Professional Documents
Culture Documents
2345-Article Text-7591-2-10-20200422aa
Uploaded by
Jihan AshariOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2345-Article Text-7591-2-10-20200422aa
Uploaded by
Jihan AshariCopyright:
Available Formats
Paediatrica Indonesiana
p-ISSN 0030-9311; e-ISSN 2338-476X; Vol.60, No.2(2020). p. 95-100; doi: http://dx.doi.org/10.14238/pi60.2.2020.95-100
Original Article
Comparison of Growth Diagrams Of Indonesian
Children to 2006 World Health Organization Growth
Standards in diagnosing stunting
Rizki Aryo Wicaksono1, Karina Sugih Arto1, Rina Amalia Caromina Saragih1,
Melda Deliana1, Munar Lubis1, Jose Rizal Latief Batubara2
Abstract Keywords: : WHO Growth Standards 2006;
Growth Diagrams of Indonesian Children; stunting
Background Stunting represents a linear growth distur-
bance due to chronic malnutrition, recurrent infection,
and inadequate psychosocial stimulation. The 2006 World
Health Organization (WHO) Growth Standards are utilized
S
as a modality in monitoring children’s growth, but to date,
there has been no recommendation on use of the Growth tunting is characterized by short stature,
Diagrams of Indonesian Children to monitor the growth of but not every child with short stature is
Indonesian children.
Objective To determine the proportion of stunting, the sen- stunted.1 Stunting reflects a disruption of
sitivity and specificity of Growth Diagrams of Indonesian Chil- linear growth due to chronic malnutrition,
dren for diagnosing stunting. In addition, we aimed to com- recurrent infections, and inadequate psychosocial
pare proportions of stunting using the 2006 WHO Growth stimulation due to environmental conditions and
Standards and Growth Diagrams of Indonesian Children.
Method A cross-sectional study was conducted in Lawe Alas socioeconomic status.2,3 By definition, stunting is the
District, Southeast Aceh, Indonesia. Subjects were children index of body length by age (BAZ) or height by age
aged 1-59 months who fulfilled the inclusion criteria. Weight (HAZ), with Z-score less than -2 standard deviations
and height measurements were plotted on the Growth Dia-
grams of Indonesian Children and on the 2006 WHO Growth (SD).3 Stunting that occurs before the age of 2 years
Standards to determine the stature of subjects. Stunting was is predicted to lead to adverse cognitive functions.4
defined as the index Z-score for HAZ of less than -2 SD for In addition to the decline of cognitive abilities, 4
the 2006 WHO Growth Standards, and an HAZ index of
below the 10th percentile (p10th) for the Growth Diagrams
of Indonesian Children.
Results Of 141 subjects, 66 (46.8%) had stunting based
on the 2006 WHO Growth Standards and 51 (34.8%) had
stunting based on Growth Diagrams of Indonesian Children.
The sensitivity and specificity of the Growth Diagrams of
From the Department of Child Health, Universitas Sumatera Utara
Indonesian Children were 75.5% and 98.66%, respectively. Medical School/H. Adam Malik Hospital, Medan, North Sumatera1 and
Significantly more children were considered to be stunted us- Universitas Indonesia Medical School/Dr. Cipto Mangunkusumo Hospital,
ing the 2006 WHO Growth Standards than using the Growth Jakarta2, Indonesia.
Diagrams of Indonesian Children.
Conclusion Stunting prevalence is high in Southeast Corresponding author: Rizki Aryo Wicaksono. Department of Child
Aceh. The Growth Diagrams of Indonesian Children is a Health, Universitas Sumatera Utara Medical School, Medan, North
spesific and sensitive tool to diagnosed stunting in accor- Sumatera, Indonesia. Jln. dr. T. Mansur No. 66 Kampus USU Medan
dance with Indonesian children’s growth patterns. [Paediatr 20154. (061) 8211045/Fax. (061) 82162624. Email: rizkiaryowicaksono@
Indones. 2020;60:95-100; doi: http://dx.doi.org/10.14238/ gmail.com.
pi60.2.2020.95-100 ].
Submitted November 28, 2019. Accepted April 17, 2020.
Paediatr Indones, Vol. 60, No. 2, March 2020 • 95
Rizki Aryo Wicaksono al.: Comparison of Growth Diagrams Of Indonesian Children to 2006 World Health Organization
Growth Standards in diagnosing stunting
patients with long term stunting have poor immunity, 2017 to May 2018. Subjects’ parents provided
so they easily get sick, increasing their morbidity and written informed consent. Children with malignant
mortality.5 or autoimmune diseases, bone abnormalities, or who
According to the National Basic Health Research received long-term steroid therapy which affects linear
Report (Riskesdas), the prevalence of stunting in growth were excluded. This study was approved by
Indonesian children was above 30% in four separate the Research Ethics Committee of the Universitas
years (2007, 2010, 2013 and 2018). Indonesia’s Sumatera Utara Medical School.
