Professional Documents
Culture Documents
A Special Case of Lower Back Pain in A 3-Year-Old Girl: Davide Tassinari, Sara Forti, Michele Torella, Giovanni Tani
Uploaded by
hiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A Special Case of Lower Back Pain in A 3-Year-Old Girl: Davide Tassinari, Sara Forti, Michele Torella, Giovanni Tani
Uploaded by
hiCopyright:
Available Formats
Rare disease
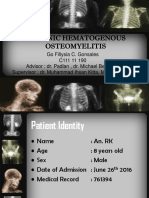
CASE REPORT
A special case of lower back pain in a 3-year-old girl
Davide Tassinari, Sara Forti, Michele Torella, Giovanni Tani
Paediatric Departement, SUMMARY oral rehydration and probiotics with complete reso-
S.Orsola-Malpighi Hospital, We describe the case of a 3-year-old girl with a 15-day lution of symptoms.
University of Bologna,
Bologna, Italy
clinical history of lower back pain. We diagnosed a At hospital admission, she presented with mild
spondylodiscitis of vertebral bodies L5–S1 caused by fever (37.5°C) and non-specific symptoms such as
Correspondence to Salmonella species group B that totally recovered with irritability, fatigue, loss of appetite and lack of
Dr Davide Tassinari, appropriate antibiotic therapy. Spondylodiscitis in desire to play. Physical examination showed mild
davide.tassinari@aosp.bo.it
children is a rare condition and Salmonella infection is lumbar spine stiffness, gross restriction of lumbar
one of the rarest aetiology. A high index of suspicion is movements and difficulty in walking. The back
needed for prompt diagnosis to ensure better long-term pain was exacerbated by movements and the
outcome. Microbiological diagnosis is essential for the patient was unable to bend over to pick up a little
appropriate choice of antibiotic treatment. toy and showed irritation of the hips when held in
extension (log-roll test).13 Neurological examin-
ation showed no signs of meningism and showed a
BACKGROUND normal lower tendon reflexes. The remaining clin-
Infective spondylodiscitis in healthy individuals is a ical examination was normal.
rare condition; in children it is more common
between 6 months and 3 years of age. INVESTIGATIONS
Mycobacterium tuberculosis is the commonest Initial blood test showed a mild increase in white
cause of spinal infection worldwide and accounts blood cell count (WBC 12.610/mmc; neutrophils
for 9–46% of cases in developed countries. The 48%, lymphocytes 41%) and platelets (557.000/
other more common organisms causing spondylo- microl) with normal red blood cells (RBC
discitis are Staphylococcus aureus, Escherichia 4.070.000/mmc), median corpuscular volume
coli, Pseudomonas, Streptococci andKlebsiella.1 (77 fl) and haemoglobin (11.0 g/dl). Erythrocyte
Salmonella organism is a rare cause of bone dis- sedimentation rate (ESR 65 mm/h) was increased
eases in immunocompetent children and spondylo- with a normal C reactive protein (CRP 0.50 mg/dl).
discitis have been reported to account for only Peripheral blood smear showed no WBC and/or
2–5% of all the cases of osteomyelitis infection.1–4 RBC abnormalities.
In non-endemic areas, most cases have been Tuberculin skin test and interferon-γ based
reported in patients who were immunologically release assay (QuantiFERON-TB Gold) were nega-
compromised by sickle-cell haemoglobinopathy,5 tive; blood culture taken on admission remained
malignant lesions, collagen or vascular diseases and negative.
diabetes.6 Only sporadic cases of Salmonella spon- Other immunological deficiencies or collagen
dylodiscitis in immunocompetent patients have diseases were ruled out.
been reported.7–12 The Widal-Wright test was positive for
The main target bone in Salmonella osteomye- Salmonella typhi H (title 1:800).12 Considering the
litis is unknown but, in general, the vertebra is previous episode of diarrhoea, the coproculture
rarely infected in the paediatric age.3 13 was repeated which confirmed the persistence of
Salmonella group B species.
CASE PRESENTATION Chest x-ray and abdominal ultrasound were
A 3-year-old Italian girl was admitted to the paedi- normal. Lateral x-ray of the lumbosacral tract
atric emergency unit with a 15-day history of lower revealed inhomogeneous appearance of the poster-
back pain exacerbated by deambulation, extended ior wall of the lumbar 5 (L5) vertebral body
to both hips with movement difficulties, especially together with a posterior irregular profile of L4
in sitting and keeping several postural positions. spine (figure 1). The lumbosacral vertebrae MRI
Her general conditions were compromised and studies showed an inhomogeneous hyperintensity
associated with mild fever since 2 days before of vertebral bodies of L5 and sacral 1 (S1), particu-
admission. larly L5 body showed a pseudolacunar and ser-
The parents correlated the onset of the pain with piginous image in its posterior part with oedema of
an accidental fall on her back 1 month prior to surrounding tissues (figure 2A). Moreover, it
admission. Moreover, 15 days before the beginning demonstrated an intervertebral disc height loss
of the lower back pain, the patient presented an between L5 and S1 with a signal strength reduction
To cite: Tassinari D, Forti S,
Torella M, et al. BMJ Case
acute episode of diarrhoea with abdominal pain (figure 2B). The MRI also confirmed the inflamma-
Rep Published online: and fever ( peak of 38.8°C) lasting for 4 days. tory state of the area located at the right-hand side
[please include Day Month A bacterial gastroenteritis was suspected and a of the intervertebral disc between L4 and L5, as
Year] doi:10.1136/ group B Salmonella species was isolated in the well as the presence of oedema and a cuff-like
bcr.09.2011.4796 coproculture. The patient was treated only with thickening of paravertebral tissues with posterior
Tassinari D, et al. BMJ Case Rep 2013. doi:10.1136/bcr.09.2011.4796 1
Rare disease
pressure on the dural membrane (figure 3). The contrast
medium caused intense and homogenous enhancement of the
aforementioned findings. To better differentiate among inflam-
matory and malignancy origin, the patient underwent
fluorine-18 fluorodeoxyglucose positron emission tomography
(18F-FDG PET) that showed mild L5–S1 hyperaccumulation of
radiopharmaceutical medium with a standard uptake value
maximum (SUV max) of 3 g/ml.14
The result supported mainly inflammatory nature of the bone
lesion like spondylodiscitis and, given the history, a Salmonella
infection was suspected. The aetiology could only be confirmed
by a percutaneous CT-guided spinal biopsy, but considering the
young age of the patient and the invasiveness of the procedure,
we decided to start intravenous antibiotic therapy based on the
coproculture antibiogram sensitivity and to follow-up the clin-
ical and radiological evolution of the vertebral lesion. After
antibiotic therapy was started in association to the use of a
lumbar corset, the patient’s clinical conditions rapidly improved.
