Professional Documents
Culture Documents
Paediatrica Indonesiana: Checklist For Autism in Toddlers: A Diagnostic Study
Uploaded by
Nurul MillatiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Paediatrica Indonesiana: Checklist For Autism in Toddlers: A Diagnostic Study
Uploaded by
Nurul MillatiCopyright:
Available Formats
Paediatrica Indonesiana
p-ISSN 0030-9311; e-ISSN 2338-476X; Vol.60, No.3(2020). p.160-6; doi: http://dx.doi.org/10.14238/pi60.3.2020.160-6
Original Article
Validation of the Indonesian Version of Modified
Checklist for Autism in Toddlers: a diagnostic study
Hendra Salim1, Soetjiningsih1, I Gusti Ayu Trisna Windiani1, I Gede Raka Widiana2
A
Abstract utism is a severe disorder of development,
Background Autism is a developmental disorder for which affecting children below 36 months of age.
early detection in toddlers is recommended because of its in- Autism often goes undetected in toddlers,
creased prevalence. The Modified Checklist for Autism in Toddlers
(M-CHAT) is an easy-to-interprete tool that can be filled out by especially in urban children with low
parents. It has been translated into the Indonesian language but socio-economic status.1,2 To our knowledge, there
needs to be validated. have been no studies reporting autism prevalence in
Objective To evaluate the diagnostic validity of the Indonesian Indonesia. A Bandung (West Java) study reported
version of M-CHAT in detection of autism spectrum disorder
in Indonesia. that 20–30% of children below five years of age have
Methods A diagnostic study was conducted at Sanglah Hospi- symptoms of delayed development.3 According to a
tal, Denpasar, Bali, from March 2011 to August 2013. Pediatric 2009 report from the Indonesian Autism Foundation,
outpatients aged 18 to 48 months were included. The Indonesian
version of the M-CHAT tool was filled by parents. Autism assess- there were more than 102 therapeutic centers and 13
ment was done according to the Diagnostic and Statistical Manual schools for autism in Indonesia.4
of Mental Disorders, 4th edition (DSM-IV-TR). The assessment From 2006, the American Academy of Pediatrics
results were analyzed with the MedCalc program software, in
(AAP) has recommended using the algorithm for de-
several steps: (i) reliability of M-CHAT; (ii) description, distri-
bution, and proportion to determine the characteristics of the velopmental surveillance and screening for early iden-
subjects of research; and (iii) validity of M-CHAT compared to tification of autism spectrum disorder (ASD), because
the gold standard DSM-IV-TR by a receiver operating charac- it allows early intervention, etiologic investigation, and
teristic curve and several area under the curve cut-off points, in
order to assess the sensitivity, specificity, positive predictive value, counseling regarding the risk of recurrence.5 Of the
negative predictive value, and positive and negative likelihood ASD screening tools, the Checklist for Autism in Toddlers
ratio, accompanied by the 95% confidence interval of each value.
Results The Indonesian version of M-CHAT in toddlers had
82.35% sensitivity and 89.68% specificity, using the cut-off point
of more than 6 failed questions.
From the Department of Child Health1 and Department of Internal
Conclusion The Indonesian version M-CHAT translated by Medicine2. Universitas Udayana Medical School/Sanglah Hospital,
Soetjiningsih has optimal diagnostic validity for detection of au- Denpasar, Bali, Indonesia.
tism in toddlers. [Paediatr Indones. 2020;60:160-6; doi: http://
dx.doi.org/10.14238/pi60.3.2020.160-6]. Corresponding author: Hendra Salim, Department of Child Health,
Universitas Udayana Medical School/Sanglah Hospital, Jalan Pulau Nias
80114, Denpasar, Bali, Indonesia. Telp. +62-361-244038; Fax. +62-361-
244038; Email: misionarispelayanan@gmail.com.
Keywords: M-CHAT; autism; screening; validity
Submitted September 25, 2019. Accepted June 16, 2020.
160 • Paediatr Indones, Vol. 60, No. 3, May 2020
Hendra Salim et al.: Validation of the Indonesian Version of Modified Checklist for Autism in Toddlers: a diagnostic study
(CHAT) was designed specifically as a level 1 screening cultural adaptation, and a short pilot study to obtain
tool. It is available at no cost to practitioners for use in the final Indonesian version of M-CHAT to be used
primary care and only requires 5 minutes to complete in Indonesia; (ii) the reliability study; and (iii) the
the questionnaire. Because of its low sensitivity, Robins validity study.
modified the CHAT to the Modified Checklist for Autism The M-CHAT questionnaire was translated
in Toddlers (M-CHAT) to better identify children at risk into the Indonesian language by Soetjiningsih
for any ASD.5 The M-CHAT is more cost- and time- with guidance that, rather than being literal, the
efficient than other tools. It only requires about 5-10 translation should had semantic, linguistic, and
minutes for parents to complete the survey, with 23 yes/ cultural equivalence. The resulting version was then
no items that are easy to understand. The M-CHAT back-translated by a native English speaker who was
can be used to screen children aged 18 to 48 months. bilingual, and sent to the original authors to compare
In the United States, community- and clinical-based it to the original M-CHAT. After several exchanges of
studies on M-CHAT reported 85% of sensitivity and opinion with the original author and making certain
93-100% of specificity.1,5-7 amendments, the Indonesian version of the M-CHAT
The M-CHAT was translated into the Indonesian questionnaire was approved by the original author.
language by Soetjiningsih, with permission from the The Indonesian language M-CHAT questionnaire
author. This Indonesian version of M-CHAT has consists of 6 critical questions and 17 other questions,
been widely used in Indonesia, but M-CHAT use total 23 questions.
and validity has not been reported. Hence, this study The reliability study of M-CHAT was done to
was conducted to evaluate the diagnostic validity of evaluate the variability of the instrument and observer
the Indonesian version of M-CHAT for detection of (parents). Our reliability study included 15 parents
ASD in Indonesia. from the Child Growth and Development Clinic of
Sanglah Hospital without inclusion nor exclusion
criteria. The Indonesian version of M-CHAT was
Methods administered to the parents twice, at the first visit
and at a visit 1 month later.
