Professional Documents
Culture Documents
Blunt Ocular Trauma A Rare Cause of Caroticocavernous Fistula 2168 9784 1000221
Uploaded by
mithaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Blunt Ocular Trauma A Rare Cause of Caroticocavernous Fistula 2168 9784 1000221
Uploaded by
mithaCopyright:
Available Formats
Di
ical agno
ed
Journal of Medical Diagnostic
st
urnal of M
ic M ods Methods
eth
Rastogi et al., J Med Diagn Meth 2016, 5:3
Jo
ISSN: 2168-9784
DOI :10.4172/2168-9784.1000221
Case Report Open Access
Blunt Ocular Trauma - A Rare Cause of Carotico-Cavernous Fistula
Rajul Rastogi*, Asif Majid Wani, Pawan Joon, Yuktika Gupta, Shourya Sharma, Pankaj Kumar Das and Vijai Pratap Singh
Teerthanker Mahaveer Medical College and Research Center, Moradabad, Uttar Pradesh, India
*Corresponding author: Rajul Rastogi, MD Radiodiagnosis, ADND, MIMSA, FIMSA, FICRI, Teerthanker Mahaveer Medical College and Research Center, Moradabad -
244001, U.P, India, Tel: 919319942162; E-mail: eesharastogi@gmail.com
Received date: Jun 29, 2016; Accepted date: Jul 25, 2016; Published date: Aug 3, 2016
Copyright: © 2016 Rajul R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted
use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Carotico-cavernous fistula (CCF) is a rare entity referring to abnormal communication between cavernous sinus
and carotid arterial system (either internal or external or both) directly or through their branches. Though majority of
cases have been reported secondary to head trauma yet spontaneous cases have also been described. We present
an interesting case of CCF that developed secondary to blunt ocular trauma not yet described in the medical
literature.
Keywords: Cavernous; Carotid; Ocular; Trauma stranding in intraconal and extraconal orbital fat without obvious signs
of any obvious mass lesion. Contrast-enhanced images with MRA
Introduction revealed enlarged cavernous sinus; dilated superior and inferior
ophthalmic veins with their draining tributaries and multiple, tiny,
Carotico-cavernous fistula (CCF) is a rare arteriovenous dilated arteries within the early enhancing left cavernous sinus. No
malformation involving the cavernous sinus and either internal or evidence of any obvious dilatation of right orbital or intercavernous
external carotid artery or both or their branches. It may be further veins or aneurysm was noted. Based on imaging findings, diagnosis of
classified in to direct or indirect types based on presence or absence of carotico-cavernous fistula (type B) was made which is rarer than other
direct communication with intra-cavernous part of internal carotid types.
artery (ICA). Direct CCF is secondary to aneurysmal rupture of ICA
or closed head trauma involving base of skull, hence commoner in Patient was then immediately referred to higher neuro-
young male working outdoors with usually acute presentation while interventional centre for further management.
indirect CCF is usually spontaneous occurring in elderly especially
postmenopausal females following a more indolent course than direct Discussion
type [1]. Though ocular trauma is also commonly seen in day-to-day
CCF is an abnormal communication between the carotid arterial
practice yet it has not been described as a cause of CCF. In this article,
system and the cavernous sinus. Barrow classification of CCF is as
we are describing a rare case of CCF that developed secondary to
follows [2]:
ocular trauma with its pathogenesis.
Type A: direct connection from cavernous ICA
Case Report Type B: connection from meningeal branches of ICA
A 36 yr-old female presented with pulsating headache and proptosis Type C: connection from meningeal branches of ECA
of left eye during last few days. History taking revealed blunt injury to
left eye by an umbrella-stick 3-4 months back that gave rise to severe Type D: connection from meningeal branches of ICA and ECA
and sudden orbital pain with reduced visual acuity in left eye. Since Type A CCF is commonest (~75%) and is high-flow fistula while
then she was having reddening of eyes and orbital swelling. She took Type B, C and D CCFs are low-flow fistulae with Type C being
local treatment for the same for few weeks without any imaging commoner.
