Professional Documents
Culture Documents
Intraventricular Glioblastoma
Uploaded by
Arif Susilo RahadiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Intraventricular Glioblastoma
Uploaded by
Arif Susilo RahadiCopyright:
Available Formats
[Downloaded free from http://www.asianjns.org on Monday, April 5, 2021, IP: 36.68.239.
94]
CASE REPORT
Intraventricular glioblastoma multiforme mimicking
meningioma and review of the literature
Ashis Patnaik, Sudhansu S. Mishra, Satya B. Senapati
Department of Neurosurgery, SCB Medical College and Hospital, Cuttack, Odisha, India
ABSTRACT
Glioblastoma multiforme (GBM) is the most common primary brain tumor and is usually found in aged persons in the
cerebral hemispheres particularly the frontotemporal region. But intraventricular GBM is rare and only few cases have been
reported in the literature. We report a case of a 27‑year‑old man who presented with headache, vision loss in both eyes,
and other signs and symptoms of increased intracranial pressure. Computed tomography and magnetic resonance imaging
showed an intraventricular, well‑circumscribed lesion with homogeneous enhancement of contrast, suggestive of meningioma
that is more common than GBM in this location. The patient underwent surgical removal through transcortical route. The
final pathologic diagnosis was GBM. We present the clinical features, radiological findings, and surgical management of
this case and discuss the pathogenesis and review of the literature of intraventricular GBM.
Key words: Glioblastoma multiforme, intraventricular, meningioma
Introduction postoperative adjuvant therapy as well as overall prognosis
of these two lesions.
Intraventricular tumors are uncommon, accounting only
1-10% of all brain tumors and include a variety of benign Case Report
tumors, malignant tumors, and cyst formations. Glioblastoma
multiforme, although, is the most common primary tumor A 27‑year‑old male patient presented to us with headache for
of brain accounting for nearly 20-25% of cases, it rarely last 2 years. The headache was gradually increasing in severity
occurs within ventricles. They are actually secondary tumors and since last 5 months, has become intense with associated
of ventricles arising from the structures adjacent to it and intermittent vomiting. There was progressive decline in visual
secondarily invading into the ventricles in an exophytic acuity in both eyes for last 3 months and patient became
manner. There have been reports of glioblastoma multiforme blind 1 month prior to admission. On physical examination,
in trigone, body, and occipital horn of the lateral ventricle[1‑7] the patient was conscious, oriented with loss of perception of
and in the third ventricle.[8] However, we could not find light in both eyes. Optic fundi showed secondary optic atrophy.
any report of frontal horn glioblastoma multiforme (GBM) There was no other significant neurologic finding.
in the literature. We report a case GBM in a young male
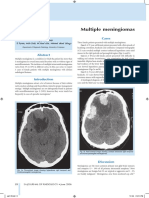
Computed tomography (CT) scan showed a well‑marginated,
patient showing radiological features suggestive of a more
iso‑ to hyperdense lesion in frontal horn and body of right
common benign lesion such as meningioma. The lesion
lateral ventricle with intense, homogeneous enhancement on
was completely excised and the histopathological study
contrast. MRI showed a well‑circumscribed lesion with regular
was consistent with GBM. There is a gross difference in the
margins showing gross enhancement and compressing the
foramen of Monroe producing hydrocephalus [Figures 1a-d].
Access this article online
MRS showed the decreased NAA level with the elevated choline
Quick Response Code:
Website: peak. But the ratio choline/creatinine was less than 2 which
www.asianjns.org
This is an open access article distributed under the terms of the Creative
Commons Attribution‑NonCommercial‑ShareAlike 3.0 License, which allows
DOI: others to remix, tweak, and build upon the work non‑commercially, as long as the
10.4103/1793-5482.145104 author is credited and the new creations are licensed under the identical terms.
For reprints contact: reprints@medknow.com
Address for correspondence : How to cite this article: Patnaik A, Mishra SS, Senapati SB.
