Professional Documents
Culture Documents
2016 - Olsen Et Al - Lifecourse HT - Lancet Comission
Uploaded by
Rafael Zambelli NobreOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2016 - Olsen Et Al - Lifecourse HT - Lancet Comission
Uploaded by
Rafael Zambelli NobreCopyright:
Available Formats
The Lancet Commissions
The mark “CDC” is owned by the US Dept of Health
and Human S ervices a nd i s used with permission.
Use of this logo is not an endorsement by HHS or
CDC or any particular product, service, or enterprise.
A call to action and a lifecourse strategy to address the global
burden of raised blood pressure on current and future
generations: the Lancet Commission on hypertension
Michael H Olsen*, Sonia Y Angell, Samira Asma, Pierre Boutouyrie, Dylan Burger, Julio A Chirinos, Albertino Damasceno, Christian Delles,
Anne-Paule Gimenez-Roqueplo, Dagmara Hering, Patricio López-Jaramillo, Fernando Martinez, Vlado Perkovic, Ernst R Rietzschel,
Giuseppe Schillaci, Aletta E Schutte, Angelo Scuteri, James E Sharman, Kristian Wachtell, Ji Guang Wang
Executive summary importance of other cardiovascular risk factors—eg, Lancet 2016; 388: 2665–712
Elevated blood pressure is the strongest modifiable risk smoking, obesity, dyslipidaemia, and diabetes mellitus— Published Online
factor for cardiovascular disease worldwide. Despite on antihypertensive treatment. However, as a September 23, 2016
http://dx.doi.org/10.1016/
extensive knowledge about ways to prevent as well as to Commission on hypertension, this report focuses mainly S0140-6736(16)31134-5
treat hypertension, the global incidence and prevalence on issues and actions related to elevated blood pressure.
*Chair
of hypertension and, more importantly, its cardiovascular Previous action plans for improving management of
Department of Internal
complications are not reduced—partly because of elevated blood pressure and hypertension have not yet Medicine, Holbæk Hospital and
inadequacies in prevention, diagnosis, and control of the provided adequate results. Therefore, the Commission Centre for Individualized
disorder in an ageing world. has identified ten essential and achievable goals and ten Medicine in Arterial Diseases
(CIMA), Odense University
The aim of the Lancet Commission on hypertension accompanying, mutually additive, and synergistic key
Hospital, University of
is to identify key actions to improve the management of actions that—if implemented effectively and broadly— Southern Denmark, Odense,
blood pressure both at the population and the individual will make substantial contributions to the management Denmark (M H Olsen DMSc);
level, and to generate a campaign to adopt the suggested of blood pressure globally. The Commission deliberately Hypertension in Africa Research
Team (HART), North-West
actions at national levels to reduce the impact of has not listed these complementary key actions by
University, Potchefstroom,
elevated blood pressure globally. The first task of the priority because the balance between strength of South Africa (M H Olsen);
Commission is this report, which briefly reviews the evidence, feasibility, and potential benefit could differ by Division of Prevention and
available evidence for prevention, identification, and country. Primary Care, New York City
Department of Health and
treatment of elevated blood pressure, hypertension,
Mental Hygiene, New York, NY,
and its cardiovascular complications. The report Introduction USA (S Y Angell MD); Global NCD
focuses on how as-yet unsolved issues might be tackled Background Branch, Division of Global
using approaches with population-wide impact and Elevated blood pressure is globally the strongest Health Protection, Center for
Global Health, Centers for
new methods for patient evaluation and education in modifiable risk factor for cardiovascular disease and Disease Control and Prevention,
the broadest sense (some of which are not always related disability. Its prevalence and downstream Atlanta, GA, USA (S Asma DDS);
strictly evidence based) to manage blood pressure detrimental impact on health are increasing because of Department of Pharmacology
worldwide. longer life expectancy and increased exposure to risk in and INSERM U 970, Georges
Pompidou Hospital, Paris
The report is built around the concept of lifetime risk the population. Despite extensive knowledge about ways Descartes University, Paris,
applicable to the entire population from conception. to both prevent and treat hypertension, its global France (Prof P Boutouyrie PhD);
Development of subclinical and sometimes clinical incidence, prevalence, and (more importantly) Kidney Research Centre, Ottawa
cardiovascular disease results from lifetime exposure to cardiovascular complications are not reduced, partly Hospital Research Institute,
Department of Cellular and
cardiovascular risk factors combined with the because of inadequacies in prevention, diagnosis, and Molecular Medicine, University
susceptibility of individuals to the harmful consequences control of the disorder in an ageing world. of Ottawa, ON, Canada
of these risk factors. The Commission recognises the (D Burger PhD); Department of
www.thelancet.com Vol 388 November 26, 2016 2665
The Lancet Commissions
Prevention: lifestyle and environmental changes
complications. The report focuses on unsolved issues,
rethinking these in the context of approaches with
Creating a healthy environment through strategies that accelerate socioeconomic
improvements and implementation of accepted health-promoting policies
population-wide impact and new techniques for patient
evaluation and education in its broadest sense, thereby
Health-promoting environment suggesting new ways to manage blood pressure globally.
Universal understanding of unhealthy and healthy lifestyles and blood pressure Because new techniques will be an important part of the
through endorsed, early, and sustained education using new technologies suggested solutions, our proposals will not always have a
Healthy behaviours
strong evidence base, but will highlight where further
research might be most beneficial. Therefore, the aim of
Universal access to measurement of blood pressure through inexpensive blood
pressure monitors (linked to establishment of global blood pressure surveillance)
the Lancet Commission will not be to conduct an extensive
review of hypertension or rewrite current guidelines on its
Measurement access management, but to create the momentum for improved
management of elevated blood pressure.
Blood pressure diagnosis and evaluation
Better quality of blood pressure measurements through endorsed protocols and Structure
certified and validated blood pressure monitors The report is built around the concept of lifetime risk
Measurement quality starting with the entire population from conception.
Development of subclinical and sometimes clinical
Better identification of people at high risk to optimise treatment approaches cardiovascular disease (figure 2) corresponds with
through endorsed education of patients and health-care professionals (linked to
stratified treatment approaches) lifetime exposure to cardiovascular risk factors combined
Empowerment with the susceptibility of individuals to the harmful
consequences of these risk factors. During the course of
Better identification of people with secondary hypertension through endorsed and
simple flow charts (linked to stratified treatment approaches) life, intervention is possible at different stages (figure 3),
with primordial (before any risk factor elevation),
Secondary hypertension primary, or secondary prevention strategies, on an
individual or population level, through environmental
Pharmacological prevention and monitoring
changes, lifestyle changes, pharmacological treatment,
Expand the workforce engaged in the management of blood pressure through or a combination of these approaches. On the basis of
task sharing and the use of endorsed education of community health workers
(linked to health-care system accountability)
available evidence and future potential, we suggest new
Workforce expansion strategies for programme-oriented, system-oriented, and
research-oriented actions. The Lancet Commission
Universal access to affordable, high-quality, and effective antihypertensive drugs
through collaboration between all major stakeholders
recognises the importance of other cardiovascular risk
factors such as smoking, obesity, dyslipidaemia, and
Medication access diabetes mellitus on cardiovascular risk, which are very
Treatment approaches stratified according to age, cardiovascular risk, social, cultural,
important to take into account for initiation and goals of
and ethnic differences through endorsed education of health-care professionals and antihypertensive treatment. However, as a Commission
initiation of new research on hypertension, this report focuses primarily on issues
Standardised treatment
and actions related to elevated blood pressure.
Nevertheless, many of the identified problems and
Blood pressure and health-care systems
suggested actions are relevant for these other risk factors
Promote and ensure capacity and accountability of the health system to conduct as well.
surveillance and monitoring, and respond appropriately to blood pressure levels
Different types of research methodology are needed to
Health-system strengthening guide action. The use of randomised controlled trials is
feasible in high-risk populations in which studies of short
Figure 1: Key actions duration and relatively small cohort size allow for the
assessment of statistically relevant outcomes, but not in
Aim relatively healthy populations in which long duration and
Medicine at University Hospital
of Pennsylvania and Veteran’s The Lancet Commission on hypertension aims to identify large sample sizes are needed to observe the outcomes of
Administration, PA, USA key actions to improve management of blood pressure at interest.
(J A Chirinos PhD); Faculty of both the population and the individual level (figure 1), and We list ten mutually additive and synergistic key actions
Medicine, Eduardo Mondlane
generate a campaign to adopt the suggested actions at directed towards ten identified essential goals, divided
University, Maputo,
Mozambique national levels to reduce the effect of elevated blood into four categories bridging public health, health-care
(A Damasceno PhD); Christian pressure worldwide. The first step of the work of the Lancet systems, and clinical practice (figure 1). The Commission
Delles: Institute of Commission on hypertension consists of this report, deliberately has not ordered these key actions by priority,
Cardiovascular and Medical
which briefly reviews the current evidence for prevention, because they are complementary and the balance between
Sciences, University of Glasgow,
Glasgow, UK (Prof C Delles MD); diagnosis, evaluation, and treatment of elevated strength of evidence and potential benefit is yet to be
INSERM, UMR970, blood pressure, hypertension, and its cardiovascular determined and varies based on country context.
2666 www.thelancet.com Vol 388 November 26, 2016
The Lancet Commissions
Definition of hypertension Health–disease continuum
Because the relationship between blood pressure and Early vascular ageing Average lifecourse
More individualised strategies
organ damage Loss of QOL
cardiovascular risk is a continuum throughout the
Elevated BP Subclinical target- CV disease
(eg, absolute risk-based)
commonly observed range, there is no biological rationale
to define a threshold from which normal blood pressure Avoidable threshold 3:
turns into hypertension. The definition of hypertension as development of clinical disease
a disease entity is relevant mainly for the initiation or
change of treatment. However, the prognostic benefit of
blood pressure reduction is dependent on both the overall Avoidable threshold 2:
development of subclinical
cardiovascular risk of the patient and perhaps also how target-organ damage
the reduction is accomplished. Therefore, initiation of
Population-based strategies
treatment is dictated by an individual’s risk profile and set
of comorbidities (ie, assessed cardiovascular risk) and the Ideal lifecourse
Avoidable threshold 1:
development of elevated BP
level of blood pressure above which there is clear evidence
Healthy
that treatment will improve prognosis.
Therefore, the Commission defines individuals as having
hypertension when they persistently cross the blood Lifecourse
pressure threshold above which there is robust scientific Childhood Early adulthood Middle-age Advanced age Elderly (>80 years)
evidence that antihypertensive treatment will improve their
prognosis. Generally—particularly if the cardiovascular Figure 2: The lifecourse approach to management of elevated blood pressure
The figure shows three lifecourse trajectories of health and disease: the average lifecourse of individuals with early
risk of the individual is unknown—this threshold will be
vascular ageing, the average lifecourse in general, and the ideal lifecourse. Preventive efforts should be focused on
the traditional cutoff values of 140 mm Hg systolic, three avoidable thresholds, with the goal (small arrows) to improve lifecourse trajectory as much as possible.
90 mm Hg diastolic, or both. However, in some groups of CV=cardiovascular. QOL=quality of life. BP=blood pressure.
individuals, other values are possible. Specifically, growing
evidence from antihypertensive trials suggests that many approach is based on the need to consider early lifetime Paris-Cardiovascular
individuals at high risk or with particular comorbidities programming, long-term benefits, and changing ResearchCenter, F-75015, Paris,
France (Prof A-P Gimenez-
should have different hypertension thresholds, as in priorities with ageing.
Roqueplo PhD); Paris Descartes
patients with type 2 diabetes.1 However, among individuals A large body of evidence suggests that up to 80% of University, F-75006, Paris,
at low risk, the support for targets below 160 mm Hg cardiovascular disease can be prevented through a healthy France
systolic, 100 mm Hg diastolic, or both, are primarily based lifestyle (sufficient physical activity, avoidance of obesity, (Prof A-P Gimenez-Roqueplo);
Assistance Publique-Hôpitaux
on epidemiological data, which cannot directly be translated moderate alcohol intake, healthy diet, and no tobacco or de Paris, Hôpital Européen
into evidence for pharmacological treatment. Inherently, drug use).5 This finding has been consistently replicated Georges Pompidou,
the threshold used to define hypertension is very likely to even when the definition of a healthy lifestyle is narrowed Department of Genetics,
be a shifting point of reference driven by emerging or expanded to use different components such as F-75015, Paris, France
(Prof A-P Gimenez-Roqueplo);
evidence, whereas the thresholds for treatment initiation sufficient sleep duration.6 Importantly, this evidence is The University of Western
and goals are likely to shift even more due to differences in derived from epidemiological surveys that query an Australia—Royal Perth
resource availability and individual preferences. individual’s habitual behaviour (or attitude), and the Hospital, Perth, WA, Australia
Independent of how hypertension is defined, the observed benefits thus result from the cumulative effects (D Hering PhD); Direccion de
Investigaciones, FOSCAL and
prevalence of hypertension is strongly influenced by two of health behaviour over an individual’s lifetime, not a Instituto de Investigaciones
opposite directed factors. On the one hand, age-specific change in lifestyle. However, it is important to emphasise MASIRA, Facultad de Medicina,
blood pressure levels in high-income (and increasingly that lifestyle is heavily influenced by socioeconomic Universidad de Santander,
middle-income) countries are falling beyond what can be factors, and therefore healthy lifestyles are not always Bucaramanga, Colombia
(Prof P López-Jaramillo PhD);
explained by improved detection and treatment of available to all individuals, communities, or populations. Hypertension Clinic, Internal
hypertension, but might partly be accounted for by The Commission finds it likely that exposure to Medicine, Hospital Clinico,
improvements in early-life health and nutrition.2,3 On the cardiovascular risk factors in childhood or even during University of Valencia, Valencia,
other hand, this positive effect is partly counteracted by the fetal life promotes the development of vascular changes Spain (F Martinez PhD); The
George Institute for Global
ageing of the population worldwide, leading to an increase that launch the individual more towards the trajectory of Health, University of Sydney,
in the prevalence of hypertension among low-income and so-called early vascular ageing, in which an accumulation Sydney, NSW, Australia
middle-income countries.4 Because of the force of ageing, of (still subclinical) vascular damage occurs already in (Prof V Perkovic PhD);
Department of Cardiology,
even a marginal additional effect on blood pressure trends early adulthood. In the Young Finns Study, risk factor
Ghent University and
will have very large health benefits globally, especially in load (defined as extreme quintiles for LDL cholesterol, Biobanking & Cardiovascular
low-income and middle-income countries.2 HDL cholesterol, systolic blood pressure, body-mass Epidemiology, Ghent
index [BMI], and smoking) at age 3–18 years predicted University Hospital, Ghent,
Belgium (E R Rietzschel PhD);
Lifecourse approach intima-media thickening,7 increased arterial pulse wave
Department of Internal
Throughout this report, the Commission tackles velocity,8 elevated blood pressure,9 and loss of carotid Medicine, University of Perugia,
prevention and treatment of elevated blood pressure with distensibility10 on re-examination 21 years later in early Terni University Hospital, Terni,
a lifecourse approach. The evidence underpinning this adulthood (age 24–39 years). In this same cohort, more Italy (G Schillaci MD); Medical
www.thelancet.com Vol 388 November 26, 2016 2667
The Lancet Commissions
Health–disease continuum
basis of epidemiological data, and by more than 45% on
Early vascular ageing Average lifecourse the basis of modelling with genetic data.5,14 The much-
organ damage Loss of QOL
Subclinical target- CV disease
lower benefit found in trials, probably related to off-target
Late preventive effort effects and poor adherence to therapy, underlines the
importance that this type of evidence demonstrates net
Health–disease
and epigenetic imprinting
Early lifecourse variability
clinical benefit. Furthermore, all these expectations are
(Influenced by maternal
continuum
influenced by genetics
Gain in disease progression
Early preventive effort based on the assumption that the relationship between
health)
Gain in time blood pressure and outcome is exponential, although
some data suggest a U-shaped association.15,16
Lifecourse Prevention of functional impairment at older ages is
Elevated BP
Birth
also important. In individuals older than 75 years, in
whom multiple diseases (primarily cardiovascular) co-
Ideal lifecourse exist, a lifecourse approach will be aimed at preservation
of functional reserve, slowing disease progression, and
mitigating complications to optimise quality of life, with
Healthy
the potential to decrease the demand on the health-
Lifecourse care system.17
Childhood Early adulthood Middle-age Advanced age Elderly (>80 years) Arterial ageing has a complex relationship with increased
blood pressure and cardiovascular risk, acting as a marker,
Figure 3: Early-life effects and impact of preventive efforts in the management of elevated blood pressure an outcome, and a driver (figures 2, 3). As shown in the
The insert shows the effects of genetic susceptibility and epigenetic imprinting during fetal life. Preventive efforts
result in downward shifts in the lifecourse curve, with earlier preventive efforts affecting lifecourse trajectory more
lifecourse approach in figure 2, there are three avoidable
than later preventive efforts. CV=cardiovascular. QOL=quality of life. BP=blood pressure. thresholds on which preventive efforts should be focused:
the development of elevated blood pressure, development
Research Council Unit on leisure-time physical activity in childhood was associated of subclinical cardiovascular damage, and, finally, the
Hypertension and with better carotid artery elasticity later in life,10 whereas development of overt cardiovascular disease leading to
Cardiovascular Disease,
an improvement in risk factor profile between youth and physical and cognitive disability, loss of autonomy, and loss
Hypertension in Africa Research
Team (HART), North-West adulthood slowed the progression of subclinical of quality of life. Some individuals with early vascular ageing
University, Potchefstroom, cardiovascular damage. Confirmatory findings were (red line) will cross these thresholds earlier in life. The
South Africa reported in the CARDIA and AGHALS cohorts.11,12 optimum or ideal lifecourse (green line) represents
(Prof A E Schutte PhD);
Hypertension Center,
In terms of genetic evidence, findings from several large- individuals who only develop elevated blood pressure or
Hypertension and Nephrology scale studies13 have clearly shown that the random subclinical cardiovascular damage, but too late in the
Unit, Department of Medicien, allocation of blood-pressure-related genetic variants (single lifecourse to substantially affect quality of life. The main
Policlinico Tor Vergata, Rome, nucleotide polymorphisms) is associated with a difference goal of preventive efforts (small grey arrows) is to shift an
Italy (A Scuteri PhD); Menzies
Institute for Medical Research,
in both blood pressure and cardiovascular outcome. individual’s lifecourse towards the ideal lifecourse. The
University of Tasmania, Hobart, Within the context of a lifecourse approach, the effect of a dashed endings of the lifecourse lines (specifically the ideal
TAS, Australia genetic variant on blood pressure seems to increase with lifecourse) are there to underscore that the goal of prevention
(J E Sharman PhD); Department ageing, suggesting a lifecourse effect of accelerated is not necessarily avoidance of ever developing cardio
of Cardiology, Division of
Cardiovascular and Pulmonary
ageing.14 Although lifestyle changes typically induce rather vascular disease, but avoidance of premature cardiovascular
Diseases Oslo University small reductions in blood pressure, they affect the large disease. Furthermore, there is always uncertainty at the end
Hospital, Oslo, Norway low-risk population and can act over decades, having the of life, and an individual on the ideal lifecourse can still
(K Wachtell DMSc); and potential to improve cardiovascular outcome on a suddenly develop cardiovascular disease. Depending upon
The Shanghai Institute of
Hypertension, RuiJin Hospital,
population level. By contrast, randomised controlled trials genetic disposition and/or epigenetic imprinting during
Shanghai Jiaotong University are typically designed to test large effects, in sick or high- fetal life, individuals can start their lifecourse higher or
School of Medicine, Shanghai, risk populations over a few years. In this sense, genetic lower on the health–disease continuum (the enlarged
China (Prof J Guang Wang PhD) studies are highly informative because they provide insert), reflecting the so-called cohort effect. The orange
Correspondence to: information about the effect of small variations in blood dashed lines show the impact of a preventive effort, with a
Mr Michael H Olsen,
Smedelundsgade 60,
pressure in the general population, in a fashion that is resultant downward shift in the lifecourse curve. Early
4300 Holbæk, Denmark randomly allocated and blinded to the individual preventive efforts are likely to result in a substantial gain in
mho@dadlnet.dk (who is usually unaware of their own genetic time (x-axis) or reduction in disease progression (y-axis)
predisposition), avoiding the risk of bias inherent in compared with later preventive efforts.
epidemiological studies about lifestyle changes. Thus,
natural genetic variation can hint at the effects that could Primordial, primary, and secondary prevention
be achievable with an intervention, provided it is both long The goal of primordial prevention is to maintain the state
term and free from off-target (ie, unwanted) effects. A of cardiovascular health and optimal blood pressure,
10 mm Hg decrease in systolic blood pressure is expected leading to an ideal lifecourse maintained within the
to reduce coronary heart disease risk by 17% on the basis of healthy range from birth to end of life. This goal
data from blood-pressure-lowering trials, by 25% on the necessitates a solid population-based strategy, combining
2668 www.thelancet.com Vol 388 November 26, 2016
The Lancet Commissions
policy and environmental change, behavioural (ie, East Asia Laos STEPS 2013
lifestyle) incentives, education, and community-level and Pacific
Cambodia STEPS 2010
actions aimed at minimising the risk factor burden for the Mongolia STEPS 2013
population at large. Because these actions are not Europe and Albania DHS 2008–09
individualised (ie, individually tailored), the Commission central Asia Armenia DHS 2005
Moldova STEPS 2013
defines these actions as population based although they
Azerbaijan DHS 2006
reach individuals. Primary prevention (preventive actions Uzbekistan STEPS 2014
after hypertension is diagnosed) aims to avoid Ukraine DHS 2007
cardiovascular complications. Secondary prevention (after Kyrgyzstan DHS 2012
subclinical end-organ damage or overt cardiovascular Latin America and Caribbean Peru DHS 2012
Middle East and Egypt DHS 2008
disease develops) aims to avoid further cardiovascular north Africa Qater STEPS 2012
damage, cardiovascular events, and reduction in quality of South Asia Bhutan STEPS 2014
life. By contrast with primordial prevention, these Nepal STEPS 2013
Bangladesh DHS 2011
preventive actions are generally driven by an individual’s Sub-Saharan Malawi STEPS 2009
absolute risk. This approach necessitates a well Africa Tanzania STEPS 2012
functioning health system with the capacity to readily Togo STEPS 2010
Benin DHS 2011–12
detect individuals whose risk or blood pressure surpasses Namibia DHS 2013
a specific risk threshold for which a more individualised, Lesotho DHS 2009–10
clinical (often drug-based) approach is indicated, and to 0 20 40 60 80 100
Percentage of adults
deliver this strategy superimposed on ongoing lifestyle
interventions. Not aware Not on medication
On medication, blood pressure not controlled On medication, blood pressure controlled
Policy makers, health-care systems, the pharmaceutical
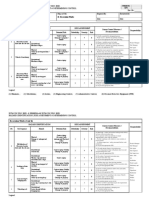
and food industries, and civil society are responsible for Figure 4: Adults with raised blood pressure or on medication for hypertension disaggregated by diagnosis
creating a healthy environment that removes barriers to and treatment status
STEPS=WHO STEPwise approach to surveillance. DHS=Demographic and Health Survey.
health and empowers populations to practise healthy
behaviours.
closely associated with different birth cohorts and mean
Summary of essential goals and key actions age of the population, it is a largely preventable condition
Previous action plans to improve prevention and caused by lifestyles increasingly characterised by
management of elevated blood pressure and hypertension reduced physical activity, unhealthy diet, overweight,
have not yet had global impact. We identified several and obesity,21–24 together with a poorly understood
achievable goals and accompanying actions that, if genetically influenced susceptibility to cardiovascular
implemented effectively and broadly, will make substantial risk factors. Social determinants of health such as
contributions to improve outcomes related to elevated socioeconomic disadvantage early in life drive related
blood pressure worldwide. Recognising the inequitable inequities in the burden of hypertension, morbidity, and
distribution of financial and other resources across and premature death in specific populations.4
within countries and regions, the Commission has further Despite blood pressure measurements in more than
classified the goals and actions appropriate at two different 150 national population-based surveys in 97 countries,
levels. We denote as essential those actions recommended no fully reliable global or regional estimates of
to be undertaken in all countries and regions, irrespective hypertension treatment coverage exist. Figure 4 shows
of income levels; the remaining actions are those that the distribution of diagnosis and control of raised blood
should be undertaken when additional resources permit. pressure in national surveys in selected countries that
are not part of the Organization for Economic Co-
The global perspective operation and Development. In most of these surveys,
Size of the problem at least half of adults with raised blood pressure had not
Because hypertension rarely causes symptoms in the been diagnosed with hypertension. Treatment coverage
early stages, it is a silent killer, causing accelerated is therefore low, ranging from 7% to 61% among people
atherosclerosis, damage to major organs, disability, and who had presented with raised blood pressure in the
death from cardiovascular disease.18 Approximately one household surveys (figure 5). Effective coverage is
in four adults have hypertension (when defined as blood considerably lower than total coverage, ranging from
pressure greater than 140 mm Hg systolic or 90 mm Hg 1% to 31%. Data from 11 national Demographics and
diastolic) and by 2025, hypertension is projected to affect Health Surveys disaggregated by wealth quintile
more than 1·5 billion people worldwide.19 In recent suggest that coverage of hypertension treatment differs
decades, there has been an epidemiological shift in the substantially across wealth quintiles in some but not all
main cause of global disease burden from communicable countries (figure 5).25 A consistent association between
to non-communicable disease, with hypertension being wealth and coverage is observed in Bangladesh, Benin,
the leading risk factor.20 Although blood pressure is Egypt, Namibia, and Peru. In nine of the 11 countries,
www.thelancet.com Vol 388 November 26, 2016 2669
The Lancet Commissions
Europe and
30 years, and the number of cases among those aged
Albania 2008–09
central Asia 75–84 years is estimated to double in the same period.37
Armenia 2005 Thus, age-related factors such as increased prevalence of
Azerbaijan 2006 type 2 diabetes and other cardiovascular risk factors
Kyrgyzstan 2012 should be considered within hypertension treatment
Ukraine 2007 plans for the future. Furthermore, it is important to realise
Latin America that successful prevention does not necessarily avoid
and Caribbean Peru 2012
Middle East and
events, but usually delays them until a later time.
Egypt 2008
north Africa For the same elevation in blood pressure, risk of
South Asia Bangladesh 2011 cardiovascular events increases with age, and treatment of
Sub-Saharan Benin 2011–12 hypertension in elderly people is therefore of particular
Africa
Lesotho 2009–10 importance.38 Most of the earlier trials showing prognostic
Namibia 2013 benefits of antihypertensive treatment in elderly people
were done in those with systolic blood pressure of
0 10 20 30 40 50 60 70
Coverage (%) 160 mm Hg or higher (a threshold greater than that
Quintile 1 (poorest) Quintile 2 Quintile 3 Quintile 4 Quintile 5 (richest) proposed in most current guidelines). The Systolic Blood
Pressure Intervention Trial (SPRINT)39 oversampled
Figure 5: Percentage of adults with raised blood pressure or on medications for hypertension, who are individuals aged 75 years or older without diabetes or a
currently taking medications for hypertension, by wealth quintile25 history of stroke, living outside of nursing homes and
Raised blood pressure defined as systolic blood pressure greater than 140 mm Hg or diastolic blood pressure
greater than 90 mm Hg. Figure shows data for adults aged 35–59 years, except for Albania, Armenia, Kyrgyzstan, assisted living facilities, and showed benefits when
and Ukraine (age 35–29 years), and Peru (age 40–59 years). treatment was targeted to a systolic blood pressure less than
120 mm Hg compared with a target of 135–139 mm Hg.
however, the poorest adults have lower treatment These data should be interpreted against the background of
coverage than adults in the richest quintile.25 the specific blood pressure measurement in SPRINT—
Epidemiologically there is a strong dose–response which is known to result in values approximately 10 mm Hg
association between blood pressure and cardiovascular lower than with standard office measurements—but
mortality that persists to 115/75 mm Hg.26,27 Thus, a nevertheless indicate benefits of tight blood pressure control
substantial residual cardiovascular risk is present even in elderly people.1,39,40 However, attainment of low blood
in individuals with controlled hypertension.28–30 Elevated pressure targets might be associated with increased adverse
blood pressure and hypertension coexist with other risk drug reactions such as dizziness, electrolyte disturbances,
factors24 and are among the most common problems and alteration of kidney function.39,41 This finding suggests
managed by general practitioners,31 yet even among that blood pressure targets might need to be individualised,
people with treated hypertension, less than half—on particularly for elderly people, although it is also these
average—have blood pressure within well controlled individuals in whom antihypertensive treatment improves
levels.32,33 Many factors affect these unfavourable prognosis the most.39,42
statistics including poor adoption of recommended
lifestyle changes and low adherence to recommended Early vascular ageing and subclinical cardiovascular
pharmacological antihypertensive treatment, to name damage
but a few. There is a major need for change, and the goal Hypertension is a systemic condition affecting the whole
of this Commission is to generate a global campaign to vasculature. In rat models of hypertension, capillary
implement priority actions to prevent elevated blood rarefaction has been found to precede the development
pressure and improve the management of hypertension.34 of hypertension43,44 and microvascular changes such as
The Commission therefore examines why the detection capillary thinning are also characteristic of human
of blood pressure is low, why blood pressure control hypertension.45 On a functional level, the ability of the
remains suboptimal, and how both can be improved. endothelium to regulate vascular tone is altered during
the development of hypertension, partly due to increased
Effect of age on risk factors and treatment goals release of reactive oxygen species and reduced availability
The average age of the world population has increased in of endothelium-derived nitric oxide.46 In human beings,
recent decades, contributing to hypertension increasing in arterial stiffening precedes hypertension.47 At the same
importance relative to other risk factors.20,35 The number of time, high blood pressure causes damage to large and
Europeans older than 65 years is predicted to double small arteries, leading to further endothelial dysfunction,
during the next 50 years to about 150 million, and in reduced vascular compliance, increased vascular
roughly the same period people older than 90 years are stiffness, reduced lumen diameter, and formation of
expected to constitute roughly 12% of elderly people in atherosclerotic plaques.48 From a clinical perspective
Europe (up from 0·5% of the US population in 200036), (and, in part, irrespective of whether they are cause or
increasing the prevalence of hypertension. Cardiovascular consequence), hypertension is clearly associated with
diseases are projected to increase by a quarter in the next changes in vascular function and structure that are more
2670 www.thelancet.com Vol 388 November 26, 2016
The Lancet Commissions
pronounced than the changes that would be expected as the context of improved national indicators, and have
part of a normal ageing process. This process is referred been observed in countries of all income levels. For
to as early vascular ageing.49 example, in the USA, although hypertension control
Findings from clinical studies have shown that improved for the population overall between
subclinical vascular damage is associated with adverse 1999 and 2012,57,58 substantial differences between black
outcome. For example, increased vascular stiffness is a populations and white populations in control of blood
predictor of cardiovascular events and all-cause mortality pressure have been reported.59,60 Within New York City,
independent of traditional cardiovascular risk factors.50,51 geocoded population surveys shows that lower-income
The availability of devices and techniques to non- neighbourhoods have higher prevalence of hypertension
invasively assess subclinical changes in vascular than wealthier neighbourhoods.61 Although proximate
structure and function has fuelled interest in vasculature and modifiable causes of hypertension include exposure
properties as a surrogate marker of cardiovascular risk. to factors such as poor diet, excessive alcohol intake, and
This approach is attractive because it would shift clinical physical inactivity, social factors such as education,
practice from the current concept of disease based on income, social norms, and attitudes (eg, racism and
risk factors towards a more precise assessment of an discrimination) are associated with health inequities
individual’s position on the cardiovascular continuum.52 including in hypertension.62,63
An individual’s vascular phenotype would be the result of During the past two decades, age-standardised
the combined action of all known and unknown risk mortality from cardiovascular disease has improved
factors and provide a personalised assessment of vascular within urban environments in high-income countries,
(and cardiac) risk. which might have resulted from improved access
However, although guidelines agree that some to medical care64 and the availability of healthier
assessment of target-organ damage is required as part of food options, smoke-free spaces, and access to
the clinical assessment of patients with hypertension, the opportunities for other healthier lifestyle options. In low-
current evidence only supports rather crude and late income and middle-income countries, however, rapid
measures such as albuminuria or assessment of left urbanisation is increasing population exposure to
ventricular hypertrophy.1,53,54 When more detailed assess- environments that are associated with a higher
ment of vascular function and structure is mentioned in prevalence of hypertension than rural environments.33,56
guidelines, the recommendations remain vague and not Factors that contribute to increased blood pressure in
binding.1 This lack of detail is related to the fact that the cities include more sedentary work life, increased use of
usefulness of assessments of subclinical vascular damage inactive transportation modes (such as driving or use of
to guide therapy, even if it were affordable, remains escalators), and intake of more calorie-dense and
unproven.55 The potential of vascular phenotyping has not nutrient-poor processed foods compared with rural
yet been sufficiently exploited and definitive clinical environments.64 Furthermore, inadequate financing and
studies to define the role of subclinical organ damage in development of the primary health-care system in low-
the definition of individual patients’ risk and subsequent income and middle-income countries often leaves
treatment are needed. disease and risk factors undetected and poorly managed.
