Professional Documents
Culture Documents
(Anes) 6-7 - Regional Anesthesia - Peripheral Nerve Block (Dr. Dela Cerna) ?
Uploaded by
NoreenOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
(Anes) 6-7 - Regional Anesthesia - Peripheral Nerve Block (Dr. Dela Cerna) ?
Uploaded by
NoreenCopyright:
Available Formats
[ANESTHESIOLOGY] Regional Anesthesia, Peripheral Nerve Blocks
Lecturer: Ernest M. Dela Cerna, MD
Transcriber: Patrick Angelo R. Bautista September 2020
References and Legends
nd
• {💻} PPT and {📕} Chapter 6-7 - Anesthesiology Manual 2 Ed
• {📖} Morgan & Mikhail’s Clinical Anesthesiology 5 Ed
th
• {📌} Transcriber’s Note
Table of Contents
I. Anatomy of the Spine 1
II. Autonomic Blockade of Regional Anesthesia 2
III. Somatic Blockade of Regional Anesthesia 3
IV. Regional Anesthesia Technique 3
V. Spinal Anesthesia 5
VI. Epidural Anesthesia 6
VII. Peripheral Nerve Blocks 8
VIII. Samplex 8
Figure: Posterior and sagittal views of the sacrum and coccyx.
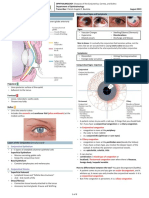
I. ANATOMY OF THE SPINE Ligamentous Layers
• The Spine is composed of: • The vertebral bodies and intervertebral disks are joined together
9 Ligamentous layers by the anterior and posterior longitudinal ligaments ventrally.
9 33 vertebrae • Supraspinous ligament (outer most layer)
§ 7 cervical § 5 sacral (fused) • Interspinous ligament (middle layer)
§ 12 thoracic § 4 coccygeal • Ligamentum flavum (innermost layer)
§ 5 lumbar
• Function: structural security and support for the spinal cord.
Figure: Sagittal section through lumbar vertebrae
Spinal Cord
• The spinal cord with its covering is enclosed in the spinal canal.
Figure: Divisions of spinal column • Adult’s spinal cord:
9 Begins at the foramen magnum
• A spinal canal is formed: 9 Ends at the level of the L1 vertebra
9 Anteriorly: vertebral body • Newborn and children:
9 Laterally: pedicles and transverse processes 9 Ends at the level of the L3 and eventually moves up.
9 Posteriorly: lamina and spinous processes
Figure: Superior view of the common vertebra
• Sacral hiatus
9 Caudal opening to the spinal canal due to the lamina of the S5
and/or part of the S4 vertebra usually not uniting.
• Normal curvature of the spinal column:
9 Follows a double C shape convexity anteriorly specifically in
the cervical and lumbar area.
• Spinal column in a lateral view:
9 Highest points: C5 and L5
9 Lowest points: T5 and S2 Figure: Sagittal view through the lumbar vertebrae and sacrum.
9 These points entail the anesthetic level and local anesthetic Note the end of the spinal cord rises with development from
spread after spinal anesthetic injection. approximately L3 to L1. The dural sac normally ends at S2.
Regional Anesthesia and Peripheral Nerve Blocks | 1 of 8
Spinal Nerve Roots
• The principal site of action for neuraxial blockade is believed to
be the nerve root.
• The paired anterior and posterior nerve roots from each vertebral
level exits the CNS via the intervertebral foramen forming
cervical (C1) to sacral (S5) spinal nerve roots.
9 Cervical vertebra level: nerves appear above the
corresponding vertebrae level
9 Starting at the T1: the nerves leave below their vertebra.
9 Consequently, they form 8 cervical nerve roots with only
7 cervical vertebras in place.
• Conus medullaris
9 Spinal cord bulbous terminal end
• Filum terminale
9 Tapering end of conus medullaris
9 Usually anchors in the sacral region
• Cauda equina
9 Horse-tail appearance; some lower spinal nerve roots courses
down before leaving the intervertebral foramen creating a
horse-tail appearance
Spinal Meninges
• Coat the spinal cord
Figure: Arterial supply to the spinal cord.
• Three layers:
A: Anterior view showing principal sources of blood supply.
9 Fibrous dura mater (outermost layer)
B: Cross-sectional view through the spinal cord showing paired posterior
9 Avascular arachnoid layer (middle layer) spinal arteries and a single anterior spinal artery.
9 Highly vascular pia mater (innermost layer) which is closely
attached to the spinal cord. Anesthesia Pearls
• Subarachnoid space aka intrathecal space • Local anesthetic target site of action is the spinal nerve roots.
9 Lies between the arachnoid and pia mater. • The endpoint in performing a subarachnoid block is the presence
9 It is also where cerebrospinal fluid (CSF) is located wherein the of the free-flowing and clear cerebrospinal fluid.
spinal anesthetic agent is injected. • During lumbar needle insertion below L1 in adults (L3 in children),
• Epidural space potential cord needle trauma is avoided since these nerve roots
9 A potential space that surrounds the spinal meninges. float in the dural sac below L1 and tend to be pushed away by
9 Bound by the dura and the ligamentum flavum posteriorly. an advancing needle.
9 Widest at the level of L2 (5-6 mm) • Epidural anesthesia can be applied at any vertebral level while
9 Narrowest at the level of the C5 (1-1.5 mm) spinal anesthesia should only be injected below the level of the
spinal cord.
