guidance Document: Ministry of HealthDocument3 pagesCOVID-19 Patient Screening Guidance Document: Ministry of HealthSureshNo ratings yet
- Doctors' Letter To Pallister, Friesen About State of Hospitals During COVIDDocument3 pagesDoctors' Letter To Pallister, Friesen About State of Hospitals During COVIDElishaDaceyNo ratings yet
- Basic Services Allowed As Others Stay Closed: Gulf TimesDocument24 pagesBasic Services Allowed As Others Stay Closed: Gulf TimesmurphygtNo ratings yet