This cross-sectional study was conducted in the The reliability test for the Indonesian version
Child Growth and Development Clinic of Sanglah of M-CHAT was done by calculating the coefficient
Hospital, Denpasar, Bali, from March 2011 to of test-retest (intraobserver) reliability, in which 15
August 2013. Children aged 18 to 48 months whose parents participated. This study used Bland-Altman
parents brought them to the clinic and agreed to curve as parameter of reliability test.9
participate were included in this study. We excluded Parents were accompanied by a resident familiar
children with global inability in language expression with the content of the questions in the Indonesian
or verbal communication (because of hearing loss or M-CHAT, so that they could request an explanation
palatoschisis), and those with global motor deficits if needed. The authors were not directly involved in
or cognitive delays such that they could not pass the this aspect of the study in order to remain blinded to
cognitive/developmental assessment (for example, the parents’ answers. Completed questionnaire was
cerebral palsy, hydrocephalus, or other severe collected and Bland-Altman analysis was carried out
congenital deformities). (M-CHAT1). The first result then will be compared
Estimation of sample size was calculated by with the result of second analysis which was done one
a single proportion sample method, with P=80%, month later (M-CHAT2).
a=0.05, Za=1.96, d=30%, and the 4.8% proportion of Children of both genders aged 18-48 months
children with ASD aged 18 to 48 months who came to who visited our clinic with parents were screened
the Child Growth and Development Clinic of Sanglah for inclusion. Subjects’ parents provided written
Hospital by 2009.8 A total of 143 subjects, the minimum informed consent. All subjects were evaluated by the
required sample size, were included in this study. authors using the Diagnostic and Statistical Manual of
This study was undertaken in the following Mental Disorders, 4th edition (DSM-IV-TR) criteria
three phases: (i) translation, back translation, from the Centers for Disease Control and Prevention
Paediatr Indones, Vol. 60, No. 3, May 2020 • 161
Hendra Salim et al.: Validation of the Indonesian Version of Modified Checklist for Autism in Toddlers: a diagnostic study
(CDC) methodology. The ASD cases were identified
and systematically defined using the DSM-IV-TR
criteria from CDC. The authors were blinded to the
M-CHAT results. The results of the M-CHAT and
DSM-IV-TR assessments were merged by way of the
research subject identity forms.
All collected data were entered and analyzed
by the MedCalc program software, in several steps: (i)
reliability of M-CHAT; (ii) description, distribution, and
proportion to determine the characteristics of the study
subjects; and (iii) validity of M-CHAT compared to
the gold standard DSM-IV-TR by a receiver operating
characteristic (ROC) curve and several area under
the curve (AUC) cut-off points, in order to assess the
sensitivity, specificity, positive predictive value (PPV),
negative predictive value (NPV), and positive and Figure 1. Bland-Altman curve
negative likelihood ratio (LR), accompanied by the
95% confidence interval of each value.
The study was approved by the Medical and with only 5.6% malnourished. Most fathers (74.8%)
Health Research Ethics Committee of Universitas did not have a college education, nor did mothers
Udayana Medical School/Sanglah Hospital, Denpasar. (80.4%). Only 19.6% of mothers completed university.
Using the DSM-IV-TR, we identified 17 (11.9%)
children with autism.
Results The cut-off M-CHAT score was determined by
the intersection between sensitivity and specificity for
A total of 175 children were screened for this study. We the AUC and the coordinates of the ROC curve.10,11
excluded 32 children with global developmental delays. The AUC values evaluated were from 50%, the worst
A Bland-Altman plot (Figure 1) revealed the systematic rating, up to 100%, the best value.11 The ROC curves
distinction between measurements and identify possible showed that the M-CHAT score of the study (Figures
outliers. Mean difference was the estimation of bias 2 and 3), had a good diagnostic value because the
and standard deviation from difference of random curve was far above the 50% line and closer to 100%.
fluctuations around the mean. This study was clinically The AUC were 91.2% (95%CI 85.2% to 95.3%) for
important because the difference was within the range M-CHAT critical questions and 93.7% (95%CI 88.3%
of SD 1.96. The P value obtained from this study was to 97.1%) for M-CHAT total questions (P<0.001).
<0.001 with 95%CI -0.725 to 0.725 (SD 1.31). Blant- The cut-off point was established clinically
Altman plot determined whether language in the and statistically in accordance with the clinical
Bahasa MCHAT questionnaire represented language expectations and interests,11 by the ROC curve
that intelligible by respondens (parents). If the plot coordinates. The diagnostic value for the critical
was between +1.96 and -1.96, the study could be items of M-CHAT at various cut-off points revealed
continued. If the plot was scattered beyond the SD 1.96, that the best validity was achieved if failure occurred
the Bahasa in the MCHAT translated quiesionnaire on more than 1 question of the six critical questions
should be improved first so it can be equally understood on the Indonesian version of M-CHAT (sensitivity
by all the respondens. 82.35% and sensitivity 91.27%).
