Professional Documents
Culture Documents
Paper Cuali-Information Sharing Its Impact On Donor Hospital - Payne Sque
Uploaded by
royfockerOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Paper Cuali-Information Sharing Its Impact On Donor Hospital - Payne Sque
Uploaded by
royfockerCopyright:
Available Formats
Information sharing: its impact on donor and
nondonor families’ experiences in the hospital
Objective—To illustrate the methods used to convey complicated information Tracy Long, MSc,
regarding the critical injury, and death diagnosed by means of brainstem testing, Magi Sque, PhD,
to the next of kin of potential organ donors.
Design—3-year, prospective, longitudinal study.
Sheila Payne, PhD
University of Southampton,
Participants and Setting—Forty-three family members who chose to donate their Southampton, United Kingdom
deceased relatives’ organs were recruited via 4 transplant coordinating centers, and (TL, MS), University of Sheffield,
3 family members who chose not to donate were recruited via 1 intensive care unit. Sheffield, United Kingdom (SP)
Method—Face-to-face qualitative interviews were carried out with 46 family
members of 43 individuals who died between June and December 2000. Family To purchase electronic or print reprints,
members who agreed to donation were interviewed during and after their next of contact:
kin’s admission to hospital and 3 to 5 months, 13 to 15 months, and 18 to 26 months The InnoVision Group
after bereavement. Three participants who chose not to donate were interviewed 101 Columbia, Aliso Viejo, CA 92656
Phone (800) 809-2273 (ext 532) or
on 1 occasion only. Interviews were audio-recorded, and the transcribed reports
(949) 448-7370 (ext 532)
were analyzed using a comparative, thematic approach focusing on the detection
Fax (949) 362-2049
of similarities and differences between cases. E-mail reprints@aacn.org
Results—Participants who were offered verbal information supported by comple-
mentary methods of communication had (1) a greater understanding of the critical
injury sustained by their next of kin, and (2) fewer questions over time regarding
brainstem testing.
Conclusion—Better methods of communicating complicated information are
needed, as the sheer load of information shared makes demands of next of kin at a
time when they are cognitively and emotionally poorly equipped to respond.
(Progress in Transplantation. 2006;16:144-149)
T he often sudden and unexpected death of a poten-
tial organ donor coupled with the complexities of
synthesizing information related to the injury causing
live-looking body with the diagnosis of brainstem
death can be difficult for family members to accept, as
brainstem death has been described as a nonstereotyp-
death, and to death certified by brainstem testing (as ical death.5 Despite the complexities inherent in both
takes place in the United Kingdom), is a complex and sudden death and brainstem testing, little research has
demanding situation for all involved.1 Brainstem test- been done to investigate the informational needs of
ing is carried out to confirm cessation of all brainstem family members who are approached about organ
functions and is required to certify death on neurolog- donation, and whether the method in which that infor-
ical grounds.2 Patients who have sustained irreversible mation is conveyed affects their experience of the
damage to the vital centers in the brainstem have per- approach and request for organ donation. Of the
manently lost the capacity to think, to be aware of them- research that has addressed issues related to family
selves and their surroundings, or to experience or members’ experiences,1,6-14 little is reported on how
communicate with others.3 In the United Kingdom, family members of potential organ donors perceive
death diagnosed by brainstem testing is defined as information-sharing methods or what their preferences
“the irreversible loss of the capacity for consciousness are in regard to this.5,9,11,14,15
combined with the irreversible loss of the capacity to As part of a longitudinal study exploring factors
breathe.”4 This medical diagnosis is presented to fam- influencing family members’ decision-making and
ilies who are faced with the reality of a body that is bereavement needs, we gained information related to
warm and pink, that has a pulse and a chest that rises relatives’ experiences of information sharing and organ
and falls. The incongruity of an externally intact and donation.
