Professional Documents
Culture Documents
Patent Matrix Assignmnet
Uploaded by
Hasan Shoukat PathanCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Patent Matrix Assignmnet
Uploaded by
Hasan Shoukat PathanCopyright:
Available Formats
PATENT MATRIX
Key Words Corruption, Dishonesty, Fraud, Health sector, Medical management, Health
protection, ICT, Computer Technology , Artificial
intelligence.____________________________________________________________________________________
Real World Problem_ Information and Communication Technology based interventions: to combat
corruption in Health care department of Sindh, Pakistan :A Case study of Civil hospital
Hyderabad.Proposed
Solution: Research will provide involvement of ICT in controlling corruption in health care department.
Title IPC Inventor Assignee Claims
1 1. . An adaptive method for healthcare claim fraud detection,
G06Q10/10 Akli Adjaoute comprising:
Healthcare Brighterion Inc a data reduction step for converting claim data into profile data
fraud protection comprising a plurality of behavioral dimensions, wherein a
minimum of a hundred fold reduction in data volume is realized;
and an individual recognition step for identifying individual healthcare
management providers in said profile data and for collecting such into
corresponding long term individual healthcare provider profiles;
a clustering step for identifying groups of healthcare providers in
said profile data and for collecting such into respective long term
group profiles;
a smart agent building step for feeding historical claim data
through the data reduction step to the individual recognition step
and the group recognition step, and for creating a plurality of
individual and group smart agents therefrom and each including
profile data organized into said plurality of behavioral
dimensions;
an updating step for using claim data fed through the data
reduction step to be added to any matching long term individual
healthcare provider profile;
a real time fraud detection step for comparing updates of
individual ones of the plurality of behavioral dimensions to their
running values in the long term individual healthcare provider
profiles and measuring any significant deviations;
a fraud classification step for scoring said deviations as being
the result of fraudulent or non-fraudulent behavior on the part of
the respective individual healthcare provider having sourced the
claim data;
wherein, the step of updating produces a self-learning and
adaptive fraud detection capability that evolves over time
healthcare provider-by-healthcare provider.
2. The method of claim 1, further comprising:
a non-fraudulent classification step for dividing score
determinations of non-fraudulent behavior into ones requiring
and not requiring further investigation
.
3. The method of claim 1, further comprising:
a group classification step for comparing updates of individual
ones of the plurality of behavioral dimensions to their running
values in related long term group healthcare provider profiles,
and for measuring any significant deviations from other
members in the group
2
Richard 1. . A centralized healthcare management and monitoring
System and Postrel
No current
G16H10/65 assignee system comprising:
method for a. a healthcare management server computer interconnected to
centralized a computer network, the healthcare management server
computer comprising:
management i. a first repository of patient records, each patient record
and monitoring associated with a patient and accessible via a unique patient
identification indicia associated with the patient, each patient
of healthcare record comprising healthcare information associated with the
services patient; and
ii. a second repository of predetermined compliance rules; each
of the compliance rules comprising information regarding an
interaction between multiple entities associated with the
healthcare management server computer;
b. a plurality of healthcare provider computers interconnected to
the computer network, each of which is associated with a
healthcare provider, each of the healthcare provider computers
comprising means for inputting a patient identification indicia
presented by a patient and communicating with the healthcare
management server computer over the computer network using
the patient identification presented by the patient;
wherein, when a patient presents, in association with healthcare
services performed by the associated healthcare provider, a
patient identification indicia associated with the patient, the
healthcare provider computer transmits to the healthcare
management server computer a query comprising parameters
comprising:
the patient identification indicia;
an identification of the healthcare services performed or
proposed to be performed by the associated healthcare
provider; and
an identification of the healthcare provider performing the
healthcare services; and
the healthcare management server computer utilizes the query
to access the first and second repositories to determine if the
parameters of the query are in compliance with one or more of
the predetermined compliance rules.
. A centralized healthcare management and monitoring system
comprising:
a. a healthcare management server computer interconnected to
a computer network, the healthcare management server
computer comprising:
i. a first repository of patient records, each patient record
associated with a patient and accessible via a unique patient
identification indicia associated with the patient, each patient
record comprising healthcare information associated with the
patient; and
ii. a second repository of predetermined compliance rules; each
of the compliance rules comprising information regarding an
interaction between multiple entities associated with the
healthcare management server computer;
b. a plurality of healthcare provider computers interconnected to
the computer network, each of which is associated with a
healthcare provider, each of the healthcare provider computers
comprising means for inputting a patient identification indicia
presented by a patient and communicating with the healthcare
management server computer over the computer network using
the patient identification presented by the patient;
wherein, when a patient presents, in association with healthcare
services performed by the associated healthcare provider, a
patient identification indicia associated with the patient, the
healthcare provider computer transmits to the healthcare
management server computer a query comprising parameters
comprising:
the patient identification indicia;
an identification of the healthcare services performed or
proposed to be performed by the associated healthcare
provider; and
an identification of the healthcare provider performing the
healthcare services; and
the healthcare management server computer utilizes the query
to access the first and second repositories to determine if the
parameters of the query are in compliance with one or more of
the predetermined compliance rules.
