Professional Documents
Culture Documents
Amat Ncma 219 Pedia Week 5 CT
Uploaded by
Raf AmatOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Amat Ncma 219 Pedia Week 5 CT
Uploaded by
Raf AmatCopyright:
Available Formats
Care of Mother and Child at risk or problem
Unique characteristics of pediatric respiratory system anatomy and physiology and application of
to the care of children with respiratory condition
The pediatric respiratory system is way different from adult respiratory system. The ribs are more
horizontally positioned in infants and young children than in adults and older children, minimizing chest
movement. In infants, the rib cartilage is springy, making the chest wall less rigid. This can cause the
chest wall to retract and reduce tidal volume during respiratory distress episodes. Until a child reaches
school age, the intercostal muscles that run between the ribs are not fully developed. This can make it
difficult to raise the rib cage, especially when the back is flat. Typically, the back of a child's head is
larger than in adults. When a child is lying on his or her back, this may cause the neck to flex and result
in a partially obstructed airway. The internal diameter of a child's airways is smaller. More serious
distress may be caused by any inflammation or obstruction. Pediatric airways in general are smaller,
less rigid, and more susceptible to obstruction. Children also have higher respiratory rate than adults,
making them more susceptible to airborne agents.
Providing care to pediatric clients with respiratory conditions begins with a thorough assessment;
obtaining the child's respiratory status from observation of physical signs and behavior. Auscultation
for lung fields is helpful in identifying pathologic conditions, it is also essential in determining patency
of airways. Palpation and percussion provide information regarding areas of pain and tissue density.
Respiration should also be included in the assessment such as respiratory rate, regularity, symmetry,
depth, effort, and use of accessory muscle when breathing. The care provider must know the normal
values of respirations in the child's age and size. Care provider should take note of retraction, nasal
flaring, head bobbing, noisy breathing, stridor, grunting, wheezing, changes in skin’s color, chest pain,
nail clubbing, and cough. Monitoring the child’s respiratory status with interpreting the blood gasses,
use of pulse oximetry, transcutaneous monitoring, and end-tidal carbon dioxide monitoring is very
essential.
Overall care of a child with respiratory condition requires a lot of skills and gentleness. Their respiratory
system is not yet fully developed. Nurses must use therapeutic communication to the child’s significant
others in order for them to accept the condition of their child. Being their companion in the child’s
health will help in the healing process.
References:
Marilyn J. Hockenberry, D. W. (2019). Wong's Nursing Care of Infants and Children . St. Louis, Missouri:
Elsevier .
Amat, Saimon Rafael T. BSN 2Y2-3s
Care of Mother and Child at risk or problem
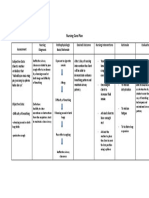
Nursing Care Plan for a 9-year old child with asthma
Assessment Diagnosis Planning and Implementation Evaluation
Goal and objectives Intervention
Subjective data: Ineffective After 15 minutes of nursing After 15 minutes of
airway clearance intervention, the client nursing intervention,
related to maintains airway patency. the client maintains
Objective data: increase sputum airway clearance.
Crackles production as Maintain adequate, Monitor respiration
Wheezes evidenced by patency airway and breath sounds,
Restlessness crackles, noting rate and
Ineffective wheezes, sounds
cough ineffective Rationale: indicative of
Difficulty cough, and respiratory distress and/or
verbalizing difficulty accumulation of secretion.
verbalizing
Evaluate client’s
cough/gag reflex,
amount or type of
secretions, and
swallowing ability
Rationale: to determine
ability to protect own airway
Position head
appropriately for
age and condition
Rationale: to open or
maintain open airway in an
at-rest or compromised
individual.
Insert oral airway
when needed
Rationale: to maintain
anatomical position of
tongue and natural airway,
especially when
tongue/laryngeal edema or
thick secretion may block
airway.
To mobilize Encourage deep-
secretions breathing and
coughing exercise.
Amat, Saimon Rafael T. BSN 2Y2-3s
Care of Mother and Child at risk or problem
Rationale: to maximize
effort
Administer
medication (e.g.,
expectorants, anti-
inflammatory
agents,
bronchodilators,
and mucolytic
agents) as prescribe
by the school
physician
Rationale: to relax smooth
respiratory musculature,
reduce airway edema, and
mobilize secretion.
Promote wellness Call the client’s
guardian
Provide
information about
necessity of raising
and expectorating
secretion versus
swallowing them
Rationale: to report changes
in color and amount in the
event that medical
intervention may be needed
to prevent or treat infection.
Clear the client to
go home from the
school clinic.
References:
Marilynn E. Doenges, M. F. (2019). Nurse's Pocket Guide: Diagnoses, Prioritized Interventions, and
Rationales. Philadelphia, Pennsylvania: F. A. Davis Company.