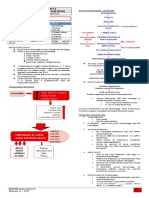
II. AUTONOMIC BLOCKADE OF
REGIONAL ANESTHESIA
1. Cardiovascular Effects
• Blockade of the sympathetic preganglionic neurons during
regional anesthesia sends signals to both arteries and veins in
which the predominant action is venodilation and thus, reduces
the following:
9 Blood pressure
9 Venous return
9 Stroke volume
9 Cardiac output
• High spinal blockade (above T4 level) or T1-T4 blockade,
9 Unopposed vagal stimulation wherein the bradycardia at this
Figure: Exit of the spinal nerves.
level is due to the cardio-accelerator fibers blockade.
9 Hence, a decreased venous return to right atrium would lead to
Blood Supply of the Spinal Cord
a decreased stretch receptor response.
• Blood supply of the spinal cord and nerve roots is derived from:
• Hypotension can be prevented or minimized by increasing the
9 Single anterior spinal artery – supplies anterior 2/3 of cord
cardiac preload → done by infusing large IV fluid (10-20 cc/kg)
9 Paired posterior spinal arteries – supplies posterior 1/3
before or during spinal anesthesia induction.
9 Intercostal arteries (thorax) and lumbar arteries (abdomen)
9 If hypotension still persists despite maximum infusion of IV
§ Supplementary blood flow to the anterior and posterior
fluids, a pharmacologic treatment may be done by giving
spinal arteries
Ephedrine or Phenylephrine.
9 Artery of Adamkiewicz
§ One of these radicular arteries; Unilateral and mostly arises
on the left side and is the major blood supply to the 2. Pulmonary Effects
anterior, lower 2/3 of the spinal cord. • Appropriate regional blockade has a little effect on ventilation.
§ A damage to this artery would result to anterior spinal • Pulmonary physiology effects even in high thoracic levels are
artery syndrome causing spinal ischemia to the anterior minimal (slight decrease in vital capacity) since the diaphragm is
portion of the spinal cord. innervated by the phrenic nerve (C3-C5).
• However, in patients with severe chronic lung disease that rely
upon accessory respiration (intercostal and abdominal muscles)
these will significantly impair the muscles of inspiration and
expiration during a high level of blockade.
Regional Anesthesia and Peripheral Nerve Blocks | 2 of 8
3. Gastrointestinal Effects 3.2 Antiplatelet Drugs
• Sympathectomy allows vagal tone dominance which results to • Aspirin / NSAIDs do not increase the risk of spinal hematoma.
small and contracted gut with active peristalsis. • Drugs needed to be stopped for a certain waiting period for which
• Use of epidural analgesia for post-operative management regional anesthesia can be administered after the drug effects
improves the return of gastrointestinal function. worn off:
9 Ticlopidine (Ticlid) – 14 days
9 Clopidogrel (Plavix) – 7 days
4. Urinary Tract Effects
9 Abciximab (Rheopro) – 48 hours
• The loss of bladder tone results in urinary retention during 9 Eptifibatide (Integrilin) – 8 hours
regional blockade.
• Placement of indwelling foley-catheter helps to drain urine 3.3Standard (Unfractionated) Heparin
intraoperatively until the blocks wears off. • Avoid regional anesthesia in patients:
9 On therapeutic doses of heparin
III. SOMATIC BLOCKADE OF 9 With elevated partial thromboplastin time
REGIONAL ANESTHESIA (LOCAL ANESTHETICS) • If epidural catheter placement is done, removal must be done:
9 1 hour prior administration of heparin or
• Regional Anesthesia provides a profound sensory blockade that
9 4 hours after administration of heparin
interrupts both somatic and visceral painful stimuli.
• For patients who receive a prophylactic “minidose” of
• Local anesthetics effect on the nerve fibers varies on the size
and characteristics of the nerve fiber. subcutaneous heparin:
9 Anesthesia is not contraindicated.
• Smaller and myelinated nerve fibers are easily blocked than larger
• For patients who are to receive IV heparin intraoperatively:
and unmyelinated fibers.
9 Regional anesthesia may be done ≥1 hour prior to regional
• Differential blockade
9 Occurs when the concentration of local anesthetic decreases
blockade.
with increasing distance from the level of injection.
9 Temperature sensitivity (alcohol swab)
3.4Low-Molecular-Weight Heparin (LMWH)
§ Two segments or more cephalad than sensory block • Enoxaparin (Lovenox)
9 Pin prick test (pain and light touch) • If a bloody regional placement happens:
§ Few segments more cephalad than the motor blockade. 9 The use of LMWH should be postponed until 24 hours
postoperatively because this traumatic placement may
Spread of Local Anesthetics increase the risk of spinal hematoma.
