Professional Documents
Culture Documents
Chemical Burn 2
Uploaded by
Yeni PuspitasariOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chemical Burn 2
Uploaded by
Yeni PuspitasariCopyright:
Available Formats
[Downloaded free from http://www.saudiendodj.com on Tuesday, February 23, 2021, IP: 110.138.197.
239]
Case Report
Chemical burn from direct application of aspirin onto a
painful tooth
Hussam Alfawaz
Department of Restorative Dental Sciences, College of Dentistry, King Saud University, Riyadh, Kingdom of Saudi Arabia
Abstract Aspirin is one of the most effective oral analgesic agents available worldwide without prescription. Aspirin
tablets can be directly placed on the painful tooth and adjunct mucosa to relieve pain and avoid dental visits.
However, aspirin is acidic in nature and its protein coagulation effects can cause severe chemical burns to the
surrounding mucosa when placed directly. Here, we describe a rare case of chemical burn caused by the direct
placement of an aspirin tablet on a painful tooth. A 55‑year‑old healthy African female presented to the clinic
with a history of pain in the right maxillary region. The patient stated that she had placed aspirin locally to
relieve her toothache for a few days. On intraoral examination, a grayish‑white fibrin‑coated ulcer was observed
on the buccal mucosa near the painful tooth, extending to the upper and lower buccal vestibules, up to the
premolar area. The source of pain was resolved by root canal treatment of #17, and the patient was advised
to discontinue the direct application of aspirin to oral tissues. Two weeks later, the lesion had healed entirely
without scarring. This case highlights the differences in the degree of clinical presentation of the lesion and the
importance of considering the injudicious use of aspirin as a potential cause of white lesions in the oral cavity.
Keywords: Aspirin, aspirin burn, chemical burn, root canal treatment, traumatic ulcer, white lesions
Address for correspondence: Dr. Hussam Alfawaz, Department of Restorative Dental Sciences, College of Dentistry, King Saud University, P.O. Box 60169,
Riyadh 11545, Kingdom of Saudi Arabia.
E‑mail: halfawaz1@ksu.edu.sa
Submission: 05-02-19 Revision: 17-02-19 Acceptance: 23-02-19 Web Publication: 27-12-19
INTRODUCTION headache, and in some cases, the tooth becomes sensitive
to percussion and biting.[3,4] Self‑medication with analgesics
A traumatic ulcer of the oral cavity is defined as a lesion for toothaches has been well‑documented.[5,6] Patients
resulting from a physical, thermal, or chemical burn.[1,2] often apply crushed analgesic tablets directly inside the
Topical application of drugs or chemicals inside the oral mouth and on the teeth to relieve toothache before seeking
cavity is the most common cause of traumatic ulcers. In professional help from dentists.[7‑9] However, this practice
chemical burns, an extensive, white, fibrin‑coated ulcer can cause mucosal necrosis, erosion, and infection.[1]
can be seen on the buccal mucosa, along with erythema of There are few case reports in the literature describing
the surrounding tissues, including the papillary, marginal, chemical oral burns caused by self‑medication for oral
and attached gingiva, with alveolar mucosal involvement. health conditions.[10] This report presents a case of acute
Patients experience severe painful mucosa, fever, and periapical abscess resulting from application of crushed
Access this article online This is an open access journal, and articles are distributed under the terms of the Creative
Commons Attribution‑NonCommercial‑ShareAlike 4.0 License, which allows others to
Quick Response Code:
Website: remix, tweak, and build upon the work non‑commercially, as long as appropriate credit
is given and the new creations are licensed under the identical terms.
www.saudiendodj.com
For reprints contact: reprints@medknow.com
DOI:
10.4103/sej.sej_24_19 How to cite this article: Alfawaz H. Chemical burn from direct application
of aspirin onto a painful tooth. Saudi Endod J 2020;10:65-8.
© 2019 Saudi Endodontic Journal | Published by Wolters Kluwer ‑ Medknow 65
[Downloaded free from http://www.saudiendodj.com on Tuesday, February 23, 2021, IP: 110.138.197.239]
Alfawaz: Chemical burn from the Aspirin
aspirin onto a painful tooth, highlighting the consequences patient received instructions regarding the proper use of
of aspirin misuse. medicines and their effects when misused; she was also
advised to discontinue direct application of aspirin to
CASE REPORT oral tissues; instead, intraoral intake of anti‑inflammatory
drugs was prescribed to relieve the pain. Furthermore, oral
A 55‑year‑old African female presented to the dental clinic hygiene instructions were reinforced.