2. he system of claim
1 wherein the
compliance rules
comprise rules related to
healthcare treatment
procedures, and wherein
the healthcare
management server
computer determines if
the healthcare services
proposed to be
performed by the
healthcare provider
identified in the query are
in compliance with the
healthcare treatment
procedures.
3 The system of claim 2 wherein healthcare information
associated with the patient identified in the query is utilized by
the healthcare management server computer to determine if the
healthcare services proposed to be performed by the healthcare
provider identified in the query are in compliance with the
healthcare treatment procedur.
3 1. A method, comprising:
G06Q10/10 Jeffrey M. Verizon Patent receiving, by one or more devices, healthcare information;
Healthcare Getchius and Licensing calculating, by the one or more devices, a geographic density of
fraud detection Inc healthcare fraud based on the healthcare information;
determining, by the one or more devices, anomalous
with machine distributions of healthcare fraud based on the healthcare
learning information;
deriving, by the one or more devices, empirical estimates of
procedure and treatment durations based on the healthcare
information;
utilizing, by the one or more devices, classifiers to determine
first inconsistencies in the healthcare information;
utilizing, by the one or more devices, language models and co-
morbidity analysis to determine second inconsistencies in the
healthcare information;
utilizing, by the one or more devices, link analysis to determine
third inconsistencies in the healthcare information;
calculating, by the one or more devices, parameters for a
healthcare fraud detection system based on the geographic
density, the anomalous distributions, the empirical estimates,
and the first, second, and third inconsistencies; and
providing, by the one or more devices, the parameters to the
healthcare fraud detection system.
2. The method of claim
1, where the one or more
devices are provided in a
healthcare fraud analysis
system.
3. The method of claim 2, where the healthcare fraud analysis
system and the healthcare fraud detection system are provided
in a healthcare fraud management system.
4 1.
2.
3.
5 1.
2.
3.
©Dr. Arabella Bhutto @ MUET
You might also like
- Senate Hearing, 110TH Congress - Carbon Sequestration TechnologiesDocument95 pagesSenate Hearing, 110TH Congress - Carbon Sequestration TechnologiesScribd Government DocsNo ratings yet
- Complete Data of The Company - Address - Phone - Mobile - MailDocument3 pagesComplete Data of The Company - Address - Phone - Mobile - MailnevevaniaNo ratings yet
- Tonoy Tarafdar MBA (3 Sem) Acharya'S Bangalore B-SchoolDocument15 pagesTonoy Tarafdar MBA (3 Sem) Acharya'S Bangalore B-SchoolDotRev IbsNo ratings yet
- 04 14 2023 Public Private Partnerships in The PhilippinesDocument32 pages04 14 2023 Public Private Partnerships in The PhilippinesJediann BungagNo ratings yet
- Policies and Regulations that Promote Sustainable MicrofinanceDocument33 pagesPolicies and Regulations that Promote Sustainable Microfinanceiamyt100% (1)
- The Mining Act of 1995 - 001Document34 pagesThe Mining Act of 1995 - 001Angelica RojasNo ratings yet
- Insurance Law in PhilippinesDocument67 pagesInsurance Law in PhilippinesAileen Vasquez-MendozaNo ratings yet
- 09 Castaneda v. AgoDocument8 pages09 Castaneda v. AgoJed SulitNo ratings yet
- Civil Code Title VII - NuisanceDocument1 pageCivil Code Title VII - NuisanceE.F.FNo ratings yet
- Offer Letter: Price ListDocument11 pagesOffer Letter: Price ListJose CastroNo ratings yet
- Assignment Professionla PracticeDocument5 pagesAssignment Professionla PracticeVinay SharmaNo ratings yet
- 33 Compliance and Control PDFDocument14 pages33 Compliance and Control PDFEkta Saraswat VigNo ratings yet