144 Progress in Transplantation, Vol 16, No. 2, June 2006
Impact of information sharing on families’ experiences in the hospital
Aims views of the participant and extended family members
In this article, we present data that highlights and regarding organ donation, (5) what needs the partici-
illustrates (1) what methods of information sharing pants identified during their visits and after they had
related to the critical injury were most helpful to rela- left the hospital, and (6) their aftercare, follow-up, and
tives of potential organ donors, (2) how death certified bereavement.
by brainstem testing was communicated, and (3) the All interviews (except for 1 interview at TP1 and
influence of sudden death as an obstacle to informa- 1 at TP2 done at the participant’s place of work) were
tion sharing. The findings contribute to understanding carried out in the participant’s home. Interviews at
how best to support families at this difficult time and TP1 lasted between 2 and 4 hours, with subsequent
how to enable them to make informed decisions about interviews at TP2 and TP3 lasting approximately 1.5
organ donation. hours. The interviews were audio-recorded. Concise,
reflective field notes were written after each interview
Method to note important points and to detail the context of the
Design and Method interview, the dynamics of the interaction, and any
Data presented here were collected as part of a 3- analytical or methodological issues for discussion by
year, longitudinal study exploring the experiences of the research team. These field notes also served to aid
bereaved adults with whom organ and tissue donation researcher reflexivity and to guide judgments and
had been discussed.5 The study used both quantitative decisions made regarding the research process.
and qualitative components, but only data from the in- Interview data were transcribed verbatim, and
depth interviews, the qualitative component, are pre- both text and recording were reviewed several times
sented here. Ethical approval for the study was given by until familiarity with the data was established. The
the South East Multi Centre Research Ethics Committee. transcribed reports were analyzed by using a compar-
ative, thematic approach focusing on the detection of
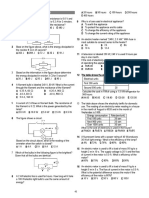
Participants similarities and differences between cases. Analysis
The next of kin of 43 individuals who died was guided by the aims of the research, with themes
between June and December 2000 were asked to par- being noted in memos, which with other field notes
ticipate in qualitative, semistructured, face-to-face, formed a preliminary analysis of the data. Thus by the
serial interviews on 3 occasions during a 24-month end of each interviewing sequence, a sound knowl-
period (Table 1). All donating family members were edge of the salient issues for participants had been
recruited via 4 transplant coordinating services in the accrued. A qualitative software program (HyperRe-
United Kingdom who sent out recruitment packs to search 2.2.3, ResearchWare Inc, Randolf, Mass) facil-
the next of kin. Families who declined donation were itated working with the data set during analysis.
recruited via 1 intensive care unit (ICU), although Three of 12 themes generated from analysis that
10 ICUs had agreed to participate in recruitment. relate to the aims of this article are expanded within
Forty-six family members who chose to donate the following sections and supported by quotes from
their deceased relative’s organs were interviewed at 3 the transcripts. In relation to the use of quotes, single
to 5 months (time point 1, TP1); of these, 44 were quotation marks are used to highlight ‘in-vivo’17 terms
interviewed at 13 to 15 months (TP2), decreasing to or words used by participants, whereas double quota-
38 being interviewed at 18 to 26 months (TP3) after tion marks indicate specific quotes made by partici-
bereavement. Three participants who chose not to pants and are evidence used to ground the findings in
donate their deceased relatives’ organs were inter- the experiences of the participants.
