Professional Documents
Culture Documents
YYY Benzoin Mech
Uploaded by
BaronKornOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
YYY Benzoin Mech
Uploaded by
BaronKornCopyright:
Available Formats
I carried out a similar procedure in this instance.
The test ointments were
covered with gauze and then secured with a loosely applied roller bandage.
Within a short time the patient complained of burning at all the test areas. The
applications were of course removed at once, with the use of warm mineral oil.
Except for the fact that the dermatitis seemed more acute, nothing of note was
recorded.
To permit the subsidence of the dermatitis accentuated by the test ointments,
the patient was instructed to return in three days, having applied nothing to her
skin and having refrained from washing" during the interval.
On her return three areas of dermatitis were selected and bandaged with several
layers of sterile gauze so that on each area there was the product of a different
manufacturer. Within ten minutes burning was experienced at all the areas, and
on the removal of the gauze dressings the observation of a noticeable increase in
redness testified to the veracity of the patient's complaint.
Similar gauze patch tests were now applied to normal-appearing cutaneous
surfaces and left in place for forty-eight hours. No reaction was noted at the end
of this period at these sites.
I believe that accentuation of dermatitis as a result of sensitivity to gauze may
occur more often than is generally suspected, as no one had called my attention to it.
631 Jenkins Building (22).
COMPOUND BENZOIN TINCTURE IN TREATMENT OF VESICULOBULLOUS
LESIONS OF MUCOUS MEMBRANES
HENRY HARRIS PERLMAN, M.D.
PHILADELPHIA
It often happens that the dermatologist is concerned with vesiculobullous lesions
of the mucous membrane of the oral cavity that tax all his skill as a therapeutist.
Treatment with compound benzoin tincture has given excellent results in these
cases, and, as there are no references to it in recent dermatologic literature, I wish
to bring it to the attention of dermatologists.
Benzoin is one of the ancient drugs of pharmacy and has enjoyed its popularity
under a masquerade of many romantic names, among them Turlington's balsam,
friars' balsam, Wade's balsam, balsam de malthe, Jesuit's drops, St. Victor's
balsam, Persian balsam, Swedish balsam and Jerusalem balsam. It is official in the
United States Pharmacoepeia and the British Pharmacopeia under the title tinctura
benzoini composita. It is prepared by the maceration of a mixture of benzoin, aloe
in the form of a moderately coarse powder, storax and tolu balsam in strong
alcohol for three days. Then the mixture is filtered and enough alcohol added so
that the tincture contains 74 to 80 per cent by volume of alcohol. Because of this
strong alcoholic content the preparation is irritating to broken tissues. Downing
and Stoklosa 1 developed a nonirritating ointment in which the compound tincture
evaporated to the consistency of an extract is incorporated in a zinc oxide base.
The antiseptic effect of the tincture is probably dependent on the benzoic and
cinnamic acids contained in the benzoin and storax, two of the active ingredients
of the compound, while the strong alcoholic content of the pharmaceutic preparation
1. Downing, J. G., and Stoklosa, M. J.: Compound Tincture of Benzoin in
Ointments, Arch. Dermat. & Syph. 54:714 (Dec.) 1946.
Downloaded From: http://archderm.jamanetwork.com/ by a UQ Library User on 06/20/2015
possibly has some additional antiseptic and dehydrating effect on the edematous
tissue.
In the following report, the application of compound tincture of benzoin to the
oral lesions resulted in the elimination of pain and the improvement of the lesions
after the failure of many other indicated methods.
REPORT OF A CASE
L. C, 19 years of age, a college student, suffering from recurrent episodes of
blisters in her mouth, was referred to me in October 1947. In November 1945
gingival lesions involving her throat and buccal areas developed. The temperature
rose at night (101 to 103 F.) but receded in the morning. The gingival lesions,
which principally were gray vesicles, healed without scarring. But they spread
over the buccal surfaces, tongue and fauces. There was submaxillary adenitis.
Treatment consisted of the use of salicylates and sulfonamide drugs and the
intramuscular injection of 300,000 units of penicillin. The temperature became
normal in a week, and the patient was well in two weeks. All laboratory tests
(including the smear for Vincent's angina) had negative results. Alkaline mouth
washes and dyes had been used without effect.
Two months later there was another attack, which commenced with a small
ulcer, resembling aphthous stomatitis, under the upper lip. It spread rapidly,
involving the whole mouth, with vesicles and small bullae that changed into crusts,
especially on the vermilion border of the lip. There was edema of the lips and
mouth, conjunctivitis and photophobia. The condition responded well to large
intravenous injections of preparations containing the vitamin B complex. The
patient was ambulatory and became well in six weeks.