To evaluate the evolution of the inflammatory lesion and to
exclude any illness progression, an MRI scan of the lumbosacral
tract was repeated after 2 weeks of treatment, showing a slight
improvement of the previously reported findings (figure 4).
Clinical and radiological improvement convinced us to continue
with the ongoing therapy without proceeding to CT-guided
biopsy.
An MRI performed 4 weeks after the initiation of the treat-
ment showed a noteworthy reduction of the vertebral lesion
along with an improvement of intervertebral and paravertebral
Figure 1 X-ray of the lumbosacral spine revealed inhomogeneous inflammatory state (figures 5 and 6).
appearance of the posterior wall of the L5 vertebral body with also a
After an intermediate MRI control at 4 months, the last
posterior irregular profile of L4 spine.
MRI at a 15-month follow-up demonstrated the complete
Figure 2 T2 (A) and STIR (B) sequences of the first MRI: dishomogeneous hyperintensity of vertebral bodies L5–S1; L5 body showed
pseudolacunar and serpiginous image in its posterior part together with disc height loss. STIR, short time inversion recovery.
2 Tassinari D, et al. BMJ Case Rep 2013. doi:10.1136/bcr.09.2011.4796
Rare disease
space (discitis) and the surrounding soft tissue (epidural or para-
spinal abscesses). When the original illness becomes clinically
symptomatic it is usually difficult to differentiate where path-
ology originated: generally in infections and/or in tumours all
three anatomical vertebral districts that are already involved.1 15
Even if the medical history along with the combination of
symptoms and laboratory and radiological findings oriented the
diagnosis towards a spondylodiscitis infection, we had further
minimal doubts in excluding other aetiologies with a similar
clinical presentation, including traumatism or neoplasm, particu-
larly osteosarcomas.
In children, diagnosis of infective vertebral spondylodiscitis
could be delayed because back pain is often related to
traumatism.1 2 13
In our patient diagnosis was oriented by a recent episode of
diarrhoea where group B Salmonella was isolated in
coproculture.
Ewing sarcoma is a condition that must be excluded in chil-
dren with back pain and radiological alterations.16 Like in spon-
dylodiscitis, vertebral involvement is very rare and generally,
when symptomatic, its advancement stage is not surgically treat-
able, especially for vertebral localisations.14 16
The symptoms of spondylodiscitis are not specific: back pain
Figure 3 MRI of the T1-weighted images: oedema and a cuff-like is very common, but up to 15% of patients may be pain free. In
thickening of paravertebral tissues with a hypointense signal in this patient the presence of progressive back pain and grossly
T1-weighted images and hyperintense signal in STIR with posterior restrictions of movements oriented for spine pathologies.1 8 17
pressure on the durale. STIR, short time inversion recovery. We also found elevated ESR and leucocytes count, but with
negative CRP.
Blood culture was negative but we found repeated positivity
normalisation of vertebral bodies L5–S1 (figure 7) with a reduc- for group B Salmonella species in the patient’s coproculture
tion of the intervertebral space caused by a permanent lesion of before and after the hospital admission.
the intervertebral disc. It is well known that in almost half of the cases of spondylo-
discitis a distant focus of infection has been identified and thus
DIFFERENTIAL DIAGNOSIS we began the antibiotic therapy on the basis of antibiogram sus-
Spine pathologies can involve various anatomical districts: the ceptibility without performing a percutaneous CT-guided
vertebral body (osteomielitis or tumours), the intervertebral disc biopsy.18
Figure 4 MRI in sequences of T2-weighted images (A) and STIR (B) after 2 weeks: dishomogeneous hyperintensity of vertebral bodies L5 and S1
was diminished. STIR, short time inversion recovery.
Tassinari D, et al. BMJ Case Rep 2013. doi:10.1136/bcr.09.2011.4796 3
Rare disease
The combination of positive coproculture with MRI sug-
gested us to begin the antibiotic therapy because of the high
probability of Salmonella group B spondylodiscitis.