Primary health-care centres in low-income and middle-
Different situations around the world income countries are often inadequately equipped with
About 80% of all cardiovascular mortality occurs in basic diagnostic tools, and health-care providers cannot
low-income and middle-income countries, where the match the demands for improved identification of
greatest burden of hypertension is observed.35 Although patients with hypertension and for more aggressive
there has been a trend towards reduction in mean systolic treatment of the condition.
blood pressure among adults in Europe, Australia, and A common theme associated with prevention of disease
North America between 1980 and 2008, systolic blood and promotion of health is to create environments that
pressure increases have been observed in low-income and make physical activity and healthy diets easily accessible,
middle-income countries.20 WHO estimates that the for example by building segregated bicycle infrastructure
prevalence of hypertension is highest in Africa (46% of and implementing systems to ensure a range of affordable
adults older than 25 years), 35% in North and South fresh fruit and vegetables in urban areas. Universal access
America together, and 40% in the rest of the world,18 with to health-care services and low-cost, high-quality
extremely low levels of awareness and control.56 However, medications makes diagnosis, treatment, and control
reliable data about frequency, rate of control, and efficacy more likely. By contrast, in environments that deter these
of interventions are not known, especially in low-income activities (for example, communities where roads are
and middle-income countries. unsafe for pedestrian traffic, where healthy foods are
In addition to geographical differences, stark disparities unavailable to purchase, or where health-care facilities or
exist within countries between specific populations and health insurance are inadequate), individuals become
local areas, with marked socioeconomic differences. disempowered to make healthy choices, resulting in less
These differences have evolved or persisted even within healthy behaviours and populations.
www.thelancet.com Vol 388 November 26, 2016 2671
The Lancet Commissions
Hypertension in the years to come and technological obtained in individuals who have not yet entered clinical
developments care and have no immediately detectable risk but might
The steady increase in the prevalence of hypertension be on a trajectory for high blood pressure on the basis of
during recent decades seems likely to continue, especially existing epidemiological trends, as well as those at high
in low-income countries. This growth has also led to risk or with existing disease.
substantial increases in mortality and morbidity due to Improvements in the prevention of blood-pressure-
suboptimal blood pressure, which is also likely to related disease will be achieved not only by better clinical
continue. The estimated number of blood-pressure- treatment strategies for people already receiving
related deaths yearly has increased by 49% to 10·4 million blood-pressure-lowering therapy, but also through system-
in 2013, and the number of disability-adjusted life-years based strategies that ensure low blood pressure levels
has increased by 45%.65 Most of this increase has probably across populations; up to half of blood-pressure-related
occurred in low-income and middle-income countries. morbidity occurs in people with a systolic blood pressure
As a result of increases in population, ageing, urban- less than 140 mm Hg.67,72 Furthermore, the strongest risk
isation, and obesity, the number of people with factor for development of hypertension is a blood pressure
hypertension can be expected to increase in low-income just below the cutoff value for hypertension—also referred
countries and some middle-income countries if not to as prehypertension. Successful population-based
counteracted by concerted action. However, in high- strategies will therefore reduce the risk for people at all
income countries, age-adjusted blood pressure is blood pressure levels, preventing incident hypertension,
decreasing, thereby mitigating the effect of the ageing delaying disease onset, and reducing risk in patients with
population on the prevalence of hypertension. It is, existing disease. Tackling this large group should be at the
therefore, clear that not only prevention and detection forefront of preventive efforts, because a substantial part
but also treatment and control of hypertension should be of blood-pressure-related disease burden originates from
top priorities that are currently not well addressed. this nominally normotensive group.67
The impact of hypertension can be reduced Despite this knowledge, the largest proportion of
through existing strategies.66,67 Cost-effective models of funding and research activities is still projected towards
interventions appropriate to use in countries with few individual pharmacological and device-based treatment,
resources have been suggested,68 and would be expected such as the best combinations of antihypertensive therapy
to reduce the global burden of non-communicable disease or new strategies to treat resistant hypertension. But within
(such as cardiovascular disease induced by high blood the global context, most individuals with hypertension are
pressure) if implemented in countries of any income still unaware of their blood pressure. This discrepancy was
level.69 The emergence and rapidly growing uptake of evident in the Prospective Urban Rural Epidemiology
technological innovations offer further opportunities to study,33 which examined hypertension prevalence,
use these tools to improve outcomes. This Commission awareness, treatment, and control figures among
proposes several strategies to lower the global burden 142 042 individuals from low-income, middle-income, and
of blood-pressure-related disease in the future high-income countries. The largest proportion of
through the better use of advanced technologies and hypertensive individuals (53·5%) were unaware of their
systems to improve individual characterisation, enhance hypertension status, and of those with hypertension, only
population-level empowerment, and strongly address 13% were controlled (figure 6)—findings consistent with
prevention across the lifecourse. other global, regional, and national studies. The questions
to be answered are why is detection so low, why is control
Prevention: lifestyle and environmental changes suboptimal, and how can these factors be improved?
Current evidence, problems, and perspectives The answers must be found through focused research.
It is striking that all blood pressure guidelines1,53,70 agree How could we target the global population with
that individual lifestyle modification is the cornerstone of hypertension (including those who are still unaware of their
prevention and is the first line of treatment. However, cardiovascular risk), those who are prehypertensive
two important challenges emerge in terms of clinical (and, therefore, have increased risk but are not targeted
hypertension guidelines. First, the guidelines are written for pharmacology intervention), and those who
mostly by clinicians, such as cardiologists and are normotensive? Individual-based pharmacological
nephrologists with training and experience in the clinical approaches in patients with hypertension are evidence
management of hypertension and cardiovascular disease, based and should be enforced. However, considering that
who therefore focus on individual patient recom- the cardiovascular risk attributable to blood pressure is a
mendations. Second, hypertension treatment guidelines continuum, the most effective solution is probably to reduce
are designed for patients already diagnosed with blood pressure in the population as a whole, although
hypertension, although individual lifestyle modifications neither the beneficial effect of this strategy or the suggested
are often not achieved despite robust evidence for the ways to accomplish it are strictly evidence based. These two
effectiveness of a healthy lifestyle to lower blood very different approaches are complementary and might—
pressure.71 Substantial community-wide benefits can be if used together—increase the chance of success.
2672 www.thelancet.com Vol 388 November 26, 2016
The Lancet Commissions
Effective incorporation of population-based approaches
is embedded in the Open Working Group on Sustainable
Development Goals endorsed by the UN General
Assembly.73 One of the 17 Sustainable Development Goals
is to “ensure healthy lives and promote well-being for all at
all ages”. Included in this goal is a target to reduce
premature mortality from non-communicable diseases by
33% by 2030, through prevention, treatment, and
promotion of mental health and wellbeing, thereby
extending the previous target of 25% reduction in
premature mortality from non-communicable diseases by
2025. Several of the non-communicable disease global
targets fit precisely within the sphere of primordial and
primary prevention, referring to specific targets for alcohol
use, physical activity, salt intake, tobacco use, and obesity.74
Many of these factors can be addressed on a population
level by governments taking action to develop the Normotensive Hypertensive Unaware Aware No Treated, blood Treated, blood
appropriate social and economic environments that and treatment pressure pressure
prehypertensive uncontrolled controlled
would support the creation of communities where
healthy choices are easy and readily available (such as
tobacco legislation75,76). Such environments will inherently
shape the health behaviours of larger populations by Figure 6: Awareness of hypertension status
encouraging individuals within those communities to In the PURE study,33 most (53·5%) individuals with hypertension were unaware of their hypertensive status,
and only 13% had well controlled blood pressure.
take up healthy behaviour, actively participate in physical
activity, or choose to cook healthy meals at home, with
much greater chance of success than stand-alone Evidence-based health behaviours
interventions targeted at individual patients. Substantial evidence supports the effectiveness of
The global prevalence of obesity and diabetes specific health behaviours to improve blood pressure,
underscores the need for effective prevention in cardiovascular morbidity, and mortality. In terms of
high-income countries77–79 as well as in the many middle- dietary intake, extensive evidence supports the beneficial
income countries that now have high obesity levels.80 It effects of the Mediterranean diet (with extra virgin olive
is important to introduce such interventions in low- oil or nuts)84–86 and Dietary Approaches to Stop
income and middle-income countries,81 where tobacco Hypertension (DASH) diet,87,88 as well as a reduction in
and alcohol use, poor nutrition,82 and subsequent salt intake16,89,90 and increased potassium intake.91
obesity are increasing.83 However, low-income countries Significant blood-pressure-lowering effects have been
are often challenged with the dual epidemics of non- shown for dietary nitrate (found in beetroot juice and
communicable and communicable diseases, which green leafy vegetables).92–94 Convincing evidence also
continue placing excessive financial burden on their supports cardiovascular protection by physical activity
health systems. Wide promotion and availability of and improved fitness,95–99 weight loss,100–102 tobacco
unhealthy diets, including processed foods and sugar- cessation,103,104 moderate105 to limited alcohol intake,106,107
sweetened beverages that are affordable and easily and management of psychosocial stress.108,109 Importantly,
available, can hardly be counteracted by individual not only do these preventive measures improve blood
promotion of healthy lifestyle by health-care pressure and cardiovascular outcome, but also most have
practitioners alone. Policy interventions to make healthy multiple cross-cutting benefits, resulting in prevention
choices easier will enable and drive these broader—and of non-communicable diseases in general. For example,
more sustainable—population-wide changes. They will lifestyle modification can be more effective than
require governments to carefully consider the long-term metformin to prevent type 2 diabetes.110
and short-term effects of decisions related to the The effects of some interventions on hard cardiovascular
social, economic, food, and physical environments, and endpoints have not yet been formally tested to date in
support evidence-informed approaches to creating adequately powered randomised trials. However, a large
health-promoting environments—for example, by en- trial assessing the effects of reducing sodium intake on
couraging the production and promotion of healthy stroke is underway in China (the China Salt Substitute
foods, differential taxation approaches, and enforced and Stroke Study; NCT02092090). Similar cluster-based
clearer labelling, in a similar way to that achieved with methods could allow evidence to be generated for other
tobacco. Translating successes and embracing new lifestyle interventions.110 Although debate continues in the
and stronger actions to change current directions absence of these types of outcome data, overall the blood
is necessary. pressure benefits achieved by lifestyle modification are
www.thelancet.com Vol 388 November 26, 2016 2673
The Lancet Commissions
expected to translate into long-term cardiovascular a low-risk lifestyle, the risk of observed stroke would be
benefits that will outweigh any putative associated risks. reduced by 62% and the risk of observed myocardial
The major challenge is to achieve sustainable changes infarction would be reduced by 79%. Evidence shows
in lifestyle and behaviour, especially when making use of that specific health behaviours such as tobacco
individual-based approaches. Sustainability has proven cessation,103 increased physical activity,95,96,98,99 reduction of
difficult with clinical approaches, which require overweight,100–102 and a healthy diet121,122 can reduce blood
substantial resources over a long period of time, and pressure and cardiovascular events. However, only 1% of
therefore are only applicable to very high-risk individuals. the Swedish population was leading a low-risk lifestyle.120
Additionally, the effects of clinical lifestyle interventions Therefore, a different strategy which does not focus on
do not persist.111 Finally, engagement and motivation of the individual is necessary.
individuals across populations is not feasible with high- To improve population cardiovascular health,
resource approaches. These problems might partly several approaches are suggested: (1) health-promoting
explain why these preventive measures have not been environments are essential, and require strong
successfully scaled at a global level. leadership of an organisation with global reach—such as
Hence, the conclusion of this report is to focus on the UN—and intense involvement from multiple
population-based strategies that involve broad public- stakeholders;123 (2) according to WHO, an effective
health and systems approaches. However, among school health programme can be one of the most cost-
individual-based approaches, some strategies could be effective investments a nation can make to simul-
worth undertaking. An important first step to mobilising taneously improve education and health.124 Health
population-wide action is probably awareness, as shown education—continuing through the lifecourse as
by findings from the PURE study.33 A global initiative will cardiovascular risk increases and hypertension begins to
be required to achieve this goal. Emerging technologies develop—would improve health literacy at all ages
using novel approaches include mobile technology, (figure 2) and increase awareness and detection of
where the findings from the Tobacco, Exercise and Diet hypertension. It will require the combined efforts of
Messages trial112 demonstrated that advice, reminders, governments, teachers, and communities; (3) technology
and support through text messaging effectively reduced can indirectly improve population blood pressure by
systolic blood pressure, LDL cholesterol, BMI, and ensuring the availability of healthy foods such as fruit
smoking, and increased physical activity. A systematic and vegetables throughout the year to wider communities
review113 further indicated that text messaging approaches and by increasing physical activity. Refrigerators can
more than doubled the odds of medication adherence, increase the availability of fresh foods and simultaneously
but long-standing effects have not yet been tested. In reduce the use of potentially harmful additives, such as
terms of health literacy, the medical community has the sodium nitrate. The videogaming industry,125 wearable
responsibility of training the trainers—ensuring quality technology (eg, fitness bands), and social media can
and consistency of the health education curriculum in increase physical activity and general knowledge about
schools—but cannot be the primary vector to deliver the healthy behaviours; (4) wider implementation of
message on a sufficiently large scale. Patient empower- successful governmental actions including smoke-free
ment could be one strategy that substantially improves policies,75,76 marketing of foods and alcohol (eg, the
adherence and thereby probably improves outcomes. banning of adverts for alcohol126 or unhealthy foods127,128),
Alternative and promising approaches include peer- sin taxes (eg, sugar taxes),129,130 and regulation of the
group interventions based on elements of social cognitive sodium content of processed foods; (5) owing to
theory,114 and disclosure of a genetic risk score, where population diversity (cultural and social environments),
preliminary results suggest that this knowledge can be a unique approaches might be necessary to ensure
positive driver to act on other modifiable risk factors.115 successful acceptable population activities.131,132 Further-
Unfortunately, the limitations of individual-based more, the global health environment is constantly
approaches in achieving behavioural change at a changing, and traditional cardiovascular risk assessment
population level are highlighted by the worldwide obesity based on large cohorts from the early 1990s might
crisis,116 reflecting difficulties in achieving and sustaining become less effective as smoking habits decrease and
lifestyle changes in individuals. This situation is mirrored obesity increases. The additive value of new risk markers
by alarming hypertension prevalence, especially in low- (eg, arterial stiffness)133 is unclear, especially regarding
income and middle-income countries.3,117,118 It is therefore functional outcomes like cognitive impairment.134
clear that different approaches are required. Therefore, continued research is needed to develop
more effective population-based cardiovascular pre-
Population-based approaches to improve vention strategies; and (6) to empower the general
cardiovascular health population and medical community, professional
Individual approaches to long-term adherence to new societies and health-care experts should contribute to
health behaviours are far from optimal.119 Findings from clear, evidence-based recommendations that are easily
a Swedish study120 showed that if all individuals followed available on websites and apps.
2674 www.thelancet.com Vol 388 November 26, 2016
The Lancet Commissions
Salt reduction in the population the cohort effect can be explained by improvements in
Globally, average estimated salt intake is 7·5 g/day maternal health influencing fetal programming and
(sodium intake 3·0 g/day), ranging from 5·5 to 13·7 g/day changes in early-life diet.153 The precise mechanisms are
(sodium intake 2·2 to 5·5 g/day).135 More than 75 countries unknown but epigenetic changes might be one of several
have national strategies for salt reduction in place.136 possible mechanisms.154
Findings from randomised trials have demonstrated that Irrespective of the mechanism, the fetal environment is a
salt restriction from high levels leads to clear reductions in crucial determinant of hypertension and efforts should be
blood pressure.137,138 In the absence of randomised studies made to improve maternal and fetal health globally. Indeed,
on cardiovascular events, findings from observational in low-income and middle-income countries an estimated
studies89,135,139 and a long-term observational follow-up of 27% of all livebirths were small for gestational age with
the TOPH I and II trials140 have suggested that sodium approximately 15% of all births being classified as low
reduction, including to less than 2300 mg per day,89 is birthweight.155 Maternal malnutrition, smoking, alcohol
likely to translate to cardiovascular benefits, while other abuse, pre-eclampsia, and diabetes all represent possible
observational studies16,141–143 have suggested that the targets to stop fetal programming of hypertension.156
relationship between sodium excretion and cardiovascular
events might be U-shaped, because an increased risk was Summary of possible actions
observed in people with a sodium excretion less than Primordial and primary prevention of hypertension
approximately 3 g/day when estimated from a morning should be applied full circle throughout the lifecourse of
fasting urine sample. However, observational studies are populations by creating and enabling sound economic
limited by their inability to determine causality. A trial and social environments that would directly result in
assessing the effect of reducing salt intake on stroke is health-promoting environments (table 1). The cross-
underway (the China Salt Substitute and Stroke Study, cutting benefits to all non-communicable diseases are
NCT02092090) and could provide further evidence. immense, and can only be achieved by strong leadership
Additionally, data from large populations undergoing and intense cooperation between multiple stakeholders
initiatives for salt reduction (such as the UK144 and more (including governmental and non-governmental
recently South Africa, the first country to legislate organisations, food and fitness industries, educational
mandatory industry salt reduction in various processed systems, media outlets, mobile technology companies,
foods)127 will also provide longitudinal information. The and employers), with full engagement of a global body
Commission finds that further research should be such as the UN; the European Union pledge for
prioritised, including randomised controlled trials— responsible marketing of food and beverages157 to children
when feasible—and trials that help to determine the most is an example of such international leadership. We should
effective population-level sodium-reduction strategies. further improve applications of technology to strengthen
health and food monitoring systems, as well as food
Maternal health and fetal programming delivery and storage, but also use novel technology and
Fetal programming refers to the concept that environ- the mobile industry that might aid in achieving this goal.
mental conditions during pregnancy can predispose to Awareness should be emphasised throughout, including
disease during adulthood. equal basic access to validated blood pressure monitors in
A substantial body of evidence links maternal health low-income and middle-income countries. Task sharing
and the fetal environment to future health of offspring. by community health workers in these countries to
In particular, epidemiological evidence indicates that low increase awareness of hypertension is also proven to be
birthweight (defined by WHO as <2500 g) increases risk effective.158 Furthermore, celebrities might be encouraged
of developing hypertension and cardiovascular disease in to become champions in promoting healthy lifestyles and
later life.145–147 A reduced number of nephrons148,149 and creating awareness of hypertension. These approaches
abnormal vascular development150 have been proposed as can be effective, as demonstrated by the Feed Me Better
possible explanations for this relationship, although campaign introduced by celebrity chef Jamie Oliver at
the underlying mechanisms responsible for fetal schools in the UK, which achieved multiple benefits
programming towards hypertension are incompletely including improved bodyweight, micronutrient intake,
understood. Epidemiologically, blood pressure has been and better educational performance.159,160
falling in high-income countries for decades well before
major lifestyle interventions such as taxation on tobacco, Diagnosis and evaluation
promotion of physical activity, and restriction of salt Introduction to diagnosis and evaluation
intake,2,151 and the same blood pressure decline has also Improved characterisation of patients, including accurate
begun in some middle-income countries.3 The blood diagnosis, is the primary requisite to guide therapy,
pressure declines have both cohort and period effects, management, and follow-up in hypertension. A (more)
suggesting that the changing determinants are a specific diagnosis of hypertension is fundamental to tailor
combination of social changes (affecting specific cohorts) therapy (eg, non-pharmacological, drug class or classes,
and technological or structural changes.152 A large part of and dose). Failures or weaknesses in this diagnostic
www.thelancet.com Vol 388 November 26, 2016 2675
The Lancet Commissions
Goals Actions Keywords
Low awareness of hypertension Every adult should know their Ensure universal access to blood pressure measurement Measurement access
blood pressure* Tailored education about hypertension throughout the life course
Exposure to an unhealthy Maximise multisectoral Implement concerted, unified strategies and policies to accelerate socioeconomic improvements Health-promoting
environment collaboration to create and development of health-promoting environments environment
health-promoting Make healthy food choices (fruit and vegetables) easier and discourage unhealthy foods
environments* (excess calories, heavily processed foods)
Promote physical activity in daily living (active living by design) throughout the life course
Disincentivise and further regulate tobacco and alcohol
Lack of understanding regarding Universal education about Early and sustained education about new technologies that leverage healthy lifestyles Healthy behaviours
the impact of unhealthy lifestyles healthy lifestyles over the life (eg, gamification)
on hypertension course* Educate and empower health workers and teachers to instil healthy lifestyles
Align and simplify educational material
Knowledge gaps in the Resource allocation for Prioritise and produce cross-disciplinary and culturally relevant evidence to promote healthy ··
effectiveness of prevention research into action-oriented lifestyles†
programmes, policies, and use of prevention
new technologies
*Essential goals. †Related to research.
Table 1: Identified problems and corresponding goals and actions relating to prevention
process can result in inappropriate treatment, potentially mercury sphygmomanometers have been phased out of
leading to increased adverse drug reactions (particularly clinical use owing to safety concerns. New measurement
in older individuals), inappropriate discontinuation of techniques are being developed161 and mercury-free blood
therapy, greater cardiovascular risk due to poor blood pressure monitors now available include oscillatory,
pressure control, or failure to treat the right patient. aneroid, and hybrid (with a mercury-like column)
Increased availability of new technologies has led to devices. Each has specific problems in terms of
opportunities on the one hand, but to substantial maintenance and calibration, and their accuracy can be
challenges on the other. Measurement devices for blood questioned in particular settings (including among
pressure have never been so available and affordable, but patients with arrhythmia or stiff arteries). Ideally, devices
many might not be validated according to scientific should comply with the validity guidelines of scientific
standards. Many devices to investigate novel parameters societies, rather than just internal testing by the
of potential pathophysiological relevance and risk manufacturer,162 and this information should be clearly
stratification are now available. Similarly, techniques to available for the customer. Correct cuff size is important
measure different omics (circulating biomarkers) are for device accuracy. Appropriately sized cuffs for children,
now available for individuals, but the huge amount of thin individuals, and (more importantly) obese
data generated has little relevance for clinical practice at individuals are underused in medical practice,163 although
this stage. One of the main hurdles in the implementation about 40% of people with hypertension require a blood
of novel diagnostic tools is that alone they do not improve pressure cuff bigger than the standard adult size.164,165
outcomes and thus often lack evidence for clinical Moreover, traditional cylindrical cuffs substantially
benefit; improved outcomes (and thus evidence for use) overestimate blood pressure compared with trunco-
can only be achieved for any type of testing if combined conical cuffs in those with a pronounced trunco-conical
with treatment in a diagnostic-therapeutic strategy. shape of the upper arm.166
Major difficulties exist in accurate determination of an
Diagnostic difficulties individual’s true blood pressure. The small number of
A key objective of this Commission is that every person blood pressure measurements taken in the physician’s
should have their blood pressure measured. Although office, commonly used to establish the diagnosis and
blood pressure monitors are becoming cheaper, there is a initiate treatment of hypertension, cannot account for
major need for wider access to very-low-cost, automated marked spontaneous variability in blood pressure. The
devices that are valid and amenable for use in resource- existence of white-coat and masked hypertension justify
restricted communities. The devices should be operable the use of out-of-office and automated, unobserved
by unskilled individuals or the patient themselves, with a measurements, but office blood-pressure measures can
preference for data to be automatically transmitted to still be used as a crude indication of blood pressure
health-care providers. control and are preferable to no measure at all. Ideally,
The time-honoured technique of auscultatory mercury diagnosis, initiation, and titration of treatment should be
sphygmomanography formed the basis for most of the guided by ambulatory, home, or automated, unobserved
current knowledge about the clinical significance of blood pressure, the latter potentially being applicable in
blood pressure and the benefits of treatment. However, resource-restricted environments.
2676 www.thelancet.com Vol 388 November 26, 2016
The Lancet Commissions
White-coat and masked hypertension are phenotypes method, SPRINT showed that lower blood-pressure
not identified by clinic blood-pressure measurement. targets were more attainable than those generally
White-coat hypertension is defined as a persistently achievable using traditional office measurements, and
elevated office measurement of blood pressure these lower blood-pressure levels were associated with
concomitant with normal blood pressure outside the better outcomes in people with high cardiovascular
office. It represents about 30% of all patients diagnosed risk. Nonetheless, for all out-of-office methods,
with hypertension and is associated with lower some adaptation of the threshold values might be
cardiovascular risk than sustained hypertension.167 necessary because they provide lower values than
The condition might not require treatment with anti- physician-measured blood pressure.182
hypertensive drugs in the absence of associated risk An additional challenge in refining the risk associated
factors and organ damage, but this strategy remains to with elevated blood pressure is that blood pressure values
be definitively tested.168 Home or ambulatory blood can vary substantially with time: beat to beat, minute to
pressure monitoring helps to confirm or exclude white- minute, hour to hour, day to night, over different days, or
coat hypertension, at least in people with mild hyper- between clinic visits over weeks, months, and even years.
tension at low or moderate total cardiovascular risk. Day-to-night variability provides important clinical
Masked hypertension is the opposite of white-coat information; a reduced (non-dipping pattern) or inverted
hypertension (normal office blood pressure and elevated (reverse dipping pattern) fall in blood pressure from day
out-of-office blood pressure), affecting about 5–10% of to night is an established marker of adverse prognosis.183,184
the general population169,170 but higher among people Such patterns are associated with increased activity of the
with untreated diabetes (29%)171 and is associated sympathetic nervous system, secondary hypertension, or
with higher cardiovascular risk than white-coat orthostatic hypertension. Ambulatory blood-pressure
hypertension.168,172 People with normal or high-normal monitoring is best suited to explore day-to-night changes
office blood pressure together with organ damage or at in blood pressure, although nocturnal self-measurement
high cardiovascular risk should be offered home or of blood pressure is also feasible.185 Long-term, visit-to-
ambulatory blood-pressure monitoring, to exclude visit variability in blood pressure is gaining interest as a
masked hypertension. Both home and ambulatory blood potential prognostic marker for stroke, cardiovascular
pressure are complementary methods173 and, when disease, and all-cause mortality, although evidence is
measured and recorded according to protocol, might conflicting.186,187
offer substantial advantage beyond physician-measured
blood pressure in the office environment.174,175 Several Haemodynamic characterisation
international guidelines recommend the use of home Haemodynamic characterisation of hypertension (par-
blood-pressure monitoring as a method that has good ticularly as it pertains to pulsatile haemodynamics) is a
reproducibility, is well tolerated by patients, is more field of growing interest. Blood pressure is the result of
widely accessible than ambulatory blood-pressure the flow generated by the left ventricle and the complex
monitoring, and is a relatively inexpensive option for impedance to that flow imposed by the arterial tree.188
improved management of hypertension.1,176–179 Some One approach to haemodynamic characterisation of
limitations of home monitoring can be overcome patients with hypertension involves the assessment of
through the use of memory-equipped devices, as well as central systolic blood pressure, which variably differs
by taking advantage of telemonitoring (transmission of from the conventionally measured brachial systolic blood
blood pressure measurements directly to the doctor) pressure.189 There are conflicting observations regarding
and smartphone applications. Further, ambulatory the incremental prognostic value of central compared
monitoring might provide more information on key with brachial blood pressure. However, it should be
issues such as blood pressure values during sleep and emphasised that considerable differences in central
routine daily activities. However, studies are still needed systolic blood pressure can occur among people with
to clarify whether antihypertensive treatment tailored on similar brachial systolic blood pressure, and that
the basis of out-of-office blood pressure, as compared antihypertensive therapy can affect central and brachial
with conventional office measurements, will result in systolic blood pressures differently.190–193 Because central
stronger prevention of cardiovascular complications. blood pressure (and how it changes in response to drug
A practical and time-efficient method of blood pressure therapy) seems to relate more strongly to end-organ
measurement could be achieved with automated, damage than brachial blood pressure,194 precise
unobserved, in-clinic measurement, which provides estimation of central blood pressure is expected to
blood pressure values close to out-of-office values and improve management decisions in hypertension, as
also limits white-coat effects.180,181 This method was used suggested by findings from a randomised trial.195
in the SPRINT study39 in which repeated blood pressure Methods to measure central blood pressure might be
measures were recorded with an automated device after particularly useful in elderly people with high prevalence
5 min of rest while the participant was seated and alone.181 of white-coat hypertension, and among young individuals
By using this refined blood-pressure-measurement with isolated systolic hypertension.196,197
www.thelancet.com Vol 388 November 26, 2016 2677
The Lancet Commissions
It should be emphasised that the study of central participant data. Because a wide range of baseline
haemodynamics can yield much more information than reference values exists,217 and the measurements are non-
brachial or central (peak) systolic blood pressure. For any invasive and well standardised,218,219 routine clinical
given peak left ventricular pressure, late systolic load measurements of aortic stiffness could be helpful in
(as opposed to early systolic load) promotes more left deciding which patients are at increased risk despite only
ventricular hypertrophy, fibrosis, dysfunction, and mildly elevated blood pressure, potentially aiding
failure.198–205 Dimensionless measures of wave reflections treatment decisions. However, simplification of the
and late systolic load derived from the pressure waveform technology will help to minimise operator variability and
are much stronger predictors of outcomes (particularly maximise utility. Importantly, reference values for aortic
heart failure) than central or peripheral pressures, stiffness only exist at present for white populations,
with statistically significant incremental prognostic emphasising the need for networks for research
value.200–203,205–209 The quantitative assessment of pulsatile collaboration to generate multiethnic reference values.
haemodynamics continues to evolve, and will probably More research into new inexpensive methods to measure
yield improved understanding of the underlying or estimate aortic stiffness is also needed.220
abnormalities leading to target-organ damage in hyper- The use of markers of subclinical cardiovascular
tension. Similarly, as technology evolves, assessments of damage for population-level screening cardiovascular
central haemodynamics are becoming increasingly risk is not recommended because these markers usually
feasible in ambulatory settings, enhancing the ability to lack specificity for future cardiovascular events, at least
characterise patients during daily activities. in the short term. Thus, a high number of false-positive
Finally, characterisation of traditional haemodynamic diagnoses might be expected (ie, patients falsely
parameters—including peripheral resistance and volume classified at high risk). Whether these are true false
status—using non-invasive techniques (such as positives or whether these individuals could benefit
impedance cardiography210) could provide useful from intervention has yet to be proven, and the cost-
information for tailored management of hypertension. effectiveness of such an approach is also unknown.
The growth in the development of wearable devices However, increased aortic stiffness is predictive of the
offers promise as potentially widely used tools that could future occurrence of hypertension in the general
facilitate detailed information along these lines as the population.47,221 Thus, if it were easier and less time
associated technology develops. However, these devices consuming to measure, aortic stiffness might be useful
will only be relevant in selected groups because of as first-line screening in certain populations.
practical reasons. People at moderate risk or patients with established
cardiovascular risk factors are typically the target
Markers of subclinical cardiovascular damage population for the use of markers of subclinical
Markers of subclinical cardiovascular damage or of cardiovascular damage; the markers can be used to
vascular health integrate the effects of long-term exposure reclassify individuals from moderate to high risk, and
to a highly variable risk factor such as blood pressure with thereby inform primary prevention,222 or help to decide
other cardiovascular risk factors, superimposed on an treatment choice and intensity.213 However, whether this
individual’s genetic background. This time-integrative use of markers leads to improved outcomes for patients is
characteristic combined with the ability to reflect both still unclear. In any case, subgroup analyses from the
known and unknown risk burden make these markers Heart Outcomes Prevention Evaluation (HOPE-3) study15
highly attractive. Elevated urine albumin–creatinine provide new perspective on the possible value of blood-
ratio,211 suggesting microvascular damage, and left pressure-lowering therapy even among adults with
ventricular hypertrophy on electrocardiography (ECG212), borderline elevated blood pressure and average risk,
suggesting cardiac damage, predict cardiovascular events irrespective of detailed measures of subclinical
independently of traditional risk factors.213 They are cardiovascular damage.
relatively inexpensive methods, and easy to measure and For patients with advanced target-organ damage or
implement, making them feasible globally. overt cardiovascular disease and already at high risk,
In hypertension, the target organs include the brain, other biomarkers could help to diagnose and stratify
heart, kidneys, and arteries. Because arteries are implied disease severity, or to guide treatment. For instance,
in the pathogenesis of target-organ lesions, they are N-terminal prohormone of brain natriuretic peptide has
logical candidates as useful markers of subclinical proven high value for the diagnosis of heart failure in
damage. Arteries adapt themselves to high blood patients with acute dyspnoea, and N-terminal
pressure by the walls becoming stiffer and thicker. Aortic prohormone of brain natriuretic peptide response to
stiffness, measured as carotid-to-femoral pulse wave treatment is indicative of outcome.223
velocity,214 has been associated with cardiovascular risk
even after adjustment for blood pressure and other Risk factor interactions
classic risk scores in more than 24 longitudinal Risk factors cluster together, and since 1994 the
studies,215,216 as confirmed in meta-analyses51 of individual prevention of cardiovascular disease has become more
2678 www.thelancet.com Vol 388 November 26, 2016
The Lancet Commissions
focused on the assessment of (and the adoption of regulation. Available evidence indicates that habitual
accurate tools to quantify) total cardiovascular risk.224 short sleep duration (less than 6 h per night) induces a
Very few patients with hypertension have isolated high sustained increase in blood pressure in normotensive
blood pressure independent of other risk factors, and a and prehypertensive adolescents and adults, increasing
synergistic effect of multiple cardiovascular risk factors the risk of developing hypertension.233 Although the direct
(eg, lipid, glucose, etc) contributes to a total cardiovascular association between sleep changes (eg, sleep deprivation,
risk that is greater than the sum of the risk carried by short sleep duration, insomnia) and elevated blood
each risk factor alone. Control of hypertension in patients pressure is not entirely understood, and involves
with multiple cardiovascular risk factors is more difficult numerous factors (eg, stress exposure, activation of the
in high-risk than in lower-risk patients.1 sympathetic nervous system and the hypothalamic–
The relatively poor control of hypertension in patients pituitary–adrenal axis, inflammation), the incidence and
with multiple risk factors despite effective anti prevalence of hypertension related to inadequate sleep
hypertensive and cardioprotective drugs225 demonstrates seems to be most important in adults younger than
that risk-factor clustering affects not only the 60 years, especially women.234 Moreover, insufficient
cardiovascular risk but also the efficacy of the sleep has been linked to weight gain and metabolic
antihypertensive treatment. In this context, even though abnormalities,235 which are implicated in the development
the metabolic syndrome is not a unique entity,132 it has of hypertension.
been associated with masked hypertension, arterial In addition to sleep disruption and abnormal breathing
remodelling, inflammation, and increased odds of pattern during sleep, patients with obstructive sleep
cardiovascular events in middle-aged and older apnoea commonly present with a non-dipping blood
individuals,131,226–228 with neurogenic abnormalities playing pressure profile. The prevalence of obstructive sleep
a crucial role.229 Therefore, detailed characterisation of apnoea is increasing, and its presence and severity are
the so-called phenotype of the individual patient with strongly associated with obesity.236 The alarmingly high
hypertension might be essential, not only for risk prevalence of excess bodyweight among children
stratification and type of antihypertensive drug, but also and adolescents suggests that obesity-related health
for the intensity of the antihypertensive treatment.230 The conditions will probably increase in younger popu
different clusters of metabolic syndrome components lations,237 leaving them at high risk for adverse health
have varying effects on arterial ageing and risk for problems throughout their lifecourse. Arterial
cardiovascular disease, with differing prevalence across hypertension, particularly resistant hypertension, often
Europe and the USA132 consistently shown in cohorts occurs in patients with obstructive sleep apnoea, and they
participating in the Metabolic Syndrome and Arteries share multiple pathophysiological mechanisms resulting
Research Consortium (eg, in populations with differing in adverse consequences on various organs.234,238 Elevated
genetic factors, lifestyle, or influence of medical sympathetic activity is evident in patients with obstructive
treatment).231 Notably, differences in blood pressure levels sleep apnoea, and further augmentation of sympathetic
among the clusters of components did not account for drive elicited by recurrent episodes of apnoea during
differences in the likelihood of having extremely stiff sleep could contribute to hypertension and cardiovascular
arteries. Thus, the burden of elevated blood pressure events.236,239 Despite the epidemiological association
differs according to the specific associated cardiovascular between obstructive sleep apnoea and hypertension,240 the
risk factors and not just by the number of associated reductions in blood pressure noted in clinical studies of
cardiovascular risk factors. continuous positive airway pressure have been
The best way to integrate multiple risk factors for treating remarkably small (roughly 1·3–3·0 mm Hg in systolic or
hypertension is still a matter of discussion. The 2013 diastolic blood pressure).241–243 The small size of this effect
European Society of Hypertension guidelines1 grade might be explained by similar overlapping patho-
interventions according only to the number of risk factors, physiological pathways linking obesity and obstructive
not to specific clusters. These scores to identify high sleep apnoea to hypertension, or because diagnosis of
cardiovascular risk lose accuracy in different ethnic groups. obstructive sleep apnoea and treatment with continuous
Additionally, the risk scores were constructed largely from positive airway pressure is often started late after lengthy
cohort studies done two or three decades ago, thus exposure to high blood pressure that has already
reflecting different levels of cardiovascular risk factors in remodelled the arterial tree.244–246 Findings from a
the population. Last, but not least, whether the scores randomised trial247 showed that a weight loss intervention
correctly estimate the total cardiovascular risk associated combined with continuous positive airway pressure
with multiple risk factors in the increasing population of therapy resulted in greater reduction in systolic blood
elderly individuals with comorbidities232 is uncertain. pressure (14·1 mm Hg) than did weight loss (6·8 mm Hg)
or continuous positive airway pressure (3·0 mm Hg)
Obstructive sleep apnoea and inadequate sleep hygiene alone at 24 week follow-up among individuals who
Impaired sleep quality unfavourably alters circadian adhered to treatment. Findings from another trial
blood-pressure profile and autonomic cardiovascular indicated that treatment with continuous positive airway
www.thelancet.com Vol 388 November 26, 2016 2679
The Lancet Commissions
pressure, but not nocturnal supplemental oxygen, genetic testing, and imaging studies253 as well as
reduced 24 h mean blood pressure in patients with long-term follow-up after surgery.254 Renovascular
obstructive sleep apnoea and controlled hypertension.248 hypertension, due to fibromuscular dysplasia (typically
With available evidence suggesting that continuous in young women) or atherosclerotic stenosis of renal
positive airway pressure is useful for the treatment of arteries (typically in elderly people with cardiovascular
obstructive sleep apnoea, targeting of obesity is essential risk factors) can be diagnosed by CT or MRI.255
to properly address cardiovascular risk in this population. Although education of general practitioners is essential,
Weight loss is clearly effective in reducing the adverse evaluation of patients by a multidisciplinary team in
metabolic consequences of obesity, sympathetic activity, centres experienced in dealing with secondary
hypertension, and obstructive sleep apnoea. Low-cost, hypertension should be favoured. Creation of dedicated
effective weight loss interventions in this population are registries at the international level should be promoted to
needed. Additionally, immediate global action and produce and validate robust and cost-effective diagnostic
policies to reduce physical inactivity, promote outdoor algorithms. Development of next-generation sequencing
activities, and institute prevention programmes to methods in the routine diagnostic setting would improve
control obesity are clearly warranted to reduce the global diagnosis for monogenic forms of hypertension and
burden attributable to hypertension. catecholamine-secreting tumours. Development of non-
invasive imaging techniques able to differentiate
Secondary hypertension fibromuscular dysplasia from atherosclerotic stenosis, to
A key objective of the Commission is to increase the quantify the degree of stenosis and to appreciate its effect
diagnosis rate of secondary hypertension, which remains on renal function should be encouraged. Given the
underdiagnosed.1,249 Secondary hypertension (caused by substantial efforts often required to accurately identify
endocrine, renal, or vascular disorders, rare monogenic secondary hypertension, diagnosis of secondary
diseases, or a drug or toxic agents) represents a rare hypertension cannot be the highest-priority goal in low-
opportunity for curative antihypertensive therapy, income and middle-income countries. However, an action
accounts for up to 5–10% of patients with hypertension, for the future should be to increase the availability of
and affects millions of people worldwide.250,251 relevant investigations in communities with few resources.
