Professional Documents
Culture Documents
Seminar: Epidemiology
Uploaded by
Sol LakosOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Seminar: Epidemiology
Uploaded by
Sol LakosCopyright:
Available Formats
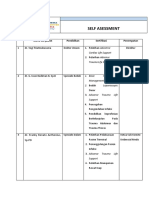
Seminar
Arterial hypertension
Sofie Brouwers, Isabella Sudano, Yoshihiro Kokubo, Elisabeth M Sulaica
Arterial hypertension is the most important contributor to the global burden of disease; however, disease control Published Online
remains poor. Although the diagnosis of hypertension is still based on office blood pressure, confirmation with out- May 18, 2021
https://doi.org/10.1016/
of-office blood pressure measurements (ie, ambulatory or home monitoring) is strongly recommended. The definition S0140-6736(21)00221-X
of hypertension differs throughout various guidelines, but the indications for antihypertensive therapy are relatively
Department of Cardiology,
similar. Lifestyle adaptation is absolutely key in non-pharmacological treatment. Pharmacologically, angiotensin- Cardiovascular Center Aalst,
converting enzyme inhibitors or angiotensin receptor blockers, calcium channel blockers, and diuretics are the first- OLV Hospital Aalst, Aalst,
line agents, with advice for the use of single-pill combination therapy by most guidelines. As a fourth-line agent, Belgium (S Brouwers MD);
Department of Experimental
spironolactone should be considered. The rapidly evolving field of device-based therapy, especially renal denervation, Pharmacology, Faculty of
will further broaden therapeutic options. Despite being a largely controllable condition, the actual rates of awareness, Medicine and Pharmacy, Vrije
treatment, and control of hypertension are disappointingly low. Further improvements throughout the process of Universiteit Brussel, Brussels,
patient screening, diagnosis, treatment, and follow-up need to be urgently addressed. Belgium (S Brouwers);
University Heart Center,
Cardiology, University Hospital
Epidemiology China, it was found that 44·7% of patients were Zurich, University of Zurich,
Hypertension is one of the most important modifiable hypertensive and only 44·7% of those with hypertension Zurich, Switzerland
risk factors for cardiovascular disease and one of were aware of their condition.4 Even more compelling, (I Sudano MD); Department of
Preventive Cardiology,
the largest contributors to morbidity and mortality only 30·1% of patients were prescribed antihypertensive National Cerebral and
worldwide. In a systematic analysis done for the Global agents and 7·2% had their blood pressure controlled. Cardiovascular Center, Suita,
Burden of Disease Study 2017, high systolic blood When standardised for age and sex, hypertension had Japan (Y Kokubo MD); Institute
pressure (SBP) was the leading risk factor for mortality rates of 37·2% for prevalence, 36·0% for awareness, of Cardiovascular and Medical
Sciences, University of
(10·4 million deaths) and disability-adjusted life-years 22·9% for treatment, and 5·7% for control. Glasgow, Glasgow, UK
(218 million).1 In a study including 8·69 million In the African population, a systematic review and (Y Kokubo); Pharmacy Practice
participants from 154 countries, it was estimated that meta-analysis of data from 25 studies showed a pooled and Translational Research,
between 1990 and 2015, the number of participants with prevalence of 5·5% in children and adolescents with University of Houston College
of Pharmacy, Houston, TX, USA
an SBP of at least 110–115 mm Hg increased from elevated blood pressure (≥95th percentile) and of 12·7% (E M Sulaica PharmD)
73·1% to 81·3%, and those with an SBP of at least in children and adolescents with slightly elevated blood Correspondence to:
140 mm Hg increased from 17·3% to 20·5%.2 Add pressure (≥90th percentile and <95th percentile).5 Prof Sofie Brouwers, Department
itionally, the estimated rate of annual deaths associated Increased body-mass index was largely associated with of Cardiology, Cardiovascular
with an SBP of at least 110–115 mm Hg increased by prevalence of elevated blood pressure, which was Center Aalst, OLV Hospital Aalst,
Aalst 9300, Belgium
7·1% from 1356 per million, and deaths associated with six times higher in children and adolescents (aged sofie.brouwers@olvz-aalst.be
an SBP of at least 140 mm Hg increased by 8·6% from 2–19 years) with obesity than in age-matched individuals
979 per million. without obesity. From a public health standpoint, it is
According to the 2019 May Measurement Month
campaign initiated by the International Society of
Hypertension (ISH), involving more than 1·5 million Search strategy and selection criteria
individuals screened from 92 countries, 32·0% had never We searched PubMed and MEDLINE for articles published
had their blood pressure measured and 34·0% had been from Jan 1, 2010, to Oct 25, 2020. We used the search terms
diagnosed with hypertension, among whom 58·7% were “blood pressure”, “hypertension”, “arterial hypertension”,
aware that they had hypertension and 54·7% were on in combination with the terms “guidelines”, “chronotropy”,
antihypertensive medications.3 In patients with hyper “resistant hypertension”, “diabetes”, “ambulatory blood
tension, 31·7% had blood pressure readings below pressure monitoring”, “home blood pressure measurement”,
140/90 mm Hg and 23·3% below 130/80 mm Hg. Of “digital health”, “mobile health”, “lifetime risk”, “prospective
patients on at least one antihypertensive, 57·8% had blood studies”, “epidemiology”, “population”, “lifetime blood
pressure readings below 140/90 mm Hg and 28·9% below pressure”, “diet”, “lifestyle”, “periodontitis”, “inflammation”,
130/80 mm Hg. Of patients taking antihypertensive “renin-angiotensin system”, “angiotensin-(1–7)”, “novel
medications, half were single-drug users. Since May, 2017, coronavirus disease 2019”, “genome-wide association”,
more than 4·2 million participants had their blood and “global”. We largely selected publications from the past
pressure measured and almost 1 million adults with 5 years, but did not exclude commonly referenced and highly
hypertension were untreated or undertreated. regarded older publications. We also searched the reference
Globally, hypertension awareness varies, with at least lists of articles identified by this search strategy and selected
70% of people with hypertension from the Americas and those we judged relevant. Review articles and book chapters
Europe being aware of their condition compared with are cited to provide readers with more details and references
only up to 40% of patients from south Asia and sub- than this Seminar has room for.
Saharan Africa. In a sample of 1·7 million adults in
www.thelancet.com Published online May 18, 2021 https://doi.org/10.1016/S0140-6736(21)00221-X 1
Seminar
essential to prevent obesity to improve hypertension, systemic inflammation, leading to increased blood
given that the factors contributing to increased body- pressure.
mass index are applicable to Africans spanning from Interactions between genes and the environment
childhood5 to adulthood.6 The meta-analysis also found illustrate the benefit of common lifestyle modifications
that elevated blood pressure was more pervasive in rural based on the recommendations of hypertension guide
areas than in urban areas; however, no differences in lines, which consist of the following elements: weight
prevalence were observed between boys and girls.5 reduction, a healthy diet, dietary sodium reduction,
Another study showed that the prevalence of hyper increased physical activity, and the cessation of smoking
tension is higher in people of African origin than in and excessive alcohol consumption.24
those of European origin.7 As well as these environmental factors, a complex genetic
In a study done in the USA, the strongest increase background has a role, which research is continuing to
from ideal blood pressure to pre-hypertension occurs at expand on.25 Data from genome-wide association studies
age 8 years for boys of White ethnicity, and at age on blood pressure traits (systolic, diastolic, and pulse
25 years for young African Americans, illustrating pressure) have led to greater understanding of important
how heterogeneity in blood pressure starts appearing loci involved in blood pressure. The discovery of novel loci
at a young age.8 Pre-emptive prophylaxis beginning has clarified new mechanisms of blood pressure regulation
in early adulthood might be necessary to prevent and the association between blood pressure and lifestyle.26,27
pre-hypertension and hyperten sion, as well as the
development of associated racial, ethnic, and gender The renin–angiotensin–aldosterone system (RAAS) and
disparities that could be variably interpreted.9,10 An COVID-19
analysis of the original cohort in the Framingham Heart Throughout the COVID-19 pandemic, a key consideration
Study showed that individuals in the community of hypertension pathophysiology and management has
generally maintained SBP below 120–125 mm Hg; been the effect of SARS-CoV-2 on the RAAS system.
however, when SBP began to rise above this range, it SARS-CoV-2 has been proposed to gain entry into cells
increased relatively rapidly towards overt hypertension.11 through endocytosis, by binding to angiotensin-
This tendency was consistent, regardless of whether or converting enzyme (ACE) 2.28 This theory has led to
not hypertension appeared early or late in life. discussion around discontinuing ACE inhibitors or
Interestingly, a large-scale analysis of individual patient angiotensin receptor blockers (ARBs) due to concern
trajectories provided evi dence that lifetime SBP and for ACE2 upregulation and subsequent increase in
diastolic blood pressure were most elevated at least SARS-CoV-2 virility. To our knowledge, clinical studies
14 years before death, and subsequently decreased until in this population are observational in nature and an
death.12 64·0% of the patients included in this analysis association between use of ACE inhibitors or ARBs and
had SBP decreases of at least 10 mm Hg. This reduction increased SARS-CoV-2 infection or severity of COVID-19
was present in all individuals, including those who did has not been found.29–35 Multiple prospective, ongoing,
not receive anti hypertensive treatment, and was most randomised trials will evaluate the outcomes of ACE
pronounced in older patients and in patients treated for inhibitor or ARB use or discontinuation in the setting of
hypertension, dementia, heart failure, or late-life weight COVID-19 (NCT04591210; NCT04353596). Interestingly,
loss. SARS-CoV-2 infection has also been shown to result
in ACE2 downregulation after initial binding to recep
Pathophysiology tors.28,36 ACE2 is important in counteracting effects of
Hypertension can be classified as essential or secondary, the RAAS system and, thus, there is also discussion
with most patients having essential hypertension.13 around the possible benefits of RAAS attenuation in
The cause of hypertension is multifactorial in nature, with COVID-19.37 Current recommendations are to avoid
environment, genetics, and social determinants having discontinuing RAAS inhibitors when they are clinically
the potential to contribute to its development.13 A better indicated and especially if they are the cornerstone of the
understanding of the interplay between these components therapy, like in heart failure and ischaemic heart
has continued to unfold.14 disease.37–39
Increasing knowledge has also been gathered on the
pathophysiology of hypertension. Besides the traditional Diagnosis
environmental factors (eg, obesity, physical inactivity, Blood pressure measurements
excessive sodium intake, and chronic stress), preterm Accurate and reliable blood pressure measurements
birth or low birthweight,15,16 and air and noise pollution,17,18 are essential for the diagnosis of hypertension. Blood
have also been shown to contribute to the development pressure changes constantly in response to endogenous
of the condition. Additionally, immune mechanisms and factors and exogenous stimuli; therefore, standardisation
systemic inflammation have proven to be important in is essential for an accurate measurement.40 Unfortunately,
the pathogenesis of hypertension.19,20 In particular, gut the problem of unstandardised measurements has
microbiota21,22 and periodontitis23 seem to play a role in persisted for decades, despite efforts in education and
2 www.thelancet.com Published online May 18, 2021 https://doi.org/10.1016/S0140-6736(21)00221-X
Seminar
simplification of the measurement process. The wide consensus on definitions, thresholds and targets, and
spread availability of non-validated blood pressure devices demonstration that interventions mitigating blood
might lead to incorrect diagnosis41 and management.42 pressure variability improve outcomes.
