Professional Documents
Culture Documents
Cerebral Venous Thrombosis: A Comprehensive Review: Clinical Neurology: Review Article
Uploaded by
danby danbyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cerebral Venous Thrombosis: A Comprehensive Review: Clinical Neurology: Review Article
Uploaded by
danby danbyCopyright:
Available Formats
Erratum
October 12, 2020. DOI: 10.1159/000511472
Clinical Neurology: Review Article
Eur Neurol 2020;83:369–379 Received: May 2, 2020
Accepted: June 27, 2020
DOI: 10.1159/000509802 Published online: September 2, 2020
Cerebral Venous Thrombosis:
A Comprehensive Review
Pretty Sara Idiculla a Dhineshreddy Gurala b Manikandan Palanisamy c
Rajendran Vijayakumar c Sindhu Dhandapani d Elanagan Nagarajan e
aUniversity
of Missouri Health Care, Columbia, MO, USA; bStaten Island University Hospital, Northwell Health,
Staten Island, NY, USA; cMajmaah University, Industrial Area, Al Majma’ah, Saudi Arabia;
dCure Hospital, Vellakovil, India; eColumbia University Medical Center, New York, NY, USA
Keywords neurological deficits, and cavernous sinus syndrome. MRI
Cerebral venous thrombosis · Dural sinus thrombosis · with magnetic resonance venogram (MRV) is considered the
Magnetic resonance venogram gold standard for diagnosis. Anticoagulation with heparin or
low-molecular-weight heparin is the mainstay of treatment.
Endovascular management is indicated for those cases with
Abstract severe symptoms or worsening of symptoms despite antico-
Background: Cerebral sinus venous thrombosis (CSVT) is a agulation therapy. Favorable outcomes have been reported
relatively rare, potentially fatal neurological condition that in patients who receive early diagnosis and treatment. Con-
can be frequently overlooked due to the vague nature of its clusion: CSVT is a potentially fatal neurological condition
clinical and radiological presentation. A literature search on that is often under-diagnosed due to its nonspecific presen-
PubMed using the keyword “Cerebral sinus venous throm- tation. Timely diagnosis and treatment can reduce morbid-
bosis” was performed. We searched for the epidemiology, ity and mortality, remarkably improving the outcome in af-
risk factors, pathophysiology, clinical features, diagnosis, fected individuals. © 2020 S. Karger AG, Basel
and treatment of CSVT. All full-text articles in the last 10
years, in adults (>18 years), and the English language were
included. We aim to give a comprehensive review of CSVT,
with a primary focus on the management of the disease. Introduction
Summary: The literature search revealed 404 articles that
met our criteria. CSVT is a relatively rare condition that ac- Cerebral sinus venous thrombosis (CSVT) is a rare
counts for approximately 1% of all forms of stroke. They can form of stroke associated with an increased mortality
be subdivided into acute, subacute, and chronic forms based rate. It can present with a multitude of signs and symp-
on the time of onset of clinical symptoms. It is a multifacto- toms, making it difficult to distinguish from other neuro-
rial disease, and the major forms of clinical presentation in- logical conditions. Early recognition of symptoms and
clude isolated intracranial hypertension syndrome, focal treatment improves overall outcome in these patients.
karger@karger.com © 2020 S. Karger AG, Basel Pretty Sara Idiculla
www.karger.com/ene University of Missouri Health Care
202 Grasmere Drive
Staten Island, NY 10305 (USA)
sarahidiculla.psi@gmail.com
CSVT demands a close functioning of both clinical and
Color version available online
radiological proficiency for prompt detection and opti-
mizing patient care.
Method and Results
A literature search was done on PubMed using the keyword
“Cerebral sinus venous thrombosis”. We searched for the epide-
miology, risk factors, pathophysiology, clinical features, diagnosis,
and treatment of CSVT. All full-text articles in the last 10 years, in
adults (>18 years), and in the English language were included. Case
reports, case series, review articles, and observational studies with
relevant documentation were analyzed for our review. The litera-
ture search revealed 404 articles that met our criteria. Our aim is
to give a comprehensive review on CSVT, with primary focus on
the management of the disease in adults.
Fig. 1. Anatomy of cerebral venous system. The figure was repro-
duced with permission from the Radiology Assistant Web site
Definition (http://www.radiologyassistant.nl/en/p4befacb3e4691/cerebral-
venous-thrombosis.html).
CSVT is a rare form of venous thromboembolism
(VTE) and based on the time of onset of clinical symp-
toms. There are 3 subtypes [1]: Anatomy of the Cerebral Venous System
1. Acute – ≤48 h.
2. Subacute – >48 h – ≤30 days. Cerebral venous system is divided into the superficial
3. Chronic – ≥1 month. and deep venous system [7–9]. They are a group of ve-
nous channels located intracranially between the endos-
teal and meningeal layers of the dura mater. Unlike sys-
Epidemiology temic veins, cerebral veins lack valves and do not follow
cerebral arterial territory. The superior sagittal sinus, in
The incidence of CSVT has increased over the past particular, also drains the cerebrospinal fluid from the
few years due to the advancement of imaging tech- subarachnoid space.
niques helping detection of the disease in its early stag- The superficial system comprises the dural sinuses and
es. Although the autopsy series approximates the inci- cortical veins. It drains the cerebral cortex and superficial
dence to be 3–4 cases per million, clinical series have white matter. The 2 major dural sinuses include the supe-
shown a 10-fold increase in these numbers [2]. An in- rior sagittal sinus that drain dorsolateral area and the cav-
creased incidence is seen among children, younger ernous sinus that drain the anteroventral region. The su-
adults, females of the reproductive age-group, and low- perior sagittal sinus drains into the transverse sinus which
income countries [3]. The estimated female-to-male ra- then drains into the straight sinus. The cavernous sinus
tio was 3:1 and comprises 0.5–1% of all stroke occur- drains into the transverse sinus posterolaterally and sig-
rences [4, 5]. moid sinus inferolaterally, along the superior and inferior
The most common form of CSVT is the subacute type, petrosal sinuses, respectively. The superficial cortical
which constitutes almost half of all the cases, and the veins are the superiorly draining veins and the inferiorly
chronic form is less frequent [6]. The ISCVT (Interna- draining veins (vein of Labbe and sylvian or superficial
tional Study on Cerebral Vein and Dural Sinus Throm- middle cerebral veins).
bosis) determined the occurrence of CSVT in various The deep system includes straight, lateral, and sigmoid
sites – transverse sinus (86%), superior sagittal sinus sinus, as well as drain the deeper cortical veins (vein of
(62%), straight sinus (18%), cortical veins (17%), jugular Galen, internal cerebral veins, Rosenthal or basal vein,
veins (12%), vein of Galen, and internal cerebral vein medullary, and subependymal veins). These vessels drain
(11%) [6]. the basal ganglia, thalamus, the upper brain stem, and
370 Eur Neurol 2020;83:369–379 Idiculla/Gurala/Palanisamy/Vijayakumar/
DOI: 10.1159/000509802 Dhandapani/Nagarajan
Table 1. Risk factors for CVT [10]
Risk factor Description Risk factor Description
Prothrombotic Hereditary: factor V Leiden mutation, Intracranial Tumors
conditions antithrombin III deficiency, protein C/S defects
deficiency, and G20210A prothrombin gene Arteriovenous malformations
mutation Dural fistula
Acquired: These are transient forms and are Venous anomalies
considered specific to females. It includes
pregnancy, puerperium, oral contraceptive pill Hematological Essential thrombocythemia
use, and hormonal replacement therapy Myeloproliferative malignancies
Infections Intracranial: meningitis Primary and secondary polycythemia
Systemic: HIV, tuberculosis, and sepsis Paroxysmal nocturnal hemoglobinuria
Local: otitis media, mastoiditis, oral, sinus, and Systemic Dehydration
head and neck infections diseases
Malignancies
Mechanical Head trauma
trauma Thyroid disease
Neurosurgical procedures
Sarcoidosis
Jugular vein catheterization
Obesity
LP
Nephrotic syndrome
Vasculitis Systemic lupus erythematosus
Inflammatory bowel disease
Sjogren’s syndrome
Drugs Hormone therapy: tamoxifen, glucocorticoids,
Temporal arteritis and androgens
Antiphospholipid syndrome Inhibitors of angiogenesis: thalidomide
Thromboangitis obliterans Hemostatic therapy
Wegener’s granulomatosis Chemotherapy: cyclosporine and l-asparaginase
Behcet’s disease
LP, lumbar puncture.
deep brain white matter. Both the superficial and deep S deficiency, and antithrombin III deficiency are less
venous systems eventually drain into the internal jugular commonly encountered risk factors [10].
veins (Fig. 1). A prospective study involving 465 women found that
65% of cases had some form of risk factors like pregnancy,
puerperium, oral contraceptive pill (OCP) use, and hor-
Risk Factors monal replacement therapy associated with CSVT [11].