To reduce the delay of diagnosis, decisional algorithms
should be simplified. General practitioners should be New cardiovascular biomarkers and omics
educated to suspect secondary hypertension in every A biomarker is a characteristic that can be objectively
patient with juvenile, resistant, or severe hypertension.1,249 measured and evaluated, and acts as an indicator of
Initially, medical history, physical examination (eg, an normal biological processes, pathogenic processes, or
abdominal bruit might reveal renal artery stenosis), and pharmacological responses to therapeutic interventions.256
simple laboratory tests—including estimated glomerular In hypertension, blood pressure is an almost ideal
filtration rate (for detection of chronic kidney disease) biomarker. Blood pressure is causally related to the
and electrolytes (hypokalaemia might indicate an development of the condition, defines the condition,
endocrine hypertension)—should be examined. If predicts the outcome, is the target of therapeutic
abnormalities are detected, physicians should be able to interventions, and serves as a surrogate marker to assess
request appropriate additional investigations. Endocrine the benefit of therapies. Therefore, the role that other
hypertension is mainly due to adrenal disorders causing biomarkers could have in hypertension requires careful
an excess of hormones which affect blood pressure thought. We discuss three relevant scenarios briefly.
regulation. Primary aldosteronism (Conn’s syndrome or First, and bearing in mind the Commission’s definition
bilateral adrenal hyperplasia) is the most common form of the condition, hypertension is not merely persistently
of secondary hypertension. The diagnostic algorithm is elevated blood pressure; we see the potential for a new
sequentially based on biochemical tests (serum definition of hypertension based on a molecular pheno-
potassium, aldosterone–renin ratio, urine aldosterone type characterised by complex biomarkers. Genetic
secretion, and confirmatory tests in the absence of intake polymorphisms have been identified with highly
of products derived from liquorice and other agents significant associations with blood pressure, but the
that affect aldosterone–renin ratio) followed by proportion of variance explained by these genetic
adrenal CT scan or MRI and adrenal venous markers is only about 3–5%.257 The specific composition
sampling to discriminate unilateral or bilateral of proteins in hypertension assessed by proteomic
disease.252 Catecholamine-producing tumours (phaeo- techniques258 and the description of the metabolome
chromocytoma or extra-adrenal paraganglioma) are associated with hypertension259 could potentially redefine
severe disorders, sometimes revealed by life-threatening hypertension at a molecular level. At present, little
emergencies or in the context of a hereditary research in this area has been done, but the potential of
predisposition (up to 40% of affected patients carry a proteomics260 and other comprehensive molecular
mutation in a susceptibility gene). Evidence-based techniques should be fully exploited to better characterise
guidelines recommend measurement of metanephrines, the condition termed hypertension.
2680 www.thelancet.com Vol 388 November 26, 2016
The Lancet Commissions
Second, biomarkers could help in the prediction of the hypertension.13,257 Functional analysis of regulated
risk of developing hypertension. In this scenario, raised pathways that emerge from these studies emphasises the
blood pressure would again be a symptom that points importance of renal salt and water handling (eg, in the
towards the underlying pathology, most likely changes in form of natriuretic peptides) and signalling.262 Whether
the resistance of small and large arteries. Blood pressure these genetic variants are also associated with the risk of
therefore only rises after functional and structural developing hypertension and associated organ damage
changes in the vasculature have already occurred, before in a truly prospective fashion remains to be explored.
diagnosis of hypertension. There are good reasons to
believe that prediction and preventive treatment before Summary of possible actions
the onset of hypertension have the potential to further In summary, the Commission identifies two basic
reduce hypertension-associated morbidity and mortality. problems. First, fundamental phenotyping of individuals
Third, in patients with hypertension, biomarkers can be with elevated blood pressure—including blood pressure
used to refine or restratify cardiovascular risk. We would measurements, basic cardiovascular risk stratification,
assume that complex molecular biomarkers based on and screening for secondary hypertension—is often not
omics techniques will provide better individual prediction done systematically. Second, further research is needed
than traditional unidimensional biomarkers such as lipids to determine the additive beneficial effect of more
or markers of cardiac damage (eg, the cardiac troponins). advanced phenotyping. In table 2, the different
Limited data are currently available about risk prediction subproblems with corresponding goals and actions are
in hypertension with omics-based biomarkers.258,259,261 listed, classifying the three actions dealing with the
The so-called higher omics techniques—eg, proteomics fundamental phenotyping of individuals with elevated
and metabolomics—will be best suited to describe the blood pressure as essential.
current state of an individual, whereas genetic and
genomic biomarkers are better suited as risk markers. In Pharmacological prevention and treatment
fact, because of the complex interplay between genes and Current evidence and problems
environment, the association between genetic and There is strong evidence that blood-pressure-lowering
phenotypic variants is not always very tight. Nevertheless, drugs are beneficial for the prevention of major events
findings from genome-wide association studies and such as stroke, myocardial infarction, kidney failure, and
other genetic studies have robustly identified candidate cardiovascular death. Compelling data are few, however,
markers associated with the risk of having concerning the role of antihypertensive treatment—in
Goals Actions Keywords
Poor measurement of blood Improve the quality of blood pressure measurement* Certification and validation of monitors and endorsement of protocols Measurement quality
pressure Increase the availability of standardised blood for measuring blood pressure by professional societies
pressure monitors* Develop simple and inexpensive blood pressure monitors
Give preference for home, ambulatory, and automated unobserved
measurements to office measurements
Poor identification of people at Improve awareness of absolute cardiovascular risk as Promote education on cardiovascular risk of patients, doctors, and Empowerment
high cardiovascular risk a target for treatment* health professionals
Improve detection of clusters of cardiovascular risk Reinforce targeting global cardiovascular risk rather than single risk
throughout the life course (eg, MetS)* factor
Improve detection of obstructive sleep apnoea*
Lack of diagnosis or delayed Increase the diagnosis rate of secondary hypertension Promote simple and robust algorithms for detecting secondary Secondary hypertension
diagnosis of secondary by doctors* hypertension
hypertension Increase the availability of relevant investigations in communities with
few resources
Favour management by multidisciplinary teams with appropriate
expertise
Lack of data on blood pressure, Address the birth-cohort effect† Capitalise on recent large existing cohorts, develop novel cohorts ··
cardiovascular risk, and arterial Update cardiovascular risk algorithms† including biomarkers, and adequate follow-up to ascertain
ageing from childhood to cardiovascular outcomes†
adulthood
Poor assessment of vascular Promote the concept of early vascular ageing for Promote the use of aortic stiffness as a robust and simple marker of ··
ageing in routine clinical monitoring cardiovascular health early vascular ageing
practice Develop simple and affordable devices to measure aortic stiffness†
Reference values for different ethnicities†
Uncertainties about the clinical Evaluation and validation of the diagnostic and Capitalise on large existing cohort with adequate follow-up and ··
use of omics-based biomarkers prognostic value of omics-related markers ascertained cardiovascular events†
*Essential goals. †Related to research.
Table 2: Identified problems and corresponding goals and actions relating to diagnosis
www.thelancet.com Vol 388 November 26, 2016 2681
The Lancet Commissions
middle-aged and older individuals—to prevent dementia Some evidence suggests that the antihypertensive drugs
or in slowing the progression of cognitive impairment. recommended by current guidelines (namely angiotensin-
In early trials into diastolic and systolic–diastolic converting enzyme inhibitors, angiotensin receptor
hypertension, blood-pressure-lowering drugs reduced, blockers, calcium channel blockers, and diuretics) achieve
on average, diastolic blood pressure by 5 mm Hg, the similar global cardiovascular prevention.1,70,270 Nonetheless,
risk of stroke by 42%, and the risk of coronary events by some of these drug classes have benefits in addition to
14%.263 In subsequent trials on systolic hypertension in blood pressure reduction. Angiotensin-converting enzyme
individuals aged 60 years or older, the average reduction inhibitors and angiotensin II receptor blockers are
in systolic blood pressure was 10 mm Hg, and the overall particularly indicated in the presence of chronic kidney
risk reduction was 30% for stroke and 23% for coronary disease, diabetes mellitus, or chronic heart failure.1,70 β
events.264 Similar trends were observed in patients aged blockers are indicated in the presence of coronary heart
80 years or older in the Hypertension in the Very Elderly disease and chronic heart failure,1,70 but tend to be less
Trial42 who were actively treated aiming for a systolic effective in the prevention of stroke.272–274 By contrast,
blood pressure lower than 150 mm Hg. The beneficial calcium channel blockers provide more protection against
effects of blood-pressure-lowering therapies to reduce stroke, but less protection against heart failure in overall
stroke, myocardial infarction, heart failure, and death analysis275 and in several single active-comparison
have also been shown in meta-analyses.27,265 trials.272,273,276 The combination of angiotensin-converting
Very recent evidence from the SPRINT trial39 and the enzyme inhibitors and angiotensin II receptor blockers
subsequent meta-analysis266 suggest that, at least in at-risk could be detrimental in clinical conditions277 other than
populations without diabetes or a history of stroke, blood chronic heart failure,278 and hence is discouraged in the
pressure targets as low as 120 mm Hg systolic are associated management of hypertension.1,70 The combination of β
with further improved outcomes, although this blood blockers and diuretics increases the risk of new-onset
pressure target is associated with substantial adverse diabetes mellitus.279,280 Findings from two trials have
effects.39 The lower target achieved in SPRINT should, suggested that the combination of angiotensin-converting
however, be interpreted in the context of the protocol for enzyme inhibitors and calcium channel blockers might be
blood pressure measurement used. Trials in patients with superior to combinations of diuretics with either
type 2 diabetes that used a similar approach to aggressively angiotensin-converting enzyme inhibitors or β blockers,
lower blood pressure including ACCORD41 and at least in white populations.279,281
ADVANCE267 showed smaller benefits on event rates than Although many large and well designed randomised
did SPRINT. This was confirmed by findings from meta- controlled trials are available on the benefits of
analyses.268,269 antihypertensive treatment, there is still insufficient
Drug treatment to achieve blood pressure of less than evidence on several clinically relevant questions for the
140/90 mm Hg still seems to reduce all types of fatal and management of hypertension. Whom should we treat?
non-fatal cardiovascular events, even in individuals with How should we treat? To which level should we treat and
mild hypertension and in those at low-to-moderate which haemodynamic component should be used for
cardiovascular risk.270 However, absolute risk reductions therapeutic evaluations? Which target should we treat?
with blood-pressure-lowering treatment are greater in Most data about the benefits and harms of
patients at higher levels of cardiovascular risk, and a antihypertensive treatment derive from short-term
higher level of baseline risk is associated with a higher randomised controlled trials (follow-up typically 5 years),
absolute residual risk on treatment.271 It therefore remains whereas information about the accrual of benefits and
unclear whether patients with mildly elevated blood potential harms over the lifecourse of treatment is
pressure, in particular those at a younger age (ie, younger lacking. In most individuals, treatment duration by far
than approximately 40 years of age in men and 50 years of exceeds the event horizon provided by most clinical trials.
age in women), need pharmacological treatment. The Commission therefore strongly suggests that
Although reserving antihypertensive treatment for high- decisions about treatment should be made with the
risk patients with hypertensive maximises the cost–benefit lifecourse framework in mind, whereby not only
ratio, only treatment of patients at low-to-moderate risk immediate cardiovascular benefits but also long-term
might prevent the increasing number of treatment remote target-organ or metabolic harms are taken into
failures associated with late initiation of treatment. account in a unifying concept of lifecourse net clinical
Furthermore, antihypertensive treatment in people with benefit. Although all classes of antihypertensive drugs
mild hypertension and at intermediate risk without reduce cardiovascular events, clinical trials and
known cardiovascular disease has recently been supported observational data suggest not only differences across
by a predefined subanalysis of the blood-pressure- antihypertensive drug classes with regard to general
lowering part of the HOPE-3 trial.15 Individual treatment efficacy and specific cardiovascular outcomess266 but also
decisions that take patients’ preferences into account will differences regarding the risk of new-onset diabetes279 and
be the best approach in some—but not all—health-care atrial fibrillation282 and the potential for renal protection283
systems. in specific clinical scenarios. It is possible that the
2682 www.thelancet.com Vol 388 November 26, 2016
The Lancet Commissions
metabolically neutral class of angiotensin-converting hypertension.291,292 Low adherence to antihypertensive
enzyme inhibitors is associated with greater lifecourse treatment has been consistently associated with poor blood
net clinical benefit than the diabetogenic class of diuretics, pressure293 and adverse cardiovascular prognosis.294 There
but in the absence of trial data with event horizons of are significant differences in discontinuation of therapy
20–30 years this proposal is purely speculative. The between antihypertensive drug classes, with angiotensin-
potential of big data to fill in this knowledge gap cannot converting enzyme inhibitors, angiotensin II receptor
be overstated.284 The Commission strongly recommends blockers, and calcium channel blockers showing the best
research into the lifecourse net clinical balance between adherence.295 Significant heterogeneity in adherence to
benefits and harms of different antihypertensive drugs antihypertensive therapy has also been reported between
and of different blood pressure targets. drugs belonging to the same drug class.296 Objective
assessment of adherence to therapy is possible by testing
General treatment and adherence for the presence drug metabolites in body fluids, particularly
Detection and management of hypertension in high- urine. Measurement methods such as high-performance
risk populations, most notably in low-income and liquid chromatography coupled to tandem mass
middle-income countries, remains suboptimal. Despite spectrometry are sensitive,292 reproducible, relatively
clear evidence for the benefits of blood pressure reduction inexpensive, and could help treatment decisions, particularly
using low-cost and safe drugs, most individuals with in patients with difficult-to-control hypertension. However,
hypertension in the world are undetected, untreated, or these drug metabolite screens provide only snapshot
poorly controlled (figure 6).33,68,285 Accordingly there is an information and—especially if done without informing the
urgent need to ensure access to affordable, high-quality patient—could substantially undermine the relationship
medicines globally. Indeed, the best-documented between doctor and patient. These extensive efforts to
antihypertensive therapies are now off patent and can, assess adherence objectively are primarily for research and
therefore, be manufactured at very low cost, which will only feasible in high-income countries.
be crucial in overcoming limitations to access, including The Commission is convinced that it is very important
regulatory, political, and corporate factors. for treatment adherence that the patient can see a clear
Most patients with hypertension require more than relationship between increase in antihypertensive
one drug to control their blood pressure.286 Single-pill treatment and decrease in blood pressure. Therefore, we
combinations of two or more antihypertensive drugs, recommend use of either ambulatory, home, or automated
therefore, have the potential to reduce the number of unobserved blood pressure to initiate and titrate treatment
tablets that patients have to take, as demonstrated in the (rather than the highly variable office blood pressure,
ACCOMPLISH trial,281,287 and generally lead to improved which could mask the effectiveness of a drug).
blood-pressure control.288 However, whether these A growing body of evidence suggests that a
combinations are cost-effective and improve adherence to multidisciplinary approach to improve adherence is
therapy remains debated.289 Available combination pills are needed.297,298 This approach includes task sharing and
based mainly on proprietary agents. The complex licensing involvement of non-physician health workers and family
legislation for new formulations and combinations makes members, as well as educating the patient and reminders
it commercially unattractive to develop combination pills to reinforce the importance of treatment adherence.
based on less expensive, off-patent compounds. Different approaches can be used depending on the
Until more definitive data are available, we propose the economic, cultural, and social context (see section on
use of simplified algorithms supported by e-health Empowerment as a tool).
technologies both for initiation of drug monotherapy in Side-effects of antihypertensive treatment are another
mild hypertension and combined therapy in more severe major factor contributing to poor blood-pressure control.
grades. To facilitate drug therapy in patients with Drug and drug-class-specific side-effects such as cough
hypertension worldwide, a core set of affordable, efficient, associated with use of angiotensin-converting enzyme
evidence-based, high-quality drugs must be widely inhibitors, peripheral oedema with dihydropyridine-type
available. The primary health-care team has to be calcium channel blockers, and tiredness with β-receptor
extended beyond physicians and should involve allied blockers are well recognised and cause treatment failure
health professionals and community workers to improve in a proportion of patients with hypertension.299 Notably,
hypertension management and to put into practice a the combination of dihydropyridine calcium channel
communication strategy with emphasis on prevention blockers with angiotensin-converting enzyme inhibitors
and control of hypertension.290 significantly reduces the occurrence of peripheral oedema,
One of the main causes for non-control of hypertension is the most common adverse drug reaction usually leading
a lack of adherence by the patient. Low medication to discontinuation of the calcium channel blockers
adherence is common in patients with hypertension, (irrespective of their efficacy in lowering blood pressure).300
especially those with resistant hypertension; indeed, Hypotension—as a side-effect of antihypertensive
the prevalence of poor adherence is reported to be as high therapy—occurs largely independently of the choice of
as 25–50% in patients with apparent resistant antihypertensive drug class. In fact, especially in older
www.thelancet.com Vol 388 November 26, 2016 2683
The Lancet Commissions
individuals, episodes of systolic hypotension are is, however, well tolerated and provides a basis for
extremely common, affecting roughly 55% of patients prevention trials in high-risk patients such as those with
aged 75 years and older.301 There is a complex interplay atherosclerosis310 or chronic renal failure,311 for whom
between hypotension, cerebral hypoperfusion, and poor there is some evidence that treatment of normotensive
adherence to therapy as a result of impaired cognition individuals to systolic blood pressures below 130 mm Hg
that add to the challenges of antihypertensive therapy, can be associated with beneficial outcomes. However,
especially in elderly people. another approach was tested in the blood-pressure-
lowering part of the HOPE-3 trial15 in which people with
Pharmacological prevention intermediate risk without known cardiovascular disease
Antihypertensive therapy has a major role in the primary were randomly assigned to candesartan 16 mg plus
and secondary prevention of cardiovascular and renal hydrochlorothiazide 12·5 mg versus placebo for 5·6 years.
diseases, both in the general population and in at-risk Significantly improved outcome, however, was only
populations such as those with diabetes or chronic observed in people with baseline systolic blood pressure
inflammatory diseases. Antihypertensive drugs are greater than 143·5 mm Hg (ie, in the top tertile of systolic
therefore part of a concerted treatment strategy to tackle blood pressure among trial participants), thus not
cardiovascular risk factors such as hypertension, obesity, supporting antihypertensive treatment in normotensive
dyslipidaemia, and hyperglycaemia. Preventive treatment individuals at intermediate cardiovascular risk—although
often starts with the assessment of biomarkers such as the study was not powered to detect benefits among
blood pressure, bodyweight, cholesterol, and glucose different subgroups defined by baseline blood pressure.
levels, followed by the targeted prescription of individual Therefore, the evidence base is not sufficiently robust for
drugs to address these risk factors. By contrast, the notion primordial prevention to be universally accepted.53
of a polypill containing fixed doses of preventive drugs
such as antihypertensive drugs, statins, and aspirin, Management of elderly individuals with hypertension
which is prescribed irrespective of the exact individual More than 30% of people older than 65 years fall at least
risk but rather depending on average population risk (eg, once annually,301,312,313 and antihypertensive treatment is a
based on an age threshold)302,303 has gained attention, major (and modifiable) risk factor for falls.314,315 The risk is
especially in low-income and middle-income countries particularly high when more than three defined daily
where the burden of cardiovascular diseases is high, doses of antihypertensive drugs are taken and is
resources for diagnostic tests are scarce, and inexpensive independent of specific drug classes such as diuretics or
and standardised treatments are more likely than β blockers.315 Aggressive treatment of older people with
individualised therapies to be taken up in clinical hypertension might not only increase their risk of falls
practice.304 The beneficial effect of lipid-lowering treat- via episodes of hypotension, but also lead to poor
ment with statins in patients with high cardiovascular adherence to therapy and increased adverse drug
risk is well supported by several studies,121,305 but findings reactions.316 However, in the SPRINT trial39,40 there was no
from the HOPE-3 study306 showed that lipid-lowering increase in falls-related injuries requiring hospital
statin treatment also reduced cardiovascular events in evaluation or admission. A useful strategy could be to
individuals with intermediate risk and no known monitor blood pressure more carefully with automated
cardiovascular disease independently of blood pressure devices (when the patient is alone and relaxed), use
and antihypertensive treatment. However, there is an systematic home or 24 h ambulatory blood-pressure
ongoing debate about indications, cost-effectiveness, and measurements, and include standing blood pressure in
composition of the polypill, making translation of this elderly people to identify patients with clinically
concept into clinical practice very difficult.307 significant hypotension before any falls occur.
Primordial prevention of hypertension can be achieved Another relevant aspect in older people with
by prescribing antihypertensive drugs at a stage when hypertension is cognitive impairment, with the prevalence
blood pressure is still within the normal range. The of dementia increasing from 7% in subjects older than
classification as high normal blood pressure1,53 for blood 65 years to 30% in subjects older than 80.317 Subjective
pressure ranges of 130–139 mm Hg systolic and reports of memory loss begin about 2–3 years before
85–90 mm Hg diastolic has been introduced because onset of dementia.318 Elevated blood-pressure levels in
individuals in this range are more likely to progress to middle-age have been associated with increased risk of
hypertension compared with those with normal or dementia in older age.319 Elevated blood pressure provokes
optimal blood pressure. Studies in individuals with high early damage of cerebral white matter microstructure320
normal blood pressure have shown with short follow-up and is associated with poor cognitive performance, even
periods (2 years in TROPHY308 and up to 3 years in at young ages.321 Thus, cerebrovascular injury should be
PHARAO309) that incident hypertension can be prevented considered and monitored as target-organ damage in
or at least delayed. However, because of insufficient hypertension in its own right322 to prevent the onset of
long-term follow-up data, primordial prevention of clinical overt dementia, to slow the progression of
hypertension is open for further research. Such treatment cognitive decline, and to postpone the onset and
2684 www.thelancet.com Vol 388 November 26, 2016
The Lancet Commissions
exacerbation of behavioural symptoms that can often lead prevalence of hypertension and diabetes mellitus
to loss of independent living of patients and can be increases, with predictable adverse effects on
devastating for caregivers. Antihypertensive treatment cardiovascular outcomes. To better manage the already
can improve cerebral microcirculation through reduced high but expanding need for antihypertensive treatment
blood pressure and protective effects on arteries of in people of non-European descent, more ethnically
specific antihypertensive drugs.191 However, as with falls, specific research is needed concerning genetic adaptation
treatment that is too aggressive can result in hypotension as a promotor for cardiovascular risk factors, development
and cerebral hypoperfusion, thereby accelerating the of target-organ damage, and, crucially, the optimal
progression of cognitive decline in older individuals.37 pharmacological management of raised blood pressure.
We should acknowledge the lack of strong evidence However, ethnic differences in culture and lifestyle and
from randomised controlled trials on the protective role underlying socioeconomic conditions probably affect
of blood pressure reduction on cognitive dysfunction. cardiovascular events more than do genetics.
Clinical trials that include cognition as primary endpoint
are needed. The randomised controlled trials should Lifestyle modifications
include predominantly older individuals and adopt Nearly all guidelines recommend non-pharmacological
accurate and cost-effective tests to screen for cognitive therapy or lifestyle modification as a first-line approach to
impairment.323 Such trials might clarify whether the hypertension management. Lifestyle modification offers
association between hypertension and cognition is causal universal appeal as an intervention because the costs, in
and which antihypertensive drugs are the most effective motivated individuals, are minimal and can lead to drug
in slowing progression of cognitive impairment and step-down or withdrawal. However, in the absence of self-
postponing the onset of overt clinical dementia. motivation, achievement-sustained lifestyle modifications
Furthermore, improved characterisation of pathways require substantial resources over a longer period.
linking hypertension to cognitive decline and dementia Furthermore, although the benefits of lifestyle modi-
could help to identify novel drug targets such as fication in cardiovascular prevention are clear, evidence to
accelerated arterial ageing,324 clearance of cerebral guide the use of individual-based lifestyle modification as
parenchymal waste products (including β-amyloid) via a stand-alone or add-on therapeutic intervention is
the perivascular circulation,325,326 and the response of the lacking, which is perhaps most evident for dietary
cerebral vasculature to injury.327 modifications. For example, investigators of the DASH-
Sodium trial138 and others have established that a low-
Ethnic and cultural differences sodium diet can lead to substantial improvements in
With a few exceptions, most mortality and morbidity blood pressure. Long-term follow-up data from the Trials
trials into hypertension management have been done in of Hypertension I and II137 also suggested that the long-
individuals of European descent, and limited trial data term risk of cardiovascular events might be reduced with
are available to inform treatment specifically for those of sodium reduction. Similarly, high potassium intake has
Asian, African, or Middle Eastern origin. been purported to reduce blood pressure.332,333 Restriction
The challenges in understanding the ethnic and of salt intake has been demonstrated to reduce blood
cultural differences in cardiovascular disease are pressure and cardiovascular events more in patients with
substantial. Ethnicity is difficult to define and classify. hypertension than in those without hypertension.16,90,137,334,335
The biology of individuals is driven by complex sets of Evidence of varying quality suggests that particular
gene–gene, environment–environment, and gene– foods (eg, beetroot, nitrate-containing foods and
environment interactions,328 and some clear physiological beverages,92 garlic,336 and flaxseed337) can reduce blood
differences are apparent across ethnic groups (eg, pressure levels. However, the usefulness of such foods to
decreased renin concentrations329 and endothelial nitric lower blood pressure remains to be proven in large
oxide bioavailability330 among those of African origin). cohorts. Ultimately, further research—including inter-
Among the environmental influences are socioeconomic ventional studies—are needed to guide the use of dietary
issues, but issues including widespread differences in modification in the treatment of hypertension.
stress handling, smoking habits, nutrition, and caloric Increased physical activity is another lifestyle modi-
and salt intake can have pronounced effects on the fication for which there is reasonable consensus on value
prevalence of hypertension and development of target- as a preventive intervention but less guidance for its use as
organ damage, including overt cardiovascular disease.331 therapy. Most recommendations suggest increased
As a consequence, the results of hypertension research physical activity in the management of hypertension and
in individuals of European descent might not apply extend logically from the large bodies of observational data
directly to those of non-European ancestry. showing associations between decreased physical activity
As the world becomes more connected and increases and cardiovascular risk.338,339 Findings from meta-analyses
in prosperity, lifestyles characterised by reduced levels of also suggest that exercise training reduces blood pressure
physical activity and unhealthy diets rich in fat, salt, and in healthy individuals340,341 and those with hypertension.342,343
sugar are more common everywhere. As a result, the Even in patients at high cardiovascular risk, the benefits of
www.thelancet.com Vol 388 November 26, 2016 2685
The Lancet Commissions
regular exercise could outweigh any risks by improvement primary aldosteronism is still controversial, especially in
in cardiac structure and function.344 Nevertheless, there very elderly patients, and the benefit of interventional
remains a paucity of data about the optimal form (eg, treatment of renal artery stenosis remains under debate.
aerobic vs resistance or isometric training), type (eg, International randomised clinical trials are still required
swimming vs running), and thresholds at which maximum to develop evidence-based indications for medical or
benefit are achieved. Moreover, there is a pressing need for interventional therapies in different categories of
strategies to optimise uptake of recommendations. secondary hypertension.
Finally, the evidence supporting the use of most Personalised treatment and management by multi-
lifestyle modifications in therapy is typically from studies disciplinary teams with appropriate expertise are
that looked at these modifications individually. In essential to achieve favourable outcomes in patients with
practice, however, lifestyle modification should be secondary hypertension. Lifelong specialised follow-up is
systematic, and assessment of the efficacy of multiple indicated, and in some cases (including catecholamine-
lifestyle modifications given together will be crucial. producing tumours caused by germline mutations of
Indeed, although the effects of individual lifestyle SDHB) follow-up includes not only the patient (who is at
modifications on blood pressure might be small, the risk of recurrence and development of metastases) but
effect of several modifications together might prove more also their relatives (when genetic testing offers the
effective than pharmacotherapy, at least in some patients. possibility to detect and treat asymptomatic disease in
Meta-analyses for this are already underway.345 family members).352 However, the profound knowledge
Irrespective of the evidence gaps, the general consensus of the natural history of the different forms of secondary
is that people should be encouraged to engage in some hypertension and specific prognosis biomarkers needed
form of regular exercise to improve their cardiovascular to precisely refine follow-up recommendations is
risk profile. still lacking.
Targeting pathophysiology Pathophysiology-based approach to essential (primary)
Pathophysiology-based approaches to secondary hypertension hypertension
Many of the factors that regulate blood pressure through The mechanisms underlying the pathophysiology of
the key mechanisms of cardiac output, volume status, essential hypertension are complex and multifactorial.
and vascular tone are known and include the sympathetic Lessons learned from the treatment of patients
nervous system, the renin–angiotensin–aldosterone with secondary forms of hypertension can, however,
system, and renal function. In primary (essential) inform therapeutic approaches to those with
hypertension, a large number of factors with fairly small essential hypertension. Activation of the sympathetic
effects act together, whereas in secondary hypertension, nervous system, which occurs in patients with
one or very few well defined factors with substantial phaeochromocytoma, also plays an important part in the
contributions to blood pressure dominate. initiation and maintenance of elevated blood pressure
Individualised treatment that targets the specific cause of and associated adverse effects in many patients with
hypertension substantially improves blood pressure control essential hypertension.353 The close association between
in most patients with secondary hypertension and even the sympathetic nervous system and the renin–
cures hypertension in at least a fifth of such patients. In angiotensin system in the pathophysiology of
patients with primary aldosteronism, adrenalectomy in hypertension has led to the development of mechanism-
cases of unilateral production of aldosterone and medical based approaches to hypertension treatment, including
therapy including aldosterone antagonists for bilateral drugs and invasive procedures targeting the neurogenic
hyperaldosteronism are therapeutic options to control component of hypertension; however, further
blood pressure.346 Surgical resection can cure hypertension investigation is needed before introduction of these
in patients with a catecholamine-producing tumour.253 therapies into the clinical setting.354 With available
Although renal percutaneous transluminal angioplasty is evidence linking excess aldosterone to disease
indicated in the first instance in patients with fibromuscular progression, resistant hypertension, and mortality,355
dysplasia,255,347 randomised trial data have shown no benefit further studies to improve selectivity and tolerability of
of surgical revascularisation or stenting compared with drugs directly aimed at the aldosterone pathway are
medical therapy in patients with atherosclerotic stenosis of needed.354 A reduction in blood pressure and sympathetic
renal arteries.348–350 In patients with rare forms of monogenic activity has been demonstrated with invasive therapeutic
hypertension, such as Liddle’s syndrome and Gordon’s strategies such as baroreflex activation therapy and renal
syndrome, blood pressure control can be achieved and denervation356–362 in treating patients with truly resistant
hypertension can be controlled with lifelong treatment with hypertension or those whose hypertension is
a single drug such as amiloride (Liddle’s syndrome) or a uncontrolled in the absence of other treatment options.
thiazide-type diuretic (Gordon’s syndrome).351 However, in the light of the similar blood-pressure
However, despite decades of research, the indication responses to renal denervation and sham control found
for adrenal surgical resection versus medical therapy for in the Symplicity Hypertension-3 trial,363,364 a better
2686 www.thelancet.com Vol 388 November 26, 2016
The Lancet Commissions
understanding of underlying pathophysiology is needed counteract the substantially altered vascular phenotype
before using these treatment approaches (for example, that truly characterises hypertension. The potential to
insufficient ablation of the renal sympathetic nerves develop a cure for hypertension that at the same time
might explain the lack of difference in blood pressure treats the phenotype of persistently elevated blood
noted in the trial). An approach which ablated a pressure should be the ultimate aim.
combination of nerves, including the main renal artery In addition to traditional and emerging risk factors,
and branches, resulted in the greatest reduction in renal molecular biomarkers will help to characterise the
sympathetic activity in an animal model,365 whereas renal phenotype of hypertension in individual patients, pointing
denervation done in all arteries including accessory renal towards the specific dysregulated pathways that can be
arteries produced a greater reduction in blood pressure targeted with specific therapies, thereby paving the way
and sympathetic nerve activity compared with ablation for personalised medicine in hypertension. In this sense,
in the main renal artery alone in patients with resistant biomarkers—for example, subclinical cardiovascular
hypertension.366 These findings might substantially phenotypes and target-organ damage—can be a target of
improve efficacy of renal denervation and reduce the antihypertensive therapy, not as a symptom to be
variability in blood pressure response to the procedure, minimised but as a definition of the condition that is
which should be assessed further in randomised, sham- altered when it has been successfully treated.
controlled clinical studies.