prevalence of stunting was 36.8% in 2007, 35.6% in Subjects’ demographic data were collected
2010, 37.2% in 2013, and 30.8% in 2018.6-9 According consisting of gender, age, gestational age, birth weight,
to the 2018 National Basic Health Research Report, and birth length. Weight measurement for young
Aceh was in the top three regions with the highest children not yet able to stand was done using a Seca
stunting prevalence in Indonesia.9 725 baby scale, while weight measurement for children
A diagnosis of stunting can be made by several able to stand was done using a Seca 803 footprint
standards, including the National Center for Health scale. The infants wore only underwear during the
Statistics/Centers for Disease Control (NCHS/CDC) weight measurement. The scale needle was read when
or the 2006 World Health Organization Child Growth the child was calm and the needle stayed constant.
Standards. The most commonly used chart in Indonesia Subjects’ body lengths were measured by a Seca 334
is the 2006 WHO Growth Standards for children infant scale for those under 2 years or a Seca 206
under 5 years.2 Many countries have used the 2006 microtoise for children above 2 years. Subjects wore
WHO Growth Standards as a modality for monitoring no footwear while body length/height was measured.
children's growth. However, the 2006 WHO Growth Anthropometric data were plotted on the
Standards are not always appropriate for assessing Growth Diagrams of Indonesian Children and the 2006
child growth due to differing racial, demographic, and WHO Growth Standards to determine the stature of
growth patterns among the world’s nations.10 subjects. Stunting was defined as the index Z-score
To date, no recommendations have been made for HAZ of less than -2 SD for the 2006 WHO
regarding child growth curves that best represent Growth Standards,3 and an HAZ index of below the
Indonesian child growth. So, in 2006 Batubara et al.11 10th percentile (p10th) for the Growth Diagrams of
conducted a study to create a standard growth curve Indonesian Children.11
for Indonesian children. However, to our knowledge, Univariate analysis was performed on the data to
no study has compared the Growth Diagrams of determine the distribution of subjects’ characteristics.
Indonesian Children to the 2006 WHO Growth Sensitivity, specificity, positive predictive value,
Standard Curve, with regards to the most appropriate negative predictive value, positive likelihood ratio,
chart for Indonesia’s health workers in daily health and negative likelihood ratio were analyzed in a
practices. Therefore, we aimed to assess the sensitivity 2x2 table. McNemar test was used to compare the
and specificity of the Growth Diagrams of Indonesian prevalence of stunting between the two growth charts.
Children in diagnosing stunting in children in the Results with P values <0.05 were considered to be
Southeast Aceh District. significant, with 95% confidence intervals.
Methods Results
This cross-sectional study was done to assess the The characteristics of 141 study subjects are shown in
sensitivity and specificity of the Growth Diagrams Table 1. The stunting prevalence was 36.2% by the
of Indonesian Children compared to the 2006 WHO Growth Diagrams of Indonesian Children and 46.8% by
Growth Standard. The subject population in this study the 2006 WHO Growth Standards.
were children aged 1 to 59 months and 30 days who The diagnostic analysis results of the 2006 WHO
lived in the Village Ngkeran and Lawe Konker, Lawe Growth Standards as the gold standard compared
Alas District, Southeast Aceh District from December to the Growth Diagrams of Indonesian Children are
96 • Paediatr Indones, Vol. 60, No. 2, March 2020
Rizki Aryo Wicaksono al.: Comparison of Growth Diagrams Of Indonesian Children to 2006 World Health Organization
Growth Standards in diagnosing stunting
shown in Table 2. The Growth Diagrams of Indonesian The population of Indonesian children has a
Children had 75.75% sensitivity, 98.66% specificity, lower mean height than the average population of
98.03% positive predictive value, 82.22% negative children in Europe. A previous study conducted a
predictive value, as well as positive likelihood ratio of meta-analysis of anthropometric data in 55 countries
75 and negative likelihood ratio of 0.24. There was a compared to the 2006 WHO Growth Standards.