investigation during which her eyelid swelling subsided and visual
acuity slightly improved but reddening of eyes increased. During last CCF leads to increase pressure in cavernous and communicating
few weeks she felt that her left eye is protruding out with limitations of sinuses leading to alteration of flow direction/drainage with
ocular movements. consequent symptoms [3]. Commonest cause of Type A is head trauma
or rupture of cavernous ICA aneurysm [2,4]. Etiology of Types B, C
Clinical examination revealed chemosis, increased intraocular and D (dural CCFs) is unclear with postulated mechanism being
pressure, mild external ophthalmoplegia and mild 6th cranial nerve tearing of small meningeal vessels with or without thrombosis leading
palsy with normal fundoscopic examination. No local bruit was noted. to neovascularization and fistula formation. Miscellaneous causes
Laboratory examinations including complete blood counts and thyroid include abnormal arteries as in Ehlers-Danlos syndrome,
functions test were unremarkable. pseudoxanthoma elasticum, fibromuscular dysplasia, etc. and
Magnetic resonance imaging (MRI) brain and orbits was then hypercoagulable states as PT mutations, pregnancy, etc.
advised for further evaluation of cause of proptosis. Noncontrast MRI However, none of the previously reported cases have preceded
revealed enlarged left cavernous sinus with multiple flow voids and ocular trauma as seen in our index case. The postulated mechanism is
dilated superior and inferior ophthalmic veins with soft tissue
J Med Diagn Meth Volume 5 • Issue 3 • 1000221
ISSN:2168-9784 JMDM, an open access journal
Citation: Rastogi R, Wani AM, Joon P, Gupta Y, Sharma S, et al. (2016) Blunt Ocular Trauma - A Rare Cause of Carotico-Cavernous Fistula. J
Med Diagn Meth 5: 221. doi:10.4172/2168-9784.1000221
Page 2 of 3
that blunt ocular trauma probably lead to sudden and significant congestion or complications of CCF as described above. Thrombi may
increase in intraocular pressure that was transmitted through be seen as filling defects in the cavernous sinus.
ophthalmic veins to the cavernous sinus leading to tear of small
They have lower sensitivity for types B to D than with Type A. CTA
meningeal vessels leading to fistulous arteriovenous communication
is optimal for Type A while MRA is superior in Type B, C and D and in
between the meningeal branches of ICA and cavernous sinus.
demonstrating venous channels which are very important in predicting
Clinical presentation is usually pulsatile exophthalmos, chemosis prognosis and optimal method of management [7,8].
with or without subconjunctival hemorrhage, proptosis, progressive
True FISP imaging, susceptibility weighted, High-Resolution Time-
visual loss, pulsatile tinnitus, signs of raised intracranial pressure and
Resolved MR-Angiography with Stochastic Trajectories (TWIST) and
complications of CCF like subarachnoid or intracerebral bleed,
Extended Parallel Acquisition Technique (ePAT 6) sequences have
otorrhagia or epistaxis [3-6] (Figure 1).
been reported to be quite useful in MRA [9-11]. Early CCF may even
require careful evaluation of source images rather than maximum
intensity projection images [12].
Though CTA / MRA may be useful in planning management but
cerebral angiography is still considered as a gold standard for diagnosis
of CCF especially in pretreatment planning which shows filling of
venous sinuses during the arterial phase, retrograde flow from
cavernous sinus to ophthalmic veins and enlarged draining veins
[13,14].
Though transcranial and orbital Duplex ultrasound may allow
visualisation of arterialized cavernous sinus and superior ophthalmic
vein and in flow measurements but not very useful in making a specific
diagnosis [15].
Transarterial embolisation with wide variety of embolising material
is management of choice for high-flow, direct CCF while low-flow,
indirect CCF may either undergo spontaneous closure or may require
transarterial as well as transvenous approach [16] (Figures 2 and 3).
Figure 1: Axial T1W and axial and coronal T2W images shows
multiple dilated and tortuous vascular structures in the orbital
(superior ophthalmic vein) and cavernous sinus region on left side
of midline appearing signal void.
Computed tomography or magnetic resonance angiography (CTA /
MRA) are the preferred noninvasive method of diagnosis. They show Figure 2: Sagittal T2W and axial T2FLAIR images shows multiple
enlarged cavernous sinus with convex lateral margin and dilated dilated and tortuous vascular structures in the orbital (superior
superior ophthalmic veins. They may also reveal signs of orbital edema, ophthalmic vein) and cavernous sinus region on left side of midline
slight enlargement of ipsilateral extraocular muscles due to venous appearing signal void.