On about May 25, 1946, the patient acquired an ulcer under the upper lip which
spread rapidly until the tongue, cheeks, vermilion border and most of the oral
mucosa were involved. There was conjunctivitis, and the edema of the pharynx
and the oral mucosa was so severe that eating and swallowing became very difficult.
The condition did not respond to treatment with 300,000 units of penicillin and 15
grains (1 Gm.) of methenamine, the latter administered three times daily. The
patient had to be hospitalized. The temperature, blood picture and blood chemistry
were normal. The Wassermann reaction of the blood was negative. Treatment
consisted of intravenous injections of methenamine, 15 grains each, for three days,
and two whole blood transfusions. The patient was discharged in nine days in
good condition.
In April 1947 the patient experienced another attack similar to the preceding
one. Five doses of 15 grains of methenamine were given intravenously over a ten
day period. Simultaneously vaccinations with smallpox virus w-ere performed with¬
out their achieving a "take." The episode was aborted, and the patient remained
ambulatory.
On Oct. 17, 1947, vesicular lesions developed on the mucous membranes of the
upper and lower lips. They spread until the entire oral mucosa was involved.
The conjunctivas and the skin remained free of lesions. The vesicles ruptured and
formed crusts. The patient remained afebrile but was unable to take food by
mouth because of great pain. Even the sipping of milk through a tube was
very painful. There was no "take" to vaccination with smallpox virus. Intravenous
injections of methenamine were given as before. The mouth was given a cleansing
with a potassium permanganate solution ( 1:2,000) followed by a wiping of the
lesions with liquid petrolatum. No relief was obtained. Then full strength com¬
pound benzoin tincture was applied with a cotton applicator. There was almost
immediate relief from pain, and within a few hours there was a noticeable decrease
Downloaded From: http://archderm.jamanetwork.com/ by a UQ Library User on 06/20/2015
in edema of the lips. The patient was able to take food, and in a few days the
lesions in the mouth subsided. During those few days the patient kept applying
the compound benzoin tincture herself every few hours. There has been no
recurrence since that time.
I ha\ e used compound benzoin tincture with excellent results in treatment
of herpes simplex of the lips, aphthous stomatitis and lesions of so-called "trench
mouth" in infants and Vincent's infection. Although I have had no experience
with its use in treatment of oral lesions of pemphigus and epidermolysis bullosa
I think it would be of help. It has given relief of pain in a case of lingua
geographica in a 6 year old white boy.
SUMMARY AXD CONCIA SI0NS
A of erythema multiforme exudativum, characterized by recurrent episodes
case
of vesiculobullous lesions on the lips and oral mucosa, is reported. Topical therapy
consisting of the use of various alkaline mouth washes and dyes and local applica¬
tions of silver nitrate failed to improve the lesions of the lips and the oral mucosa.
The aforementioned vesiculobullous lesions promptly responded to topical
applications of compound benzoin tincture U. S. P.
Some of the commoner dermatologie entities affecting the mucous membranes of
the lips and mouth in which the topical application of the official compound
benzoin tincture has proved of value are listed.
1726 Pine Street. ;
LICHEN PLANUS HYPERTROPHICUS
Possiible Clue to Etiology
CHARLES C. DENNIE, M.D.
AND
FRANCIS P. COOMBS, M.D.
KANSAS CITY, MO.
A.H., a 58 year old married woman, was first seen by us on Nov. 4, 1947,
and diagnosis of lichen planus hypertrophicus of the anterolateral surface of the
a
left thigh was made. Pronounced varicose veins of both legs were found. The
lesions had first appeared one year previous to the patient's first visit. Leading
from the area was a moderately large varicose vein, tortuously running toward
the saphenous vein at the junction of the upper and the middle third of the thigh.
This varix had been present for some time previous to the appearance of the
lesions. Biopsy showed typical lichen planus hypertrophicus.
Microscopic observations were as follows : The keratin layer was thickened.
One follicle was widened, with decided keratotic plugging. Relative and absolute
hyperkeratosis, an increase in the stratum granulosum, acanthosis, slight liquefactive
degeneration of the basal cell layer and mild lymphocytic infiltration in the upper
portion of the cutis, with some histiocytosis around the keratinized follicle,
were seen.