Local anesthetic solution will soak the cauda equine area • If LMWH thromboprophylaxis is necessary:
↓ 9 Epidural catheters should be removed 2 hours prior to the
LA solution moves cephalad to the spinal cord first dose
↓ • in cases LMWH are already administered:
Diffusing laterally to the primary targets: nerve rootlets, nerve roots 9 The catheter should be removed at least 10 hours after a
dose of LMWH and the next dose must be not given for
1. Common Clinical Indications of Regional Anesthesia another 2 hours.
• Lower abdominal surgeries 3.5 Fibrinolytic or Thrombolytic Therapy
9 Urogenital surgery (Ob-Gyne procedures)
9 Rectal surgery
• A regional anesthesia should not be done in a patient who has
9 Lower extremities (hip, femur, knee and foot surgery)
received a fibrinolytic and thrombolytic therapy.
• It is also advantageous to patients with:
9 Full stomach IV. REGIONAL ANESTHESIA TECHNIQUE
9 Anatomic distortions of the upper airway
• Favorable to post-operative analgesia management through
continuous infusion.
2. Contraindications to Regional Anesthesia
• Absolute Contraindication
9 Patient refusal
• Relative Contraindication
9 Infection
9 Coagulopathy
9 Severe hypotension
9 Increased intracranial pressure Regional Anesthesia encompasses:
9 Severe Aortic or Mitral Stenosis • Spinal Anesthesia (Subarachnoid Block)
• Epidural Anesthesia
3. Regional Anesthesia in the Anticoagulated Patient • Peripheral Nerve Blocks
• The American Society of Regional Anesthesia (ASRA) continue • Regional anesthesia must be performed in a sterile facility with
to update guidelines whether a block be performed in complete equipment and drugs for general anesthesia in case
anticoagulated patient. regional anesthesia fails.
• Preparation for regional anesthesia (spinal or epidural anesthesia)
3.1 Oral Anticoagulants requires a vigilant cardiac, sensory and motor monitoring prior,
• In patients who are receiving warfarin therapy, a normal during and after local anesthetic administration.
prothrombin time and international normalized ratio should be • Patient must be hooked to a cardiac monitor equipped with:
done prior to regional anesthesia. 9 Electrocardiogram
• Coordination with the primary physician must be initiated prior 9 Non-invasive blood pressure monitoring
discontinuation of the anticoagulant. 9 Pulse oximeter
• Proper hydration – to minimize hypotension perioperatively.
Regional Anesthesia and Peripheral Nerve Blocks | 3 of 8
1. Surface Anatomy Landmarks
• When spinal and lumbar epidural anesthesia is to perform, the
surface landmark at the back would be an:
9 Imaginary line drawn between the highest points of both iliac
crests (Tuffier’s line) which usually crosses the L4 vertebral
body or the L4-L5 interspace.
• When performing a cervical epidural block:
9 First palpable spinous process – C2
9 Most prominent spinous process – C7 (vertebra prominens).
9 Needle is inserted with only a slight cephalad angle.
• When thoracic epidural anesthesia is contemplated
9 The surface landmark of the spinous process of T7 is usually
at the same level of the inferior angle of the scapulae.
9 Needle is inserted more cephalad to enter.
Cervical Epidural C7 (Vertebra Prominens)
Thoracic Epidural T7
Spinal and Lumbar Tuffier’s line (L4-L5 interspace)
Figure: The effect of flexion on adjacent vertebrae. A: Posterior view.
B: Lateral view. Note the target area (interlaminar foramen) for neuraxial
blocks increases in size with flexion.
2.2Sitting Position
• Obese and pregnant patients may benefit from this position since
these patients cannot tolerate the fetal position of lateral decubitus
because of their enlarged abdomen.
• Patients sit on the side of the operating table with knees pushed at
the edge of the bed with legs/feet resting in a chair or footstool and
the arms comfortably hugging a pillow.
• The flexion of the spine arching like a “mad cat” brings the target
area closer to the skin surface
Figure: Surface landmarks for identifying spinal levels.
2. Positioning
2.1 Lateral Decubitus
• Patients lie on their side (right or left) with their knees flexed pulled
high against the abdomen in which it assumes a “fetal position”
Figure: Sitting position for neuraxial blockade.
Note an assistant helps in obtaining maximal spinal flexion.
2.3Buie’s (Jackknife) Prone
• This position is best utilized among anorectal procedures with an
isobaric or hypobaric local anesthesia.
• The block is done in the same position as the operative procedure,
the patient does not have to be moved after spinal blockade.
Figure: Lateral decubitus position for neuraxial blockade.
• The CSF in this position will not freely flow so a CSF aspiration
Note the assistant helping to provide maximal spine flexion.
must be done to confirm placement of the needle.
Regional Anesthesia and Peripheral Nerve Blocks | 4 of 8
V. SPINAL ANESTHESIA
• aka Subarachnoid Block
9 Sensory function → analgesia
9 Autonomic function → sympathetic block
9 Motor function → paralysis
• Process:
9 Lumbar tap
9 Injection of the Local Anesthetic
1. Technique
• Spinal anesthesia or aka subarachnoid or intrathecal block can
be performed in a midline or paramedian/lateral approach in a
patient lying in a lateral decubitus, sitting or prone position.
Figure: The prone jackknife position often used for anorectal surgery • As needle traverses at the entry site:
can also be used for caudal anesthesia in adults. 9 First pop (resistance) – penetration of ligamentum flavum
9 Second pop – dura-arachnoid membrane in which upon
3. Anatomic Needle Approach withdrawing the needle stylet, a free-flowing CSF is
appreciated.