The Lancet Commission on hypertension43,44 aimed to
identify key actions for improving global management Classification
of blood pressure, both at population and individual The definition of arterial hypertension is based in all
levels. To obtain correct blood pressure measurements, available guidelines on office blood pressure.48–50 Although
trained observers using standardised methodologies are the definition of arterial hypertension differs between the
needed.45–47 Multiple readings over time are required to 2018 European Society of Cardiology (ESC)–European
estimate blood pressure, allowing for regression to the Society of Hypertension (ESH) guidelines,48 the 2017
mean, and mitigating risk of obtaining elevated readings American College of Cardiology (ACC)–American Heart
secondary to white-coat hypertension.43,48 The most used Association (AHA) guidelines,49 and the 2020 ISH
methods for measuring blood pressure in a clinical care guidelines (table 1),50 the indications for antihypertensive
setting are either direct (ie, intra-arterial) or indirect (ie, therapy are similar: patients with a blood pressure of
cuff-based). Indirect blood pressure measurements are at least 140/90 mm Hg should be treated if the cardio
typically done via auscultation or with a semi-automated vascular risk is high or if signs of target organ damage are
or fully automated device, which most often uses the present. In patients with grade 1 hypertension (definitions
oscillometric technique. Use of automated measurements vary depending on the guideline),48,49 at low-to-moderate
might avoid observer bias; however, there are situations cardiovascular risk, and without evidence of hypertension-
(eg, increased arterial stiffness or arrhythmias) in which mediated organ damage, drug treatment to lower blood
use of automated devices can lead to error. Although office pressure is recommended if the patient remains
blood pressure is still the gold standard for diagnosing hypertensive after a period of lifestyle intervention.58
arterial hypertension, contemporary guidelines recom All guidelines agree that many blood pressure
mend confirming the diagnosis with out-of-office mea measurements are necessary to correctly diagnose
surements, such as ambulatory or home blood pressure arterial hypertension.48–50 In all patients who have an
monitoring.48–51 24 h ambulatory and home blood pressure elevated office blood pressure, diagnosis should be
monitoring were shown to be superior to office mea confirmed by use of out-of-office blood pressure
surements for prediction of cardiovascular events and are measurements (ie, home or ambulatory blood pressure
ideal for follow-up monitoring in the long term.48–50 monitoring). Out-of-office measurements are also useful
Unattended blood pressure measurements eliminate for diagnosing white coat or masked hypertension. It
patient–observer interaction, minimise patient anxiety, should be noted that values classified as normal are
and reduce observer error associated with manual different for office and out-of-office measurements
measurement.52 This method was used for the first time (table 2).
in the SPRINT trial.53 On average, unattended SBP is
10 mm Hg lower than the office sphygmomanometer
Systolic and diastolic blood pressure,
or oscillometric value (depending on baseline blood mm Hg
pressure), and should not be used interchangeably with
American College of Cardiology–American Heart Association49
other office measurements.54 Large randomised con
Normal <120 and <80
trolled trials exploring use of unattended blood pressure
Increased 120–129 and <80
measurements for predicting hypertension-mediated
organ damage, as well as the correlation between this Stage 1 130–139 or 80–89
method and cardiovascular morbidity and mortality, are Stage 2 ≥140 or ≥90
still needed. European Society of Cardiology–European Society of Hypertension48
Blood pressure variability is considered to be a potential Optimal <120 and <80
novel risk factor for cardiovascular disease. Blood pressure Normal 120–129 or 80–84, or both
is not a constant variable; rather, it shows marked High-normal 130–139 or 85–89, or both
spontaneous oscillations over short-term (minutes to days) Stage 1 140–159 or 90–99, or both
and long-term (day-to-day, visit-to-visit, or seasonal) Stage 2 160–179 or 100–109, or both
periods, and studies in animal models indicate that Stage 3 ≥180 or ≥110, or both
development of target organ damage is associated with Isolated systolic hypertension ≥140 and <90
increased variability in blood pressure.55 Additionally, International Society of Hypertension50
in both the general population and patients with hyper Normal <130 and <85
tension, studies have shown that the degree of short-term High-normal 130–139 or 85–89, or both
and long-term variability in blood pressure is independently Grade 1 hypertension 140–159 or 90–99, or both
associated with target organ damage and an increased rate Grade 2 hypertension ≥160 or ≥100, or both
of cardiovascular events.56,57 However, many aspects related
Table 1: Classification of office blood pressure by class or grade, mm Hg
to blood pressure variability need to be clarified, including
www.thelancet.com Published online May 18, 2021 https://doi.org/10.1016/S0140-6736(21)00221-X 3
Seminar
additional markers of increased risk of cardiovascular
American College of Cardiology– European Society of Cardiology–
American Heart Association49 European Society of disease.
Hypertension48 and International Optimal blood pressure target is still a matter of debate.
Society of Hypertension50 The SPRINT trial53 showed a reduction in cardiovascular
Office BPM, mm Hg <130/80 <140/90 outcomes (including death) with an intensive unattended
Home BPM, mm Hg <130/80 <135/85 SBP target of below 120 mm Hg, compared with the
24 h ambulatory BPM, mm Hg <125/75 <130/80 standard SBP target of below 140 mm Hg. This reduction
Awake ambulatory BPM, mm Hg <130/80 <135/85 was counterbalanced by an increase in side-effects,
Sleep ambulatory BPM, mm Hg <110/65 <120/70 including electrolyte abnormalities, worsening of renal
function, and hypotension. This study excluded patients
BPM=blood pressure monitoring.
with a history of diabetes or stroke, thus limiting extra
Table 2: Normal values of blood pressure according to the methods used for screening polation of these results to all patients with hypertension.
Of note, unattended blood pressure might be up to
10 mm Hg lower than blood pressure measured with a
Panel 1: Assessment of hypertension-mediated organ damage health-care professional present;59 however, hypertensive
organ damage appears to be similar regardless of the
Asymptomatic hypertension-mediated organ damage measurement method used.60
• Arterial stiffening The ACCORD study61 and multiple meta-analyses62
• Pulse pressure >60 mm Hg (in older people aged >65 years) have not found significant benefits with more intensive
• Carotid–femoral pulse wave velocity >10 m/s versus less intensive blood pressure targets. Furthermore,
• Electrocardiogram LV hypertrophy (Sokolow-Lyon index >35 mm or R in augmented the results from the HOPE-3 trial58 did not reflect a
Vector Left ≥11 mm; Cornell voltage-duration product >2440 mm ms, or Cornell reduction in cardiovascular outcomes with blood pressure
voltage >28 mm in men or >20 mm in women) reduction to below 140/90 mm Hg. In contrast to these
• Echocardiographic LV hypertrophy (LV mass index >50 g/m²·⁷ in men and >47 g/m²·⁷ in reports, a robust meta-analysis evaluated individual
women [height in m²·⁷]; indexation for BSA [LV mass/BSA] might be used in patients participant-level data from randomised clinical trials
with healthy weight: >115 g/m² in men and >95 g/m² in women) from the Blood Pressure Lowering Treatment Trialists
• Microalbuminuria (30–300 mg/24 h) or elevated albumin–creatinine ratio Collaboration63 and showed that a 5 mm Hg reduction in
(30–300 mg/g; 3·4–34·0 mg/mmol), preferentially on morning spot urine blood pressure resulted in a decrease of major adverse
• Moderate CKD with eGFR >30–59 mL/min/1·73 m² (BSA) or severe CKD with cardiovascular events by approximately 10%, regardless
eGFR <30 mL/min/1·73 m² of baseline blood pressure (range <120 to ≥170 mm Hg)
• Ankle-brachial index <0·9 or history of a previous cardiovascular event. These
• Advanced retinopathy: haemorrhages or exudates, papilloedema results suggest the consideration of blood pressure
Established cardiovascular or renal disease lowering treatment to reduce elevated cardiovascular risk,
• Cerebrovascular disease—eg, ischaemic stroke, cerebral haemorrhage, transient independent of thresholds or history of cardiovascular
ischaemic attack disease.
• Coronary artery disease—eg, myocardial infarction, angina, myocardial revascularisation Considering the nuances of the data, an SBP target of
• Presence of atheromatous plaque on imaging below 130 mm Hg for attended blood pressure or below
• Heart failure, including heart failure with preserved ejection fraction 120 mm Hg for unattended blood pressure might be
• Peripheral artery disease reasonable to target to optimise the balance of efficacy and
• Atrial fibrillation safety for most patients. Specific patient characteristics
should be taken into account when establishing blood
LV=left ventricular. BSA=body surface area. CKD=chronic kidney disease. eGFR=estimated glomerular filtration rate. pressure targets (eg, age, comorbidities, level of cardio
vascular risk).
Treatment thresholds and targets Screening for hypertension-mediated organ damage
The ESC–ESH guidelines suggest that office blood All guidelines agree that assessment of hypertension-
pressure should be reduced below 140/90 mm Hg, with mediated organ damage is needed to estimate the
an optimal range around 130/80 mm Hg.48 If tolerated, cardiovascular risk of a patient with hypertension.48–50
office blood pressure could be further reduced, but Assessment of hypertension-mediated organ damage is
possibly not below 120/70 mm Hg. The ACC–AHA summarised in panel 1.