The patient related that in 1940 she had had a patch of identical lesions on.
the anterior surface of the lower part of the left leg, also associated with a varicose
Downloaded From: http://archderm.jamanetwork.com/ by a UQ Library User on 06/20/2015
You might also like
- Vincent’s Angina, (Trench Mouth) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandVincent’s Angina, (Trench Mouth) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Treatment of the diseases of the eye, by means of prussic acid vapour, and other medicinal agentsFrom EverandTreatment of the diseases of the eye, by means of prussic acid vapour, and other medicinal agentsNo ratings yet
- Referat 1Document3 pagesReferat 1Tupicica GabrielNo ratings yet
- 2014 Oral Mucosal Ulceration Caused by The TopicalDocument5 pages2014 Oral Mucosal Ulceration Caused by The TopicalAnjungAdelNo ratings yet
- Erythema Multiforme: A Case Series and Review of Literature: November 2018Document8 pagesErythema Multiforme: A Case Series and Review of Literature: November 2018Nurlina NurdinNo ratings yet
- Use of A Mupirocin Clobetasol Proprionate Mixture in Severe Atopic Hand EczemaDocument2 pagesUse of A Mupirocin Clobetasol Proprionate Mixture in Severe Atopic Hand EczemaYoichiNo ratings yet
- THE Canadian Medical Association: Associate, Department of Dermatology, Vancouver General Hospital, Vancouver, B.CDocument5 pagesTHE Canadian Medical Association: Associate, Department of Dermatology, Vancouver General Hospital, Vancouver, B.CAndrew Surya Putra SccNo ratings yet
- 1 PBDocument4 pages1 PBbregedek makanbanggamingNo ratings yet
- Acute Parapharyngeal Abscess Secondary To Streptococcal MastoiditisDocument2 pagesAcute Parapharyngeal Abscess Secondary To Streptococcal Mastoiditiswawansiswadi01No ratings yet
- Chemical Burn 2Document4 pagesChemical Burn 2Yeni PuspitasariNo ratings yet
- Acad Dermatol Venereol - 2019 - Nowak - Rosacea Fulminans Coincidence of The Disease With Inflammatory Bowel DiseaseDocument2 pagesAcad Dermatol Venereol - 2019 - Nowak - Rosacea Fulminans Coincidence of The Disease With Inflammatory Bowel DiseasecamilabettiomatosNo ratings yet
- Aspirin BurnDocument4 pagesAspirin BurnNabila AzzahraNo ratings yet
- Eaat 04 I 1 P 2Document5 pagesEaat 04 I 1 P 2Dr.O.R.GANESAMURTHINo ratings yet
- Cjim 4 793Document4 pagesCjim 4 793Mega WulandariNo ratings yet
- Successful Treatment of Herpes Simplex-Associated Erythema Multiforme With A Combination of Acyclovir and PrednisoneDocument3 pagesSuccessful Treatment of Herpes Simplex-Associated Erythema Multiforme With A Combination of Acyclovir and PrednisoneannisafebriezaNo ratings yet
- Section Of: LaryngologyDocument8 pagesSection Of: LaryngologyIcusWulanNo ratings yet
- Management of Necrotizing Ulcerative Gingivitis in A Pregnant Patient - A Rare Case ReportDocument6 pagesManagement of Necrotizing Ulcerative Gingivitis in A Pregnant Patient - A Rare Case ReportAZWAN RAHMADHAN PUTRANo ratings yet
- Recurrent Acute SinusitisDocument3 pagesRecurrent Acute SinusitisMEDS easyNo ratings yet
- Treatment of Otomycosis Due To Aspergillus Niger With Tolnaftate PDFDocument3 pagesTreatment of Otomycosis Due To Aspergillus Niger With Tolnaftate PDFMei Risanti SiraitNo ratings yet
- The Peritonsillar Abscess Is A Fairly Common Sequel To Chronic Tonsillitis andDocument7 pagesThe Peritonsillar Abscess Is A Fairly Common Sequel To Chronic Tonsillitis andAyu Rahmi AMyNo ratings yet
- Sempervivum Tectorum: Other Names: Made FromDocument4 pagesSempervivum Tectorum: Other Names: Made FromDohn JoeNo ratings yet