The characteristics of subjects are presented in The AUC revealed that the best validity for the
Table 1. Of 143 study subjects, the median age was total M-CHAT questions was if failure occurred on 5
33 months, ranging from 18-48 months. More boys or more out of 23 questions (sensitivity 88.24% and
participated than girls, with a ratio of 1.9:1. Subjects’ specificity 85.71%). The diagnostic values for the
nutritional status was mostly well-nourished (94.4%), critical and total items of the Indonesian version of
162 • Paediatr Indones, Vol. 60, No. 3, May 2020
Hendra Salim et al.: Validation of the Indonesian Version of Modified Checklist for Autism in Toddlers: a diagnostic study
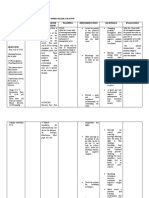
Table 1. Characteristics of subjects
Characteristics Autism (DSM-IV-TR) Total
(n = 17) (N = 143)
Sex, n (%)
Male 14 94 (65.7)
Female 3 49 (34.3)
Median age (range), months 38 (29 to 48) 33 (18 to
48)
Nutritional status, n (%)
Malnourished 1 8 (5.6)
Well-nourished 15 127 (88.8)
Overweight 1 8 (5.6)
Maternal education, n (%)
Elementary 0 13 (9.1)
Junior high 5 27 (18.9)
Senior high 10 75 (52.4)
University 2 28 (19.6)
Paternal education, n (%)
Elementary 0 14 (9.8)
Junior high 4 26 (18.2)
Senior high 10 67 (46.8)
University 3 36 (25.2)
Figure 2. ROC curve and AUC cut-off for critical questions of M-CHAT
Figure 3. ROC curve and AUC cut-off for total questions of M-CHAT
Paediatr Indones, Vol. 60, No. 3, May 2020 • 163
Hendra Salim et al.: Validation of the Indonesian Version of Modified Checklist for Autism in Toddlers: a diagnostic study
M-CHAT at various cut-off points are shown in Table 3.37) in children aged 7-12 years.15 A study conducted
2 and Table 3, respectively. two stages of community-based studies in Spain and
The value of the likelihood ratio is varying from reported prevalences of 0.92% and 0.29% of children
zero to infinity. A strong positive result of diagnostic aged 18-36 months.16
test provides positive LR >6, while a strong negative We found more autism in boys than in girls, with
result will gives the negative LR <0.2.10,12 Table 3 ratio of 4.7:1. Our finding was similar to that of a 2008
shows that at the >6 item failure cut-off point with surveillance study in the US which reported a ratio
82.35% sensitivity and 89.68% specificity, the positive of 5:1.14 Eldin et al.17 studied children aged 18 to 124
LR was 7.98 and negative LR was 0.2, which fulfilled months in 9 Arabic countries, and reported 84.4%
the above criterion. boys and 15.6% girls in their autism subjects (5.4:1).
Table 2. Diagnostic values of critical M-CHAT items compared to the gold standard at various cut-off points
Cut-off Sensitivity, % Specifity , % PPV, % NPV, % Positive LR, % Negative LR, %
(95%CI) (95%CI) (95%CI) (95%CI) (95%CI) (95%CI)
>0 94.12 70.63 30.2 98.9 3.21 0.083
(71.3 to 99.9) (61.9 to 78.4) (18.2 to 44.5) (94.0 to 100) (2.4 to 4.3) (0.01 to 0.6)
>1 82.35 91.27 56.0 97.5 9.43 0.19
(56.6 to 96.2) (84.9 to 95.6) (34.9 to 75.6) (92.7 to 99.5) (5.1 to 17.3) (0.07 to 0.5)
>2 47.06 96.83 66.7 93.1 14.82 0.55
(23.0 to 72.2) (92.1 to 99.1) (34.9 to 90.1) (87.4 to 96.8) (5.0 to 44.0) (0.3 to 0.9)
Table 3. Diagnostic values of total M-CHAT items compared to the gold standard at various cut-off points
Cut-off Sensitivity, % Specifity , % PPV, % NPV, % Positive LR, % Negative LR, %
(95%CI) (95%CI) (95%CI) (95%CI) (95%CI) (95%CI)
>3 94.12 78.57 37.2 99.0 4.39 0.0075
(71.3 to 99.9) (70.4 to 85.4) (23.0 to 53.3) (94.6 to 100) (3.1 to 6.3) (0.01 to 0.5)
>4 88.24 85.71 45.5 98.2 6.18 0.14
(63.6 to 98.5) (78.4 to 91.3) (28.1 to 63.6) (93.6 to 99.8) (3.9 to 9.8) (0.04 to 0.5)
>5 82.35 88.10 48.3 97.4 6.92 0.2
(56.6 to 96.2) (81.1 to 93.2) (29.4 to 67.5) (92.5 to 99.5) (4.1 to 11.7) (0.07 to 0.6)
>6 82.35 89.68 51.9 97.4 7.98 0.2
(56.6 to 96.2) (83.0 to 94.4) (31.6 to 71.7) (92.6 to 99.5) (4.6 to 14.0) (0.07 to 0.6)
>7 64.71 94.44 61.1 95.2 11.65 0.37
(38.3 to 85.8) (88.9 to 97.7) (35.7 to 82.7) (89.8 to 98.2) (5.2 to 25.9) (0.2 to 0.7)
Discussion The best age for autism screening in children
is still debated. The AAP recommended autism
The autism prevalence at the Child Growth and screening for all children aged 18 to 24 months.18
Development Clinic, Sanglah Hospital, Bali, was Firstly, M-CHAT was used to screen autism for
9.7% for children aged 18-48 months. After excluding children aged 16 to 30 months. Robins19 included
children with global delayed development, the 4,797 children aged 14 to <27 months in her study.