statistically significant difference in the diagnosis of The study found that European populations had
stunting using Growth Diagrams of Indonesian Children a +0.5 SD higher mean height compared to the
compared to the 2006 WHO Growth Standards height of the 2006 WHO Growth Standards. Asian
(P <0.001). populations such as Saudi Arabia and India had a
-0.5 SD lower mean height compared to the 2006
WHO Growth Standards.12 Another study stated
Discussion that the German population of children less than 5
years of age had mean height at the 60th percentile
The 2006 WHO Growth Standards is the current in males and 62nd percentile in females.13 Although
growth chart used in Indonesia for children under 5 the WHO recommends using only one type of growth
years of age. This chart was made based on data from chart standard, a previous study recommended that
8,500 children from several health centers throughout national growth chart standards be the guide for each
the world. The study was conducted on children from country.13 Consistent with this recommendation,
various ethnic backgrounds who received exclusive another previuous study showed that the use of the
breastfeeding,3 but there were no representatives 2006 WHO Growth Standards led to underdiagnosed
from Southeast Asian countries in the sampling of stunting in children in Australia.14
the study.2
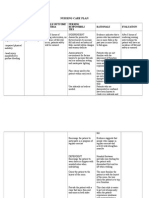
Table 1. Characteristics of study subjects
Characteristics (N = 141)
Sex, n (%)
Male 73 (51.8)
Female 68 (48.2)
Median age (range), months 17.0 (1.0-60.0)
Median weight (range), kg 9.2 (3.0-21.0)
Mean height (SD), cm 77.8 (13.68)
Median gestational age (range), weeks 39.0 (35.0-40.0)
Median birth weight (range), grams 2750.0 (2100.0-3150.0)
Median birth height (range), cm 48.0 (44.0-51.0)
Height/age by 2006 WHO Growth Standards, n (%)
Stunted 66 (46.8)
Not stunted 75 (53.2)
Height/age by Growth Diagrams of Indonesian Children, n (%)
Stunted 51 (36.2)
Not stunted 90 (63.8)
Table 2. Analysis of the 2006 WHO Growth Standards compared to the Growth Diagrams of Indonesian Children
Height/age based on Growth Diagrams of Indonesian Height/age based on 2006 WHO Growth Standards
Total P value*
Children Stunted (%) Not stunted (%)
Stunted 50 (98.1) 1 (1.9) 51 (36.2) < 0.001
Not stunted 16 (17.8) 74 (82.2) 90 (63.8)
Total 66 (46.8) 75 (53.2) 141 (100)
* McNemar test
Paediatr Indones, Vol. 60, No. 2, March 2020 • 97
Rizki Aryo Wicaksono al.: Comparison of Growth Diagrams Of Indonesian Children to 2006 World Health Organization
Growth Standards in diagnosing stunting
Children should be screened for stunting in order child growth projection, and not based on real growth
to make an early diagnosis to correct the problem. data.3
Hence, a high sensitivity diagnostic examination A study reported that Indonesian boys and girls
is needed. Moreover, positive predictive value and were significantly shorter than the 2006 WHO Growth
negative predictive value are more important than Standards.22 In our study, there was a significant
sensitivity and specificity. These values can predict difference in the proportion of stunting based on
the likelihood of someone suffering from a disease if 2006 WHO Growth Standards (46.8%) compared to
the results are positive, and the likelihood of someone the Growth Diagrams of Indonesian Children (36.2%).
to be healthy if the results of the examination are Our results were similar to several studies in other
negative.15 In the comparison to the 2006 WHO developing countries. Another study stated that the
Growth Standards, the Growth Diagrams of Indonesian average height population of Indonesia’s children was
Children had sensitivity of 75.75%, specificity of 1.47 SD lower in males and 1.43 SD lower in females,
98.66%, positive predictive value of 98.03%, negative compared to the population of children in America.
predictive value of 82.22%, positive likelihood ratio The WHO has 0.5 SD as the standard for significant
of 75, and negative likelihood ratio of 0.24. Previous difference. This greatest difference is at four years of
study comparing the proportions of stunting based age in boys and twelve years in girls.11 This situation
on the two growth charts, showed that stunting is may lead to lower proportions of stunting using the
often overdiagnosed with the WHO Growth Standards Growth Diagrams of Indonesian Children compared to
assessment.12 To our knowledge, this is the first study the 2006 WHO Growth Standards.
to compare the accuracy of the Growth Diagrams of Internal and external factors play important
Indonesian Children as a national growth chart to the roles in the cause of stunting. Pre-natal and post-
2006 WHO Growth Standards. natal factors are included in the internal risk factors
The Basic Health Research Report recorded the that cause stunting. In addition, chronic infections in
prevalence of national stunting in 2018 to be 30.8%.9 infants and children also greatly affect the occurrence
Several national surveys in other countries such of stunting.23 Other post-natal factors that can cause
as Nigeria in 2018,16 India in 2017,17 Ethiopia in stunting are chronic recurrent infections, such as
2018,18 Guatemala in 2019,19 and Gabon in 2008,20 chronic diarrhea and acute respiratory infection.24
showed that successive stunting prevalences were External factors including sanitation and hygiene, play
30.2%, 38.4%, 41.8%, 46.5% and 30.5%, respectively. an important role in preventing stunting, since poor
The 2006 WHO Growth Standards were used in sanitation and hygiene increase the risk of chronic
those studies as a reference for the classification of infection.25
stunting. The limitations of this study were the small
A study in Argentina compared the 2006 WHO sample size, no risk factor analysis, and the population
Growth Standards to the Argentina Pediatric Society was comprised from only one region. This study also
(APS) Committee of Growth and Development Chart had potential risks of bias because workups on other
found prevalences of stunting to be 7.9% and 5.3%, causes of short stature, such as Patau syndrome or
respectively.21 The authors noted that the difference growth hormone deficiency, were not conducted. For
in proportion may have been due to differences in such reasons, further multicenter study needs to be
age group and cut-offs between the APS and WHO done with a larger number of study subjects and with
criteria. Moreover, the WHO sample was standardized a risk factor analysis for causes of stunting.