guidelines49 suggest an office blood pressure target of
below 130/80 mm Hg for adults with confirmed Secondary hypertension
hypertension and cardiovascular disease or for those Secondary hypertension is a type of hypertension with
with a 10-year event risk of atherosclerotic cardiovascular a potentially correctable underlying cause. Secondary
disease of 10% or higher. An office blood pressure hypertension should be considered in young patients
target of below 130/80 mm Hg is also noted to be without a family history of arterial hypertension, in
reasonable in patients with hypertension but without patients with resistant hypertension, and in patients with
4 www.thelancet.com Published online May 18, 2021 https://doi.org/10.1016/S0140-6736(21)00221-X
Seminar
Possible diagnosis Diagnostic tests
Different blood pressure (≥20/10 mm Hg) between upper and lower Coarctation of the aorta Echocardiography, chest radiograph, MRI
extremities, right and left arms, or both; delayed femoral pulsations,
interscapular ejection murmur, rib notching on chest radiograph
Peripheral oedema, pallor, loss of muscle mass Renal parenchymal disease Creatinine, ultrasound of the kidney
Abdominal bruits, peripheral vascular disease Renal artery stenosis Duplex, CT, MRI, angiography
Fatigue, constipation, polyuria, polydipsia, muscle weakness Primary aldosteronism Aldosterone–renin ratio
Weight gain, impotence, fatigue, psychological changes, polydipsia and Cushing’s syndrome 24 h urinary cortisol, dexamethasone
polyuria, obesity, hirsutism, skin atrophy, striae rubrae, muscle testing
weakness, osteopenia
Headache, palpitations, flushing, anxiety, paroxysmal hypertension, Pheochromocytoma Plasma or 24 h urinary metanephrines,
pounding, headache, perspiration, palpitations, pallor 24 h urinary catecholamine
Palpitations, weight loss, anxiety, heat intolerance, tachycardia, atrial Hyperthyroidism (thyroid disease) Thyroid stimulating hormone,
fibrillation, accentuated heart sounds, exophthalmos tri-iodothyronine, thyroxine
Weight gain, fatigue, obstipation, bradycardia, muscle weakness, Hypothyroidism (thyroid disease) Thyroid stimulating hormone,
myxoedema tri-iodothyronine, thyroxine
Snoring, daytime sleepiness, morning headache, irritability, increase in Obstructive sleep apnoea Screening questionnaire,
neck circumference, obesity, peripheral oedema polysomnography
Modified from Sudano and colleagues.64
Table 3: Signs and symptoms suggesting specific causes of secondary hypertension
a late sudden onset of hypertension.64 In addition to
medical history, a secondary cause might be suggested by Panel 2: Examples of selective drugs that can elevate blood
symptoms (eg, flushing and sweating, suggestive of pressure
pheochromocytoma), examination findings (eg, a renal
bruit, suggestive of renal artery stenosis), or laboratory Oestrogen
abnormalities (eg, low or low-to-normal kalaemia, sug • Oral contraceptives
gestive of aldosteronism). Approximately 5–10% of adults Herbal
with hypertension have a secondary cause. The prevalence • Ephedra (Ma huang)
of secondary hypertension and the most common causes • Ginseng
vary by age group. Whenever a patient is diagnosed with
hypertension, the aim of the initial assessment must be Illicit
to rule in or out possible secondary causes (table 3). • Amphetamines
Additionally, adherence to therapy and use of substances • Cocaine
and drugs, which can increase blood pressure, should be Non-steroidal anti-inflammatory
considered (panel 2). • COX-2 inhibitors
• Ibuprofen
Treatment • Naproxen
Non-pharmacological and pharmacological
management of hypertension Psychiatric
Within the past 4 years, four major guideline writing • Buspirone
entities have published updates regarding hypertension • Carbamazepine
management: the ACC–AHA, the ESC–ESH, the • Clozapine
National Institute for Health and Care Excellence • Fluoxetine
(NICE), and, most recently, the ISH guidelines. The • Lithium
intent of the ISH guideline was to be written in a manner • Tricyclic antidepressants
that would be easy to use and apply in low-income, Steroid
middle-income, and high-income countries.50 • Methylprednisolone
Each set of guidelines notes that sodium restriction in • Prednisone
patients with hypertension is needed as there is a linear
relationship between reduction in sodium intake and Sympathomimetic
subsequent reduction in blood pressure in patients with • Decongestants
hypertension. Recommendations for sodium intake • Diet pills
range from up to 1·5–2·0 g/day to a general reduction Modified from Sudano and colleagues.64
in sodium intake.48–50 In conjunction with sodium
www.thelancet.com Published online May 18, 2021 https://doi.org/10.1016/S0140-6736(21)00221-X 5
Seminar
American College of Cardiology– European Society of Cardiology– National Institute for International Society of
American Heart Association European Society of Health and Care Hypertension 202050
201749 Hypertension 201848 Excellence 201967
Sodium <1500 mg/day (ideal) Limit to up to 2000 mg/day Encourage a reduction Avoid foods with high salt content
consumption in sodium intake
Diet DASH High in fruits and vegetables, Encourage a healthy DASH diet; high in fruits and vegetables,
low-fat dairy, fish, whole grains; diet polyunsaturated fats, and dairy; low in foods
low in red meat and saturated fats high in sugar, saturated fats, and trans fats
Alcohol ≤2 standard drinks* per day for <14 units/week for men†; Encourage a reduction ≤2 standard drinks‡ per day for men;
consumption men; ≤1 standard drinks* per day <8 units/week for women† in intake if excessive ≤1·5 standard drinks‡ per day for women
for women
Physical Aerobic exercise: 90–150 mins/ Aerobic exercise for ≥30 mins/day Encourage regular Moderate aerobic activity for 30 mins/day
activity week; dynamic resistance training: ≥5 days/week exercise ≥5 days/week or high-intensity interval
90–150 mins/week training; resistance or strength exercises
2–3 days/week
Weight Target ideal bodyweight Avoid BMI >30 kg/m² or waist NA Ethnic-specific BMI and waist
reduction circumference >102 cm in men or circumference cutoffs to avoid obesity
>88 cm in women
DASH=dietary approach to stop hypertension. NA=not applicable. BMI=body-mass index. *One standard drink contains roughly 14 g of pure alcohol, which is typically found in
12 oz of regular beer (usually about 5% alcohol), 5 oz of wine (usually about 12% alcohol), and 1·5 oz of distilled spirits (usually about 40% alcohol). †1 unit is equal to 125 mL of
wine or 250 mL of beer. ‡One standard drink is equivalent to 10 g of alcohol.
Table 4: Key lifestyle recommendations
dairy products should replace dairy high in saturated
Angiotensinogen Ca2+
fats. Plant-based diets have shown benefits, with a meta-
analysis finding a reduction in SBP of –5·53 mm Hg in
Calcium channel blocker participants following the DASH diet (Dietary Approach
Outside cell to Stop Hypertension), –0·95 mm Hg in those on a
Mediterranean diet, and –5·47 mm Hg in those on a
Renin
lacto-ovo-vegetarian diet.65 Diet, physical activity, and
weight reduction work to address obesity and subse
Inside cell quently reduce blood pressure. There is a complex
interplay between hypertension and risk factors for
Vasoconstriction • Myocardial contraction cardiovascular disease that stems from mechanisms
• Increased heart rate*
Angiotensin 1
such as insulin resistance, dysregulation of the RAAS
system, and endothelial dysfunction.66 Addressing
modifiable risk factors (eg, tobacco use, diabetes,
ACE Lumen Blood
dyslipidaemia, etc) might result in blood pressure
reduction and mitigation of overall progression of
Na+ cardiovascular disease. Key lifestyle recommendations
are summarised in table 4.
K+ Both the ESC–ESH and ACC–AHA guidelines
ACE inhibitor recommend ACE inhibitors, ARBs, calcium channel
blockers, and thiazide or thiazide-like diuretics as first-
Angiotensin 2 Na+
line agents (figure 1).48,49 It should be noted that first-line
pharmacological therapy should always be accompanied
Cl –
ARB
by non-pharmacological education and reinforcement at
Cl –
follow-up visits. Additionally, although lifestyle modifica
Thiazide-type tions can delay hypertension or allow patients to meet
Angiotensin receptor diuretic
their blood pressure targets, initiation of first-line phar
macological therapy should not be delayed in patients
Figure 1: Mechanisms of action for first-line antihypertensive medications with hypertension who qualify.
ACE=angiotensin-converting enzyme. ARB=angiotensin receptor blocker. Ca²⁺=calcium ion. Na⁺=sodium ion. The ESC–ESH guidelines only recommend β blockers as
Cl⁻=chloride ion. *Decreased heart rate associated with non-dihydropyridine calcium channel blocker use.
first-line therapy in the setting of a compelling comorbidity.48
Both the 2020 ISH and 2019 NICE guide lines provide
reduction, diet is also important. Intake should be high stepwise algorithms for management of antihypertensive
in fruits, vegetables, fish, and whole grains, and low in therapy.50,67 Table 5 provides an overview of guideline
processed foods, saturated fat, and red meat. Low-fat recommendations for therapy initiation.
6 www.thelancet.com Published online May 18, 2021 https://doi.org/10.1016/S0140-6736(21)00221-X
Seminar
The NICE guidelines recommend initiation with one
Therapy recommendations
agent for most patients.67 The authors provide rationale
that there is no new or compelling evidence to recom National Institute for Health and Care Excellence67
mend dual therapy upfront in most cases. By contrast, the Patients with hypertension and diabetes or aged <55 years and not of Black African or African-Caribbean
family origin (without diabetes)
ESC–ESH guidelines recommend upfront dual therapy
Step 1 A
because patients are less likely to reach blood pressure
Step 2 A plus C or D
targets with monotherapy and are likely to benefit with
Patients with hypertension without diabetes and either aged ≥55 years or of Black African or African-
multimodal pharmacological approaches.48 Caribbean family origin
Guideline writing entities are still divided over
Step 1 C
thiazide versus thiazide-like diuretics for hypertension
Step 2 C plus A or D
management. Current NICE and ISH guidelines recom
European Society of Cardiology–European Society of Hypertension48
mend initiation of thiazide-like diuretics (eg, indapamide
Step 1 A plus C or D
or chlorthalidone) over thiazide diuretics (eg, hydro
Step 2 A plus C plus D
chlorothiazide or bendroflumethiazide), and ACC–AHA
International Society of Hypertension50
guidelines note that chlorthalidone is preferred.49,50,67 By
Step 1 A plus C*† (low dose)
contrast, ESC–ESH guidelines state that either thiazide-
Step 2 A plus C* (full dose)
like or thiazide diuretics are reasonable to use for blood
Step 3 A plus C* plus D
pressure management.48 The conflict between guidelines
American College of Cardiology–American Heart Association49
stems from an absence of large, prospective, head-to-head
Step 1 A or C or D‡
trials comparing thiazide with thiazide-like diuretics in
patients with hypertension. A multicentre cohort study A is angiotensin-converting enzyme inhibitor or angiotensin receptor blocker; C is calcium channel blocker; and D is
comparing chlorthalidone with hydrochlorothiazide found thiazide-like or thiazide diuretic. *Dihydropyridine calcium channel blocker. †Angiotensin receptor blocker preferred in
no difference between the two treatment groups with Black patients. ‡Dual therapy upfront for patients with stage 2 hypertension and blood pressure ≥20/10 mm Hg above
target.
regard to cardiovascular outcomes (eg, acute myocardial
infarction, heart failure hospitalisation, or stroke); however, Table 5: Guideline recommendations for therapy initiation
there were more adverse effects, including electrolyte
abnor malities, syncope, and acute renal failure, in
patients taking chlorthalidone.6 An ongoing, open-label, calcium channel blockers.71,72 A 2019 study compared
randomised trial comparing chlorthalidone with hydro between amlodipine–hydrochlorothiazide, amlodipine–
chlorothiazide in veterans aged 65 years and older and perindopril, and perindopril–hydrochloro thiazide in
assessing time to a major cardiovascular event will African men and women with elevated blood pressure in
hopefully provide more clarity when deciding between six sub-Saharan African countries.73 These patients were
these agents (NCT021854).68 either on no antihypertensive therapy or on mono
Single-pill combination therapy, a combination of two therapy and had no history of cardiovascular disease. At
or more antihypertensive agents, is a way to decrease pill 6 months, SBP was significantly lower in the amlodipine–
burden and improve patient adherence.48 Quad therapy hydrochlorothiazide group and amlodipine–perindopril
(ie, four antihypertensive medications in one) was group than in the perindopril–hydrochlorothiazide group.