Studies also show that these gender-specific risk factors
CSVT is a multifactorial disease with at least one risk are not applicable to the pediatric or elderly population
factor implicated in 85% of affected adults [6] (Table 1). [12, 13]. A meta-analysis has shown that OCP users have
These risk factors are usually always associated with 6 times higher risk of developing CSVT than non-users.
thrombogenic triad of Virchow, which includes vessel The same study also concluded an increased risk of CSVT
wall injury, blood stasis, and hypercoagulability [5]. Pro- in patients with G20210A prothrombin polymorphism,
thrombotic conditions are the most common implicated factor V Leiden deficiency, and hyperhomocysteinemia
risk factor for CVT. Patients with hereditary thrombo- [14]. Studies also show an increased risk of CSVT in OCP
philia have an increased predisposition for developing users who are overweight or obese and are carriers of he-
any form of thrombosis, including CSVT. G20210A pro- reditary thrombophilia [15, 16].
thrombin polymorphism, factor V Leiden, and antiphos- Local head and neck infections are the most common
pholipid syndrome are most frequent causes. Protein C, infectious cause of CSVT, and studies have shown that it
Cerebral Venous Thrombosis Eur Neurol 2020;83:369–379 371
DOI: 10.1159/000509802
Extensive anastomoses found within the cerebral venous
Thrombosis of
system often allow the development of collateral circula-
Thrombosis of cerebral veins cerebral venous sinuses tion if there is an occlusion to venous flow. Cortical vein
occlusion can result in increased small vessel pressure,
depending on the extent of thrombosis and availability of
Increased venular and
capillary pressure
Decreased CSF absorption collaterals. This can further lead to disruption of the
blood-brain barrier, leakage of blood components into
the interstitial space causing vasogenic edema, and paren-
chymal tissue damage [24].
Increase in intracranial pressure Decrease in the cerebrospinal fluid drainage due to si-
nus occlusion can result from the dysfunction of arach-
noid granulations, causing an increase in intracranial
Cytotoxic and vasogenic edema pressure. A continuous rise in pressure results in capillary
hypertension, cerebral edema, and venous hemorrhage
Disruption of blood-brain barrier [25]. This further results in a decrease in the cerebral per-
fusion pressure and metabolic failure, followed by intra-
cellular edema and cytotoxic edema [26].
Parenchymal hemorrhage
Hemorrhagic infarction
Clinical Features
The clinical presentation of CVT is often variable, and
patients may present with a constellation of symptoms
Fig. 2. Pathophysiology of CVT [22]. CSF, cerebrospinal fluid.
depending on the site and extent of thrombosis, patient’s
age, and the underlying etiological factors. The most
common presentation includes signs of raised intracra-
is more common in lesser developed countries [17, 18]. nial pressure such as headache, reduced visual acuity, and
Intracranial neoplasm can result in CSVT due to local papilledema, focal neurological deficits, seizures, and dif-
compression or tumor invasion of the sinus [19]. A ret- fuse encephalopathy. Other uncommon presentations in-
rospective study conducted in a tertiary center involving clude subarachnoid hemorrhage, thunderclap headache,
90 CSVT patients showed that 14% of their patients had recurrent transient ischemic attacks, tinnitus, isolated
a history of some form of head trauma prior to the diag- headache, and multiple cranial nerve palsies in the setting
nosis, 7% of affected individuals had head and neck infec- of cavernous sinus thrombosis [4].
tions, and 8% had brain tumors [20].
Headache
Headache is one of the most common presentations
Pathophysiology and is seen in more than 80% of patients with CSVT [27].
Patients with headache often present in isolation or asso-
The pathophysiological mechanisms of CVT are not ciated with other signs and symptoms such as vomiting,
fully understood and are a complex mix of changes in he- papilledema, visual field defects, vision loss, tinnitus, as
modynamics and brain parenchyma [21]. The current well as abducens nerve palsy. Vision loss and papilledema
knowledge of the CVT pathophysiology is based on avail- is usually seen in patients with a chronic onset [10]. Stud-
able animal model studies. The clinical presentation of ies have shown that CVT patients can present with iso-
CVT can be explained by 2 pathological mechanisms – lated headache without any evidence of raised intracra-
thrombosis of cerebral veins and thrombosis of cerebral nial hypertension and is frequently seen in patients who
venous sinuses (Fig. 2). seek early medical attention [28]. Headache due to raised
Animal model studies have shown that sinus throm- intracranial pressure can occur as a result of large venous
bosis leads to sinus occlusion and backflow of blood into sinus thrombosis like sagittal sinus. These patients pres-
venules and capillaries, resulting in increased local pres- ent with sudden, severe, generalized, and progressive
sure, eventually resulting in massive cerebral edema [23]. headache that worsens with Valsalva, straining, and lying
372 Eur Neurol 2020;83:369–379 Idiculla/Gurala/Palanisamy/Vijayakumar/
DOI: 10.1159/000509802 Dhandapani/Nagarajan
down [29]. Some individuals may develop a sudden, se- eral motor deficits and focal or generalized seizures [22].
vere, explosive form called thunderclap headache that Isolated cortical vein thrombosis presents with headache,
mimic subarachnoid hemorrhage [30]. With the involve- seizures, and focal neurological deficits [10]. Deep venous
ment of the lateral sinus, patients can have raised intra- system thrombosis results in centrally located, bilateral
cranial pressure and symptoms similar to a middle ear thalamic lesions that presents with behavioral manifesta-
infection like fever, ear discharge, headache, and pain tions like amnesia, delirium, and mutism [35]. Cerebral
over the mastoid region [31]. herniation can result from diencephalon or brain stem
compression due to large unilateral infarcts or hemor-
Focal Neurological Deficits rhages. Coma can occur due to involvement of the brain
The most common form of deficit is motor weakness stem, thalamus, or from generalized seizures [33].
seen in the form of monoparesis, hemiparesis, or bilat-
eral involvement in patients with deep venous system
thrombosis. Though motor involvement is common, Diagnosis
these patients rarely have visual or sensory deficits [32].
Thrombosis of the cavernous sinus is usually associated The wide variety of clinical presentations makes it par-
with infection and affects extra ocular movements due to ticularly difficult for the diagnosis of CSVT. A high index
the involvement of oculomotor, abducent, and/or troch- of suspicion and appropriate clinical acumen is essential
lear nerves. They present with headache, eye pain, consti- for the detection of affected individuals.
tutional symptoms, proptosis, chemosis, periorbital ede-
ma, and paralysis of eye movements [33]. Laboratory Tests
CSVT patients should have a panel of tests done, in-
Seizures cluding complete blood count, comprehensive metabolic
Seizures are a common presentation in patients with panel, and a coagulation profile. These tests help identify
CSVT, especially in the acute phase of the disease [33]. It associated etiological risk factors of CVT [36]. A lumbar
is more common in patients with hemorrhagic supraten- puncture (LP) can be performed to rule out other causes
torial lesions, superior sagittal sinus or cortical vein like intracranial infections [36].