prevalence rose to 11.9%. In a population-based study, Also, a Thai study included 48 children aged 18 to 36
a previous study reported a prevalence of 2.66%.5 months.20 In addition, another study included 18,989
A previous study estimated an ASD prevalence of children aged 16 to 30 months in their study.18 Several
8.5 per 1,000 children aged 3 to 5 years in the United longitudinal studies screened children at an early age,
States.13 Research on the 14 sites in the United States then reevaluated them at 2 to 4 years old. The authors
revealed a prevalence of 11.3 per 1,000 children aged concluded that M-CHAT validity was high, although
8 years.14 A community-based study in South Korea the children had reached >30 months of age.19
noted an ASD prevalence of 2.64% (95%CI 1.91 to The ROC curve for M-CHAT showed the
164 • Paediatr Indones, Vol. 60, No. 3, May 2020
Hendra Salim et al.: Validation of the Indonesian Version of Modified Checklist for Autism in Toddlers: a diagnostic study
best sensitivity when failing seven or more items of Screening instruments need high sensitivity to
M-CHAT, similar to results from previous study.5 exclude a disease diagnosis for normal results. For
However, another study reported 87% sensitivity and conditions with a low prevalence, a test with high
94% specificity for the Thai language M-CHAT with specificity is more important than one with high
failure criteria cut-off of 8 or more questions.20 sensitivity.10 Using a cut-off of >6 items of the total
The earlier study found 85 to 87% of sensitiv- M-CHAT items, specificity was good at 89.68%.
ity and 93 to 99% of specificity, with 80% positive The specificity was higher than sensitivity (Table 3),
predictive value and 99% negative predictive value. indicating that the Indonesian version of M-CHAT
Another study resulted in a 95-99% sensitivity and is a suitable screening tool for autism.
95-99% specificity.21 Aakre22 noted that the M- The pre-test odds of this study were calculated
CHAT has been available in Spain, Turkey, China from probability divided with (1-probability), resulting
and Japan. 0.135. The post-test odds is the multiplication value
The Spanish M-CHAT had good sensitivity of pretest odds with positive LR, i.e. 1.078. Thus, the
(100%), specificity (98%), and NPV (100%), as well as post-test probability according to Bayes theory could
moderate PPV (35%) if failure occurred on more than be calculated, i.e., the post-test odds divided with
1 question of critical question or more than 2 question (1+post-test odds), amounting to 51.87%.
of total question.16 The Arabic M-CHAT had 86% The limitations of our study was that we did
sensitivity, 80% specificity, and good PPV (88%).17 not perform CHAT evaluation on the subjects which
In addition, a study modified the Chinese language suspected with the M-CHAT, as some other studies
CHAT-23 and M-CHAT questions into a new version did, we directly performing DSM-IV-TR on the first
of 15 questions, with 100% sensitivity and 96.5% visit. In addition, this study was not community based,
specificity if failing of 5 or 6 of 15 questions.23 We so the community-based autism prevalence remains
used the Indonesian version of M-CHAT translated unknown. This research needs to be continued with
by Soetjiningsih and found 82.35% sensitivity (95%CI a larger sample size for a higher level of precision and
56.6 to 96.2%) and 89.68% specificity (95%CI 83.0 to narrower validity.
94.4%) if failing more than 6 of 23 questions (Table 3). In conclusion, the Indonesian version of
The likelihood ratio is a semi-quantitative M-CHAT translated by Soetjiningsih is a suitable
measurement of assessing a diagnostic test that screening tool for autism. It has optimal diagnostic
reveals how big a diagnostic procedure will change validity in detection of autism for failure criteria of
the possibility of a disease that is calculated from more than 6 of 23 questions, with 82.35% sensitivity
sensitivity and specificity of a diagnostic test.12 This and 89.68% specificity. Of 6 critical M-CHAT
ratio expresses the magnitude of the likelihood that questions, a failure of two or more had 82.35%
ill patients would have a certain diagnostic test result sensitivity and 91.27% specificity. As such, the tool
divided by the possibility of well patients having can be applied to children aged 18 to 48 months
the same test results.10 The positive LR >6 and whose parents fill the form directly. If the result of
the negative LR <0.2 in a study indicates that the the screening reveals suspected autism, parents are
Indonesian M-CHAT is a good instrument because advised to seek expert opinion.
it can change the hypothesis against the probability
of disease of pre-test to post-test.12 Our LRs for a
cut-off of failing >6 items were 7.98 (95%CI 4.6 to Conflict of Interest
14.0) for positive LR and 0.2 (95%CI 0.07 to 0.6) for
negative LR. None declared.
Pre-test probability is the likelihood of a person
having a disease prior to diagnostic test, also defined
as the prevalence of the disease based on clinical and References
demographic characteristics.10 The prevalence of our
study was 9.7%. After excluding children with global 1. Johnson CP, Myers SM, American Academy of Pediatrics
developmental delay, the prevalence was 11.9%. Council on Children with Disabilities. Identification and
Paediatr Indones, Vol. 60, No. 3, May 2020 • 165
Hendra Salim et al.: Validation of the Indonesian Version of Modified Checklist for Autism in Toddlers: a diagnostic study
evaluation of children with autism spectrum disorders. 13. Kogan MD, Blumberg SJ, Schieve LA, Boyle CA, Perrin JM,
Pediatrics. 2007;120:1183–215. DOI: 10.1542/peds.2007- Ghandour RM, et al. Prevalence of parent-reported diagnosis
2361. of autism spectrum disorder among children in the US, 2007.