viewed on 1 occasion only at approximately 13 months
after bereavement (Table 1). Results
Theme 1: Information Related to the Critical Injury
Data Collection and Analysis Participants were given verbally what they viewed
An interview guide was developed from previous as complicated information about the nature of the
work16 and available literature. The interview guide brain injury. Most participants had little previous
consisted of questions about (1) the attributes of the knowledge of brain anatomy or function, and there-
deceased, his or her relationship to the participant, and fore the dependence on verbal information left most
what role he or she had played in the family, (2) how participants struggling to understand what the injury
the person being interviewed found out about the crit- meant in relation to their relative. When more visual
ical injury and the events that followed, (3) the partic- means of explaining the nature of the brain injury
ipant’s view of the care provided to their family member, were used, families’ understanding of the injury was
themselves, and other relatives, including information greater than the understanding among next of kin who
sharing regarding the critical injury, the diagnosis of did not receive such visual explanations. These meth-
death, and the approach about organ donation, (4) the ods included the following:
Progress in Transplantation, Vol 16, No. 2, June 2006 145
Long et al
Table 1 Demographic data for participants and donors
Age of partici-
pant, years Relationship Age of donor, Completed
Participant to donor years Critical injury interviews
71
1 47 Husband 65 Subarachnoid hemorrhage 3
2 39 Partner 48 Subarachnoid hemorrhage 3
3 55 Mother 21 Motor vehicle crash 2
4 36 Wife 59 Brainstem bleeding 3
5 Both 57 Daughter 59 Brainstem bleeding 1
6 53 Mother/Father 23 Motor vehicle crash 3
7 47 Wife 40 Motor vehicle crash 3
8 44 Wife 52 Brain hemorrhage 3
9 51 Mother 23 Motor vehicle crash 3
10 52 Husband 48 Brainstem bleeding 3
11 50 Husband 50 Brain hemorrhage 3
12 31 Wife 57 Brain hemorrhage 3
13 70 Mother 11 Brain hemorrhage 3
14 50 Wife 70 Brain hemorrhage 3
15 31 Husband 45 Brain hemorrhage 3
16 40 Wife 41 Brain hemorrhage 3
17 24 Sister 37 Brain hemorrhage 3
18 52 Son 40 Brain hemorrhage 3
19 45 Wife 53 Brain hemorrhage 3
20 51 Husband 42 Brain hemorrhage 2
21 52/50 Cousin 42 Brain hemorrhage 3
22 74/71 Parents 21 Motor vehicle crash 3
23 52 Parents 43 Brain hemorrhage 3
24 54 Wife 54 Brain hemorrhage 3
25 Husband 48 Brain hemorrhage 1
40
26 Husband 38 Brain hemorrhage 3
71
27 Mother 44 Brain hemorrhage 3
46/48
28 Parents 23 Brain hemorrhage 2
50
29 Husband 52 Brain hemorrhage 3
56
30 Mother 30 Brain hemorrhage 3
50
31 Husband 50 Brain hemorrhage 3
61/64
32 Parents 29 Brain hemorrhage 3
42
33 Mother 17 Motor vehicle crash 3
28
34 Partner/Father 26/2 Motor vehicle crash 2
73
35 Father 34 Brain hemorrhage 3
42
36 Wife 50 Heart attack 2
20
37 Daughter 45 Heart attack 3
52
38 Mother 18 Head injury 3
46
39 Husband 46 Brain hemorrhage 3
52
40 Mother 34 Brain hemorrhage 3
42
41 Son 72 Brain hemorrhage 3
32 Nondonor
42 45/46 Daughter 50 Brain hemorrhage 1
43 Parents 17 Postoperative complications 1
• Being shown computed tomography (CT) scans • The use of an anatomical model of the brain to
and radiographs. “He [doctor] showed us the brain indicate the area of injury, the damage caused, and the
scan . . . which was just amazing, all this black.” consequences of the damage. “He [doctor] brought in
146 Progress in Transplantation, Vol 16, No. 2, June 2006
Impact of information sharing on families’ experiences in the hospital
a model of the brain with removable bits, which he Table 2 Methods used to communicate complicated infor-
took apart and showed us which bit was affected. That mation regarding the critical brain injury
really put us in the picture!”