to be children who were healthy, well fed according to In conclusion, the prevalence of stunting in this
the WHO nutrition recommendation, and growing in study is high by using both of the Growth Diagrams
good socioeconomic environments which supported of Indonesian Children and the 2006 WHO Growth
good growth and development. Complex statistical Standards. Therefore, prevalence is higher when the
analysis was done to normalize the asymmetrical 2006 WHO Growth Standards is used. The Growth
distribution by removing extreme values.21 The 2006 Diagrams of Indonesian Children appear to be a solid
WHO Growth Standards also has selective drop out and reliable tool to diagnose stunting in Indonesian
criteria, which means that the chart is based on ideal children. Shifting to the Growth Diagrams of Indonesian
98 • Paediatr Indones, Vol. 60, No. 2, March 2020
Rizki Aryo Wicaksono al.: Comparison of Growth Diagrams Of Indonesian Children to 2006 World Health Organization
Growth Standards in diagnosing stunting
Children may have considerable implications for child Indonesia tahun 2018. Jakarta: Kemenkes RI; 2018.
health programmes. 10. Fenn B, Penny ME. Using the new World Health Organisation
growth standards: differences from 3 countries. J Pediatr
Gastroenterol Nutr. 2008;46:316-21. DOI: 10.1097/
Conflict of Interest MPG.0b013e31815d6968.
11. Batubara JRL, Alisjahbana A, Gerver-Jansen AJGM,
None declared. Alisjahbana B, Sadjimin T, Tasli Y, et al. Growth
diagrams of Indonesian children The nationwide
survey of 2005. Paediatr Indones. 2006;46:118-26.
Funding Acknowledgment DOI: 10.14238/pi46.3.2006.118-26
12. Natale V, Rajagopalan A. Worldwide variation in human
The authors received no specific grants from any funding agency growth and the World Health Organization growth
in the public, commercial, or not-for-profit sectors. standards: a systematic review. BMJ Open. 2014;4:e003735.
DOI: 10.1136/bmjopen-2013-003735.
13. Rosario AS, Schienkiewitz A, Neuhauser H. German height
References references for children aged 0 to under 18 years compared
to WHO and CDC growth charts. Ann Hum Biol. 2011;
1. Asworth A. Nutrition, food security, and health. In: Kliegman 38:121-30. DOI: 10.3109/03014460.2010.521193.
RM, Stanton BF, Schor NF, St Geme III JW, editors. Nelson 14. Hughes I, Harris M, Cotterill A, Garnett S, Bannink E,
textbook of pediatrics. 20th ed. Philadelphia: Elsevier; 2016. Pennell C, et al. Comparison of Centers for Disease Control
p. 295-306. and Prevention and World Health Organization references/
2. Pulungan AB. Exploring the big picture of stunting: standards for height in contemporary Australian children:
Indonesian perspective. In: 15th Pediatric update exploring analyses of the Raine Study and Australian National
the big picture of childhood stunting: Indonesian perspective. Children's Nutrition and Physical Activity cohorts. J Paediatr
Jakarta: Ikatan Dokter Anak Indonesia; 2016. p. 3-7. Child Health. 2014;50:895-901. DOI: 10.1111/jpc.12672.
3. World Health Organization. Interpretation Guide Nutrition 15. Dahlan SM. Penelitian diagnostik: dasar-dasar teoritis dan
Landscape Information System (NLIS). Geneva: WHO; aplikasi dengan program SPSS dan stata. Jakarta: Salemba
2010. p.1-2. Medika; 2009. p.103-6.
4. Grantham-McGregor S, Cheung YB, Cueto S, Glewwe 16. National Bureau of Statistics Nigeria. National Nutrition
P, Richter L, Strupp B. Developmental potential in the and Health Survey 2018. Abuja: UNICEF; 2018. p.41-6.
first 5 years for children in developing countries. Lancet. 17. Ministry of Health and Family Welfare. National Family
2007;369:60-70. DOI: 10.1016/S0140-6736(07)60032-4. Health Survey (NFHS-4) 2015-2016. Mumbai: International
5. Black RE, Victora CG, Walker SP, Bhutta ZA, Christian Institute of Population Sciences. 2017.
P, de Onis M, et al. Maternal and child undernutrition 18. Tariku EZ, Abebe GA, Melketsedik ZA, Gutema BT.
and overweight in low-income and middle-income Prevalence and factors associated with stunting and
countries. Lancet. 2013;382:427-51. DOI: 10.1016/S0140- thinness among school-age children in Arba Minch Health
6736(13)60937-X. and Demographic Surveillance Site, Southern Ethiopia.