3.1 Midline Approach
1) The plane of the back is usually perpendicular to that of the floor. 1) Lateral decubitus; Tuffier’s line identified
2) Tuffier’s line (L4-L5 interspace) is identified → needle entry site 2) Asepsis and antisepsis
3) Asepsis and antisepsis: Prior to needle entry, a 10% betadine 3) Local anesthesia (2% Lidocaine)
will be applied on and around the needle site entry. 4) 1st pop → ligamentum flavum
4) Local anesthesia (2% Lidocaine) on the desired needle site entry 5) 2nd pop → dura-arachnoid membrane
5) After 2-3 minutes of local infiltration, a procedure needle is inserted 6) Free-flowing CSF
midline with slightly cephalad direction (spinous processes at this
level are more caudad) traversing the following layers:
9 Skin → subcutaneous → supraspinous → interspinous
ligament → ligamentum flavum
6) From this point, the techniques for spinal and epidural differ.
Figure: Spinal anesthesia
2. Factors Influencing Level of Spinal Block
Figure: Lumbar epidural anesthesia; midline approach. TABLE 45-2
Factors affecting the dermatomal spread of spinal anesthesia
3.2 Paramedian or Lateral Approach Most important factors
• Applicable in patients who cannot positioned easily Baricity of anesthetic solution
9 Severe arthritis, kyphoscoliosis or spine surgery Position of the patient
1) Tuffier’s line identified During injection
2) Asepsis and antisepsis Immediately after injection
3) Local anesthesia (2% Lidocaine) → 2 cm lateral to the inferior Drug dosage
aspect of the superior spinous process of the desired level. Site of injection
4) Needle is directed and advanced at a 10-25° angle toward midline. Other factors
5) Techniques for spinal and epidural applies Age
Cerebrospinal fluid
Curvature of the spine
Drug volume
Intraabdominal pressure
Needle direction
Patient height
Pregnancy
1.1Baricity of the Anesthetic Solution
• The migration of local anesthetic depends on its density relative to
CSF (baricity).
• The CSF specific gravity is 1.003-1.008 at 37°C.
9 Hyperbaric anesthetic solution is heavier (denser) than CSF
that tend to move to the most dependent area of the spine]
9 Hypobaric is lighter than CSF that tends to move to the most
independent area of the spine.
Figure: Paramedian approach.
Regional Anesthesia and Peripheral Nerve Blocks | 5 of 8
1.2 Position of the Patient 5. Failed Subarachnoid Block
• When in a head-down position • Spinal anesthesia: one of the most reliable regional block methods.
9 Hyperbaric solution will move to the cephalad area. 9 The appearance of free-flowing CSF is a clear indicator that
9 Hypobaric solution moves to the caudad area. the needle is in the correct space.
9 Isobaric solution tends to stay at the level of injection since it 9 1% chance of failure even in the most skilled hands.
has the same as CSF density.
• Failure can be described as no block or a partial block leading
1.3 Drug Dosage and Site of Injection to inadequate block height, block duration or quality as
• The larger the dosage of local anesthetic solution or the more originally planned for the surgical procedure.
cephalad the site of injection, overall, the more cephalad • Several mechanisms for the occurrence of failure:
distribution level of anesthesia is expected. 1) Failed lumbar tap
2) Solution injection errors e.g. wrong or inadequate drug dose
1.4 Patient’s Height and Vertebral Column Anatomy 3) Inadequate preoperative anxiety alleviation of the patient
• Spinal curvature affects the anesthesia level by changing the
contour or shape of the subarachnoid space. • One mechanism by which there can be loss of injectate is during
needle tip displacement after locking the syringe with the drug
1.5 Direction of the needle bevel and the spinal needle.
9 Pencil tip needles need only a small amount of backward
• Higher levels of anesthesia are attained if when the injection is
displacement to result in an accidental epidural injection.
directed cephalad than if the point of injection is directed laterally
9 The needle may also be inserted just between the dura and
or caudad.
epidural space, resulting in inadequate block.
1.6 CSF volume
• Barbotage, or the admixing of local anesthetic and CSF thru
• Inversely correlates with dermatomal distribution careful aspiration of the latter during before administration of spinal
• In cases of increased abdominal pressure (obese and pregnant anesthesia has been traditionally done to assure that the spinal
women), epidural veins are engorged thus decreasing CSF volume needle is still in the subarachnoid space after connecting it to the
are more associated with greater dermatomal distribution for a syringe containing the local anesthetic.
given volume of anesthetic solution. 9 However, this practice is being questioned.
9 It has been proposed that the dura or arachnoid matter may
1.7 Increasing Age act as a “flap valve” so that initial aspiration of CSF is evident,
• Increasing age is associated with decrease CSF volume thus likely but subsequent pushing of the local anesthetic pushes the flap
responsible for the higher levels of anesthesia. forward, causing a misplaced injection
3. Spinal Anesthesia Levels VI. EPIDURAL ANESTHESIA
Dermatome Application 1. Technique
C4 (Clavicle) Chest Surgery • An epidural anesthesia can be done at cervical, thoracic, lumbar
T4-T5 (Nipples) Upper Abdominal Surgery and sacral (caudal) level.