with a history of pain and burning sensation in the right
maxillary region over the previous week. She reported no Two weeks later, at her recall visit, the RCT was
history of unhealthy habits, such as tobacco consumption, completed [Figure 3c]. The lesion had completely and
or any chronic medical illness. Her vital signs, blood pressure, uneventfully healed without scarring, and the patient
blood sugar level, and lymph nodes were unremarkable. was asymptomatic [Figure 3a and b]. The timeline from
However, she reported placing aspirin near a painful tooth patient presentation to the outcome is summarized in
and around the buccal vestibule for 2 consecutive days Figure 4.
to alleviate toothache. Intraoral examination revealed an
extensive, white, fibrin‑coated ulcer in the right buccal DISCUSSION
mucosa, as well as erythema of the surrounding tissues,
including the papillary, marginal, and attached gingiva, Aspirin‑induced chemical injury is rare; this case highlights
with alveolar mucosal involvement [Figure 1a and b]. The an oral soft‑tissue burn caused by the topical use of aspirin
lesion was ill‑defined with diffuse irregular boundaries; to relieve pain. In the literature, oral chemical burns with
it extended to the upper and lower buccal vestibules up various chemicals – cleansing agents, remedies, disinfectants,
to the premolar area. With gentle traction, the surface acids or bases, and cosmetics – were described only as case
slough peeled from the denuded connective tissue, thereby reports, and most of them occurred accidentally.[11] There is
exposing erythematous areas in the affected region; these a lack of information on the epidemiology of oral chemical
were tender on palpation [Figure 2a]. The maxillary burns in the literature.
right second molar (#17) was sensitive on percussion
and showed no response to thermal and electrical pulp Patients with a chemical burn usually experience acute
tests; all other tested teeth showed normal responses. severe throbbing pain, accompanied by fever, malaise,
A periapical radiograph of #17 showed substantial, deep headache, and occasionally, a systemic infection. These
decay approaching the pulp chamber, as well as widening patients did not seek professional dental care from fear of
of the periodontal ligament space [Figure 2b]. Plaque visiting dentists, financial difficulties, or a lack of available
control by the patient was inadequate. Considering the dental care in the area.[12] Therefore, these patients adopt
patient’s history and clinical findings, the lesion was self‑medication with analgesics both orally and topically
diagnosed as an aspirin burn; tooth #17 was diagnosed and visit a dental clinic only if they experience acute
as showing a necrotic pulp and acute periapical abscess. unbearable pain. Pain is the leading reason for visiting
A treatment plan was discussed with the patient, and her dental clinics among patients with lower socioeconomic
written consent was obtained. The treatment included root status, which may have been the case in this patient.[9,13]
canal treatment (RCT) for #17, which was initiated during Topical application of chemicals and drugs in the oral
the first visit with proper cleaning and shaping of the root
canal system and filling with intracanal medicament. The
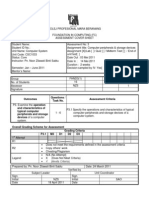
a b
a b Figure 2: (a) Intraoral photograph of the lesion at the first visit showing
Figure 1: (a) Intraoral photograph of the lesion at the first visit, extensive epithelial necrosis surrounded by erythema of the buccal
showing extensive white epithelial necrosis of the right buccal mucosa. mucosa and vestibule. (b) Preoperative periapical radiograph of #17
(b) Intraoral photograph of the lesion at the first visit to the clinic, showing extensive decay and widening of the periodontal ligament
showing the area of #17 space
66 Saudi Endodontic Journal | Volume 10 | Issue 1 | January-April 2020
[Downloaded free from http://www.saudiendodj.com on Tuesday, February 23, 2021, IP: 110.138.197.239]
Alfawaz: Chemical burn from the Aspirin
b c
Figure 3: (a) Intraoral photograph after 2 weeks in the area of #17.
(b) Erythema of the buccal mucosa and vestibule. (c) Tooth #17 after
complete root canal treatment
cavity by patients or dentists is the primary reason for
chemical burns.[14]
Aspirin (acetylsalicylic acid) is one of the oldest, cheapest,
and most effective analgesic agents available worldwide
without prescription. It is widely taken orally, with
50–120 billion tablets consumed each year for analgesia. It
is also applied as a topical cream, especially to relieve joint
and muscle pain. Occasional direct application of crushed
nonsteroidal anti‑inflammatory drug or aspirin tablets
on the tooth and buccal mucosa to relieve pain has been
reported to result in local tissue injury.[15] Aspirin, which
is acidic and a proton donor, causes epithelial necrosis,
erosion, and chemical burn through its protein coagulation
effects.[16] Coagulation necrosis occurs when tissue loses Figure 4: Timeline summarizing the patient information, clinical
blood supply, leading to cell death, but the cellular structure findings, investigations, diagnosis, therapeutic intervention, and
follow‑up
remains intact, even after several days of cell death.