Although pathophysiological principles should be Targeting haemodynamics
explicitly considered within personalised management of Haemodynamic assessment might help in the choice of
hypertension control, the contribution of individual antihypertensive therapy by identifying individuals who
pathophysiological factors to a patient’s elevated blood might benefit more from ad-hoc regimens (based on
pressure is difficult to assess in clinical practice, where matching the haemodynamic action of drugs with the
comprehensive assessment of the sympathetic nervous haemodynamic pattern of hypertension) and assisting in
system and renin–angiotensin system to the same the titration of the intensity of therapy to specific goals.
standard as in clinical research studies is not feasible. To achieve this goal, new methods that assess arterial
However, findings from the PATHWAY-2 study367 showed pressure and flow dynamics, beyond focus on
that the blood pressure response to classes of conventional upper-arm blood pressure, are needed.
antihypertensive drugs could be predicted by plasma Antihypertensive medications can have different haemo-
renin concentration, a crude measure of the activity of the dynamic effects in the large central arteries (eg, aorta,
renin–angiotensin system. Additionally, assessment of carotids) compared with the brachial artery where the blood
haemodynamic profiles with non-invasive devices that are pressure cuff is applied. For instance, organic nitrates
simple to use seems to help in deciding on initiation of lower central aortic systolic blood pressure more than
treatment, choice of drugs, and monitoring of therapy.210 systolic brachial blood pressure.371–373 By contrast, β blockers
The potential cause and underlying mechanisms of (primarily atenolol) less effectively lower central aortic
unresponsiveness to antihypertensive drugs in patients systolic blood pressure but have similar effects on brachial
who adhere to treatment need to be addressed in future systolic blood pressure compared with calcium channel
clinical trials. The role of lifestyle modifications including blockers, angiotensin-converting enzyme inhibitors, or
stress management in the treatment of hypertension and angiotensin II receptor blockers.191,193,374–376 Thus, assessment
the question of whether behavioural and procedure- of left ventricular hypertrophy and geometry and arterial
based therapies can favourably modulate neurogenic pressure waveforms to determine haemodynamic and
mechanisms and ultimately prevent hypertension and its volume status, and central aortic loading conditions, can
cardiovascular consequences still need to be explored efficiently refine hypertension management decisions, as
systematically. supported by findings from two randomised trials.195,377 The
BEAUTY study210 compared haemodynamic monitoring
Treatment of hypertension beyond the treatment of elevated using impedance cardiography (combined with a drug
blood pressure selection algorithm) versus conventional drug selection for
Treatment of hypertension currently focuses on blood- the treatment of uncontrolled hypertension. Both strategies
pressure-lowering measures. However, in the future, we resulted in similar reductions in ambulatory daytime and
suggest that additional therapeutic strategies beyond the office systolic blood pressure, although therapy based on
mere lowering of blood pressure will have to be explored impedance cardiography therapy was associated with more
and applied. use of diuretics and fewer side-effects than conventional
Recent data suggest that the pathophysiology of management.
hypertension is more complex than originally thought Blood pressure variability has been recognised as a
and involves processes such as endothelial dysfunction,368 prognostic factor independent of the level of blood
inflammation,369 altered sodium handling,370 and oxidative pressure per se. Most of the evidence, however, relates
stress.46 Targeting of these mechanisms will, in most blood pressure variability with the risk of stroke,186 whereas
cases, not immediately reduce blood pressure but rather the association with other cardiovascular events seems to
www.thelancet.com Vol 388 November 26, 2016 2687
The Lancet Commissions
be less robust. Different ways to calculate blood pressure An important problem is that target-organ damage is
variability, different modalities of variability (short term, slow to respond to treatment,393 thereby reducing its
long term, day–night, and others378), and little evidence value as a monitoring tool in the acute care of patients.
about therapeutic approaches specifically directed to However, changes in target-organ damage can detect
change blood pressure variability hinder the translation of failure or success of therapeutic strategies before the
a potentially useful concept to clinical practice. Different development of myocardial infarction, stroke, or
effects of various drug classes on blood pressure variability cardiovascular death. Whether targeting of subclinical
have, however, been described379,380 and could form a basis organ damage rather than or in addition to blood
for prospective evaluation in clinical trials. pressure provides additional benefit to the patient or to
At this point, it is clear that measurements of society remains to be clearly demonstrated. For example,
haemodynamic patterns of hypertension are of interest to the ongoing SPARTE trial394 will address the question of
elucidate mechanisms related to the pathophysiology of whether arterial stiffness assessed as carotid-to-femoral
hypertension in individual patients, and hold promise as pulse wave velocity can be used as a surrogate endpoint.
a therapeutic strategy in hypertension. However, further The demonstration that such monitoring of treatment
investigations are needed before they can be recom- is advantageous over the classic approach based on
mended for routine clinical use. In particular, trials blood pressure measurement should be tested in
designed to target specifically central blood pressure at clinical trials.
any given level of brachial blood pressure are required.
Summary of possible actions
Targeting subclinical organ damage There is a large arsenal of effective pharmacological
Targeting of biomarkers might be useful if improvements agents with established efficacy in the treatment
in biomarker profiles are associated with improved of hypertension. To improve the pharmacological
outcome.381 Left ventricular hypertrophy in hypertension management of hypertension globally, a crucial first step
has previously been considered as adaptive, but the is to ensure universal access to affordable, high-quality
presence of left ventricular hypertrophy is associated therapeutics. However, even with this access, therapy is
with increased cardiovascular risk. More importantly, not always given optimally. We therefore recommend the
treatments such as angiotensin-converting enzyme development of evidence-based decisional algorithms to
inhibitors and angiotensin II receptor blockers382,383 inform health-care professionals precisely on the required
decrease in left ventricular hypertrophy, which is diagnostic and therapeutic steps. Such algorithms should
predictive of improved prognosis.384,385 It remains unclear be based on the most current evidence, be clear and
whether treatment guided by the level of left ventricular simple, and aim to standardise the diagnostic work-up
hypertrophy adds incremental benefit over blood- and therapy of almost all patients with hypertension.
pressure-targeted treatment. Such algorithms will probably include predominant use
For detection of vascular and renal damage, urine of generic drugs from major antihypertensive classes,
albumin–creatinine ratio is the most robustly studied combination therapy as an initial treatment approach,
parameter. When increased, it is associated with and measures to monitor treatment and improve
atherosclerotic disease, myocardial infarction, and adherence. When coupled with better identification of
cardiovascular risk. Furthermore, any substantial reduction hypertensive individuals with the help of “more hands” in
is associated with improved prognosis,386 especially in health service through task sharing, these actions will
diabetes in some387 but not all trials.388 The major challenge greatly improve blood pressure control and reduce the
related to urine albumin–creatinine ratio is the variability global burden of hypertension and related cardiovascular
of this parameter with time and intervention.389,390 For other complications not only in individual patients but in whole
subclinical markers, the evidence is more scarce. populations.
Markers of large artery structure and function,213 In addition to these recommendations, research is
especially carotid-to-femoral pulse wave velocity51 and needed to better understand the potential of targeted
carotid distensibility,213,391 have demonstrated their added therapy depending on age, ethnicity, and cardiovascular
value against cardiovascular risk scores. They appear risk on treatment, the utility of lifestyle modification in
simple to use and are applicable in large groups. Reference therapy, and the benefits of monotherapy versus
values are available217,392 and efforts have been made to combination therapy as an initial treatment strategy. It
standardise measurements, but whether arterial markers will also be important to assess whether treatment based
can be used to target therapy remains unclear. Similarly, on targets such as left ventricular hypertrophy,
early brain damage can be detected by MRI through white haemodynamics, and biomarker-based approaches are
matter hyperintensities.233 However, by contrast with left superior to blood pressure control for reduction of
ventricular hypertrophy and urine albumin–creatinine cardiovascular risk in hypertension. Prior to the
ratio, whether intervention can reverse these lesions is development of hypertension, preventive therapeutic
unclear. Further information is needed before considering strategies including the use of polypills or targeting
cerebral lesions a target for therapy. prehypertension also have the potential to delay the
2688 www.thelancet.com Vol 388 November 26, 2016
The Lancet Commissions
natural lifecourse of hypertension, but require evidential lifestyle modifications, self-administered treatment and
support. monitoring, and the provision of health information
Finally, the Commission sees a continued need for the (eg, biochemistry) directly to the patient. Irrespective of
development of new drugs, both those that act on new the method, strategies that foster patient empowerment
therapeutic targets and those that target existing have consistently been shown to increase patient
pathways but have improved pharmacokinetic or satisfaction, encourage adherence, and improve out-
pharmacodynamics profiles (table 3). comes in chronic diseases including hypertension.396–398
A complementary and essential relative of patient
Empowerment as a tool empowerment is community empowerment, the process
Introduction to empowerment of empowering communities of people—defined by
Education and empowerment are related tools that offer geographic proximity, shared common interests, or even
great potential to improve the global management of disease (eg, hypertension)—to take control over their
elevated blood pressure. Abundant evidence suggests conditions and improve the quality of their lives and
that early health education improves outcomes in terms collectively overcome inequities.399,400 Strategies for
of primordial prevention; education can also be tailored community empowerment include provision of
to improve interactions between patients, doctors, education, technical information, and tools necessary for
health-care providers, pharmacists, and key participants action, ultimately enabling the community to define the
in the management of hypertension to maximise its problem, determine the best solution, and implement
effectiveness. the response.300,401 However, a community-based pro-
Patient empowerment more specifically refers to the gramme that includes stakeholders from the community
process of shifting a patient’s mentality from a passive is not necessarily a community empowerment approach.
recipient of health care towards an active role where they In community empowerment, an essential component is
understand their condition and their role in the health- leadership and control of the process by the community,
care process, and take self-initiated actions to benefit coupled with availability of essential resources and
their health.395,396 The many strategies for patient capacity to act. An empowered community is confident,
empowerment include shared decision making, self-led inclusive, organised, cooperative, and influential. All of
Goals Actions Keywords
Lack of antihypertensive Improve availability of affordable, high-quality, and Universal availability of at least one of each class of antihypertensive drug Medication access
drug availability effective antihypertensive agents worldwide* Availability of single-pill combinations where resources permit
Development of novel therapeutics based on improved knowledge of pathophysiology†
Lack of available health- Increase capacity for management of hypertension Train community health workers to detect, initiate, and monitor treatment of Workforce
care professionals for worldwide* hypertension expansion
management Expand health-care workforce by facilitating task sharing in the management of
hypertension
Lack of stratified Optimise treatment initiation, goals, and Harness existing data to provide rational information on optimisation of targets, Standardised
approaches to the combinations according to age, ethnicity, and treatment initiation, and therapy based on age, ethnicity, and cardiovascular risk treatment
treatment of cardiovascular risk* Support randomised controlled trials that focus on optimisation of BP targets, treatment
hypertension initiation, and therapy†
Poor adherence to Improve approaches to overcome poor adherence Harness information technology tools to facilitate patient adherence ··
treatment Identify determinants of poor adherence†
Develop treatment approaches targeting causes of poor adherence†
Limited information on Establish defined approaches to incorporate Integrate existing knowledge into management strategies ··
how to use lifestyle culture-specific lifestyle modification into Randomised controlled trial to determine optimal lifestyle modification approaches to
modification as therapy management of hypertension hypertension management†
Brachial blood pressure Determine whether treatment to alternative targets Assess the relative benefit of management based on target-organ damage† ··
might be a suboptimal improves cost efficacy and effectiveness of Evaluate the relative benefit of management based on haemodynamics†
measure to guide antihypertensive treatment Assess the relative benefit of management based on biomarkers†
treatment
Uncertain effect of Assess the benefits and determine optimal Randomised controlled trials to assess the effectiveness of self-treatment† ··
empowering patients to implementation of self-treatment
take control of their
antihypertensive
management
Physician inertia in Counteract physician inertia Promote education of doctors and health-care professionals through the availability of ··
increasing simple guidelines for daily management of hypertension
antihypertensive
medication
*Essential goals. †Related to research.
Table 3: Identified problems and corresponding goals and actions relating to pharmacological treatment
www.thelancet.com Vol 388 November 26, 2016 2689
The Lancet Commissions
these aspects, when brought to bear on preventing and non-physician community health workers in Pakistan,
controlling hypertension,402 can result in effective and South Africa, and Iran has shown that lay health workers
sustainable changes in a community’s health trajectory. could effectively deliver health-promotion materials, detect
high blood pressure, and reduce blood pressure levels in the
Education population.414–416 Indeed, team-based care and task sharing
In addition to population-wide education strategies, with nurses, pharmacists, and medical assistants are
patients and individuals at risk of hypertension represent effective in improving blood pressure control, particularly
an audience potentially receptive to more focused when coupled with education on medication,417–420 which
educational initiatives. Education in such populations could also be extended to other professions.421,422
might be expected to improve communication between Primary-care physicians must also ensure that they are
provider and patient, and ultimately empower the patient applying best practice based on the best available
to play an active role in managing their risk factors and knowledge. For future physicians, the university medical
disease. Indeed, abundant and long-standing evidence training curriculum must sufficiently address current
suggests that patient education improves outcomes in guidelines and also include novel approaches such as
hypertension.403–406 Physicians who spend more time with patient empowerment, self-treatment, and the use of
patients and engage more in lifestyle and prevention new technologies. International and national professional
education generally prescribe less medication. However, societies should also work together to produce consistent
long-term follow-up of this strategy is needed to measure guidelines, because real or perceived inconsistencies are
the effect on patient outcome.407 Despite this evidence, and a likely cause of therapeutic inertia.423
the fact that virtually all practice guidelines for hypertension
advise lifestyle modifications as first-line treatment, Self-monitoring of blood pressure
educational initiatives are not universally implemented, Self-monitoring empowers individuals to engage in their
even in patients with hypertension. In one study,408 only own management of blood pressure, leading to many
55% of young adults with hypertension had documented possible benefits, including more active treatment by
evidence of lifestyle education after diagnosis. doctors,424 facilitation of discussion with doctors,
A major gap in knowledge is the lack of clarity about what improved patient–doctor relationships, greater possibility
constitutes effective lifestyle counselling for hypertension. for adhering to antihypertensive therapy, and reduction
For example, how many sessions, of what duration, over of blood pressure.425–429 Self-monitored blood pressure
what period of time, and in what format are most effective? must be done with a standardised protocol to minimise
Systematic reviews of educational interventions in patients the potential for erroneous readings from extrinsic (eg,
with hypertension are underway and could ultimately device validation) and intrinsic (eg, level of relaxation)
provide some clarity in this area.409 In addition to this factors affecting reading quality. The widespread
consideration, health-care delivery systems are unlikely to availability of educational material on self-monitoring
adequately deliver patient education in the clinical should make this information easily accessible to patients
environment. Conventionally, physicians are seen as being and doctors. Despite all the potential advantages of self-
central to oversee lifestyle change,410 but this strategy might monitoring, there are still evidence gaps relevant to both
not be the best approach.411 The World Development patients and clinicians. Patients lack education about
Indicators on Health Systems412 indicate that there are only what they should be concerned about and how to act;
0·1 physicians and 0·5 nurses for every 1000 people in low- physicians have insufficient clarity about how to optimise
income countries, and even in high-income countries the the use of self-monitoring in the clinical encounter, and
available 3·1 physicians and 8·6 nurses per 1000 are need better guidance in interpreting self-monitored
insufficient to carry out this important task effectively. It is, values (including how to handle differences from clinic
therefore, understandable that major reports and guidelines blood-pressure measures).425 Future developments in
on prevention of cardiovascular disease state the im- wearable devices that are appropriately validated could
portance of an integrated approach or shared responsibility overcome some of these hurdles. For health-care systems,
involving numerous stakeholders to ensure successful an expanding number of monitors now include
implementation of preventive strategies.68,87,119,123,410,413 technology for the immediate communication of a
Community health workers, pharmacists, nurses, patient’s home-measured blood pressure reading to the
physiotherapists, dietitians, and other allied health doctor’s office or another third party. Clinical protocols,
professionals are probably better positioned than medical capacity, and response systems need to be developed to
doctors to provide consistent and substantive lifestyle support timely, appropriate, and meaningful feedback to
education. Introducing or strengthening community patients to improve control. The use of these devices in
linkages and resources creates new opportunities for the self-titration is described further below.
delivery of health information and patient-centred disease
management. In parallel, continuing education of all health Self-administered treatment
workers remains crucial to ensure delivery of optimal care Self-administered treatment provides an important
based on current knowledge. Experience with trained opportunity to improve management of chronic diseases
2690 www.thelancet.com Vol 388 November 26, 2016
The Lancet Commissions
such as hypertension.430 This approach seeks to shift consistent message through the creation of a universally
patients from mere receivers of drugs prescribed by the recognised seal of approval to ensure confidence in the
physician to active participants in the shared decision quality of the content.
making regarding their treatment.431 For this approach to Information and communications technology systems
be effective, patients should be given advice based on the are a potential key to empowerment in hypertension
best available scientific evidence, with alternative care. These technologies can empower patient-centred
approaches and outcomes presented so they can choose medicine with enhanced access and continuity of health
the treatment strategy that is most suitable for them. care, management planning according to the best
The patient’s individual goals are prioritised while available scientific evidence through computerised
ensuring that they understand the short-term and long- decision-support technology, and tools to promote self-
term consequences of their choices.432 management including patient-guided services such as
Only a few studies have assessed self-management and electronic or mobile health applications and
self-titration in hypertension. One pilot study433 assessed telemedicine.437,438 Information and communication
the effectiveness of self-management and self-titration technologies can also reduce medical errors and improve
with a web-based system; blood pressure was effectively response to adverse events. There is also emerging
reduced, but there were barriers to implementation of evidence that telehealth and e-counselling services could
the system including the patients’ lack of trust in the be effective addenda to pharmacological interventions or
protocol.433 Findings from the SETHI434 and TASMINH2435 as a preventive strategy in hypertension.439,440
trials further showed that self-monitoring and self- Finally, we have to consider the potential of mobile and
titration could engage patients in their treatment, wearable technologies, which are increasingly integrated
resulting in improved blood-pressure control and into life, to enhance self-monitoring and treatment.
reductions in cardiovascular risk up to 12 months after Wearable technologies that assist in fitness monitoring are
initiation. Further clinical trials will be necessary to increasingly popular and could motivate individuals to
better identify the target populations, develop algorithms improve their overall lifestyle. Hypertension-specific
or procedures for drug adjustment, and evaluate the wearable technology is now emerging and could ultimately
most effective duration of the intervention. There is also increase awareness, engagement, and, potentially, self-
a need for specific training for both patients and doctors monitoring. To fully engage patients, this technology
and to monitor progress regularly. It is possible that should be easy to use, without the need for complicated
self-titration could reduce clinical inertia (ie, resistance to access or operation, while providing feedback on
change), but this notion remains to be proven. hypertension control in real time.441 One successful model
of such an approach was deployed by Logan and
Technology colleagues,441–444 who used a system of Bluetooth home
Mobile and internet technologies already play an blood-pressure monitoring connected to a pre-
important role in the management of hypertension by programmed smartphone working through a central
educating patients and supporting disease management; server to receive messages to inform the patient about the
this role is expected to grow alongside a global increase status of their blood pressure control. In patients with
in availability. diabetes and hypertension, this system significantly
App and web-based content provide an opportunity to reduced systolic and diastolic blood pressure compared
reach both the patient and the general population, with patients who were only controlled by home blood-
especially in low-income and middle-income countries. pressure measurement after 1 year. Interestingly, the
By providing resources that are available to patients at all higher rate of blood pressure control was not related to
times, there is increased opportunity to educate and higher use of blood pressure medications. The system
influence a patient’s lifestyle outside of the clinic at times seemed to be well accepted by patients and did not increase
when they are more receptive to change. However, the number of visits to the doctor. There are also some
such approaches must adhere to current clinical promising results about the efficacy of mobile technologies
recommendations. Investigators of a study436 that for blood pressure control even for patients with low
assessed whether internet content accurately reflected literacy living in low-income or middle-income countries,
the American Academy of Paediatrics recommendations who reported a high level of satisfaction with care.445
for infant sleep safety found that less than half of all high-
traffic websites were consistent with recommendations, Summary
with a substantial influence of low-accuracy retail- It is clear that there are several approaches to the
product sites and blogs.436 Accordingly, the hypertension management of hypertension that encourage patient
community will need to guard against the circulation of engagement and empowerment and improve dialogue
outdated or erroneous educational material within the between patient and provider. An important consideration
plethora of available health-related content. One possible for such strategies will be the need for both educated
approach would be for international and national patients and responsive health-care teams and providers
professional societies to collaborate in endorsing a to ensure the persistence of empowered behaviours.
www.thelancet.com Vol 388 November 26, 2016 2691
The Lancet Commissions
It should be noted that, to date, the benefits of these cardiovascular events reduction estimated to be cost
patient empowerment strategies have typically been saving.451 Salt reduction was identified by WHO as a “best
evaluated only over fairly short periods of time buy” for non-communicable disease prevention and
(ie, <2 years). The effects of these interventions could control, particularly as some of the relevant strategies can
conceivably diminish over extended periods of time. be implemented at very low cost.452 South Africa, Brazil,
Accordingly, for chronic diseases such as hypertension it Argentina, and Chile are countries with industry
will be important to assess the long-term feasibility, cost- agreements to reduce salt in processed food, and
effectiveness, and benefits of any approach. It will also be approaches to change behavioural patterns can be used
important to incorporate empowerment and technology where salt is added at the table, as in India.
into hypertension management within the context of
available resources. Pioneering approaches, particularly Health systems in relation to elevated blood pressure
those involving expensive technology in resource-rich A health system is a broad term that includes elements
locations, can inform future universal application. from population surveillance to clinical care to public health
infrastructure, as well as the financing to support it.453
Blood pressure and health systems The population-level impact of interventions pertaining
The economics of managing blood pressure to blood pressure management depends on the strength
Blood pressure control was identified as a leading target of the health system that delivers them. In low-resource
of the 2013 WHO Global Monitoring Framework to settings where primary care systems are underdeveloped,
reduce deaths from non-communicable diseases by public systems will need to incorporate new capacity for
25% by 2025.446 Elevated blood pressure is a main hypertension management, and explore efficiencies by
indicator of high risk for cardiovascular disease, and linking with existing systems for addressing other
many premature deaths can be averted cost-effectively diseases, such as HIV/AIDS, which might help alleviate
through community and clinic-delivered interventions. administrative and delivery costs.454 Even in high-income
Because most deaths related to non-communicable countries where delivery systems for primary care are
disease are projected to occur in the future in low-income already established, these systems have to be updated
and middle-income countries, specific consideration of through financing and delivery reform to ensure they
the benefits and costs of hypertension prevention and remain effective and can deliver improved outcome. For
control in resource-limited countries is warranted. chronic diseases to be managed successfully, delivery
However, a comprehensive health system initiative to systems must be designed to avoid patterns of patient
prevent and treat hypertension would need to encompass use that are episodic and acute in nature, supporting,
efforts to address other important cardiovascular risk instead, planned patient visits and continuity of care.
factors such as smoking, excessive alcohol intake, There are hallmarks of health-care delivery systems that
unhealthy diet, hyperlipidaemia, obesity, and inactivity. will improve the control of hypertension relevant to all
Economic analysis can guide priority setting related to health systems, high income or low. These include
blood pressure management. Hypertension management standardisation of treatment, team-based care, broad scale
can be cost-effective, with an estimated annual cost per availability of affordable medications, and community
person of implementing simple population management engagement.455 The Innovative Care for Chronic Conditions
programmes (including distribution of base blood Model proposed by WHO provides a framework for
pressure diagnostic tools and at least one of eight essential organising chronic care delivery, emphasising the
medicines to lower cardiovascular disease risk in importance of preventing the fragmentation of services
medium-risk or high-risk patients) of less than US$1 in from inpatient, to outpatient and pharmacy services, to
low-income countries, less than $1·50 in lower-middle- prevention and community efforts.456 The Chronic Care
income countries, and $2·50 in upper-middle-income Model, which emphasises proactive, planned, patient-
countries.18,447 A multidrug package targeting hypertension centred, and team-based care, and connections between
and cardiovascular disease in 23 low-income and middle- clinics and communities, has been shown to improve
income countries has been estimated to reduce outcomes.457 Creating registries of patients with hypertension
cardiovascular death rates by 1·5% per year at an average can allow for efficient management approaches across the
annual cost of $1·08 per person.448 With a large proportion continuum of care delivery points, allows for system
of the population in low-income and middle-income accountability, and has been used in effective models.458
countries having elevated blood pressure, hypertension These aspects need to be implemented to achieve success in
management for even half of patients at moderate to high reducing the burden of blood-pressure-related disease.
risk in these settings could avert an estimated 0·77 million Access to medication is another key requirement.
deaths, or 15·4 million disability-adjusted life-years at a Assuring sustained broad-scale access to affordable
ratio of $23 in benefits per $1 spent.449 Population-level medications is challenging and approaches vary by
drug treatment for elevated blood pressure is highly cost- country depending on health-system organisation and
effective,450 based on the assumption of a linear financing. In general, procurement and distribution
relationship between reduction in blood pressure and processes should be carefully reviewed. Use of generic
2692 www.thelancet.com Vol 388 November 26, 2016
The Lancet Commissions
formulations, simplified packages, or polypills, and wide opportunity to focus on strengthening countries’ health
distribution mechanisms such as primary health or information systems, using an integrated, comprehensive
outpatient facilities, can help scale up distribution in approach based on each country’s individual needs.25
low-resource settings. In the Americas, the Pan American In summary, national health systems can influence the
Health Organization’s Strategic Fund provides a model global burden of hypertension. However, continuing
of regional support for drug availability by offering commitment is needed by national governments to
member states technical assistance with management of prioritise the protection and promotion of health and
the drug supply chain and drug quality, creating a capital wellbeing of their citizens by ensuring best practices are
account to prevent stock-outs during emergencies, and implemented.465
negotiating favourable prices for drugs on their products
list, including medications to treat hypertension.459 Global health initiatives to reduce elevated blood pressure
The promise and potential scale of universal health Several initiatives are underway worldwide focusing on
coverage throughout the world is expected to improve health systems improvement within the context of
outcomes for non-communicable diseases. Universal hypertension prevention, treatment, and control. Million
health coverage is defined by WHO as “ensuring that all Hearts is a national initiative from the USA to affect
people have access to needed promotive, preventive, population health, aiming to prevent 1 million heart
curative and rehabilitative health services, of sufficient attacks and strokes in the USA by 2017 through health-
quality to be effective, while also ensuring that people do system strengthening by increasing focus on
not suffer financial hardship when paying for these cardiovascular prevention and by improving access to
services”.460 Universal health coverage involves three effective cardiovascular health care. The Centers for
coverage dimensions—health services, finance, and Disease Control and Prevention and Centers for Medicare
population—and is a dynamic, continuous process & Medicaid Services, co-leaders of Million Hearts within
that changes in response to shifting demographic, the US Department of Health and Human Services, are
epidemiological, and technological trends, as well as collaborating with other federal agencies and private-
people’s expectations.25 sector organisations to make a long-lasting impact against
The 2013 WHO World Health Report encourages global cardiovascular disease. Million Hearts aims to prevent
adoption of universal health coverage, which has most heart attacks and strokes by improving access to effective
recently been introduced in Thailand and Mexico, and is care and improving quality of care for the ABCS of heart
under consideration in India.461,462 The 2009 health reform in health: aspirin (when appropriate), blood pressure
China emphasised the role of efficient health-care delivery control, cholesterol management, and smoking cessation.
for chronic diseases, including hypertension.463 The WHO It focuses clinical attention on the prevention of heart
and World Bank global monitoring report, Bringing universal attack and stroke, encouraging the public to lead a heart-
health coverage (universal health coverage) into focus, for the healthy lifestyle, and improving the prescription and
first time quantified and tracked progress in universal adherence to appropriate medications for the ABCS.466,467
health coverage in key areas of financial protection and The Global Standardized Hypertension Treatment
health services coverage for populations as a whole, as well Project was originally developed across the Americas in
as subpopulations living in rural areas and the poor. 2012 with a focus on strengthening of clinical health
Strong health information systems are also necessary to systems. The initiative focused pharmacological manage-
advance the conditions for hypertension prevention, ment, with a core set of antihypertensive medications,
treatment, and control.464 Although there is no single cross- ensuring their availability through efficient procurement
national surveillance system for cardiovascular disease and mechanisms, using patient registries to monitor blood
hypertension, several surveys, registries, cohort studies, pressure control using standard treatment protocols, and
and vital statistics can be used by different stakeholders to encouraging team-based care and patient empower-
gather different kinds of information about these ment.455 Demonstration projects have been initiated in
conditions. Technological advances in health-care systems two countries, Barbados and Malawi, to improve control
and electronic health-care records can be used for of hypertension through improved management in
surveillance and monitoring of health-care interventions primary health-care settings in Barbados and using an
in hypertension, including randomised trials testing the existing HIV/AIDS platform in Malawi. Results from
effects of different public health policies. As noted earlier these projects are expected in 2017. The project framework
in this Commission report, data necessary for even the and activities have been expanded to include lifestyle
most descriptive surveillance needs of prevalence are components, and it is being integrated into a global
lacking. Government investment in health information initiative, Global HEARTS.
systems at all levels is necessary to inform and advance China’s Shandong province (population 96 million),
efforts to prevent and control hypertension throughout the where hypertension and excessive sodium intake in adults
world. Monitoring the new objectives of the Sustainable are major public health problems, provides an example of
Development Goals, for example promoting wellbeing and hypertension control with population approaches such as
ensuring universal health coverage, presents an sodium reduction through lifestyle changes. Most salt in
www.thelancet.com Vol 388 November 26, 2016 2693
The Lancet Commissions
the diet is added at the table or during cooking. The the approach to this growing public health problem is
Chinese Ministry of Health and the Shandong Government multifaceted. First, there is a need to respond immediately
collaboratively launched the Shandong–Ministry of Health to those at highest risk for related complications—those
Action on Salt Reduction and Hypertension in 2011, with evident hypertension and perhaps subclinical or
introducing expanded blood-pressure screening and even clinical cardiovascular disease—through evidence-
treatment, and driving changes in social norms by based clinical treatment, delivered effectively by health
supporting health-promoting environmental policies. systems designed to assure successful control for every
These strategies were implemented in concert with a patient. However, even if expertly delivered to all, such an
surveillance system, funding mobilisations, and approach is inefficient and does not thoroughly address
strengthening of local capacity of health services. Provincial the true breadth of the problem. The size of the
and local government agencies and health-sector teams hypertension problem, the previous relative failure of
target interventions in household and educational settings individual non-pharmacological prevention and the large
such as elementary schools, and also prehypertension and proportion of undiagnosed and untreated patients with
hypertension populations from a representative study essential hypertension, underlines the need for solutions
cohort selected by a complex, four-stage cluster sampling468 focused on population-based approaches including public
with strategic partners such as food industry, businesses, health. The pipeline of future patients includes virtually
and restaurants to reduce sodium intake. Mid-term every human being. Even those who reach middle-age
evaluation reported a decrease in the per-person seasoning without hypertension have a more than 90% chance of
salt intake in Shandong from 12·5 g to 11·58 g per day.469,470 developing the condition during their remaining
By contrast, in the UK—where most dietary sodium lifetime.471 Aggressive population-wide interventions that
consumption is through packaged and restaurant foods—a fundamentally include changes to the social and
government-led initiative included a focus on reducing the economic living environments will dynamically shape
amount of sodium in processed foods. Results are how populations behave, and will directly affect
promising.144 The Institute of Medicine recommended a primordial and primary prevention. Such approaches are
similar strategy to sodium reduction in processed foods in crucial and must be a part of any strategic approach that
the USA. Areas of future research that could benefit low- will successfully address the management of hypertension
income and middle-income countries in particular include at the global level. Primary prevention will include early
country-specific cost–benefit analysis of different information on the importance of a healthy lifestyle and
hypertension interventions. This strategy could help to help to make appropriate lifestyle changes. However, for
optimise resource allocations in low-resource settings, and real impact, policies are required that will improve the
inform decisions to invest in strengthening of health socioeconomic environment, strategically framed on
systems (table 4). improving the population living environment as a whole.
This approach must include intentions to reach people
Key actions and implementation of all ages in the environments where they live,
Setting the scene for a multifaceted approach work, and play.
10·4 million people are estimated to die each year because Population-level interventions will require multisectoral
of elevated blood pressure.65 The costs in terms of engagement from government, industry, non-govern-
morbidity and mortality, as well as economic and societal mental organisations, and civil society as a whole. The
costs, are substantial. The causes of hypertension are solutions we develop must be multidimensional,
complex, as are the solutions. Hypertension is often the transforming the communities (reaching individuals
product of a lifelong interplay of individual and indirectly) in which we live into health-promoting environ-
environmental factors, starting even before birth. Thus, ments, and supporting innovations and improvements not
Goals Actions Keywords
Lack of standardised, All countries create, maintain, and act on Endorse the WHO/World Health Assembly NCD Global Monitoring Framework Health-system
comprehensive a national surveillance system that Advocate for appropriate resourcing of surveillance systems strengthening
knowledge about blood regularly captures blood pressure and Create accessible reports
pressure levels related measures of risk*
Lack of system Health system collects, monitors, and Develop efficient health-care delivery systems that monitor blood pressure levels for their ··
accountability for blood responds appropriately to blood pressure populations and act appropriately
pressure control levels* Develop task-sharing approaches that effectively deliver care in resource-constrained settings
Connect health-care delivery centres with appropriate community points of blood pressure
measurement
The action to endorse WHO/World Health Assembly NCD Global Monitoring Framework is closely connected to the key action on universal access to measurement of blood pressure, whereas the action to ensure
accountability of the health system to collect, monitor, and respond appropriately to blood pressure levels is closely connected to the key action on expanding the capacity of the clinical workforce engaged in
management of blood pressure. These two health-care system actions are later combined to one key action. NCD=non-communicable disease.*Essential goals.
Table 4: Identified problems and corresponding goals and actions relating to health systems
2694 www.thelancet.com Vol 388 November 26, 2016
The Lancet Commissions
only in the health-care systems from which we access care, Key actions within prevention, in relation to current
but also in the broader socioeconomic environment (eg, global initiatives
food systems and availability). Introduction
Many doctors consider preventive measures against
Essential goals and related key actions hypertension to be ineffective, time-consuming, and
The Commission has identified ten essential goals and with poor results. The time-pressured and stressful
related key actions that, not surprisingly, overlap to a lifestyles that are increasingly the norm create
large extent with current global health initiatives within environments that promote hypertension, encouraging
the field of hypertension (table 5). The key actions are easy or less expensive options such as sedentary
not prioritised among each other because they are behaviours and consuming cheap, salty, sugary, and
complementary, and the balance between strength of fatty foods. Because many of the changes required to
evidence and potential benefits are inherently different address these challenges are social and political rather
between selective pharmacological intervention in than medical, this report is not intended to be read
high-risk patients versus broad implementation of exclusively by scientists and health-care professionals
health-promoting programmes. In essence, the key but instead aims for a broader audience—including
actions aim to stimulate goal-oriented dialogue, various industries, policy makers, and civil society.
bridging concepts and strategies from public health, Hence, the fundamental key action would be to strongly
health-care systems, and clinical practice. The support policies and strategies that enhance changes in
Commission approaches the hypertension problem at the broader socioeconomic environment with the
many different levels through improvement of public greatest likelihood of population-wide benefits for
knowledge (to motivate healthy living including cardiovascular health (figure 7).
checking blood pressure); the environment (to support
healthy living); education of health workers (to increase Creating a health-promoting environment
capacity and quality of detection and management); The key to global prevention and control of hypertension
access to affordable, good-quality antihypertensive is to support global adoption of health-promoting diets
drugs; and health-care systems (to monitor and high in vegetables, fruits, legumes, whole grains, and
coordinate the actions). quality proteins, with no introduction to tobacco and no
Key actions Keywords
Prevention: lifestyle and environmental changes
Unhealthy environment Strategies and policies to accelerate socioeconomic improvements Make healthy food choices easier, combat tobacco, and promote Health-promoting
and development of health-promoting environments; accelerate physical activity in daily living environment
the implementation of accepted health-promoting policies
Lack of understanding about Early and sustained education about healthy lifestyles and blood Educate and empower health workers and teachers to instil Healthy behaviours
unhealthy lifestyle pressure (new technology) healthy lifestyles
Low awareness Ensure universal access to blood pressure measurement through Tailored education about hypertension throughout the life course Measurement access
inexpensive monitors and surveillance
Diagnosis and evaluation
Poor measurements Certification and validation of monitors and endorsement of Develop simple, inexpensive blood pressure monitors; preference Measurement
protocols for measuring blood pressure by professional societies for home, ambulatory, automated, and unobserved blood pressure quality
measurement
Poor cardiovascular risk Promote education of patients, doctors, and health professionals Reinforce targeting of global cardiovascular risk rather than single Empowerment
assessment risk factors
Poor or delayed diagnosis of Simple protocols for detecting secondary hypertension in Improve the availability of relevant investigations Secondary
secondary hypertension communities with few resources hypertension
Pharmacological prevention and treatment
Lack of available health-care Expand the capacity of the clinical workforce through task sharing Health system collects, monitors, and responds appropriately to Workforce expansion
professionals and the use of endorsed education of community health workers blood pressure levels (accountability)
Lack of good-quality and Universal availability of at least one of each class of Availability of single-pill combinations where resources permit Medication access
effective antihypertensive drugs antihypertensive drug
Lack of stratified treatment Information about optimisation of blood pressure targets, Support RCTs that focus on optimisation of treatment targets, Standardised
treatment initiation, and therapy based on ethnicity, age, and risk initiation, and choice taking into account ethnicity, age, and risk† treatment
Blood pressure and health-care systems
Promote and ensure capacity and accountability of the health Promote and ensure accountability of the health system to Health-system
system to conduct surveillance and monitoring respond appropriately to blood pressure levels strengthening
RCT=randomised controlled trial. †Related to research.