How method was
• Being present when brainstem testing was carried The method perceived to help
out. “He [doctor] was absolutely brilliant. He said he
Talking Responsive
had one set of tests and they had done the scan, which
showed that there wasn’t anything that could be done, Seeing computed tomography Confirmatory
scans
and so after a period of time, I don’t know how long it
was, hours, he was going to do another set of tests, and Seeing radiographs Illustrative
he said we could be in there to see them if we wanted to Use of anatomical models Explanatory
or not, and I think we were probably the only people Witnessing brainstem testing Confirmatory
who ever said we wanted to be there, but from our point Reading and sharing information Informative and stimu-
of view I wanted to see what they were doing to him and leaflets lating discussion
I wanted to be sure that he was really dead.”
• Being given a leaflet that explained the possible about how brain injury leads to the ‘loss of personal-
consequences of different kinds of brain injury and the ity,’ which was often cited as being the result of the
type of questions frequently asked by families in this brain injury, and questions about what the tests were
situation. “The trouble is, at that time, you can’t think designed to show. Importantly, most of the partici-
of any [questions to ask].” pants in this study made decisions about organ dona-
In interviews at TP1, participants who had expe- tion without gaining an understanding of death certified
rienced any of these complementary methods of com- by brainstem testing. This pattern appeared to be due,
municating complicated information were asked in in part, to their motivation to have the wishes of the
what way this method assisted their understanding. deceased fulfilled (the deceased had indicated by
Their views are reflected in the preceding quotes and donor card, driver’s license, passport, or discussion
are summarized in Table 2. that they wished their organs to be donated). This
The findings for those families who did not emotional need, to have the wishes of their family mem-
donate were limited because of the small sample size, ber met, appeared to override their own informational
but those families were dissatisfied with the amount of needs at the time of approach and request for organ
information provided to them during their hospital stay. donation, but left them with questions during their
None of the complementary methods of communicat- subsequent bereavement. A further consideration in
ing the complicated information regarding the nature relation to brainstem testing is the terminology that is
of the brain injury sustained by their relative had been used by health professionals. ‘Being kept alive on the
offered to them, nor had they been offered easy access ventilator,’ ‘life support,’ and the term ‘brainstem death’
to medical staff who could have provided explana- all suggest that death certified by brainstem testing is
tions. This failure resulted in 1 family accessing med- inclusive of the brain and exclusive of the body. This
ical textbooks to gain the information they felt they terminology can support the view that the family
needed. These participants also felt that they had not member could recover with intensive rehabilitation.
been given sufficient opportunity to ask questions. In view of the findings from participants who
wanted to observe brainstem testing, a question was
Theme 2: Communication About Brainstem Death added to the interview schedule for TP2, which asked
Four participants were asked if they wanted to be participants whether they would have wanted to watch
present when brainstem testing was carried out. All brainstem testing being carried out. All participants
other participants were given limited information about felt that they would have liked to have been asked if
brainstem testing (see shaded box), and none had a they wanted to watch the tests or if a member of their
clear understanding of what would happen during tests. family could watch on their behalf. Most participants
During interviews at all time points, participants were unsure as to whether they would or would not
raised questions related to brainstem testing, questions have viewed brainstem tests being carried out. Five
participants said they would have attended brainstem
A father explains how health professionals introduced the testing if they had been offered this opportunity because
procedure of brainstem testing to him: they were seeking confirmation of death.
A suggestion by 2 participants was that they
“and she [transplant coordinator] went through the proce-
dure that the consultant and the doc, the surgeon have to thought that a video or DVD of the testing process,
do this stem test and then they do it again, an hour later. which they could watch with other family members,
And if there is nothing, then he is declared stem dead, may have helped discredit issues related to coma that
which I presume, I mean, I never got up to the point were raised by extended family members: “Well I
where I could, basically he’s declared dead I presume.”
heard you can wake up after 2 years in a coma.”