6. Badan Penelitian dan Pengembangan Kesehatan Kemenkes PLoS One. 2018;13:e0206659. DOI: 10.1371/journal.
RI. Laporan Hasil Riset Kesehatan Dasar (Riskesdas) pone.0206659.
Indonesia tahun 2007. Jakarta: Kemenkes RI; 2008. 19. Gatica-Domínguez G, Victora C, Barros A. Ethnic
7. Badan Penelitian dan Pengembangan Kesehatan Kemenkes inequalities and trends in stunting prevalence among
RI. Laporan Hasil Riset Kesehatan Dasar (Riskesdas) Guatemalan children: an analysis using National Health
Indonesia tahun 2010. Jakarta: Kemenkes RI; 2010. Surveys 1995–2014. Int J Equity Health. 2019;18:110.
8. Badan Penelitian dan Pengembangan Kesehatan Kemenkes DOI: 10.1186/s12939-019-1016-0.
RI. Laporan Hasil Riset Kesehatan Dasar (Riskesdas) 20. Schwarz NG, Grobusch MP, Decker ML, Goesch J, Poetschke
Indonesia tahun 2013. Jakarta: Kemenkes RI; 2013. M, Oyakhirome S, et al. WHO 2006 Child Growth Standards:
9. Badan Penelitian dan Pengembangan Kesehatan Kemenkes implications for the prevalence of stunting and underweight-
RI. Laporan Hasil Riset Kesehatan Dasar (Riskesdas) for-age in a birth cohort of Gabonese children in comparison
Paediatr Indones, Vol. 60, No. 2, March 2020 • 99
Rizki Aryo Wicaksono al.: Comparison of Growth Diagrams Of Indonesian Children to 2006 World Health Organization
Growth Standards in diagnosing stunting
to the Centers for Disease Control and Prevention 2000 23. Millward DJ. Nutrition, infection and stunting: the role
growth charts and the National Center for Health Statistics of deficiencies of individual nutrients and foods, and of
1978 growth references. Public Health Nutr. 2008;11:714-19. inflammation, as determinants of reduced linear growth
DOI: 10.1017/S1368980007001449. of children. Nutr Res Rev. 2017;30:50-72. DOI: 10.1017/
21. Padula G, Seoane AI, Salceda SA. Variatons in estimates S0954422416000238.
of underweight, stunting, wasting, overweight and obesity 24. Aguayo VM, Menon P. Stop stunting: improving child
in children from Argentina comparing three growth charts. feeding, women's nutrition and household sanitation in
Public Healt Nutr. 2012;15:2086-90. DOI: 10.1017/ South Asia. Matern Child Nutr. 2016;12;3-11. DOI: 10.1111/
S136898001200095X. mcn.12283.
22. Pulungan AB, Julia M, Batubara JRL, Hermanussen M. 25. Bagcchi S. India's poor sanitation and hygiene practices
Indonesian national synthetic growth charts. Acta Sci Pediatr. are linked to stunting in children, study finds. BMJ.
2018;1:20-34. 2015;350:1564. DOI: 10.1136/bmjopen-2014-005180.
100 • Paediatr Indones, Vol. 60, No. 2, March 2020
You might also like
- The Patient History An Evidence-Based Approach To Differential DiagnosisDocument4 pagesThe Patient History An Evidence-Based Approach To Differential DiagnosisISAYK13% (8)
- Vaccine Science vs. Science FictionDocument16 pagesVaccine Science vs. Science FictionBright09100% (1)
- A Guide To Getting Started in TelemedicineDocument405 pagesA Guide To Getting Started in TelemedicineAnthony WilsonNo ratings yet
- NVBSP Form15Document6 pagesNVBSP Form15Rhodz Caballes RefuerzoNo ratings yet
- Risk For FallDocument3 pagesRisk For FallLesValenzuela100% (1)
- Paediatrica IndonesianaDocument8 pagesPaediatrica Indonesianachartreuse avonleaNo ratings yet
- Paediatrica IndonesianaDocument8 pagesPaediatrica Indonesianafkia2013No ratings yet
- 2.jurnal Kepkel4Document7 pages2.jurnal Kepkel4Himatul AliyahNo ratings yet
- Jurnal Indonesia 1Document11 pagesJurnal Indonesia 1Juli ArnithaNo ratings yet
- 1 s2.0 S2352013216300205 MainDocument9 pages1 s2.0 S2352013216300205 MainDendy FebriantNo ratings yet
- Analysis of Factors Affecting The Prevalence of Stunting On Children Under Five Years 8429Document11 pagesAnalysis of Factors Affecting The Prevalence of Stunting On Children Under Five Years 8429Demsa SimbolonNo ratings yet