Microscopically, the cells show intact outlines but without
history taking during the patient interview is essential since
nuclei.[17] Shedding of the necrosed epithelium occurs after
incorrect diagnosis in such cases may lead to unnecessary
several days of cell death.[18] Aspirin burns cause severe
gingival and mucosal erosion, with diffuse white sloughing investigational procedures that cause inconvenience to
of the mucosa throughout the affected area.[14] The degree the patient and increase the cost of treatment. Most
of damage varies depending on the duration of exposure, chemical burns with mild‑to‑moderate tissue damage will
the extent of penetration, and the amount, concentration, heal spontaneously.[14] Full‑mouth scaling and good oral
pH, and physical form of the agent.[16] In the present case, hygiene habits such as rinsing mouth with warm saline
to relieve the tooth pain, the patient placed aspirin directly water can facilitate ulcer healing within 1–2 weeks without
in the mouth. In the initial stages of the burn, the soft tissue any scarring.
is usually friable with a burning sensation and resembles an
aphthous ulcer.[19] Without knowledge of the consequences, In this case, the source of pain was treated by RCT of #17,
the patient continued applying crushed aspirin, resulting in which was completely cleaned and shaped and medicated
coagulation necrosis of the oral tissues.[18] with calcium hydroxide (Ca (OH) 2) in the first visit to
decrease the number of viable bacteria in the root canal
Management of aspirin burn requires identification and system till the next appointment. Ca (OH) 2 has antimicrobial
removal of the offending agent that caused the burn, as activity due to its high pH and the release of hydroxyl
well as proper treatment for the source of pain. Good ions, which cause destruction of the bacterial cytoplasmic
Saudi Endodontic Journal | Volume 10 | Issue 1 | January-April 2020 67
[Downloaded free from http://www.saudiendodj.com on Tuesday, February 23, 2021, IP: 110.138.197.239]
Alfawaz: Chemical burn from the Aspirin
membrane, denaturation of proteins, or destruction of the 2016;2016:7278925.
3. Matthews DC, Sutherland S, Basrani B. Emergency management of
DNA.[20] Systemic antibiotic treatment is not indicated for
acute apical abscesses in the permanent dentition: A systematic review
acute apical abscess because the disease source was treated of the literature. J Can Dent Assoc 2003;69:660.
mechanically by RCT through cleaning and shaping of the 4. Siqueira JF Jr., Rôças IN. Microbiology and treatment of acute apical
canal system. Antibiotic prescription is indicated in acute abscesses. Clin Microbiol Rev 2013;26:255‑73.
5. Agbor MA, Azodo CC. Self medication for oral health problems in
apical abscess when there is systemic manifestation of Cameroon. Int Dent J 2011;61:204‑9.
the infection and/or diffuse swelling noted extraorally.[3,21] 6. Jain A, Bhaskar DJ, Gupta D, Agali C, Yadav P, Khurana R, et al. Practice
of self‑medication for dental problems in Uttar Pradesh, India. Oral
CONCLUSION Health Prev Dent 2016;14:5‑11.
7. Furst IM, Ersil P, Caminiti M. A rare complication of tooth
abscess – Ludwig’s angina and mediastinitis. J Can Dent Assoc
Although chemical burns and ulcers in the oral cavity are
2001;67:324‑7.
common, few reports of aspirin burns have been documented. 8. Stoller EP, Gilbert GH, Pyle MA, Duncan RP. Coping with tooth pain:
Here, we highlighted the differences in the degree of clinical A qualitative study of lay management strategies and professional
presentation of the lesion and the importance of considering consultation. Spec Care Dentist 2001;21:208‑15.
9. Cohen LA, Bonito AJ, Akin DR, Manski RJ, Macek MD, Edwards RR,
the injudicious use of aspirin as a potential cause of ulceration et al. Toothache pain: Behavioral impact and self‑care strategies. Spec
in the oral cavity. Comprehensive patient education regarding Care Dentist 2009;29:85‑95.
the effect of medication misuse is urgently required, as is 10. Dellinger TM, Livingston HM. Aspirin burn of the oral cavity. Ann
reiteration of the importance of visiting a dentist every Pharmacother 1998;32:1107.
11. Nehrlich J, Klöcking HP, Hentschel H, Lupp A. Oral chemical burns
6 months for a checkup. These assessments can help avoid reported to the poisons information centre in Erfurt, Germany, from
tooth loss while ensuring optimal oral health and enhancing 1997 to 2014. J Burn Care Res 2017;38:e913‑22.
the quality of life. 12. Cohen LA, Harris SL, Bonito AJ, Manski RJ, Macek MD, Edwards RR,
et al. Coping with toothache pain: A qualitative study of low‑income
persons and minorities. J Public Health Dent 2007;67:28‑35.