Ashis Patnaik, Flat No. 313, Metro Manorama Complex, Intraventricular glioblastoma multiforme mimicking meningioma
Kathagola Sahi, Mangalabag, Cuttack, Odisha, India. and review of the literature. Asian J Neurosurg 2017;12:75-7.
E‑mail: dr_ash007@yahoo.co.in
75 © 2014 Asian Journal of Neurosurgery | Published by Wolters Kluwer - Medknow
[Downloaded free from http://www.asianjns.org on Monday, April 5, 2021, IP: 36.68.239.94]
Patnaik, et al.: Intraventricular GBM mimicking meningioma
was not typical of GBM. Ratio more than 3 is suggestive of a Fibrillary Acidic Protein [Figure 4]. The final diagnosis was
highly malignant lesion such as GBM. glioblastoma multiforme.
A right frontal transcortical approach taken. A highly vascular, Discussion
soft, friable tumor found protruding into the frontal horn of
right lateral ventricle. Near total tumor removal done in piece Glioblastoma multiforme is the most common primary brain
meal. Histopathology showed highly pleomorphic tumor tumor in adults and accounts for 15-20% of all intracranial
cells with increased cellularity, endothelial cell proliferation, tumors and approximately 50% of gliomas. Although it can
and nuclear palisading around central zone of necrosis arise anywhere in the CNS, nearly two-thirds are found in the
suggestive of glioblastoma multiforme [Figures 2 and 3]. fronto-temporal region. But, intraventricular GBM is relatively
Immunohistochemistry showed strong positivity toward Glial rare. It has been mentioned to be usually found predominantly
in the frontal horn or body of lateral ventricle in some reports;
however, such finding we could not find in any literature.
Intraventricular tumors have been classically divided
into two types according to their origin: Primary and
secondary. Neoplasms that arise from the ventricular wall
and its lining or from structures within the ventricles are
considered primary ventricular tumors, and ependymoma,
choroid plexus papilloma, choroid plexus carcinoma,
a b
c d
Figure 1: (a) T1‑weighted MRI showing the tumor in frontal horn
(b) T1 weighted sagittal MRI with gadolinium contrast showing well
circumscribed tumor with intense enhancement (c) Coronal contrast Figure 2: Nuclear palisading around areas of necrosis (arrow marks)
MRI (d) Axial contrast MRI of the tumor showing the extension of tumor with endovascular proliferation (arrow head)
to opposite frontal horn and body
Figure 4: Immunohistochemistry showing intense Glial Fibrillary Acidic
Figure 3: Highly pleomorphic tumor cells and increased cellularity Protein positivity
Asian Journal of Neurosurgery 76
Volume 12, Issue 1, January‑March 2017
[Downloaded free from http://www.asianjns.org on Monday, April 5, 2021, IP: 36.68.239.94]
Patnaik, et al.: Intraventricular GBM mimicking meningioma
meningioma belong to this group. Tumors that arise from report of a GBM in frontal horn in the literature. In both of
structures adjacent to the ventricle and gradually enlarge, their cases the tumor was located in trigone area. Sarsilmaz
so that more than two-thirds of them reside within the et al.[5] reported a pediatric GBM located in posterior body and
ventricle, are considered secondary ventricular tumors occipital horn of the left lateral ventricle. Seccer et al.[6] reported
with transependymal development. These tumors have nine cases of intraventricular GBM, out of which seven were
their origin primarily from the cerebral tissue. Gliomas in body and rest arising in septum pellucidum.
that include astrocytomas, subependymal giant cell
astrocytomas, other less common variants, including choroid Conclusion
glioma, glioblastoma multiforme, and mixed glial neuronal
Intraventricular tumors are relatively rarer, heterogeneous
tumors are included in this group.