thrombosis, and in patients with focal neurological defi-
cits [10]. A prospective study of 194 patients with acute Neuroimaging
CVT found early symptomatic seizures in 44.3% patients Neuroimaging is the gold standard and is ultimately
and status epilepticus in 12.8% patients. They also found required for diagnosis and localization of CVT. Imaging
a high incidence of Todd’s paresis associated with sei- of the cerebral venous system is recommended in patients
zures [34]. with cortical hemorrhage of the unclear origin or with
infarction in multiple arterial territories by the American
Diffuse Encephalopathy Heart Association (AHA) and American Stroke Associa-
It is a more severe presentation of CSVT and individu- tion (ASA) [11].
als with deep venous system affection may develop en-
cephalopathy resulting in an alteration of consciousness, Computed Tomography Scan
mental status changes, delirium, apathy, or dysexecutive The recommended initial diagnostic imaging is a non-
symptoms. These patients can also develop bilateral or contrast computed tomography (CT) head for all patients
multifocal deficits or present with seizures. Encephalopa- presenting with acute neurological complaints such as
thy is a common occurrence among the elderly popula- headache, focal neurological deficits, altered mental sta-
tion [12]. tus, and seizures [10]. In about 30% of cases, CT may be
ISCVT summarized the occurrence of clinical mani- normal or show nonspecific abnormalities; thus, a nor-
festations – progressively worsening headache (most mal scan does not rule out CSVT [37]. Non-contrast CT
common symptom – 88.8%), seizures (39.3%), paresis shows direct signs like dense clot sign (visualization of
(37.2%), papilledema (28.3%), altered mental status thrombus in the cerebral veins and sinuses) and string or
(22%), aphasia (19.1%), stupor or coma (13.9%), diplopia cord sign (string or cord-like density indicating CSVT);
(13.5%), and visual field defects (13.2%) [6]. Left trans- as well as indirect signs like cerebral edema, mass effect,
verse sinus involvement may present with aphasia and and intracranial hemorrhage that can range from small
sagittal sinus involvement can result in unilateral or bilat- juxtacortical lesions to subarachnoid hemorrhage and
Cerebral Venous Thrombosis Eur Neurol 2020;83:369–379 373
DOI: 10.1159/000509802
Color version available online
Fig. 3. Presentations of CVT on CT head.
The figure was reproduced with permis-
sion from the Radiology Assistant website
(http://www.radiologyassistant.nl/en/
p4befacb3e4691/cerebral-venous-throm-
bosis.html). a Dense clot sign (blue arrows,
dense transverse sinus due to thrombosis).
Hemorrhagic infarction of the temporal
lobe (red arrow). b Empty delta sign (right
and left transverse sinus; and sigmoid sinus a b
thrombosis).
Color version available online
Fig. 4. Time-dependent appearance of
thrombus on different sequences of MRI
brain. The figure was reproduced with per-
mission from the Radiology Assistant web-
site (http://www.radiologyassistant.nl/en/
p4befacb3e4691/cerebral-venous-throm-
bosis.html). a T1-weighted images: red ar-
row, hyperintense signal due to thrombo-
sis. b T2-weighted image: blue arrow, nor-
mal flow in right sigmoid sinus and jugular
vein; red arrow, hyperintense signal due to a b
thrombosis.
large hemorrhagic infarcts. Contrast-enhanced CT shows MRI and Magnetic Resonance Venogram
direct signs like empty delta sign (a low-attenuated center MRI with contrast and magnetic resonance venogram
surrounded by a triangular area of contrast enhance- (MRV) is the most preferred diagnostic modality for
ment) and indirect signs, similar to non-contrast CT [38, CSVT, and the appearance of thrombus on different MRI
39] (Fig. 3). sequences are time dependent. Within 5 days, it appears
isointense on T1 and hypointense on T2-weighted im-
CT Venography ages. In 6–15 days, thrombus appears hyperintense on
Venous enhancement following a CT scan help evalu- both T1 and T2 sequences. After 15 days, they appear
ate filling defects in the cortical sinuses and veins, in- isointense on T1 and iso- or hyperintense on T2 sequenc-
creased collateral venous drainage, as well as enhance- es. Four months later, no abnormalities on T1 and subtle
ment of sinus walls in these patients [40]. CT venography abnormalities on T2 sequences can be detected [42–44]
(CTV) has an overall sensitivity of about 95% and may be (Fig. 4). The MRI appearances in the acute form occur
useful for patients with a subacute or chronic presenta- due to an increased amount of deoxyhemoglobin in the
tion [5]. Studies support the use of CTV for the diagnosis thrombus, and the changes seen with the subacute form
of cerebral sinus thrombosis and show it has less diagnos- is due to an increased concentration of methemoglobin
tic value for cortical vein thrombosis [41]. CTV is a rapid [8]. The absence of changes in the T1 signal sequence and
and reliable option, especially in those patients with con- normal flow pattern on the T2 sequence makes diagnosis
traindication to perform an MRI. particularly difficult in the acute form of the disease [45].
374 Eur Neurol 2020;83:369–379 Idiculla/Gurala/Palanisamy/Vijayakumar/
DOI: 10.1159/000509802 Dhandapani/Nagarajan
Table 2. Comparing the pros and cons of imaging modalities used in CVT diagnosis [8, 40, 42, 48]
Imaging modality Advantages Disadvantages
CT/CTV of brain Less expensive Ionizing radiation exposure
[40, 48]
Faster results were hence useful in an acute setting
Reduced motion-related artifacts Visualization of skull base structures is limited
Equivocal imaging findings and increased image resolution
No contraindication to using in patients with ferromagnetic
devices or pacemakers
A better demonstration of smaller cerebral vessels
MRI/MRV of brain Higher sensitivity for demonstrating parenchymal It is contraindicated in patients with many
[8, 42, 48] lesions like brain swelling, edema, and venous infarction pacemakers or ferromagnetic devices
No risk of radiation exposure More time to acquire results
A motion artifact is common
Diagnosing cortical vein thrombosis and partial
sinus occlusion is limited with MRV
Harder to distinguish between thrombosis and
hypoplasia of sinus
Cerebral The gold standard for diagnosis Invasive with associated surgical risks
angiography [40]
MRV, magnetic resonance venogram; CT, computed tomography; CTV, CT venography.
Gradient-echo T2 and susceptibility-weighted imaging circulation. There is an abrupt stopping of cortical veins
sequences help identify a thrombus as a hypointense area with surrounding tortuous and dilated collateral “cork-
and can be useful in the detection of acute CSVT. Suscep- screw” vessels [10].
tibility-weighted sequences are also beneficial for the di-
agnosis of an isolated cortical vein involvement [46]. Advantages and Disadvantages of Diagnostic
MRV is a noninvasive diagnostic modality used for the Modalities
diagnosis of CSVT suggested by the absence of normal A comparison of the various imaging modalities in-
flow in a vein or sinus. A contrast-enhanced MRV is con- cluding CT/CTV, MRI/MRV, and a digital subtraction
sidered more sensitive to time-of-flight MRV for the de- angiography is summarized in Table 2.
tection of thrombus in smaller veins [47].
Digital Subtraction Angiography Treatment
Cerebral angiography was considered the primary di-
agnostic procedure used for the diagnosis of intracranial Anticoagulant Therapy
venous abnormalities but has very well been replaced by Anticoagulant therapy is indicated in CSVT patients
CTV and MRI. It is performed when other imaging mo- to promote clot resolution and prevent clot expansion.