2. Volkmar F, Wiesner L. Autism and related disorders. In: Pediatrics. 2009;124:1395-403. DOI: 10.1542/peds.2009-
Carey WB, Crocker AC, Coleman WL, Elias ER, Feldman 1522.
HM, editors. Developmental-behavioral pediatrics. 4th ed. 14. Autism and Developmental Disabilities Monitoring Network
Philadelphia: Saunders Elsevier; 2009. p. 675-85. Surveillance Year 2008 Principal Investigators; Centers for
3. Alisjahbana EM. Asuhan dini tumbuh kembang anak. In: Disease Control and Prevention (CDC). Prevalence of autism
Siswanto MT, editor. Simposium penatalaksanaan mutakhir spectrum disorders - Autism and Developmental Disabilities
bidang Ilmu Kesehatan Anak untuk mencapai tumbuh Monitoring Network, 14 Sites, United States, 2008. MMWR
kembang optimal, 21-22 Juli 2000. Bandung: IDAI cabang Surveill Summ. 2012;61:1-19. PMID: 22456193.
Jawa Barat; 2000. p.34-53. 15. Kim YS, Leventhal BL, Koh YJ, Fombonne E, Laska E,
4. Yuwono J. Memahami anak autistik (Kajian teoritik dan Lim EC, et al. Prevalence of autism spectrum disorders in a
empirik). Bandung: Penerbit Alfabeta; 2009. p. 1-36. total population sample. Am J Psychiatry. 2011;168:904-12.
5. Robins DL, Fein D, Barton ML, Green JA. The modified DOI: 10.1176/appi.ajp.2011.10101532.
checklist for autism in toddlers: an initial study investigating 16. Canal-Bedia R, García-Primo P, Martín-Cilleros MV, Santos-
the early detection of autism and pervasive developmental Borbujo J, Guisuraga-Fernández Z, Herráez-García L, et al.
disorders. J Autism Dev Disord. 2001;31:131-44. DOI: Modified checklist for autism in toddlers: cross-cultural
10.1023/a:1010738829569. adaptation and validation in Spain. J Autism Dev Disord.
6. Dumont-Mathieu T, Fein D. Screening for autism in young 2011;41:1342-51. DOI: 10.1007/s10803-010-1163-z.
children: The Modified Checklist for Autism in Toddlers 17. Seif Eldin A, Habib D, Noufal A, Farrag S, Bazaid K, Al-
(M-CHAT) and other measures. Ment Retard Dev Disabil Sharbati M, et al. Use of M-CHAT for a multinational
Res Rev. 2005;11:253-62. DOI: 10.1002/mrdd.20072. screening of young children with autism in the Arab
7. Council on Children With Disabilities, Section on Countries. Int Rev Psychiatry. 2008;20:281-9. DOI:
Developmental Behavioral Pediatrics, Bright Futures Steering 10.1080/09540260801990324.
Committee; Medical Home Initiatives for Children with 18. Chlebowski C, Robins DL, Barton ML, Fein D. Large-scale
Special Needs Project Advisory Committee. Identifying use of the modified checklist for autism in low-risk toddlers.
infants and young children with developmental disorders Pediatrics. 2013;131:e1121-7. DOI: 10.1542/peds.2012-
in the medical home: an algorithm for developmental 1525.
surveillance and screening [published correction appears 19. Robins DL. Screening for autism spectrum disorders in
in Pediatrics. 118:1808-9]. Pediatrics. 2006;118:405-20. primary care settings. Autism. 2008;12:537-56. DOI:
DOI: 10.1542/peds.2006-1231. 10.1177/1362361308094502.
8. Lemeshow S, Hosmer DW Jr, Klar J, Lwanga SK. Adequacy 20. Pintunan P, Chonchaiya W, Pruksananonda C. Screening
of sample size in health studies. Chichester: World Health Thai children who have delayed language development with
Organization; 1990. p. 1-4. M-CHAT (a modified checklist for autism in toddlers) and
9. Bland JM, Altman DG. Statistical methods for assessing CHAT (checklist for autism in toddlers) Section B. Thai J
agreement between two methods of clinical measurement. Pediatr. 2009;48:221-9.
Lancet. 1986;8:307-10. PMID: 2868172. 21. Robins DL, Dumont-Mathieu TM. Early screening for autism
10. Pusponegoro HD, Wirya IGN. W, Pudjiadi AH, Bisanto spectrum disorders: update on the modified checklist for
J, Zulkarnain SZ. Uji diagnostik. In: Sastroasmoro S, autism in toddlers and other measures. J Dev Behav Pediatr.
Ismael S, editors. Dasar-dasar metodologi penelitian klinis. 2006;27:111-9. DOI: 10.1097/00004703-200604002-00009.
3rd ed. Jakarta: Sagung Seto; 2008. p. 193-216. 22. Aakre KJ, Paul K, Barry S. Developmental screening
11. Dahlan MS. Analisis Penelitian diagnostik. Jakarta: Sagung “preferred tool list” for children birth to three years.
Seto; 2009. p. 19-30. Burlington: Vermont Child Health Improvement Program;
12. Akobeng AK. Understanding diagnostic tests 2: likelihood 2010. p. 6-25.
ratios, pre- and post-test probabilities and their use 23. Tsai WC, Soong WT, Shyu YI. Toddler autism screening
in clinical practice. Acta Paediatr. 2007;96:487-91. questionnaire: development and potential clinical validity.
DOI: 10.1111/j.1651-2227.2006.00179.x. Autism. 2012;16:340-9. DOI: 10.1177/1362361311429694.