J Med Diagn Meth Volume 5 • Issue 3 • 1000221
ISSN:2168-9784 JMDM, an open access journal
Citation: Rastogi R, Wani AM, Joon P, Gupta Y, Sharma S, et al. (2016) Blunt Ocular Trauma - A Rare Cause of Carotico-Cavernous Fistula. J
Med Diagn Meth 5: 221. doi:10.4172/2168-9784.1000221
Page 3 of 3
2. Barrow DL, Spector RH, Braun IF, Landman JA, Tindall SC, et al.
(1985) Classification and treatment of spontaneous carotid cavernous
sinus fistulas. J Neurosurg 62: 248-256.
3. Kaplan JB, Bodhit AN, Falgiani ML (2012) Communicating carotid-
cavernous sinus fistula following minor head trauma. International
Journal of Emergency Medicine 5: 10.
4. Chaudry AI, Elkhamry SM, Al-Rashed W, Bosley TM (2009) Carotid
cavernous fistula: ophthalmological implications. Middle East Afr J
Ophthalmology 16: 57-63.
5. Oishi A, Miyamoto K, Yoshimura N (2009) Etiology of carotid cavernous
fistula in Japanese. Jpn J Ophthalmol 53: 40-43.
6. Uehara T, Tabuchi M, Kawaguchi T, Mori E (1998) Spontaneous dural
carotid cavernous sinus fistula presenting isolated ophthalmoplegia:
evaluation with MR angiography. Neurology 50: 814-816.
7. Coskun O, Hamon M, Catroux G, Gosme L, Courtheoux P, et al. (2000)
Carotid-cavernous fistula: diagnosis with spiral CT angiography. AJNR
Am J Neuroradiol 21: 712–716.
8. Aralasmak A, Karaali K, Cevikol C, Senol U, Sindel T, et al. (2014) Venous
Drainage Patterns in Carotid Cavernous Fistulas. ISRN Radiology 2014:
7.
9. Hirai T, Korogi Y, Hamatake S, Ikushima I, Sugahara T, et al. (1998)
Three-dimensional FISP imaging in the evaluation of carotid cavernous
fistula: comparison with contrast-enhanced CT and spin-echo MR. AJNR
Am J Neuroradiol 19: 253–259.
10. Harsha KJ, Basti RS, Kesavadas C, Thomas B (2013) Susceptibility-
weighted imaging in carotido-cavernous fistulas. A case control
Figure 3: Coronal, oblique and axial postcontrast MIP images and study. Interv Neuroradiol 19: 438-444.
SSD image show multiple dilated and tortuous vascular structures 11. Seeger A, Kramer U, Bischof F, Schuettauf F, Ebner F, et al. (2015)
in the orbital (superior ophthalmic vein) and cavernous sinus Feasibility of Noninvasive Diagnosis and Treatment Planning in a Case
region on left side of midline representing carotico-cavernous Series with Carotid-Cavernous Fistula using High-Resolution Time-
fistula. Resolved MR-Angiography with Stochastic Trajectories (TWIST) and
Extended Parallel Acquisition Technique (ePAT 6) at 3 T. Clin
Neuroradiol 25: 241-247.
12. Rucker JC, Biousse V, Newman NJ (2004) Magnetic resonance
Conclusion angiography source images in carotid cavernous fistulas. Br J Ophthalmol
88: 311.
CCFs are usually of high-flow type secondary to cranial trauma 13. Chang CCC, Chang PCT, Shy CG, Chang WS, Hung HC (2005) CT
presenting with ipsilateral ocular pain, increased intraocular pressure angiography and MRI angiography in the evaluation of carotid cavernous
and proptosis. However, slow-type of CCF may also be secondary to sinus fistula prior to embolisation: A comparison of Techniques. AJNR
ocular trauma as seen in our case. Though, cerebral angiography is 26: 2349-2356.
gold standard especially prior to coil embolisation of fistula but a 14. Chi CT, Nguyen D, Duc VT, Chau HH, Son VT (2014) Direct traumatic
combination of dilated superior ophthalmic vein and dilated cavernous carotid cavernous fistula: angiographic classification and treatment
sinus with internal flow voids is diagnostic of CCF on CTA / MRA. strategies. Study of 172 cases. Interv Neuroradiol 20: 461-475.