dalities are inconclusive or unavailable. Angiography can Small-scale studies comparing the safety and efficacy of
be challenging to interpret in the presence of anatomic anticoagulation with placebo has shown a clinically fa-
variations like superior sagittal sinus duplication, hypo- vorable trend toward the use of anticoagulants in patients
plasia of the anterior part of superior sagittal sinus, and with CSVT [49, 50]. A meta-analysis done with these
hypoplasia or aplasia of the transverse sinuses. The usual studies showed a reduction in poor outcome rates in CVT
findings include a partial or complete filling defect in the patients treated with unfractionated heparin or low-mo-
sinuses or veins, delayed emptying, and dilated collateral lecular-weight heparin (LMWH) [51]. The duration of
Cerebral Venous Thrombosis Eur Neurol 2020;83:369–379 375
DOI: 10.1159/000509802
anticoagulation, as well as the use of direct oral antico- though favored by some studies, remains controversial
agulants, is still a controversial topic since no large-scale [56]. A prospective study identified intracranial hemor-
randomized control trials are available. The 2017 Euro- rhage, cortical vein thrombosis, and focal neurological
pean Stroke Organization guidelines for the diagnosis deficits as independent predictors of early seizures and
and treatment of CSVT, endorsed by the European Acad- suggested that prophylactic antiepileptic therapy may
emy of Neurology, recommend the following for antico- benefit these patients [34]. Another study found focal
agulation therapy in CSVT [52]: sensory deficits and admission imaging showing focal
− Therapeutic dosage of heparin to all patients with acute edema or infarcts (ischemic/hemorrhagic) as significant
CVT, even in the presence of intracerebral hemorrhage. predictors of seizures in CVT patients [57]. Several stud-
− LMWH over unfractionated heparin except in patients ies have also demonstrated the presence of supratentorial
who are allergic to the LMWH or if fast anticoagulant lesion to be a predictor for seizures [58, 59]. Though the
effect reversal is required. duration of treatment is uncertain, it is recommended to
− The AHA/ASA guidelines recommend anticoagula- give antiepileptic therapy to acute CSVT patients with
tion for 3–6 months in provoked CSVT, 6–12 months seizures and supratentorial lesions to prevent recurrence
in unprovoked CSVT, and potentially lifelong in re- [52].
current CSVT, VTE following CSVT, or CSVT associ-
ated with severe thrombophilia with target interna- Treatment of Raised Intracranial Pressure
tional normalized ratio of 2–3 [5]. Cerebral edema is common in CSVT patients. How-
ever, mild swelling improves with anticoagulant therapy,
Thrombolysis which dissolves thrombus, improving flow, and thereby
CSVT patients have a favorable clinical outcome with reducing intracranial pressure. Patients who develop a
anticoagulant therapy; however, some patients may fail to headache can be given analgesics for symptomatic relief.
improve or clinically deteriorate despite treatment. AHA/ Transtentorial herniation of the brain is the most com-
ASA suggests that these patients may have an added treat- mon cause of death in CSVT patients [60]. Carbonic an-
ment option of endovascular thrombolysis performed in hydrase inhibitors like acetazolamide help in reducing
advanced centers [5]. Thrombolysis aids the dissolution of the intracranial pressure (ICP) and alleviating headache
the clot and reopens occluded cerebral sinus or veins. A sys- as well as preventing visual damage [61]. The European
tematic review of 15 studies showed that thrombolysis has Federation of Neurological Societies recommends the
a significant increase in major bleeding complications as- following [62]:
sociated with it [53]. The thrombolysis or anticoagulation − LP can be considered before initiation of anticoagula-
for cerebral venous thrombosis trial is an ongoing multi- tion, in the absence of parenchymal abnormalities
center, randomized control study to determine if throm- (large infarcts or hemorrhages) in patients with intra-
bolysis will improve outcome in severe CVT patients with cranial hypertension.
poor outcome [54]. In the near future, this study may pro- − Acetazolamide may be considered in patients with
vide a better understanding of the use of thrombolytics in persistent papilledema.
CSVT patients. The British Committee for Standards in − In patients with continuing visual deterioration de-
Hematology recommends that endovascular thrombolysis spite repeated LP and Acetazolamide administration,
be used as a last resort in patients who have a fatal outcome shunting procedures like lumboperitoneal, ventriculo-
or do not respond to anticoagulant therapy. However, it is peritoneal shunts, and optic nerve fenestration can be
not indicated in patients whose deterioration is attributed considered.
to intracranial hemorrhage [55]. − Steroid therapy is ineffective due to lack of scientific
evidence.
Symptomatic Therapy − Anti-edema treatment should be carried out based on
Symptomatic treatment mainly involves the manage- the general principles of treatment for raised ICP.
ment of seizures and increased intracranial pressure, These include elevating head at 30°, hyperventilation
which can result in vision loss and headache. (target PaCO2 = 30–35 mm Hg), and intravenous ad-
ministration of osmotic diuretics.
Seizure Control − Decompressive surgery (craniectomy) is recommend-
Seizures are frequent, affecting up to 50% of all CVT ed in patients with severe thrombosis and with im-
patients, and the prophylactic use of antiepileptic drugs pending herniation due to a large parenchymal lesion.
376 Eur Neurol 2020;83:369–379 Idiculla/Gurala/Palanisamy/Vijayakumar/
DOI: 10.1159/000509802 Dhandapani/Nagarajan
Pregnancy and Contraception worse long-term prognosis include male sex, intracranial
CSVT occurrence during pregnancy or puerperium is hemorrhage on imaging, infectious or malignant etiolo-
not a contraindication for future pregnancies [10]. CSVT gy, altered mental status and/or Glasgow Coma Scale < 9,
occurring during these periods should be treated with and thrombosis of the deep cerebral venous system [6,
LMWH and continued through 6 weeks of postpartum. 12].
All forms of hormonal contraception except progester-
one-only therapies should be stopped in patients who de-
velop CSVT with OCP or hormone replacement therapy. Conclusion
Other forms of contraception can be used as an alterna-
tive in these patients. CSVT is a rare form of stroke that often affects young-
er age-groups, especially reproductive age-group females.
Treatment of Underlying Risk Factors The clinical presentation is variable with headache being
A thorough diagnostic evaluation to identify underly- the most common presenting symptom, and a high index
ing etiological factors followed by proper treatment is es- of clinical suspicion is required for detecting affected in-
sential in the management of CSVT. dividuals. The diagnosis is predominantly using a CTV/
− Antibiotics for sepsis and other intra- and extracranial MRI/MRV and cerebral angiography if other imaging
infections. modalities fail. Anticoagulation with LMWH is the main-
− Chemotherapy should be given as recommended for stay of the treatment, and endovascular thrombolysis is
specific cancers. still controversial. Intracranial hemorrhage is not consid-
− Stop all hormonal therapy like oral contraceptive pills ered a contraindication to the use of anticoagulants in
and hormone replacement therapy. Progesterone- CVT. Patients with CVT have an increased risk of recur-
containing treatments can be used [10]. rence of CVT and other VTEs.
− Steroids are recommended in patients with acute
CSVT and Behcet’s disease, vasculitis, or other inflam-
matory diseases like systemic lupus erythematosus Future Research
[52].
There is still a lot of research required to fully under-
stand the natural course of CVT, which will further aid
Outcomes with the diagnosis and management of the disease. Future
studies are required to understand the epidemiology and
The predictors of acute mortality were transtentorial etiological risk factors due to the rarity of the disease.
herniation resulting from raised ICP, status epilepticus, Newer diagnostic techniques are essential, and large-scale
and underlying comorbidities. Predictors of mortality at comparative studies of existing imaging techniques are
30 days were depressed consciousness, altered mental sta- required. Large randomized control trials are required for
tus, thrombosis of the deep venous system, right hemi- providing stronger evidence for the various therapeutic
sphere hemorrhage, and posterior fossa lesions [60]. A interventions of CVT. Further studies are required that
systematic review that studied the natural course of CSVT compare the different therapies to help aid better treat-
found a mortality rate of 5.6% in the acute phase and 9.4% ment to patients with CVT because of increased mortal-
at the end of follow-up. The study also found that com- ity rates.
plete or partially complete recovery (mild cognitive and
functional deficits) was seen in 88% of cases, and the re-
currence rate was 2.8% [63]. Headache is the most com- Acknowledgements
mon complaint that is encountered during the follow-up
The authors would like to thank Deanship of Scientific Re-
of a CVT patient, which, if persistent, can raise the con-
search at Majmaah University for supporting this work under
cerns of recurrence. It should be evaluated with neuroim- project number R-1441-96.
aging (CT/MRI) and LP if necessary [10]. Patients with
CSVT have an increased risk of developing CSVT recur-
rence in about one-third of cases or other forms of VTE. Statement of Ethics
In these cases, thrombophilic states should be ruled out
with appropriate diagnostic modalities [32]. Markers for The authors have no conflicts of interest to declare.