T6-T8 (Xiphoid) Intestinal Surgery, Appendectomy, • This technique can be performed in a single shot or a continuous
Gynecologic Pelvic Surgery, Ureter epidural anesthesia (intermittent boluses through an epidural
and Rectal Pelvic Surgery catheter).
T8 (Lower border of ribcage) Abdominal Surgery • Midline or Paramedian Approach
T10 (Umbilicus) Transurethral resection, Obstetric 9 Can be used in inserting the epidural needle.
vaginal Delivery and Hip Surgery 9 As the needle traverses the skin, subcutaneous, supraspinous
L1 (Inguinal ligament) Transurethral resection, If no ligaments and interspinous ligaments, the needle must stop
bladder distension, Thigh surgery, piercing the dura layer.
Lower limb amputation 1) Lateral decubitus; Tuffier’s line identified
L2-L3 (Knee and below) Foot surgery 2) Asepsis and antisepsis
S2-S5 (Perineum) Perineal Surgery, 3) Local anesthesia (2% Lidocaine)
Hemorrhoidectomy, Anal Dilation 4) Epidural needle must stop piercing the dura layer
5) 2 techniques to identify epidural space
4. Pharmacology of Spinal Anesthetic Agents 6) Loss of resistance technique / Hanging drop technique
• Hyperbaric bupivacaine and Tetracaine • Two techniques are used to identify the epidural space:
9 Most common spinal local anesthetic solutions. 1) Loss of resistance technique (most preferred by clinicians)
9 Onset of action: Slow (5-10 minutes) 2) Hanging drop technique
9 Duration of action: Long (90-120 minutes)
• Addition of vasoconstrictors to anesthetic solution 1.1 Loss of Resistance Technique
9 The use of vasoconstrictors like alpha-adrenergic agonists
1) Advance the needle until the interspinous ligament
and epinephrine during spinal anesthesia prolongs the 2) Stylet is removed after which a 2-ml syringe filled with saline or air
duration of anesthetic block by decreasing the rate of uptake of is attached to the hub of the epidural needle.
local anesthetics from the CSF. 3) Gentle application of pressure is done as the needle is advanced
to the potential space
Anesthesia Pearls 4) As the tip of the needle reaches the epidural space, a sudden loss
• Only preservative-free local anesthetic solutions are used in
of resistance will be felt and will be seen → saline or air will be
regional anesthesia.
pulled inside by the negative pressure of the potential space.
• Use of lidocaine in spinal anesthesia is no longer used because of
the phenomenon “transient neurological symptoms and cauda
equine syndrome”.
• Saddle block is attained by keeping the patient in sitting position
after local anesthetic injection soaking the lower lumbar nerves
and sacral nerves.
Regional Anesthesia and Peripheral Nerve Blocks | 6 of 8
1.2 Hanging Drop Technique 5. Caudal Anesthesia
• Almost the same technique with the loss of resistance except that • This is a common technique among the pediatric population.
the hub of the needle will be filled with a solution. • Surface landmark:
9 The needle will be advanced forward until the drop of saline 9 Depression above the coccyx and between the sacral cornua.
gets sucked into the epidural space due to its relative negative • The needle placement is performed by penetrating the
pressure. sacrococcygeal ligament at 90° (covering the sacral hiatus created
• An epidural catheter will be inserted if a continuous (intermittent by the unfused S4 and S5 laminae) then must be angle
bolus) epidural anesthesia is desired. downwards as it advanced to enter the sacral hiatus
2. Epidural Anesthesia Test Dose
• This test dose preparation is intended to detect both subarachnoid
and intravascular injection.
• Usual test dose:
9 3-ml of 1.5% Lidocaine with Epinephrine 1: 200,000 solution
(0.005 mg/ml)
• If the epidural catheter in placed is located intrathecally, the
45 mg of Lidocaine will produce spinal anesthesia rapidly
(motor and sensory blockade).
• if the epidural catheter in place is near or threaded intravascularly,
the 15 mcg of Epinephrine will increase the heart rate by 20% Figure: Positioning an anesthetized child for caudal block and palpation
from the baseline for the sacral hiatus. An assistant gently helps flex the spine.
9 If patient taking β-blockers, only an increase in BP is observed.
Anesthesia Pearls
• The onset of the epidural anesthesia is slower; the anesthetic
solution travels and soaks first (entry site level) the surrounding the
dura mater posteriorly, laterally and anteriorly where the nerve
roots are also located.
• Epidural anesthesia block may be differential or segmental block
(anesthetic solution confined near to the injection site). It is
described as a well-defined band of anesthesia at a certain
nerve roots while sparing other nerve roots.
• The lumbar epidural space contains fatty connective tissue,
lymphatics and a rich venous (Batson’s) plexus.
• In some patients where intravascular epinephrine is not prudent,
Fentanyl 100 mcg in the intravascular space will result in
dizziness or drowsiness.
• Care should be given to prevent accidental IV injection of local
anesthetics to prevent Local Anesthetic Systemic Toxicity
(LAST) – done by:
9 Aspirating for blood before administering doses Figure: Caudal block. Note the sacrococcygeal ligament is penetrated
9 Intermittent dosing with the needle almost at 90° and then must be angled down and
9 Using dilute solutions, especially during labor analgesia advanced to enter the sacral hiatus.
9 Maintaining verbal contact with the patient during giving of the
anesthetic 6. Complications assoc. with Needle / Catheter Insertion
9 Recognition of the initial signs of LAST is important
• The most common complication of regional anesthesia is back
pain followed by inadequate anesthesia or failed block and post-
3. Factors Affecting Blockade of Epidural Anesthesia
dural puncture headache.