Table 5: Summary of main problems and key actions
www.thelancet.com Vol 388 November 26, 2016 2695
The Lancet Commissions
or low alcohol use, and to encourage an active lifestyle. Technological applications in food systems, social media,
Success will require the adoption of policies that create and wearable and mobile technology
urban environments with working, living, and leisure Much more could be done to apply technology in food
conditions that support increased physical activity systems: for example, such efforts could ensure the
throughout the day. Similarly, increased year-round consumption of fruit and vegetables all year round.
availability of healthy, low-cost foods known to promote Especially in low-income and middle-income countries,
cardiovascular health—such as potassium-rich advanced technologies to facilitate distribution of foods to
vegetables—and decreased availability or increased all communities and basic technologies such as
pricing of unhealthy food items are an additional key refrigeration will result in increased consumption of
aspect of a healthy environment. Progressive regulatory fresh, nutritious foods, known to be beneficial in
and taxation schemes offer the opportunity both to improving vascular health. Technology already exists to
improve health directly and to generate funds that can be enforce and monitor food regulations, but can be applied
used to implement other high-value preventive strategies more widely to, for example, monitor the real-time
without immediate financial return. Such initiatives measurement and transmission of contents of packaged
should be driven by the health community, politicians, foods. Social media offers unprecedented potential to
teachers, city planners, architects, and a range of other affect systemic change in the understanding, prevention,
non-medical professions with strong civic and political and management of hypertension at all lifecourse stages.
leadership, because the financial benefits achieved will More than 3 billion people worldwide are active internet
take decades to accrue, but will be very large. users, with about 70% maintaining social media accounts.
Improved success of social media campaigns to educate,
Health literacy monitor, and control hypertension, but also to improve
Governments and civic society should encourage community health behaviour, can be achieved by improved
community-based strategies that promote health literacy, collaboration between different health professional
including early and continuous education on organisations (eg, specialists in hypertension, heart
hypertension as a so-called silent killer, and emphasise disease, stroke, kidney disease, cancer) and social-media
how a healthy lifestyle can help to avoid elevated blood public health platforms. For example, coordination of
pressure. Health-literacy education should empower efforts to existing activities such as World Health Day and
teachers to encourage children, through education, to World Hypertension Day can also help to attract
make healthy life choices, such as being active, avoiding widespread engagement.
smoking and alcohol, and eating fruits and vegetables The Commission recommends a close collaboration
regularly—all known to have a direct effect on between a wide range of stakeholders such as
cardiovascular health. Ideally, every child on the planet governments, the mobile communications industry,
should finish school as a health-literate adult. health-care professionals, the pharmaceutical industry,
and professional societies to not only develop and
distribute inexpensive, validated, and certified blood
Health–disease continuum pressure monitors, but also to ensure correct use through
simple mobile apps and online education endorsed by
organ damage Loss of QOL
Subclinical target- CV disease
the professional societies. In parallel, the Commission
Individualised strategies
Create a healthy environment
through strategies that accelerate
proposes that governments and health-care systems
socioeconomic improvements Avoidable threshold 3: respond to the national goals, targets, and indicators
development of clinical disease
and implementation of accepted outlined in the Sustainable Development Goals and the
health-promoting policies
WHO Global Monitoring Framework.
Avoidable threshold 2:
Universal access to development of subclinical
Key actions within diagnosis and evaluation in relation
measurement of blood pressure taget-organ damage to current global initiatives
Elevated BP
through inexpensive monitors
Population-based strategies
and establish global surveillance Better characterisation of individual phenotype will not
Universal understanding of
only improve hypertension risk assessment and help
Avoidable threshold 1: unhealthy and healthy lifestyles and guide the choice of intervention, but can also act to
development of elevated BP
blood pressure through endorsed, empower people towards greater ownership of their
early, and sustained education using
Healthy
new technologies condition and adherence to recommended intervention.
Enhanced phenotypic characterisation, including
Lifecourse identification of secondary hypertension, will also serve to
Childhood Early adulthood Middle-age Advanced age Elderly (>80 years) strengthen the quality of health information systems for
hypertension prevention, treatment, and control. Thus,
Figure 7: Key actions within prevention
The blue line represents the general lifecourse. The horizontal black dotted lines represent three avoidable clinical
important goals will be to ensure widespread access to
thresholds. The three green boxes represent the key actions within prevention. CV=cardiovascular. QOL=quality of valid and endorsed blood pressure devices, as well as
life. BP=blood pressure. enabling greater focus on global cardiovascular risk
2696 www.thelancet.com Vol 388 November 26, 2016
The Lancet Commissions
management instead of single risk-factor focus, and also bodies, and the pharmaceutical industry to join forces and
simplifying protocols to improve detection of secondary address these issues jointly and urgently. Not all questions
hypertension (figure 8). A method to help achieve these have been solved and a consensus on the exact research
goals will be to provide widely accessible and professional- question or implementation steps has to be reached as a
society-endorsed educational material by dissemination first step. We can therefore only highlight the areas that
to the general community and treating doctors. need urgent attention.
Provider-led efforts in education, empowerment, and
lifestyle interventions are often restricted to the time that Ensure access to affordable, high-quality medicine worldwide
a patient is in the clinic (when they might not be receptive As the best-documented antihypertensive therapies are
to such efforts), whereas online resources have unlimited now off patent, a minimum recommendation is that at
availability and provide great opportunity for widespread least one of each class of antihypertensive medication
education. Endorsement and promotion of online should be available to all individuals around the world.
educational material by professional societies related to Limitations to access include regulatory, political, and
hypertension should help to disseminate appropriate corporate factors. Where resources allow, single-pill
information and advocate against erroneous material. combination therapy should be available. Future research
This endorsement should be consistent with national should focus on the development of novel therapeutic
and international recommendations and can serve as a approaches based on improved understanding of
reassurance that the content being accessed is based on underlying pathophysiology. Combination therapy
the most up-to-date clinical knowledge. Resources for should also be expanded. Within antihypertensive
patients and doctors about blood pressure measurement classes, there should be a focus on improving pharma-
should be with preference for home blood pressure, cokinetic profiles. Such changes could further reduce
ambulatory blood pressure, and automated, unobserved side-effect profiles and improve adherence.
blood pressure methods. Modest investments in strategies to improve the
In a similar manner, professional societies could also availability and uptake of effective blood-pressure-lowering
give consideration to providing a seal of approval or medications, including investments in the development of
certification of blood pressure devices meeting appropriate systems that identify people who will benefit from therapy
accuracy standards, which is particularly important given and deliver appropriate treatment, promise huge benefits
the rapid developments in wearable technologies marketed that would probably be extremely cost-effective. Global,
without validation testing according to current inter- concerted action between governments, industry, civil
national expectations.162 Active warnings on substandard society, and international organisations has made HIV
devices can be provided. These options would help to therapy available at affordable costs to patients in low-
safeguard measurement quality more broadly and might income and middle-income countries, and similar efforts
even provide a potential source of revenue for professional are currently underway for treatment of hepatitis C.472
societies. The seal of approval could, in turn, be used by There is no reason why concerted strategies with the goal
manufacturers for marketing. Mechanisms to manage
cross-society coordination and harmonisation of Health–disease continuum
messaging in these efforts will be needed. It will also be
organ damage Loss of QOL
Subclinical target- CV disease
important to develop resources that are accessible and
empowering to doctors, including simplified guidelines Better identification of people Individualised strategies
with secondary hypertension
with truncated flow charts addressing management of through endorsed and simple flow
Avoidable threshold 3:
development of clinical disease
global cardiovascular risk and identification of secondary charts
hypertension to aid examination and treatment decisions.
All material endorsed by professional societies related to
hypertension should be produced with standardised Better quality of blood Avoidable threshold 2:
pressure measurements development of subclinical
instructions that are clear and easy to follow for the end through endorsed protocols, target-organ damage
Elevated BP
Population-based strategies
user, to enable wide uptake into different health-care and certified and validated
monitors
services beyond those that focus on cardiovascular disease
Better identification of people
(eg, HIV/AIDS services) and into under-resourced regions. Avoidable threshold 1:
at high risk through endorsed
development of elevated BP
education of patients and
health-care professionals
Healthy
Key actions within pharmacological prevention and
treatment in relation to current global initiatives
Introduction Lifecourse
Our recommendations relate to affordable therapies, Childhood Early adulthood Middle-age Advanced age Elderly (>80 years)
monitoring and self-monitoring of treatment, composition
Figure 8: Key actions within diagnosis and evaluation
of health-care teams, risk assessment, and decisional
The blue line represents the general lifecourse. The horizontal black dotted lines represent three avoidable clinical
algorithms (figure 9). The Commission encourages the thresholds. The three blue boxes represent the key actions within diagnosis and evaluation. CV=cardiovascular.
scientific community, health-care providers, funding QOL=quality of life. BP=blood pressure.
www.thelancet.com Vol 388 November 26, 2016 2697
The Lancet Commissions
to make quality treatment available worldwide should not provider experience. Examples of these provider-related
be successful in hypertension. choices are most promising lifestyle modifications; when
to add pharmacological antihypertensive treatment; use
Extend health-care workforce task sharing of lifetime cardiovascular risk versus 10-year risk; initial
An extension of existing health-care workforce capacity medical treatment strategies (eg, choice of drugs,
can be achieved at modest cost by promoting team-based monotherapy vs combination therapy); titration strategies;
care and task sharing. Especially in low-income and and monitoring of treatment success (monitoring blood
middle-income countries, where health-care professionals pressure alone or alongside target-organ damage).
are too scarce to effectively reach the population at risk, it Algorithms developed by professional societies and
is crucial to engage communities and train community health-care institutions based on the best evidence are
health workers to detect and initiate treatment of rarely adopted or applied consistently across institutions
hypertension. Data showing this approach to be feasible by all providers.
and effective are accumulating. Even well-resourced This Commission sees the urgent need to develop and
countries have suboptimal recognition of blood-pressure- implement simple algorithms that inform health-care
related cardiovascular risk, and inconsistent assessment professionals precisely on the required diagnostic and
and monitoring. Accordingly, more comprehensive therapeutic steps. Such algorithms should be evidence
strategies using approaches beyond opportunistic based, or evidence from pragmatic and prospective
screening at medical visits for other purposes are required. clinical studies could be used. The potential for cost
The approaches successfully used in childhood vaccination savings through standardisation of diagnosis and therapy
for infectious disease offer lessons in this regard. New extends to the more targeted use of specialist services for
models need to be developed and carefully assessed in the minority of patients with complex issues, whereas
clinical trials. Through task sharing and alternative most patients could be managed by general practitioners
community points of blood pressure measurement, we and allied health-care professionals in partnership, with
need to develop efficient systems for health-care delivery appropriate means for patient empowerment and self-
that are held accountable for monitoring blood pressure monitoring.
levels in their populations and for acting appropriately. Implementation of simple evidence-based algorithms
that standardise evaluation and treatment of hypertension
Evidence-based decisional algorithms and stratified treatment will indirectly identify areas with less evidence and create
strategies a perfect basis for investigator-initiated prospective
For the PATHWAY studies see Although the current management of hypertension is studies on treatment strategies. The PATHWAY studies
www.bhsoc.org/research/ based on principles regarding assessment of absolute risk show that investigator-initiated studies of treatment
pathway-project
and blood pressure reduction that are supported by strong strategies are possible and can lead to clear answers. This
evidence, many important parts of antihypertensive Commission, therefore, encourages the scientific
treatment are often applied on the basis of individual community to develop and define treatment strategies
and then test them in clinical trials. Furthermore, the
Health–disease continuum
knowledge of the effects of age, social background,
culture, and ethnicity on antihypertensive treatment is
organ damage Loss of QOL
Subclinical target- CV disease
Individualised strategies
scarce. Therefore, the Commission encourages establish-
Universal access to affordable,
high-quality, and effective
ment of international collaborations to combine existing
antihypertensive drugs through Avoidable threshold 3:
development of clinical disease
population surveys and create large web-based
collaboration between all major registries—using cloud computing technology—based
stakeholders
on data generated by patients’ use of widely available,
Expand the workforce engaged in Avoidable threshold 2: easy to use, certified apps, following the simple evidence-
development of subclinical
the management of blood pressure based algorithms mentioned above.
target-organ damage
through task sharing and the use of
Elevated BP
endorsed education of community
Population-based strategies
health workers (includes health-care Key actions within health-care systems
system accountability) Treatment approaches stratified Reducing raised blood pressure is one of the key targets
according to age, cardiovascular risk,
Avoidable threshold 1:
development of elevated BP and social, cultural, and ethnic of the WHO Global Monitoring Framework aimed at
differences through endorsed education decreasing deaths from non-communicable diseases
of health–care professionals and
Healthy
initiation of new research globally. Strengthening health systems, which encom-
passes all of those structures responsible for advancing
Lifecourse health from population surveillance to public health and
Childhood Early adulthood Middle-age Advanced age Elderly (>80 years) clinical care delivery, is an essential overarching goal
required not only for preventing and controlling
Figure 9: Key actions within pharmacological prevention and treatment
The blue line represents the general lifecourse. The horizontal black dotted lines represent three avoidable clinical
hypertension but to advance population health at large.
thresholds. The three red boxes represent the key actions within pharmacological prevention and treatment. All of the key actions noted earlier in this report
CV=cardiovascular. QOL=quality of life. BP=blood pressure. ultimately rely upon highly functioning health systems
2698 www.thelancet.com Vol 388 November 26, 2016
The Lancet Commissions
to be implemented successfully and sustainably. This A multifaceted approach to the key actions
includes actions related to creating health-promoting Hypertension and all its associated complications are
environments, to assure access to affordable quality products of a lifelong interplay of individual and
medications, and to establish care delivery systems that environmental factors, and, therefore, a multifaceted
produce equitable and accountable health outcomes. approach to this growing global problem is essential. The
Universal health coverage, which ensures everyone key actions proposed by the Commission (figure 10) are
access to the benefits of the health system without targeted at different populations, age groups, groups of
financial hardship related to payment, is a recognised health professionals and social workers, and groups of
prerequisite, and strongly supported by this Commission, individuals at different stages of hypertension; the
WHO, and the UN. Many different actions have to be actions are either dominated by programmes and system
implemented in parallel to improve management of change when evidence is convincing and by research
hypertension globally. Therefore, it is necessary to when evidence is missing.
develop surveillance models, taking advantage of new The key actions of this report follow from the
technologies that can measure the needs of the identification of the most pressing needs on a global level.
population, assess the functioning of the health system, Hypertension will—at some point in life—affect almost
and guide improvements in the system. Government every individual in the world, many of whom live in
investment in health information systems at all levels is countries with very few economic resources. Therefore,
essential to combine these many streams of actions the key actions in this report are mostly key actions at the
against hypertension in one comprehensive approach population level. Furthermore, in light of the massive
under the framework of health systems. burden of hypertension in low-income and middle-income
Health–disease continuum
Individualised strategies
Better identification of people
Loss of QOL
Treatment approaches stratified according to age,
CV disease
cardiovascular risk, and social, cultural, and ethnic with secondary hypertension
differences through endorsed education of health- through endorsed and simple flow
care professionals and initiation of new research charts
Avoidable threshold 3:
development of clinical disease
Universal access to affordable, high-quality,
and effective antihypertensive drugs through
Subclinical target-
collaboration between all major stakeholders
organ damage
Expand the workforce engaged in the
management of blood pressure through
task sharing and the use of endorsed
Better identification of people at high education of community health workers
risk through endorsed education of patients Avoidable threshold 2: (includes health care system
and health-care professionals development of subclinical accountability)
target-organ damage
Elevated BP
Better quality of blood pressure Universal access to measurement of blood pressure
measurements through endorsed protocols, through inexpensive monitors and establish global
and certified and validated monitors surveillance
Avoidable threshold 1: Promote and ensure capacity and accountability
development of elevated BP of the health system to conduct surveillance and
monitoring, and respond appropriately to blood
Population-based strategies
pressure levels
Healthy
Create a healthy environment through
strategies that accelerate socioeconomic
improvements and implementation of Universal understanding of unhealthy and healthy
accepted health-promoting policies lifestyles and blood pressure through endorsed, early,
and sustained education using new technologies
Lifecourse
Childhood Early adulthood Middle-age Advanced age Elderly (>80 years)
Figure 10: Summary of all key action points
The blue line represents the general lifecourse. The horizontal black dotted lines represent three avoidable clinical thresholds. The green, blue, or red boxes represent the key
actions within prevention, diagnosis and evaluation, and pharmacological prevention and treatment. CV=cardiovascular. QOL=quality of life. BP=blood pressure.
www.thelancet.com Vol 388 November 26, 2016 2699
The Lancet Commissions
countries, we have explicitly pursued a globally feasible engage civil society; political and partner commitment to
approach, partly by leveraging new technologies. obtain resources and support for effective action including
Overall, the Commission suggests intervening in related health-system strengthening initiatives such as
parallel throughout the spectrum of risk from population universal health coverage.473 In cardiovascular prevention it
level to patients at high cardiovascular risk. The proposed is crucial to reduce risk factors, including high blood
interventions (the key actions) consist of a mixture of pressure, tobacco smoking and second-hand smoke
research, development, programmes, and system change exposure, exposure to air pollution, high BMI, physical
all leading to the creation of a health-promoting inactivity, alcohol use, and diets low in fruits and vegetables
environment (figure 1). They build on the idea of and high in sodium and saturated fats both at individual
empowerment: empowerment of individuals through (clinical) and population levels. The Commission supports
broad health education, which is a prerequisite for an the WHO Global Monitoring Framework initiative to
individual to make informed choices and to take reduce the high-value prevention targets, which can be
ownership of their condition; empowerment of effectively addressed through implementing the so-called
communities with socioeconomic difficulties to offer best buys for prevention of non-communicable diseases.452
medical care to all individuals at risk of developing The Commission proposes a unifying implementation
hypertension and cardiovascular disease; and em- plan, articulated as a technical package, designed to
powerment of the medical community by offering support two general and interelated areas: prevention
simpler and more efficient tools to manage hypertension. and treatment. Each area will include selected high
priority and scalable interventions that can mobilise,
Global technical package for hypertension commit, and boost international and national capabilities.
As noted in the introduction to this report, the ultimate The prevention-related technical package would cover
aim of this Commission is to generate a globally unifying improved public understanding of unhealthy and healthy
campaign to prevent raised blood pressure, improve the lifestyles and blood pressure and its consequences, policy
management of elevated blood pressure, and reduce the and environmental approaches to promote health and
impact of hypertension all over the world. The support healthy behaviours, and improved access to
Commission has identified ten key actions that are effective health-care delivery systems and use of
additive and synergistic. They range from population- preventive and clinical services, and better cross-talks
based environmental policies aimed at shifting the between community programmes and clinical services.
population distribution of blood pressure downward by We envisage the treatment package to include standard
supporting healthier lifestyles and behaviours, to more protocols for investigation (diagnosis and risk
individualised approaches targeted at high-risk groups stratification), treatment (stratified and risk based), and
with hypertension and increased cardiovascular risk. monitoring, and team-based care, task sharing, and
Interventions aimed at individuals include effective and workforce development, with decentralised, community-
good-quality antihypertensive treatment with the aim to based, and patient-centred care, and training and capacity
reduce the size of the upper population distribution tail building. The treatment package should also include
of blood pressure. As such, the Commission recognises access to affordable medications, technology, and health
the importance of bridging public health, health-care care, with promotion of access to a high-quality core set
systems, and clinical practice. The actions we have of medications, including fixed-dose combination pills at
identified are many, and full implementation will require affordable cost to improve adherence. Finally, the
diligence and persistence over time. treatment package should include enhanced surveillance,
Although the details of roll-out will be refined over time patient registries, and information systems to monitor
with input and leadership from a variety of stakeholders trends in hypertension management, ensure
from local to global, we believe it is useful to reflect on accountability and equitable outcomes, and promote
approaches used by other major global efforts to advance interoperable information systems to monitor imple-
health. Public health programmes, including smallpox mentation needs and effectiveness of interventions.
eradication, tuberculosis control, tobacco control, polio
eradication, and others, have made progress by addressing Future plans after this report
six key areas: innovation to develop the evidence base for It is the intention and the ambition of The Lancet and the
action; a technical package of a small number of high- Commission on hypertension that this report should be a
priority, evidence-based interventions that together will step towards an enhanced collective action to implement
have a major impact; effective performance management, suggested actions to improve the management of blood
especially through rigorous, real-time monitoring, pressure and reduce the impact of elevated blood
evaluation, and programme improvement; partnerships pressure globally. With this report in hand, the
and coalitions with public-sector and private-sector Commission will contact hypertension organisations
organisations; communication of accurate and timely including the international, regional, and national
information to the health-care community, decision societies, as well as other relevant international agencies
makers, and the public to effect behaviour changes and (including cardiology, neurology, and nephrology
2700 www.thelancet.com Vol 388 November 26, 2016
The Lancet Commissions
societies) to propose global alliance. With the support of 2 Tunstall-Pedoe H, Connaghan J, Woodward M, Tolonen H,
these professional societies, together we will carry Kuulasmaa K. Pattern of declining blood pressure across replicate
population surveys of the WHO MONICA project, mid-1980s to
forward the mission to draw up a broad-based campaign mid-1990s, and the role of medication. BMJ 2006; 332: 629–35.
of advocacy and action, involving governments, industry, 3 Danaei G, Finucane MM, Lin JK, et al, and the Global Burden of
civic and consumer organisations, and health Metabolic Risk Factors of Chronic Diseases Collaborating Group
(Blood Pressure). National, regional, and global trends in systolic
professional bodies. The Commission will call for blood pressure since 1980: systematic analysis of health
relevant international, national, and subnational examination surveys and epidemiological studies with
786 country-years and 5·4 million participants. Lancet 2011;
agencies, policy makers, researchers, public-health 377: 568–77.
practitioners, development agencies, and donors to 4 Mills KT, Bundy JD, Kelly TN, et al. Global disparities of
champion the recommendations of the report. The hypertension prevalence and control: a systematic analysis of
campaign will not just be a health campaign, but a much population-based studies from 90 countries. Circulation 2016;
134: 441–50.
broader multisectoral campaign, bringing together of all 5 Stampfer MJ, Hu FB, Manson JE, Rimm EB, Willett WC.
elements of society to address the lifelong health burden Primary prevention of coronary heart disease in women through
of elevated blood pressure using the lifecourse strategy diet and lifestyle. N Engl J Med 2000; 343: 16–22.
6 Hoevenaar-Blom MP, Spijkerman AM, Kromhout D,
described in the report. This goal cannot be realised Verschuren WM. Sufficient sleep duration contributes to lower
without accelerated and substantial commitment from cardiovascular disease risk in addition to four traditional lifestyle
donors and national governments. factors: the MORGEN study. Eur J Prev Cardiol 2014; 21: 1367–75.
7 Raitakari OT, Juonala M, Kähönen M, et al. Cardiovascular risk
Contributors factors in childhood and carotid artery intima-media thickness in
All authors contributed to strategic planning, literature search, data adulthood: the Cardiovascular Risk in Young Finns Study. JAMA
interpretation, and the writing and revision of the report. 2003; 290: 2277–83.
Declaration of interests 8 Aatola H, Hutri-Kähönen N, Juonala M, et al. Lifetime risk factors
and arterial pulse wave velocity in adulthood: the cardiovascular risk
MHO reports grants from Centers for Disease Control and Prevention,
in young Finns study. Hypertension 2010; 55: 806–11.
during the conduct of the study, and personal fees from Boehringer
9 Oikonen M, Nuotio J, Magnussen CG, et al. Repeated blood
Ingelheim, outside the submitted work. PB reports grants from Servier,
pressure measurements in childhood in prediction of hypertension
and grants and personal fees from Withings, during the conduct of the in adulthood. Hypertension 2016; 67: 41–47.
study. JAC reports grants and personal fees from BMS, Fukuda Denshi,
10 Pälve KS, Pahkala K, Magnussen CG, et al. Association of physical
and Microsoft Research, and personal fees from OPKO Healthcare, activity in childhood and early adulthood with carotid artery
Vital Labs, and Merck, during the conduct of the study. JAC is named elasticity 21 years later: the cardiovascular risk in Young Finns
inventor in a patent application (pending) for the use of inorganic nitrate Study. J Am Heart Assoc 2014; 3: e000594.
and nitrite in heart failure and preserved ejection fraction. VP reports 11 Ferreira I, van de Laar RJ, Prins MH, Twisk JW, Stehouwer CD.
grants from Abbvie, Astellas, Bayer, Baxter, GSK, Bristol-Myers Squibb Carotid stiffness in young adults: a life-course analysis of its early
Company, Eli Lilly, Servier, Pfizer, and the National Health and Medical determinants: the Amsterdam Growth and Health Longitudinal
Research Council; personal fees from Servier; other support from Study. Hypertension 2012; 59: 54–61.
Janssen, Boehringer Ingelheim, AstraZeneca, Novo Nordisk, Pharmalink, 12 Liu K, Daviglus ML, Loria CM, et al. Healthy lifestyle through
and Relypsa, outside the submitted work. ERR reports grants from young adulthood and the presence of low cardiovascular disease
Amgen, Sanofi, and Unilever, outside the submitted work. GS reports risk profile in middle age: the Coronary Artery Risk Development in
grants from AtCor Medical, and personal fees from Fukuda-Denshi, (Young) Adults (CARDIA) study. Circulation 2012; 125: 996–1004.
Servier, Daiichi-Sankyo, Menarini, Novartis, and Guidotti, outside the 13 Ehret GB, Munroe PB, Rice KM, et al, and the International
submitted work. JES has received equipment and support in kind for Consortium for Blood Pressure Genome-Wide Association Studies,
research projects related to blood pressure from AtCor Medical and IEM the CARDIoGRAM consortium, the CKDGen Consortium, the
GmbH. JGW reports personal fees from Daiichi-Sankyo, MSD, Novartis, KidneyGen Consortium, the EchoGen consortium, and the
CHARGE-HF consortium. Genetic variants in novel pathways
Pfizer, Sanofi, and Servier, outside the submitted work. All other authors
influence blood pressure and cardiovascular disease risk.
declare no competing interests. The findings and conclusions in this
Nature 2011; 478: 103–09.
report are those of the authors and do not necessarily represent the
14 Ference BA, Julius S, Mahajan N, Levy PD, Williams KAS Sr,
official position of the Centers for Disease Control and Prevention.
Flack JM. Clinical effect of naturally random allocation to lower
Acknowledgments systolic blood pressure beginning before the development of
We are extremely grateful to Prof Neil Poulter, Prof John Chalmers, hypertension. Hypertension 2014; 63: 1182–88.
Prof Stephane Laurent, and Prof Majid Ezzati for face-to-face critique and 15 Lonn EM, Bosch J, Lopez-Jaramillo P, et al. Blood-pressure lowering
advice during preparation of the report. The International Society for in intermediate-risk persons without cardiovascular disease.
Hypertension, Odense University Hospital, University of Southern N Engl J Med 2016; 374: 2009–20.
Denmark, and US Center for Disease Control generously provided 16 Mente A, O’Donnell M, Rangarajan S, et al. Associations of urinary
financial support for Commission meetings. And we are grateful to sodium excretion with cardiovascular events in individuals with and
without hypertension: a pooled analysis of data from four studies.
Prof Rhian Touyz and the local organisers of the 50th Anniversary ISH
Lancet 2016; published online May 20. DOI:10.1016/S0140-
meeting in Seoul for providing time in the programme to present and 6736(16)30467-6.
discuss the report of the Commission. We thank Manan Pareek
17 Scuteri A, Lattanzio F, Bernabei R. The life-course approach to
(Department of Internal Medicine, Holbæk Hospital and Centre for chronic disease: the active and healthy ageing view/perspective.
Individualized Medicine in Arterial Diseases, Odense University Hospital, J Am Geriatr Soc 2016; published online July 26. DOI:10.1111/
University of Southern Denmark, Denmark, and Brigham and Women’s jgs.14271.
Hospital Heart & Vascular Center, Harvard Medical School, Boston, MA, 18 WHO. A global brief on hypertension: silent killer, global public
USA) for his help with the references and general technical support. health crisis. 2013. http://www.who.int/cardiovascular_diseases/
References publications/global_brief_hypertension/en/ (accessed
1 Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines Dec 28, 2015).
for the management of arterial hypertension: the Task Force for the 19 Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK,
Management of Arterial Hypertension of the European Society of He J. Global burden of hypertension: analysis of worldwide data.
Hypertension (ESH) and of the European Society of Cardiology Lancet 2005; 365: 217–23.
(ESC). Eur Heart J 2013; 34: 2159–219.
www.thelancet.com Vol 388 November 26, 2016 2701
The Lancet Commissions
20 Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of 40 Williamson JD, Supiano MA, Applegate WB, et al. Intensive vs
burden of disease and injury attributable to 67 risk factors and risk standard blood pressure control and cardiovascular disease
factor clusters in 21 regions, 1990–2010: a systematic analysis for outcomes in adults aged >/=75 years: a randomized clinical trial.
the Global Burden of Disease Study 2010. Lancet 2012; 380: 2224–60. JAMA 2016; 315: 2673–82.
21 Whelton PK, He J, Appel LJ, et al, and the National High Blood 41 The ACCORD Study Group. Effects of intensive blood-pressure
Pressure Education Program Coordinating Committee. Primary control in type 2 diabetes mellitus. N Engl J Med 2010; 362: 1575–85.
prevention of hypertension: clinical and public health advisory from 42 Beckett NS, Peters R, Fletcher AE, et al, and the HYVET Study
The National High Blood Pressure Education Program. JAMA 2002; Group. Treatment of hypertension in patients 80 years of age or
288: 1882–88. older. N Engl J Med 2008; 358: 1887–98.
22 Andersson OK, Almgren T, Persson B, Samuelsson O, Hedner T, 43 le Noble JL, Tangelder GJ, Slaaf DW, van Essen H, Reneman RS,
Wilhelmsen L. Survival in treated hypertension: follow up study Struyker-Boudier HA. A functional morphometric study of the
after two decades. BMJ 1998; 317: 167–71. cremaster muscle microcirculation in young spontaneously
23 Poulter NR, Prabhakaran D, Caulfield M. Hypertension. hypertensive rats. J Hypertens 1990; 8: 741–48.
Lancet 2015; 386: 801–12. 44 Pladys P, Sennlaub F, Brault S, et al. Microvascular rarefaction
24 Kannel WB. Blood pressure as a cardiovascular risk factor: and decreased angiogenesis in rats with fetal programming of
prevention and treatment. JAMA 1996; 275: 1571–76. hypertension associated with exposure to a low-protein diet in
25 World Bank, WHO. Tracking universal health coverage: first global utero. Am J Physiol Regul Integr Comp Physiol 2005; 289: R1580–88.
monitoring report. 2015. http://reliefweb.int/report/world/ 45 Landau J, Davis E. Capillary thinning and high capillary
tracking-universal-health-coverage-first-global-monitoring-report blood-pressure in hypertension. Lancet 1957; 272: 1327–30.
(accessed March 10, 2016). 46 Montezano AC, Dulak-Lis M, Tsiropoulou S, Harvey A,
26 Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, and the Briones AM, Touyz RM. Oxidative stress and human hypertension:
Prospective Studies Collaboration. Age-specific relevance of usual vascular mechanisms, biomarkers, and novel therapies.
blood pressure to vascular mortality: a meta-analysis of individual Can J Cardiol 2015; 31: 631–41.
data for one million adults in 61 prospective studies. Lancet 2002; 47 Kaess BM, Rong J, Larson MG, et al. Aortic stiffness, blood pressure
360: 1903–13. progression, and incident hypertension. JAMA 2012; 308: 875–81.
27 Xie X, Atkins E, Lv J, et al. Effects of intensive blood pressure 48 Laurent S, Boutouyrie P. The structural factor of hypertension:
lowering on cardiovascular and renal outcomes: updated systematic large and small artery alterations. Circ Res 2015; 116: 1007–21.
review and meta-analysis. Lancet 2015; 387: 435–43. 49 Nilsson PM, Boutouyrie P, Laurent S. Vascular aging: a tale of
28 Blacher J, Evans A, Arveiler D, et al, and the PRIME Study Group. EVA and ADAM in cardiovascular risk assessment and prevention.
Residual cardiovascular risk in treated hypertension and Hypertension 2009; 54: 3–10.
hyperlipidaemia: the PRIME Study. J Hum Hypertens 2010; 50 Vlachopoulos C, Aznaouridis K, O’Rourke MF, Safar ME, Baou K,
24: 19–26. Stefanadis C. Prediction of cardiovascular events and all-cause
29 Lawes CM, Vander Hoorn S, Law MR, Elliott P, MacMahon S, mortality with central haemodynamics: a systematic review and
Rodgers A. Blood pressure and the global burden of disease 2000. meta-analysis. Eur Heart J 2010; 31: 1865–71.
Part II: estimates of attributable burden. J Hypertens 2006; 51 Ben-Shlomo Y, Spears M, Boustred C, et al. Aortic pulse wave
24: 423–30. velocity improves cardiovascular event prediction: an individual
30 Asayama K, Satoh M, Murakami Y, et al, and the Evidence for participant meta-analysis of prospective observational data from
Cardiovascular Prevention From Observational Cohorts in Japan 17,635 subjects. J Am Coll Cardiol 2014; 63: 636–46.
(EPOCH-JAPAN) Research Group. Cardiovascular risk with and 52 O’Rourke MF, Safar ME, Dzau V. The Cardiovascular Continuum
without antihypertensive drug treatment in the Japanese general extended: aging effects on the aorta and microvasculature.
population: participant-level meta-analysis. Hypertension 2014; Vasc Med 2010; 15: 461–68.
63: 1189–97.
53 James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline
31 Britt H, Miller G, Charles J, et al. General practice activity in for the management of high blood pressure in adults: report from
Australia 2009–10. 2010. http://www.aihw.gov.au/publication- the panel members appointed to the Eighth Joint National
detail/?id=6442472433 (accessed Dec 28, 2015). Committee (JNC 8). JAMA 2014; 311: 507–20.