Cerebral Venous Thrombosis Eur Neurol 2020;83:369–379 377
DOI: 10.1159/000509802
Conflict of Interest Statement Author Contributions
The authors declare that they have no conflict of interests. All authors have been involved in the preparation of this man-
uscript. All authors have read and approved the manuscript. The
corresponding author has full access to data and has the right to
publish this data.
Funding Sources
Deanship of Scientific Research at Majmaah University, under
project number R-1441-96.
References
1 Alvis-Miranda HR, Milena Castellar-Leones 14 Dentali F, Crowther M, Ageno W. Thrombo- 25 Ueda K, Nakase H, Miyamoto K, Otsuka H,
S, Alcala-Cerra G, Rafael Moscote-Salazar L. philic abnormalities, oral contraceptives, and Sakaki T. Impact of anatomical difference of
Cerebral sinus venous thrombosis. J Neurosci risk of cerebral vein thrombosis: a meta-anal- the cerebral venous system on microcircula-
Rural Pract. 2013;4(4):427–38. ysis. Blood. 2006;107(7):2766–73. tion in a gerbil superior sagittal sinus occlu-
2 Guenther G, Arauz A. Cerebral venous 15 Zuurbier SM, Arnold M, Middeldorp S, sion model. Acta Neurochir. 2000;142(1):75–
thrombosis: a diagnostic and treatment up- Broeg-Morvay A, Silvis SM, Heldner MR, et 82.
date. Neurologia. 2011;26(8):488–98. al. Risk of cerebral venous thrombosis in 26 Gotoh M, Ohmoto T, Kuyama H. Experimen-
3 Ferro JM, Canhão P. Cerebral venous sinus obese women. JAMA Neurol. 2016; 73(5): tal study of venous circulatory disturbance by
thrombosis: update on diagnosis and man- 579–84. dural sinus occlusion. Acta Neurochir. 1993;
agement. Curr Cardiol Rep. 2014;16(9):523. 16 de Bruijn SF, Stam J, Koopman MM, Vanden- 124(2–4):120–6.
4 Bousser MG, Ferro JM. Cerebral venous broucke JP. Case-control study of risk of ce- 27 Bousser MG, Ross Russell R. Cerebral venous
thrombosis: an update. Lancet Neurol. 2007; rebral sinus thrombosis in oral contraceptive thrombosis. London: WB Saunders; 1997.
6(2):162–70. users and in [correction of who are] carriers Vol. 1.
5 Saposnik G, Barinagarrementeria F, Brown of hereditary prothrombotic conditions. The 28 Cumurciuc R, Crassard I, Sarov M, Valade D,
RD Jr, Bushnell CD, Cucchiara B, Cushman Cerebral Venous Sinus Thrombosis Study Bousser MG. Headache as the only neurolog-
M, et al. Diagnosis and management of cere- Group. BMJ. 1998;316(7131):589–92. ical sign of cerebral venous thrombosis: a se-
bral venous thrombosis: a statement for 17 Sidhom Y, Mansour M, Messelmani M, Der- ries of 17 cases. J Neurol Neurosurg Psychia-
healthcare professionals from the American bali H, Fekih-Mrissa N, Zaouali J, et al. Cere- try. 2005;76(8):1084–7.
Heart Association/American Stroke Associa- bral venous thrombosis: clinical features, risk 29 Timóteo Â, Inácio N, Machado S, Pinto AA,
tion. Stroke. 2011;42(4):1158–92. factors, and long-term outcome in a Tunisian Parreira E. Headache as the sole presenta-
6 Ferro JM, Canhão P, Stam J, Bousser MG, cohort. J Stroke Cerebrovasc Dis. 2014;23(6): tion of cerebral venous thrombosis: a pro-
Barinagarrementeria F. Prognosis of cerebral 1291–5. spective study. J Headache Pain. 2012; 13(6):
vein and dural sinus thrombosis: results of the 18 Korathanakhun P, Petpichetchian W, Sathi- 487–90.
International Study on Cerebral Vein and rapanya P, Geater SL. Cerebral venous throm- 30 Heckmann JG, Schüttler M, Tomandl B.
Dural Sinus Thrombosis (ISCVT). Stroke. bosis: comparing characteristics of infective Achard-Lévi syndrome: pupil-sparing oculo-
2004;35(3):664–70. and non-infective aetiologies: a 12-year retro- motor nerve palsy due to midbrain stroke.
7 Zivadinov R, Chung CP. Potential involve- spective study. Postgrad Med J. 2015; Cerebrovasc Dis. 2003;16(1):109–10.
ment of the extracranial venous system in 91(1082):670–4. 31 Teichgraeber JF, Per-Lee JH, Turner JS. Lat-
central nervous system disorders and aging. 19 Grisold W, Oberndorfer S, Struhal W. Stroke eral sinus thrombosis: a modern perspective.
BMC Med. 2013;11:260. and cancer: a review. Acta Neurol Scand. Laryngoscope. 1982;92(7 Pt 1):744–51.
8 Dmytriw AA, Song JSA, Yu E, Poon CS. Ce- 2009;119(1):1–16. 32 Turner SE, Parry-Jones AR, Punter M, Hur-
rebral venous thrombosis: state of the art di- 20 Giladi O, Steinberg DM, Peleg K, Tanne D, ford R, Thachil J. Cerebral venous thrombo-
agnosis and management. Neuroradiology. Givon A, Grossman E, et al. Head trauma is sis-a primer for the haematologist. Blood Rev.
2018 Jul;60(7):669–85. the major risk factor for cerebral sinus-vein 2015;29(1):45–50.
9 Meder JF, Chiras J, Roland J, Guinet P, Bra- thrombosis. Thromb Res. 2016;137:26–9. 33 Stam J. Thrombosis of the cerebral veins and
card S, Bargy F. Venous territories of the 21 Schaller B, Graf R. Cerebral venous infarc- sinuses. N Engl J Med. 2005;352(17):1791–8.
brain. J Neuroradiol. 1994;21(2):118–33. tion: the pathophysiological concept. Cere- 34 Masuhr F, Busch M, Amberger N, Ortwein H,
10 Ferro JM, Canhão P, Aguiar de Sousa D. Ce- brovasc Dis. 2004;18(3):179–88. Weih M, Neumann K, et al. Risk and predic-
rebral venous thrombosis. Presse Med. 2016 22 Long B, Koyfman A, Runyon MS. Cerebral tors of early epileptic seizures in acute cere-
Dec;45(12 Pt 2):e429–50. venous thrombosis: a challenging neurologic bral venous and sinus thrombosis. Eur J Neu-
11 Coutinho JM, Ferro JM, Canhão P, Bari- diagnosis. Emerg Med Clin North Am. 2017 rol. 2006;13(8):852–6.
nagarrementeria F, Cantú C, Bousser MG, et Nov;35(4):869–78. 35 Kothare SV, Ebb DH, Rosenberger PB, Buon-
al . Cerebral venous and sinus thrombosis in 23 Röttger C, Bachmann G, Gerriets T, Kaps M, anno F, Schaefer PW, Krishnamoorthy KS.
women. Stroke. 2009;40(7):2356–61. Kuchelmeister K, Schachenmayr W, et al. A Acute confusion and mutism as a presenta-
12 Ferro JM, Canhão P, Bousser MG, Stam J, new model of reversible sinus sagittalis supe- tion of thalamic strokes secondary to deep ce-
Barinagarrementeria F, Investigators I. Cere- rior thrombosis in the rat: magnetic reso- rebral venous thrombosis. J Child Neurol.
bral vein and dural sinus thrombosis in elder- nance imaging changes. Neurosurgery. 2005; 1998;13(6):300–3.
ly patients. Stroke. 2005;36(9):1927–32. 57(3):573–80. 36 Canhão P, Abreu LF, Ferro JM, Stam J, Bouss-
13 deVeber G, Andrew M, Adams C, Bjornson B, 24 Ungersböck K, Heimann A, Kempski O. Ce- er MG, Barinagarrementeria F, et al. Safety of
Booth F, Buckley DJ, et al. Cerebral sinove- rebral blood flow alterations in a rat model of lumbar puncture in patients with cerebral ve-
nous thrombosis in children. N Engl J Med. cerebral sinus thrombosis. Stroke. 1993;24(4): nous thrombosis. Eur J Neurol. 2013; 20(7):
2001;345(6):417–23. 563–70. 1075–80.