• Epidural anesthesia is not as predictable as spinal anesthesia.
• Dermatomal spread of epidural anesthesia is only partially 6.1Post-Dural Puncture Headache (PDPH/Spinal Headache)
affected by gravity. • The onset of the headache is usually 12-72 hours prior injection.
9 However, patient positioning through lateral decubitus and
• It is described to be bilateral, frontal, retro-orbital or occipital that
Trendelenburg can be applied to attain desired level or block. extends into the nape area.
• Distribution of local anesthetic is computed according to the
• Hallmark of PDPH: its association with body position
desired level. 9 Pain is aggravated with sitting or standing and pain is relieved
9 In adults: a 1-2 ml per segment (vertebra) is accepted.
by lying down.
9 An attempt to block the T4 sensory level requires 12-24-ml
9 This is explained from the leaking CSF from the dural defect
of local anesthetic given at intermittent boluses. causing increased traction on structures that support the brain.
9 Taller patients: require a higher dose at least 2 ml/segment
• Treatment:
9 Shorter patients: may only require 1 ml/segment
9 Treatment is aimed at reducing the symptoms until the point of
leakage seals itself.
4. Epidural Anesthetic Agents § Flat on bed, application of abdominal binder, analgesic
• Common epidural anesthetic agents are: administration and infusion of IV fluids and/or oral fluids to
9 Lidocaine (short acting – 30 minutes) promote adequate hydration are some of the methods to
9 Mepivacaine (intermediate acting – 1 hour) alleviate PDPH.
9 Levobupivacaine / Bupivacaine (long acting – 90 min-2 hrs) 9 Caffeine can also help by vasoconstricting intracranial vessels.
• Addition of vasoconstrictors (Epinephrine 5 mcg/ml) 9 However, in cases where headache persists despite
9 Can also prolong the effect of epidural lidocaine by delaying conservative treatment, an epidural blood patch is effective
vascular absorption. (90% of patients improve from a single blood patch).
• Addition of opioids (fentanyl and morphine) 9 Epidural blood patch works by sealing the dural defect by
9 Can enhance the quality of epidural anesthesia rather than the placing 10-20 ml of autologous blood in the epidural space.
duration of block.
Regional Anesthesia and Peripheral Nerve Blocks | 7 of 8
VII. PERIPHERAL NERVE BLOCKS 2.4Sural Nerve
• A branch of posterior tibial nerve.
1. Upper Extremity Nerve Block • Supplies sensory to the posterior lateral half of the calf and
lateral side of the foot and 5th toe.
Brachial Plexus
• A local anesthetic solution must be injected posterior to the lateral
• As the brachial plexus emerges below the clavicle, the local
malleolus.
anesthetic solution can be deposited at any point depending on the
desired block effects.
2.5Deep Peroneal Nerve
9 Musculocutaneous, Median, Ulnar, Radial, Axillary
• The continuation of the common peroneal nerve.
• This nerve can be block by identifying the depression between the
extensor hallucis longus and extensor digitorum longus tendon in
which the dorsalis pedis artery is appreciated.
• A local infiltration is injected lateral to the pulse.
Figure: Cutaneous innervation of the foot
Figure: The location of local anesthetic deposition along the brachial
plexus depends on the desired effects of the block.
1.1 Axillary Nerve Block
• Position:
9 Patient is in a supine position
9 Head turned away from the arm being blocked
9 Arm is abducted to 90°
9 Forearm is flexed to 90° Figure: Needle placement for ankle block.
9 Brachial artery pulse is palpated
• Tourniquet band is usually applied in the arm to allow the local
VIII. SAMPLEX
anesthetic concentration to soak the axilla area.
• This block provides anesthesia to distal forearm and wrist, but it 1. What is the principal site of action for neuraxial blockade?
has no block to the musculocutaneous nerve because it lies A. CSF C. Spinal cord
outside the sheath and this must be blocked separately. B. Nerve root D. Epidural space
2. Which of the following statement is true regarding hyperbaric
2. Lower Extremity Nerve Block anesthetic solution during spinal anesthesia?
• Ankle Block – A complete ankle block requires 5 separate A. The solution is not dependent on positioning.
injections that provides anesthesia for surgical procedures of the B. The solution will spread cephalad in head-up position.
foot and these nerves are the following: C. The solution will spread caudad in head-down position.
D. The solution will have a greater effect in the dependent side in a
2.1 Tibial Nerve lateral position.
• The largest nerve to block. 3. The adult spinal cord ends at the level of:
• Supplies sensory to the heel and medial side sole of the foot. A. L1 C. L3
• Local infiltration can be injected by identifying first the posterior B. L2 D. L4
tibial artery pulse behind the medial malleolus, thereafter the local 4. In which level is epidural space widest?
anesthetic solution is deposited posterior to the artery in the deep A. L1 C. L3
pocket to the flexor retinaculum. B. L2 D. L4
2.2 Superficial Peroneal Nerve 5. What dermatomal level is needed in doing spinal anesthesia for
appendectomy?