group of tumors, presenting with nonspecific signs and
The area just below the ependymal lining of the ventricles is symptoms delaying their diagnosis. Glioblastoma multiforme,
called the subventricular zone (SVZ) and contains pluripotent although the most common primary intracranial tumor, is
stem cells that can give rise to ependymal cells as well relatively uncommon in this location in comparison to their
as various cells upon stimulation. According to Doetsch benign counterparts. In addition, they can present quite
et al. this zone contains as many as four distinct cell types; differently from their intracerebral component, both in
ependymal cells, astrocyte like type B cells, type C cells, and clinically and radiologically, thereby making their preoperative
oligodendrocyte progenitors. Genetic mutation followed diagnosis difficult. This case illustrates this by resembling a
by uncontrolled proliferation could lead to pathogenesis of meningioma, which shows a great difference in the prognosis.
malignant tumors such as glioblastoma multiforme in this So glioblastoma multiforme should be kept in the differential
rarer site. Once originated, these tumors could secondarily diagnosis of intraventricular tumor during preoperative
invade the ventricle through transependymal migration. management planning.
Most lateral ventricular tumors enlarge slowly and typically Financial support and sponsorship
cause no symptoms until reaching a size large enough to cause Nil.
obstructive hydrocephalus or compression of surrounding
Conflicts of interest
eloquent structures. Due to their aggressive behavior,
There are no conflicts of interest.
glioblastomas usually become symptomatic within a short
interval. This usually manifests as headache, vomiting, and References
other signs of increased intracranial pressure. In this case
the extreme degree of it led to complete blindness due to 1. Karmilov VO. Primary intraventricular brain tumor (glioblastoma
multiforme) in a child 2 years and 7 months. Pediatr Akus Ginekol
secondary optic atrophy. 1978;2:30.
2. Kim YJ, Lee SK, Cho MK, Kim YJ. Intraventricular glioblastoma
Radiologically, the glioblastomas usually show irregular, multiforme with previous history of intracerebral hemorrhage: A case
infiltrative borders with heterogeneous enhancement in form report. J Korean Neurosurg Soc 2008;44:405‑8.
3. Klein O, Marchal JC. Intraventricular glioblastoma: A paediatric case
of rim or peripheral enhancement of tumor tissue and areas
report. Br J Neurosurg 2007;21:411‑3.
of necrosis. However, in this case there was a well defined, 4. Park P, Choksi VR, Gala VC, Kaza AR, Murphy HS, Ramnath S.
round to oval, well circumscribed lesion showing homogeneous Well‑circumscribed, minimally enhancing glioblastoma multiforme
intense enhancement. This feature in a relatively young of the trigone; a case report and review of the literature. AJNR Am J
Neuroradiol 2005;26:1475‑8.
patient with long‑standing symptoms strongly suggested 5. Sarsilmaz A, Gelal F, Apaydin M, Varer M, Bezircioglu H, Rezanko T.
the diagnosis as meningioma. Intraoperatively the tumor Intraventricular glioblastoma multiforme: A pediatric case report.
was highly vascular, friable with lots of neo‑vascularization J Pediatr Hematol Oncol 2010;32:519‑22.
6. Seccer HI, Dinc C, Anik I, Duz B, Gonul E. Glioblastoma multiforme
suggestive of a malignant lesion. Histopathology confirmed of the lateral ventricle: Report of nine cases. Br J Neurosurg
the nature of lesion as glioblastoma multiforme. We could 2008;22:398‑401.
not find a report of glioblastoma in the frontal horn of lateral 7. Shapiro B. Intraventricular glioblastoma multiforme with the
ventricle in the literature. Although Park et al.[4] and Kim et al.[2] pneumographic characteristics of intraventricular epidermoids; a case
report with a critical analysis. Radiology 1950;55:852‑4.
mentioned that the glioblastoma in intraventricular location 8. Lee TT, Manzano GR. Third ventricular glioblastoma multiforme; case
are common in frontal horn or body, we could not find any report. Neurosurg Rev 1997;20:291‑4.