378 Eur Neurol 2020;83:369–379 Idiculla/Gurala/Palanisamy/Vijayakumar/
DOI: 10.1159/000509802 Dhandapani/Nagarajan
37 Tanislav C, Siekmann R, Sieweke N, Allen- 46 Boukobza M, Crassard I, Bousser MG, Chab- 55 Tait C, Baglin T, Watson H, Laffan M, Makris
dörfer J, Pabst W, Kaps M, et al. Cerebral vein riat H. MR imaging features of isolated corti- M, Perry D, et al. Guidelines on the investiga-
thrombosis: clinical manifestation and diag- cal vein thrombosis: diagnosis and follow-up. tion and management of venous thrombosis
nosis. BMC Neurol. 2011;11:69. AJNR Am J Neuroradiol. 2009;30(2):344–8. at unusual sites. Br J Haematol. 2012; 159(1):
38 van Dam LF, van Walderveen MAA, Kroft 47 Ganeshan D, Narlawar R, McCann C, Jones 28–38.
LJM, Kruyt ND, Wermer MJH, van Osch HL, Curtis J. Cerebral venous thrombosis-A 56 Breteau G, Mounier-Vehier F, Godefroy O,
MJP, et al. Current imaging modalities for di- pictorial review. Eur J Radiol. 2010; 74(1): Gauvrit JY, Mackowiak-Cordoliani MA, Gi-
agnosing cerebral vein thrombosis: a critical 110–6. rot M, et al. Cerebral venous thrombosis
review. Thromb Res. 2020 Mar 19;189:132–9. 48 Linn J, Ertl-Wagner B, Seelos KC, Strupp M, 3-year clinical outcome in 55 consecutive pa-
39 Coutinho JM, van den Berg R, Zuurbier SM, Reiser M, Brückmann H, et al. Diagnostic val- tients. J Neurol. 2003;250(1):29–35.
VanBavel E, Troost D, Majoie CB. et al. Small ue of multidetector-row CT angiography in 57 Ferro JM, Correia M, Rosas MJ, Pinto AN,
juxtacortical hemorrhages in cerebral venous the evaluation of thrombosis of the cerebral Neves G. Seizures in cerebral vein and dural
thrombosis. Ann Neurol. 2014;75(6):908–16. venous sinuses. AJNR Am J Neuroradiol. sinus thrombosis. Cerebrovasc Dis. 2003;
40 Rodallec MH, Krainik A, Feydy A, Hélias A, 2007;28(5);946–52. 15(1–2):78–83.
Colombani JM, Jullès MC, et al. Cerebral ve- 49 De Bruijn SFTM, Stam J; for the Cerebral Ve- 58 Neves JM, Canhão P, Bousser MG, Stam J,
nous thrombosis and multidetector CT angi- nous Sinus Thrombosis Study Group. Ran- Barinagarrementeria F. Early seizures in cere-
ography: tips and tricks. Radiographics. 2006 domized, placebo-controlled trial of antico- bral vein and dural sinus thrombosis: risk fac-
Oct;26(Suppl 1):S5–3. agulant treatment with low-molecular-weight tors and role of antiepileptics. Stroke. 2008;
41 Linn J, Michl S, Katja B, Pfefferkorn T, Wies- heparin for cerebral sinus thrombosis. Stroke. 39(4):1152–8.
mann M, Hartz S, et al. Cortical vein throm- 1999;30(3):484–8. 59 Kalita J, Chandra S, Misra UK. Significance of
bosis: the diagnostic value of different imag- 50 Stam KM, Villringer A, Meister,W, Mehraein seizure in cerebral venous sinus thrombosis.
ing modalities. Neuroradiology. 2010;52(10): S, Garner C, Pellkofer M, et al. Heparin treat- Seizure. 2012;21(8):639–42.
899–911. ment in sinus venous thrombosis. Lancet. 60 Canhão P, Ferro JM, Lindgren AG, Bousser
42 Leach JL, Fortuna RB, Jones BV, Gaskill-Shi- 1991;338(8767):597–600. MG, Stam J, Barinagarrementeria F, et al.
pley MF. Imaging of cerebral venous throm- 51 Stam J, de Bruijn SFTM, deVeber G. Antico- Causes and predictors of death in cerebral ve-
bosis: current techniques, spectrum of find- agulation for cerebral venous sinus thrombo- nous thrombosis. Stroke. 2005;36(8);1720–5.
ings, and diagnostic pitfalls. Radiographics. sis. Cochrane Database Syst Rev. 2001: 4(8): 61 Wall M, McDermott MP, Kieburtz KD, Cor-
2006;26(Suppl 1):S19–3. CD002005. bett JJ, Feldon SE. Effect of acetazolamide on
43 Bergui M, Bradac GB. Clinical picture of pa- 52 Stam JM, Bousser MG, Canhão P, Coutinho visual function in patients with idiopathic in-
tients with cerebral venous thrombosis and JM, Crassard I, Dentali F, et al. European tracranial hypertension and mild visual loss:
patterns of dural sinus involvement. Cerebro- Stroke Organization guideline for the diagno- the idiopathic intracranial hypertension
vasc Dis. 2003;16(3):211–6. sis and treatment of cerebral venous throm- treatment trial. JAMA. 2014; 311(16): 1641–
44 Idbaih A, Boukobza M, Crassard I, Porcher R, bosis: endorsed by the European Academy of 1651.
Bousser MG, Chabriat H. MRI of clot in cere- Neurology. Eur J Neurol. 2017; 24(10): 1203– 62 Einhäupl K, Stam J, Bousser MG, De Bruijn
bral venous thrombosis: high diagnostic value 13. SF, Ferro JM, Martinelli I, et al. EFNS guide-
of susceptibility-weighted images. Stroke. 53 Dentali F, Squizzato A, Gianni M, De Lodovi- line on the treatment of cerebral venous and
2006;37(4):991–5. ci ML, Venco A, Paciaroni M, et al. Safety of sinus thrombosis in adult patients. Eur J Neu-
45 Hinman JM, Provenzale JM. Hypointense thrombolysis in cerebral venous thrombosis. rol. 2010;17(10):1229–35.
thrombus on T2-weighted MR imaging: a po- A systematic review of the literature. Thromb 63 Dentali F, Gianni M, Crowther MA, Ageno
tential pitfall in the diagnosis of dural sinus Haemost. 2010;104(5):1055–62. W. Natural history of cerebral vein thrombo-
thrombosis. Eur J Radiol. 2002;41(2):147–52. 54 Coutinho JM, Ferro JM, Zuurbier SM, Mink sis: a systematic review. Blood. 2006; 108(4):
MS, Canhão P, Crassard I, et al. Thrombolysis 1129–34.
or anticoagulation for cerebral venous throm-
bosis: rationale and design of the TO-ACT
trial. Int J Stroke. 2013;8(2):135–40.