• A branch of common peroneal nerve. A. T4 (answer key) C. T6 (proposed answers)
• Supplies sensory to the dorsal (top) portion of the foot. B. T5 D. T7
• A local infiltration is injected near the lateral malleolus.
6. Which layer of the back is NOT traversed by the spinal needle in a
2.3 Saphenous Nerve paramedian approach?
A. Supraspinous C. Dura
• A branch of femoral nerve
B. Intraspinous D. Ligamentum flavum
• Supplies sensory to the medial side of the leg, ankle and foot.
• This can be block by injecting a local anesthetic solution toward 7. The vascular spinal meningeal layer that coats the spinal cord:
the medial malleolus. A. Dura C. Subarachnoid
B. Arachnoid D. Pia
📌 No proofreading. Use at your own risk.
Regional Anesthesia and Peripheral Nerve Blocks | 8 of 8
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- (GYNE) 2018 April Midterms Ratio (Pucca)Document31 pages(GYNE) 2018 April Midterms Ratio (Pucca)NoreenNo ratings yet
- Clinical Therapeutics Oral Revalida Review Notes: CASE 1: Dr. Abraham Daniel C. CruzDocument31 pagesClinical Therapeutics Oral Revalida Review Notes: CASE 1: Dr. Abraham Daniel C. CruzNoreenNo ratings yet
- (Gyne) Family Planning (Dra Ona - Dra Castro) Updated Version (2022)Document14 pages(Gyne) Family Planning (Dra Ona - Dra Castro) Updated Version (2022)NoreenNo ratings yet
- (Anes) 3 - Monitoring of Anesthetized Patient (Dra. Mendoza) ?Document4 pages(Anes) 3 - Monitoring of Anesthetized Patient (Dra. Mendoza) ?NoreenNo ratings yet
- (Cardio B) 1 - Acute Rheumatic Fever and Rheumatic Heart Disease (Dr. Antolin, 2019)Document4 pages(Cardio B) 1 - Acute Rheumatic Fever and Rheumatic Heart Disease (Dr. Antolin, 2019)NoreenNo ratings yet
- (Anes) 1 - Preanesthetic Evaluation (Dra. Luna-Gomez) ?Document5 pages(Anes) 1 - Preanesthetic Evaluation (Dra. Luna-Gomez) ?NoreenNo ratings yet
- (Anes) 5 - Local Anesthetics (Dra. Bonoan-Chan) ?Document5 pages(Anes) 5 - Local Anesthetics (Dra. Bonoan-Chan) ?NoreenNo ratings yet
- (IM A) (Com Dse) Typhoid Fever (Strawberry)Document4 pages(IM A) (Com Dse) Typhoid Fever (Strawberry)NoreenNo ratings yet
- (IM A) (Com Dse) Typhoid Fever-Dr. Salandanan, Dr. Tan (Trisha Oberio, Kristine Navarro, Aisle Paler)Document4 pages(IM A) (Com Dse) Typhoid Fever-Dr. Salandanan, Dr. Tan (Trisha Oberio, Kristine Navarro, Aisle Paler)NoreenNo ratings yet
- Case 9 Section EDocument12 pagesCase 9 Section ENoreenNo ratings yet
- (IM A) (Hema) IDA and Hypoproliferative Anemias-Dr. Perez 2 (Kim Villanueva)Document5 pages(IM A) (Hema) IDA and Hypoproliferative Anemias-Dr. Perez 2 (Kim Villanueva)NoreenNo ratings yet
- (IM A) (Com Dse) Rabies-Dr. Coronel (Vision)Document7 pages(IM A) (Com Dse) Rabies-Dr. Coronel (Vision)Noreen100% (1)
- (MED) 3.05 Approach To Edema, Chest Pain, & Palpitations - AzaresDocument18 pages(MED) 3.05 Approach To Edema, Chest Pain, & Palpitations - AzaresNoreenNo ratings yet
- (Pedia 3A) Immunology-Dr. de Jesus (Pinky Square)Document6 pages(Pedia 3A) Immunology-Dr. de Jesus (Pinky Square)NoreenNo ratings yet
- Clinical Therapeutics: Case 1Document17 pagesClinical Therapeutics: Case 1NoreenNo ratings yet
- Cardiology: Normal and Abnormal Myocardial Function: LendldeornmanDocument2 pagesCardiology: Normal and Abnormal Myocardial Function: LendldeornmanNoreenNo ratings yet
- (Pedia 3A) NEPHRO COMPILED PDFDocument40 pages(Pedia 3A) NEPHRO COMPILED PDFNoreenNo ratings yet
- (Ophtha) 7 - Diseases of The Conjunctiva, Cornea, and Sclera (2019)Document8 pages(Ophtha) 7 - Diseases of The Conjunctiva, Cornea, and Sclera (2019)NoreenNo ratings yet
- (MED1) 3.04 Approach To Hypertension (Dr. Bago-Azares)Document11 pages(MED1) 3.04 Approach To Hypertension (Dr. Bago-Azares)NoreenNo ratings yet
- Hypovolemic Shock & DIC (Bernabe)Document4 pagesHypovolemic Shock & DIC (Bernabe)NoreenNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Neuroanatómia Vizsgatételek A És B Csoport Képletekkel HZ ENDocument25 pagesNeuroanatómia Vizsgatételek A És B Csoport Képletekkel HZ ENTowan NguyenNo ratings yet