Nevertheless, we had further minimal doubts in excluding
osteosarcomas. PET is a non-invasive method that can help in
differentiating among inflammatory and malignancy origin. A
variety of tracers have been used in the radionuclide imaging of
spondylodiscitis with different sensibility and specificity.19 21
Among them a recent technique using 18F-FDG PET seems to
offer some advantages. In fact it offers the opportunity to
distinguish infections from degenerative changes and/or neo-
plasm.22 23 There is a direct correlation between tumoural
mitotic count and SUV max. In this patient SUV max was 3 g/
ml which was a value low enough to exclude Ewing sarcoma
and osteosarcoma. SUV max in Ewing sarcoma ranged from 1.6
to 9.2 g/ml and in osteosarcoma it is 3.5–20.4 g/ml. The SUV
max values of all inflammatory bone lesions at 30 min ranged
from 0.5 to 3.5 g/ml.24
The clinical course of the patient improved rapidly after the
beginning of the antibiotic therapy and a second MRI did not
Figure 5 MRI of the T1-weighted images at 4 weeks showed strong reveal any worsening of the imaging. For this reason we did not
reduction of the inflammatory state at the right-hand side of the perform CT-guided biopsy.
intervertebral disc between L4 and L5 together with the hyperintensity
reduction of the paravertebral tissues cuff-like effect. TREATMENT
Following the antibiotic sensitivity reported on coproculture we
started piperacillin/tazobactam therapy (0.2 g/kg/die divided in
As in our patient, plain radiography is frequently used as a four doses) with the purpose of extending treatment to the wide
screening test. It may reveal some early changes of vertebral range of possible spondylodiscitis aetiologies including mainly S
bodies and relative spines: subchondral radiolucency, loss of def- aureus.1
inition of the endplate and loss of disc height. Later, the This treatment generated a rapid clinical improvement.
changes include destruction of the endplate, loss of vertebral Further improvement of symptomatology was reached with the
height and paravertebral soft tissue mass.17 19 application of a lumbar corset as prescribed by the orthopaedic
A CT is the gold-standard for bony abnormalities, but it is consultant.
inferior to MRI in defining neural damaging, disc appearance After 23 days of therapy the coproculture was still positive for
and epidural abscesses. At MRI this patient showed diffuse Salmonella group B species and antibiogram demonstrated in
involvement of all the three anatomical districts of the lumbar vitro resistance to piperacillin/tazobactam but was susceptible to
vertebrae: disc, bone and paravertebral soft tissues.13 20 ceftazidime; the antibiotic therapy was then switched to
Figure 6 MRI after 4 weeks: further great decrease of the signal alteration of vertebral bodies L5 and S1 (A); the contrast medium technique did
not show pathological enhancement (B).
4 Tassinari D, et al. BMJ Case Rep 2013. doi:10.1136/bcr.09.2011.4796
Rare disease
Figure 7 MRI of the T1-weighted images after 15 months: resolution of the inflammatory state of L4 and L5 vertebral bodies (A), together with
the normalisation of paravertebral district (B).
intravenous ceftazidime (0.1 g/kg/die divided in three doses). In children, different from adults, the intervertebral disc is vascu-
Intravenous antibiotic therapy was continued for a total of larised with a lot of anastomotic vessels directly communicating
5 weeks. with the metaphyseal ring of the above and below two adjacent ver-
After discharge, the treatment was continued for two more tebrae.1 13 This vascular distribution explains the higher incidence
weeks with oral sulfamethoxazole/trimethoprim, on the basis of of spondylodiscitis in children and the findings of clinical and
the last Salmonella’s susceptibility antibiogram. imaging examinations. The main step of the antimicrobial therapy
Body corset therapy has been continued for 4 months after is the cultural isolation of the pathogens causing spondylodiscitis.
MRI demonstrated almost complete resolution of the vertebral A distant focus of the infection has been identified in almost
body lesions. half the cases of spondylodiscitis: genitourinary tract (17%),
The patient continued physiotherapy exercises for a total of skin and soft tissues (11%), gastrointestinal tract (9%), intravas-
12 months with complete resolution of symptomatology. cular devices (5%) and respiratory tract (2%).26
As a complication of spondylodiscitis, an endocarditis was
reported in 12% of affected patients.1 For these reasons and
OUTCOME AND FOLLOW-UP
before antibiotic use, multiple cultures from various anatomical
Clinical conditions of the child improved gradually after the
districts should be taken.
beginning of intravenous antibiotic therapy.
Since spondylodiscitis is mainly monomicrobial and often has
After 6 weeks of antibiotic therapy she walked without diffi-
a haematogenous source, blood cultures are reported to be posi-
culties and her lower back movements were almost normal.
tive in a range between 40 and 60% of the patients.1 13
She continued with physiotherapy and with lumbar support
A CT-guided biopsy is also another important tool used in
corset for several months.
identifying various pathogens affecting spine districts. Till now
An MRI of the lumbosacral vertebrae was performed at 0, 2,
the mandatory role of biopsy in children is debated on the basis
4 and 16 weeks that showed a progressive improvement of the
of the risk–benefit analysis and on the fact that as many as 40%
lesions up to a total resolution.
of them are negative even before antibiotic use, as described by
The only negative outcome was the complete degeneration of
Karadimas et al.2
L5–S1 disc demonstrated with a loss of height of the interverte-
In this case an anti-Salmonella antibiotic therapy was oriented
bral space in the last MRI, at 15 months follow-up.
by the following main points: a repeated positive coproculture,
a clinical history of diarrhoea, a high Widal titre and the MRI.