Cerebral Venous Thrombosis Eur Neurol 2020;83:369–379 379
DOI: 10.1159/000509802
You might also like
- Clinical Handbook of Cardiac ElectrophysiologyFrom EverandClinical Handbook of Cardiac ElectrophysiologyBenedict M. GloverNo ratings yet
- Radiologic Clues To Cerebral Venous ThrombosisDocument18 pagesRadiologic Clues To Cerebral Venous ThrombosisRudolph MuliawanNo ratings yet
- Microcirculation in Cardiovascular DiseasesFrom EverandMicrocirculation in Cardiovascular DiseasesEnrico Agabiti-RoseiNo ratings yet
- Cerebral Venous Sinus ThrombosisDocument34 pagesCerebral Venous Sinus ThrombosisNeurologia homicNo ratings yet
- Symptomatic non-stenotic carotid disease: current challenges and opportunities for diagnosis and treatmentDocument8 pagesSymptomatic non-stenotic carotid disease: current challenges and opportunities for diagnosis and treatmentsnzbtk8df9No ratings yet
- Research Article: Retinal Structural and Microvascular Alterations in Different Acute Ischemic Stroke SubtypesDocument10 pagesResearch Article: Retinal Structural and Microvascular Alterations in Different Acute Ischemic Stroke SubtypesKarina NathaniaNo ratings yet
- Visualizing Cerebral Small Vessel Degeneration During Aging and Diseases Using2Document15 pagesVisualizing Cerebral Small Vessel Degeneration During Aging and Diseases Using2Sofía ValdésNo ratings yet
- Evidence-Based Diagnosis and Management of Chronic Subdural HematomaDocument9 pagesEvidence-Based Diagnosis and Management of Chronic Subdural HematomaJorge MontenegroNo ratings yet
- Cerebral Vein and Dural Sinus ThrombosisDocument32 pagesCerebral Vein and Dural Sinus ThrombosisdwiNo ratings yet
- Fmedt 04 748949Document12 pagesFmedt 04 748949Orlin ZlatarskiNo ratings yet
- A Review of The Management of Cerebral Vasospasm After Aneurysmal Subarachnoid HemorrhageDocument15 pagesA Review of The Management of Cerebral Vasospasm After Aneurysmal Subarachnoid HemorrhageAlanNo ratings yet
- Scientific Report Journal 22 NovDocument6 pagesScientific Report Journal 22 Novnaresh kotraNo ratings yet
- J Jacc 2022 09 044Document17 pagesJ Jacc 2022 09 044Ivan BitunjacNo ratings yet
- Stroke Prevention and Treatment in Sickle Cell Disease: Robert J. Adams, MS, MDDocument4 pagesStroke Prevention and Treatment in Sickle Cell Disease: Robert J. Adams, MS, MDMeshaki MbarukaNo ratings yet
- 128 FullDocument12 pages128 FullYovita LimiawanNo ratings yet
- Acute Intracerebral Haemorrhage - Pract Neurol (2021)Document12 pagesAcute Intracerebral Haemorrhage - Pract Neurol (2021)Billy Priyanto HNo ratings yet
- Acute Intracerebral Haemorrhage BMJ 2021Document12 pagesAcute Intracerebral Haemorrhage BMJ 2021Jennifer MorenoNo ratings yet
- Imaging Findings of Intraventricular and Ependymal LesionsDocument16 pagesImaging Findings of Intraventricular and Ependymal Lesionsanggi abNo ratings yet
- Current Concepts and Future Perspectives of Stem Cell Therapy in Peripheral Arterial DiseaseDocument3 pagesCurrent Concepts and Future Perspectives of Stem Cell Therapy in Peripheral Arterial DiseaseAyushmanNo ratings yet
- Current Endovascular Strategies For Cerebral Venous Thrombosis: Report of The SNIS Standards and Guidelines CommitteeDocument8 pagesCurrent Endovascular Strategies For Cerebral Venous Thrombosis: Report of The SNIS Standards and Guidelines CommitteeRafika Ayu NadiaNo ratings yet
- Cerebral Venous Thrombosis: J.M.CoutinhoDocument7 pagesCerebral Venous Thrombosis: J.M.CoutinhoWilliam ReinaldyNo ratings yet
- 1 s2.0 S0022510X13013646 MainDocument2 pages1 s2.0 S0022510X13013646 Mainfakhrusy rizqyNo ratings yet
- Farhat Research ArticleDocument1 pageFarhat Research ArticleDr MS HarisNo ratings yet
- Practneurol 2020 002763Document12 pagesPractneurol 2020 002763Fitri ainun MalahayatiNo ratings yet
- Stroke NarrativeDocument10 pagesStroke Narrativecfalcon.medicinaNo ratings yet
- Mitral Valve Prolapse Research Jacc December 2022Document17 pagesMitral Valve Prolapse Research Jacc December 2022Nox ÁtroposNo ratings yet
- 803 FullDocument8 pages803 FullYud yaoNo ratings yet
- Acv PDFDocument14 pagesAcv PDFFelipe AlcainoNo ratings yet
- AnimalDocument29 pagesAnimalDwi ApriyantiNo ratings yet
- Cerebral AneurysmsDocument12 pagesCerebral AneurysmsDyah Ayu Puspita AnggarsariNo ratings yet
- Mei 2018Document9 pagesMei 2018FidelisaNo ratings yet
- Dural Venous Sinus Thrombosis in Patients Presenting With Blunt Traumatic Brain Injuries and Skull Fractures - A Systematic Review and Meta-AnalysisDocument14 pagesDural Venous Sinus Thrombosis in Patients Presenting With Blunt Traumatic Brain Injuries and Skull Fractures - A Systematic Review and Meta-Analysisclaudio RivasNo ratings yet
- Beyond The Brain Stroke AhaDocument11 pagesBeyond The Brain Stroke AhaAmet Arturo Gutierrez CorderoNo ratings yet
- Mks 054Document7 pagesMks 054Mirela CiobanescuNo ratings yet
- Doppler Transcreaneal y Ecografía Del Nervio ÓpticoDocument15 pagesDoppler Transcreaneal y Ecografía Del Nervio ÓpticoBenjamínGalvanNo ratings yet
- Thick and Diffuse Cisternal Clot Independently Predicts Vasospasm-Related Morbidity and Poor Outcome After Aneurysmal Subarachnoid HemorrhageDocument9 pagesThick and Diffuse Cisternal Clot Independently Predicts Vasospasm-Related Morbidity and Poor Outcome After Aneurysmal Subarachnoid HemorrhageVanessa LandaNo ratings yet
- Brain Arteriovenous MalformationsDocument20 pagesBrain Arteriovenous MalformationsTony NgNo ratings yet
- Neuro-Ultrasonography 2020Document15 pagesNeuro-Ultrasonography 2020Santiago PovedaNo ratings yet
- Hemodinamika SSSDocument12 pagesHemodinamika SSSEmir BegagićNo ratings yet
- Transcranial Doppler: An Introduction For Primary Care PhysiciansDocument7 pagesTranscranial Doppler: An Introduction For Primary Care PhysiciansdediNo ratings yet
- 3book ChaptersupratentorialbraintumorsinchildrenDocument13 pages3book ChaptersupratentorialbraintumorsinchildrenLuciano AlvesNo ratings yet
- Endovascular Management of Acute Epidural Hematomas: Clinical Experience With 80 CasesDocument7 pagesEndovascular Management of Acute Epidural Hematomas: Clinical Experience With 80 CasesDeby AnditaNo ratings yet
- Acute Intracerebral HaemorrhageDocument12 pagesAcute Intracerebral HaemorrhageZARF27No ratings yet
- Kim 2019Document7 pagesKim 2019Edison Chiriboga OrtegaNo ratings yet
- ACV HemorrágicoDocument12 pagesACV HemorrágicoLUIS FELIPE ARTEAGA ARREDONDONo ratings yet
- Cerebral Venous Thrombosis: A Practical GuideDocument12 pagesCerebral Venous Thrombosis: A Practical Guidedanby danbyNo ratings yet
- Cerebral Venous ThrombosisDocument14 pagesCerebral Venous ThrombosisSrinivas PingaliNo ratings yet
- Intracranial CystsDocument9 pagesIntracranial CystsjosephNo ratings yet
- Tomasello ContourDocument11 pagesTomasello ContourangelNo ratings yet
- Acute Intracerebral HeamorrhageDocument12 pagesAcute Intracerebral HeamorrhagePaul CalderónNo ratings yet