Endovascular treatment is the treatment of choice for high-flow fistula. 15. Molnar LJ, Caldas JG, Garcia RG, Cerri GG (2001) Doppler mapping of
direct carotid-cavernous fistulae (DCCF). Ultrasound Med Biol 27: 367–
371.
References 16. Korkmazer B, Kocak B, Tureci E, Islak C, Kocer N, et al. (2013)
1. Gemmete JJ, Chaudhary N, Pandey A, Ansari S (2010) Treatment of Endovascular treatment of carotid cavernous sinus fistula: A systematic
carotid cavernous fistulas. Current Treatment Options in review. World J Radiol 5: 143-155.
Neurology 12: 43-53.
J Med Diagn Meth Volume 5 • Issue 3 • 1000221
ISSN:2168-9784 JMDM, an open access journal
You might also like
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Natalya Master CardioDocument71 pagesNatalya Master CardioTaman Hoang100% (1)
- Emergency Medicine Mcqs Exam 2010-2011Document4 pagesEmergency Medicine Mcqs Exam 2010-2011Adam Adamako100% (4)
- Adult BLSDocument50 pagesAdult BLSVijay Krishna Murthy80% (5)
- Atrial FibrillationDocument13 pagesAtrial FibrillationChristianneMikeNo ratings yet
- Stroke and Cerebrovascular DiseaseDocument14 pagesStroke and Cerebrovascular DiseaseMarwan M.No ratings yet
- HypotensionDocument7 pagesHypotensionNader Smadi100% (2)
- Measuring Central Venous Pressure: Elaine ColeDocument8 pagesMeasuring Central Venous Pressure: Elaine ColednllkzaNo ratings yet
- 2022 Non-Cardiac SurgeryDocument105 pages2022 Non-Cardiac Surgeryhosameldin ahmedNo ratings yet
- Carotid Cavernous Fisstula (CCF)Document78 pagesCarotid Cavernous Fisstula (CCF)Deny Handayanto0% (1)
- Illustrative Teaching Case: Carotid-Cavernous FistulaDocument3 pagesIllustrative Teaching Case: Carotid-Cavernous FistulaDeborah Anasthasia PakpahanNo ratings yet
- CCF Clinical Presentation, Imaging, and Endovascular TreatmentDocument9 pagesCCF Clinical Presentation, Imaging, and Endovascular TreatmentmithaNo ratings yet
- Revisi 3 Case ReportDocument8 pagesRevisi 3 Case Reportzazaza94No ratings yet
- Indirect Carotid-Cavernous Fistula Mimicking Scleritis: MagesDocument1 pageIndirect Carotid-Cavernous Fistula Mimicking Scleritis: MagesClarithq LengguNo ratings yet
- Treatment of Carotid Cavernous FistulasDocument11 pagesTreatment of Carotid Cavernous FistulaskameliasitorusNo ratings yet
- Articulo FistulaDocument6 pagesArticulo FistulaOpti MonturasNo ratings yet
- 2019 - Chung Et Al-AnnotatedDocument6 pages2019 - Chung Et Al-AnnotatedCemal GürselNo ratings yet
- 20584Document6 pages20584Naga MuthuNo ratings yet
- Pseudoaneurysm of Internal Carotid Artery: N.V. Beena, M.S. Kishore, Ajit Mahale and Vinaya PoornimaDocument3 pagesPseudoaneurysm of Internal Carotid Artery: N.V. Beena, M.S. Kishore, Ajit Mahale and Vinaya PoornimaGordana PuzovicNo ratings yet
- Diagnostic Difficulties in Fibrous Dysplasia - A 5-Case Series and A Literature ReviewDocument9 pagesDiagnostic Difficulties in Fibrous Dysplasia - A 5-Case Series and A Literature Reviewsolikin ikinNo ratings yet
- Combined Treatment of Surgery and Sclerotherapy For Sinus PericraniiDocument5 pagesCombined Treatment of Surgery and Sclerotherapy For Sinus Pericranii相壮壮No ratings yet
- Carotid Cavernous Fistula: Images in Clinical MedicineDocument1 pageCarotid Cavernous Fistula: Images in Clinical MedicineRudolf Fernando WibowoNo ratings yet