DISCUSSION Generally, in paediatric patients the antibiotic therapy is
Vertebral infective spondylodiscitis is uncommon in children accepted when a pathogen is isolated and demonstrated the
and accounts for only 2–5% of all osteomyelitis.1 2 focus-source infection. A CT biopsy is mandatory when the
The main documented pathogens are Mycobacterium tubercu- initial response to therapy is poor and/or the presence of atyp-
losis and, among pyogenic infections, S aureus.1 ical microorganism is suspected.1 18
The two greatest retrospective paediatric studies described 16 The frequency of performing biopsies varied among spondy-
and 18 children, respectively, none of them affected lodiscitis studies (19–100%) and the positivity of culture-
bySalmonella.18 25 This infectious aetiology is a rare condition samples ranges from 43 to 78% of the cases.1–3
in immunologically normal children and it is described mainly Symptoms in children with vertebral spondylodiscitis are vari-
in the case reports.7 9–11 Also, in adults, it is a very rare condi- able and they depend on the gravity-stage of the infection and the
tion presented in the literature in few retrospective studies.2 4 12 age of the patient. A high-grade fever with back pain and refusal to
Pathogens can infect the spine from three main sources: by crawl, sit or walk is usually present in older children, whereas in
haematogenous spread (arterial and venous), by contiguous younger ones may predominate subtly with non-specific symptoms
spread and by external inoculation. like low-grade fever, malaise, weight loss and irritability.3 8 17 20
Tassinari D, et al. BMJ Case Rep 2013. doi:10.1136/bcr.09.2011.4796 5
Rare disease
The aim of the treatment consists of an antimicrobial therapy
together with physiotherapy and immobilisation with a lumbar Learning points
corset. These support treatments are used to alleviate back pain,
to reduce intradiscal pressure and to support lumbar
▸ Spondylodiscitis is a rare pathology in children: Salmonella
vertebrae.11 27
infection should also be considered in immunocompetent
In this patient we started antibiotic therapy with piperacillin/
patients.
tazobactam according to antibiogram. After 2 weeks we
▸ Cultural isolation from various anatomical districts is an
switched to antibiotic treatment from piperacillin/tazobactam to
important guide to begin antibiotic therapy.
ceftazidime because of a developed in vitro resistance to our
▸ A CT-guided needle biopsy should be considered when no
Salmonella strain.
organism can be identified by less-invasive techniques or
In Salmonella’s spondylodiscitis the response to antimicrobial
when malignant lesions are highly suspected.
treatment may vary with age, antibiotic used, antibiotic sensibil-
▸ Only repeated MRI gives the opportunity to follow-up strictly
ity, immunocompromised conditions, illness severity and dur-
the illness evolution until complete resolution.
ation of diarrhoea before the starting of antibiotic treatment.
One of the potential risks of intestinal salmonellosis in young
infants is an extraintestinal infection, but it is not known if anti-
biotics have a significant impact in preventing the risk of extra- Patient consent Obtained.
intestinal infections in children.28–30
Competing interests None.
Many authors describe different treatment lengths, but there
is a significantly increased risk of therapy failure in patients Provenance and peer review Not commissioned; externally peer reviewed.
treated for less than 4 weeks instead of longer periods.13 31
Several authors demonstrated that intravenous antibiotic
therapy should be administered for 2–3 weeks and after that it
is possible to switch to oral administration.28 REFERENCES
There is a general agreement that antibiotic treatment should 1 Gouliouris T, Aliyu SN, Brown NM. Spondylodiscitis: update on diagnosis and
management. J Antimicrob Chemoter 2010;65(Suppl 3):11–24.
be prolonged, at least, for 4 weeks, but data specifically related 2 Karadimas EB, Bunger C, Lindblad BE, et al. Spondylodiscitis. A retrospective study
to paediatric Salmonella spondylodiscitis are very limited.13 of 163 patients. Acta Orthop 2008;79:650–9.
The diagnosis of infective spondylodiscitis in children remains 3 Dupeux S, Pouchot B. Osteomyelitis and septic arthritis. Vertebral osteomyelitis. Rev
a medical challenge and it is often delayed owing to the rarity Prat 2008;58:1943–51.
4 Gaujoux-Viala C, Zeller V, Leclerc P, et al. Osteomyelitis in adults: an
of the disease and the insidious onset of symptoms.
underrecognized clinical entity in immunocompetent hosts. A report of six cases.
In the early stage of unspecified spondylodiscitis, x-rays have Joint Bone Spine 2011;78:75–9.
very low sensitivity and specificity. It is frequently employed as a 5 Chambers JB, Forsythe DA, Bertrand SL, et al. Retrospective review of osteoarticular
screening test in patients with lumbar pain and may occasionally infections in a pediatric sickle cell age group. J Pediatr Orthop 2000;20:682–5.
reveal early changes like in our patient. In fact MRI is the most 6 Gondusky JS, Gondusky CJ, Helmers SW. Salmonella osteomyelitis in new onset
diabetes mellitus. Orthopedics 2009;32:9.
useful method for the investigation of the spine infections, espe- 7 Barkai G, Leibovitz E, Smolnikov A, et al. Salmonella diskitis in a 2-year-old
cially in the early stages of the illness. MRI has high sensitivity immunocompetent child. Scand J Infect Dis 2005;37:232–5.
(96%) and specificity (94%). It is not invasive and it does not 8 Anastassiades CP, Virk A. From gut to bone. Am J Med 2008;121:767–9.
use radiations, which is especially important in children. It gives 9 Akiba T, Arai T, Ota T, et al. Vertebral osteomyelitis and paravertebral abscess due
to Salmonella oranienburg in a child. Pediatr Int 2001;43:81–3.
many advantages if compared with CT because it can also
10 Miller ME, Fogel GR, Dunham WK. Salmonella spondylitis: a review and report of
explore the disc spaces and soft and neural tissues.1 13 19 There two immunologically normal patients. J Bone Joint Surg 1988;70:463–6.
does not exist a general agreement about the timing of repeated 11 Santos E, Sapico FL. Vertebral osteomyelitis due to salmonellae: report of two cases
MRI to follow-up the illness evolution. Probably in this case the and review. Clin Infect Dis 1998;27:287–95.
time for MRI follow-up was too short, but this was because of 12 Amritanand R, Venkatesh K, Sundararaj GD, et al. Salmonella spondylodiscitis in the
immunocompetent. Spine 2010;35:1317–21.
some imaging doubts on the benignity of our patient’s lesions. 13 De Moraes Barros Fucs PM, Meves R, Yamada HH. Spinal infection in children: a
However, the second MRI showed a light involution of the review. Int Orthop 2012;36:387–95.
spinal lesions and confirmed the exclusion of the malignancies. 14 London K, Stege C, Cross S, et al. 18F-FDG PET/CT compared to conventional
Sometimes, at the onset of the spondylodiscitis, MRI could imaging modalities in pediatric primary bone tumors. Pediatr Radiol
2012;42:418–30.
be inconclusive in distinguishing infections from degenerative
15 Calderone RR, Larsen JM. Overview and classification of spinal infections. Orthop
illnesses like osteosarcoma.23 Clin North Am 1996;27:1–8.