166 • Paediatr Indones, Vol. 60, No. 3, May 2020
You might also like
- Parent-Child Interaction Therapy with Toddlers: Improving Attachment and Emotion RegulationFrom EverandParent-Child Interaction Therapy with Toddlers: Improving Attachment and Emotion RegulationNo ratings yet
- Indonesian Modified Checklist For Autism in ToddleDocument5 pagesIndonesian Modified Checklist For Autism in ToddleAfifah AtsmaraNo ratings yet
- M Chat RDocument5 pagesM Chat RClarestaNo ratings yet
- 39-Article Text-77-1-10-202007Document7 pages39-Article Text-77-1-10-202007MageeNo ratings yet
- Two-Step Screening of The Modified Checklist For AutismDocument13 pagesTwo-Step Screening of The Modified Checklist For AutismKarel GuevaraNo ratings yet
- M Chat Tamil 2020Document8 pagesM Chat Tamil 2020Profe CatalinaNo ratings yet
- Communicationof AutismDocument4 pagesCommunicationof AutismDayna DamianiNo ratings yet
- OA UNBRAH 1260-4244-2-SM Rana Atikah, Sri Pandu UtamiDocument5 pagesOA UNBRAH 1260-4244-2-SM Rana Atikah, Sri Pandu UtamipanduutamidrgNo ratings yet
- Paper+21+ (2022 3 4) +The+Relationship+between+Family+Function+and+Emotional+Mental+ProblemsDocument6 pagesPaper+21+ (2022 3 4) +The+Relationship+between+Family+Function+and+Emotional+Mental+ProblemsWinonaNo ratings yet
- Paediatrica IndonesianaDocument8 pagesPaediatrica Indonesianafkia2013No ratings yet
- Validation of The Modified Checklist For Autism M CHAT RFDocument12 pagesValidation of The Modified Checklist For Autism M CHAT RFAmal AhamedNo ratings yet
- Modified Checklist For Autism in Toddlers Revised (MCHAT R/F) in An Urban Metropolitan Sample of Young Children in TurkeyDocument8 pagesModified Checklist For Autism in Toddlers Revised (MCHAT R/F) in An Urban Metropolitan Sample of Young Children in TurkeyProfe CatalinaNo ratings yet
- Priyanka K P Synopsis-1Document18 pagesPriyanka K P Synopsis-1RAJESHWARI PNo ratings yet
- Psychosocial Development Description of Preschool-Aged Children Esti Mediastini, Livana PH, Yazid BasthomiDocument6 pagesPsychosocial Development Description of Preschool-Aged Children Esti Mediastini, Livana PH, Yazid Basthomironi septiawanNo ratings yet
- Validation of The Modified Checklist For Autism in ToddlersDocument11 pagesValidation of The Modified Checklist For Autism in ToddlersFrancisca Aliaga ArellanoNo ratings yet
- Negotiating Knowledge - Parents Experience of The NeuropsychiatricDocument11 pagesNegotiating Knowledge - Parents Experience of The NeuropsychiatricKarel GuevaraNo ratings yet
- PMC7926898 AutismDocument13 pagesPMC7926898 AutismMageeNo ratings yet
- Research Article: Parental Perceptions of A Manchester Service For Autistic Spectrum DisordersDocument7 pagesResearch Article: Parental Perceptions of A Manchester Service For Autistic Spectrum DisordersElian Y. Sanchez-RiveraNo ratings yet
- Using The Modified ChecklistDocument8 pagesUsing The Modified ChecklistKarel GuevaraNo ratings yet
- Hodge 2018Document7 pagesHodge 2018Ines Arias PazNo ratings yet
- Pertumbuhan Dan Perkembangan Anak Usia 3-6 TahunDocument8 pagesPertumbuhan Dan Perkembangan Anak Usia 3-6 TahunSilvi EkaNo ratings yet
- Prevalence of Mental DisordersDocument6 pagesPrevalence of Mental DisordersKaram Ali ShahNo ratings yet
- AU StudiesDocument6 pagesAU StudiesHec ChavezNo ratings yet
- Achildwith Autism Spectrum DisorderDocument4 pagesAchildwith Autism Spectrum DisorderRamya SaravananNo ratings yet
- Barbaro & Dissanayake (2010) - SACS PDF FINAL PDFDocument10 pagesBarbaro & Dissanayake (2010) - SACS PDF FINAL PDFAnonymous 75M6uB3Ow100% (1)
- Ing GrisDocument6 pagesIng GrisDiny Nur FauziahNo ratings yet
- M Chat RDocument4 pagesM Chat RAsia CNo ratings yet
- PCST AsdDocument8 pagesPCST Asd409530315fjuNo ratings yet
- 480-Article Text-1063-1-10-20190131 PDFDocument13 pages480-Article Text-1063-1-10-20190131 PDFPrita AuliaNo ratings yet
- CitarDocument3 pagesCitarVictor NamurNo ratings yet
- Computational Methods To Measure Patterns of GazeDocument14 pagesComputational Methods To Measure Patterns of GazeDaniel NovakNo ratings yet
- Pelatihan Singkat Tentang Pengetahuan Dan Keterampilan Dalam Deteksi Dini Perkembangan Anak BalitaDocument7 pagesPelatihan Singkat Tentang Pengetahuan Dan Keterampilan Dalam Deteksi Dini Perkembangan Anak BalitaVanisya DtNo ratings yet
- Oral Hygiene Autis PDFDocument7 pagesOral Hygiene Autis PDFNoviyana Idrus DgmapatoNo ratings yet
- Nguyen 2019Document13 pagesNguyen 2019Jose Alonso Aguilar ValeraNo ratings yet
- A Study Exploring The Autism AwarenessDocument8 pagesA Study Exploring The Autism AwarenessAndrés Mauricio Diaz BenitezNo ratings yet