Declaration of patient consent 13. Macfarlane TV, Blinkhorn AS, Davies RM, Kincey J, Worthington HV.
The authors certify that they have obtained all appropriate Factors associated with health care seeking behaviour for orofacial pain
patient consent forms. In the form the patient(s) has/have in the general population. Community Dent Health 2003;20:20‑6.
given his/her/their consent for his/her/their images and 14. Rawal SY, Claman LJ, Kalmar JR, Tatakis DN. Traumatic lesions of
the gingiva: A case series. J Periodontol 2004;75:762‑9.
other clinical information to be reported in the journal. 15. Rossi LA, Braga EC, Barruffini RC, Carvalho EC. Childhood burn
The patients understand that their names and initials will injuries: Circumstances of occurrences and their prevention in Ribeirão
not be published and due efforts will be made to conceal Preto, Brazil. Burns 1998;24:416‑9.
16. Mamede RC, de Mello Filho FV. Ingestion of caustic substances and
their identity, but anonymity cannot be guaranteed. its complications. Sao Paulo Med J 2001;119:10‑5.
17. Adigun R, Bhimji SS. Necrosis, Cell (Liquefactive, Coagulative, Caseous,
Financial support and sponsorship Fat, Fibrinoid, and Gangrenous). In: StatPearls. Treasure Island (FL):
Nil. StatPearls Publishing; January, 2018. Available from: https://www.ncbi.
nlm.nih.gov/books/NBK430935/. [Last updated on 2018 Oct 27].
Conflicts of interest 18. Azodo C, Orhue V. Chemical oral burn cum erosive gingival lesion arising
from self‑medication for toothache. SRM J Res Dent Sci 2018;9:40.
There are no conflicts of interest. 19. Ramaling am K, Abdalla KA. Traumatic chemical oral
ulceration – Aspirin burn – A case report from Libya. CIBTech J
REFERENCES Surg 2016;5:1‑3.
20. Pacios MG, Lagarrigue G, Nieva N, López ME. Effect of calcium
1. Gani BA, Nasution AI, Nazaruddin N, Sartika L, Alam RK. Potential hydroxide pastes and vehicles on root canal dentin microhardness.
of Jatropha multifida sap against traumatic ulcer. Dent J (Majalah Saudi Endod J 2014;4:53.
Kedokteran Gigi) 2015;48:119‑25. 21. Cope A, Francis N, Wood F, Mann MK, Chestnutt IG. Systemic
2. Mortazavi H, Safi Y, Baharvand M, Rahmani S. Diagnostic features of antibiotics for symptomatic apical periodontitis and acute apical abscess
common oral ulcerative lesions: An updated decision tree. Int J Dent in adults. Cochrane Database Syst Rev 2014;26:CD010136.
68 Saudi Endodontic Journal | Volume 10 | Issue 1 | January-April 2020
You might also like
- Athletic KnitDocument31 pagesAthletic KnitNish A0% (1)
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Aspirin BurnDocument4 pagesAspirin BurnNabila AzzahraNo ratings yet
- Aspergillosis Induced Osteomyelitis Involving The.125Document4 pagesAspergillosis Induced Osteomyelitis Involving The.125Andreea CiorneaNo ratings yet
- Oral MedicineDocument4 pagesOral MedicineRizki Dwi LestariNo ratings yet
- Allergic Contact Stomatitis From Composite Restoration: Acta Scientific Dental Sciences (Issn: 2581-4893)Document4 pagesAllergic Contact Stomatitis From Composite Restoration: Acta Scientific Dental Sciences (Issn: 2581-4893)Tharisa YosriNo ratings yet
- 1 PBDocument4 pages1 PBbregedek makanbanggamingNo ratings yet
- Ramsay Hunt Syndrome With Oral Findings - A Rare Case - CASE REPORT KEDUA BAGUSDocument7 pagesRamsay Hunt Syndrome With Oral Findings - A Rare Case - CASE REPORT KEDUA BAGUSfoto pasienNo ratings yet
- Extraoral Cutaneous Sinus Tracts of Dental OriginDocument4 pagesExtraoral Cutaneous Sinus Tracts of Dental OriginAyu SawitriNo ratings yet
- Odontogenic Fungal Maxillary Sinusitis A Case Report of A Displaced Dental Foreign BodyDocument5 pagesOdontogenic Fungal Maxillary Sinusitis A Case Report of A Displaced Dental Foreign BodyAngelia PratiwiNo ratings yet