- Pengaruh Stimulasi Terhadap Perkembangan Motorik Kasar Pada Anak Usia 1-3 Tahun Di Desa Renda Kecamatan Towea Kabupaten Muna Sulawesi TenggaraDocument7 pagesPengaruh Stimulasi Terhadap Perkembangan Motorik Kasar Pada Anak Usia 1-3 Tahun Di Desa Renda Kecamatan Towea Kabupaten Muna Sulawesi TenggaraHidayahNo ratings yet
- Paediatrica IndonesianaDocument8 pagesPaediatrica IndonesianaAnna ClarkNo ratings yet
- Jurnal KasmaDocument13 pagesJurnal KasmaAhmad ZahirNo ratings yet
- Prenatal Factors Associated With The Risk of Stunting: A Multilevel Analysis Evidence From Nganjuk, East JavaDocument7 pagesPrenatal Factors Associated With The Risk of Stunting: A Multilevel Analysis Evidence From Nganjuk, East JavaRido SaputraNo ratings yet
- 451 1378 1 PBDocument11 pages451 1378 1 PBprawira heroNo ratings yet
- Jurnal Stunting PDFDocument10 pagesJurnal Stunting PDFNanang SupriyantoNo ratings yet
- The Dominant Factors of Stunting Incidence in Toddlers (0 - 59 Months) in East Lombok Regency A Riskesdas Data Analysis 2018Document11 pagesThe Dominant Factors of Stunting Incidence in Toddlers (0 - 59 Months) in East Lombok Regency A Riskesdas Data Analysis 2018International Journal of Innovative Science and Research Technology100% (1)
- JPaediatrNursSci 3 3 73 761Document4 pagesJPaediatrNursSci 3 3 73 761vaideeswari kumarNo ratings yet
- Anastasia 2023Document17 pagesAnastasia 2023lalallili2No ratings yet
- Ana Riandari (152221039) Tugas Penelitian Kebidanan 2 (Dosen Isfaizah, S.si.T.,MPH)Document12 pagesAna Riandari (152221039) Tugas Penelitian Kebidanan 2 (Dosen Isfaizah, S.si.T.,MPH)Ana RiandariNo ratings yet
- Faktor - Faktor Yang Berhubungan Dengan Pertumbuhan Bayi 6-12 Bulan Di Puskesmas Simpang BaruDocument7 pagesFaktor - Faktor Yang Berhubungan Dengan Pertumbuhan Bayi 6-12 Bulan Di Puskesmas Simpang BaruWidhea novita putriNo ratings yet
- Rifda Azkiatus Salamah - 4411418014Document26 pagesRifda Azkiatus Salamah - 4411418014Rifda AzkiaNo ratings yet
- Investigating Minimum Acceptable Diet and Infant and Child Feeding Index As Indicators of Stunting in Children Aged 6-23 MonthsDocument10 pagesInvestigating Minimum Acceptable Diet and Infant and Child Feeding Index As Indicators of Stunting in Children Aged 6-23 MonthsAlif riadiNo ratings yet
- Determinants of Stunting in Children Aged 12-59 MonthsDocument10 pagesDeterminants of Stunting in Children Aged 12-59 MonthsMichimichi 78No ratings yet
- Wellness and Healthy Wellness and Healthy Magazine MagazineDocument10 pagesWellness and Healthy Wellness and Healthy Magazine MagazineGalih EkaNo ratings yet
- Naskah Publikasi P1337424415045Document9 pagesNaskah Publikasi P1337424415045rechybsNo ratings yet
- Association of Energy Intake and Physical Activity With OverweighDocument6 pagesAssociation of Energy Intake and Physical Activity With OverweighArdanNo ratings yet
- 2246-Article Text-8369-9706-10-20230606Document11 pages2246-Article Text-8369-9706-10-20230606Gek Sinta ManuabaNo ratings yet
- 247 767 1 PB PDFDocument10 pages247 767 1 PB PDFAnnisa Abdul AzisNo ratings yet
- Journal Determinants of Stunting and Child Development in Jombang District With Summary (Background Underlying The Occurrence of Stunting)Document27 pagesJournal Determinants of Stunting and Child Development in Jombang District With Summary (Background Underlying The Occurrence of Stunting)Alifia 123No ratings yet
- Pone 0233949Document13 pagesPone 0233949Shanya rahma AdrianiNo ratings yet
- A Determinant Analysis of Stunting Prevalence On Under 5-Year-Old Children To Establish Stunting Management PolicyDocument6 pagesA Determinant Analysis of Stunting Prevalence On Under 5-Year-Old Children To Establish Stunting Management PolicypuspitaNo ratings yet
- Jurnal Metodologi Penelitian (Afria Novita)Document24 pagesJurnal Metodologi Penelitian (Afria Novita)Afria NovitaNo ratings yet
- Esay Bahasa InggrisDocument6 pagesEsay Bahasa Inggrisni madeNo ratings yet
- Health Literacy and Health Promotion Behaviors of Adolescents in TurkeyDocument5 pagesHealth Literacy and Health Promotion Behaviors of Adolescents in Turkeyege fNo ratings yet