Amat, Saimon Rafael T. BSN 2Y2-3s
You might also like
- Caplan, Michael J-Reference Module in Biomedical Research-Elsevier (2014) PDFDocument17 pagesCaplan, Michael J-Reference Module in Biomedical Research-Elsevier (2014) PDFMuhammad IkbarNo ratings yet
- Ineffective Breathing Pattern Pneumonia Nursing Care PlanDocument1 pageIneffective Breathing Pattern Pneumonia Nursing Care PlanJasonlee Baluyot100% (2)
- Checklist For Evaluation of Potential Airway & Breathing DisordersDocument7 pagesChecklist For Evaluation of Potential Airway & Breathing DisordersSaran BNo ratings yet
- Guyton & Hall Physio: Chapter 26 Urine Formation by The KidneysDocument66 pagesGuyton & Hall Physio: Chapter 26 Urine Formation by The KidneysMedSchoolStuff90% (21)
- 5 Bronchiolitis Nursing Care Plans - NurseslabsDocument14 pages5 Bronchiolitis Nursing Care Plans - NurseslabsAnnapoorna SHNo ratings yet
- NCP Pedia Ward...Document3 pagesNCP Pedia Ward...Whitney CabanganNo ratings yet
- Pulmo Nursing Care PlanDocument3 pagesPulmo Nursing Care PlanVincent RoyNo ratings yet
- Er NCP AddahDocument2 pagesEr NCP AddahAddah, Dhenaraiza H.No ratings yet
- Lopez, Maria Sofia B. 10/07/2020 3-BSN-B Prof. Zoleta: Nursing Care Plan: PneumoniaDocument9 pagesLopez, Maria Sofia B. 10/07/2020 3-BSN-B Prof. Zoleta: Nursing Care Plan: PneumoniaSofia Lopez100% (2)
- Prioritized Nursing Problem For Pneumothorax Nursing Diagnosis Nursing Intervention RationaleDocument3 pagesPrioritized Nursing Problem For Pneumothorax Nursing Diagnosis Nursing Intervention RationaleJoshua VillarbaNo ratings yet
- NCP TBDocument7 pagesNCP TBLorraine CilloNo ratings yet
- Ineffective Breathing Pattern Pneumonia Nursing Care PlanDocument1 pageIneffective Breathing Pattern Pneumonia Nursing Care PlanJasonlee BaluyotNo ratings yet
- Bukidnon State University: Subjective: Short Term: Short TermDocument1 pageBukidnon State University: Subjective: Short Term: Short TermSimbo Ralph JulesNo ratings yet
- Nursing Care Plan in Pedia Ward: Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationDocument3 pagesNursing Care Plan in Pedia Ward: Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationCharlynne AraojoNo ratings yet
- Nursing Care Plan FinalDocument9 pagesNursing Care Plan FinalJny SthaNo ratings yet
- Assesment Diagnosis Planning Intervention Rationale EvaluationDocument3 pagesAssesment Diagnosis Planning Intervention Rationale EvaluationTrisha Suazo100% (1)
- MSU-Iligan Institute of TechnologyDocument3 pagesMSU-Iligan Institute of TechnologyYuvi Rociandel LUARDONo ratings yet
- Date/ Time/ Shift Cues Need Nursing Diagnosis With Rationale Objectives of Care Nursing Interventions With Rationale EvaluationDocument2 pagesDate/ Time/ Shift Cues Need Nursing Diagnosis With Rationale Objectives of Care Nursing Interventions With Rationale EvaluationPauleen Trisha SamparaniNo ratings yet
- Assessment Planning Nursing Intervention Rationale Evaluation SubjectiveDocument4 pagesAssessment Planning Nursing Intervention Rationale Evaluation SubjectiveChristian Paul Reyes100% (1)
- Group 2 - Activity (NCP, Drug)Document25 pagesGroup 2 - Activity (NCP, Drug)christelNo ratings yet
- FisioterapiarespDocument7 pagesFisioterapiarespArnold Barra100% (1)
- Subjective: Short Independent Intervention: Streptococcus Pneumoniae andDocument1 pageSubjective: Short Independent Intervention: Streptococcus Pneumoniae andKarla SombilloNo ratings yet
- Thoracic and Lung Assessment: College of Nursing and Allied Health Sciences Maasin City, Southern LeyteDocument4 pagesThoracic and Lung Assessment: College of Nursing and Allied Health Sciences Maasin City, Southern LeytePrincess Diana Jean ModesteNo ratings yet
- NCM118RLE SDL1 Almaden PDFDocument3 pagesNCM118RLE SDL1 Almaden PDFclaire yowsNo ratings yet