- UNFAIR LABOR PRACTICESDocument19 pagesUNFAIR LABOR PRACTICESLeaneSacaresNo ratings yet
- Investment - PHP Foreign InvestmentDocument4 pagesInvestment - PHP Foreign InvestmentYash ThakkarNo ratings yet
- 3 Codal Avenues For Citizen's ParticipationDocument26 pages3 Codal Avenues For Citizen's ParticipationYang RheaNo ratings yet
- Guiding PrinciplesDocument39 pagesGuiding PrinciplestiwariajaykNo ratings yet
- GR No 86889Document4 pagesGR No 86889ElephantNo ratings yet
- Loi - Portland Cement (Cif) For Buyers (Blank) - Ns CommerceDocument3 pagesLoi - Portland Cement (Cif) For Buyers (Blank) - Ns CommerceRahool KatariyaNo ratings yet
- ALECO Articles of IncorporationDocument5 pagesALECO Articles of IncorporationEloisa YusonNo ratings yet
- Waumini by LawsDocument31 pagesWaumini by LawsxprettyNo ratings yet
- Study Now Pay Later Pilot ProgramDocument6 pagesStudy Now Pay Later Pilot Programrommel5No ratings yet
- Phase 1 Cbre Team54 1Document6 pagesPhase 1 Cbre Team54 1api-401088780No ratings yet
- De RiskingDocument9 pagesDe RiskingKerine HeronNo ratings yet
- Ridge Hoise Development Company Act SummaryDocument12 pagesRidge Hoise Development Company Act SummaryPinnacle MfbNo ratings yet
- Manila Tax Code PDFDocument502 pagesManila Tax Code PDFJBBIllonesNo ratings yet
- As To Manner of Amendment Case DigestDocument8 pagesAs To Manner of Amendment Case DigestAna MergalNo ratings yet
- Bank of Uganda Releases Agent Banking RegulationsDocument2 pagesBank of Uganda Releases Agent Banking RegulationspokechoNo ratings yet
- Property Relations Between Husband and Wife: Title IvDocument39 pagesProperty Relations Between Husband and Wife: Title Ivshirlyn cuyongNo ratings yet
- Proposed Ordinance MangrovesDocument5 pagesProposed Ordinance Mangrovesjeffrey100% (1)
- Sample Due Diligence ChecklistDocument7 pagesSample Due Diligence Checklistaca_traderNo ratings yet
- Samridhi Foundation - Draft MoaDocument7 pagesSamridhi Foundation - Draft MoaPawan KumarNo ratings yet
- Audit of Non Profit OrganisationDocument2 pagesAudit of Non Profit Organisationmeera sNo ratings yet
- Procedure For Registering A Private Limited CompanyDocument2 pagesProcedure For Registering A Private Limited CompanykwikbukNo ratings yet
- Enasol TeaserDocument17 pagesEnasol TeaserIvan JelićNo ratings yet
- Template Resolution Removal of Authorised Signatories 28112021Document3 pagesTemplate Resolution Removal of Authorised Signatories 28112021Shiela Mae BalbastroNo ratings yet
- Allocation of Net SurplusDocument3 pagesAllocation of Net SurplusJA LogsNo ratings yet
- Discounted Cash FlowDocument5 pagesDiscounted Cash FlowEKANGNo ratings yet
- Eo 229Document52 pagesEo 229rachelle almonteNo ratings yet
- Sample Term Sheet (Appendix2)Document6 pagesSample Term Sheet (Appendix2)Tan Swee KoonNo ratings yet
- Ref.: Ip/ /11 Date: To: From:: Investment Proposal MemorandumDocument1 pageRef.: Ip/ /11 Date: To: From:: Investment Proposal MemorandummfaisalidreisNo ratings yet
- Kosamattam Finance Limited Prospectus AprilDocument287 pagesKosamattam Finance Limited Prospectus Aprilmehtarahul999No ratings yet
- Assignment of Franchise DraftDocument4 pagesAssignment of Franchise DraftSai KrishnaNo ratings yet
- Order Form Jan16Document2 pagesOrder Form Jan16Bjena100% (1)
- MC2021-001 2020 Ipp GP&SGDocument47 pagesMC2021-001 2020 Ipp GP&SGRaffy BelloNo ratings yet
- Dy vs. Koninklijke Philips ElectronicsDocument16 pagesDy vs. Koninklijke Philips ElectronicsJerome ArañezNo ratings yet
- CARE Credit and Savings Source Book, Methodology ChapterDocument53 pagesCARE Credit and Savings Source Book, Methodology ChaptermufeesmNo ratings yet
- Memorandum of AssociationDocument13 pagesMemorandum of AssociationRavi KrishnanNo ratings yet
- Four Types of Foreign InvestmentsDocument2 pagesFour Types of Foreign InvestmentsErgo Wings50% (6)