- Management of Acute Ischemic Stroke Due To Large-Vessel OcclusionDocument12 pagesManagement of Acute Ischemic Stroke Due To Large-Vessel OcclusionYaiza VillalobosNo ratings yet
- Cerebral Venous Sinus Thrombosis Review: Diagnosis and Treatment AdvancesDocument11 pagesCerebral Venous Sinus Thrombosis Review: Diagnosis and Treatment AdvancesdjcafNo ratings yet
- Role of CT Scan in Diagnosis and Management of Otogenic Intracranial AbscessDocument5 pagesRole of CT Scan in Diagnosis and Management of Otogenic Intracranial AbscessayundariprimaraniNo ratings yet
- 2022 Perioperative Complications of Transvenous Embolization of Ruptured Intracranial Arteriovenous MalformationsDocument7 pages2022 Perioperative Complications of Transvenous Embolization of Ruptured Intracranial Arteriovenous MalformationsstaseaditNo ratings yet
- Practneurol 2020 002763Document12 pagesPractneurol 2020 002763Edgar MoralesNo ratings yet
- 128 FullDocument12 pages128 FullMarlen Adriana Hilario GómezNo ratings yet
- Lotivio Midterm-AssignmentDocument14 pagesLotivio Midterm-AssignmentEmmadelone Rah LotivioNo ratings yet
- 33288539: Acute Intracerebral Haemorrhage Diagnosis and Management PDFDocument12 pages33288539: Acute Intracerebral Haemorrhage Diagnosis and Management PDFnz mzNo ratings yet
- Resumption of Antithrombotic Agents in C PDFDocument28 pagesResumption of Antithrombotic Agents in C PDFNurul FajriNo ratings yet
- Article Zamboni BMJDocument9 pagesArticle Zamboni BMJfxchaserNo ratings yet
- Jamaneurology Ferro 2019 Oi 190070 PDFDocument9 pagesJamaneurology Ferro 2019 Oi 190070 PDFusman choudhryNo ratings yet
- ITP Saudi 2019Document7 pagesITP Saudi 2019danby danbyNo ratings yet
- Cerebral Venous Thrombosis: A Comprehensive Review: Clinical Neurology: Review ArticleDocument11 pagesCerebral Venous Thrombosis: A Comprehensive Review: Clinical Neurology: Review Articledanby danbyNo ratings yet
- Tips For Trainees: Some Practical Tips On Clinical ExaminationDocument5 pagesTips For Trainees: Some Practical Tips On Clinical Examinationdanby danbyNo ratings yet
- Cerebral Venous Thrombosis: A Practical GuideDocument12 pagesCerebral Venous Thrombosis: A Practical Guidedanby danbyNo ratings yet
- 01 STR 0000117571 76197 26Document7 pages01 STR 0000117571 76197 26danby danbyNo ratings yet
- Tips For Trainees: Some Practical Tips On Clinical ExaminationDocument5 pagesTips For Trainees: Some Practical Tips On Clinical Examinationdanby danbyNo ratings yet
- Jamaneurology Ferro 2019 Oi 190070 PDFDocument9 pagesJamaneurology Ferro 2019 Oi 190070 PDFusman choudhryNo ratings yet
- Cerebral Venous Thrombosis: A Practical GuideDocument12 pagesCerebral Venous Thrombosis: A Practical Guidedanby danbyNo ratings yet
- 01 STR 0000117571 76197 26Document7 pages01 STR 0000117571 76197 26danby danbyNo ratings yet
- North of Tyne Formulary Version 5 4finalDocument194 pagesNorth of Tyne Formulary Version 5 4finalAnonymous VfSIDMyrmENo ratings yet
- Mwami Schools of Nursing and MidwiferyDocument47 pagesMwami Schools of Nursing and MidwiferyBaldwin Hamzcorp HamoongaNo ratings yet
- VTE Prophylaxis GuidelinesDocument1 pageVTE Prophylaxis GuidelinesSylvia Ruth Alisa Nababan100% (1)
- Anorectal Disorders Guide: Hemorrhoids, Fissures, Fistulas & MoreDocument41 pagesAnorectal Disorders Guide: Hemorrhoids, Fissures, Fistulas & MoreMuhammadNo ratings yet
- TISSEEL Fibrin Sealant Prescribing InformationDocument3 pagesTISSEEL Fibrin Sealant Prescribing InformationCNo ratings yet
- CTEPH - JACC 2020 - FocusDocument15 pagesCTEPH - JACC 2020 - FocusDaniela PekeNo ratings yet
- Basics Arthroplasty ShrinandDocument420 pagesBasics Arthroplasty ShrinandPon Aravindhan A SNo ratings yet
- Robbins Basic Pathology 9th Edition Kumar Test BankDocument25 pagesRobbins Basic Pathology 9th Edition Kumar Test BankJamesGonzalezwbpg100% (43)
- Stroke - RN YoutubeDocument10 pagesStroke - RN YoutubeMarina Wasem NetzlaffNo ratings yet
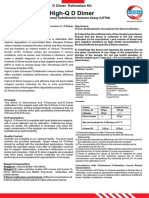
- D DimerDocument2 pagesD DimerRaji Creations - தமிழன்No ratings yet
- Post Stroke Scalp AcupunctureDocument64 pagesPost Stroke Scalp AcupunctureJosé Mário91% (11)
- Total Hip Replacement Rehab ProtocolDocument11 pagesTotal Hip Replacement Rehab ProtocolnurulishtimalNo ratings yet
- Atrial Fibrillation Epidemiology, Pathophysiology, and Clinical OutcomesDocument17 pagesAtrial Fibrillation Epidemiology, Pathophysiology, and Clinical OutcomesRESIDENTES MEDICINA INTERNANo ratings yet
- JCM 09 00743 v2 PDFDocument20 pagesJCM 09 00743 v2 PDFGordon BongNo ratings yet
- Stroke: BackgroundDocument10 pagesStroke: Backgroundjhay-r reyesNo ratings yet
- Peer Reviewed Medical Papers Submitted To Various Medical Journals, Evidencing A Multitude of Adverse Events in Covid-19 Vaccine RecipientsDocument77 pagesPeer Reviewed Medical Papers Submitted To Various Medical Journals, Evidencing A Multitude of Adverse Events in Covid-19 Vaccine RecipientsKraft DinnerNo ratings yet
- Controversies in Venous Thromboembolism - To Treat or Not To Treat Superficial Vein ThrombosisDocument8 pagesControversies in Venous Thromboembolism - To Treat or Not To Treat Superficial Vein ThrombosisNestor DuránNo ratings yet
- Anticoagulants 161120143945Document29 pagesAnticoagulants 161120143945Roshan SahuNo ratings yet
- Stroke 1Document43 pagesStroke 1n&t3000No ratings yet
- BJH 12107Document12 pagesBJH 12107Bernard NazaraNo ratings yet
- A Case of Acute Ischemic Stroke With Left HemiparesisDocument18 pagesA Case of Acute Ischemic Stroke With Left HemiparesisSafoora RafeeqNo ratings yet
- Venous Supply of Head, Neck and FaceDocument67 pagesVenous Supply of Head, Neck and FaceAlisha AranhaNo ratings yet
- D'Dimer, Fibrinogen Dan IL6 PAD CovidDocument8 pagesD'Dimer, Fibrinogen Dan IL6 PAD CovidWartimah imahNo ratings yet
- Warfarin therapy monitoring and managementDocument1 pageWarfarin therapy monitoring and managementmtbartNo ratings yet
- ECP device instruction manualDocument28 pagesECP device instruction manualBryanJermyHendrikNo ratings yet
- Ankle Brachial Index PDFDocument8 pagesAnkle Brachial Index PDFIncredibleNo ratings yet
- Frequently Prescribed DrugsDocument47 pagesFrequently Prescribed DrugsMahogony ScottNo ratings yet
- Hemodynamic Disorders: BY Dr. Birhane H (MD)Document88 pagesHemodynamic Disorders: BY Dr. Birhane H (MD)Biruck BirhanuNo ratings yet
- Approach To Debridement in Necrotizing FasciitisDocument6 pagesApproach To Debridement in Necrotizing FasciitisdenmasasinggihNo ratings yet
- Newer Oral Anticoagulant: DR Shivaom Chaurasia Resident Internal MedicineDocument57 pagesNewer Oral Anticoagulant: DR Shivaom Chaurasia Resident Internal MedicineMuhammad Reza FirdausNo ratings yet
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (15)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (5)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- The Tennis Partner: A Doctor's Story of Friendship and LossFrom EverandThe Tennis Partner: A Doctor's Story of Friendship and LossRating: 4.5 out of 5 stars4.5/5 (4)