- Lichen Planus of Lip - Report of A Rare Case With Review of LiteratureDocument7 pagesLichen Planus of Lip - Report of A Rare Case With Review of LiteratureDharmapadmi KasilaniNo ratings yet
- Chem Ical BurnDocument3 pagesChem Ical BurnvasabakaNo ratings yet
- Canina Fossa Abscess and Treatment: Muhammad H. ChandhaDocument4 pagesCanina Fossa Abscess and Treatment: Muhammad H. ChandhaasadNo ratings yet
- Jurnal Mursicatio BucarumDocument4 pagesJurnal Mursicatio BucarumhairiahdjNo ratings yet
- Ccide 14 183Document7 pagesCcide 14 183DANNU LAREZHANo ratings yet
- Oral Lichen Planus in An 8-Year-Old Child: A Case Report With A Brief Literature ReviewDocument9 pagesOral Lichen Planus in An 8-Year-Old Child: A Case Report With A Brief Literature ReviewFebri YolandaNo ratings yet
- Jurnal Gingivitis Vivian 190631174Document5 pagesJurnal Gingivitis Vivian 190631174VivianNo ratings yet
- Over-The-Counter Oral Hygiene Products Misuse: A Case ReportDocument4 pagesOver-The-Counter Oral Hygiene Products Misuse: A Case ReportDr Sharique AliNo ratings yet
- Chemical Burn 4Document2 pagesChemical Burn 4Yeni PuspitasariNo ratings yet
- Angular Cheilitis - An Updated Overview of The Etiology, Diagnosis, and ManagementDocument7 pagesAngular Cheilitis - An Updated Overview of The Etiology, Diagnosis, and ManagementVicky RahmaniahNo ratings yet
- Management of Submandibular Abscess in Pregnant Woman: A Case ReportDocument4 pagesManagement of Submandibular Abscess in Pregnant Woman: A Case ReportmilantariNo ratings yet
- Podj 4 PDFDocument3 pagesPodj 4 PDFNur Sita DewiNo ratings yet
- Odontogenic Submandibular Space Infection Complicated by Temporal Space AbscessDocument5 pagesOdontogenic Submandibular Space Infection Complicated by Temporal Space AbscessAyu SawitriNo ratings yet
- 2014 Oral Mucosal Ulceration Caused by The TopicalDocument5 pages2014 Oral Mucosal Ulceration Caused by The TopicalAnjungAdelNo ratings yet
- Jurnal 1Document4 pagesJurnal 1restuasNo ratings yet
- DE1 CR Baksh 2 5 36CDocument4 pagesDE1 CR Baksh 2 5 36CAyu SawitriNo ratings yet
- Angular Cheilitis An Updated Overview ofDocument6 pagesAngular Cheilitis An Updated Overview ofjuliaoliveiira15No ratings yet
- YYY Benzoin MechDocument3 pagesYYY Benzoin MechBaronKornNo ratings yet
- Oral Chemical Burns Caused by Topical Application of Policresulen A Case ReportDocument4 pagesOral Chemical Burns Caused by Topical Application of Policresulen A Case Reportrahmania alikhlashNo ratings yet
- Jurnal Terapi Bedah 3Document3 pagesJurnal Terapi Bedah 3Mutiara FauziahNo ratings yet
- Sept2020 ToothDocument3 pagesSept2020 ToothTrina ViskhawatNo ratings yet
- Stomatitis Venenata: A Rarity: Case ReportDocument2 pagesStomatitis Venenata: A Rarity: Case ReportJoel Nathaniel Richard JosephNo ratings yet
- Apical Periodontitis After Intense BruxismDocument6 pagesApical Periodontitis After Intense BruxismdevitakomalaNo ratings yet
- Paper Carillas DirectasDocument11 pagesPaper Carillas DirectasAnahis IbacetaNo ratings yet
- Drug Induced Erythema Multiforme: Two Case Series With Review of LiteratureDocument5 pagesDrug Induced Erythema Multiforme: Two Case Series With Review of LiteraturefersaNo ratings yet
- Epulis Fissuratum: Consequence of Ill-Fitting ProsthesisDocument2 pagesEpulis Fissuratum: Consequence of Ill-Fitting ProsthesisMichelle VelezNo ratings yet
- Eaat 04 I 1 P 2Document5 pagesEaat 04 I 1 P 2Dr.O.R.GANESAMURTHINo ratings yet
- ArsenicDocument4 pagesArsenicAnonymous SZqzD30YNo ratings yet
- Allergicstomatitis 2012Document6 pagesAllergicstomatitis 2012Agustine Hanafi PutriNo ratings yet