Progress in Transplantation, Vol 16, No. 2, June 2006 147
Long et al
Theme 3: Internal Dialogue and A mother speaking about her teenage son:
Information Synthesis
The emotional turmoil that participants experi- “And I was just thinking positively you’re going to wake up in
a minute and be normal so I wasn’t really giving those
enced at the suddenness of the collapse of their family things [brainstem testing] any thought. Certainly not about
member had an impact on information processing and him dying, no I didn’t really suppose, I wasn’t accepting it.
accessing that information at a later time. Families As I say I was going through the formalities of everything,
needed time to absorb the complexity of the informa- playing along with it but not really…”
tion that was given to them about the critical injury and
death. Time was an issue in some cases, as the interval Discussion
between admission to the emergency department and The results from each time point illustrate families’
diagnosis of death was as short as 3 to 6 hours. needs in relation to the content and manner in which
An obstacle to information processing was the information could be best delivered, as well as the obsta-
emotional mindset of participants and the amount of cles to processing this information by the effects of sud-
time they spent in a form of ‘internal dialogue’ (see den injury and the, albeit necessarily so, complicated
shaded box). This internal dialogue comprised ‘recall- information related to brainstem testing and death.
ing’ the deceased and their life spent together, the The need for accurate, understandable, and con-
minute detail of the last conversation held with their sistent information regarding the course of illness in
family member, ‘hoping’ for survival, and ‘bargain- relation to organ donation has been reported8,9,11,13,15 and
ing with God.’ These ruminations acted as ‘pull factors,’ is the most commonly identified need for family
drawing the family member away from the informa- members in the ICU.18-20 Fulfilling the informational
tional flow around them. As the time in the hospital needs of family members reduces anxiety, especially
exended, the internal dialogue and ruminations changed if more than 1 channel of communication is used to
and were influenced by ‘push factors’ such as thoughts transmit the desired information,20 and yet the need for
of brain damage and death, which focused family information has been reported as one of the most
members on the informational flow available to them poorly met needs within the ICU.21 A number of fac-
and triggered some to become extra vigilant of moni- tors appear to be relevant to this poorly met need: the
toring equipment and to seek ‘repeated reassurances’ methods used to transmit information, the content of
from medical and nursing staff. the information, the state of mind of the person receiv-
Dissonance was clearly articulated by partic- ing the information, and the nature of the critical injury
ipants as they learned the extent of the brain damage and diagnosis of death. In relation to the means by
and recalled their family member’s expressed view of which information regarding organ donation is shared,
not wanting to survive with brain damage. Participants Sque et al15 have indicated how sudden death and
hoped for what were increasingly mutually exclusive the discussions about organ donation make specific
outcomes: for their family member to live, but not be demands of the next of kin at a time when they are emo-
profoundly brain damaged. This internal conflict was tionally and cognitively poorly equipped to respond.
happening at a time when participants were attending Dissatisfaction with information regarding brain-
to (or attempting to attend to) the information being stem death received during the approach and request
offered to them about the nature of the brain injury, for organ donation has been reported.5,8,9,11 In a survey
the carrying out of brainstem tests, and the diagnosis exploring the care offered to families and the ade-
of death. Sudden death not only robbed participants of quacy of the information provided to them during the
a significant relationship, but also robbed them of approach and request for organ donation, Pearson et
many of their usual coping mechanisms, imposing a al9 found that 36% of the 69 next of kin in their sam-
sequence of events that left participants feeling dis- ple felt confused because of insufficient information
possessed of physical and psychological equilibrium. and the use of overtly complex medical terminology.