- Allergic Contact Stomatitis: A Case Report and Review of LiteratureDocument5 pagesAllergic Contact Stomatitis: A Case Report and Review of LiteratureFajar RamadhanNo ratings yet
- Acute SinusitisDocument11 pagesAcute Sinusitisعبدالله فائز غلامNo ratings yet
- Jurnal SinusitisDocument25 pagesJurnal SinusitisDwi Ayu NovianaNo ratings yet
- Allergicstomatitis 2012Document6 pagesAllergicstomatitis 2012Agustine Hanafi PutriNo ratings yet
- Review Articles: Scientific SectionDocument4 pagesReview Articles: Scientific SectionAbdul Rahman MahafuddinNo ratings yet
- Chapter 34: Dermatologic Disorders Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionDocument8 pagesChapter 34: Dermatologic Disorders Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionHelen UgochukwuNo ratings yet
- Interappointment Flare-Up in Endodontics: A Case Report and An OverviewDocument4 pagesInterappointment Flare-Up in Endodontics: A Case Report and An OverviewAnonymous cTV8BbsCeNo ratings yet
- Oral MedicineDocument4 pagesOral MedicineRizki Dwi LestariNo ratings yet
- Pyostomatitis Vegetans. Report of Two Cases and Review of The LiteratureDocument8 pagesPyostomatitis Vegetans. Report of Two Cases and Review of The LiteratureBimalKrishnaNo ratings yet
- Behcets DisDocument3 pagesBehcets DisHany ElbarougyNo ratings yet
- 657-Article Text-1074-1-10-20221221Document3 pages657-Article Text-1074-1-10-20221221putraNo ratings yet
- Canina Fossa Abscess and Treatment: Muhammad H. ChandhaDocument4 pagesCanina Fossa Abscess and Treatment: Muhammad H. ChandhaasadNo ratings yet
- Chronic RhinosinusitisDocument8 pagesChronic RhinosinusitisYunardi Singgo100% (1)
- Ramsay Hunt Syndrome With Oral Findings - A Rare Case - CASE REPORT KEDUA BAGUSDocument7 pagesRamsay Hunt Syndrome With Oral Findings - A Rare Case - CASE REPORT KEDUA BAGUSfoto pasienNo ratings yet
- 1 s2.0 S2405469023001590 MainDocument3 pages1 s2.0 S2405469023001590 MainLeo TorresNo ratings yet
- Iaat 12 I 2 P 458Document5 pagesIaat 12 I 2 P 458Virma PutraNo ratings yet
- Flare Up in Endodontics: A Review: Tharangini Raveenthiraraja, Pradeep SoleteDocument3 pagesFlare Up in Endodontics: A Review: Tharangini Raveenthiraraja, Pradeep SoleteDarshilNo ratings yet
- Amir Ali Khan, Amanat Ali Shah, Tehmina Rehman, Abdullah: Original Article Open AccessDocument4 pagesAmir Ali Khan, Amanat Ali Shah, Tehmina Rehman, Abdullah: Original Article Open AccessdumpalacaNo ratings yet
- HTTP WWW - Sciencedirect.com Science Ob MImg& Imagekey B6WP1-4HGNP77-G-1& Cdi 6977& User 8187385& OrigDocument2 pagesHTTP WWW - Sciencedirect.com Science Ob MImg& Imagekey B6WP1-4HGNP77-G-1& Cdi 6977& User 8187385& OrigBimalKrishnaNo ratings yet
- 4.management of Aphthous Ulceration With Topical QuercetinDocument9 pages4.management of Aphthous Ulceration With Topical QuercetinCoste Iulia RoxanaNo ratings yet
- Treatment of Maxillary SinusitisDocument15 pagesTreatment of Maxillary SinusitisRabina PantaNo ratings yet
- Management of Herpes Labialis Triggered by Emotion PDFDocument5 pagesManagement of Herpes Labialis Triggered by Emotion PDFUmmiNo ratings yet
- 15 D16 298 Popovska MirjanaDocument5 pages15 D16 298 Popovska MirjanaVera Radojkova NikolovskaNo ratings yet
- A CASE OF RADIATION - INDUCED MUCOSITiS - PPTX NAVITADocument44 pagesA CASE OF RADIATION - INDUCED MUCOSITiS - PPTX NAVITANavita SharmaNo ratings yet
- Hookworms (Human and Zoonotic)Document5 pagesHookworms (Human and Zoonotic)Kyaru FuentesNo ratings yet