- NtionvioletDocument10 pagesNtionvioletGeorgi GugicevNo ratings yet
- 01 Dentin HypersensitivityDocument8 pages01 Dentin Hypersensitivityiraqi iraqiNo ratings yet
- Chronic Suppurative Osteomyelitis of The Mandible CaseDocument4 pagesChronic Suppurative Osteomyelitis of The Mandible Caseporsche_cruiseNo ratings yet
- Traumatic Chemical Oral Ulceration A Case Report ADocument5 pagesTraumatic Chemical Oral Ulceration A Case Report Afebrina zwestianaNo ratings yet
- Orthodontic Treatment of A Severe Combined Anterior and Posterior Open Bite Case, Involving AnkylosisDocument8 pagesOrthodontic Treatment of A Severe Combined Anterior and Posterior Open Bite Case, Involving Ankylosisgifar ihsanNo ratings yet
- Successful Endodontic Management of Endo Perio Lesions With Different Treatment Modalities: Case SeriesDocument5 pagesSuccessful Endodontic Management of Endo Perio Lesions With Different Treatment Modalities: Case Seriesclara.kristantiNo ratings yet
- Post Extraction Lingual Mucosal Ulceration With Bone NecrosisDocument4 pagesPost Extraction Lingual Mucosal Ulceration With Bone Necrosisandrianiputri916No ratings yet
- Pain and FL Are-Up After Endodontic Treatment Procedures: ReviewDocument6 pagesPain and FL Are-Up After Endodontic Treatment Procedures: ReviewGin Gin GustianaNo ratings yet
- Al-Sharani (2019), THE EFFECT OF NANOSILVER AND CHLORHEXIDINE MOUTHWASH ON ANAEROBIC PERIODONTAL PATHOGENS COUNTSDocument6 pagesAl-Sharani (2019), THE EFFECT OF NANOSILVER AND CHLORHEXIDINE MOUTHWASH ON ANAEROBIC PERIODONTAL PATHOGENS COUNTSPhuong ThaoNo ratings yet
- Jurnal IntiDocument5 pagesJurnal IntiFajar RamadhanNo ratings yet
- Odontogenic Sinusitis: A Review of The Current LiteratureDocument5 pagesOdontogenic Sinusitis: A Review of The Current LiteraturefransAPNo ratings yet
- Oral Candidiasis: A Short Review and A Case Report: December 2018Document5 pagesOral Candidiasis: A Short Review and A Case Report: December 2018RAfii KerenNo ratings yet
- Actinomycosis Ostemyelitis PDFDocument7 pagesActinomycosis Ostemyelitis PDFHusni MubarakNo ratings yet
- Erythema Multiforme: A Case Series and Review of Literature: November 2018Document8 pagesErythema Multiforme: A Case Series and Review of Literature: November 2018Nurlina NurdinNo ratings yet
- Oral Medicine and Pathology Quiz - Case 9: Continuing Medical Education Συνεχιζομενη Ιατρικη ΕκπαιδευσηDocument1 pageOral Medicine and Pathology Quiz - Case 9: Continuing Medical Education Συνεχιζομενη Ιατρικη ΕκπαιδευσηHeidy StefanieNo ratings yet
- Chronic Suppurative Osteomyelitis: A Case ReportDocument4 pagesChronic Suppurative Osteomyelitis: A Case ReportashariNo ratings yet
- ANUG in A HIV Seronegative Patient - A Case ReportDocument6 pagesANUG in A HIV Seronegative Patient - A Case ReportPringgo EfbiNo ratings yet
- Keywords:-Zot, Zop and ZoeDocument6 pagesKeywords:-Zot, Zop and ZoeInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 10 1111@ipd 12690Document7 pages10 1111@ipd 12690Tiara HapkaNo ratings yet
- DentHypotheses7267-3698345 101623Document4 pagesDentHypotheses7267-3698345 101623Aliyah SaraswatiNo ratings yet
- Successful Treatment of Herpes Simplex-Associated Erythema Multiforme With A Combination of Acyclovir and PrednisoneDocument3 pagesSuccessful Treatment of Herpes Simplex-Associated Erythema Multiforme With A Combination of Acyclovir and PrednisoneannisafebriezaNo ratings yet
- Gingival Abscess Case ReportDocument4 pagesGingival Abscess Case ReportKrishan GuliaNo ratings yet
- Knowledge Risk Perception and Attitudes of DentistDocument11 pagesKnowledge Risk Perception and Attitudes of DentistYeni PuspitasariNo ratings yet