- General Question: "Ineffective Airway Clearance" in Children With AsthmaDocument3 pagesGeneral Question: "Ineffective Airway Clearance" in Children With AsthmaGil GanibanNo ratings yet
- Case Pres Ncps FinalDocument13 pagesCase Pres Ncps FinalMariejoy YadaoNo ratings yet
- NUR 171 Supportive Educative Nursing Comprehensive Nursing Care PlanDocument13 pagesNUR 171 Supportive Educative Nursing Comprehensive Nursing Care Planapi-354043622No ratings yet
- Nursing Care Plan Name: Group: Group DateDocument5 pagesNursing Care Plan Name: Group: Group DateKen PerezNo ratings yet
- Nursing Care Plan For A Person With Croup Nursing DiagnosisDocument2 pagesNursing Care Plan For A Person With Croup Nursing DiagnosisMonica RiveraNo ratings yet
- Nursing Care Plan For A Person With Croup Nursing DiagnosisDocument2 pagesNursing Care Plan For A Person With Croup Nursing DiagnosisMonica Rivera100% (1)
- Nursing Care Plan Ineffective Airway Clearance: Assessment Diagnosis Outcome IdentificationDocument9 pagesNursing Care Plan Ineffective Airway Clearance: Assessment Diagnosis Outcome IdentificationAngelokeizer GavinoNo ratings yet
- Impaired SwallowingDocument2 pagesImpaired SwallowingfaizaNo ratings yet
- NCP PesebreDocument2 pagesNCP PesebreFrancoise Nicolette PesebreNo ratings yet
- Chronic Obstructive Pulmonary Disease (COPD)Document1 pageChronic Obstructive Pulmonary Disease (COPD)Bheru LalNo ratings yet
- 2 NCP Impaired Swallowing EditedDocument4 pages2 NCP Impaired Swallowing EditedLeonardo Montemayor100% (3)
- Case Scenerio PneumoniaDocument10 pagesCase Scenerio PneumoniaEllen AngelNo ratings yet
- NCP - NewbornDocument1 pageNCP - NewbornChristine Michelle A. BalancadNo ratings yet
- NCP-Ineffective Breathing Pattern-ManaoisDocument2 pagesNCP-Ineffective Breathing Pattern-ManaoisDan Dan ManaoisNo ratings yet
- NCP - Respiratory DistressDocument3 pagesNCP - Respiratory DistressDarwin QuirimitNo ratings yet
- NCP Ineffective Airway Clearance PediaDocument2 pagesNCP Ineffective Airway Clearance PediaFaith CalimlimNo ratings yet
- @acelleisboring - NCP Risk For AspirationDocument6 pages@acelleisboring - NCP Risk For AspirationAngela NeriNo ratings yet
- Nursing Care PlanDocument4 pagesNursing Care PlanKoleen KirstenNo ratings yet
- SecretoDocument2 pagesSecretoKeepItSecretNo ratings yet
- PNNCPDocument2 pagesPNNCPJacky BrightNo ratings yet
- Course Task 3Document1 pageCourse Task 3Jurielyn RiveraNo ratings yet
- Nursing Diagnosis Nursing Intervention Rationale Breathing PatternDocument7 pagesNursing Diagnosis Nursing Intervention Rationale Breathing PatternJinaan MahmudNo ratings yet
- 2 NCP Impaired Swallowing EditedDocument4 pages2 NCP Impaired Swallowing EditedZharm MayNo ratings yet
- Nursing Care Plan: Lorma Colleges Con Template Related Learning ExperienceDocument6 pagesNursing Care Plan: Lorma Colleges Con Template Related Learning ExperiencePauline GarciaNo ratings yet
- NCMB 312 Lec Course Task CU3Document2 pagesNCMB 312 Lec Course Task CU3Mushy_ayaNo ratings yet
- Asthma AssessmentDocument1 pageAsthma AssessmentnarstinesirkNo ratings yet
- NCP1223Document3 pagesNCP1223Divine Mercy De JulianNo ratings yet
- Nursing Care of A Child With Physical AND Developmental ChallengesDocument9 pagesNursing Care of A Child With Physical AND Developmental ChallengesAngelo ArabejoNo ratings yet
- Nursing Care For A High Risk NewbornDocument16 pagesNursing Care For A High Risk NewbornAj MacotoNo ratings yet
- NCPDocument3 pagesNCPAmal MUTIANo ratings yet
- 1 Impaired Gas ExchangeDocument11 pages1 Impaired Gas ExchangeKristian Dave DivaNo ratings yet
- NCP Ineffective Airway ClearanceDocument1 pageNCP Ineffective Airway ClearanceLucky RiusNo ratings yet
- NCP SciDocument3 pagesNCP SciJaylord VerazonNo ratings yet