evaluated in the Quadpill trial.69 This trial assessed a A significant difference in SBP was not found between
quarter dose of four medications (irbesartan, amlodipine, the amlodipine–hydrochlorothiazide and amlodipine–
hydrochlorothiazide, and atenolol) in a single pill versus perindopril groups. Antihypertensive management for
placebo in patients with hypertension, and found a most Black patients can include a combination of calcium
greater reduction in blood pressure in the group receiving channel blocker plus RAAS inhibitor, calcium channel
a single-pill combination at 4 weeks. Although the sample blocker plus thiazide or thiazide-like diuretic, or RAAS
size was small and an assessment of cardiovascular inhibitor plus thiazide or thiazide-like diuretic to reach
outcomes is still needed, these results are promising and blood pressure targets. Of note, various guidelines
highlight the efficacy of a multimodal agent approach to recommend ARBs over ACE inhibitors in this population
hypertension management. Nevertheless, the potential due to the increased risk of angioedema observed in Black
for adverse effects with a polypill (eg, dizziness or hypo patients.50,74 Although there are some data (albeit scarce) in
tension in sensitive patients) should be carefully weighed, the Black population, more evidence is needed in these
especially in older patients or in patients prone to falls. patients and in the Asian population to better tailor
Black patients have a higher prevalence of hypertension therapy. The consensus statement for hypertension
diagnoses and are more likely to have poorer cardiovascular management in Asian patients recommends upfront
outcomes associated with the condition than non-Black initiation with a calcium channel blocker and RAAS
patients.49,70 ACE inhibitors or ARB monotherapy have inhibitor.75
been found to be less effective at controlling blood Resistant hypertension is defined as inadequate blood
pressure in Black patients than has monotherapy with pressure control with adherence to three antihypertensive
agents such as thiazide or thiazide-like diuretics and agents (calcium channel blocker, ACE inhibitor or ARB,
www.thelancet.com Published online May 18, 2021 https://doi.org/10.1016/S0140-6736(21)00221-X 7
Seminar
or thiazide or thiazide-like diuretic) at maximally tolerated control in this age group. Decisions for antihypertensive
doses.48–50,67 Options for add-on therapy include miner management should be all encompassing, not solely based
alocorticoid receptor antagonists, β blockers, and on age, and take into account considerations such as
α1 blockers. A meta-analysis found mineralocorticoid patient comorbidities, other medications that can affect
receptor antagonists to be the most effective add-on blood pressure, and level of frailty.
therapy for resistant hypertension. Compared with Although not approved for hypertension, SGLT2
doxazosin and bisoprolol, a significantly greater reduction inhibitors have been found to decrease SBP by around
in SBP was achieved with spironolactone in a double- 4 mm Hg.82 The mechanism for this reduction is thought
blind, placebo-controlled, crossover trial.76,77 Spironolactone to be secondary to inhibition of sodium reuptake and
should be considered as a fourth-line agent for hyper subsequent sodium excretion.83 This effect of SGLT2
tension in the absence of contraindications. inhibitors is something to consider when managing
There might be instances in which reducing a medication patients with diabetes and hypertension; although not an
dose or even discontinuing medication altogether could be antihypertensive agent, its antihypertensive effects could
considered in patients with blood pressures below the allow for maximisation of blood pressure control in
optimal target, or in the case of adverse events. A systematic conjunction with diabetes management.
review found that factors such as monotherapy and lower
blood pressure before withdrawal were both predictors of Device-based treatment
success with regard to blood pressure control.78 The blood Various device-based therapies have emerged, such as
pressure of approximately 40% of patients was found to renal denervation, carotid baroreceptor stimulation,
still be controlled 1 year after medication withdrawal. creation of an arteriovenous fistula, or endovascular
Regardless of why medications are reduced in dose or are carotid body modification, and principally target the
discontinued, continual follow-up and monitoring for treatment of resistant or difficult-to-treat hypertension.
return of hypertension is paramount. Additionally, abrupt Renal denervation is the treatment modality with the
withdrawal of medications, particularly β blockers or most available data to date. The principle of this therapy
clonidine, should be avoided due to risk of deleterious is to eliminate sympathetic nerves around the renal
effects. Further research is needed to identify ideal patients artery, resulting in lower renal efferent and afferent
for whom to consider withdrawal, and to assess the long- sympathetic nervous activity and ultimately lower blood
term outcomes. pressure. The first results of renal denervation were
A 2020 publication longitudinally evaluating blood obtained with devices that used radiofrequency appli
pressure differences between sexes found that women cation in the open-label SYMPLICITY HTN-184 and
had a more precipitous increase in blood pressure than SYMPLICITY HTN-285 trials, along with several case
men, starting in early adulthood.79 These results warrant series and observational studies. Despite showing
further exploration; however, they have not yet led to safety, the SYMPLICITY HTN-386 trial was unable
changes in hypertension management between sexes. In to show efficacy of renal denervation with a radio
general, sex-specific management should be considered, frequency catheter over sham treatment in patients with
especially in pregnant women. ACE inhibitors, ARBs, severe resistant hypertension on multiple medications.48
and direct renin inhibitors are contraindicated due to However, post-hoc analyses of the SYMPLICITY HTN-3
risk of foetal injury and death. Appropriate agents for trial underlined important trial limitations to consider,
hypertensive management include methyldopa, labetalol, including trial patient selection, differences in adherence
or nifedipine.48,49 Despite how women aged 65 years and to antihypertensive medications between the treatment
older are more likely to have higher blood pressure later groups, a higher use of antihypertensive drugs in the
in life than are men, there is currently no distinction in sham group, and technical failure in carrying out renal
pharmacological management between the two sexes.70 denervation in the intervention group (eg, an insufficient
It is well known that hypertension prevalence increases number of ablations, ablation in the distal part of the
with age. It was found that more than 50% of patients with artery and limited to the main renal artery, and first-time
hypertension aged 80 years and older in the USA have performance of renal denervation for some operators).
uncontrolled hypertension.80 Elevated blood pressure has These limitations led to a revision of renal denervation
been associated with poor cardiovascular outcomes in technology and technique. Since SYMPLICITY HTN-3,
older patients, yet questions of how much to lower SBP by several novel, sham-controlled studies have been done or
in this population continue to arise.81 In a subgroup are underway. The SPYRAL HTN-OFF MED,87,88 SPYRAL
analysis from the SPRINT trial, patients aged 75 years and HTN-ON MED,89 and RADIANCE-HTN SOLO90 trials
older were found to benefit more from intensive blood showed significant and consistent reductions in blood
pressure treatment (SBP <120 mm Hg) than from stan pressure (both office and ambulatory) in patients with
dard treatment (SBP <140 mm Hg). Current guidelines and without concomitant antihypertensive use. The
recommend that providers work with patients to reach SPYRAL HTN-OFF MED trial showed catheter-based
blood pressure targets in patients aged 65 years and older, renal denervation to be superior to a sham procedure,
given that data indicate benefits from blood pressure with the intervention safely lowering blood pressure in
8 www.thelancet.com Published online May 18, 2021 https://doi.org/10.1016/S0140-6736(21)00221-X
Seminar
the absence of antihypertensive medications.88 Possible pressure control is therapeutic inertia, which includes
response indicators to renal denervation therapy can be failure to start or intensify antihypertensive therapy,
divided into patients with increased arterial stiffness and despite not having blood pressure under control. This
those with increased neurogenic activity.91 Consideration conundrum can consequently lead to additional years of
of these factors and use of the revised techniques will exposure to high blood pressure. When the decision is
considerably improve future studies and ultimately made to start antihypertensive treatment, the patient
expand our knowledge on renal denervation. Data should have regularly scheduled follow-ups in the early
showing efficacy of renal denervation for hypertension phase that continue until blood pressure is controlled
in patients without pharmacological therapy led to under stable treatment. Another major concern in
discussion about device treatment of hypertension as a unsuccessful treatment is non-adherence. This common
possible area of a shared decision making approach. and persistent problem should be addressed from the
Less evidence is available on the effect of carotid start of treatment and throughout its course. From early
baroreceptor stimulation and endovascular carotid body on, it is important to extensively counsel the patient and
modification. Both techniques aim to reduce blood their support system about the clinical reasoning for
pressure through reduction of sympathetic tone. The treatment and the long-term risk of elevated blood
first-generation carotid baroreceptor stimulation device pressure. The sharing of responsibility for a patient’s
reduced blood pressure in controlled and uncontrolled cardiovascular health is pivotal to improve patient
clinical trials. Currently, there are no controlled clinical investment in their health, diet, lifestyle, and medication
trials proving efficacy in blood pressure reduction for the compliance. In addition, obtaining blood pressure targets
second-generation carotid sinus stimulator.92 Some (mostly in the short term will reinforce the patient’s confidence
uncontrolled) studies suggest that other techniques, such in their treatment and promote persistent blood pressure
as baroreflex amplification and carotid body modulation, control to increase the likelihood of cardiovascular
might lead to blood pressure reduction in patients with benefit. Simplified and tailored treatment regimens (eg,
difficult-to-treat hypertension. However, more evidence considering costs, use of single-pill combinations, etc)
regarding the safety and efficacy of these techniques from will be of great importance for treatment success.96,97
large, randomised, sham-controlled trials is needed before The greatest challenge beyond the short-term manage
implementing baroreflex amplification and carotid body ment of hypertension is maintaining therapy adherence.
modulation into routine clinical practice.93
Furthermore, the creation of an iliac arteriovenous Health-care system
anastomosis to safely reduce blood pressure in patients
Awareness
with uncontrolled hypertension was assessed.94 The
ROX CONTROL HTN study95 evaluated this intervention
with the novel arteriovenous ROX Coupler (ROX
Screening
Medical; San Clemente, CA, USA). This small study, Treatment
Simplified and
involving 44 patients in the treatment group and tailored
39 patients in the standard care group, found that
creation of an arteriovenous anastomosis was associated
with a significant reduction in blood pressure. Due to
Sex, age, ethnicity, and
adverse events, including the development of venous concomitant disease
stenosis, the pivotal ROX HTN 2 trial was stopped.
The 2018 ESC–ESH guidelines do not recommend use
of device-based therapies for the routine treatment of Socioeconomic
hypertension, unless in the context of clinical studies status, lifestyle,
and behaviour
and randomised controlled trials.48 Nevertheless, device- Diagnosis Follow-up
based therapy for hypertension is a fast-moving field and • Blood pressure monitoring,
compliance, treatment
newly emerging data are now becoming available, which • Strongly supported by
could change this recommendation. digital health
Education
Timescales of treatment and follow-up
Hypertension Primary Patient
A short-term, medium-term, and long-term timescale Pharmacist
clinic care*
Patient
environment
can be distinguished in the course, challenges, and
treatment of arterial hypertension. A timely diagnosis, Figure 2: Key contributors in the process of blood pressure control and therapy adherence
which can only be obtained by regular blood pressure The patient is an integral part of their environment, and all interactions between the patient and various actors
measurements throughout an individual’s lifetime, is within the health-care system fall within this environment. The left side of the figure represents interactions
during the screening and diagnosis phase, whereas the right side represents the treatment and follow-up phase,
crucial in the management of hypertension. Additionally, containing many factors involved in therapy adherence. Treatment and follow-up are inseparably linked. The role
timely initiation of therapy is essential. Unfortunately, an of the pharmacist and hypertension clinic can vary widely among different health-care settings. *General
important issue in improving population-wide blood practitioner or community health worker.
www.thelancet.com Published online May 18, 2021 https://doi.org/10.1016/S0140-6736(21)00221-X 9
Seminar
Non-adherence is particularly frequent in patients with brain aminopeptidase A inhibitor, firibastat, is currently
apparently resistant hypertension and contributes to undergoing phase 2 (NCT03715998), and will soon
poor cardiovascular prognosis. Monitoring of adherence begin phase 3 (NCT04277884) trials.103 Upcoming trials
should be done routinely through open and non- will evaluate firibastat versus ramipril after myocardial
accusatory communication between the clinician and infarction (NCT03715998), and firibastat versus placebo
patient. Furthermore, indirect methods (eg, pill counts, in patients with uncontrolled primary hypertension.