- Determinants of Stunting in Children Aged 12-59 MonthsDocument10 pagesDeterminants of Stunting in Children Aged 12-59 MonthsMichimichi 78No ratings yet
- Denver Developmental Screening Test - ValidityDocument7 pagesDenver Developmental Screening Test - Validitymodaberi1988No ratings yet
- Screening of 18-24-Month-Old Children For Autism in A Semi-Urban Community in Sri LankaDocument4 pagesScreening of 18-24-Month-Old Children For Autism in A Semi-Urban Community in Sri LankaJose Alonso Aguilar ValeraNo ratings yet
- Sobrecarga CuidadoresDocument6 pagesSobrecarga CuidadoresMARIA FRANCISCA VERGARA AGUILARNo ratings yet
- Jurnal Pengaruh Musik Mozart Terhadap Perubahan Perilaku Hiperaktif Anak Adhd Usia 7-12 TahunDocument16 pagesJurnal Pengaruh Musik Mozart Terhadap Perubahan Perilaku Hiperaktif Anak Adhd Usia 7-12 TahunroryputrisartikaNo ratings yet
- Smart Toothbrush As An Educational Medium To Improve The Toothbrushing Skills of Blind ChildrenDocument8 pagesSmart Toothbrush As An Educational Medium To Improve The Toothbrushing Skills of Blind ChildrenInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- tmp44FD TMPDocument11 pagestmp44FD TMPFrontiersNo ratings yet
- Bmjopen 2016 014730Document11 pagesBmjopen 2016 014730marinaNo ratings yet
- Etiological Study of Autism and Assessment by ISAA (Indian Scale For Assessment of Autism) For Diagnosis of Autism Spectrum Disorder in Children at Hi Tech Medical College and Hospital, BhubaneswarDocument2 pagesEtiological Study of Autism and Assessment by ISAA (Indian Scale For Assessment of Autism) For Diagnosis of Autism Spectrum Disorder in Children at Hi Tech Medical College and Hospital, BhubaneswarMageeNo ratings yet
- Pervasive Developmental Disorders in Preschool Children: Original ContributionDocument7 pagesPervasive Developmental Disorders in Preschool Children: Original ContributionrachelrojNo ratings yet
- Journal The Effect of Interactive Therapeutic PlayDocument9 pagesJournal The Effect of Interactive Therapeutic Playella bolotaNo ratings yet
- 2345-Article Text-7591-2-10-20200422aaDocument6 pages2345-Article Text-7591-2-10-20200422aaJihan AshariNo ratings yet
- EvidencesynthpaperfinalDocument9 pagesEvidencesynthpaperfinalapi-260120536No ratings yet
- Asd Jurnal 1Document12 pagesAsd Jurnal 1Fitria YusriNo ratings yet
- Assessment of Knowledge Regarding Oral Hygiene Among Parents of Pre-School Children Attending Pediatric Out Patient Department in Dhulikhel HospitalDocument6 pagesAssessment of Knowledge Regarding Oral Hygiene Among Parents of Pre-School Children Attending Pediatric Out Patient Department in Dhulikhel HospitalSri HariNo ratings yet
- 1 s2.0 S0021755720302138 MainDocument6 pages1 s2.0 S0021755720302138 MainMichele CezarNo ratings yet
- A Cross-Sectional Study of Behavioural Disorders in Children With Human Immunodeficiency Virus / Acquired Immuno Deficiency Syndrome Attending An Anti-Retroviral Therapy CentreDocument6 pagesA Cross-Sectional Study of Behavioural Disorders in Children With Human Immunodeficiency Virus / Acquired Immuno Deficiency Syndrome Attending An Anti-Retroviral Therapy CentreKumaravel KSNo ratings yet
- EvyDxen AutismoDocument9 pagesEvyDxen AutismocynthiaNo ratings yet
- Nygren 2012Document11 pagesNygren 2012Jose Alonso Aguilar ValeraNo ratings yet
- 354-Original Article-2609-1-10-20210108Document9 pages354-Original Article-2609-1-10-20210108Dwi Septia RiniNo ratings yet
- Prevalence, Severity and Associated Factors of Dental Caries in 3-6 Year Old Children - A Cross Sectional StudyDocument7 pagesPrevalence, Severity and Associated Factors of Dental Caries in 3-6 Year Old Children - A Cross Sectional StudysaravananspsNo ratings yet
- Paediatrica Indonesiana: Nicholas Calvin, Yetty RamliDocument6 pagesPaediatrica Indonesiana: Nicholas Calvin, Yetty RamliriloaddNo ratings yet
- Kajian Teori WHO Mengenai Jumlah Kunjungan Ibu Ke PosyanduDocument7 pagesKajian Teori WHO Mengenai Jumlah Kunjungan Ibu Ke PosyanduNatasha NaomiNo ratings yet
- Early Signs of Autism in Toddlers - A Follow Up StudyDocument10 pagesEarly Signs of Autism in Toddlers - A Follow Up StudyLu MoreiraNo ratings yet
- Cross Sectional Study On Language Assessment of Speech Delay in Children 0 To 6 YearsDocument4 pagesCross Sectional Study On Language Assessment of Speech Delay in Children 0 To 6 YearsIOSRjournalNo ratings yet
- A Proposed Model of Lifestyle Balance: Journal of Occupational Science April 2008Document10 pagesA Proposed Model of Lifestyle Balance: Journal of Occupational Science April 2008Nurul MillatiNo ratings yet