- Optical Coherence Tomography Angiography of Pathological Myopia Sourced and Idiopathic Choroidal Neovascularization With Follow-UpDocument7 pagesOptical Coherence Tomography Angiography of Pathological Myopia Sourced and Idiopathic Choroidal Neovascularization With Follow-UpVlady BordaNo ratings yet
- Seio CavernosoDocument19 pagesSeio CavernosoIngrid GomesNo ratings yet
- Arachnoidal Diverticula of Sacral Extradural Meningeal CysDocument7 pagesArachnoidal Diverticula of Sacral Extradural Meningeal Cysjabarin.hNo ratings yet
- E255406 FullDocument3 pagesE255406 Fullroweis AdelNo ratings yet
- Austin Biomarkers & DiagnosisDocument3 pagesAustin Biomarkers & DiagnosisAustin Publishing GroupNo ratings yet
- A Child With Acute Eyelid Edema and Proptosis: JAMA Ophthalmology Clinical ChallengeDocument2 pagesA Child With Acute Eyelid Edema and Proptosis: JAMA Ophthalmology Clinical ChallengePatriciaNo ratings yet
- Diagnosis and Minimally Invasive Treatment of Posterior Fossa Dural Arteriovenous Fistula Presenting Clinically As A Carotid Cavernous FistulaDocument5 pagesDiagnosis and Minimally Invasive Treatment of Posterior Fossa Dural Arteriovenous Fistula Presenting Clinically As A Carotid Cavernous FistulaAthenaeum Scientific PublishersNo ratings yet
- Spontaneous Coronary Artery Dissection With Clinical Presentation of Acute Myocardial InfarctionDocument3 pagesSpontaneous Coronary Artery Dissection With Clinical Presentation of Acute Myocardial InfarctionSabrina JonesNo ratings yet
- Pathogenesis of Aortic Dissection: Elastic Fiber Abnormali-Ties and Aortic Medial WeaknessDocument9 pagesPathogenesis of Aortic Dissection: Elastic Fiber Abnormali-Ties and Aortic Medial WeaknessMonique BorresNo ratings yet
- Video: FocusDocument2 pagesVideo: Focusivonne perezNo ratings yet
- Bilateral Radiation Retinopathy 17 Years Following.62Document3 pagesBilateral Radiation Retinopathy 17 Years Following.62ShivcharanLalChandravanshiNo ratings yet
- 9.pediatric Dural Arteriovenous MalformationsDocument7 pages9.pediatric Dural Arteriovenous MalformationsNisa MahdiataraNo ratings yet
- Multiply Recurrent Solitary Fibrous Tumor of The Orbit Without Malignant Degeneration - A 45-Year Clinicopathologic Case StudyDocument3 pagesMultiply Recurrent Solitary Fibrous Tumor of The Orbit Without Malignant Degeneration - A 45-Year Clinicopathologic Case StudyJave GajellomaNo ratings yet
- Retina AnswersDocument5 pagesRetina AnswersKhushal Khan KakarNo ratings yet
- Complete Occlusion of Extracranial Internal Carotid Artery: Clinical Features, Pathophysiology, Diagnosis and ManagementDocument5 pagesComplete Occlusion of Extracranial Internal Carotid Artery: Clinical Features, Pathophysiology, Diagnosis and ManagementAndreea Raluca CimpoiNo ratings yet
- Vascular Abnormalities in Uveitis: SciencedirectDocument15 pagesVascular Abnormalities in Uveitis: Sciencedirect2456708893No ratings yet
- September 2020 Ophthalmic PearlsDocument4 pagesSeptember 2020 Ophthalmic PearlsBernardo RomeroNo ratings yet
- Carotid Cavernous FistulaDocument4 pagesCarotid Cavernous FistulaCarlos Del Carpio EnriquezNo ratings yet
- (10920684 - Neurosurgical Focus) Endovascular Management of Fusiform Aneurysms in The Posterior Circulation - The Era of Flow DiversionDocument7 pages(10920684 - Neurosurgical Focus) Endovascular Management of Fusiform Aneurysms in The Posterior Circulation - The Era of Flow DiversionCharles MorrisonNo ratings yet