tracking prescription refills, and self-reports) and direct Another promising pathway for new treatment targets
methods (eg, detection of drugs or their metabolites in is the protective arm of the RAAS (eg, ACE2, angiotensin
urine or plasma) have been developed.98 A continuous [1–7], AT2 receptor, Mas receptor axis), which has a
effort between patients and their health-care team needs counter-regulatory role in opposing AT1 receptor-
to be made to maintain, improve, and regain therapy mediated actions by mediating tissue protective and
adherence. regenerative actions (eg, vasodilation, natriuresis, and
Arterial hypertension is a chronic disease that requires anti-inflammatory, antiproliferative, and antifibrotic
regular follow-up in the long term. Management is a responses).104 Sex differences have been established in
multidisciplinary matter that should involve the primary the different mechanisms of action of the RAAS.105
health-care physician, hypertension specialist, and phar However, there are still important gaps in the scientific
macist, among other caregivers of the patient (figure 2). knowledge on the preclinical and clinical level of sex
Treatment plans should be made in conjunction with the differences in the pathogenesis and treatment of
most important member of the team—the patient—and hypertension.
their support system. By effectively educating patients A challenge in the management of hypertension is the
and their family, long-term compliance and adherence, follow-up of numerous patients. The field of digital
as well as early detection of changes in blood pressure, health, combining digital technologies and health care, is
are likely to be more successful. expanding rapidly and can improve different aspects of
The efforts of controlling blood pressure, along with the blood pressure management. The use of mobile health
other modifiable cardiovascular risk factors, ultimately applications are especially promising self-management
serve to reduce cardiovascular risk by preventing the tools, although not yet fully developed for hypertension.
progression of vascular damage. Conventional 10-year This technology not only provides information on home
risk prediction models identify individuals who would blood pressure measurements but also promotes lifestyle
benefit from therapy over the relative short term, whereas changes by giving advice on physical activity and healthy
cardiovascular risk estimations over a lifetime might be diet, and sending medication reminders.106–108 By actively
better suited to younger individuals who have a longer involving the patient, improved detection and manage
cumulative exposure to elevated blood pressure but a low ment of hypertension can be obtained, with promising
10-year cardiovascular risk. While awaiting evidence to opportunities for resource-limited settings.109 However,
establish the role of lifetime risk in treatment decisions, it further research is needed to identify effective strategies
is important to recognise that early implementation of for the wide implementation of evidence-based digital
preventative measures in younger patients might be health in this field.110
delayed with use of conventional 10-year risk prediction Machine learning and deep learning, two components
models. However, this subset of the population is likely to of artificial intelligence, are being increasingly used in
have the most success in maintaining a low-risk status the management of chronic diseases; however, they
and having a life free from cardiovascular disease, remain underexplored in the field of hypertension. More
by reducing cumulative exposure to elevated blood knowledge is needed on how to implement artificial
pressure.99–102 Older individuals, who are already at an intelligence in risk prediction, accuracy of blood pressure
elevated risk, are more likely to receive treatment but are measurement, treatment decisions, and management of
less likely to capture long-term benefits due to their age. patients with hypertension. Artificial intelligence will
also become an important tool for guiding clinical trials,
Future perspectives contributing to further development and implementation
For a largely controllable condition, the rates of awareness, of precision medicine.
treatment, and control of hypertension are disappointingly Contributors
low. There is room for improvement among the various SB designed the Seminar and coordinated the writing process, with input
levels of health care and throughout the process of patient from EMS. The epidemiology and pathophysiology sections were written
by YK, EMS, and SB. The diagnosis section was written by IS, EMS, and
screening, diagnosis, treatment, and follow-up. Previous SB. In the treatment section, the subsections on non-pharmacological
initiatives have reviewed the necessary actions to improve and pharmacological management of hypertension and timescales of
management of blood pressure worldwide.44 treatment and follow-up were written by EMS and SB, and the subsection
Medications available for hypertension management on device-based treatment was written by IS, SB, and EMS. The section
on future perspectives was written by SB and EMS. All authors
have not changed profoundly throughout previous participated in the literature search. SB and EMS produced the figures
decades. Excitingly, as more has been learned about the and entirely revised all versions of the manuscript. All authors approved
central regulation of blood pressure, a first-in-class the final version for publication.
10 www.thelancet.com Published online May 18, 2021 https://doi.org/10.1016/S0140-6736(21)00221-X
Seminar
Declaration of interests 19 Drummond GR, Vinh A, Guzik TJ, Sobey CG. Immune
IS reports consulting fees, speaker fees, and travel grants from Amgen, mechanisms of hypertension. Nat Rev Immunol 2019; 19: 517–32.
AstraZeneca, Boston Scientific, Daiichi Sankyo, Medtronic, Novartis, 20 Rodriguez-Iturbe B, Pons H, Johnson RJ. Role of the immune
Recordati, Sanofi, and Servier. All other authors declare no competing system in hypertension. Physiol Rev 2017; 97: 1127–64.
interests. 21 Marques FZ, Mackay CR, Kaye DM. Beyond gut feelings: how the gut
microbiota regulates blood pressure. Nat Rev Cardiol 2018; 15: 20–32.
Acknowledgments
22 Vallianou NG, Geladari E, Kounatidis D. Microbiome and
We thank H Zekollari for the fruitful discussions and help with the hypertension: where are we now? J Cardiovasc Med (Hagerstown)
design of figure 2. YK is supported by the Intramural Research Fund for 2020; 21: 83–88.
the National Cerebral and Cardiovascular Center (20–4–9), Osaka, Japan. 23 Muñoz Aguilera E, Suvan J, Buti J, et al. Periodontitis is associated
References with hypertension: a systematic review and meta-analysis.
1 Stanaway JD, Afshin A, Gakidou E, et al. Global, regional, Cardiovasc Res 2020; 116: 28–39.
and national comparative risk assessment of 84 behavioural, 24 Kokubo Y, Padmanabhan S, Iwashima Y, Yamagishi K, Goto A.
environmental and occupational, and metabolic risks or clusters of Gene and environmental interactions according to the components
risks for 195 countries and territories, 1990–2017: a systematic of lifestyle modifications in hypertension guidelines.
analysis for the Global Burden of Disease Study 2017. Lancet 2018; Environ Health Prev Med 2019; 24: 19.
392: 1923–94. 25 Ehret GB, Munroe PB, Rice KM, et al. Genetic variants in novel
2 Forouzanfar MH, Liu P, Roth GA, et al. Global burden of pathways influence blood pressure and cardiovascular disease risk.
hypertension and systolic blood pressure of at least Nature 2011; 478: 103–09.
110 to 115 mm Hg, 1990–2015. JAMA 2017; 317: 165–82. 26 Warren HR, Evangelou E, Cabrera CP, et al. Genome-wide association
3 Beaney T, Schutte AE, Stergiou GS, et al. May measurement month analysis identifies novel blood pressure loci and offers biological
2019: The Global Blood Pressure Screening Campaign of the insights into cardiovascular risk. Nat Genet 2017; 49: 403–15.
International Society of Hypertension. Hypertension 2020; 76: 333–41. 27 Evangelou E, Warren HR, Mosen-Ansorena D, et al. Genetic
4 Lu J, Lu Y, Wang X, et al. Prevalence, awareness, treatment, and analysis of over 1 million people identifies 535 new loci associated
control of hypertension in China: data from 1·7 million adults in a with blood pressure traits. Nat Genet 2018; 50: 1412–25.
population-based screening study (China PEACE Million Persons 28 Furuhashi M, Moniwa N, Takizawa H, Ura N, Shimamoto K.
Project). Lancet 2017; 390: 2549–58. Potential differential effects of renin-angiotensin system inhibitors
5 Noubiap JJ, Essouma M, Bigna JJ, Jingi AM, Aminde LN, on SARS-CoV-2 infection and lung injury in COVID-19.
Nansseu JR. Prevalence of elevated blood pressure in children and Hypertens Res 2020; 43: 837–40.
adolescents in Africa: a systematic review and meta-analysis. 29 Reynolds HR, Adhikari S, Pulgarin C, et al. Renin–angiotensin–
Lancet Public Health 2017; 2: e375–86. aldosterone system inhibitors and risk of covid-19. N Engl J Med
6 Colhoun HM, Hemingway H, Poulter NR. Socio-economic status 2020; 382: 2441–48.
and blood pressure: an overview analysis. J Hum Hypertens 1998; 30 Mancia G, Rea F, Ludergnani M, Apolone G, Corrao G.
12: 91–110. Renin-angiotensin-aldosterone system blockers and the risk of
7 Ibrahim MM, Damasceno A. Hypertension in developing countries. COVID-19. N Engl J Med 2020; 382: 2431–40.
Lancet 2012; 380: 611–19. 31 Mehra MR, Desai SS, Kuy S, Henry TD, Patel AN. Cardiovascular
8 Hardy ST, Holliday KM, Chakladar S, et al. Heterogeneity in blood disease, drug therapy, and mortality in COVID-19. N Engl J Med
pressure transitions over the life course: age-specific emergence of 2020; 382: e102.
racial/ethnic and sex disparities in the united states. JAMA Cardiol 32 Mehta N, Kalra A, Nowacki AS, et al. Association of use of
2017; 2: 653–61. angiotensin-converting enzyme inhibitors and angiotensin II
9 Falkner B, Lurbe E. Primordial prevention of high blood pressure in receptor blockers with testing positive for coronavirus disease 2019
childhood an opportunity not to be missed. Hypertension 2020; (COVID-19). JAMA Cardiol 2020; 5: 1020–26.
75: 1142–50. 33 de Abajo FJ, Rodríguez-Martín S, Lerma V, et al. Use of renin-
10 Kavey R-EW, Daniels SR, Lauer RM, Atkins DL, Hayman LL, angiotensin-aldosterone system inhibitors and risk of COVID-19
Taubert K. American Heart Association guidelines for primary requiring admission to hospital: a case-population study. Lancet
prevention of atherosclerotic cardiovascular disease beginning in 2020; 395: 1705–14.
childhood. Circulation 2003; 107: 1562–66. 34 Son M, Seo J, Yang S. Association between renin-angiotensin-
11 Niiranen TJ, Henglin M, Claggett B, et al. Trajectories of blood aldosterone system inhibitors and COVID-19 infection in
pressure elevation preceding hypertension onset: an analysis of the South Korea. Hypertension 2020; 76: 742–49.
Framingham Heart Study original cohort. JAMA Cardiol 2018; 35 Li J, Wang X, Chen J, Zhang H, Deng A. Association of renin-
3: 427–31. angiotensin system inhibitors with severity or risk of death in
12 Delgado J, Bowman K, Ble A, et al. Blood pressure trajectories in patients with hypertension hospitalized for coronavirus disease
the 20 years before death. JAMA Intern Med 2018; 178: 93–99. 2019 (COVID-19) infection in Wuhan, China. JAMA Cardiol 2020;
13 Carey RM, Muntner P, Bosworth HB, Whelton PK. Prevention and 5: 825–30.
control of hypertension: JACC Health Promotion Series. 36 Kuba K, Imai Y, Rao S, et al. A crucial role of angiotensin converting
J Am Coll Cardiol 2018; 72: 1278–93. enzyme 2 (ACE2) in SARS coronavirus-induced lung injury.
14 Taddei S, Bruno RM, Masi S, Solini A. Epidemiology and Nat Med 2005; 11: 875–79.
pathophysiology of hypertension. In: Camm AJ, Lüscher TF, 37 Vaduganathan M, Vardeny O, Michel T, McMurray JJV, Pfeffer MA,
Maurer G, Serruys PW, eds. The ESC textbook of cardiovascular Solomon SD. Renin-angiotensin-aldosterone system inhibitors in
medicine. Oxford: Oxford University Press, 2018: 2377–88. patients with COVID-19. N Engl J Med 2020; 382: 1653–59.