Recently, some evidences emerged on 18F-FDG PET as an 16 Yalniz E, Ozcan M, Copuroglu C, et al. Ewing osteosarcoma of the lumbar vertebra:
important tool in evaluating the aetiology of various spine disor- case report and review of the literature. Arch Orthop Trauma Surg
ders including differential diagnosis with some malignancies, 2009;129:1701–5.
17 Offiah AC. Acute osteomyelitis, septic arthritis and discitis: differences between
even if it shows a low specificity for neoplasm.13 22 In fact, neonates and older children. Eur J Radiol 2006;60:221–32.
there are many overlapping values of SUV max in Ewing 18 Chandrasenan J, Klezl Z, Bommireddy R, et al. Spondylodiscitis in children. J Bone
sarcoma (1.6–9.2 g/ml) if compared with osteosarcoma (3.5– Joint Surg Br 2011;93-B:1122–5.
20.4 g/ml).13 The 18F-FDG PET has a direct positive correl- 19 Modic MT, Feiglin DH, Piraino DW, et al. Vertebral osteomyelitis: assessment using
MR. Radiology 1985;157:157–66.
ation between the tumoural mitotic count and the SUV max.22
20 Jaramillo D, Treves ST, Kasser JR, et al. Osteomyelitis and septic arthritis in children:
Spondylodiscitis in children remains rare and Salmonella appropriate use of imaging to guide treatment. AJR Am J Roentgenol
infection is one of the rarest aetiology. Its diagnosis is actually 1995;165:399–403.
easier because of the availability of more effective diagnostic 21 Palestro CJ, Kim CK, Swyer AJ, et al. Radionuclide diagnosis of vertebral
tools. A high index of suspicion is needed for prompt diagnosis osteomyelitis: indium-111-leukocyte and technetium-99m-methylene diphosphonate
bone scintigraphy. J Nucl Med 1991;32:1861–5.
to ensure improved long-term outcomes. Microbiological diag- 22 Schmitz A, Risse JH, Grünwald F, et al. Fluorine-18 fluorodeoxyglucose positron
nosis is essential for the appropriate choice of antibiotic emission tomography findings in spondylodiscitis: preliminary results. Eur Spine J
treatment. 2001;10:534–9.
6 Tassinari D, et al. BMJ Case Rep 2013. doi:10.1136/bcr.09.2011.4796
Rare disease
23 Stumpe KD, Zanetti M, Weishaupt D. et al. FDG-positron emission tomography for 27 Sato N, Sekiguchi M, Kikuchi S, et al. Effects of long-term corset wearing on
differentiation of degenerative and infectious endplate abnormalities in the lumbar chronic low back pain. Fukushima J Med Sci 2012;58:60–5.
spine detected on MR imaging. AJR Am J Roentgenol 2002;179:1151–7. 28 Sarinavin S, Garner P. Antibiotics for treating salmonella gut infetions (rewiew).
24 Walter F, Federman N, Apichairuk W, et al. 18F-fluorodeoxyglucose uptake of bone Cochrane Library 2009;1:1–31.
and soft tissue sarcomas in paediatric patients. Pediatr Hematol Oncol 29 Fleege C, Wichelhaus TA, Rauschmann M. Systemic and local antibiotic therapy of
2011;28:579–87. conservative and operative treatment of spondylodiscitis. Orthopade 2012;41:727–35.
25 Moreno R Tapia, Espinosa Fernández MG, Martìnez Leòn MI, et al. Spondylodiscitis: 30 Butler T. Treatment of typhoid fever in the 21st century: promise and shortcomings.
diagnosis and medium-long term follow up of 18 cases. An Pediatr (Barc) Clin Microbiol Infect 2011;17:959–63.
2009;71:391–9. 31 Celak F Cakmak, Sayli TR, Ocguder DA, et al. Primary subacute Salmonella
26 Mylona E, Samarkos M, Kakalou E, et al. Pyogenic vertebral osteomyelitis: a osteomyelitis of the navicular bone in a child with normal immunity. J Pediatr
systematic review of clinical characteristics. Semin Arthritis Rheum 2009;39:10–17. Orthop B 2009;18:225–7.
Copyright 2013 BMJ Publishing Group. All rights reserved. For permission to reuse any of this content visit
http://group.bmj.com/group/rights-licensing/permissions.
BMJ Case Report Fellows may re-use this article for personal use and teaching without any further permission.