- 2022 10 50 Images KimDocument2 pages2022 10 50 Images KimJuan David Pineda MontoyaNo ratings yet
- Hemangioma of The Cavernous Sinus: A Case SeriesDocument5 pagesHemangioma of The Cavernous Sinus: A Case SerieshamdanNo ratings yet
- The Management of Intracranial AbscessesDocument3 pagesThe Management of Intracranial AbscessesDio AlexanderNo ratings yet
- Radiologic Clues To Cerebral Venous ThrombosisDocument18 pagesRadiologic Clues To Cerebral Venous ThrombosisRudolph MuliawanNo ratings yet
- Angina MicrovasvularDocument8 pagesAngina MicrovasvularLex X PabloNo ratings yet
- Calcified Pseudoneoplasm of The Neuraxis Capnon A Lesson Learnt From A Rare Entity PDFDocument3 pagesCalcified Pseudoneoplasm of The Neuraxis Capnon A Lesson Learnt From A Rare Entity PDFKisspetre PetreNo ratings yet
- Vascular Malformations: A Review: Joshua A. Cox, MD Erica Bartlett, MD Edward I. Lee, MDDocument6 pagesVascular Malformations: A Review: Joshua A. Cox, MD Erica Bartlett, MD Edward I. Lee, MDYusmiatiNo ratings yet
- 2002 Metastatic Renal Cell Carcinoma To The Head and NeckDocument5 pages2002 Metastatic Renal Cell Carcinoma To The Head and NeckAlfonsoSánchezNo ratings yet
- Varicose Veins: BSC Mbbs Mrcs PHDDocument9 pagesVaricose Veins: BSC Mbbs Mrcs PHDNelly ElizabethNo ratings yet
- 2016 Optical Coherence Tomography Angiography of Indocyanine Green Angiographic Plaques in Asymptomatic Intermediate AgeRelated Macular DegenerationDocument16 pages2016 Optical Coherence Tomography Angiography of Indocyanine Green Angiographic Plaques in Asymptomatic Intermediate AgeRelated Macular DegenerationSergio ArrascueNo ratings yet
- tmp980 TMPDocument3 pagestmp980 TMPFrontiersNo ratings yet
- Issue Apr2012 Pdffiles CasereportDocument5 pagesIssue Apr2012 Pdffiles CasereportyunjaealwaysNo ratings yet
- Mature Cystic Teratoma of The Right Cerebellopontine Angle A Rare Case ReportDocument5 pagesMature Cystic Teratoma of The Right Cerebellopontine Angle A Rare Case ReportHaribabuBabuNo ratings yet
- Percutaneous Coronary Intervention in A Patient With Severe Systemic Vasculitis and Myocardial InfarctionDocument4 pagesPercutaneous Coronary Intervention in A Patient With Severe Systemic Vasculitis and Myocardial Infarctionvam buddhaNo ratings yet
- Case Report: Saudi Journal of Kidney Diseases and TransplantationDocument5 pagesCase Report: Saudi Journal of Kidney Diseases and TransplantationAleksandre KordzadzeNo ratings yet
- Caroticocavernous Fistula - Radiology Reference Article - RadiopaediaDocument8 pagesCaroticocavernous Fistula - Radiology Reference Article - RadiopaediaKhushi TahilianiNo ratings yet
- International Journal of Surgery Case ReportsDocument3 pagesInternational Journal of Surgery Case ReportsYipno Wanhar El MawardiNo ratings yet
- Anterior Submitral Aneurysm Rare EntityDocument4 pagesAnterior Submitral Aneurysm Rare EntityInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Delayed Diagnosis of Central Skull-Base Osteomyelitis With Abscess: Case Report and Learning PointsDocument4 pagesDelayed Diagnosis of Central Skull-Base Osteomyelitis With Abscess: Case Report and Learning PointsKarenNo ratings yet
- v18n3 221transarterialDocument6 pagesv18n3 221transarterialUssiy RachmanNo ratings yet
- Tuberculosis of Sphenoid Sinus Report of Two CasesDocument4 pagesTuberculosis of Sphenoid Sinus Report of Two CasesDevikaNo ratings yet