- Case Report Benign Mucosal Membrane Pemphigoid As A Differential Diagnosis of Necrotizing Periodontal DiseaseDocument4 pagesCase Report Benign Mucosal Membrane Pemphigoid As A Differential Diagnosis of Necrotizing Periodontal DiseaseYeni PuspitasariNo ratings yet
- Pancytopenia: A Clinico Hematological Study: Gayathri B N, Kadam Satyanarayan RaoDocument6 pagesPancytopenia: A Clinico Hematological Study: Gayathri B N, Kadam Satyanarayan RaoYeni PuspitasariNo ratings yet
- Oral Manifestations in Patients With Hypogammaglobulinemia: June 2012Document7 pagesOral Manifestations in Patients With Hypogammaglobulinemia: June 2012Yeni PuspitasariNo ratings yet
- Clinical, Immunological, and Molecular Findings in 57 Patients With Severe Combined Immunodeficiency (SCID) From IndiaDocument16 pagesClinical, Immunological, and Molecular Findings in 57 Patients With Severe Combined Immunodeficiency (SCID) From IndiaYeni PuspitasariNo ratings yet
- Case Report Benign Mucosal Membrane Pemphigoid As A Differential Diagnosis of Necrotizing Periodontal DiseaseDocument4 pagesCase Report Benign Mucosal Membrane Pemphigoid As A Differential Diagnosis of Necrotizing Periodontal DiseaseYeni PuspitasariNo ratings yet
- Smoker'S Perception To Message Public Service Announcements About Danger of SmokingDocument12 pagesSmoker'S Perception To Message Public Service Announcements About Danger of SmokingYeni PuspitasariNo ratings yet
- Scid:: A Pediatric EmergencyDocument2 pagesScid:: A Pediatric EmergencyYeni PuspitasariNo ratings yet
- Clinical: Contact Allergy To Cinnamon: Case ReportDocument4 pagesClinical: Contact Allergy To Cinnamon: Case ReportGrace Victoria OctavianusNo ratings yet
- 1 s2.0 S0190962214018714 MainDocument7 pages1 s2.0 S0190962214018714 MainYeni PuspitasariNo ratings yet
- Autoimmunity Reviews: SciencedirectDocument10 pagesAutoimmunity Reviews: SciencedirectYeni PuspitasariNo ratings yet
- MMP 8Document5 pagesMMP 8Yeni PuspitasariNo ratings yet
- Vila 2020Document28 pagesVila 2020Anisa ArmadaniNo ratings yet
- LichenoidreactionDocument4 pagesLichenoidreactionYeni PuspitasariNo ratings yet
- PaperDocument7 pagesPaperAgya Nanda PrasetyaNo ratings yet
- Lichen Planus and Lichenoid Reactions of The Oral Mucosa: Bethanee J. SchlosserDocument17 pagesLichen Planus and Lichenoid Reactions of The Oral Mucosa: Bethanee J. SchlosserYeni PuspitasariNo ratings yet
- 536 914 1 SMDocument9 pages536 914 1 SMFitri Perdana PutriNo ratings yet
- Neonatal Thrush of Newborns Oral CandidiasisDocument3 pagesNeonatal Thrush of Newborns Oral CandidiasisYeni PuspitasariNo ratings yet
- LR 1Document4 pagesLR 1Yeni PuspitasariNo ratings yet
- Histological and Molecular Aspects of Oral Squamous Cell Carcinoma (Review)Document5 pagesHistological and Molecular Aspects of Oral Squamous Cell Carcinoma (Review)Yeni PuspitasariNo ratings yet
- Peripheral Giant Cell GranulomaDocument8 pagesPeripheral Giant Cell GranulomaTeiza NabilahNo ratings yet
- Prevalence of Oral Lichenoid Reactions in A Sample of Qazvin Population (2004)Document4 pagesPrevalence of Oral Lichenoid Reactions in A Sample of Qazvin Population (2004)Yeni PuspitasariNo ratings yet
- Current Aspects On Oral Squamous Cell Carcinoma: Anastasios K. MarkopoulosDocument5 pagesCurrent Aspects On Oral Squamous Cell Carcinoma: Anastasios K. MarkopoulosYeni PuspitasariNo ratings yet
- Chemokines in The Pathogenesis of Lichenoid TissueDocument6 pagesChemokines in The Pathogenesis of Lichenoid TissueYeni PuspitasariNo ratings yet
- Keywords: Peripheral Giant Cell Granuloma/giant Cell Epulis, Jaw, ReactiveDocument4 pagesKeywords: Peripheral Giant Cell Granuloma/giant Cell Epulis, Jaw, ReactiveYeni PuspitasariNo ratings yet
- PaperDocument7 pagesPaperAgya Nanda PrasetyaNo ratings yet