- NCP GiDocument6 pagesNCP GiTroy MagcalasNo ratings yet
- Original Article: Pedicle Tongue Flap Surgery in Oral Submucous FibrosisDocument4 pagesOriginal Article: Pedicle Tongue Flap Surgery in Oral Submucous FibrosisZuzu FinusNo ratings yet
- Ok PM BellaDocument25 pagesOk PM Bellapark kinanNo ratings yet
- 4.1 Pemphigus: Case 38 Pemphigus Vulgaris (Involving The Skin and Oral Mucosa) BDocument16 pages4.1 Pemphigus: Case 38 Pemphigus Vulgaris (Involving The Skin and Oral Mucosa) BIrma NovitasariNo ratings yet
- Oral Pemphigus Vulgaris: A Case Report With Direct Immunofluorescence StudyDocument4 pagesOral Pemphigus Vulgaris: A Case Report With Direct Immunofluorescence StudyYeni PuspitasariNo ratings yet
- Otitis Externa Complicated With Chloramphenicol Ear Drops-Induced PerichondritisDocument2 pagesOtitis Externa Complicated With Chloramphenicol Ear Drops-Induced Perichondritisrachel0301No ratings yet
- Saliva and Wound Healing: Henk S. Brand, Enno C.I. VeermanDocument6 pagesSaliva and Wound Healing: Henk S. Brand, Enno C.I. Veermanrozh rasulNo ratings yet
- Jurnal Mursicatio BucarumDocument4 pagesJurnal Mursicatio BucarumhairiahdjNo ratings yet
- Taneja2011 PDFDocument5 pagesTaneja2011 PDFمعتزعليNo ratings yet
- Ulcerative Lesions of The Oral Mucosa: Yu Zhou, Xiaoying Li, Xin Jin, and Qianming ChenDocument20 pagesUlcerative Lesions of The Oral Mucosa: Yu Zhou, Xiaoying Li, Xin Jin, and Qianming ChenIrma NovitasariNo ratings yet
- Lichen Planus of Lip - Report of A Rare Case With Review of LiteratureDocument7 pagesLichen Planus of Lip - Report of A Rare Case With Review of LiteratureDharmapadmi KasilaniNo ratings yet
- YCYSt DocumentDocument24 pagesYCYSt DocumentDodo AlsunaidiNo ratings yet
- Treatment of Lingual Traumatic Ulcer Accompanied With Fungal InfectionsDocument5 pagesTreatment of Lingual Traumatic Ulcer Accompanied With Fungal InfectionsYuganya SriNo ratings yet
- The Use of Ivermectin in Controlling An Outbreak of Scabies in A PrisonDocument4 pagesThe Use of Ivermectin in Controlling An Outbreak of Scabies in A Prisonarum palupiNo ratings yet
- Finnsonetal 2013 ADWCcomprehensivereviewDocument21 pagesFinnsonetal 2013 ADWCcomprehensivereviewBaronKornNo ratings yet
- The Management of Cancer Pain: Nathan I. Cherny, MBBSDocument47 pagesThe Management of Cancer Pain: Nathan I. Cherny, MBBSBaronKornNo ratings yet
- Non-Steroidal Anti-Inflammatory Drugs: Therapeutic EffectsDocument8 pagesNon-Steroidal Anti-Inflammatory Drugs: Therapeutic EffectsBaronKornNo ratings yet
- 09 PT Ed HyponatremiaDocument2 pages09 PT Ed HyponatremiaBaronKornNo ratings yet
- Clinical Review: Antidepressant-Induced Hyponatremia in Older AdultsDocument12 pagesClinical Review: Antidepressant-Induced Hyponatremia in Older AdultsBaronKornNo ratings yet
- Hyponatremia Associated With Selective Serotonin-Reuptake Inhibitors in Older AdultsDocument5 pagesHyponatremia Associated With Selective Serotonin-Reuptake Inhibitors in Older AdultsBaronKornNo ratings yet
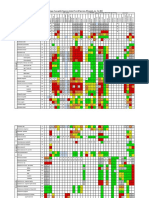
- Organism: Percentage of Susceptible Organisms Isolated From All Specimen, 83 Hospitals, Jan - Dec 2020Document2 pagesOrganism: Percentage of Susceptible Organisms Isolated From All Specimen, 83 Hospitals, Jan - Dec 2020BaronKornNo ratings yet
- Unit 5 Conclusion and DiscussionDocument4 pagesUnit 5 Conclusion and DiscussionBaronKornNo ratings yet
- Antibiotics 10 01278Document11 pagesAntibiotics 10 01278BaronKornNo ratings yet
- SAT Practice TestDocument77 pagesSAT Practice TestfhfsfplNo ratings yet