- HTP Ineffective BreathingDocument3 pagesHTP Ineffective BreathingShyrra Edades PinderNo ratings yet
- The Reliability of The Neonatal Oral-Motor Assessment Scale: KeywordsDocument6 pagesThe Reliability of The Neonatal Oral-Motor Assessment Scale: KeywordsJosé Ignacio SepúlvedaNo ratings yet
- 2015 Dentallib Sridhar Premkumar-148-154Document7 pages2015 Dentallib Sridhar Premkumar-148-154Zhafirah HauraNo ratings yet
- A Multi-Dimensional Model of Dysfunctional BreathiDocument4 pagesA Multi-Dimensional Model of Dysfunctional Breathimari_kundera19No ratings yet
- Lec. 4 Cell InjuryDocument6 pagesLec. 4 Cell InjuryMehdi MohammedNo ratings yet
- SA Exit Block (Andrea Romandini)Document10 pagesSA Exit Block (Andrea Romandini)Swempi Melchiadi AbollaNo ratings yet
- Pengaruh Komunikasi Terapeutik Dan Senam Hamil Terhadap Proses Persalinan Kala I, Ii, Iii, IvDocument8 pagesPengaruh Komunikasi Terapeutik Dan Senam Hamil Terhadap Proses Persalinan Kala I, Ii, Iii, IvlaniNo ratings yet
- Reference Card For Who Emergency Unit Form GeneralDocument2 pagesReference Card For Who Emergency Unit Form GeneralGideon BahuleNo ratings yet
- Australasian Emergency Care: Jeremy Pallas, John-Paul SmilesDocument3 pagesAustralasian Emergency Care: Jeremy Pallas, John-Paul Smileszaenal abidinNo ratings yet
- The Structure of The Nervous SystemDocument4 pagesThe Structure of The Nervous SystemThelNo ratings yet
- Grade 10 - 3rd Quarter BIOLOGY (Key Concepts: Nervous System)Document3 pagesGrade 10 - 3rd Quarter BIOLOGY (Key Concepts: Nervous System)Ionacer Viper100% (3)
- Newborn AdaptationDocument13 pagesNewborn Adaptationrevathidadam55555No ratings yet
- The Nervous System: by - Brett Bennell and Lisa MatzelleDocument27 pagesThe Nervous System: by - Brett Bennell and Lisa MatzelleJames PerianayagamNo ratings yet
- 351255266-Tetanus Id enDocument14 pages351255266-Tetanus Id enRezki IndriyantiyusufNo ratings yet
- Aortic DissectionDocument2 pagesAortic DissectionIka MelaniaNo ratings yet
- MS LAB Oxygenation Nursing SkillsDocument9 pagesMS LAB Oxygenation Nursing SkillsRouwi DesiatcoNo ratings yet
- Cardiotonics & Inotropic Drugs PDFDocument10 pagesCardiotonics & Inotropic Drugs PDFZehra AmirNo ratings yet
- ScienceDocument33 pagesScienceI am JNo ratings yet
- First Aid, Emergency Care, and Disaster ManagementDocument7 pagesFirst Aid, Emergency Care, and Disaster Managementsabrina AliNo ratings yet
- THERMOREGULATION - A Process That Allows Your Body To Maintain Its Core Internal Temperature. AllDocument1 pageTHERMOREGULATION - A Process That Allows Your Body To Maintain Its Core Internal Temperature. AllKeisha BartolataNo ratings yet
- Cellular Work SheetDocument4 pagesCellular Work Sheetlow. PathNo ratings yet
- Maniba Bhula Nursing College: Subject: TopicDocument6 pagesManiba Bhula Nursing College: Subject: TopicRinal BaradNo ratings yet
- ME Sci 9 Q1 0103 PSDocument18 pagesME Sci 9 Q1 0103 PScassiopeia bianca sartigaNo ratings yet
- Physio Xtra Slides Color 2021Document17 pagesPhysio Xtra Slides Color 2021teapalmtreeNo ratings yet
- HypertensionDocument2 pagesHypertensionRodel Yacas0% (1)
- Flashcards - Topic 1.6-1.9 Circulation - Edexcel IAL Biology A-Level PDFDocument78 pagesFlashcards - Topic 1.6-1.9 Circulation - Edexcel IAL Biology A-Level PDFMontaser Abd-al-hamedNo ratings yet
- PULMONOLOGYDocument3 pagesPULMONOLOGYfr.faisal8265No ratings yet
- Oxygen TherapyDocument31 pagesOxygen TherapyChayan BhowmikNo ratings yet
- Pulse Oximetry - UpToDate PDFDocument26 pagesPulse Oximetry - UpToDate PDFLOIDA ESTHER DIAZ MONTESNo ratings yet
- Respiration Course ObjectivesDocument8 pagesRespiration Course Objectivesjoshy220996No ratings yet
- Pham Ngoc Thach University of Medicine DUOC2019Document109 pagesPham Ngoc Thach University of Medicine DUOC2019Nhung PhamNo ratings yet