- Eye 2011101Document2 pagesEye 2011101ashnagupta1571No ratings yet
- Lawrence Et Al 2021 Contralateral Transmaxillary Approach For Resection of Chondrosarcoma of The Petrous Apex A CaseDocument4 pagesLawrence Et Al 2021 Contralateral Transmaxillary Approach For Resection of Chondrosarcoma of The Petrous Apex A CaseSourabh PatroNo ratings yet
- Intracranial Dural Arteriovenous Fistulae: Presentation and Natural History ClassificationDocument3 pagesIntracranial Dural Arteriovenous Fistulae: Presentation and Natural History ClassificationFinger JempolNo ratings yet
- A Case Report of Hydrocephalus in A US Military RecruitDocument3 pagesA Case Report of Hydrocephalus in A US Military RecruitRomita PutriNo ratings yet
- WJR 5 143Document13 pagesWJR 5 143andre halimNo ratings yet
- Brain Aneurysm ArticleDocument5 pagesBrain Aneurysm ArticleFarisa Jane BanggoNo ratings yet
- Atlas of Coronary Intravascular Optical Coherence TomographyFrom EverandAtlas of Coronary Intravascular Optical Coherence TomographyNo ratings yet
- Keracunan SianidaDocument7 pagesKeracunan SianidaYulianti Risa TonapaNo ratings yet
- Profil Skabies Di Poliklinik Kulit Dan Kelamin RSUP Prof. Dr. R. D. Kandou Manado Periode Januari-Desember 2013Document7 pagesProfil Skabies Di Poliklinik Kulit Dan Kelamin RSUP Prof. Dr. R. D. Kandou Manado Periode Januari-Desember 2013sinta mahastutiNo ratings yet
- 2619 7786 1 SM PDFDocument11 pages2619 7786 1 SM PDFSezyArisandiNo ratings yet
- Clinical Case in Neurology - by SlidesgoDocument86 pagesClinical Case in Neurology - by SlidesgoGabriel AlvesNo ratings yet
- Delayed Detection of Carotid-Cavernous Fistulas Associated With Wartime Blast-Induced Craniofacial TraumaDocument5 pagesDelayed Detection of Carotid-Cavernous Fistulas Associated With Wartime Blast-Induced Craniofacial TraumamithaNo ratings yet
- Life Cycle Sarcoptes Scabei and Pathogenicity Mite in Boarding Scholl Malang, IndonesianDocument7 pagesLife Cycle Sarcoptes Scabei and Pathogenicity Mite in Boarding Scholl Malang, IndonesianmithaNo ratings yet
- Faktor Resiko Skabies Di MasyarakatDocument6 pagesFaktor Resiko Skabies Di MasyarakatmithaNo ratings yet
- Congenital Hemangioma of The SkullDocument3 pagesCongenital Hemangioma of The SkullmithaNo ratings yet
- Epidemiology, Diagnosis, and Treatment of Scabies in DermatologyDocument7 pagesEpidemiology, Diagnosis, and Treatment of Scabies in DermatologymithaNo ratings yet
- KDIGO AKI Guideline DownloadDocument141 pagesKDIGO AKI Guideline DownloadSandi AuliaNo ratings yet
- ScabiesDocument12 pagesScabiesalston96No ratings yet
- 4 - Respiratory Phyiology PDFDocument27 pages4 - Respiratory Phyiology PDFjuweriyNo ratings yet
- Diabetes and Liver An Association Hepatogenous Diabetes Mechanism Andsome Evidences 2157 7013 1000257Document5 pagesDiabetes and Liver An Association Hepatogenous Diabetes Mechanism Andsome Evidences 2157 7013 1000257mithaNo ratings yet
- Akutkidney InjuryDocument10 pagesAkutkidney InjuryUmbu EndyNo ratings yet
- What Is Coronavirus English PDFDocument1 pageWhat Is Coronavirus English PDFmithaNo ratings yet
- Bedtime Routines For Young ChildrenDocument6 pagesBedtime Routines For Young ChildrenmithaNo ratings yet
- Organochlorine Pesticides FactDocument5 pagesOrganochlorine Pesticides FactmithaNo ratings yet