- Perdarahan Intra Dan Extra AxialDocument19 pagesPerdarahan Intra Dan Extra AxialFarmasi FKUNSNo ratings yet
- Gambaran CT SCAN: (Kasus: Edh, SDH, Ich, Sah, Infark Cerebri, IvhDocument44 pagesGambaran CT SCAN: (Kasus: Edh, SDH, Ich, Sah, Infark Cerebri, Ivhfahmi rosyadiNo ratings yet
- Necropsy Procedures and Basic Diagnostic Methods For Practicing VeterinariansDocument262 pagesNecropsy Procedures and Basic Diagnostic Methods For Practicing VeterinariansDenisa VescanNo ratings yet
- Imaging Anatomy Brain and Spine Anne G Osborn Full ChapterDocument67 pagesImaging Anatomy Brain and Spine Anne G Osborn Full Chaptervicki.wilson456100% (10)
- Introduction To NeuropsychologyDocument15 pagesIntroduction To NeuropsychologyPsychology Department Ilahia Arts CollegeNo ratings yet
- Nervous SystemDocument29 pagesNervous SystemMuhammed Aslam NVNo ratings yet
- 116 - Concept of Perception and CoordinationDocument3 pages116 - Concept of Perception and Coordinationalaisahmae02No ratings yet
- SPINAL CORD (External Features)Document39 pagesSPINAL CORD (External Features)Drravikumar BhandariNo ratings yet
- Imagerie Des TumeursDocument14 pagesImagerie Des TumeursOuma TaziNo ratings yet
- Ms - Angeline M.SC (N) Previous Year Psychiatric Nursing Choithram College of NursingDocument79 pagesMs - Angeline M.SC (N) Previous Year Psychiatric Nursing Choithram College of NursingPankaj TirkeyNo ratings yet
- Icd 9 CM (Tabulasi) 2012Document263 pagesIcd 9 CM (Tabulasi) 2012M Taufik Harahap100% (1)
- Epidural Space - Lies Between The Dura and The Vertebral BonesDocument4 pagesEpidural Space - Lies Between The Dura and The Vertebral BonesDaniel DanielNo ratings yet
- Robin Bhatia, Ian Sabin-Challenging Concepts in Neurosurgery - Cases With Expert Commentary-Oxford University Press (2015)Document253 pagesRobin Bhatia, Ian Sabin-Challenging Concepts in Neurosurgery - Cases With Expert Commentary-Oxford University Press (2015)rogeriotorres13100% (1)
- Gross Anatomy PDFDocument55 pagesGross Anatomy PDFDeborah RochaNo ratings yet
- 9th-10-11th May-2016 Papers (1650 MCQS) by Amlodipine Besylate PDFDocument161 pages9th-10-11th May-2016 Papers (1650 MCQS) by Amlodipine Besylate PDFAmlodipine BesylateNo ratings yet
- Lesson 3 Nervous SystemDocument11 pagesLesson 3 Nervous SystemMARY JANE ANGELICA SEVANo ratings yet
- The 12 Cranial NervesDocument11 pagesThe 12 Cranial Nervesapi-306342919No ratings yet
- Reconstruction of Skull Base Defects After Minimally Invasive Endoscopic Resection of Anterior Skull Base NeoplasmsDocument7 pagesReconstruction of Skull Base Defects After Minimally Invasive Endoscopic Resection of Anterior Skull Base NeoplasmsFemale calmNo ratings yet
- An Epidural Hemorrhage: Anatomy and Key ConceptsDocument14 pagesAn Epidural Hemorrhage: Anatomy and Key Concepts'Danang ヌグロホNo ratings yet
- Cervical Spine CYRIAXDocument16 pagesCervical Spine CYRIAXCarlos TavaresNo ratings yet
- ACNS Surgical Manual PDFDocument248 pagesACNS Surgical Manual PDFKevin EdroNo ratings yet
- Skullbase SurgeryDocument64 pagesSkullbase Surgeryzrated786100% (6)
- Chapter 3 Anatomical Organization of Cranial Nerves 2009 Manual Therapy For The Cranial NervesDocument4 pagesChapter 3 Anatomical Organization of Cranial Nerves 2009 Manual Therapy For The Cranial NervesDaniela Bustos PéndolaNo ratings yet
- Myelography in ChildrenDocument16 pagesMyelography in ChildrenFinna Tryasti Fidianti1BNo ratings yet
- EncehaDocument29 pagesEncehaToko RaMy Line100% (1)
- Ch. 12 & 13 Anaphy Reviewer (Long Quiz)Document12 pagesCh. 12 & 13 Anaphy Reviewer (Long Quiz)googlegirl18No ratings yet
- General Anatomy SyllabusDocument3 pagesGeneral Anatomy SyllabusPatricia patriciaNo ratings yet
- Nanda 2016Document15 pagesNanda 2016Novia AyuNo ratings yet
- Chapter 7 THE MENINGESDocument16 pagesChapter 7 THE MENINGESRoger Fernando Abril DiazNo ratings yet