15 Haikerwal A, Doyle LW, Cheung MM, et al. High blood pressure in 38 Bozkurt B, Kovacs R, Harrington B. Joint HFSA/ACC/AHA
young adult survivors born extremely preterm or extremely low Statement addresses concerns re: using RAAS antagonists in
birthweight in the post surfactant era. Hypertension 2020; 75: 211–17. COVID-19. J Card Fail 2020; 26: 370.
16 Kanda T, Murai-Takeda A, Kawabe H, Itoh H. Low birth weight 39 De Simone G. Position statement of the ESC council on
trends: possible impacts on the prevalences of hypertension and hypertension on ACE-inhibitors and angiotensin receptor blockers.
chronic kidney disease. Hypertens Res 2020; 43: 859–68. March 13, 2020. https://www.escardio.org/Councils/Council-on-
17 Münzel T, Sørensen M, Gori T, et al. Environmental stressors and Hypertension-(CHT)/News/position-statement-of-the-esc-council-
cardio-metabolic disease: part I-epidemiologic evidence supporting on-hypertension-on-ace-inhibitors-and-ang (accessed Oct 25, 2020).
a role for noise and air pollution and effects of mitigation strategies. 40 Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood
Eur Heart J 2017; 38: 550–56. pressure measurement in humans and experimental animals:
18 Fuks KB, Weinmayr G, Basagaña X, et al. Long-term exposure to part 1: blood pressure measurement in humans: a statement for
ambient air pollution and traffic noise and incident hypertension in professionals from the Subcommittee of Professional and Public
seven cohorts of the European study of cohorts for air pollution Education of the American Heart Association Co. Circulation 2005;
effects (ESCAPE). Eur Heart J 2017; 38: 983–90. 111: 697–716.
www.thelancet.com Published online May 18, 2021 https://doi.org/10.1016/S0140-6736(21)00221-X 11
Seminar
41 Sharman JE, Marwick TH. Accuracy of blood pressure monitoring 60 Salvetti M, Paini A, Aggiusti C, et al. Unattended versus attended
devices: a critical need for improvement that could resolve blood pressure measurement. Hypertension 2019; 73: 736–42.
discrepancy in hypertension guidelines. J Hum Hypertens 2019; 61 Cushman WC, Evans GW, Byington RP, et al. Effects of intensive
33: 89–93. blood-pressure control in type 2 diabetes mellitus. N Engl J Med
42 Picone DS, Deshpande RA, Schultz MG, et al. Nonvalidated home 2010; 362: 1575–85.
blood pressure devices dominate the online marketplace in 62 Bangalore S, Toklu B, Gianos E, et al. Optimal systolic blood
Australia: major implications for cardiovascular risk management. pressure target after SPRINT: insights from a network meta-
Hypertension 2020; 75: 1593–99. analysis of randomized trials. Am J Med 2017; 130: 707–19.
43 Padwal R, Campbell NRC, Schutte AE, et al. Optimizing observer 63 Blood Pressure Lowering Treatment Trialists' Collaboration.
performance of clinic blood pressure measurement: a position Pharmacological blood pressure lowering for primary and
statement from the Lancet Commission on Hypertension Group. secondary prevention of cardiovascular disease across different
J Hypertens 2019; 37: 1737–45. levels of blood pressure: an individual participant-level data meta-
44 Olsen MH, Angell SY, Asma S, et al. A call to action and a lifecourse analysis. Lancet 2021; 397: 1625–36.
strategy to address the global burden of raised blood pressure on 64 Sudano I, Beuschlein F, Lüscher TF. Secondary causes of
current and future generations: the Lancet Commission on hypertension. In: Camm AJ, Lüscher TF, Maurer G, Serruys PW,
hypertension. Lancet 2016; 388: 2665–712. eds. The ESC Textbook of Cardiovascular Medicine, 3rd edit.
45 Picone DS, Padwal R, Campbell NRC, et al. How to check whether a Oxford: Oxford University Press, 2018: 2409–19.
blood pressure monitor has been properly validated for accuracy. 65 Gibbs J, Gaskin E, Ji C, Miller MA, Cappuccio FP. The effect of
J Clin Hypertens (Greenwich) 2020; 22: 2167–74. plant-based dietary patterns on blood pressure: a systematic review
46 Campbell NRC, Khalsa T, Ordunez P, et al. Brief online certification and meta-analysis of controlled intervention trials. J Hypertens 2020;
course for measuring blood pressure with an automated blood 39: 23–37.
pressure device. A free new resource to support World Hypertension 66 Kim J, Montagnani M, Koh KK, Quon MJ. Reciprocal relationships
Day Oct 17, 2020. J Clin Hypertens (Greenwich) 2020; 22: 1754–56. between insulin resistance and endothelial dysfunction. Circulation
47 Stergiou GS, Alpert B, Mieke S, et al. A universal standard for the 2006; 113: 1888–904.
validation of blood pressure measuring devices: Association for the 67 Jones NR, McCormack T, Constanti M, McManus RJ. Diagnosis and
Advancement of Medical Instrumentation/European Society of management of hypertension in adults: NICE guideline
Hypertension/International Organization for Standardization update 2019. Br J Gen Pract 2020; 70: 90–91.
(AAMI/ESH/ISO) Collaboration Statement. J Hypertens 2018; 68 Lederle FA, Cushman WC, Ferguson RE, Brophy MT, Fiore Md LD.
36: 472–78. Chlorthalidone versus hydrochlorothiazide: a new kind of veterans
48 Williams B, Mancia G, Spiering W, et al. 2018 practice guidelines affairs cooperative study. Ann Intern Med 2016; 165: 663–64.
for the management of arterial hypertension of the European 69 Chow CK, Thakkar J, Bennett A, et al. Quarter-dose quadruple
society of cardiology and the European society of hypertension combination therapy for initial treatment of hypertension: placebo-
ESC/ESH task force for the management of arterial hypertension. controlled, crossover, randomised trial and systematic review. Lancet
Eur Heart J 2018; 39: 3021–104. 2017; 389: 1035–42.
49 Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ 70 Virani SS, Alonso A, Benjamin EJ, et al. Heart disease and stroke
ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the statistics—2020 update: a report from the American Heart
prevention, detection, evaluation, and management of high blood Association. Circulation 2020; 141: e139–596.
pressure in adults: a report of the American College of Cardiology/
71 Wright JTJ Jr, Dunn JK, Cutler JA, et al. Outcomes in hypertensive
American Heart Association Task Force on clinical practice
Black and non-Black patients treated with chlorthalidone,
guidelines. J Am Coll Cardiol 2018; 71: e127–248.
amlodipine, and lisinopril. JAMA 2005; 293: 1595–608.
50 Unger T, Borghi C, Charchar F, et al. 2020 International Society of
72 Sulaica EM, Wollen JT, Kotter J, Macaulay TE. A review of
Hypertension global hypertension practice guidelines. Hypertension
hypertension management in Black male patients. Mayo Clin Proc
2020; 75: 1334–57.
2020; 95: 1955–63.
51 Stergiou GS, Palatini P, Parati G et al. 2021 European Society of
73 Ojji DB, Mayosi B, Francis V, et al. Comparison of dual therapies
Hypertension practice guidelines for office and out-of-office blood
for lowering blood pressure in Black Africans. N Engl J Med 2019;
pressure measurement. J Hypertens 2021; published online March 11.
380: 2429–39.
https://doi.org/10.1097/HJH.0000000000002843.
74 Kostis JB, Kim HJ, Rusnak J, et al. Incidence and characteristics of
52 Myers MG, Godwin M, Dawes M, Kiss A, Tobe SW, Kaczorowski J.
angioedema associated with enalapril. Arch Intern Med 2005;
Measurement of blood pressure in the office: recognizing the
165: 1637–42.
problem and proposing the solution. Hypertension 2010;
55: 195–200. 75 Kario K, Chen C-H, Park S, et al. Consensus document on
improving hypertension management in Asian patients, taking into
53 Wright JT Jr, Williamson JD, Whelton PK, et al. A randomized trial
account Asian characteristics. Hypertension 2018; 71: 375–82.
of intensive versus standard blood-pressure control. N Engl J Med
2015; 373: 2103–16. 76 Sinnott S-J, Tomlinson LA, Root AA, et al. Comparative
effectiveness of fourth-line anti-hypertensive agents in resistant
54 Wohlfahrt P, Cifkova R, Krajcoviechova A, et al. Unattended
hypertension: a systematic review and meta-analysis.
automated office blood pressure measurement. Does it differ from
Eur J Prev Cardiol 2017; 24: 228–38.
office blood pressure? Insight from a random population sample.
J Hypertens 2019; 37: e67. 77 Williams B, MacDonald TM, Morant S, et al. Spironolactone versus
placebo, bisoprolol, and doxazosin to determine the optimal
55 Irigoyen M-C, De Angelis K, Dos Santos F, Dartora DR,
treatment for drug-resistant hypertension (PATHWAY-2):
Rodrigues B, Consolim-Colombo FM. Hypertension, blood pressure
a randomised, double-blind, crossover trial. Lancet 2015;
variability, and target organ lesion. Curr Hypertens Rep 2016; 18: 31.
386: 2059–68.
56 McMullan CJ, Bakris GL, Phillips RA, Forman JP. Association of
78 van der Wardt V, Harrison JK, Welsh T, Conroy S, Gladman J.
BP variability with mortality among African Americans with CKD.
Withdrawal of antihypertensive medication: a systematic review.
Clin J Am Soc Nephrol 2013; 8: 731–38.
J Hypertens 2017; 35: 1742–49.
57 Sega R, Corrao G, Bombelli M, et al. Blood pressure variability and
79 Ji H, Kim A, Ebinger JE, et al. Sex differences in blood pressure
organ damage in a general population: results from the PAMELA
trajectories over the life course. JAMA Cardiol 2020; 5: 19–26.
study (Pressioni Arteriose Monitorate E Loro Associazioni).
Hypertension 2002; 39: 710–14. 80 Bromfield SG, Bowling CB, Tanner RM, et al. Trends in hypertension
prevalence, awareness, treatment, and control among US adults
58 Lonn EM, Bosch J, López-Jaramillo P, et al. Blood-pressure lowering
80 years and older, 1988–2010. J Clin Hypertens (Greenwich) 2014;
in intermediate-risk persons without cardiovascular disease.
16: 270–76.
N Engl J Med 2016; 374: 2009–20.
81 Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific
59 Keeley EC, Villanueva M, Chen YE, et al. Attended vs unattended
relevance of usual blood pressure to vascular mortality: a meta-
systolic blood pressure measurement: a randomized comparison in
analysis of individual data for one million adults in 61 prospective
patients with cardiovascular disease. J Clin Hypertens (Greenwich)
studies. Lancet 2002; 360: 1903–13.
2020; 22: 1987–92.
12 www.thelancet.com Published online May 18, 2021 https://doi.org/10.1016/S0140-6736(21)00221-X
Seminar
82 Baker WL, Buckley LF, Kelly MS, et al. Effects of sodium-glucose 96 Rea F, Corrao G, Merlino L, Mancia G. Initial antihypertensive
cotransporter 2 inhibitors on 24-hour ambulatory blood pressure: treatment strategies and therapeutic inertia evidence from a large
a systematic review and meta-analysis. J Am Heart Assoc 2017; population-based cohort. Hypertension 2018; 72: 846–53.