77 Asian Journal of Neurosurgery
Volume 12, Issue 1, January‑March 2017
You might also like
- Ectopic Choroid Plexus Papilloma: Case ReportDocument4 pagesEctopic Choroid Plexus Papilloma: Case ReportJosé MateusNo ratings yet
- Jurnal Radiologi 1Document9 pagesJurnal Radiologi 1Nia RwNo ratings yet
- 8 PDFDocument8 pages8 PDFAnonymous V4TNCnDbNo ratings yet
- Ajns - AJNS 268 19Document4 pagesAjns - AJNS 268 19Elmo KrisnawanNo ratings yet
- Extracranial Metastases of Anaplastic Meningioma: Case ReportDocument6 pagesExtracranial Metastases of Anaplastic Meningioma: Case ReportRizky AdriansahNo ratings yet
- Medi 101 E28665Document5 pagesMedi 101 E28665S Francisco MotNo ratings yet
- Surgical Neurology International: Unusual Growth Pattern of A MeningiomaDocument3 pagesSurgical Neurology International: Unusual Growth Pattern of A MeningiomaJamie NicholsNo ratings yet
- Late Recurrence of A Brain Tumor: Michael N. Needle,, Lucy B. Rorke,, and Peter WinklerDocument5 pagesLate Recurrence of A Brain Tumor: Michael N. Needle,, Lucy B. Rorke,, and Peter WinklerantonioopNo ratings yet
- 1 Neurosurgery Cases and ReviewsDocument5 pages1 Neurosurgery Cases and ReviewsintodoieblissNo ratings yet
- E - Uniform Round Tumour Cells With Small Nucleus and Clear Vacuolated CytoplasmDocument16 pagesE - Uniform Round Tumour Cells With Small Nucleus and Clear Vacuolated CytoplasmAien LeeNo ratings yet
- Sni 8 181Document14 pagesSni 8 181nabila shofia afifahNo ratings yet
- Imaging of Skull Base Tumors: Review ArticleDocument15 pagesImaging of Skull Base Tumors: Review ArticleBALEWNo ratings yet
- 3book ChaptersupratentorialbraintumorsinchildrenDocument13 pages3book ChaptersupratentorialbraintumorsinchildrenLuciano AlvesNo ratings yet
- Abdollahi Et AlDocument5 pagesAbdollahi Et AlMarc DaouNo ratings yet
- Otorhinolaryngology: Fibromatosis Colli or Pseudotumour of Sternocleidomastoid Muscle, A Rare Infantile Neck SwellingDocument3 pagesOtorhinolaryngology: Fibromatosis Colli or Pseudotumour of Sternocleidomastoid Muscle, A Rare Infantile Neck SwellingMohammedNo ratings yet
- Multiple Meningiomas Consisting of Fibrous Meningioma, Transitional Meningioma, and Meningotheliomatous Meningioma in One Adult PatientDocument2 pagesMultiple Meningiomas Consisting of Fibrous Meningioma, Transitional Meningioma, and Meningotheliomatous Meningioma in One Adult Patientrachel0301No ratings yet
- Multiple MeningiomasDocument3 pagesMultiple Meningiomasarun gowdaNo ratings yet
- A Rare Case of Space Occupying Lesion of Brainstem in An Elderly Male PatientDocument3 pagesA Rare Case of Space Occupying Lesion of Brainstem in An Elderly Male PatientInternational Journal of Clinical and Biomedical Research (IJCBR)No ratings yet
- LP Brain TumorDocument20 pagesLP Brain TumorMuhammad PanduNo ratings yet
- AsianJNeurosurg8121-7546405 205744Document8 pagesAsianJNeurosurg8121-7546405 205744WildaHanimNo ratings yet
- Laryngeal Plasmacytoma in Kahlers Disease: A Case ReportDocument6 pagesLaryngeal Plasmacytoma in Kahlers Disease: A Case ReportIJAR JOURNALNo ratings yet