32 Briganti EM, Shaw JE, Chadban SJ, et al, and the Australian 54 National Institute for Health and Care Excellence. Hypertension in
Diabetes, Obesity and Lifestyle Study (AusDiab). Untreated adults: diagnosis and management. NICE guidelines [CG127]. 2011.
hypertension among Australian adults: the 1999–2000 Australian https://www.nice.org.uk/guidance/cg127 (accessed Dec 28, 2015).
Diabetes, Obesity and Lifestyle Study (AusDiab). Med J Aust 2003;
55 Fok H, Cruickshank JK. Future treatment of hypertension: shifting
179: 135–39.
the focus from blood pressure lowering to arterial stiffness
33 Chow CK, Teo KK, Rangarajan S, et al, and the PURE modulation? Curr Hypertens Rep 2015; 17: 67.
(Prospective Urban Rural Epidemiology) Study investigators.
56 Ibrahim MM, Damasceno A. Hypertension in developing countries.
Prevalence, awareness, treatment, and control of hypertension in
Lancet 2012; 380: 611–19.
rural and urban communities in high-, middle-, and low-income
countries. JAMA 2013; 310: 959–68. 57 Gillespie CD, Kuklin EV, Briss PA, Blair NA, Hong Y. Vital signs:
prevalence, treatment, and control of hypertension—United States,
34 Olsen MH, Spencer S. A global perspective on hypertension:
1999–2002 and 2005–2008. MMWR Morb Mortal Wkly Rep 2011;
a Lancet Commission. Lancet 2015; 386: 637–38.
60: 103–08.
35 Lozano R, Naghavi M, Foreman K, et al. Global and regional
58 Nwankwo T, Yoon SS, Burt V, Gu Q. Hypertension among adults in
mortality from 235 causes of death for 20 age groups in 1990 and
the United States: National Health and Nutrition Examination
2010: a systematic analysis for the Global Burden of Disease Study
Survey, 2011–2012. NCHS data brief, no 133. Hyattsville, MD:
2010. Lancet 2012; 380: 2095–128.
National Center for Health Statistics, 2013.
36 United Nations, Department of Economic and Social Affairs,
59 Gillespie CD, Hurvitz KA. Prevalence of hypertension and
Population Division. World population prospects, the 2015 revision.
controlled hypertension—United States, 2007–2010.
2015. http://esa.un.org/unpd/wpp/ (accessed May 10, 2016).
MMWR Morb Mortal Wkly Rep 2013; 62: 144–48.
37 Odden MC, Coxson PG, Moran A, Lightwood JM, Goldman L,
60 Yoon SS, Burt V, Louis T, Carroll MD. Hypertension among adults
Bibbins-Domingo K. The impact of the aging population on
in the United States, 2009–2010. NCHS data brief, no 107.
coronary heart disease in the United States. Am J Med 2011;
Hyattsville, MD: National Center for Health Statistics, 2012.
124: 827–33.e5.
61 New York City Department of Health and Mental Hygiene. Epiquery:
38 MRC Working Party. Medical Research Council trial of treatment of
NYC interactive health data system—community health survey 2013.
hypertension in older adults: principal results. BMJ 1992;
https://a816-healthpsi.nyc.gov/epiquery/ (accessed March 11, 2016).
304: 405–12.
62 Angell SY, Garg RK, Gwynn RC, Bash L, Thorpe LE, Frieden TR.
39 Wright JT Jr, Williamson JD, Whelton PK, et al, and the SPRINT
Prevalence, awareness, treatment, and predictors of control of
Research Group. A randomized trial of intensive versus standard
hypertension in New York City. Circ Cardiovasc Qual Outcomes
blood-pressure control. N Engl J Med 2015; 373: 2103–16.
2008; 1: 46–53.
2702 www.thelancet.com Vol 388 November 26, 2016
The Lancet Commissions
63 Office of Disease Prevention and Health Promotion. 83 Nanditha A, Ma RC, Ramachandran A, et al. Diabetes in Asia and
Social determinants of health. 2011. https://www.healthypeople. the Pacific: implications for the global epidemic. Diabetes Care 2016;
gov/2020/topics-objectives/topic/social-determinants-of-health 39: 472–85.
(accessed March 13, 2016). 84 Sofi F, Abbate R, Gensini GF, Casini A. Accruing evidence on benefits
64 Danaei G, Singh GM, Paciorek CJ, et al. The global cardiovascular of adherence to the Mediterranean diet on health: an updated
risk transition: associations of four metabolic risk factors with systematic review and meta-analysis. Am J Clin Nutr 2010; 92: 1189–96.
national income, urbanization, and Western diet in 1980 and 2008. 85 Domenech M, Roman P, Lapetra J, et al. Mediterranean diet reduces
Circulation 2013; 127: 1493–502, 1502.e1–8. 24-hour ambulatory blood pressure, blood glucose, and lipids:
65 GBD 2013 Risk Factors Collaborators, Forouzanfar MH, one-year randomized, clinical trial. Hypertension 2014; 64: 69–76.
Alexander L, et al. Global, regional, and national comparative risk 86 Estruch R, Ros E, Salas-Salvadó J, et al, and the PREDIMED Study
assessment of 79 behavioural, environmental and occupational, and Investigators. Primary prevention of cardiovascular disease with a
metabolic risks or clusters of risks in 188 countries, 1990–2013: Mediterranean diet. N Engl J Med 2013; 368: 1279–90.
a systematic analysis for the Global Burden of Disease Study 2013. 87 Appel LJ, Brands MW, Daniels SR, Karanja N, Elmer PJ, Sacks FM,
Lancet 2015; 386: 2287–323. and the American Heart Association. Dietary approaches to prevent
66 Falaschetti E, Mindell J, Knott C, Poulter N. Hypertension and treat hypertension: a scientific statement from the American
management in England: a serial cross-sectional study from 1994 to Heart Association. Hypertension 2006; 47: 296–308.
2011. Lancet 2014; 383: 1912–19. 88 Appel LJ, Moore TJ, Obarzanek E, et al, and the DASH
67 Rodgers A, Ezzati M, Vander Hoorn S, Lopez AD, Lin RB, Collaborative Research Group. A clinical trial of the effects of
Murray CJ, and the Comparative Risk Assessment Collaborating dietary patterns on blood pressure. N Engl J Med 1997; 336: 1117–24.
Group. Distribution of major health risks: findings from the 89 Cook NR, Appel LJ, Whelton PK. Lower levels of sodium intake and
Global Burden of Disease study. PLoS Med 2004; 1: e27. reduced cardiovascular risk. Circulation 2014; 129: 981–89.
68 WHO. Global status report on noncommunicable diseases 2010. 90 Mente A, O’Donnell MJ, Rangarajan S, et al, and the PURE
2011. http://www.who.int/nmh/publications/ncd_report2010/en/ Investigators. Association of urinary sodium and potassium
(accessed Dec 28, 2015). excretion with blood pressure. N Engl J Med 2014; 371: 601–11.
69 World Economic Forum. The global economic burden of 91 Adrogue HJ, Madias NE. Sodium and potassium in the
non-communicable diseases. 2011. http://www.weforum.org/ pathogenesis of hypertension. N Engl J Med 2007; 356: 1966–78.
reports/global-economic-burden-non-communicable-diseases 92 Kapil V, Khambata RS, Robertson A, Caulfield MJ, Ahluwalia A.
(accessed Dec 28, 2015). Dietary nitrate provides sustained blood pressure lowering in
70 Weber MA, Schiffrin EL, White WB, et al. Clinical practice hypertensive patients: a randomized, phase 2, double-blind,
guidelines for the management of hypertension in the community placebo-controlled study. Hypertension 2015; 65: 320–27.
a statement by the American Society of Hypertension and the 93 Siervo M, Lara J, Ogbonmwan I, Mathers JC. Inorganic nitrate and
International Society of Hypertension. J Hypertens 2014; 32: 3–15. beetroot juice supplementation reduces blood pressure in adults:
71 Kotseva K, De Bacquer D, Jennings C, et al, and the EUROASPIRE a systematic review and meta-analysis. J Nutr 2013; 143: 818–26.
Investigators. Adverse lifestyle trends counter improvements in 94 Lidder S, Webb AJ. Vascular effects of dietary nitrate (as found in
cardiovascular risk factor management in coronary patients. green leafy vegetables and beetroot) via the nitrate-nitrite-nitric
J Am Coll Cardiol 2015; 66: 1634–36. oxide pathway. Br J Clin Pharmacol 2013; 75: 677–96.
72 Lawes CM, Vander Hoorn S, Rodgers A, and the International 95 Nocon M, Hiemann T, Müller-Riemenschneider F, Thalau F, Roll S,
Society of Hypertension. Global burden of blood-pressure-related Willich SN. Association of physical activity with all-cause and
disease, 2001. Lancet 2008; 371: 1513–18. cardiovascular mortality: a systematic review and meta-analysis.
73 United Nations. Sustainable development goals. Transforming Eur J Cardiovasc Prev Rehabil 2008; 15: 239–46.
our world—the 2030 agenda for sustainable development. 2015. 96 Parker ED, Schmitz KH, Jacobs DR Jr, Dengel DR, Schreiner PJ.
https://sustainabledevelopment.un.org/?menu=1300 (accessed Physical activity in young adults and incident hypertension over
Dec 28, 2015). 15 years of follow-up: the CARDIA study. Am J Public Health 2007;
74 WHO. Global status report on noncommunicable diseases 2014. 97: 703–09.
http://www.who.int/nmh/publications/ncd-status-report-2014/en/ 97 Huai P, Xun H, Reilly KH, Wang Y, Ma W, Xi B. Physical activity
(accessed Dec 28, 2015). and risk of hypertension: a meta-analysis of prospective cohort
75 Donaldson EA, Waters HR, Arora M, Varghese B, Dave P, Modi B. studies. Hypertension 2013; 62: 1021–26.
A cost-effectiveness analysis of India’s 2008 prohibition of smoking 98 Diaz KM, Shimbo D. Physical activity and the prevention of
in public places in Gujarat. Int J Environ Res Public Health hypertension. Curr Hypertens Rep 2013; 15: 659–68.
2011; 8: 1271–86.
99 Berry JD, Willis B, Gupta S, et al. Lifetime risks for cardiovascular
76 Gaudreau K, Sanford CJ, Cheverie C, McClure C. The effect of a disease mortality by cardiorespiratory fitness levels measured at
smoking ban on hospitalization rates for cardiovascular and ages 45, 55, and 65 years in men: the Cooper Center Longitudinal
respiratory conditions in Prince Edward Island, Canada. Study. J Am Coll Cardiol 2011; 57: 1604–10.
PLoS One 2013; 8: e56102.
100 Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM. Influence of
77 Gortmaker SL, Swinburn BA, Levy D, et al. Changing the future of weight reduction on blood pressure: a meta-analysis of randomized
obesity: science, policy, and action. Lancet 2011; 378: 838–47. controlled trials. Hypertension 2003; 42: 878–84.
78 Roberto CA, Swinburn B, Hawkes C, et al. Patchy progress on 101 Stevens VJ, Obarzanek E, Cook NR, et al, and the Trials for the
obesity prevention: emerging examples, entrenched barriers, and Hypertension Prevention Research Group. Long-term weight loss
new thinking. Lancet 2015; 385: 2400–09. and changes in blood pressure: results of the Trials of Hypertension
79 Krug EG. Trends in diabetes: sounding the alarm. Lancet 2016; Prevention, phase II. Ann Intern Med 2001; 134: 1–11.
387: 1485–86. 102 Caterson ID, Finer N, Coutinho W, et al. Maintained intentional
80 NCD Risk Factor Collaboration (NCD-RisC). Trends in adult weight loss reduces cardiovascular outcomes: results from the
body-mass index in 200 countries from 1975 to 2014: a pooled Sibutramine Cardiovascular OUTcomes (SCOUT) trial.
analysis of 1698 population-based measurement studies with Diabetes Obes Metab 2012; 14: 523–30.
19·2 million participants. Lancet 2016; 387: 1377–96. 103 Lightwood JM, Glantz SA. Declines in acute myocardial infarction
81 Global Burden of Metabolic Risk Factors for Chronic Diseases after smoke-free laws and individual risk attributable to secondhand
Collaboration. Cardiovascular disease, chronic kidney disease, smoke. Circulation 2009; 120: 1373–79.
and diabetes mortality burden of cardiometabolic risk factors from 104 Celermajer DS, Sorensen KE, Georgakopoulos D, et al. Cigarette
1980 to 2010: a comparative risk assessment. smoking is associated with dose-related and potentially reversible
Lancet Diabetes Endocrinol 2014; 2: 634–47. impairment of endothelium-dependent dilation in healthy young
82 Crino M, Sacks G, Vandevijvere S, Swinburn B, Neal B. adults. Circulation 1993; 88: 2149–55.
The influence on population weight gain and obesity of the 105 Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association
macronutrient composition and energy density of the food supply. of alcohol consumption with selected cardiovascular disease outcomes:
Curr Obes Rep 2015; 4: 1–10. a systematic review and meta-analysis. BMJ 2011; 342: d671.
www.thelancet.com Vol 388 November 26, 2016 2703
The Lancet Commissions
106 Briasoulis A, Agarwal V, Messerli FH. Alcohol consumption and 124 WHO. School and youth health. 2016. http://www.who.int/school_
the risk of hypertension in men and women: a systematic review youth_health/en (accessed March 13, 2016).
and meta-analysis. J Clin Hypertens (Greenwich) 2012; 14: 792–98. 125 Taylor MJ, McCormick D, Shawis T, Impson R, Griffin M.
107 Zatu MC, Van Rooyen JM, Kruger A, Schutte AE. Alcohol intake, Activity-promoting gaming systems in exercise and rehabilitation.
hypertension development and mortality in black South Africans. J Rehabil Res Dev 2011; 48: 1171–86.
Eur J Prev Cardiol 2016; 23: 308–15. 126 Siegfried N, Pienaar DC, Ataguba JE, et al. Restricting or banning
108 Rainforth MV, Schneider RH, Nidich SI, Gaylord-King C, alcohol advertising to reduce alcohol consumption in adults and
Salerno JW, Anderson JW. Stress reduction programs in patients adolescents. Cochrane Database Syst Rev 2014; 11: CD010704.
with elevated blood pressure: a systematic review and meta-analysis. 127 Hofman KJ, Tollman SM. Population health in South Africa:
Curr Hypertens Rep 2007; 9: 520–28. a view from the salt mines. Lancet Glob Health 2013; 1: e66–67.
109 Park J, Lyles RH, Bauer-Wu S. Mindfulness meditation lowers 128 Harris JL, Bargh JA. Television viewing and unhealthy diet:
muscle sympathetic nerve activity and blood pressure in implications for children and media interventions.
African-American males with chronic kidney disease. Health Commun 2009; 24: 660–73.
Am J Physiol Regul Integr Comp Physiol 2014; 307: R93–101. 129 Torjesen I. BMA calls for 20% sugar tax to subsidise cost of fruit
110 Knowler WC, Barrett-Connor E, Fowler SE, et al, and the Diabetes and vegetables. BMJ 2015; 351: h3803.
Prevention Program Research Group. Reduction in the incidence of 130 Stafford N. Denmark cancels “fat tax” and shelves “sugar tax”
type 2 diabetes with lifestyle intervention or metformin. because of threat of job losses. BMJ 2012; 345: e7889.
N Engl J Med 2002; 346: 393–403.
131 Anand SS, Yusuf S, Vuksan V, et al. Differences in risk factors,
111 Hinderliter AL, Sherwood A, Craighead LW, et al. The long-term atherosclerosis, and cardiovascular disease between ethnic groups
effects of lifestyle change on blood pressure: one-year follow-up in Canada: the Study of Health Assessment and Risk in Ethnic
of the ENCORE study. Am J Hypertens 2014; 27: 734–41. groups (SHARE). Lancet 2000; 356: 279–84.
112 Chow CK, Redfern J, Hillis GS, et al. Effect of lifestyle-focused text 132 Scuteri A, Laurent S, Cucca F, et al, and the Metabolic Syndrome
messaging on risk factor modification in patients with coronary and Arteries Research (MARE) Consortium. Metabolic syndrome
heart disease: a randomized clinical trial. JAMA 2015; across Europe: different clusters of risk factors. Eur J Prev Cardiol
314: 1255–63. 2015; 22: 486–91.
113 Thakkar J, Kurup R, Laba TL, et al. Mobile telephone text messaging 133 Nilsson PM, Boutouyrie P, Cunha P, et al. Early vascular ageing in
for medication adherence in chronic disease: a meta-analysis. translation: from laboratory investigations to clinical applications in
JAMA Intern Med 2016; 176: 340–49. cardiovascular prevention. J Hypertens 2013; 31: 1517–26.
114 Glanz K, Bishop DB. The role of behavioral science theory in 134 Gorelick PB, Scuteri A, Black SE, et al. Vascular contributions to
development and implementation of public health interventions. cognitive impairment and dementia: a statement for healthcare
Annu Rev Public Health 2010; 31: 399–418. professionals from the American Heart Association/American
115 Kullo IJ, Jouni H, Olson JE, Montori VM, Bailey KR. Design of a Stroke Association. Stroke 2011; 42: 2672–713.
randomized controlled trial of disclosing genomic risk of coronary 135 Mozaffarian D, Fahimi S, Singh GM, et al. Global sodium
heart disease: the Myocardial Infarction Genes (MI-GENES) study. consumption and death from cardiovascular causes. N Engl J Med
BMC Med Genomics 2015; 8: 51. 2014; 371: 624–34.
116 Swinburn BA, Sacks G, Hall KD, et al. The global obesity pandemic: 136 Trieu K, Neal B, Hawkes C, et al. Salt reduction initiatives around
shaped by global drivers and local environments. Lancet 2011; the world: a systematic review of progress towards the global target.
378: 804–14. PLoS One 2015; 10: e0130247.
117 Lloyd-Sherlock P, Beard J, Minicuci N, Ebrahim S, Chatterji S. 137 Adler AJ, Taylor F, Martin N, Gottlieb S, Taylor RS, Ebrahim S.
Hypertension among older adults in low- and middle-income Reduced dietary salt for the prevention of cardiovascular disease.
countries: prevalence, awareness and control. Int J Epidemiol 2014; Cochrane Database Syst Rev 2014; 18: CD009217.
43: 116–28.
138 Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure
118 Schutte AE, Schutte R, Huisman HW, et al. Are behavioural risk of reduced dietary sodium and the Dietary Approaches to Stop
factors to be blamed for the conversion from optimal blood Hypertension (DASH) diet. DASH-Sodium Collaborative Research
pressure to hypertensive status in black South Africans? A 5-year Group. N Engl J Med 2001; 344: 3–10.
prospective study. Int J Epidemiol 2012; 41: 1114–23.
139 Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP,
119 Artinian NT, Fletcher GF, Mozaffarian D, et al, and the American Meerpohl JJ. Effect of lower sodium intake on health: systematic
Heart Association Prevention Committee of the Council on review and meta-analyses. BMJ 2013; 346: f1326.
Cardiovascular Nursing. Interventions to promote physical activity
140 He FJ, Li J, Macgregor GA. Effect of longer-term modest salt
and dietary lifestyle changes for cardiovascular risk factor reduction
reduction on blood pressure. Cochrane Database Syst Rev 2013;
in adults: a scientific statement from the American Heart
4: CD004937.
Association. Circulation 2010; 122: 406–41.
141 O’Donnell M, Mente A, Rangarajan S, et al. Urinary sodium and
120 Larsson SC, Akesson A, Wolk A. Healthy diet and lifestyle and risk of
potassium excretion, mortality, and cardiovascular events.
stroke in a prospective cohort of women. Neurology 2014; 83: 1699–704.
N Engl J Med 2014; 371: 612–23.
121 Piepoli MF, Hoes AW, Agewall S, et al. 2016 European Guidelines
142 O’Donnell MJ, Yusuf S, Mente A, et al. Urinary sodium and
on cardiovascular disease prevention in clinical practice:
potassium excretion and risk of cardiovascular events. JAMA 2011;
The Sixth Joint Task Force of the European Society of Cardiology
306: 2229–38.
and Other Societies on Cardiovascular Disease Prevention in
Clinical Practice (constituted by representatives of 10 societies and 143 Stolarz-Skrzypek K, Kuznetsova T, Thijs L, et al. Fatal and nonfatal
by invited experts): developed with the special contribution of the outcomes, incidence of hypertension, and blood pressure changes
European Association for Cardiovascular Prevention & in relation to urinary sodium excretion. JAMA 2011; 305: 1777–85.
Rehabilitation (EACPR). Eur J Prev Cardiol 2016; published online 144 He FJ, Pombo-Rodrigues S, Macgregor GA. Salt reduction in
May 23. DOI:10.1093/eurheartj/ehw106. England from 2003 to 2011: its relationship to blood pressure, stroke
122 Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC guideline on and ischaemic heart disease mortality. BMJ Open 2014; 4: e004549.
lifestyle management to reduce cardiovascular risk: a report of the 145 Barker DJ, Bull AR, Osmond C, Simmonds SJ. Fetal and placental
American College of Cardiology/American Heart Association Task size and risk of hypertension in adult life. BMJ 1990; 301: 259–62.
Force on Practice Guidelines. J Am Coll Cardiol 2014; 63: 2960–84. 146 Curhan GC, Chertow GM, Willett WC, et al. Birth weight and adult
123 Arena R, Guazzi M, Lianov L, et al, and the AHA Writing Group, hypertension and obesity in women. Circulation 1996; 94: 1310–15.
the ESC/EACPR Writing Group, and the ACPM Writing Group. 147 Curhan GC, Willett WC, Rimm EB, Spiegelman D, Ascherio AL,
Healthy lifestyle interventions to combat noncommunicable Stampfer MJ. Birth weight and adult hypertension, diabetes
disease-a novel nonhierarchical connectivity model for key mellitus, and obesity in US men. Circulation 1996; 94: 3246–50.
stakeholders: a policy statement from the American Heart 148 Manalich R, Reyes L, Herrera M, Melendi C, Fundora I. Relationship
Association, European Society of Cardiology, European Association between weight at birth and the number and size of renal glomeruli
for Cardiovascular Prevention and Rehabilitation, and American in humans: a histomorphometric study. Kidney Int 2000; 58: 770–73.
College of Preventive Medicine. Eur Heart J 2015; 36: 2097–109.
2704 www.thelancet.com Vol 388 November 26, 2016
The Lancet Commissions
149 Hughson M, Farris AB 3rd, Douglas-Denton R, Hoy WE, 169 Hanninen MR, Niiranen TJ, Puukka PJ, Mattila AK, Jula AM.
Bertram JF. Glomerular number and size in autopsy kidneys: Determinants of masked hypertension in the general population:
the relationship to birth weight. Kidney Int 2003; 63: 2113–22. the Finn-Home study. J Hypertens 2011; 29: 1880–88.
150 Leeson CP, Kattenhorn M, Morley R, Lucas A, Deanfield JE. 170 Bobrie G, Chatellier G, Genes N, et al. Cardiovascular prognosis of
Impact of low birth weight and cardiovascular risk factors on “masked hypertension” detected by blood pressure self-
endothelial function in early adult life. Circulation 2001; measurement in elderly treated hypertensive patients. JAMA 2004;
103: 1264–68. 291: 1342–49.
151 Ikeda N, Gakidou E, Hasegawa T, Murray CJ. Understanding the 171 Franklin SS, Thijs L, Li Y, et al, and the International Database on
decline of mean systolic blood pressure in Japan: an analysis of Ambulatory blood pressure in Relation to Cardiovascular
pooled data from the National Nutrition Survey, 1986–2002. Outcomes Investigators. Masked hypertension in diabetes mellitus:
Bull World Health Organ 2008; 86: 978–88. treatment implications for clinical practice. Hypertension 2013;
152 Goff DC, Howard G, Russell GB, Labarthe DR. Birth cohort 61: 964–71.
evidence of population influences on blood pressure in the 172 Pierdomenico SD, Cuccurullo F. Prognostic value of white-coat and
United States, 1887–1994. Ann Epidemiol 2001; 11: 271–79. masked hypertension diagnosed by ambulatory monitoring in
153 McCarron P, Smith GD, Okasha M. Secular changes in blood initially untreated subjects: an updated meta analysis.
pressure in childhood, adolescence and young adulthood: Am J Hypertens 2011; 24: 52–58.
systematic review of trends from 1948 to 1998. J Hum Hypertens 173 Stergiou GS, Omboni S, Parati G. Home or ambulatory blood
2002; 16: 677–89. pressure monitoring for the diagnosis of hypertension? J Hypertens
154 Scherrer U, Rimoldi SF, Sartori C, Messerli FH, Rexhaj E. 2015; 33: 1528–30.
Fetal programming and epigenetic mechanisms in arterial 174 Ward AM, Takahashi O, Stevens R, Heneghan C. Home
hypertension. Curr Opin Cardiol 2015; 30: 393–7. measurement of blood pressure and cardiovascular disease:
155 Lee AC, Katz J, Blencowe H, et al, and the CHERG SGA-Preterm systematic review and meta-analysis of prospective studies.
Birth Working Group. National and regional estimates of term and J Hypertens 2012; 30: 449–56.
preterm babies born small for gestational age in 138 low-income 175 Mancia G, Facchetti R, Bombelli M, Grassi G, Sega R. Long-term
and middle-income countries in 2010. Lancet Glob Health 2013; risk of mortality associated with selective and combined elevation in
1: e26–36. office, home, and ambulatory blood pressure. Hypertension 2006;
156 Luyckx VA, Brenner BM. Birth weight, malnutrition and 47: 846–53.
kidney-associated outcomes—a global concern. Nat Rev Nephrol 176 Parati G, Stergiou GS, Asmar R, et al, and the ESH Working Group
2015; 11: 135–49. on Blood Pressure Monitoring. European Society of Hypertension
157 Jensen JD, Ronit K. The EU pledge for responsible marketing of practice guidelines for home blood pressure monitoring.
food and beverages to children: implementation in food companies. J Hum Hypertens 2010; 24: 779–85.
Eur J Clin Nutr 2015; 69: 896–901. 177 Daskalopoulou SS, Khan NA, Quinn RR, et al, and the Canadian
158 Gaziano TA, Abrahams-Gessel S, Denman CA, et al. An assessment Hypertension Education Program. The 2012 Canadian hypertension
of community health workers’ ability to screen for cardiovascular education program recommendations for the management of
disease risk with a simple, non-invasive risk assessment instrument hypertension: blood pressure measurement, diagnosis, assessment
in Bangladesh, Guatemala, Mexico, and South Africa: of risk, and therapy. Can J Cardiol 2012; 28: 270–87.
an observational study. Lancet Glob Health 2015; 3: e556–63. 178 Imai Y, Kario K, Shimada K, et al. The Japanese Society of
159 Jamie Oliver for Chief Medical Officer? Lancet 2005; 365: 1282. Hypertension Guidelines for Self-monitoring of Blood Pressure at
160 Flego A, Herbert J, Gibbs L, et al. Methods for the evaluation of the Home (Second Edition). Hypertens Res 2012; 35: 777–95.
Jamie Oliver Ministry of Food program, Australia. 179 Sharman JE, Howes FS, Head GA, et al. Home blood pressure
BMC Public Health 2013; 13: 411. monitoring: Australian Expert Consensus Statement.
161 Fujikawa T, Tochikubo O, Sugano T, Umemura S. Accuracy of the J Hypertens 2015; 33: 1721–28.
pulse delay time technique with triple cuff for objective indirect 180 Myers MG, Godwin M, Dawes M, Kiss A, Tobe SW, Kaczorowski J.
blood pressure measurement. J Hypertens 2013; 31: 278–86. Measurement of blood pressure in the office: recognizing the
162 Campbell NR, Gelfer M, Stergiou GS, et al. A call to regulate problem and proposing the solution. Hypertension 2010;
manufacture and marketing of blood pressure devices and cuffs: 55: 195–200.
a position statement from the World Hypertension League, 181 Armstrong D, Matangi M, Brouillard D, Myers MG. Automated
International Society of Hypertension and Supporting office blood pressure—being alone and not location is what matters
Hypertension Organizations. J Clin Hypertens (Greenwich) 2016; most. Blood Press Monit 2015; 20: 204–08.
18: 378–80. 182 Myers MG, Kaczorowski J, Paterson JM, Dolovich L, Tu K.
163 Graves JW, Bailey KR, Sheps SG. The changing distribution of arm Thresholds for diagnosing hypertension based on automated office
circumferences in NHANES III and NHANES 2000 and its impact blood pressure measurements and cardiovascular risk.
on the utility of the ‘standard adult’ blood pressure cuff. Hypertension 2015; 66: 489–95.
Blood Press Monit 2003; 8: 223–27. 183 Verdecchia P, Porcellati C, Schillaci G, et al. Ambulatory blood
164 Ostchega Y, Dillon C, Carroll M, Prineas RJ, McDowell M. pressure: an independent predictor of prognosis in essential
US demographic trends in mid-arm circumference and hypertension. Hypertension 1994; 24: 793–801.
recommended blood pressure cuffs: 1988–2002. J Hum Hypertens 184 Fagard RH, Celis H, Thijs L, et al. Daytime and nighttime blood
2005; 19: 885–91. pressure as predictors of death and cause-specific cardiovascular
165 Zdrojewski T, Kozicka-Kakol K, Chwojnicki K, Szpakowski P, events in hypertension. Hypertension 2008; 51: 55–61.
Konarski R, Wyrzykowski B. Arm circumference in adults in 185 Ishikawa J, Shimizu M, Sugiyama Edison E, et al, and the J-TOP
Poland as an important factor influencing the accuracy of blood (Japan Morning Surge-Target Organ Protection) Study Investigators
pressure readings. Blood Press Monit 2005; 10: 73–77. Group. Assessment of the reductions in night-time blood pressure
166 Palatini P, Benetti E, Fania C, Malipiero G, Saladini F. Rectangular and dipping induced by antihypertensive medication using a home
cuffs may overestimate blood pressure in individuals with large blood pressure monitor. J Hypertens 2014; 32: 82–89.
conical arms. J Hypertens 2012; 30: 530–36. 186 Rothwell PM, Howard SC, Dolan E, et al. Prognostic significance of
167 Fagard RH, Cornelissen VA. Incidence of cardiovascular events in visit-to-visit variability, maximum systolic blood pressure, and
white-coat, masked and sustained hypertension versus true episodic hypertension. Lancet 2010; 375: 895–905.
normotension: a meta-analysis. J Hypertens 2007; 25: 2193–98. 187 Gao S, Hendrie HC, Wang C, et al. Redefined blood pressure
168 Stergiou GS, Asayama K, Thijs L, et al, and the International variability measure and its association with mortality in elderly
Database on HOme blood pressure in relation to Cardiovascular primary care patients. Hypertension 2014; 64: 45–52.
Outcome (IDHOCO) Investigators. Prognosis of white-coat and 188 Zamani P, Bluemke DA, Jacobs DR Jr, et al. Resistive and pulsatile
masked hypertension: International Database of HOme blood arterial load as predictors of left ventricular mass and geometry:
pressure in relation to Cardiovascular Outcome. Hypertension 2014; the multi-ethnic study of atherosclerosis. Hypertension 2015;
63: 675–82. 65: 85–92.
www.thelancet.com Vol 388 November 26, 2016 2705
The Lancet Commissions
189 Herbert A, Cruickshank JK, Laurent S, Boutouyrie P, and the 209 Zamani P, Jacobs DR Jr, Segers P, et al. Reflection magnitude as
Reference Values for Arterial Measurements Collaboration. a predictor of mortality: the Multi-Ethnic Study of Atherosclerosis.
Establishing reference values for central blood pressure and its Hypertension 2014; 64: 958–64.
amplification in a general healthy population and according to 210 Fadl Elmula FE, Rebora P, Talvik A, et al, and the BEtter control of
cardiovascular risk factors. Eur Heart J 2014; 35: 3122–33. blood pressure in hypertensive pAtients monitored Using the
190 Pucci G, Ranalli MG, Battista F, Schillaci G. Effects of β-blockers HOTMAN sYstem (BEAUTY) Study Investigators. A randomized
with and without vasodilating properties on central blood pressure: and controlled study of noninvasive hemodynamic monitoring as
systematic review and meta-analysis of randomized trials in a guide to drug treatment of uncontrolled hypertensive patients.
hypertension. Hypertension 2016; 67: 316–24. J Hypertens 2015; 33: 2534–45.
191 Williams B, Lacy PS, Thom SM, et al, and the CAFE Investigators, 211 Borch-Johnsen K, Feldt-Rasmussen B, Strandgaard S, Schroll M,
the Anglo-Scandinavian Cardiac Outcomes Trial Investigators, and Jensen JS. Urinary albumin excretion. An independent predictor of
the CAFE Steering Committee and Writing Committee. Differential ischemic heart disease. Arterioscler Thromb Vasc Biol 1999;
impact of blood pressure-lowering drugs on central aortic pressure 19: 1992–97.
and clinical outcomes: principal results of the Conduit Artery 212 Okin PM, Devereux RB, Jern S, et al. Regression of
Function Evaluation (CAFE) study. Circulation 2006; 113: 1213–25. electrocardiographic left ventricular hypertrophy by losartan versus
192 Boutouyrie P, Achouba A, Trunet P, Laurent S, and the EXPLOR atenolol: The Losartan Intervention for Endpoint reduction in
Trialist Group. Amlodipine-valsartan combination decreases central Hypertension (LIFE) Study. Circulation 2003; 108: 684–90.
systolic blood pressure more effectively than the 213 Vlachopoulos C, Xaplanteris P, Aboyans V, et al. The role of vascular
amlodipine-atenolol combination: the EXPLOR study. biomarkers for primary and secondary prevention. A position paper
Hypertension 2010; 55: 1314–22. from the European Society of Cardiology Working Group on
193 Asmar RG, London GM, O’Rourke ME, Safar ME, and the peripheral circulation: Endorsed by the Association for Research
REASON Project Coordinators and Investigators. Improvement in into Arterial Structure and Physiology (ARTERY) Society.
blood pressure, arterial stiffness and wave reflections with a Atherosclerosis 2015; 241: 507–32.
very-low-dose perindopril/indapamide combination in hypertensive 214 Bramwell J, Hill AY. Velocity of transmission of the pulse-wave and
patient: a comparison with atenolol. Hypertension 2001; 38: 922–26. elasticity of arteries. Lancet 1922; 199: 891–92.
194 Kollias A, Lagou S, Zeniodi ME, Boubouchairopoulou N, 215 Laurent S, Boutouyrie P, Asmar R, et al. Aortic stiffness is an
Stergiou GS. Association of central versus brachial blood pressure independent predictor of all-cause and cardiovascular mortality in
with target-organ damage: systematic review and meta-analysis. hypertensive patients. Hypertension 2001; 37: 1236–41.
Hypertension 2016; 67: 183–90. 216 Laurent S, Cockcroft J, Van Bortel L, et al. Expert consensus
195 Sharman JE, Marwick TH, Gilroy D, Otahal P, Abhayaratna WP, document on arterial stiffness: methodological issues and clinical
Stowasser M, and the Value of Central Blood Pressure for GUIDing applications. Eur Heart J 2006; 27: 2588–605.
ManagEment of Hypertension Study Investigators. Randomized 217 Reference Values for Arterial Stiffness’ Collaboration. Determinants
trial of guiding hypertension management using central aortic of pulse wave velocity in healthy people and in the presence of
blood pressure compared with best-practice care: principal findings cardiovascular risk factors: ‘establishing normal and reference
of the BP GUIDE study. Hypertension 2013; 62: 1138–45. values’. Eur Heart J 2010; 31: 2338–50.