6: e005686. 97 Carey RM, Calhoun DA, Bakris GL, et al. Resistant hypertension:
83 Lopaschuk GD, Verma S. Mechanisms of cardiovascular benefits of detection, evaluation, and management a scientific statement from
sodium glucose co-transporter 2 (SGLT2) inhibitors: a state-of-the- the American Heart Association. Hypertension 2018; 72: e53–90.
art review. JACC Basic Transl Sci 2020; 5: 632–44. 98 Burnier M, Wuerzner G, Struijker-Boudier H, Urquhart J.
84 Krum H, Schlaich M, Whitbourn R, et al. Catheter-based renal Measuring, analyzing, and managing drug adherence in resistant
sympathetic denervation for resistant hypertension: a multicentre hypertension. Hypertension 2013; 62: 218–25.
safety and proof-of-principle cohort study. Lancet 2009; 373: 1275–81. 99 Ma Y, Wolters FJ, Chibnik LB, et al. Variation in blood pressure and
85 Esler MD, Krum H, Sobotka PA, Schlaich MP, Schmieder RE, long-term risk of dementia: a population-based cohort study.
Böhm M. Renal sympathetic denervation in patients with PLoS Med 2019; 16: e1002933.
treatment-resistant hypertension (The SYMPLICITY HTN-2 Trial): 100 Zhang Y, Vittinghoff E, Pletcher MJ, et al. Associations of blood
a randomised controlled trial. Lancet 2010; 376: 1903–09. pressure and cholesterol levels during young adulthood with
86 Bhatt DL, Kandzari DE, O’Neill WW, et al. A controlled trial of renal later cardiovascular events. J Am Coll Cardiol 2019; 74: 330–41.
denervation for resistant hypertension. N Engl J Med 2014; 101 Satoh M, Ohkubo T, Asayama K, et al. Lifetime risk of stroke and
370: 1393–401. coronary heart disease deaths according to blood pressure level:
87 Townsend RR, Mahfoud F, Kandzari DE, et al. Catheter-based renal EPOCH-JAPAN (Evidence for Cardiovascular Prevention From
denervation in patients with uncontrolled hypertension in the Observational Cohorts in Japan). Hypertension 2019; 73: 52–59.
absence of antihypertensive medications (SPYRAL HTN-OFF MED): 102 Qiu C, Winblad B, Fratiglioni L. The age-dependent relation of
a randomised, sham-controlled, proof-of-concept trial. Lancet 2017; blood pressure to cognitive function and dementia. Lancet Neurol
390: 2160–70. 2005; 4: 487–99.
88 Böhm M, Kario K, Kandzari DE, et al. Efficacy of catheter-based 103 Ferdinand KC, Balavoine F, Besse B, et al. Efficacy and safety of
renal denervation in the absence of antihypertensive medications firibastat, a first-in-class brain aminopeptidase A inhibitor,
(SPYRAL HTN-OFF MED Pivotal): a multicentre, randomised, in hypertensive overweight patients of multiple ethnic origins.
sham-controlled trial. Lancet 2020; 395: 1444–51. Circulation 2019; 140: 138–46.
89 Kandzari DE, Böhm M, Mahfoud F, et al. Effect of renal denervation 104 Unger T, Steckelings UM, Dzau VJ. The protective arm of the renin
on blood pressure in the presence of antihypertensive drugs: angiotensin system (RAS): functional aspects and therapeutic
6-month efficacy and safety results from the SPYRAL HTN-ON MED implications. London: Elsevier, 2015.
proof-of-concept randomised trial. Lancet 2018; 391: 2346–55. 105 Medina D, Mehay D, Arnold AC. Sex differences in cardiovascular
90 Azizi M, Schmieder RE, Mahfoud F, et al. Endovascular ultrasound actions of the renin-angiotensin system. Clin Auton Res 2020;
renal denervation to treat hypertension (RADIANCE-HTN SOLO): 30: 393–408.
a multicentre, international, single-blind, randomised, 106 Lu X, Yang H, Xia X, et al. Interactive mobile health intervention
sham-controlled trial. Lancet 2018; 391: 2335–45. and blood pressure management in adults: a meta-analysis of
91 Kandzari DE, Mahfoud F, Bhatt DL, et al. Confounding factors in randomized controlled trials. Hypertension 2019; 74: 697–704.
renal denervation trials: revisiting old and identifying new 107 Pellegrini D, Torlasco C, Ochoa JE, Parati G. Contribution of
challenges in trial design of device therapies for hypertension. telemedicine and information technology to hypertension control.
Hypertension 2020; 76: 1410–17. Hypertens Res 2020; 43: 621–28.
92 Heusser K, Thöne A, Lipp A, et al. Efficacy of electrical baroreflex 108 Parati G, Torlasco C, Omboni S, Pellegrini D. Smartphone
activation is independent of peripheral chemoreceptor modulation. applications for hypertension management: a potential game-
Hypertension 2020; 75: 257–64. changer that needs more control. Curr Hypertens Rep 2017; 19: 48.
93 Groenland EH, Spiering W. Baroreflex amplification and carotid 109 WHO. WHO guideline: recommendations on digital interventions
body modulation for the treatment of resistant hypertension. for health system strengthening. Geneva: World Health
Curr Hypertens Rep 2020; 22: 27. Organization, 2019.
94 Brouwers S, Droogmans S, Dolan E, et al. A prospective 110 World Health Assembly. Seventy-first World Health Assembly.
non-randomized open label multi-center study to evaluate the effect of Agenda item 12·4. Digital health. May 26, 2018. https://apps.who.
an iliofemoral arteriovenous fistula on blood pressure in patients with int/gb/ebwha/pdf_files/WHA71/A71_R7-en.pdf (accessed
therapy-resistant hypertension. Eur Heart J 2013; 34 (suppl 1): 3616. Oct 25, 2020).
95 Lobo MD, Sobotka PA, Stanton A, et al. Central arteriovenous
anastomosis for the treatment of patients with uncontrolled © 2021 Elsevier Ltd. All rights reserved.
hypertension (the ROX CONTROL HTN study): a randomised
controlled trial. Lancet 2015; 385: 1634–41.
www.thelancet.com Published online May 18, 2021 https://doi.org/10.1016/S0140-6736(21)00221-X 13
You might also like
- Cambridge Igcse Chemistry Revision Guide - Public PDFDocument50 pagesCambridge Igcse Chemistry Revision Guide - Public PDFMoarz Galaxy64% (11)
- Course Plan M.SC 2 YearDocument93 pagesCourse Plan M.SC 2 YearSanthu Su80% (5)
- Study of HypertensionDocument44 pagesStudy of HypertensionMathew PiNo ratings yet
- Nais Ew3002Document21 pagesNais Ew3002soring4No ratings yet
- Respiratory & Circulatory System Regents QuestionsDocument10 pagesRespiratory & Circulatory System Regents Questionsabisantiago613140% (5)
- Arterial HypertensionDocument13 pagesArterial HypertensionZedodurex100% (1)
- Frequency of ABO:Rh Blood Groups and Social Condition of Hypertensive Patients in LuanDocument5 pagesFrequency of ABO:Rh Blood Groups and Social Condition of Hypertensive Patients in LuanEduardo Ekundi ValentimNo ratings yet
- Prevalence and Prognosis of Atrial Fibrillation in A HypertensiveDocument8 pagesPrevalence and Prognosis of Atrial Fibrillation in A HypertensiveSyadzwina Putri salsabilaNo ratings yet
- The Prevalence of ArterialDocument8 pagesThe Prevalence of ArterialInternational Medical PublisherNo ratings yet
- JCH 13 523Document6 pagesJCH 13 523Bunga dewanggi NugrohoNo ratings yet
- Tgs Jurnal 1Document7 pagesTgs Jurnal 1suciNo ratings yet
- Farmacocinetica e Genero - Grupo 2Document17 pagesFarmacocinetica e Genero - Grupo 2Paula ValeriNo ratings yet
- Ibpc 13 95 PDFDocument8 pagesIbpc 13 95 PDFKevin Palma AnguloNo ratings yet
- Resistant HypertensionDocument12 pagesResistant Hypertensionsury listinNo ratings yet
- MMM19Document3 pagesMMM19CLAUDIO MBALANo ratings yet
- Management of HypertensionDocument4 pagesManagement of HypertensionPutri ReginaNo ratings yet
- Effects of Different Antihypertensive Drug Combinations On Blood Pressure and Arterial StiffnessDocument6 pagesEffects of Different Antihypertensive Drug Combinations On Blood Pressure and Arterial StiffnessbimaNo ratings yet
- Risk Factors For Hypertension and Its Complications Case Control StudyDocument4 pagesRisk Factors For Hypertension and Its Complications Case Control StudyutarinuNo ratings yet
- Jurnal Internasional 5 HipertensiDocument9 pagesJurnal Internasional 5 HipertensiMutiara Anak NegeriNo ratings yet
- 23 - KMB - Luddiana Husen - Id.enDocument6 pages23 - KMB - Luddiana Husen - Id.enLuddiana HusenNo ratings yet
- 23 - KMB - Luddiana Husen - Id.enDocument6 pages23 - KMB - Luddiana Husen - Id.enLuddiana HusenNo ratings yet
- Jurnal Int 2Document14 pagesJurnal Int 2rike aprilianaNo ratings yet
- Beckett 2008Document12 pagesBeckett 2008Cifa Maurer ParinussaNo ratings yet
- Jurnal 1Document14 pagesJurnal 1Ira TryNo ratings yet
- Journal Pone 0172745 PDFDocument13 pagesJournal Pone 0172745 PDFselamat parminNo ratings yet
- STR6Document12 pagesSTR6ali akbar meccaNo ratings yet
- Study of Drug Use in Essential Hypertension and Their ComplianceDocument13 pagesStudy of Drug Use in Essential Hypertension and Their ComplianceRachmat MuhammadNo ratings yet
- Nacl Untuk HipertensiDocument7 pagesNacl Untuk HipertensiyulitaNo ratings yet
- Correa 2018Document52 pagesCorrea 2018Esteban Matus MuñozNo ratings yet
- A Literature Review On Hypertensive Crisis: European Journal of Pharmaceutical and Medical ResearchDocument6 pagesA Literature Review On Hypertensive Crisis: European Journal of Pharmaceutical and Medical ResearchCindy MaslagNo ratings yet
- JCH-22-663Document10 pagesJCH-22-663fani rudiyantiNo ratings yet
- Litrev Bu2Document8 pagesLitrev Bu2Deudeu Durotun NafisahNo ratings yet
- Epidemiology of The Metabolic Syndrome in Hungary: Public HealthDocument7 pagesEpidemiology of The Metabolic Syndrome in Hungary: Public Healthadi suputraNo ratings yet
- Characteristics of hypertension patients in Ternate, IndonesiaDocument7 pagesCharacteristics of hypertension patients in Ternate, Indonesiatutorialll enam duaNo ratings yet
- Thesis Hypertension PDFDocument7 pagesThesis Hypertension PDFnelowow1vut3100% (2)