Become a Fellow of BMJ Case Reports today and you can:
▸ Submit as many cases as you like
▸ Enjoy fast sympathetic peer review and rapid publication of accepted articles
▸ Access all the published articles
▸ Re-use any of the published material for personal use and teaching without further permission
For information on Institutional Fellowships contact consortiasales@bmjgroup.com
Visit casereports.bmj.com for more articles like this and to become a Fellow
Tassinari D, et al. BMJ Case Rep 2013. doi:10.1136/bcr.09.2011.4796 7
You might also like
- Piriformis Pyomyositis, An Unusual Presentation of Leg Pain Post Partum Case Report and Review of LiteratureDocument4 pagesPiriformis Pyomyositis, An Unusual Presentation of Leg Pain Post Partum Case Report and Review of Literaturesatyagraha84No ratings yet
- WhateverDocument3 pagesWhatevergaurav sharmaNo ratings yet
- Kolker, 2012, Osteomielitis Debido A SalmonellaDocument5 pagesKolker, 2012, Osteomielitis Debido A SalmonellaJavier Zuñiga AguilarNo ratings yet
- Spinal Tuberculosis Potts DiseaseDocument3 pagesSpinal Tuberculosis Potts Diseaseshrishti shadangiNo ratings yet
- Ovadia 2007Document7 pagesOvadia 2007uditNo ratings yet
- Kikuchi's Disease: Malathi Sathiyasekaran R. Varadharajan So. ShivbalanDocument3 pagesKikuchi's Disease: Malathi Sathiyasekaran R. Varadharajan So. Shivbalanzulfikar adiNo ratings yet
- Cervical Spine Tuberculosis: A Case ReportDocument3 pagesCervical Spine Tuberculosis: A Case ReportSabrina JonesNo ratings yet
- Ameratunga 2000Document3 pagesAmeratunga 2000pipilepew14No ratings yet
- 2020 Infantile Tuberculous Osteomyelitis of The Proximal TibiaDocument4 pages2020 Infantile Tuberculous Osteomyelitis of The Proximal TibiaMuhammad Muttaqee MisranNo ratings yet
- Spinal Epidural Abscess in Two CalvesDocument8 pagesSpinal Epidural Abscess in Two CalvesRachel AutranNo ratings yet
- Jurnal 4Document4 pagesJurnal 4Putri Maghfirah BahriNo ratings yet
- A Neonatal Septic Arthritis Case Caused by Klebsiella Pneumoniae - A Case ReportDocument2 pagesA Neonatal Septic Arthritis Case Caused by Klebsiella Pneumoniae - A Case Reportkartini ciatawiNo ratings yet
- Smith 1999Document8 pagesSmith 1999smithl25No ratings yet
- BCR 2019 231802Document4 pagesBCR 2019 231802Sarah Ariefah SantriNo ratings yet
- Case Report: Wouter Meersseman, Patrick Verschueren, Thomas Tousseyn, Rita de Vos, David CassimanDocument1 pageCase Report: Wouter Meersseman, Patrick Verschueren, Thomas Tousseyn, Rita de Vos, David Cassimanmafe alvarezNo ratings yet
- Calvarial Tuberculosis: E Ünüvar, F O Guz, B Sadiko Glu, M Sidal, Ü One S and S TetikkurtDocument2 pagesCalvarial Tuberculosis: E Ünüvar, F O Guz, B Sadiko Glu, M Sidal, Ü One S and S Tetikkurtkbianca26No ratings yet
- AaaaaaaDocument4 pagesAaaaaaaGeorgi GugicevNo ratings yet
- Mycobacterium Tuberculosis Monoarthritis of The Knee in Children: A Case ReportDocument8 pagesMycobacterium Tuberculosis Monoarthritis of The Knee in Children: A Case ReportBima Saphien AlpanaceaNo ratings yet
- Chronic Hematogenous OsteomyelitisDocument45 pagesChronic Hematogenous OsteomyelitisNur Jannah NasirNo ratings yet
- Pott DiseaseDocument6 pagesPott DiseaseMicah TuringanNo ratings yet
- 3I. Scoiuosis: AnomaliesDocument7 pages3I. Scoiuosis: AnomaliesValentina OprisanNo ratings yet
- Spinal TB SacrumDocument6 pagesSpinal TB SacrumfebriantaraNo ratings yet
- Multifocal Osteoarticular Tuberculosis in Children: Journal of Orthopaedic Surgery 2011 19 (3) :336-40Document5 pagesMultifocal Osteoarticular Tuberculosis in Children: Journal of Orthopaedic Surgery 2011 19 (3) :336-40Suci IryandaNo ratings yet
- Krastev 1Document7 pagesKrastev 1diditNo ratings yet
- Osteomyelitis of The Left Humerus With Secondary Septic Arthritis of TheShoulder Joint in Neonate A Case ReportDocument3 pagesOsteomyelitis of The Left Humerus With Secondary Septic Arthritis of TheShoulder Joint in Neonate A Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Mal de PottDocument6 pagesMal de PottROCIONo ratings yet
- Yersinia Enterocolitica: A Rare Cause of Infective EndocarditisDocument3 pagesYersinia Enterocolitica: A Rare Cause of Infective EndocarditisDIEGO FERNANDO TULCAN SILVANo ratings yet
- Mistaken Identity Reporting Two Cases of Rare Fo 2024 International JournalDocument7 pagesMistaken Identity Reporting Two Cases of Rare Fo 2024 International JournalRonald QuezadaNo ratings yet
- Ankylosing Spondylitis Review JournalDocument12 pagesAnkylosing Spondylitis Review Journaloccha_fun08100% (1)
- Generalized Tetanus: Clinical Case Report and Review of The LiteratureDocument5 pagesGeneralized Tetanus: Clinical Case Report and Review of The LiteratureSebastian Orlando MedinaNo ratings yet