Evidence in interviews at TP1 indicates that par- Participants said that they would have liked methods
ticipants who were with their family member at the such as radiographs, diagrams, models, or pictures used
time of the critical injury were sensitized to the possi- to explain the patient’s brain injury, and 55% would
bility of death as they reported less ‘hope’ of their have liked these methods used specifically in relation
family member’s survival and had a greater expecta- to brain death because 20% felt that this topic was
tion of being told ‘bad news.’ Those participants who poorly explained. Pearson et al found that next of kin
were not with their family members at the time of the wished to have information shared with them, a result
critical injury expressed more ‘hope’ of survival and supported by our findings, but uniquely, we suggest
took longer to recognize the inevitability of death. that the use of visual aids in the discussion surround-
Being present at the critical injury may be an indica- ing the critical injury and the diagnosis of death by
tor of how quickly information related to the progno- brainstem testing could (1) increase understanding of
sis can be presented to a family member. the nature of the brain injury, (2) increase feelings of
148 Progress in Transplantation, Vol 16, No. 2, June 2006
Impact of information sharing on families’ experiences in the hospital
confidence in any decision that is made in response to Acknowledgment
brainstem testing, and (3) reduce the amount of fanta- The research was commissioned by the British Organ
sizing after the death about the nature of coma, as the Donor Society and funded by a grant from the UK Commu-
understanding of those participants who had experi- nity Fund to the chief investigator, Magi Sque.
enced complementary methods of information sharing
was more detailed than the understanding among those References
1. Sanner M. Attitudes toward organ donation and transplanta-
who had not received information supported by visual tion. Soc Sci Med. 1995;38:1141-1152.
aids. Also those participants who had received infor- 2. Powner DJ, Darby JM. Current considerations in the issue of
mation supported by visual aids (1) had fewer questions brain death. Neurosurgery. 1999;45:1222-1226.
3. Sullivan J, Seem DL, Chabalewski F. Determining brain
about the nature of the brain injury during interviews death. Crit Care Nurse. April 1999;19:37-45.
carried out at all time points, (2) stated that they felt 4. Criteria for the diagnosis of brainstem death. Review by a
involved in what was happening, and (3) expressed working group convened by the Royal College of Physicians
and endorsed by the Conference of Medical Royal Colleges
feelings of being fully informed. and their Faculties in the United Kingdom. J R Coll Physi-
When consideration is given to the time and train- cians Lond. 1995;29:381-382.
ing it takes for health professionals to feel confident in 5. Sque M, Long T, Payne S. Organ and tissue donation:
Exploring the needs of families. Final report of a three-year
their understanding of death certified by brainstem test- study commissioned by the British Organ Donor Society,
ing, it seems unreasonable to expect family members, funded by the Community Fund; February 2003. Available
even those with some medical background, to under- at: http://body.orpheusweb.co.uk/Report.html. Accessed
April 24, 2006.
stand and accept this diagnosis in what is often a very 6. Nielson G, Brandt MR. Attitude to the criteria of death and
short time span from admission to brainstem assess- kidney transplantation of the relatives of kidney donors [in
ment (in the past it was usual to wait 24 hours before Danish]. Ugeskr Laeger. 1990;152:806-809.
7. Tymstra T, Heyink JW, Pruim J, Slooff MJ. Experience of
beginning brainstem assessment, R. Hodge, personal bereaved relatives who granted or refused permission for
communication, 2005). The fact that most participants organ donation. Fam Pract. 1992;9:141-144.
were still unclear about what brainstem tests were, and 8. Pelletier M. The organ donor family members’ perception of
stressful situations during the organ donation experience. J
how these tests related to the death of their family Adv Nurs. 1992;17:90-97.
member, at 2 years after bereavement, is testimony to 9. Pearson IY, Bazeley P, Spencer-Plane T, Chapman JR, Robert-
the need for a change of practice in this area. son P. A survey of families of brain dead patients: their experi-
ences, attitudes to organ donation and transplantation. Anaesth
Intensive Care. 1995;23:88-95.
Conclusion 10. Sque M, Payne S. Dissonant loss: the experience of donor
The role of the type and method of information relatives. Soc Sci Med. 1996;43:1359-1370.