- 10 1016@j CCL 2016 12 005 PDFDocument16 pages10 1016@j CCL 2016 12 005 PDFjomoralesr91No ratings yet
- Adhrence 1Document9 pagesAdhrence 1nabilahbilqisNo ratings yet
- Arterial Hypertension and Aortic Valve Stenosis: Shedding Light On A Common "Liaison"Document6 pagesArterial Hypertension and Aortic Valve Stenosis: Shedding Light On A Common "Liaison"Adriana VasilicaNo ratings yet
- Management of Hypertensive Elderly in Clinical Dentistry: Patcharaphol Samnieng, Kantapong PloydanaiDocument9 pagesManagement of Hypertensive Elderly in Clinical Dentistry: Patcharaphol Samnieng, Kantapong PloydanaiSatya AsatyaNo ratings yet
- Hypertension ThesisDocument31 pagesHypertension ThesisNavin AdhikariNo ratings yet
- 23 - KMB - Luddiana Husen - Mini Review - Id.enDocument6 pages23 - KMB - Luddiana Husen - Mini Review - Id.enLuddiana HusenNo ratings yet
- Epih 40 E2018020Document9 pagesEpih 40 E2018020Toth CsongorNo ratings yet
- Levy2012 PDFDocument9 pagesLevy2012 PDFDianNo ratings yet
- Subclinical Hypertensive Heart Disease in Black Patients With Elevated Blood Pressure in An Inner-City Emergency DepartmentDocument9 pagesSubclinical Hypertensive Heart Disease in Black Patients With Elevated Blood Pressure in An Inner-City Emergency DepartmentDianNo ratings yet
- Hypertension Control, Apparent Treatment Resistance, and Outcomes in The Elderly Population With Chronic Kidney DiseaseDocument12 pagesHypertension Control, Apparent Treatment Resistance, and Outcomes in The Elderly Population With Chronic Kidney Diseasetika_876267153No ratings yet
- Fibrilação Atrial e AVC IsquêmicoDocument9 pagesFibrilação Atrial e AVC IsquêmicoCalouro Carlos André SoaresNo ratings yet
- CKD HT 3Document8 pagesCKD HT 3Peer TutorNo ratings yet
- Initiation of Antihypertensive Therapy Based On.480Document2 pagesInitiation of Antihypertensive Therapy Based On.480jackie funtanillaNo ratings yet
- Manejo Hta Unidad Cuidados Criticos PediátricoDocument9 pagesManejo Hta Unidad Cuidados Criticos PediátricoCatalina Cruz NunjaNo ratings yet
- Treatment of HypertensionDocument23 pagesTreatment of HypertensionRABIATUL ADAWIYAHNo ratings yet
- Hypertension Prevention and Control Strategies Focus on Team-Based CareDocument30 pagesHypertension Prevention and Control Strategies Focus on Team-Based Care2130020043 RIDHO INAYAHNo ratings yet
- Medication Adherence and Blood Pressure Control Among Hypertensive Patients With Coexisting Long-Term Conditions in Primary Care SettingsDocument10 pagesMedication Adherence and Blood Pressure Control Among Hypertensive Patients With Coexisting Long-Term Conditions in Primary Care SettingsmadhurocksktmNo ratings yet
- Nota 2Document8 pagesNota 2Hector GuzmanNo ratings yet
- Risk Factors of Hypertension in The ElderlyDocument7 pagesRisk Factors of Hypertension in The ElderlyMashar yonoNo ratings yet
- The Prevalence of Resistant Hypertension Among TypDocument7 pagesThe Prevalence of Resistant Hypertension Among TypProfessor Kamel AjlouniNo ratings yet
- Long Ter OutcomeDocument7 pagesLong Ter OutcomeTeodor BicaNo ratings yet
- Synopsis 142Document8 pagesSynopsis 142AneesUrRahmanNo ratings yet
- HTN Guidelines 1Document12 pagesHTN Guidelines 1lakshminivas PingaliNo ratings yet
- Hypertension in Adolescents and Young Adults Referred To A Tertiary Hypertension Clinic in Cape Town, South AfricaDocument5 pagesHypertension in Adolescents and Young Adults Referred To A Tertiary Hypertension Clinic in Cape Town, South AfricahanifahNo ratings yet
- Challenges in The Management of Hypertension in Asia: Bernard Man Yung Cheung and Tommy Tsang CheungDocument2 pagesChallenges in The Management of Hypertension in Asia: Bernard Man Yung Cheung and Tommy Tsang CheungHolly JonesNo ratings yet
- Gupea 2077 35191 1Document81 pagesGupea 2077 35191 1pearl ikebuakuNo ratings yet
- Preventive Medicine: Xiaolei Xie, Tianhua He, Jian Kang, David S. Siscovick, Yan Li, José A. PagánDocument5 pagesPreventive Medicine: Xiaolei Xie, Tianhua He, Jian Kang, David S. Siscovick, Yan Li, José A. PagánDewiNo ratings yet
- Secondary HypertensionFrom EverandSecondary HypertensionAlberto MorgantiNo ratings yet
- Hypertension in Children and Adolescents: New PerspectivesFrom EverandHypertension in Children and Adolescents: New PerspectivesEmpar LurbeNo ratings yet
- Selvarajah 2013Document7 pagesSelvarajah 2013Sol LakosNo ratings yet
- Danchin 2008Document10 pagesDanchin 2008Sol LakosNo ratings yet
- DOCUMENT Early Symptoms of Schizophrenia: A Study of Age and Gender DifferencesDocument10 pagesDOCUMENT Early Symptoms of Schizophrenia: A Study of Age and Gender DifferencesSol LakosNo ratings yet
- Labinaz 2019Document7 pagesLabinaz 2019Sol LakosNo ratings yet
- Pelletier 2014Document8 pagesPelletier 2014Sol LakosNo ratings yet
- Lancet 2016 Valvulopatias Estenosis AórticaDocument12 pagesLancet 2016 Valvulopatias Estenosis AórticaSol LakosNo ratings yet
- Oberlander 2016Document14 pagesOberlander 2016Sol LakosNo ratings yet
- Implementation of The NIH Sex-Inclusion Policy: Attitudes and Opinions of Study Section MembersDocument8 pagesImplementation of The NIH Sex-Inclusion Policy: Attitudes and Opinions of Study Section MembersBL OeiNo ratings yet
- BMJ Insuficiencia Mitral y Estenosis Ao en EmbarazoDocument4 pagesBMJ Insuficiencia Mitral y Estenosis Ao en EmbarazoSol LakosNo ratings yet
- Westenbroek 2004Document6 pagesWestenbroek 2004Sol LakosNo ratings yet
- 1 s2.0 S0140673620326581 MainDocument14 pages1 s2.0 S0140673620326581 MainSol LakosNo ratings yet
- Sympathetic Nervous Tone Limits The Development of Myeloid-Derived Suppressor CellsDocument13 pagesSympathetic Nervous Tone Limits The Development of Myeloid-Derived Suppressor CellsSol LakosNo ratings yet
- Sciimmunol Abe9950Document18 pagesSciimmunol Abe9950Sol LakosNo ratings yet
- Heart 2018 Valvulopatias Estenosis Aortica Cirugia EHDocument11 pagesHeart 2018 Valvulopatias Estenosis Aortica Cirugia EHSol LakosNo ratings yet
- IGCSE Chemistry NotesDocument70 pagesIGCSE Chemistry NotesKim Seng OnnNo ratings yet
- s41467 019 13177 3 PDFDocument13 pagess41467 019 13177 3 PDFFelipe Douglas de PaulaNo ratings yet
- The Spread of MisinformationDocument2 pagesThe Spread of MisinformationSol LakosNo ratings yet
- Question Bank For Pharmacology - WJP AnsweredDocument55 pagesQuestion Bank For Pharmacology - WJP AnsweredGeorge MoshiNo ratings yet
- CPR PresentationDocument22 pagesCPR PresentationAlan HabalNo ratings yet
- From Snake Venom To ACE Inhibitor The Discovery and Rise of CaptoprilDocument4 pagesFrom Snake Venom To ACE Inhibitor The Discovery and Rise of CaptoprilEmy Noviana SandyNo ratings yet
- Self Asessment: Nama Karyawan Pendidikan Sertifikasi PenempatanDocument8 pagesSelf Asessment: Nama Karyawan Pendidikan Sertifikasi PenempatanRora Dhe OlalaNo ratings yet
- Tif30Document49 pagesTif30HCX dghhqNo ratings yet
- KBA Dyslipidemia 2023 Oct 31 TueDocument36 pagesKBA Dyslipidemia 2023 Oct 31 TueKamran B AliNo ratings yet
- Assessment and Management of Heart Failure in Patients With Chronic Kidney DiseaseDocument16 pagesAssessment and Management of Heart Failure in Patients With Chronic Kidney DiseaseElian BenjaminNo ratings yet
- Iabp 3Document10 pagesIabp 3Diana Marcela Franco SanchezNo ratings yet
- Brain Natriuretic PeptideDocument8 pagesBrain Natriuretic PeptidegunawanNo ratings yet
- Ten Factors That Can Temporarily Elevate Blood Pressure ReadingsDocument2 pagesTen Factors That Can Temporarily Elevate Blood Pressure Readingsamanuel melakuNo ratings yet
- Intensive Care Unit (ICU) Manual 2020-21Document146 pagesIntensive Care Unit (ICU) Manual 2020-21anithaNo ratings yet
- 03 How To Wean A CABG PatientDocument2 pages03 How To Wean A CABG PatientChing BanagNo ratings yet
- Effect of Exercise and Posture On Blood PressureDocument19 pagesEffect of Exercise and Posture On Blood PressureSreedeep TejaNo ratings yet
- Heparin Prevents Blood Clots & May Inhibit TumorsDocument2 pagesHeparin Prevents Blood Clots & May Inhibit TumorsUzumaki KNo ratings yet
- PRMRJDocument326 pagesPRMRJfiling rsstNo ratings yet
- Kewenangan Klinis SP - JPDocument3 pagesKewenangan Klinis SP - JPVania Lystia TantraNo ratings yet
- Determination of Arterial Compliance Using Blood Pressure Waveform Analysis With The CR-2000 SystemDocument7 pagesDetermination of Arterial Compliance Using Blood Pressure Waveform Analysis With The CR-2000 SystemSofiene MansouriNo ratings yet
- Anatomy and Physiology of Cardiovascular SystemDocument2 pagesAnatomy and Physiology of Cardiovascular SystemKezzel Grace MaquillaNo ratings yet
- Cardiac Sequential AnalysisDocument34 pagesCardiac Sequential AnalysisMochamad Rizky HendiperdanaNo ratings yet
- Quick Guide To TTEDocument16 pagesQuick Guide To TTEwen1190No ratings yet
- Pulmonary Heart DiseaseDocument379 pagesPulmonary Heart DiseaseJose CastellonNo ratings yet
- LIFEPAK 1000 Users Manual 2014Document86 pagesLIFEPAK 1000 Users Manual 2014Forum PompieriiNo ratings yet
- Cardiovascular SystemDocument23 pagesCardiovascular Systemapi-247077900No ratings yet
- Diagnosis Dan Tatalaksana Tromboangitis Obliterans/penyakit Buerger Dengan Fenomena RaynaudDocument4 pagesDiagnosis Dan Tatalaksana Tromboangitis Obliterans/penyakit Buerger Dengan Fenomena RaynaudHendra Putra SanjayaNo ratings yet
- HCM 2020 GuidelinesDocument81 pagesHCM 2020 Guidelinesdipak patadeNo ratings yet
- ICD Code Patient Data ReportDocument2 pagesICD Code Patient Data ReportpkmmenurNo ratings yet
- Ecg PDFDocument38 pagesEcg PDFKeerthana BalachandiranNo ratings yet