- Case Report: Tuberculous Spondylitis: A Report of Different Clinical Scenarios and Literature UpdateDocument5 pagesCase Report: Tuberculous Spondylitis: A Report of Different Clinical Scenarios and Literature UpdatepuaanNo ratings yet
- Tuberculous Spondylitis PDFDocument5 pagesTuberculous Spondylitis PDFpuaanNo ratings yet
- Magini 2012Document5 pagesMagini 2012rossibNo ratings yet
- Whipple S DiseaseDocument12 pagesWhipple S DiseaseGrifanda HumairahNo ratings yet
- Colonic StenosisDocument3 pagesColonic StenosisBell SwanNo ratings yet
- Familial Aggregation of Primary Glomerulonephritis in An Italian Population Isolate: Valtrompia StudyDocument8 pagesFamilial Aggregation of Primary Glomerulonephritis in An Italian Population Isolate: Valtrompia Studym_kamenovaNo ratings yet
- Kawasaki DiseaseDocument14 pagesKawasaki DiseaseFransiskus Beat Batmomolin100% (1)
- AstraZeneca COVID-19 Vaccine and Guillain - Barre Syndrome in Tasmania PDFDocument5 pagesAstraZeneca COVID-19 Vaccine and Guillain - Barre Syndrome in Tasmania PDFMelissa GuerreroNo ratings yet
- Ijerph 18 05895Document13 pagesIjerph 18 05895JHon Hendrik TambunanNo ratings yet
- Splenic Abscess: Conservative Management in Children: Case ReportDocument2 pagesSplenic Abscess: Conservative Management in Children: Case ReportyutefupNo ratings yet
- Laryngeal TuberculosisDocument5 pagesLaryngeal TuberculosisastralmaniaNo ratings yet
- Laparoscopic Splenectomy For Pediatric Wandering Spleen - A Case ReportDocument11 pagesLaparoscopic Splenectomy For Pediatric Wandering Spleen - A Case ReportAdlyn Bea Albesa-BernaldezNo ratings yet
- Article or ReviewDocument3 pagesArticle or Reviewv-santNo ratings yet
- Jurnal Radiologi 1Document3 pagesJurnal Radiologi 1NoviLindriatiNo ratings yet
- Severe Plasmodium Knowlesi Infection With Multiorgan Involvement in North East Peninsular MalaysiaDocument5 pagesSevere Plasmodium Knowlesi Infection With Multiorgan Involvement in North East Peninsular MalaysiaLili YaacobNo ratings yet
- Acute Encephalopathy Preceding Infection: ShigellaDocument2 pagesAcute Encephalopathy Preceding Infection: ShigellaOasis LimitedNo ratings yet
- Spondilitis TBDocument14 pagesSpondilitis TBaswad 0008No ratings yet
- Primary Review: Psoas Abscess: Case of The LiteratureDocument3 pagesPrimary Review: Psoas Abscess: Case of The LiteratureDung Tran HoangNo ratings yet
- Pi Is 0272638698001097Document6 pagesPi Is 0272638698001097Mita AdrianiNo ratings yet
- JCM 11 05684 v2Document13 pagesJCM 11 05684 v2Qwerty AsdfghNo ratings yet
- Ajol File Journals - 76 - Articles - 114038 - Submission - Proof - 114038 901 318286 1 10 20150309Document2 pagesAjol File Journals - 76 - Articles - 114038 - Submission - Proof - 114038 901 318286 1 10 20150309alysNo ratings yet
- Subacute Transverse Myelitis Developed Depending On Lyme Disease: A Case ReportDocument3 pagesSubacute Transverse Myelitis Developed Depending On Lyme Disease: A Case ReportmuthmainnahNo ratings yet
- BrianDocument3 pagesBrianArdiansyah Yolanda PutraNo ratings yet
- Jawt 11 I 2 P 48Document3 pagesJawt 11 I 2 P 48Irma NoviantiNo ratings yet
- Lazaroni 16Document4 pagesLazaroni 16adiNo ratings yet
- Lancet 2000 p399Document2 pagesLancet 2000 p399Handris SupriadiNo ratings yet
- Congenital Insensitivity To Pain and Anhydrosis (CIPA) Syndrome A Report of 4 CasesDocument6 pagesCongenital Insensitivity To Pain and Anhydrosis (CIPA) Syndrome A Report of 4 CasesAhmad DiazNo ratings yet
- Acute Hypotonia in An Infant (2017)Document3 pagesAcute Hypotonia in An Infant (2017)nikos.alexandrNo ratings yet
- Pott's Puffy Tumor in A 12-Year-Old Boy: ReferencesDocument4 pagesPott's Puffy Tumor in A 12-Year-Old Boy: ReferencesssmasterNo ratings yet
- Rheumatology Multiple Choice Questions with ExplanationsFrom EverandRheumatology Multiple Choice Questions with ExplanationsRating: 4.5 out of 5 stars4.5/5 (6)
- Bleedng GIT HarrisonDocument4 pagesBleedng GIT HarrisonhiNo ratings yet
- Bab 8 EngDocument25 pagesBab 8 EnghiNo ratings yet
- Jogi - Hordoleum KalazionDocument4 pagesJogi - Hordoleum KalazionhiNo ratings yet
- AK Khurana - Hordoleum KalazionDocument3 pagesAK Khurana - Hordoleum KalazionhiNo ratings yet
- Stimulasi Otak Non-Invasif Untuk Gangguan Judi - Tinjauan SistematisDocument21 pagesStimulasi Otak Non-Invasif Untuk Gangguan Judi - Tinjauan SistematishiNo ratings yet
- Transport of Critically Ill: Himanshu Khurana, Yatin MehtaDocument9 pagesTransport of Critically Ill: Himanshu Khurana, Yatin MehtahiNo ratings yet
- Atrioventricular Nodal Reentrant Tachycardia: AvnrtDocument13 pagesAtrioventricular Nodal Reentrant Tachycardia: AvnrthiNo ratings yet