11. Franz HG, Dejong W, Wolfe SM, et al. Explaining brain death:
sharing in the hospital is only one of the factors that a critical feature of the donation process. J Transplant Coord.
affects the experiences of family members who are 1997;7:14-20.
approached regarding organ donation, but that factor 12. Verble M, Worth J. Fears and concerns expressed by families
in the donation discussion. Prog Transplant. 2000;10:48-53.
may be far more important than previously realized. 13. Sque M. Being a carer in acute crisis: the situation for rela-
Relatives of potential organ donors are the most criti- tives of organ donors. In: Payne S, Ellis-Hill C, eds. Chronic
cal link in maintaining organ availability, because and Terminal Illness: New Perspectives on Caring and Car-
ers. Oxford: Oxford University Press; 2001:101-122.
they must express their lack of objection before organ 14. Haddow G. Donor and nondonor families’ accounts of com-
retrieval can take place. The choice that family mem- munication and relations with health care professionals. Prog
bers make regarding organ donation may be influenced Transplant. 2004;14:41-48.
15. Sque M, Long T, Payne S. Organ donation: key factors influ-
by the quality of, and the methods used to convey, encing families’ decision-making. Transplant Proc. 2005;
information regarding the nature of the critical injury, 37:543-546.
and death certified by brainstem testing, due to the 16. Sque M. The Experiences of Donor Relatives, and Nurses’
Attitudes, Knowledge and Behaviour Regarding Cadaveric
sheer amount of information that is passed on to them. Donor Transplantation [dissertation]. Southampton, UK:
If better information-sharing techniques (like those out- University of Southampton; 1996.
lined in this article) are used, families can be helped to 17. Strauss A, Corbin J. Basics of Qualitative Research. New-
bury Park, Calif: Sage Publications; 1998.
make informed decisions about organ donation with 18. Hickey ML, Leske JS. Needs of families of critically ill
which they are comfortable and remain confident patients: state of the science and future directions. Crit Care
in. Finally, further ethnographic studies are needed Nurse. August 1992;4:645-649.
19. Lorenz BT. Needs of family members of critically ill adults.
that facilitate the prospective exploration of the infor- Medsurg Nurs. 1995;4:445-451.
mation culture of ICUs and emergency departments.22 20. Zazpe C, Margall MA, Otano C, Perochena MP, Asiain MC.
Studies of this nature offer the opportunity to observe Meeting needs of family members of critically ill patients in a
Spanish intensive care unit. Intensive Crit Care Nurs. 1997;
information sharing and the interaction between 13:12-16.
health professionals and families and to further expli- 21. Barbret LC, Westphal CG, Daly GA. Meeting information
cate the role that information sharing regarding the needs of families of critical care patients. J Healthc Qual.
March-April 1997;19:5-9.
critical injury and death of a potential organ donor 22. Seymour JE. Critical Moments: Death and Dying in Intensive
plays in decision making and grief. Care. Buckingham, UK: Open University Press; 2001.
Progress in Transplantation, Vol 16, No. 2, June 2006 149
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5796)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- ISX15 E5 4954042 Wiring Diagram Rev 4Document3 pagesISX15 E5 4954042 Wiring Diagram Rev 4刘sir82% (17)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- CIGRE Brochure348Document114 pagesCIGRE Brochure348christiansasso100% (5)
- Ethical TheoriesDocument18 pagesEthical TheoriesKlyde EvangelistaNo ratings yet
- Dissonant Loss: The Experiences of Donor Relatives: Social Science & Medicine December 1996Document13 pagesDissonant Loss: The Experiences of Donor Relatives: Social Science & Medicine December 1996royfockerNo ratings yet