- Bhil Tribal Mobilisation in AlirajpurDocument14 pagesBhil Tribal Mobilisation in Alirajpurrahul banerjeeNo ratings yet
- Module 1 Notes The White Bird Reading The Image Painting Analysis PDFDocument4 pagesModule 1 Notes The White Bird Reading The Image Painting Analysis PDFMelbely Rose Apigo BaduaNo ratings yet
- Solutions GoldsteinDocument10 pagesSolutions GoldsteinAnyiNo ratings yet
- 2015 Nos-Dcp National Oil Spill Disaster Contingency PlanDocument62 pages2015 Nos-Dcp National Oil Spill Disaster Contingency PlanVaishnavi Jayakumar100% (1)
- Twilight PrincessDocument49 pagesTwilight PrincessHikari DiegoNo ratings yet
- Updated G10 Class Routine Effective From 12 January 2023Document1 pageUpdated G10 Class Routine Effective From 12 January 2023NiloyNo ratings yet
- NCP Orif Right Femur Post OpDocument2 pagesNCP Orif Right Femur Post OpCen Janber CabrillosNo ratings yet
- Manual Wire Rope Winches Wall-Mounted Wire Rope Winch SW-W: Equipment and ProcessingDocument1 pageManual Wire Rope Winches Wall-Mounted Wire Rope Winch SW-W: Equipment and Processingdrg gocNo ratings yet
- Midterm Exam Gor Grade 11Document2 pagesMidterm Exam Gor Grade 11Algelle AbrantesNo ratings yet
- Cecilia-Puff-Tee-Final-OUSM-Designs-12 MESES A TALLA 8Document19 pagesCecilia-Puff-Tee-Final-OUSM-Designs-12 MESES A TALLA 8Jose SanchezNo ratings yet
- S TR GEN ID (Component Marking) (Rev 3 2009) - AN Marked UpDocument6 pagesS TR GEN ID (Component Marking) (Rev 3 2009) - AN Marked UpsnclgsraoNo ratings yet
- Niir Integrated Organic Farming Handbook PDFDocument13 pagesNiir Integrated Organic Farming Handbook PDFNatalieNo ratings yet
- Technical Information: Range-Free Controller FA-M3 System Upgrade GuideDocument33 pagesTechnical Information: Range-Free Controller FA-M3 System Upgrade GuideAddaNo ratings yet
- Plastics and Polymer EngineeringDocument4 pagesPlastics and Polymer Engineeringsuranjana26No ratings yet
- Tuberculosis PowerpointDocument69 pagesTuberculosis PowerpointCeline Villo100% (1)
- Poly 103Document20 pagesPoly 103Sharifah Zulaikha BenYahyaNo ratings yet
- SP Essay 1Document14 pagesSP Essay 1api-511870420No ratings yet
- Syllabus Unit Iv Unit Commitment and Economic DispatchDocument23 pagesSyllabus Unit Iv Unit Commitment and Economic DispatchBALAKRISHNANNo ratings yet
- Presentation On 4G TechnologyDocument23 pagesPresentation On 4G TechnologyFresh EpicNo ratings yet
- The Broadband ForumDocument21 pagesThe Broadband ForumAnouar AleyaNo ratings yet
- The FOA Reference For Fiber Optics - Fiber Optic TestingDocument19 pagesThe FOA Reference For Fiber Optics - Fiber Optic TestingvsalaiselvamNo ratings yet
- Managing Diabetic Foot Ulcers ReadingDocument21 pagesManaging Diabetic Foot Ulcers Readinghimanshugupta811997No ratings yet
- Dual Shield 7100 Ultra: Typical Tensile PropertiesDocument3 pagesDual Shield 7100 Ultra: Typical Tensile PropertiesDino Paul Castro HidalgoNo ratings yet
- Parts Catalogue of Foton: (TC2A504-034K)Document132 pagesParts Catalogue of Foton: (TC2A504-034K)МаксимNo ratings yet
- 5G Transport Slice Control in End-To-End 5G NetworksDocument19 pages5G Transport Slice Control in End-To-End 5G NetworksmorganNo ratings yet
- Presentation - Delight Bulb PDFDocument22 pagesPresentation - Delight Bulb PDFShiva KishoreNo ratings yet
- Indor Lighting DesignDocument33 pagesIndor Lighting DesignRajesh MalikNo ratings yet
- Save Water SpeechDocument4 pagesSave Water SpeechHari Prakash Shukla0% (1)
- Hopeless PlacesDocument1,304 pagesHopeless Placesmoreblessingmarvellous659No ratings yet