- Accepted Manuscript: 10.1016/j.oooo.2017.02.007Document22 pagesAccepted Manuscript: 10.1016/j.oooo.2017.02.007Fajar RamadhanNo ratings yet
- Dento-Maxillofacial Abnormalities Caused by Radiotherapy and ChemotherapyDocument6 pagesDento-Maxillofacial Abnormalities Caused by Radiotherapy and ChemotherapyYeni PuspitasariNo ratings yet
- Pato LRDocument5 pagesPato LRYeni PuspitasariNo ratings yet
- XT 125Document54 pagesXT 125ToniNo ratings yet
- S1-TITAN Overview BrochureDocument8 pagesS1-TITAN Overview BrochureصصNo ratings yet
- Muscle Building MythsDocument5 pagesMuscle Building MythsKarolNo ratings yet
- 1classic Greek SaladDocument6 pages1classic Greek SaladEzekiel GumayagayNo ratings yet
- Assisted Reproductive Technology945Document35 pagesAssisted Reproductive Technology945Praluki HerliawanNo ratings yet
- The Rime of The Ancient Mariner (Text of 1834) by - Poetry FoundationDocument19 pagesThe Rime of The Ancient Mariner (Text of 1834) by - Poetry FoundationNeil RudraNo ratings yet
- The Organization of PericentroDocument33 pagesThe Organization of PericentroTunggul AmetungNo ratings yet
- Physics Tadka InstituteDocument15 pagesPhysics Tadka InstituteTathagata BhattacharjyaNo ratings yet
- Unit 4Document2 pagesUnit 4Sweta YadavNo ratings yet
- Ereneta ReviewerDocument32 pagesEreneta ReviewerAleezah Gertrude RaymundoNo ratings yet
- A Detailed Lesson Plan - The Fundamental Law of ProportionDocument10 pagesA Detailed Lesson Plan - The Fundamental Law of ProportionPrincess De LeonNo ratings yet
- Presentation Airbnb ProfileDocument14 pagesPresentation Airbnb ProfileGuillermo VillacrésNo ratings yet
- Pau Inglés-7Document2 pagesPau Inglés-7AlfodNo ratings yet
- The Health Anxiety Inventory Development and Validation of Scales For The Measurement of Health Anxiety and HypochondriasisDocument11 pagesThe Health Anxiety Inventory Development and Validation of Scales For The Measurement of Health Anxiety and HypochondriasisJan LAWNo ratings yet
- The Invisible Museum: History and Memory of Morocco, Jewish Life in FezDocument1 pageThe Invisible Museum: History and Memory of Morocco, Jewish Life in FezmagnesmuseumNo ratings yet
- Business Emails - Style and StructureDocument4 pagesBusiness Emails - Style and StructureFall Eljed100% (1)
- 3 Pseudoscience and FinanceDocument11 pages3 Pseudoscience and Financemacarthur1980No ratings yet
- The City of GodDocument16 pagesThe City of GodJei Em MonteflorNo ratings yet
- NetEco Commissioning Guide (V200R003C01 - 01) (PDF) - enDocument116 pagesNetEco Commissioning Guide (V200R003C01 - 01) (PDF) - enabdo elmozogyNo ratings yet
- Peace Corps Samoa Medical Assistant Office of The Public Service of SamoaDocument10 pagesPeace Corps Samoa Medical Assistant Office of The Public Service of SamoaAccessible Journal Media: Peace Corps DocumentsNo ratings yet
- CTY1 Assessments Unit 6 Review Test 1Document5 pagesCTY1 Assessments Unit 6 Review Test 1'Shanned Gonzalez Manzu'No ratings yet
- Jsu Matematik SR Tahun 1Document24 pagesJsu Matematik SR Tahun 1Nurul NazierahNo ratings yet
- Poetry Analysis The HighwaymanDocument7 pagesPoetry Analysis The Highwaymanapi-257262131No ratings yet
- Evolut Pro Mini Product Brochure PDFDocument8 pagesEvolut Pro Mini Product Brochure PDFBalázs PalcsikNo ratings yet
- Assignment 2 Format Baru 17042011Document8 pagesAssignment 2 Format Baru 17042011Noor Zilawati SabtuNo ratings yet
- VC++ Splitter Windows & DLLDocument41 pagesVC++ Splitter Windows & DLLsbalajisathyaNo ratings yet
- AgrippaDocument4 pagesAgrippaFloorkitNo ratings yet
- Spoken Word (Forever Song)Document2 pagesSpoken Word (Forever Song)regNo ratings yet
- CV - Cover LetterDocument2 pagesCV - Cover LetterMoutagaNo ratings yet