- Executive Order No 79Document9 pagesExecutive Order No 79Ivy KatrinaNo ratings yet
- Local Government AdministrationDocument56 pagesLocal Government AdministrationAnirtsNo ratings yet
- Foreign Collaboration: Financial, Technical & Marketing TypesDocument13 pagesForeign Collaboration: Financial, Technical & Marketing TypesIlakkiya SathiyamoorthyNo ratings yet
- Bank Marketing Mix New Stretegy in TodayDocument10 pagesBank Marketing Mix New Stretegy in TodayMirjana StefanovskiNo ratings yet
- Module in General Banking Law of 2000Document9 pagesModule in General Banking Law of 2000Nieves GalvezNo ratings yet
- SRC Cases DigestedDocument5 pagesSRC Cases DigestedTalina BinondoNo ratings yet
- Proclamation For Disclosure and Registration AssetsDocument12 pagesProclamation For Disclosure and Registration AssetsAnonymous dLIq7U3DKzNo ratings yet
- Digital Assignment - 2: Team MembersDocument12 pagesDigital Assignment - 2: Team MembersTarang GargNo ratings yet
- The Future of Life Sciences and Healthcare Logistics: Key Trends Driving Digital TransformationDocument19 pagesThe Future of Life Sciences and Healthcare Logistics: Key Trends Driving Digital TransformationMete0ra-SanNo ratings yet
- Liang 2017Document5 pagesLiang 2017helloNo ratings yet
- Considerations For A Successful Clinical Decision Support SystemDocument8 pagesConsiderations For A Successful Clinical Decision Support SystemRudi IlhamsyahNo ratings yet
- Chapter 2. Integrating Risk Management, Quality, Management, and Patient SafetyDocument10 pagesChapter 2. Integrating Risk Management, Quality, Management, and Patient SafetyNi Putu Sri wahyuniNo ratings yet
- Chapter 1 IFMDocument32 pagesChapter 1 IFMHasan Shoukat PathanNo ratings yet
- Week 06Document36 pagesWeek 06Hasan Shoukat PathanNo ratings yet
- Week 06Document36 pagesWeek 06Hasan Shoukat PathanNo ratings yet
- Week 3 Applying The Three Step Writing ProcessDocument19 pagesWeek 3 Applying The Three Step Writing ProcessHasan Shoukat PathanNo ratings yet
- Business Communication: Introduction To The CourseDocument17 pagesBusiness Communication: Introduction To The CourseHasan Shoukat PathanNo ratings yet
- Corporate Restructuring StrategiesDocument42 pagesCorporate Restructuring StrategiesHasan Shoukat PathanNo ratings yet
- ICT Interventions to Combat Corruption in Civil HospitalDocument20 pagesICT Interventions to Combat Corruption in Civil HospitalHasan Shoukat PathanNo ratings yet
- PESTEL Analysis of Ehsan Chappal Store (ECS)Document14 pagesPESTEL Analysis of Ehsan Chappal Store (ECS)Hasan Shoukat PathanNo ratings yet
- Corporate Restructuring StrategiesDocument42 pagesCorporate Restructuring StrategiesHasan Shoukat PathanNo ratings yet
- HRM PresentationDocument17 pagesHRM PresentationHasan Shoukat PathanNo ratings yet
- What Is Your Research ProblemDocument1 pageWhat Is Your Research ProblemHasan Shoukat PathanNo ratings yet
- Islamic vs Conventional BankingDocument8 pagesIslamic vs Conventional BankingHasan Shoukat PathanNo ratings yet
- The Marketing Environment: A Global PerspectiveDocument42 pagesThe Marketing Environment: A Global PerspectiveAneek IslamNo ratings yet
- ECS Shoes Brand Report: History, Products, BranchesDocument71 pagesECS Shoes Brand Report: History, Products, BranchesFatima ShahidNo ratings yet
- Current AffairDocument21 pagesCurrent AffairfileNo ratings yet
- Job Analysis and Job Design 3Document50 pagesJob Analysis and Job Design 3Hasan Shoukat PathanNo ratings yet
- A Case Study of Ehsan Chappal Store CompleteDocument21 pagesA Case Study of Ehsan Chappal Store CompleteHasan Shoukat Pathan100% (1)
- Elasticity of Demand: Presented By: Hasan Shoukat Teacher: Sir Iqbal Panhwar Course: EconomicsDocument14 pagesElasticity of Demand: Presented By: Hasan Shoukat Teacher: Sir Iqbal Panhwar Course: EconomicsHasan Shoukat PathanNo ratings yet