- Pineal Germ Cell Tumors ReviewDocument6 pagesPineal Germ Cell Tumors ReviewWinda HaeriyokoNo ratings yet
- Ijar 2581 3919 5 131Document5 pagesIjar 2581 3919 5 131kireyna88 aNo ratings yet
- Surgical Neurology International: Cordectomy For Intramedullary Spinal Cord Glioblastoma With A 12 Year SurvivalDocument5 pagesSurgical Neurology International: Cordectomy For Intramedullary Spinal Cord Glioblastoma With A 12 Year Survivallucasnegromonte0001No ratings yet
- Rare Cause of Seizure MMDDocument4 pagesRare Cause of Seizure MMDGilbert Sterling OctaviusNo ratings yet
- EncephalitisDocument17 pagesEncephalitiseko andryNo ratings yet
- Primary Spinal Cord Glioblastoma Multiforme A Report of Two CasesDocument4 pagesPrimary Spinal Cord Glioblastoma Multiforme A Report of Two CasesginadaisluNo ratings yet
- Olfactory Groove MeningiomaDocument16 pagesOlfactory Groove Meningiomaclaudio RivasNo ratings yet
- Histological Subtypes and Anatomical Location SWMDocument7 pagesHistological Subtypes and Anatomical Location SWMYuwan RamjadaNo ratings yet
- Pathophysiology of Meningiomas 2003Document18 pagesPathophysiology of Meningiomas 2003Klinik medan DeliNo ratings yet
- Bulbo-Medullary Ependymoma in An Adult: Case ReportDocument6 pagesBulbo-Medullary Ependymoma in An Adult: Case ReportIJAR JOURNALNo ratings yet
- Letters: Kumar S, Nair S, Alexander MDocument2 pagesLetters: Kumar S, Nair S, Alexander MAbubakar BashirNo ratings yet
- Pediatric Desmoid Fibromatosis of TheDocument4 pagesPediatric Desmoid Fibromatosis of ThevatankhahpooyaNo ratings yet
- Ctoij MS Id 555925Document8 pagesCtoij MS Id 555925lucasnegromonte0001No ratings yet
- Imaging Findings of Intraventricular and Ependymal LesionsDocument16 pagesImaging Findings of Intraventricular and Ependymal Lesionsanggi abNo ratings yet
- Magnetic Resonance Imaging of Meningiomas: A Pictorial ReviewDocument10 pagesMagnetic Resonance Imaging of Meningiomas: A Pictorial ReviewKevin EdroNo ratings yet
- Intramedullary Spinal Cord TumorsDocument7 pagesIntramedullary Spinal Cord TumorsmutalimNo ratings yet
- Jkns 57 315Document8 pagesJkns 57 315arcobaleno589No ratings yet
- Absceso Cerebral en RN Asociado A Infeccion UmbilicalDocument5 pagesAbsceso Cerebral en RN Asociado A Infeccion UmbilicalAbrahamKatimeNo ratings yet
- MeningiomaDocument4 pagesMeningiomaHariyehNo ratings yet
- BMJ Case Reports-2014-Yi-bcr-2013-202851Document2 pagesBMJ Case Reports-2014-Yi-bcr-2013-202851mkfireNo ratings yet
- Synchronous Squamous Cell Carcinoma of The Lip and Nasopharyngeal Carcinoma - A Rare Case Report.Document4 pagesSynchronous Squamous Cell Carcinoma of The Lip and Nasopharyngeal Carcinoma - A Rare Case Report.International Journal of Innovative Science and Research Technology100% (1)
- Buka Folder JURNALDocument11 pagesBuka Folder JURNAL57z8crwcfjNo ratings yet
- 1009 Case 2Document4 pages1009 Case 2willygopeNo ratings yet
- Craniopharyngioma: Case SummaryDocument3 pagesCraniopharyngioma: Case SummaryeugeniaNo ratings yet
- Bakst 2018Document16 pagesBakst 2018tiaraNo ratings yet
- International 2Document4 pagesInternational 2daffunkmadansyahNo ratings yet