- What Makes Protest Powerful? Reintroducing and Elaborating Charles Tilly'S Wunc ConceptDocument24 pagesWhat Makes Protest Powerful? Reintroducing and Elaborating Charles Tilly'S Wunc ConceptroyfockerNo ratings yet
- Qualitative Text AnalysisDocument5 pagesQualitative Text AnalysisroyfockerNo ratings yet
- The Statistics of Causal Inference: A View From Political MethodologyDocument23 pagesThe Statistics of Causal Inference: A View From Political MethodologyroyfockerNo ratings yet
- Essential Skills and Qualities of A Successful AcademicDocument7 pagesEssential Skills and Qualities of A Successful AcademicMagda GacparskaNo ratings yet
- Energía Solar La Creciente Solución Solar en Las Zonas Rurales de América LatinaDocument3 pagesEnergía Solar La Creciente Solución Solar en Las Zonas Rurales de América LatinawilderNo ratings yet
- Andrea Janine Lucina M4W4 Media and Information SourcesDocument3 pagesAndrea Janine Lucina M4W4 Media and Information SourcesJomein Aubrey BelmonteNo ratings yet
- Sample Fees Calculation Sheet For Mixed ProjectDocument6 pagesSample Fees Calculation Sheet For Mixed Projectssmorthy8053No ratings yet
- Super Star Group: Subject: Work Order For Supply of Switch With Box SingleDocument29 pagesSuper Star Group: Subject: Work Order For Supply of Switch With Box SingleAntora HoqueNo ratings yet
- V7 Host Implementation Guide v2.0.6 - LiquorDocument54 pagesV7 Host Implementation Guide v2.0.6 - LiquorShubham Namdev100% (1)
- Mayer+empl: Architectural Space InterventionDocument55 pagesMayer+empl: Architectural Space InterventionQuirin EmplNo ratings yet
- Program ATP EMTP in Overvoltage EducationDocument4 pagesProgram ATP EMTP in Overvoltage Educationrodrigoct88No ratings yet
- 4 - Classical Management 2Document64 pages4 - Classical Management 2Prof. Maseera PatelNo ratings yet
- Emotional Intelligence ExerciseDocument8 pagesEmotional Intelligence Exercisem.syedNo ratings yet
- Internal - External ReportsDocument2 pagesInternal - External ReportsSarahCariagaNo ratings yet
- Stevenson Hinde2007Document7 pagesStevenson Hinde2007Fuel45No ratings yet
- AI For Decision Making Wharton 10722Document18 pagesAI For Decision Making Wharton 10722Pra RNo ratings yet
- Ds AutoCADDocument2 pagesDs AutoCADfl_in1No ratings yet
- 04 Unit 03 Procedure-KCDocument19 pages04 Unit 03 Procedure-KCfitriNo ratings yet
- Xy-lanh-dien-loai-truot-SMC-LEFS-Series 29012018105735 PDFDocument183 pagesXy-lanh-dien-loai-truot-SMC-LEFS-Series 29012018105735 PDFĐặng HoàngNo ratings yet
- Practical Research RRLDocument6 pagesPractical Research RRLtriciaprivate000No ratings yet
- Monarch TT 30Document4 pagesMonarch TT 30Migue ToasaNo ratings yet
- Physics! Unit 03 MTM Packet 2013Document8 pagesPhysics! Unit 03 MTM Packet 2013Kelly O'SheaNo ratings yet
- Hi Focus f152 HBDocument4 pagesHi Focus f152 HBAna Bogdanovic GagiNo ratings yet
- JRVelasco - Lesson 21, Art AppreciationDocument4 pagesJRVelasco - Lesson 21, Art AppreciationJon Ruemer Pontawe VelascoNo ratings yet
- Lloyd'S Register Integrated Fatigue Design: Assessment SystemDocument17 pagesLloyd'S Register Integrated Fatigue Design: Assessment SystemAna TNo ratings yet
- Markets and DestinationDocument55 pagesMarkets and DestinationJorim Sumangid100% (1)
- Tutorial 7.5Document2 pagesTutorial 7.5sidNo ratings yet
- Uniaxial Loading: Design For Strength, Stiffness, and Stress ConcentrationsDocument11 pagesUniaxial Loading: Design For Strength, Stiffness, and Stress ConcentrationsDanishIqbalNo ratings yet
- The ABC's of Interviewing: A Is For AttitudeDocument5 pagesThe ABC's of Interviewing: A Is For AttitudeSnehal PatilNo ratings yet
- Group 14 Monitoring SystemDocument27 pagesGroup 14 Monitoring SystemAndrei 26No ratings yet