- Screenshot 2021-01-12 at 16.57.57Document36 pagesScreenshot 2021-01-12 at 16.57.57hiNo ratings yet
- High School Weekly Planner: - MinimalistDocument48 pagesHigh School Weekly Planner: - Minimalistjetlee estacion100% (1)
- Julia SlidesManiaDocument17 pagesJulia SlidesManiahiNo ratings yet
- Scanned With CamscannerDocument5 pagesScanned With CamscannerhiNo ratings yet
- Reading Comprehension SKILL 3: Answer DetailDocument7 pagesReading Comprehension SKILL 3: Answer DetailhiNo ratings yet
- 7.9.1.3 Soap Gizi: Reward Your CuriosityDocument1 page7.9.1.3 Soap Gizi: Reward Your CuriosityhiNo ratings yet
- Answerkey Longmancompletecourseforthetoefltest51 72 191123151625 PDFDocument22 pagesAnswerkey Longmancompletecourseforthetoefltest51 72 191123151625 PDFhiNo ratings yet
- Kursus 7 ReadingDocument7 pagesKursus 7 ReadinghiNo ratings yet
- Pain ManagementDocument1 pagePain ManagementhiNo ratings yet
- Kursus 7 Listening Part ADocument5 pagesKursus 7 Listening Part AhiNo ratings yet
- Izombie Rules (D20 Modern Variant Rule) : Zombie StatsDocument7 pagesIzombie Rules (D20 Modern Variant Rule) : Zombie StatsJames LewisNo ratings yet
- Are You Talkin' To Me - The Role of Culture in Crisis Management SensemakingDocument17 pagesAre You Talkin' To Me - The Role of Culture in Crisis Management SensemakingSongyin CaiNo ratings yet
- Kode IcdDocument1 pageKode IcdSintiaNo ratings yet
- Dengue FNCPDocument1 pageDengue FNCPleo0% (1)
- Bahasa Inggris: WWW - Senamptn.co - CCDocument4 pagesBahasa Inggris: WWW - Senamptn.co - CCamirahalimaNo ratings yet
- Endoscopy: Accepted ManuscriptDocument37 pagesEndoscopy: Accepted ManuscriptShivaraj S ANo ratings yet
- Medela Boon HospitalsDocument22 pagesMedela Boon HospitalsAkash RajNo ratings yet
- Kode DiagnosaDocument50 pagesKode DiagnosaRekam Medis RS Kartika CibadakNo ratings yet
- 8 - Lymphoproliferative DisordersDocument14 pages8 - Lymphoproliferative DisordersRegla Mailyn Perez PerezNo ratings yet
- Induction and Augmentation of LabourDocument73 pagesInduction and Augmentation of LabourSanthosh.S.U100% (4)
- Metabolic EncephalopathyDocument22 pagesMetabolic Encephalopathytricia isabellaNo ratings yet
- A Comprehensive Literature Review On The Clinical Presentation, and Management of The Pandemic Coronavirus Disease 2019 (COVID-19)Document18 pagesA Comprehensive Literature Review On The Clinical Presentation, and Management of The Pandemic Coronavirus Disease 2019 (COVID-19)Zihan Zetira100% (1)
- Physical Examination Form: Medications AllergiesDocument4 pagesPhysical Examination Form: Medications AllergiesIris Ann PhillipsNo ratings yet
- Measuring Particulate MattersDocument20 pagesMeasuring Particulate MattersJORDAN MALLARINo ratings yet
- We Are Intechopen, The World'S Leading Publisher of Open Access Books Built by Scientists, For ScientistsDocument25 pagesWe Are Intechopen, The World'S Leading Publisher of Open Access Books Built by Scientists, For ScientistsJosue GarciaNo ratings yet
- Asma 2020Document66 pagesAsma 2020sarifullatang laseNo ratings yet
- Recurrent Laryngeal Nerve Injury in Thyroid SurgeryDocument5 pagesRecurrent Laryngeal Nerve Injury in Thyroid SurgeryDiornald MogiNo ratings yet
- Usg Abdomen Pelvis MaleDocument2 pagesUsg Abdomen Pelvis MaleBhaktivedanta HospitalNo ratings yet
- Emotional and Behavioral DisordersDocument32 pagesEmotional and Behavioral DisordersMokonaNo ratings yet
- JETT Brochure LiftPlasma Ophtalmo EU 2019 3 Prev MinDocument4 pagesJETT Brochure LiftPlasma Ophtalmo EU 2019 3 Prev MinCecilia OurensNo ratings yet
- Incredible 5-Second Water-Hack Kills Food CravingsDocument4 pagesIncredible 5-Second Water-Hack Kills Food CravingsSteeven MartínezNo ratings yet
- NotesDocument4 pagesNotesDip ThapaNo ratings yet
- Retaining Primary Molars With Instrument Seperation A Case Report and Clinical GuideDocument5 pagesRetaining Primary Molars With Instrument Seperation A Case Report and Clinical GuideNguyễn QuỳnhNo ratings yet
- Unit 5 - 5.1 PP TAYLORDocument23 pagesUnit 5 - 5.1 PP TAYLORKrista KloseNo ratings yet
- Mask Order 2021Document1 pageMask Order 2021Leah MoreauNo ratings yet
- Onyenwe Et alHOUSEFLYDocument8 pagesOnyenwe Et alHOUSEFLYAsrock 1No ratings yet
- B2 - A - Cystic FibrosisDocument1 pageB2 - A - Cystic FibrosisfaisalNo ratings yet
- OHSMS AwarenessDocument12 pagesOHSMS AwarenessAbdul MueedNo ratings yet
- Simplified Mathematical Model of Glucose-Insulin SystemDocument12 pagesSimplified Mathematical Model of Glucose-Insulin SystemBrasoveanu GheorghitaNo ratings yet
- Perspectives and Application of Community Engagement, Solidarity and CitizenshipDocument5 pagesPerspectives and Application of Community Engagement, Solidarity and Citizenshipkimberson alacyangNo ratings yet