- Hakikat Manusia Sebagai Individu Dan Mah-DikonversiDocument8 pagesHakikat Manusia Sebagai Individu Dan Mah-DikonversiNurul MillatiNo ratings yet
- Role of Individuals in Conservation of Resources: June 2010Document9 pagesRole of Individuals in Conservation of Resources: June 2010Nurul MillatiNo ratings yet
- The Person As Individual and Social BeinDocument7 pagesThe Person As Individual and Social BeinNurul MillatiNo ratings yet
- Structure and Written Expression Pertemuan V KirimDocument21 pagesStructure and Written Expression Pertemuan V KirimNurul MillatiNo ratings yet
- EXERCISE 22: Each of The Following Sentences Contains An Inverted Subject and VerbDocument1 pageEXERCISE 22: Each of The Following Sentences Contains An Inverted Subject and VerbNurul MillatiNo ratings yet
- Exercise 25Document1 pageExercise 25Nurul MillatiNo ratings yet
- Natures Hidden Health MiracleDocument38 pagesNatures Hidden Health MiracleGorneau100% (2)
- Pa Tas Database (Conso)Document40 pagesPa Tas Database (Conso)AlbeldaArnaldoNo ratings yet
- 3 NURSING-CARE-PLAN FinaaalDocument7 pages3 NURSING-CARE-PLAN FinaaalSam PothNo ratings yet
- How To Prepare For ExamDocument4 pagesHow To Prepare For ExamJaspreet KaurNo ratings yet
- Glaucoma: by Tekia BuntynDocument18 pagesGlaucoma: by Tekia BuntynTekia BuntynNo ratings yet
- Hemorrhagic Disease of The NewbornDocument3 pagesHemorrhagic Disease of The NewbornDevi SuryandariNo ratings yet
- Regenerative Medicine From Protocol To PatientDocument257 pagesRegenerative Medicine From Protocol To PatientMandraludinNo ratings yet
- Jurnal Kesehatan Dr. SoebandiDocument6 pagesJurnal Kesehatan Dr. SoebandiHary BudiartoNo ratings yet
- Determining The Expected Competencies For OncologyDocument5 pagesDetermining The Expected Competencies For OncologyNaghib BogereNo ratings yet
- Graphic Organizer ExampleDocument1 pageGraphic Organizer Exampleapi-398530613No ratings yet
- Genito Urinary TraumaDocument16 pagesGenito Urinary TraumaAjibola OlamideNo ratings yet
- Icd X: Diagnose ICD Diagnosa ICDDocument33 pagesIcd X: Diagnose ICD Diagnosa ICDannisa statiraNo ratings yet
- Updates On Clinical Trials Evaluating The Regenerative Potential of Allogenic Mesenchymal Stem Cells in COVID-19Document11 pagesUpdates On Clinical Trials Evaluating The Regenerative Potential of Allogenic Mesenchymal Stem Cells in COVID-19diana.alyNo ratings yet
- Nursing Care Plans - Nursing Dia - Gulanick, MegDocument1,374 pagesNursing Care Plans - Nursing Dia - Gulanick, Megeric parl91% (22)
- 1translation and MedicineDocument202 pages1translation and MedicineMNNo ratings yet
- DYSRHYTHMIASDocument9 pagesDYSRHYTHMIASgudobenNo ratings yet
- The Effects of Exercise On The Nervous SystemDocument2 pagesThe Effects of Exercise On The Nervous SystemramadanNo ratings yet
- Refresher Course: Preboard Examination Nursing Practice III: Care of Clients With Physiologic and Psychosocial Alterations (Part A)Document9 pagesRefresher Course: Preboard Examination Nursing Practice III: Care of Clients With Physiologic and Psychosocial Alterations (Part A)Jastine Sabornido0% (1)
- Homoeopathy in Breast Cancer: AbstractsDocument5 pagesHomoeopathy in Breast Cancer: Abstractskathir_cNo ratings yet
- Las - Mapeh - Health Module 1Document5 pagesLas - Mapeh - Health Module 1Analiza SantosNo ratings yet
- Pediatric AnesthesiaDocument70 pagesPediatric AnesthesiaEliyan KhanimovNo ratings yet
- Orbino, Frances Anne N. 4th Rot FdarDocument2 pagesOrbino, Frances Anne N. 4th Rot FdarFrances OrbinoNo ratings yet
- Cps-Pg-Admission-2019 First Selection Round of Neet Eligible Candidates For The State of MaharashtraDocument93 pagesCps-Pg-Admission-2019 First Selection Round of Neet Eligible Candidates For The State of MaharashtrarohankananiNo ratings yet
- Effectiveness of The Bobath Concept in The Treatment of Stroke: A Systematic ReviewDocument15 pagesEffectiveness of The Bobath Concept in The Treatment of Stroke: A Systematic ReviewAfrizal BintangNo ratings yet
- SUPER KIDZ Pain ScaleDocument10 pagesSUPER KIDZ Pain Scalepfi_jenNo ratings yet
- Limpeza PedeDocument9 pagesLimpeza Pedemarisa araujoNo ratings yet
- GMMMC Sukkur MbbsDocument6 pagesGMMMC Sukkur MbbsSherazAhmedNo ratings yet
- Home Study Course-HomeopathDocument155 pagesHome Study Course-HomeopathAzad Ansari67% (6)
- Journal Reading - Myringitis - Elisabeth PattyDocument14 pagesJournal Reading - Myringitis - Elisabeth PattyLipatOla123No ratings yet
- DEPRESSANTSDocument18 pagesDEPRESSANTSElisha Arwynne Postrero RomaNo ratings yet