196 Hulsen HT, Nijdam ME, Bos WJ, et al. Spurious systolic 218 Van Bortel LM, Laurent S, Boutouyrie P, et al, and the Artery
hypertension in young adults; prevalence of high brachial systolic Society, the European Society of Hypertension Working Group on
blood pressure and low central pressure and its determinants. Vascular Structure and Function, and the European Network for
J Hypertens 2006; 24: 1027–32. Noninvasive Investigation of Large Arteries. Expert consensus
197 O’Rourke MF, Adji A. Guidelines on guidelines: focus on isolated document on the measurement of aortic stiffness in daily practice
systolic hypertension in youth. J Hypertens 2013; 31: 649–54. using carotid-femoral pulse wave velocity. J Hypertens 2012;
198 Kobayashi S, Yano M, Kohno M, et al. Influence of aortic impedance 30: 445–48.
on the development of pressure-overload left ventricular 219 Townsend RR, Wilkinson IB, Schiffrin EL, et al, and the American
hypertrophy in rats. Circulation 1996; 94: 3362–68. Heart Association Council on Hypertension. Recommendations for
199 Gillebert TC, Lew WY. Influence of systolic pressure profile on rate improving and standardizing vascular research on arterial stiffness:
of left ventricular pressure fall. Am J Physiol 1991; 261: H805–13. a scientific statement from the American Heart Association.
200 Chirinos JA, Segers P, Rietzschel ER, et al, and the Asklepios Hypertension 2015; 66: 698–722.
Investigators. Early and late systolic wall stress differentially relate 220 Greve SV, Blicher MK, Kruger R, et al. Estimated carotid-femoral
to myocardial contraction and relaxation in middle-aged adults: pulse wave velocity has similar predictive value as measured
the Asklepios study. Hypertension 2013; 61: 296–303. carotid-femoral pulse wave velocity. J Hypertens 2016; 34: 1279–89.
201 Chirinos JA, Segers P, Gillebert TC, et al, and the Asklepios 221 Najjar SS, Scuteri A, Shetty V, et al. Pulse wave velocity is an
Investigators. Arterial properties as determinants of time-varying independent predictor of the longitudinal increase in systolic blood
myocardial stress in humans. Hypertension 2012; 60: 64–70. pressure and of incident hypertension in the Baltimore
202 Chirinos JA, Kips JG, Jacobs DR Jr, et al. Arterial wave reflections and Longitudinal Study of Aging. J Am Coll Cardiol 2008; 51: 1377–83.
incident cardiovascular events and heart failure: MESA (Multiethnic 222 Greve SV, Blicher MK, Sehestedt T, et al. Effective risk stratification
Study of Atherosclerosis). J Am Coll Cardiol 2012; 60: 2170–77. in patients with moderate cardiovascular risk using albuminuria
203 Shah SJ, Wasserstrom JA. Increased arterial wave reflection and atherosclerotic plaques in the carotid arteries. J Hypertens 2015;
magnitude: a novel form of stage B heart failure? J Am Coll Cardiol 33: 1563–70.
2012; 60: 2178–81. 223 Januzzi JL, Troughton R. Are serial BNP measurements useful in
204 Sung SH, Yu WC, Cheng HM, et al. Excessive wave reflections on heart failure management? Serial natriuretic peptide measurements
admission predict post-discharge events in patients hospitalized are useful in heart failure management. Circulation 2013;
due to acute heart failure. Eur J Heart Fail 2012; 14: 1348–55. 127: 500–07.
205 Chirinos JA, Segers P, Duprez DA, et al. Late systolic central 224 Pyorala K, De Backer G, Graham I, Poole-Wilson P, Wood D.
hypertension as a predictor of incident heart failure: the Multi- Prevention of coronary heart disease in clinical practice.
ethnic Study of Atherosclerosis. J Am Heart Assoc 2015; 4: e001335. Recommendations of the Task Force of the European Society of
206 Wang KL, Cheng HM, Sung SH, et al. Wave reflection and arterial Cardiology, The European Atherosclerosis Society and the European
stiffness in the prediction of 15-year all-cause and cardiovascular Hypertension Society. A short overview for general practitioners.
mortalities: a community-based study. Hypertension 2010; Lijec Vjesn 1996; 118: 220–26 (in Croatian).
55: 799–805. 225 Daugherty SL, Powers JD, Magid DJ, et al. Incidence and prognosis
207 Weber T, Wassertheurer S, Rammer M, et al. Validation of a of resistant hypertension in hypertensive patients. Circulation 2012;
brachial cuff-based method for estimating central systolic blood 125: 1635–42.
pressure. Hypertension 2011; 58: 825–32. 226 Asayama K, Sato A, Ohkubo T, et al. The association between
208 Hughes AD. Ahead of the curve: waveform analysis of blood masked hypertension and waist circumference as an obesity-related
pressure, reflection magnitude, and outcomes. Hypertension 2014; anthropometric index for metabolic syndrome: the Ohasama study.
64: 929–30. Hypertens Res 2009; 32: 438–43.
2706 www.thelancet.com Vol 388 November 26, 2016
The Lancet Commissions
227 Schillaci G, Pirro M, Vaudo G, et al. Prognostic value of the 247 Chirinos JA, Gurubhagavatula I, Teff K, et al. CPAP, weight loss, or
metabolic syndrome in essential hypertension. J Am Coll Cardiol both for obstructive sleep apnea. N Engl J Med 2014; 370: 2265–75.
2004; 43: 1817–22. 248 Gottlieb DJ, Punjabi NM, Mehra R, et al. CPAP versus oxygen in
228 Schillaci G, Pirro M, Vaudo G, et al. Metabolic syndrome is obstructive sleep apnea. N Engl J Med 2014; 370: 2276–85.
associated with aortic stiffness in untreated essential hypertension. 249 Chobanian AV, Bakris GL, Black HR, et al, and the National Heart,
Hypertension 2005; 45: 1078–82. Lung, and Blood Institute Joint National Committee on Prevention,
229 Grassi G, Seravalle G, Trevano FQ, et al. Neurogenic abnormalities Detection, Evaluation, and Treatment of High Blood Pressure, and
in masked hypertension. Hypertension 2007; 50: 537–42. the National High Blood Pressure Education Program Coordinating
230 Scuteri A, Najjar SS, Orru’ M, et al. The central arterial burden of Committee. The seventh report of the Joint National Committee on
the metabolic syndrome is similar in men and women: the Prevention, Detection, Evaluation, and Treatment of High Blood
SardiNIA Study. Eur Heart J 2010; 31: 602–13. Pressure: the JNC 7 report. JAMA 2003; 289: 2560–72.
231 Scuteri A, Cunha PG, Rosei EA, et al, and the MARE Consortium. 250 Sinclair AM, Isles CG, Brown I, Cameron H, Murray GD,
Arterial stiffness and influences of the metabolic syndrome: Robertson JW. Secondary hypertension in a blood pressure clinic.
a cross-countries study. Atherosclerosis 2014; 233: 654–60. Arch Intern Med 1987; 147: 1289–93.
232 Vishram JK, Borglykke A, Andreasen AH, et al, and the MORGAM 251 Anderson GH Jr, Blakeman N, Streeten DH. The effect of age
Project. Impact of age and gender on the prevalence and prognostic on prevalence of secondary forms of hypertension in 4429
importance of the metabolic syndrome and its components in consecutively referred patients. J Hypertens 1994; 12: 609–15.
Europeans. The MORGAM Prospective Cohort Project. 252 Funder JW, Carey RM, Mantero F, et al. The management of
PLoS One 2014; 9: e107294. primary aldosteronism: case detection, diagnosis, and treatment:
233 Palagini L, Bruno RM, Gemignani A, Baglioni C, Ghiadoni L, an Endocrine Society Clinical Practice Guideline.
Riemann D. Sleep loss and hypertension: a systematic review. J Clin Endocrinol Metab 2016; 101: 1889–916.
Curr Pharm Des 2013; 19: 2409–19. 253 Lenders JW, Duh QY, Eisenhofer G, et al, and the Endocrine Society.
234 Calhoun DA, Harding SM. Sleep and hypertension. Chest 2010; Pheochromocytoma and paraganglioma: an endocrine society
138: 434–43. clinical practice guideline. J Clin Endocrinol Metab 2014; 99: 1915–42.
235 Bass J, Turek FW. Sleepless in America: a pathway to obesity and 254 Plouin PF, Amar L, Dekkers OM, et al, and the Guideline Working
the metabolic syndrome? Arch Intern Med 2005; 165: 15–16. Group. European Society of Endocrinology Clinical Practice
236 Somers VK, White DP, Amin R, et al, and the American Heart Guideline for long-term follow-up of patients operated on for a
Association Council for High Blood Pressure Research Professional phaeochromocytoma or a paraganglioma. Eur J Endocrinol 2016;
Education Committee, Council on Clinical Cardiology, the 174: G1–10.
American Heart Association Stroke Council, the American Heart 255 Persu A, Giavarini A, Touzé E, et al, and the ESH Working Group
Association Council on Cardiovascular Nursing, and the American Hypertension and the Kidney. European consensus on the
College of Cardiology Foundation. Sleep apnea and cardiovascular diagnosis and management of fibromuscular dysplasia. J Hypertens
disease: an American Heart Association/American College Of 2014; 32: 1367–78.
Cardiology Foundation Scientific Statement from the American 256 Biomarkers Definitions Working Group. Biomarkers and surrogate
Heart Association Council for High Blood Pressure Research endpoints: preferred definitions and conceptual framework.
Professional Education Committee, Council on Clinical Cardiology, Clin Pharmacol Ther 2001; 69: 89–95.
Stroke Council, and Council On Cardiovascular Nursing. In 257 Ji W, Foo JN, O’Roak BJ, et al. Rare independent mutations in renal
collaboration with the National Heart, Lung, and Blood Institute salt handling genes contribute to blood pressure variation.
National Center on Sleep Disorders Research (National Institutes of Nat Genet 2008; 40: 592–99.
Health). Circulation 2008; 118: 1080–111. 258 Carty DM, Schiffer E, Delles C. Proteomics in hypertension.
237 Mozaffarian D, Benjamin EJ, Go AS, et al, and the American Heart J Hum Hypertens 2013; 27: 211–16.
Association Statistics Committee and Stroke Statistics Subcommittee. 259 Nikolic SB, Sharman JE, Adams MJ, Edwards LM. Metabolomics in
Heart disease and stroke statistics—2015 update: a report from the hypertension. J Hypertens 2014; 32: 1159–69.
American Heart Association. Circulation 2015; 131: e29–322.
260 Lindsey ML, Mayr M, Gomes AV, et al, and the American Heart
238 Logan AG, Perlikowski SM, Mente A, et al. High prevalence of Association Council on Functional Genomics and Translational
unrecognized sleep apnoea in drug-resistant hypertension. Biology, Council on Cardiovascular Disease in the Young, Council
J Hypertens 2001; 19: 2271–77. on Clinical Cardiology, Council on Cardiovascular and Stroke
239 Gami AS, Howard DE, Olson EJ, Somers VK. Day-night pattern of Nursing, Council on Hypertension, and Stroke Council.
sudden death in obstructive sleep apnea. N Engl J Med 2005; Transformative impact of proteomics on cardiovascular health and
352: 1206–14. disease: a Scientific Statement from the American Heart
240 Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the Association. Circulation 2015; 132: 852–72.
association between sleep-disordered breathing and hypertension. 261 Pena MJ, Jankowski J, Heinze G, et al. Plasma proteomics
N Engl J Med 2000; 342: 1378–84. classifiers improve risk prediction for renal disease in patients with
241 Haentjens P, Van Meerhaeghe A, Moscariello A, et al. The impact hypertension or type 2 diabetes. J Hypertens 2015; 33: 2123–32.
of continuous positive airway pressure on blood pressure in 262 Padmanabhan S, Caulfield M, Dominiczak AF. Genetic and
patients with obstructive sleep apnea syndrome: evidence from a molecular aspects of hypertension. Circ Res 2015; 116: 937–59.
meta-analysis of placebo-controlled randomized trials. 263 Collins R, Peto R, MacMahon S, et al. Blood pressure, stroke,
Arch Intern Med 2007; 167: 757–64. and coronary heart disease. Part 2. Short-term reductions in blood
242 Bazzano LA, Khan Z, Reynolds K, He J. Effect of nocturnal nasal pressure: overview of randomised drug trials in their
continuous positive airway pressure on blood pressure in epidemiological context. Lancet 1990; 335: 827–38.
obstructive sleep apnea. Hypertension 2007; 50: 417–23. 264 Staessen JA, Gasowski J, Wang JG, et al. Risks of untreated and
243 Barbe F, Durán-Cantolla J, Capote F, et al, and the Spanish Sleep treated isolated systolic hypertension in the elderly: meta-analysis of
and Breathing Group. Long-term effect of continuous positive outcome trials. Lancet 2000; 355: 865–72.
airway pressure in hypertensive patients with sleep apnea. 265 Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure
Am J Respir Crit Care Med 2010; 181: 718–26. lowering on outcome incidence in hypertension. 1. Overview,
244 Tasali E, Ip MS. Obstructive sleep apnea and metabolic syndrome: meta-analyses, and meta-regression analyses of randomized trials.
alterations in glucose metabolism and inflammation. J Hypertens 2014; 32: 2285–95.
Proc Am Thorac Soc 2008; 5: 207–17. 266 Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for
245 Pack AI, Gislason T. Obstructive sleep apnea and cardiovascular prevention of cardiovascular disease and death: a systematic review
disease: a perspective and future directions. Prog Cardiovasc Dis and meta-analysis. Lancet 2016; 387: 957–67.
2009; 51: 434–51. 267 Patel A, ADVANCE Collaborative Group, MacMahon S, et al.
246 McNicholas WT, Bonsigore MR, and the Management Committee Effects of a fixed combination of perindopril and indapamide on
of EU COST ACTION B26. Sleep apnoea as an independent risk macrovascular and microvascular outcomes in patients with type 2
factor for cardiovascular disease: current evidence, basic diabetes mellitus (the ADVANCE trial): a randomised controlled
mechanisms and research priorities. Eur Respir J 2007; 29: 156–78. trial. Lancet 2007; 370: 829–40.
www.thelancet.com Vol 388 November 26, 2016 2707
The Lancet Commissions
268 Brunstrom M, Carlberg B. Effect of antihypertensive treatment at 287 Bakris GL, Sarafidis PA, Weir MR, et al, and the ACCOMPLISH
different blood pressure levels in patients with diabetes mellitus: Trial investigators. Renal outcomes with different fixed-dose
systematic review and meta-analyses. BMJ 2016; 352: i717. combination therapies in patients with hypertension at high risk for
269 Emdin CA, Rahimi K, Neal B, Callender T, Perkovic V, Patel A. cardiovascular events (ACCOMPLISH): a prespecified secondary
Blood pressure lowering in type 2 diabetes: a systematic review analysis of a randomised controlled trial. Lancet 2010; 375: 1173–81.
and meta-analysis. JAMA 2015; 313: 603–15. 288 Gupta AK, Arshad S, Poulter NR. Compliance, safety, and
270 Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure effectiveness of fixed-dose combinations of antihypertensive agents:
lowering on outcome incidence in hypertension: 4. Effects of a meta-analysis. Hypertension 2010; 55: 399–407.
various classes of antihypertensive drugs—overview and 289 Ambrosioni E, Borghi C. Pharmacoeconomic and cost-benefit
meta-analyses. J Hypertens 2015; 33: 195–211. aspects. In: Mancia G, Grassi G, Redon J, eds. Manual of
271 Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure hypertension of the European Society of Hypertension, 2nd edn.
lowering on outcome incidence in hypertension: 3. Effects in Boca Raton, FL: CRC Press, 2014.
patients at different levels of cardiovascular risk—overview and 290 Ordunez P, Luciani S, Barojas A, Fitzgerald J, Hennis AJ. A public
meta-analyses of randomized trials. J Hypertens 2014; 32: 2305–14. health approach to hypertension. Lancet 2015; 385: 1833.
272 Hansson L, Hedner T, Lund-Johansen P, et al. Randomised trial 291 Strauch B, Petrák O, Zelinka T, et al. Precise assessment of
of effects of calcium antagonists compared with diuretics and noncompliance with the antihypertensive therapy in patients with
beta-blockers on cardiovascular morbidity and mortality in resistant hypertension using toxicological serum analysis.
hypertension: the Nordic Diltiazem (NORDIL) study. Lancet 2000; J Hypertens 2013; 31: 2455–61.
356: 359–65. 292 Tomaszewski M, White C, Patel P, et al. High rates of
273 Dahlof B, Devereux RB, Kjeldsen SE, et al, and the LIFE Study non-adherence to antihypertensive treatment revealed by
Group. Cardiovascular morbidity and mortality in the Losartan high-performance liquid chromatography-tandem mass
Intervention For Endpoint reduction in hypertension study (LIFE): spectrometry (HP LC-MS/MS) urine analysis. Heart 2014;
a randomised trial against atenolol. Lancet 2002; 359: 995–1003. 100: 855–61.
274 Lindholm LH, Carlberg B, Samuelsson O. Should beta blockers 293 Yiannakopoulou EC, Papadopulos JS, Cokkinos DV,
remain first choice in the treatment of primary hypertension? Mountokalakis TD. Adherence to antihypertensive treatment:
A meta-analysis. Lancet 2005; 366: 1545–53. a critical factor for blood pressure control.
275 Staessen JA, Wang JG, Thijs L. Cardiovascular protection and blood Eur J Cardiovasc Prev Rehabil 2005; 12: 243–49.
pressure reduction: a meta-analysis. Lancet 2001; 358: 1305–15. 294 Burnier M, Wuerzner G, Struijker-Boudier H, Urquhart J.
276 Leenen FH, Nwachuku CE, Black HR, et al, and the Measuring, analyzing, and managing drug adherence in resistant
Antihypertensive and Lipid-Lowering Treatment to Prevent Heart hypertension. Hypertension 2013; 62: 218–25.
Attack Trial Collaborative Research Group. Clinical events in 295 Corrao G, Zambon A, Parodi A, et al. Discontinuation of and
high-risk hypertensive patients randomly assigned to calcium changes in drug therapy for hypertension among newly-treated
channel blocker versus angiotensin-converting enzyme inhibitor in patients: a population-based study in Italy. J Hypertens 2008;
the antihypertensive and lipid-lowering treatment to prevent heart 26: 819–24.
attack trial. Hypertension 2006; 48: 374–84. 296 Mancia G, Parodi A, Merlino L, Corrao G. Heterogeneity in
277 Yusuf S, Teo KK, Pogue J, et al, and the ONTARGET Investigators. antihypertensive treatment discontinuation between drugs
Telmisartan, ramipril, or both in patients at high risk for vascular belonging to the same class. J Hypertens 2011; 29: 1012–18.
events. N Engl J Med 2008; 358: 1547–59. 297 Atreja A, Bellam N, Levy SR. Strategies to enhance patient
278 McMurray JJ, Ostergren J, Swedberg K, et al, and the CHARM adherence: making it simple. MedGenMed 2005; 7: 4.
Investigators and Committees. Effects of candesartan in patients 298 Morgado M, Rolo S. Factors influencing medication adherence and
with chronic heart failure and reduced left-ventricular systolic hypertension management revisited: recent insights from cancer
function taking angiotensin-converting-enzyme inhibitors: the survivors. Hypertens Res 2012; 35: 894–96.
CHARM-Added trial. Lancet 2003; 362: 767–71. 299 Tedla YG, Bautista LE. Drug side effect symptoms and adherence to
279 Dahlof B, Sever PS, Poulter NR, et al, and the ASCOT Investigators. antihypertensive medication. Am J Hypertens 2016; 29: 772–79.
Prevention of cardiovascular events with an antihypertensive 300 Epstein BJ, Vogel K, Palmer BF. Dihydropyridine calcium channel
regimen of amlodipine adding perindopril as required versus antagonists in the management of hypertension. Drugs 2007;
atenolol adding bendroflumethiazide as required, in the 67: 1309–27.
Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure
301 Scuteri A, Modestino A, Frattari A, Di Daniele N, Tesauro M.
Lowering Arm (ASCOT-BPLA): a multicentre randomised
Occurrence of hypotension in older participants. Which 24-hour
controlled trial. Lancet 2005; 366: 895–906.
ABPM parameter better correlate with? J Gerontol A Biol Sci Med Sci
280 Lindholm LH, Ibsen H, Borch-Johnsen K, et al, and the LIFE study 2012; 67: 804–10.
group. Risk of new-onset diabetes in the Losartan Intervention For
302 Sanz G, Fuster V. Polypill and global cardiovascular health
Endpoint reduction in hypertension study. J Hypertens 2002;
strategies. Semin Thorac Cardiovasc Surg 2011; 23: 24–29.
20: 1879–86.
303 Wald NJ, Law MR. A strategy to reduce cardiovascular disease by
281 Jamerson K, Weber MA, Bakris GL, et al, and the ACCOMPLISH
more than 80%. BMJ 2003; 326: 1419.
Trial Investigators. Benazepril plus amlodipine or
hydrochlorothiazide for hypertension in high-risk patients. 304 Sanz G, Fuster V. Fixed-dose combination therapy and secondary
N Engl J Med 2008; 359: 2417–28. cardiovascular prevention: rationale, selection of drugs and target
population. Nat Clin Pract Cardiovasc Med 2009; 6: 101–10.
282 Marott SC, Nielsen SF, Benn M, Nordestgaard BG.
Antihypertensive treatment and risk of atrial fibrillation: 305 Sever PS, Dahlof B, Poulter NR, et al. Prevention of coronary and
a nationwide study. Eur Heart J 2014; 35: 1205–14. stroke events with atorvastatin in hypertensive patients who have
average or lower-than-average cholesterol concentrations, in the
283 Jafar TH, Schmid CH, Landa M, et al. Angiotensin-converting
Anglo-Scandinavian Cardiac Outcomes Trial—Lipid Lowering Arm
enzyme inhibitors and progression of nondiabetic renal disease.
(ASCOT-LLA): a multicentre randomised controlled trial.
A meta-analysis of patient-level data. Ann Intern Med 2001;
Lancet 2003; 361: 1149–58.
135: 73–87.
306 Yusuf S, Bosch J, Dagenais G, et al. Cholesterol lowering in
284 Chalmers J, Woodward M, Borghi C, Manolis A, Mancia G.
intermediate-risk persons without cardiovascular disease.
Strategies to meet the need for long-term data. J Hypertens 2016;
N Engl J Med 2016; 374: 2021–31.
34: 1473–79.
307 Chrysant SG, Chrysant GS. Future of polypill use for the prevention
285 Adeloye D, Basquill C, Aderemi AV, Thompson JY, Obi FA.
of cardiovascular disease and strokes. Am J Cardiol 2014;
An estimate of the prevalence of hypertension in Nigeria:
114: 641–45.
a systematic review and meta-analysis. J Hypertens 2015; 33: 230–42.
308 Julius S, Nesbitt SD, Egan BM, et al, and the Trial of Preventing
286 Bakris G, Sarafidis P, Agarwal R, Ruilope L. Review of blood
Hypertension (TROPHY) Study Investigators. Feasibility of treating
pressure control rates and outcomes. J Am Soc Hypertens
prehypertension with an angiotensin-receptor blocker. N Engl J Med
2014; 8: 127–41.
2006; 354: 1685–97.
2708 www.thelancet.com Vol 388 November 26, 2016
The Lancet Commissions
309 Luders S, Schrader J, Berger J, et al, and the PHARAO Study 330 Mason RP, Kalinowski L, Jacob RF, Jacoby AM, Malinski T. Nebivolol
Group. The PHARAO study: prevention of hypertension with the reduces nitroxidative stress and restores nitric oxide bioavailability in
angiotensin-converting enzyme inhibitor ramipril in patients with endothelium of black Americans. Circulation 2005; 112: 3795–801.
high-normal blood pressure: a prospective, randomized, controlled 331 Ezzati M, Riboli E. Behavioral and dietary risk factors for
prevention trial of the German Hypertension League. J Hypertens noncommunicable diseases. N Engl J Med 2013; 369: 954–64.
2008; 26: 1487–96. 332 Aburto NJ, Hanson S, Gutierrez H, Hooper L, Elliott P,
310 McAlister FA, and the Renin Angiotension System Modulator Cappuccio FP. Effect of increased potassium intake on
Meta-Analysis Investigators. Angiotensin-converting enzyme cardiovascular risk factors and disease: systematic review and
inhibitors or angiotensin receptor blockers are beneficial in meta-analyses. BMJ 2013; 346: f1378.
normotensive atherosclerotic patients: a collaborative meta-analysis 333 Whelton PK, He J, Cutler JA, et al. Effects of oral potassium on
of randomized trials. Eur Heart J 2012; 33: 505–14. blood pressure. Meta-analysis of randomized controlled clinical
311 Lewis JB, Berl T, Bain RP, Rohde RD, Lewis EJ, and the trials. JAMA 1997; 277: 1624–32.
Collaborative Study Group. Effect of intensive blood pressure 334 Graudal NA, Hubeck-Graudal T, Jurgens G. Effects of low-sodium
control on the course of type 1 diabetic nephropathy. diet vs high-sodium diet on blood pressure, renin, aldosterone,
Am J Kidney Dis 1999; 34: 809–17. catecholamines, cholesterol, and triglyceride (Cochrane Review).
312 Scuffham P, Chaplin S, Legood R. Incidence and costs of Am J Hypertens 2012; 25: 1–15.
unintentional falls in older people in the United Kingdom. 335 Pimenta E, Gaddam KK, Oparil S, Aban I, Husain S, Dell’Italia LJ,
J Epidemiol Community Health 2003; 57: 740–44. Calhoun DA. Effects of dietary sodium reduction on blood pressure
313 Rubenstein LZ, Josephson KR. Falls and their prevention in elderly in subjects with resistant hypertension: results from a randomized
people: what does the evidence show? Med Clin North Am 2006; trial. Hypertension 2009; 54: 475–81.
90: 807–24. 336 Rohner A, Ried K, Sobenin IA, Bucher HC, Nordmann AJ.
314 Woolcott JC, Richardson KJ, Wiens MO, et al. Meta-analysis of the A systematic review and metaanalysis on the effects of garlic
impact of 9 medication classes on falls in elderly persons. preparations on blood pressure in individuals with hypertension.
Arch Intern Med 2009; 169: 1952–60. Am J Hypertens 2015; 28: 414–23.
315 Callisaya ML, Sharman JE, Close J, Lord SR, Srikanth VK. 337 Khalesi S, Irwin C, Schubert M. Flaxseed consumption may reduce
Greater daily defined dose of antihypertensive medication increases blood pressure: a systematic review and meta-analysis of controlled
the risk of falls in older people—a population-based study. trials. J Nutr 2015; 145: 758–65.
J Am Geriatr Soc 2014; 62: 1527–33. 338 Warburton DE, Charlesworth S, Ivey A, Nettlefold L, Bredin SS.
316 Onder G, Bonassi S, Abbatecola AM, et al, and the Geriatrics A systematic review of the evidence for Canada’s Physical Activity
Working Group of the Italian Medicines Agency. High prevalence of Guidelines for Adults. Int J Behav Nutr Phys Act 2010; 7: 39.
poor quality drug prescribing in older individuals: a nationwide 339 Shiroma EJ, Lee IM. Physical activity and cardiovascular health:
report from the Italian Medicines Agency (AIFA). lessons learned from epidemiological studies across age, gender,
J Gerontol A Biol Sci Med Sci 2014; 69: 430–37. and race/ethnicity. Circulation 2010; 122: 743–52.
317 Chan KY, Wang W, Wu JJ, et al, and the Global Health Epidemiology 340 Cornelissen VA, Smart NA. Exercise training for blood pressure:
Reference Group (GHERG). Epidemiology of Alzheimer’s disease a systematic review and meta-analysis. J Am Heart Assoc 2013;
and other forms of dementia in China, 1990–2010: a systematic 2: e004473.
review and analysis. Lancet 2013; 381: 2016–23.
341 Carlson DJ, Dieberg G, Hess NC, Millar PJ, Smart NA. Isometric
318 Wilson RS, Boyle PA, Yu L, et al. Temporal course and pathologic exercise training for blood pressure management: a systematic
basis of unawareness of memory loss in dementia. Neurology 2015; review and meta-analysis. Mayo Clin Proc 2014; 89: 327–34.
85: 984–91.
342 Fagard RH, Cornelissen VA. Effect of exercise on blood pressure
319 Knopman D, Boland LL, Mosley T, et al. Cardiovascular risk factors control in hypertensive patients. Eur J Cardiovasc Prev Rehabil 2007;
and cognitive decline in middle-aged adults. Neurology 2001; 56: 42–48. 14: 12–17.
320 Maillard P, Seshadri S, Beiser A, et al. Effects of systolic blood 343 Sharman JE, La Gerche A, Coombes JS. Exercise and cardiovascular
pressure on white-matter integrity in young adults in the risk in patients with hypertension. Am J Hypertens 2015; 28: 147–58.
Framingham Heart Study: a cross-sectional study. Lancet Neurol
344 Boman K, Gerdts E, Wachtell K, et al. Exercise and cardiovascular
2012; 11: 1039–47.
outcomes in hypertensive patients in relation to structure and
321 Au R, Massaro JM, Wolf PA, et al. Association of white matter function of left ventricular hypertrophy: the LIFE study.
hyperintensity volume with decreased cognitive functioning: the Eur J Cardiovasc Prev Rehabil 2009; 16: 242–48.
Framingham Heart Study. Arch Neurol 2006; 63: 246–50.
345 Li J, Zheng H, Du HB, et al. The multiple lifestyle modification for
322 Scuteri A. Brain injury as end-organ damage in hypertension. patients with prehypertension and hypertension patients:
Lancet Neurol 2012; 11: 1015–17. a systematic review protocol. BMJ Open 2014; 4: e004920.
323 Pendlebury ST, Cuthbertson FC, Welch SJ, Mehta Z, Rothwell PM. 346 Funder JW, Carey RM, Fardella C, et al, and the Endocrine Society.
Underestimation of cognitive impairment by Mini-Mental State Case detection, diagnosis, and treatment of patients with primary
Examination versus the Montreal Cognitive Assessment in patients aldosteronism: an endocrine society clinical practice guideline.
with transient ischemic attack and stroke: a population-based study. J Clin Endocrinol Metab 2008; 93: 3266–81.
Stroke 2010; 41: 1290–93.
347 Trinquart L, Mounier-Vehier C, Sapoval M, Gagnon N, Plouin PF.
324 Scuteri A, Wang H. Pulse wave velocity as a marker of cognitive Efficacy of revascularization for renal artery stenosis caused by
impairment in the elderly. J Alzheimers Dis 2014; 42 : S401–10. fibromuscular dysplasia: a systematic review and meta-analysis.
325 Arbel-Ornath M, Hudry E, Eikermann-Haerter K, et al. Interstitial Hypertension 2010; 56: 525–32.
fluid drainage is impaired in ischemic stroke and Alzheimer’s 348 Wheatley K, Ives N, Gray R, et al, and the ASTRAL Investigators.
disease mouse models. Acta Neuropathol 2013; 126: 353–64. Revascularization versus medical therapy for renal-artery stenosis.
326 Iliff JJ, Wang M, Zeppenfeld DM, et al. Cerebral arterial pulsation N Engl J Med 2009; 361: 1953–62.
drives paravascular CSF-interstitial fluid exchange in the murine 349 Bax L, Woittiez AJ, Kouwenberg HJ, et al. Stent placement in
brain. J Neurosci 2013; 33: 18190–99. patients with atherosclerotic renal artery stenosis and impaired
327 Scuteri A, Tesauro M, Guglini L, Lauro D, Fini M, Di Daniele N. renal function: a randomized trial. Ann Intern Med 2009; 150: 840.
Aortic stiffness and hypotension episodes are associated with 350 Cooper CJ, Murphy TP, Cutlip DE, et al, and the CORAL
impaired cognitive function in older subjects with subjective Investigators. Stenting and medical therapy for atherosclerotic
complaints of memory loss. Int J Cardiol 2013; 169: 371–77. renal-artery stenosis. N Engl J Med 2014; 370: 13–22.
328 Jones DW, Hall JE. Racial and ethnic differences in blood pressure: 351 Zennaro MC, Boulkroun S, Fernandes-Rosa F. Inherited forms of
biology and sociology. Circulation 2006; 114: 2757–59. mineralocorticoid hypertension. Best Pract Res Clin Endocrinol Metab
329 Gafane LF, Schutte R, Van Rooyen JM, Schutte AE. Plasma renin 2015; 29: 633–45.
and cardiovascular responses to the cold pressor test differ in black 352 Favier J, Amar L, Gimenez-Roqueplo AP. Paraganglioma and
and white populations: The SABPA study. J Hum Hypertens 2016; phaeochromocytoma: from genetics to personalized medicine.
30: 346–51. Nat Rev Endocrinol 2015; 11: 101–11.
www.thelancet.com Vol 388 November 26, 2016 2709
The Lancet Commissions
353 Hering D, Schlaich M. The Role of Central Nervous System 374 Manisty CH, Hughes AD. Meta-analysis of the comparative effects
Mechanisms in Resistant Hypertension. Curr Hypertens Rep 2015; of different classes of antihypertensive agents on brachial and
17: 58. central systolic blood pressure, and augmentation index.
354 Laurent S, Steckelings U. New drugs under development for Br J Clin Pharmacol 2013; 75: 79–92.
cardiovascular prevention. In: Nilsson PM, Olsen MH, Laurent S, 375 Chen CH, Ting CT, Lin SJ, et al. Different effects of fosinopril and
eds. Early vascular aging (EVA): new directions in cardiovascular atenolol on wave reflections in hypertensive patients. Hypertension
protection, 1st edn. Cambridge, MA: Academic Press, 2015. 1995; 25: 1034–41.
355 Calhoun DA. Aldosterone and cardiovascular disease: smoke and 376 Asmar R. Effect of telmisartan on arterial distensibility and central
fire. Circulation 2006; 114: 2572–74. blood pressure in patients with mild to moderate hypertension and
356 Hoppe UC, Brandt MC, Wachter R, et al. Minimally invasive system type 2 diabetes mellitus. J Renin Angiotensin Aldosterone Syst 2001;
for baroreflex activation therapy chronically lowers blood pressure 2 (suppl 2): S8–11.
with pacemaker-like safety profile: results from the Barostim neo 377 Borlaug BA, Olson TP, Abdelmoneim SS, et al. A randomized pilot
trial. J Am Soc Hypertens 2012; 6: 270–76. study of aortic waveform guided therapy in chronic heart failure.
357 Heusser K, Tank J, Engeli S, et al. Carotid baroreceptor stimulation, J Am Heart Assoc 2014; 3: e000745.
sympathetic activity, baroreflex function, and blood pressure in 378 Parati G, Ochoa JE, Lombardi C, Bilo G. Blood pressure variability:
hypertensive patients. Hypertension 2010; 55: 619–26. assessment, predictive value, and potential as a therapeutic target.
358 Bakris GL, Nadim MK, Haller H, Lovett EG, Schafer JE, Curr Hypertens Rep 2015; 17: 537.
Bisognano JD. Baroreflex activation therapy provides durable 379 Webb AJ, Wilson M, Lovett N, Paul N, Fischer U, Rothwell PM.
benefit in patients with resistant hypertension: results of long-term Response of day-to-day home blood pressure variability by
follow-up in the Rheos Pivotal Trial. J Am Soc Hypertens antihypertensive drug class after transient ischemic attack or
2012; 6: 152–58. nondisabling stroke. Stroke 2014; 45: 2967–73.