- Stunting Among Children Under Two Years in IndonesiaDocument12 pagesStunting Among Children Under Two Years in Indonesiarezky_tdNo ratings yet
- Correlation Between Non-Exclusive Breastfeeding and Low Birth Weight To Stunting in ChildrenDocument5 pagesCorrelation Between Non-Exclusive Breastfeeding and Low Birth Weight To Stunting in ChildrenAnonymous hETtEBkk7No ratings yet
- Sharma2011 Article GrowthAndNeurosensoryOutcomesODocument6 pagesSharma2011 Article GrowthAndNeurosensoryOutcomesOSayak ChowdhuryNo ratings yet
- Development of Stunting Early Detection Kit For Children Under Two Years: Validity and ReliabilityDocument8 pagesDevelopment of Stunting Early Detection Kit For Children Under Two Years: Validity and ReliabilityviharadewiNo ratings yet
- 35064-Article Text-104064-1-10-20200902Document8 pages35064-Article Text-104064-1-10-20200902kirito azumaNo ratings yet
- Perceived Susceptibility, Barriers, and Cues To Action As Determinant Factors of Reproductive Health BehaviorDocument9 pagesPerceived Susceptibility, Barriers, and Cues To Action As Determinant Factors of Reproductive Health BehaviorIJPHSNo ratings yet
- Sociocultural Transformation in Efforts To Reduce Mortality of Infants in Bone Regency IndonesiaDocument4 pagesSociocultural Transformation in Efforts To Reduce Mortality of Infants in Bone Regency IndonesiaidhaNo ratings yet
- Nusantara Hasana JournalDocument14 pagesNusantara Hasana JournalSiska Andariani RukmanaNo ratings yet
- Jurnal - Faktor Risiko Kejadian Stunting Pada Anak Usia 6-7 TahunDocument8 pagesJurnal - Faktor Risiko Kejadian Stunting Pada Anak Usia 6-7 TahunRezki Sari Anastasya TarmaniNo ratings yet
- Mentoring Program To Eradicate Malnutrition On Changes in The Nutritional Status of Stunting ToddlersDocument8 pagesMentoring Program To Eradicate Malnutrition On Changes in The Nutritional Status of Stunting ToddlersNIKENNo ratings yet
- Penelitian Pak Dodik Maternal Factor Ke Panjang LahirDocument4 pagesPenelitian Pak Dodik Maternal Factor Ke Panjang LahirRiri Amanda PratiwiNo ratings yet
- 1365-Article Text-4113-1-10-20220601Document6 pages1365-Article Text-4113-1-10-20220601hyunNo ratings yet
- Ejhs3203 0569Document10 pagesEjhs3203 0569ERNINo ratings yet
- Muhoozi 2017Document11 pagesMuhoozi 2017Dewi PrasetiaNo ratings yet
- Pertumbuhan Dan Perkembangan Anak Usia 3-6 TahunDocument8 pagesPertumbuhan Dan Perkembangan Anak Usia 3-6 TahunSilvi EkaNo ratings yet
- Hasriani PharmacognJ 15-5-833Document6 pagesHasriani PharmacognJ 15-5-833ardisukardi31No ratings yet
- PYMS Is A Reliable Malnutrition Screening ToolsDocument8 pagesPYMS Is A Reliable Malnutrition Screening ToolsRika LedyNo ratings yet
- Arindah Nur Sartika Prenatal and Postnatal Determinants of Stunting at Age 0-11 MonthsDocument14 pagesArindah Nur Sartika Prenatal and Postnatal Determinants of Stunting at Age 0-11 MonthsHanifa W PNo ratings yet
- Faktor-Faktor Yang Mempengaruhi Terjadinya Stunting Pada Balita Usia 24-59 BulanDocument8 pagesFaktor-Faktor Yang Mempengaruhi Terjadinya Stunting Pada Balita Usia 24-59 Bulansusi hendriyatiNo ratings yet
- Priyanka K P Synopsis-1Document18 pagesPriyanka K P Synopsis-1RAJESHWARI PNo ratings yet
- Survai Dasar Gizi Dan Kesehatan Di Wilayah Kerja World Vision Indonesia Dan Wahana Visi Indonesia Di Kabupaten MeraukeDocument8 pagesSurvai Dasar Gizi Dan Kesehatan Di Wilayah Kerja World Vision Indonesia Dan Wahana Visi Indonesia Di Kabupaten Meraukedwisuci91No ratings yet
- Kurva Pertumbuhan Anak Sehat Usia 3-18 Bulan Dari Keluarga Ekonomi Menengah Ke AtasDocument9 pagesKurva Pertumbuhan Anak Sehat Usia 3-18 Bulan Dari Keluarga Ekonomi Menengah Ke Atasracut_khansatraNo ratings yet
- STUNTINGDocument33 pagesSTUNTINGNini FarahNo ratings yet
- Etiologies and Early Diagnosis of Short Stature and Growth Failure in Children and AdolescentsDocument20 pagesEtiologies and Early Diagnosis of Short Stature and Growth Failure in Children and AdolescentsAnonymous 4N1GrDNo ratings yet