- Blunt Abdominal and Pelvic Trauma: Abdullah Alabousi, Vincent M. Mellnick, Michael N. PatlasDocument8 pagesBlunt Abdominal and Pelvic Trauma: Abdullah Alabousi, Vincent M. Mellnick, Michael N. PatlasmithaNo ratings yet
- Acute Kidney Injury in Diabetes MellitusDocument8 pagesAcute Kidney Injury in Diabetes MellitusmithaNo ratings yet
- Circadian Rhythms: 2. The Underlying Molecular MechanismsDocument13 pagesCircadian Rhythms: 2. The Underlying Molecular MechanismsferianaNo ratings yet
- Effectiveness of Statin Therapy in Ischemic Post Stroke PatientsDocument6 pagesEffectiveness of Statin Therapy in Ischemic Post Stroke Patientsvhania baniNo ratings yet
- Arif 2009Document2 pagesArif 2009FihzanNo ratings yet
- Diastolic Murmurs Valvular Diseases ChartDocument2 pagesDiastolic Murmurs Valvular Diseases ChartNaman KanakiyaNo ratings yet
- EKG Cheat Sheet - Henry Del RosarioDocument1 pageEKG Cheat Sheet - Henry Del RosarioanwarNo ratings yet
- Sicksinussyndrome: Roberto de Ponti,, Jacopo Marazzato,, Giuseppe Bagliani,, Fabio M. Leonelli,, Luigi PadelettiDocument13 pagesSicksinussyndrome: Roberto de Ponti,, Jacopo Marazzato,, Giuseppe Bagliani,, Fabio M. Leonelli,, Luigi Padelettijose noel garcia perezNo ratings yet
- U6C6 - Carty Soriano - Heart ValvesDocument6 pagesU6C6 - Carty Soriano - Heart ValvesXio LinaresNo ratings yet
- The Impact of Dominant Ventricular Morphology On The Early Postoperative Course After The Glenn ProcedureDocument7 pagesThe Impact of Dominant Ventricular Morphology On The Early Postoperative Course After The Glenn ProcedureEitan KeizmanNo ratings yet
- Cardiology FMDocument25 pagesCardiology FMtrushaNo ratings yet
- Medical AbbreviationDocument3 pagesMedical AbbreviationWaode FitriNo ratings yet
- DR Sandeep - EISENMENGER SYNDROMEDocument81 pagesDR Sandeep - EISENMENGER SYNDROMEAlexandrescuNo ratings yet
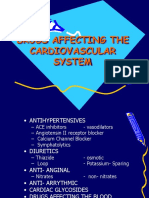
- Drugs Affecting The Cardiovascular SystemDocument21 pagesDrugs Affecting The Cardiovascular SystemAudrey Beatrice ReyesNo ratings yet
- Coronary Guidewires: Choice & Appropriate Use in PciDocument84 pagesCoronary Guidewires: Choice & Appropriate Use in PcierickNo ratings yet
- Ecg InterpretationDocument3 pagesEcg Interpretationman0billi0% (1)
- Basics of ECGDocument32 pagesBasics of ECGNachiket Vijay PotdarNo ratings yet
- Hemant Surgical Double Lumen CathetersDocument2 pagesHemant Surgical Double Lumen CathetersKaushik Hanskumar ShahNo ratings yet
- Vimal PAD - SlidesDocument53 pagesVimal PAD - SlidesVimal NishadNo ratings yet
- UW - Cardiovascular - Educational ObjectivesDocument52 pagesUW - Cardiovascular - Educational ObjectivesUsama BilalNo ratings yet
- DR Sujata: Professor Dept - of Anaesthesiology &critical Care Ucms & GTB HospitalDocument53 pagesDR Sujata: Professor Dept - of Anaesthesiology &critical Care Ucms & GTB HospitalMiniNo ratings yet
- Arterial LinesDocument13 pagesArterial LinesberhanubedassaNo ratings yet
- Mindmap CVS Liana Naamnih Group3Document1 pageMindmap CVS Liana Naamnih Group3Liana NaamnehNo ratings yet
- 03-Ischemic Heart Disease - 2020 OngoingDocument151 pages03-Ischemic Heart Disease - 2020 OngoingDana MohammadNo ratings yet
- Risk of Arrhythmia and Sudden Death - M. Malik (BMJ, 2001) WWDocument429 pagesRisk of Arrhythmia and Sudden Death - M. Malik (BMJ, 2001) WWRohan Upadhyay UpadhyayNo ratings yet