359 Krum H, Schlaich MP, Sobotka PA, et al. Percutaneous renal 380 Webb AJ, Fischer U, Mehta Z, Rothwell PM. Effects of
denervation in patients with treatment-resistant hypertension: final antihypertensive-drug class on interindividual variation in blood
3-year report of the Symplicity HTN-1 study. Lancet 2014; pressure and risk of stroke: a systematic review and meta-analysis.
383: 622–29. Lancet 2010; 375: 906–15.
360 Esler MD, Böhm M, Sievert H, et al. Catheter-based renal 381 Hlatky MA, Greeland P, Arnett DK, et al, and the American Heart
denervation for treatment of patients with treatment-resistant Association Expert Panel on Subclinical Atherosclerotic Diseases and
hypertension: 36 month results from the SYMPLICITY HTN-2 Emerging Risk Factors and the Stroke Council. Criteria for evaluation
randomized clinical trial. Eur Heart J 2014; 35: 1752–59. of novel marker of cardiovascular risk: a scientific statement from
361 Hering D, Marusic P, Walton AS, et al. Sustained sympathetic and the American Heart Association. Circulation 2009; 119: 2343–49.
blood pressure reduction 1 year after renal denervation in patients 382 Fagard RH, Celis H, Thijs L, Wouters S. Regression of left
with resistant hypertension. Hypertension 2014; 64: 118–24. ventricular mass by antihypertensive treatment: a meta-analysis of
362 Azizi M, Sapoval M, Gosse P, et al, and the Renal Denervation for randomized comparative studies. Hypertension 2009; 54: 1084–91.
Hypertension (DENERHTN) investigators. Optimum and stepped 383 Devereux RB, Dahlöf B, Gerdts E, et al. Regression of hypertensive
care standardised antihypertensive treatment with or without renal left ventricular hypertrophy by losartan compared with atenolol: the
denervation for resistant hypertension (DENERHTN): Losartan Intervention for Endpoint Reduction in Hypertension
a multicentre, open-label, randomised controlled trial. Lancet 2015; (LIFE) trial. Circulation 2004; 110: 1456–62.
385: 1957–65. 384 Okin PM, Devereux RB, Jern S, et al, and the LIFE Study
363 Bhatt DL, Kandzari DE, O’Neill WW, et al, and the SYMPLICITY Investigators. Regression of electrocardiographic left ventricular
HTN-3 Investigators. A controlled trial of renal denervation for hypertrophy during antihypertensive treatment and the prediction
resistant hypertension. N Engl J Med 2014; 370: 1393–401. of major cardiovascular events. JAMA 2004; 292: 2343–49.
364 Kandzari DE, Bhatt DL, Brar S, et al. Predictors of blood pressure 385 Devereux RB, Wachtell K, Gerdts E, et al. Prognostic significance of
response in the SYMPLICITY HTN-3 trial. Eur Heart J 2015; left ventricular mass change during treatment of hypertension.
36: 219–27. JAMA 2004; 292: 2350–56.
365 Mahfoud F, Tunev S, Ewen S, et al. Impact of lesion placement on 386 Olsen MH, Wachtell K, Ibsen H, et al, and the LIFE Study
efficacy and safety of catheter-based radiofrequency renal Investigators. Reductions in albuminuria and in
denervation. J Am Coll Cardiol 2015; 66: 1766–75. electrocardiographic left ventricular hypertrophy independently
366 Hering D, Marusic P, Walton AS, et al. Renal artery anatomy affects improve prognosis in hypertension: the LIFE study. J Hypertens
the blood pressure response to renal denervation in patients with 2006; 24: 775–81.
resistant hypertension. Int J Cardiol 2016; 202: 388–93. 387 Savarese G, Dei Cas A, Rosano G, et al. Reduction of albumin
367 Williams B, MacDonald TM, Morant S, et al, and the British urinary excretion is associated with reduced cardiovascular events
Hypertension Society’s PATHWAY Studies Group. Spironolactone in hypertensive and/or diabetic patients. A meta-regression analysis
versus placebo, bisoprolol, and doxazosin to determine the optimal of 32 randomized trials. Int J Cardiol 2014; 172: 403–10.
treatment for drug-resistant hypertension (PATHWAY-2): 388 Haller H, Ito S, Izzo JL Jr, et al, and the ROADMAP Trial
a randomised, double-blind, crossover trial. Lancet 2015; Investigators. Olmesartan for the delay or prevention of
386: 2059–68. microalbuminuria in type 2 diabetes. N Engl J Med 2011; 364: 907–17.
368 Li Q, Youn JY, Cai H. Mechanisms and consequences of endothelial 389 Wang TJ, Gona P, Larson MG, et al. Multiple biomarkers for the
nitric oxide synthase dysfunction in hypertension. J Hypertens 2015; prediction of first major cardiovascular events and death.
33: 1128–36. N Engl J Med 2006; 355: 2631–39.
369 Wenzel U, Turner JE, Krebs C, Kurts C, Harrison DG, Ehmke H. 390 Vermeer SE, Prins ND, den Heijer T, Hofman A, Koudstaal PJ,
Immune mechanisms in arterial hypertension. J Am Soc Nephrol Breteler MM. Silent brain infarcts and the risk of dementia and
2016; 27: 677–86. cognitive decline. N Engl J Med 2003; 348: 1215–22.
370 Titze J. A different view on sodium balance. 391 van Sloten TT, Sedaghat S, Laurent S, et al. Carotid stiffness is
Curr Opin Nephrol Hypertens 2015; 24: 14–20. associated with incident stroke: a systematic review and individual
371 Westerbacka J, Tamminen M, Cockcroft J, Yki-Järvinen H. participant data meta-analysis. J Am Coll Cardiol 2015; 66: 2116–25.
Comparison of in vivo effects of nitroglycerin and insulin on the 392 Engelen L, Bossuyt J, Ferreira I, et al, and the Reference Values for
aortic pressure waveform. Eur J Clin Invest 2004; 34: 1–8. Arterial Measurements Collaboration. Reference values for local
372 Kelly RP, Gibbs HH, O’Rourke MF, et al. Nitroglycerin has more arterial stiffness. Part A: carotid artery. J Hypertens 2015;
favourable effects on left ventricular afterload than apparent from 33: 1981–96.
measurement of pressure in a peripheral artery. Eur Heart J 1990; 393 Ait-Oufella H, Collin C, Bozec E, et al. Long-term reduction in
11: 138–44. aortic stiffness: a 5.3-year follow-up in routine clinical practice.
373 Jiang XJ, O’Rourke MF, Jin WQ, et al. Quantification of glyceryl J Hypertens 2010; 28: 2336–41.
trinitrate effect through analysis of the synthesised ascending aortic 394 Laurent S, Briet M, Boutouyrie P. Arterial stiffness as surrogate end
pressure waveform. Heart 2002; 88: 143–48. point: needed clinical trials. Hypertension 2012; 60: 518–22.
2710 www.thelancet.com Vol 388 November 26, 2016
The Lancet Commissions
395 Aujoulat I, Marcolongo R, Bonadiman L, Deccache A. 415 Coleman R, Gill G, Wilkinson D. Noncommunicable disease
Reconsidering patient empowerment in chronic illness: a critique management in resource-poor settings: a primary care model from
of models of self-efficacy and bodily control. Soc Sci Med 2008; rural South Africa. Bull World Health Organ 1998; 76: 633–40.
66: 1228–39. 416 Farzadfar F, Murray CJ, Gakidou E, et al. Effectiveness of diabetes
396 Simmons LA, Wolever RQ, Bechard EM, Snyderman R. Patient and hypertension management by rural primary health-care
engagement as a risk factor in personalized health care: a workers (Behvarz workers) in Iran: a nationally representative
systematic review of the literature on chronic disease. Genome Med observational study. Lancet 2012; 379: 47–54.
2014; 6: 16. 417 Wal P, Wal A, Bhandari A, Pandey U, Rai AK. Pharmacist
397 Chodosh J, Morton SC, Mojica W, et al. Meta-analysis: chronic involvement in the patient care improves outcome in hypertension
disease self-management programs for older adults. Ann Intern Med patients. J Res Pharm Pract 2013; 2: 123–29.
2005; 143: 427–38. 418 Carter BL, Rogers M, Daly J, Zheng S, James PA. The potency of
398 Kuo CC, Lin CC, Tsai FM. Effectiveness of empowerment-based team-based care interventions for hypertension: a meta-analysis.
self-management interventions on patients with chronic metabolic Arch Intern Med 2009; 169: 1748–55.
diseases: a systematic review and meta-analysis. 419 Santschi V, Chiolero A, Colosimo AL, et al. Improving blood
Worldviews Evid Based Nurs 2014; 11: 301–15. pressure control through pharmacist interventions:
399 WHO. Health promotion. Track 1: community empowerment. 2010. a meta-analysis of randomized controlled trials. J Am Heart Assoc
http://www.who.int/healthpromotion/conferences/7gchp/track1/ 2014; 3: e000718.
en/ (accessed May 10, 2016). 420 Zillich AJ, Jaynes HA, Bex SD, et al. Evaluation of pharmacist care
400 The Popular Aid For Relief And Development. Strategy two: for hypertension in the Veterans Affairs patient-centered medical
community empowerment. 2016. http://www.pard-lb.org/en/what- home: a retrospective case-control study. Am J Med 2015;
we-do/community-empowerment (accessed May 10, 2016). 128: 539.e1–6.
401 Hartono B. Empowering the community to fight against 421 Hess PL, Reingold JS, Jones J, et al. Barbershops as hypertension
hypertension: the Indonesian experience. 2013. http://www.searo. detection, referral, and follow-up centers for black men.
who.int/publications/journals/regional_health_forum/rhfv17n1p32. Hypertension 2007; 49: 1040–46.
pdf (accessed May 10, 2016). 422 Victor RG, Ravenell JE, Freeman A, et al. Effectiveness of a
402 CDX & Changes. What is community empowerment? 2008. barber-based intervention for improving hypertension control in
http://www.iacdglobal.org/files/what_is_community_ black men: the BARBER-1 study: a cluster randomized trial.
empowerment.pdf (accessed May 10, 2016). Arch Intern Med 2011; 171: 342–50.
403 Morisky DE, Levine DM, Green LW, Shapiro S, Russell RP, 423 Aujoulat I, Jacquemin P, Rietzschel E, et al. Factors associated with
Smith CR. Five-year blood pressure control and mortality following clinical inertia: an integrative review. Adv Med Educ Pract
health education for hypertensive patients. Am J Public Health 1983; 2014; 5: 141–47.
73: 153–62. 424 Ward AM, Heneghan C, Perera R, et al. What are the basic
404 Mattila R, Malmivaara A, Kastarinen M, Kivelä SL, Nissinen A. self-monitoring components for cardiovascular risk management?
Effectiveness of multidisciplinary lifestyle intervention for BMC Med Res Methodol 2010; 10: 105.
hypertension: a randomised controlled trial. J Hum Hypertens 2003; 425 Fletcher BR, Hinton L, Hartmann-Boyce J, Roberts NW,
17: 199–205. Bobrovitz N, McManus RJ. Self-monitoring blood pressure in
405 Sawicki PT, Mühlhauser I, Didjurgeit U, Berger M. Improvement of hypertension, patient and provider perspectives: a systematic review
hypertension care by a structured treatment and teaching and thematic synthesis. Patient Educ Couns 2016; 99: 210–19.
programme. J Hum Hypertens 1993; 7: 571–73. 426 McManus RJ, Mant J, Roalfe A, et al. Targets and self monitoring in
406 Iso H, Shimamoto T, Yokota K, Sankai T, Jacobs DR Jr, Komachi Y. hypertension: randomised controlled trial and cost effectiveness
Community-based education classes for hypertension control. analysis. BMJ 2005; 331: 493.
A 1·5-year randomized controlled trial. Hypertension 1996; 427 Cappuccio FP, Kerry SM, Forbes L, Donald A. Blood pressure
27: 968–74. control by home monitoring: meta-analysis of randomised trials.
407 Wilson A, Childs S. The relationship between consultation length, BMJ 2004; 329: 145.
process and outcomes in general practice: a systematic review. 428 Halme L, Vesalainen R, Kaaja M, Kantola I, and the HOme
Br J Gen Pract 2002; 52: 1012–20. MEasuRement of blood pressure study group. Self-monitoring of
408 Johnson HM, Olson AG, LaMantia JN, et al. Documented lifestyle blood pressure promotes achievement of blood pressure target in
education among young adults with incident hypertension. primary health care. Am J Hypertens 2005; 18: 1415–20.
J Gen Intern Med 2015; 30: 556–64. 429 Fletcher BR, Hartmann-Boyce J, Hinton L, McManus RJ. The effect
409 Ribeiro CD, Resqueti VR, Lima I, Dias FA, Glynn L, Fregonezi GA. of self-monitoring of blood pressure on medication adherence and
Educational interventions for improving control of blood pressure lifestyle factors: a systematic review and meta-analysis.
in patients with hypertension: a systematic review protocol. Am J Hypertens 2015; 28: 1209–21.
BMJ Open 2015; 5: e006583. 430 Laine C, Davidoff F. Patient-centered medicine. A professional
410 Perk J, De Backer G, Gohlke H, et al, and the European Association evolution. JAMA 1996; 275: 152–56.
for Cardiovascular Prevention & Rehabilitation (EACPR), and the 431 Marshall M, Bibby J. Supporting patients to make the best
ESC Committee for Practice Guidelines (CPG). European decisions. BMJ 2011; 342: d2117.
Guidelines on cardiovascular disease prevention in clinical practice 432 Keirns CC, Goold SD. Patient-centered care and
(version 2012). The Fifth Joint Task Force of the European Society of preference-sensitive decision making. JAMA 2009; 302: 1805–06.
Cardiology and Other Societies on Cardiovascular Disease
433 Grant RW, Pandiscio JC, Pajolek H, et al. Implementation of a
Prevention in Clinical Practice (constituted by representatives of
web-based tool for patient medication self-management: the
nine societies and by invited experts). Eur Heart J 2012; 33: 1635–701.
Medication Self-titration Evaluation Programme (Med-STEP) for
411 Stead LF, Buitrago D, Preciado N, Sanchez G, Hartmann-Boyce J, blood pressure control. Inform Prim Care 2012; 20: 57–67.
Lancaster T. Physician advice for smoking cessation.
434 Bobrie G, Postel-Vinay N, Delonca J, Corvol P, and the SETHI
Cochrane Database Syst Rev 2013; 5: CD000165.
Investigators. Self-measurement and self-titration in hypertension:
412 The World Bank. World development indicators: health systems. a pilot telemedicine study. Am J Hypertens 2007; 20: 1314–20.
2015. http://wdi.worldbank.org/table/2.15 (accessed Dec 28, 2015).
435 McManus RJ, Mant J, Bray EP, et al. Telemonitoring and
413 Bauer UE, Briss PA, Goodman RA, Bowman BA. Prevention of self-management in the control of hypertension (TASMINH2):
chronic disease in the 21st century: elimination of the leading a randomised controlled trial. Lancet 2010; 376: 163–72.
preventable causes of premature death and disability in the USA.
436 Chung M, Oden RP, Joyner BL, Sims A, Moon RY. Safe infant sleep
Lancet 2014; 384: 45–52.
recommendations on the Internet: let’s Google it. J Pediatr 2012;
414 Jafar TH, Islam M, Hatcher J, et al, and the Hypertension Research 161: 1080–84.
Group. Community based lifestyle intervention for blood pressure
437 Finkelstein J, Barr MS, Kothari PP, Nace DK, Quinn M.
reduction in children and young adults in developing country:
Patient-centered medical home cyberinfrastructure current and
cluster randomised controlled trial. BMJ 2010; 340: c2641.
future landscape. Am J Prev Med 2011; 40 (suppl 2): S225–33.
www.thelancet.com Vol 388 November 26, 2016 2711
The Lancet Commissions
438 Greenhalgh T, Stramer K, Bratan T, Byrne E, Russell J, Potts HW. 458 Jaffe MG, Lee GA, Young JD, Sidney S, Go AS. Improved blood
Adoption and non-adoption of a shared electronic summary record pressure control associated with a large-scale hypertension
in England: a mixed-method case study. BMJ 2010; 340: c3111. program. JAMA 2013; 310: 699–705.
439 Nolan RP, Liu S, Payne AY. E-counseling as an emerging preventive 459 Pan American Health Organization. PAHO Strategic Fund. 2014.
strategy for hypertension. Curr Opin Cardiol 2014; 29: 319–23. http://www.paho.org/hq/index.php?option=com_content&view=cat
440 Liu S, Dunford SD, Leung YW, et al. Reducing blood pressure with egory&layout=blog&id=1159&Itemid=452&lang=en (accessed
Internet-based interventions: a meta-analysis. Can J Cardiol 2013; March 15, 2016).
29: 613–21. 460 WHO. Universal health coverage. 2014. http://www.who.int/
441 Logan AG. Transforming hypertension management using mobile healthsystems/universal_health_coverage/en/ (accessed
health technology for telemonitoring and self-care support. March 15, 2016).
Can J Cardiol 2013; 29: 579–85. 461 Dalton AR. Universal health insurance—a prerequisite of a
442 Logan AG. Community hypertension programs in the age of 21st century health system: the case for hypertension management.
mobile technology and social media. Am J Hypertens 2014; Future Cardiol 2014; 10: 327–31.
27: 1033–35. 462 Mathauer I, Theisling M, Mathivet B, Vilcu I. State budget transfers
443 Logan AG, Irvine MJ, McIsaac WJ, et al. Effect of home blood to health insurance funds: extending universal health coverage in
pressure telemonitoring with self-care support on uncontrolled low- and middle-income countries of the WHO European Region.
systolic hypertension in diabetics. Hypertension 2012; 60: 51–57. Int J Equity Health 2016; 15: 27.
444 Trudel M, Cafazzo JA, Hamill M, et al. A mobile phone based 463 Feng XL, Pang M, Beard J. Health system strengthening and
remote patient monitoring system for chronic disease hypertension awareness, treatment and control: data from the
management. Stud Health Technol Inform 2007; 129: 167–71. China Health and Retirement Longitudinal Study.
445 Piette JD, Datwani H, Gaudioso S, et al. Hypertension management Bull World Health Organ 2014; 92: 29–41.
using mobile technology and home blood pressure monitoring: 464 German RR, Lee LM, Horan JM, Milstein RL, Pertowski CA,
results of a randomized trial in two low/middle-income countries. Waller MN, for the Guidelines Working Group Centers for Disease
Telemed J E Health 2012; 18: 613–20. Control and Prevention (CDC). Updated guidelines for evaluating
446 WHO. NCD Global Monitoring Framework. Ensuring progress on public health surveillance systems: recommendations from the
noncommunicable diseases in countries. 2011. http://www.who.int/ Guidelines Working Group. MMWR Recomm Rep 2001;
nmh/global_monitoring_framework/en/ (accessed March 14, 2016). 50 (RR-13): 1–35.
447 WHO. Scaling up action against NCDs: how much will it cost? 465 Mackenbach JP, McKee M. A comparative analysis of health policy
2011. http://www.who.int/nmh/publications/cost_of_inaction/en/ performance in 43 European countries. Eur J Public Health 2013;
(accessed March 15, 2016). 23: 195–201.
448 Lim SS, Gaziano TA, Gakidou E, et al. Prevention of cardiovascular 466 Centers for Disease Control and Prevention. Centers for Medicare
disease in high-risk individuals in low-income and middle-income & Medicaid Services. Million hearts. 2016. http://millionhearts.hhs.
countries: health effects and costs. Lancet 2007; 370: 2054–62. gov/about-million-hearts/index.html (accessed March 15, 2016).
449 Nugent R. Benefits and costs of the non-communicable disease 467 Wright JS, Wall HK, Briss PA, Schooley M. Million hearts—where
targets for the post-2015 development agenda. 2015. http://www. population health and clinical practice intersect.
copenhagenconsensus.com/sites/default/files/health_perspective_ Circ Cardiovasc Qual Outcomes 2012; 5: 589–91.
ncd_-_nugent.pdf (accessed Feb 7, 2016). 468 Bi Z, Liang X, Xu A, et al. Hypertension prevalence, awareness,
450 Barton P, Andronis L, Briggs A, McPherson K, Capewell S. treatment, and control and sodium intake in Shandong Province,
Effectiveness and cost effectiveness of cardiovascular disease China: baseline results from Shandong-Ministry of Health Action
prevention in whole populations: modelling study. BMJ 2011; on Salt Reduction and Hypertension (SMASH), 2011.
343: d4044. Prev Chronic Dis 2014; 11: EE8.
451 Wang G, Labarthe D. The cost-effectiveness of interventions 469 Chen X, Guo X, Ma J, et al. Urinary sodium or potassium excretion
designed to reduce sodium intake. J Hypertens 2011; 29: 1693–99. and blood pressure in adults of Shandong province, China:
preliminary results of the SMASH project. J Am Soc Hypertens 2015;
452 WHO, World Economic Forum. From burden to “best buys”:
9: 754–62.
reducing the economic impact of NCDs in low- and middle-income
countries. 2011. http://www.who.int/nmh/publications/best_buys_ 470 Centers for Disease Control and Prevention. Global NCD, injury,
summary/en/ (accessed Feb 7, 2016). and environmental health. Sodium reduction and hypertension:
controlling the ‘silent killer’. 2016. http://www.cdc.gov/
453 WHO. Health systems strategy. 2007. http://www.who.int/
globalhealth/healthprotection/ncd/pdf/factsheets/ncd_sodium_
healthsystems/strategy/en/ (accessed March 15, 2016).
reduction_hypertension_01-2016.pdf (accessed March 3, 2016).
454 Sweeney S, Obure CD, Maier CB, Greener R, Dehne K, Vassall A.
471 Vasan RS, Beiser A, Seshadri S, et al. Residual lifetime risk for
Costs and efficiency of integrating HIV/AIDS services with other
developing hypertension in middle-aged women and men:
health services: a systematic review of evidence and experience.
the Framingham Heart Study. JAMA 2002; 287: 1003–10.
Sex Transm Infect 2012; 88: 85–99.
472 Wiktor S, Ford N, Ball A, Hirnschall G. HIV and HCV: distinct
455 Angell SY, De Cock KM, Frieden TR. A public health approach to
infections with important overlapping challenges. J Int AIDS Soc
global management of hypertension. Lancet 2015; 385: 825–27.
2014; 17: 19323.
456 WHO. Innovative care for chronic conditions: building blocks for
473 Frieden TR. Six components necessary for effective public health
action. 2002. http://www.who.int/chp/knowledge/publications/
program implementation. Am J Public Health 2014; 104: 17–22.
icccreport/en/ (accessed March 15, 2016).
457 Coleman K, Austin BT, Brach C, Wagner EH. Evidence on the
chronic care model in the new millennium. Health Aff (Millwood)
2009; 28: 75–85.
2712 www.thelancet.com Vol 388 November 26, 2016
You might also like
- Safety Management in An Organisational Context: Editor: Leonie LouwDocument210 pagesSafety Management in An Organisational Context: Editor: Leonie LouwLerato Mnguni100% (3)
- CPCWHS3001 - Presentation V1.0Document45 pagesCPCWHS3001 - Presentation V1.0sharma SoniaNo ratings yet
- JNC 7 - Complete VersionDocument48 pagesJNC 7 - Complete VersionTheresia WilliNo ratings yet
- HypertensionDocument11 pagesHypertensionRajeev NepalNo ratings yet
- JCH 14072Document11 pagesJCH 14072Cristina Saldias PorrasNo ratings yet
- Katigbak 2018Document9 pagesKatigbak 2018nabilahbilqisNo ratings yet
- 2021 World Health Organization Guideline On PharmaDocument10 pages2021 World Health Organization Guideline On PharmaGiselleNo ratings yet
- JNC 7Document48 pagesJNC 7ji tosanNo ratings yet
- SA-Hypertension-guidelinesDocument26 pagesSA-Hypertension-guidelinesMaleehaNo ratings yet
- Primary Prevention of HypertensionDocument7 pagesPrimary Prevention of HypertensioncinthyaaaNo ratings yet
- 10 1001@jama 2018 16755Document2 pages10 1001@jama 2018 16755Papilionanthae MalindaeNo ratings yet
- Cir 0000000000000450Document44 pagesCir 0000000000000450indah sundariNo ratings yet
- Hypertension Annals of Internal Medicine 2014Document16 pagesHypertension Annals of Internal Medicine 2014jhazpeitiaNo ratings yet
- Hypertension (HighBloodPressure) (NHLBI) PDFDocument2 pagesHypertension (HighBloodPressure) (NHLBI) PDFHarsha Jeevan Kishore KaranamNo ratings yet
- ioannidis2017Document2 pagesioannidis2017Endang Dwii SuhartiningsihNo ratings yet
- AHAjournal Cardio Outcomes Research Pprs On HypertensionDocument10 pagesAHAjournal Cardio Outcomes Research Pprs On HypertensionScribdOnlineReaderNo ratings yet
- US Hypertension Management Guidelines: A Review of The Recent Past and Recommendation For The FutureDocument12 pagesUS Hypertension Management Guidelines: A Review of The Recent Past and Recommendation For The FuturemagreaNo ratings yet
- Hypertension Prevention and Control Strategies Focus on Team-Based CareDocument30 pagesHypertension Prevention and Control Strategies Focus on Team-Based Care2130020043 RIDHO INAYAHNo ratings yet
- JNC 8Document12 pagesJNC 8Maya_AnggrainiKNo ratings yet
- 3.3 Hyp.0000000000000202Document13 pages3.3 Hyp.0000000000000202Chemicol QuimicosNo ratings yet
- US Hypertension Management Guidelines: A Review of The Recent Past and Recommendations For The FutureDocument12 pagesUS Hypertension Management Guidelines: A Review of The Recent Past and Recommendations For The Futureirvan121No ratings yet
- Effects of isometric exercise on BPDocument4 pagesEffects of isometric exercise on BPSintariNo ratings yet
- Arterial HypertensionDocument13 pagesArterial HypertensionZedodurex100% (1)
- Jurnal HipertensiDocument5 pagesJurnal HipertensiRanhie Pen'ned CendhirhieNo ratings yet
- CPG Management of Hypertension (3rd Edition)Document44 pagesCPG Management of Hypertension (3rd Edition)patricktiew100% (2)
- Kidney News Article p29 17Document1 pageKidney News Article p29 17annafebrinaputriNo ratings yet
- US Hypertension Review GuidelinesDocument12 pagesUS Hypertension Review Guidelinesmefav7778520100% (1)
- Brunstrm 2020 Oi 190702 PDFDocument12 pagesBrunstrm 2020 Oi 190702 PDFJudah ObengNo ratings yet
- J of Clinical Hypertension - 2014 - Weber - Clinical Practice Guidelines For The Management of Hypertension in TheDocument13 pagesJ of Clinical Hypertension - 2014 - Weber - Clinical Practice Guidelines For The Management of Hypertension in TheHanifah RifdaNo ratings yet
- Preoperative Hypertension BJA 2021Document7 pagesPreoperative Hypertension BJA 2021lim sjNo ratings yet
- A stepwise approach to managing resistant hypertensionDocument11 pagesA stepwise approach to managing resistant hypertensionAreli KamuiNo ratings yet
- Trends in Prevalence and Control of Hypertension According To The 2017 American College of Cardiology/American Heart Association (ACC/AHA) GuidelineDocument11 pagesTrends in Prevalence and Control of Hypertension According To The 2017 American College of Cardiology/American Heart Association (ACC/AHA) GuidelineDiana Alvarez SedanoNo ratings yet
- Hypertension Management GuidelineDocument11 pagesHypertension Management GuidelineAdeNeaNo ratings yet
- Hipertensi AdherenceDocument17 pagesHipertensi AdherenceBudi RiyantoNo ratings yet
- Hypertension Dissertation TopicsDocument5 pagesHypertension Dissertation TopicsInstantPaperWriterUK100% (1)
- Hypertensionaha 123 21592Document5 pagesHypertensionaha 123 21592Juan Diego JImenez AlvizoNo ratings yet
- jnc8 PDFDocument14 pagesjnc8 PDFRizki NovitasariNo ratings yet
- Seminar: EpidemiologyDocument13 pagesSeminar: EpidemiologySol LakosNo ratings yet
- Hansford 2021Document12 pagesHansford 2021Acilino PortelaNo ratings yet
- Byrd 2019Document22 pagesByrd 2019Miriam TorresNo ratings yet
- Assessing Patient Knowledge and Compliance With Antihypertensive Treatment in Techiman MunicipalityDocument8 pagesAssessing Patient Knowledge and Compliance With Antihypertensive Treatment in Techiman MunicipalityIJAR JOURNALNo ratings yet
- Farmacoterapia Actual y Futura en HTADocument15 pagesFarmacoterapia Actual y Futura en HTAGilbertoNo ratings yet
- Study of Drug Use in Essential Hypertension and Their ComplianceDocument13 pagesStudy of Drug Use in Essential Hypertension and Their ComplianceRachmat MuhammadNo ratings yet
- 2020 Hypertension Evolving From Standardized To PrecisionDocument4 pages2020 Hypertension Evolving From Standardized To PrecisionPeter Albeiro Falla CortesNo ratings yet
- Litrev Bu2Document8 pagesLitrev Bu2Deudeu Durotun NafisahNo ratings yet
- New Trends in The Diagnosis and Management of HypertensionDocument10 pagesNew Trends in The Diagnosis and Management of HypertensionJULIANA SANCHEZNo ratings yet
- CPG Management of Hypertension (4th Edition)Document98 pagesCPG Management of Hypertension (4th Edition)ssfdsNo ratings yet
- Guias Hipertension 2023 Esc AnalisisDocument12 pagesGuias Hipertension 2023 Esc Analisismiguel contrerasNo ratings yet
- 2019 In-Hospital Cardiac ArrestDocument11 pages2019 In-Hospital Cardiac Arrestbogeg74816No ratings yet
- Treatment of HypertensionDocument23 pagesTreatment of HypertensionRABIATUL ADAWIYAHNo ratings yet
- Circresaha 118 313220Document17 pagesCircresaha 118 313220Sarah ParadillahNo ratings yet
- JNC 8 SummaryDocument14 pagesJNC 8 Summaryamm1101No ratings yet
- In-Hospital Cardiac Arrest A ReviewDocument11 pagesIn-Hospital Cardiac Arrest A ReviewWawan JokoNo ratings yet
- 1 s2.0 073510979390074B Main PDFDocument2 pages1 s2.0 073510979390074B Main PDFRazali DerausNo ratings yet
- Hypertension in High Risk African Americans: Current Concepts, Evidence-based Therapeutics and Future ConsiderationsFrom EverandHypertension in High Risk African Americans: Current Concepts, Evidence-based Therapeutics and Future ConsiderationsNo ratings yet
- Hypertension in Children and Adolescents: New PerspectivesFrom EverandHypertension in Children and Adolescents: New PerspectivesEmpar LurbeNo ratings yet
- Reversing Chronic Hypertension Naturally : The Healthy way to Prevent the Silent KillerFrom EverandReversing Chronic Hypertension Naturally : The Healthy way to Prevent the Silent KillerNo ratings yet
- Drug Adherence in Hypertension and Cardiovascular ProtectionFrom EverandDrug Adherence in Hypertension and Cardiovascular ProtectionMichel BurnierNo ratings yet
- Secondary HypertensionFrom EverandSecondary HypertensionAlberto MorgantiNo ratings yet
- Precision Medicine in Cardiovascular Disease PreventionFrom EverandPrecision Medicine in Cardiovascular Disease PreventionSeth S. MartinNo ratings yet
- ZQMS-ARC-REC-002 Assignment CoverDocument9 pagesZQMS-ARC-REC-002 Assignment CoverGanizani MkandawireNo ratings yet
- Project Management Skills Unit 3 Notes - v1Document12 pagesProject Management Skills Unit 3 Notes - v1nikhilesh Prashanth100% (2)
- AQR InstitutionalInvestorMagazineArticle PDFDocument8 pagesAQR InstitutionalInvestorMagazineArticle PDFShyngys SuiindikNo ratings yet
- Decision Analysis: Dr. Keerti JainDocument54 pagesDecision Analysis: Dr. Keerti JainTushar GoelNo ratings yet
- OHSAS 18001 GuideDocument10 pagesOHSAS 18001 Guidevij2009No ratings yet
- Life Coaching Course HandbookDocument30 pagesLife Coaching Course HandbookAnne-Marie Abboud100% (2)
- Risk Assesment For Shifting of MEP Services and Re-Installations 26-03-2022Document5 pagesRisk Assesment For Shifting of MEP Services and Re-Installations 26-03-2022Zameer Basha Navzath AliNo ratings yet
- Application of Linear OptimizationDocument43 pagesApplication of Linear OptimizationAjey MendiolaNo ratings yet
- COSO I e IIDocument9 pagesCOSO I e IIcarakholNo ratings yet
- Basel III Fundamental Review of The Trading BookDocument20 pagesBasel III Fundamental Review of The Trading Book0123456789raNo ratings yet
- AASTU Mining Engineering project risk managementDocument11 pagesAASTU Mining Engineering project risk managementSarem AlemuNo ratings yet
- GreedzoneDocument2 pagesGreedzoneMatíasNo ratings yet
- Samiah International Builders LTD - Harshit VermaDocument27 pagesSamiah International Builders LTD - Harshit VermaStarNo ratings yet
- Introduction To Risk ManagementDocument20 pagesIntroduction To Risk ManagementLovelyn Megio ViolangoNo ratings yet
- Midterm Exam Risk Management PMGT 530Document8 pagesMidterm Exam Risk Management PMGT 530Shailesh MauryaNo ratings yet
- Ch5 - Test BankDocument12 pagesCh5 - Test BankMALAKNo ratings yet
- Excavation Works: R4 / BBR111, Bandar Bukit Raja 2, Klang, Selangor. 31. Excavation WorksDocument2 pagesExcavation Works: R4 / BBR111, Bandar Bukit Raja 2, Klang, Selangor. 31. Excavation WorksRafee Pie100% (2)
- Stress and Coping NotesDocument10 pagesStress and Coping NotesMinal Jain100% (1)
- Deliverable 4.4.: Forecasting Road Traffic Fatalities in European CountriesDocument411 pagesDeliverable 4.4.: Forecasting Road Traffic Fatalities in European CountriesEndashu KeneaNo ratings yet
- HarvardDocument7 pagesHarvardnochieng634No ratings yet
- Accidental Loading On BuildingsDocument22 pagesAccidental Loading On Buildingssubin_mampallyNo ratings yet
- Marine Risk Assessment PDFDocument160 pagesMarine Risk Assessment PDFPeyman Mzn100% (1)
- Re InsuranceDocument9 pagesRe Insurancepradeep3673No ratings yet
- Corporate Governance Business Ethics Risk Management and Internal Control by Cabrera 2019 2020 PDF FreeDocument355 pagesCorporate Governance Business Ethics Risk Management and Internal Control by Cabrera 2019 2020 PDF FreeRose Marie Miag-aoNo ratings yet
- The Story of Statistics in Geotechnical EngineeringDocument24 pagesThe Story of Statistics in Geotechnical EngineeringfakeNo ratings yet
- Risk Management Plan: Shangrila May Dimol-Bergonio, MDDocument15 pagesRisk Management Plan: Shangrila May Dimol-Bergonio, MDShang DimolNo ratings yet
- DLL 4th Week HazardsDocument16 pagesDLL 4th Week HazardsmjcNo ratings yet
- Kingston Marine Park Plans PAPER DDocument8 pagesKingston Marine Park Plans PAPER DOnTheWightNewsNo ratings yet