- Paper+21+ (2022 3 4) +The+Relationship+between+Family+Function+and+Emotional+Mental+ProblemsDocument6 pagesPaper+21+ (2022 3 4) +The+Relationship+between+Family+Function+and+Emotional+Mental+ProblemsWinonaNo ratings yet
- Neurodesarrollo PEG Japón 2015Document9 pagesNeurodesarrollo PEG Japón 2015Carlos Manuel Carranza VegaNo ratings yet
- Modelling Number of Stunting Binominal RegressionDocument16 pagesModelling Number of Stunting Binominal RegressionFikran Ahmad Ahmad Al-HadiNo ratings yet
- A Review of Child Stunting Determinants in IndonesiaDocument10 pagesA Review of Child Stunting Determinants in IndonesiaPutri SaripaneNo ratings yet
- Social Determinants of Health and Knowledge About Hiv/Aids Transmission Among AdolescentsFrom EverandSocial Determinants of Health and Knowledge About Hiv/Aids Transmission Among AdolescentsNo ratings yet
- Kebabs With A Side of SalmonellaDocument8 pagesKebabs With A Side of SalmonellaAlana TindaleNo ratings yet
- Cancer EpidemiologyDocument18 pagesCancer EpidemiologyMariaLisseth MoralesNo ratings yet
- AZOL 100 & AZOL 200: Azolnew Zealand Data SheetDocument11 pagesAZOL 100 & AZOL 200: Azolnew Zealand Data SheetSwempi Melchiadi AbollaNo ratings yet
- Ortho CaseDocument26 pagesOrtho CaseYusra ShaukatNo ratings yet
- GN RH AnaloguesDocument8 pagesGN RH Analoguesmahesh bhosaleNo ratings yet
- Service Annotated BibliographyDocument6 pagesService Annotated Bibliographyapi-355966257No ratings yet
- Alexandra Charrow: Implicit in What You're Asking Is The: MedicineDocument4 pagesAlexandra Charrow: Implicit in What You're Asking Is The: MedicineAletheia LaiNo ratings yet
- NCP Acute PainDocument3 pagesNCP Acute PainPrincess Alane MorenoNo ratings yet
- Resume' of AnreiDocument3 pagesResume' of AnreianreilegardeNo ratings yet
- "Dr. Pam" Gumbs Recognized As A Professional of The Year For Two Consecutive Years by Strathmore's Who's Who WorldwideDocument2 pages"Dr. Pam" Gumbs Recognized As A Professional of The Year For Two Consecutive Years by Strathmore's Who's Who WorldwidePR.comNo ratings yet
- Form Etik RevisiDocument12 pagesForm Etik RevisiRoma WestNo ratings yet
- Pit Fissure Sealants The Added Link in Preventative DentistryDocument1 pagePit Fissure Sealants The Added Link in Preventative Dentistryapi-348271404No ratings yet
- Risk Assessment For Lifting OperationDocument2 pagesRisk Assessment For Lifting OperationdsadasNo ratings yet
- Ebright Testimony UpdatedDocument28 pagesEbright Testimony UpdatedDeborah WeismanNo ratings yet
- Employee Benefits Program by Etiqa Life Insurance BerhadDocument23 pagesEmployee Benefits Program by Etiqa Life Insurance BerhadNurain SarinaNo ratings yet
- Biểu Đồ Không Có Tiêu Đề.drawioDocument46 pagesBiểu Đồ Không Có Tiêu Đề.drawioha thong thuongNo ratings yet
- Essentials of Nursing Leadership and Management 6th Edition Weiss Test Bank DownloadDocument4 pagesEssentials of Nursing Leadership and Management 6th Edition Weiss Test Bank Downloademmanuelmabelnjt7nn100% (32)
- Geria LecturetteDocument64 pagesGeria LecturetteSVPSNo ratings yet
- Viva Questions For MFD Part 2 ConsolidatedDocument34 pagesViva Questions For MFD Part 2 ConsolidatedEnea Nastri100% (1)
- Autohemotherapy - Treatment of SclerodermaDocument7 pagesAutohemotherapy - Treatment of SclerodermaOlivarNo ratings yet
- Law & Medicine Unit - 1Document4 pagesLaw & Medicine Unit - 1RosylaNo ratings yet
- ANM-Manual HIVAIDS PDFDocument203 pagesANM-Manual HIVAIDS PDFhemihemaNo ratings yet
- UlcerativecolitisDocument27 pagesUlcerativecolitisMohamed Abdulrazaq100% (1)
- Clinical Solid Waste Management Practices and Its Impact On Human Health and EnvironmentDocument13 pagesClinical Solid Waste Management Practices and Its Impact On Human Health and EnvironmentLi NearNo ratings yet
- Meningitis - 2018Document55 pagesMeningitis - 2018Abraham Anaely100% (1)