- 20090716FoxReiki PDFDocument40 pages20090716FoxReiki PDFAgustina RomeroNo ratings yet
- Vrs PresentationDocument24 pagesVrs PresentationshrutipalkarNo ratings yet
- Volcanic Eruption Types and ProcessDocument18 pagesVolcanic Eruption Types and ProcessRosemarie Joy TanioNo ratings yet
- Effects of Cutting Classes For Grade 11 TEC Students of AMA Computer College Las PiñasDocument5 pagesEffects of Cutting Classes For Grade 11 TEC Students of AMA Computer College Las PiñasGgssNo ratings yet
- Introducion To Load Cells UtilcellDocument22 pagesIntroducion To Load Cells UtilcellRifi MohamedNo ratings yet
- Subway 2009Document12 pagesSubway 2009sparklers_mNo ratings yet
- TDI - Full Cave Diver Course: TDI Instructor Manual Part 2 - Diver Standards Date: 12/31/2009 Revision: 10.0Document5 pagesTDI - Full Cave Diver Course: TDI Instructor Manual Part 2 - Diver Standards Date: 12/31/2009 Revision: 10.0BraulioNo ratings yet
- Muscle Mag August 2014Document148 pagesMuscle Mag August 2014ElthonJeffrey100% (5)
- Uganda National Urban ProfileDocument74 pagesUganda National Urban ProfileUnited Nations Human Settlements Programme (UN-HABITAT)No ratings yet
- RR No. 6-2015 PDFDocument5 pagesRR No. 6-2015 PDFErlene CompraNo ratings yet
- Bab 06 PindahPanasDocument41 pagesBab 06 PindahPanasPurna Satria NugrahaNo ratings yet
- Name: Sport: Movement PrepDocument24 pagesName: Sport: Movement PrepS HNo ratings yet
- GCS Guilford County Schools 2020 Staff Manual Omits Obesity From CDC Covid WarningsDocument26 pagesGCS Guilford County Schools 2020 Staff Manual Omits Obesity From CDC Covid WarningscitizenwellsNo ratings yet
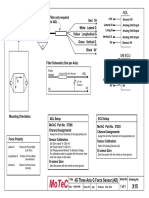
- Filter and wiring schematic for 3-axis ADL G-force sensorDocument1 pageFilter and wiring schematic for 3-axis ADL G-force sensorJuan Ramón Pérez LorenzoNo ratings yet
- Basic Science JSS 1 2NDDocument29 pagesBasic Science JSS 1 2NDAdeoye Olufunke100% (2)
- Section - A: Holiday Homework For Grade XiDocument7 pagesSection - A: Holiday Homework For Grade XiGM Ali KawsarNo ratings yet
- Codex CRD26Document9 pagesCodex CRD26arely svetlana gaspar badilloNo ratings yet
- Dupont Heir Sexually Abuses DaughterDocument3 pagesDupont Heir Sexually Abuses DaughterJuandelaCruzNo ratings yet
- CS Risk and Crisis Management FinalDocument62 pagesCS Risk and Crisis Management FinaldangermanNo ratings yet
- With Reference To Relief, Drainage and Economic Importance, Explain The Differences Between The Northern Mountains and Western MountainsDocument3 pagesWith Reference To Relief, Drainage and Economic Importance, Explain The Differences Between The Northern Mountains and Western Mountainshajra chatthaNo ratings yet
- Diagnosis and Management of Ulnar Nerve PalsyDocument20 pagesDiagnosis and Management of Ulnar Nerve PalsyamaliafarahNo ratings yet
- TS68Document52 pagesTS68finandariefNo ratings yet
- Medical Power PointDocument124 pagesMedical Power PointPhysiology by Dr Raghuveer75% (4)
- English Try Out UN 1 2008/2009Document4 pagesEnglish Try Out UN 1 2008/2009Cepiana Abas100% (10)
- Cast Resin Planning Guidelines GEAFOL PDFDocument24 pagesCast Resin Planning Guidelines GEAFOL PDFtenk_man100% (1)
- Warm Vs Cold ShockDocument8 pagesWarm Vs Cold ShockmarleeramirezNo ratings yet
- Sampling Methods for Terrestrial Amphibians and ReptilesDocument39 pagesSampling Methods for Terrestrial Amphibians and ReptilesBenzu Shawn100% (1)
- The Secret of Eternal Youth PDFDocument36 pagesThe Secret of Eternal Youth PDFArunesh A Chand100% (4)
- Health Behaviour: Current Issues and ChallengesDocument13 pagesHealth Behaviour: Current Issues and ChallengesK.A.No ratings yet
- Aircraft Instruments and Avionics PDFDocument211 pagesAircraft Instruments and Avionics PDFairbuk doeing88% (8)