- Spinal Cord EnhancementDocument3 pagesSpinal Cord EnhancementGabriel PinillaNo ratings yet
- PROCEEDINGS OF THE PAEDlATRlC NEURO-ONCOLOGY TUMOUR BOARDDocument9 pagesPROCEEDINGS OF THE PAEDlATRlC NEURO-ONCOLOGY TUMOUR BOARDfriiday.qNo ratings yet
- AsianJNeurosurg102126-4310714 115827 PDFDocument3 pagesAsianJNeurosurg102126-4310714 115827 PDFSucipto HartonoNo ratings yet
- Biomedicines: Meningioma: A Review of Epidemiology, Pathology, Diagnosis, Treatment, and Future DirectionsDocument23 pagesBiomedicines: Meningioma: A Review of Epidemiology, Pathology, Diagnosis, Treatment, and Future DirectionsAlfian_Dwi_SNo ratings yet
- Meningioma Quístico, Un Desafío DiagnósticoDocument4 pagesMeningioma Quístico, Un Desafío DiagnósticoPamela WheelockNo ratings yet
- Spinal Tumors ArticleDocument5 pagesSpinal Tumors ArticleNouman Safdar AliNo ratings yet
- Spinal Tumors ArticleDocument5 pagesSpinal Tumors ArticleMariaLakhaniNo ratings yet
- Astrocytoma 10.1007/s00401-015-1410-7Document14 pagesAstrocytoma 10.1007/s00401-015-1410-7Rikizu HobbiesNo ratings yet
- Ijss Nov Oa28Document5 pagesIjss Nov Oa28Irsanti sasmitaNo ratings yet
- A 6-Month-Old Infant Girl Presents With Neck Stiffness: SciencedirectDocument2 pagesA 6-Month-Old Infant Girl Presents With Neck Stiffness: Sciencedirectbuco ufmaNo ratings yet
- 2020 - Jie Wei - Criptococoma Imitando Una Enfermedad DesmielinizanteDocument4 pages2020 - Jie Wei - Criptococoma Imitando Una Enfermedad DesmielinizanteEduardo RodriguezNo ratings yet
- Intramedullary Conus Medullaris Tuberculoma: A Case Report and Review of The LiteratureDocument7 pagesIntramedullary Conus Medullaris Tuberculoma: A Case Report and Review of The LiteratureanggipuspaNo ratings yet
- Fast Facts: Blastic Plasmacytoid Dendritic Cell Neoplasm: Shedding light on a rare diseaseFrom EverandFast Facts: Blastic Plasmacytoid Dendritic Cell Neoplasm: Shedding light on a rare diseaseNo ratings yet
- Neuro-Oncology: The 2021 WHO Classification of Tumors of The Central Nervous System: A SummaryDocument21 pagesNeuro-Oncology: The 2021 WHO Classification of Tumors of The Central Nervous System: A SummaryArif Susilo RahadiNo ratings yet
- Cardiac Surgery, The Brain, and Inflammation: Expert ReviewsDocument8 pagesCardiac Surgery, The Brain, and Inflammation: Expert ReviewsArif Susilo RahadiNo ratings yet
- Follicular Carcinoma of Thyroid Presenting As Brain MetastasisDocument3 pagesFollicular Carcinoma of Thyroid Presenting As Brain MetastasisArif Susilo RahadiNo ratings yet
- Jadwal Jaga ICU MARET 2021Document2 pagesJadwal Jaga ICU MARET 2021Arif Susilo RahadiNo ratings yet
- A Silent' Skull Metastatic Follicular Thyroid Carcinoma Mimicking As A Benign Scalp Tumor in A Pregnant WomanDocument6 pagesA Silent' Skull Metastatic Follicular Thyroid Carcinoma Mimicking As A Benign Scalp Tumor in A Pregnant WomanArif Susilo RahadiNo ratings yet
- Jadwal Jaga Ruangan April 2021Document2 pagesJadwal Jaga Ruangan April 2021Arif Susilo RahadiNo ratings yet
- Jadwal Jaga IGD April 2021 PerubahanDocument2 pagesJadwal Jaga IGD April 2021 PerubahanArif Susilo RahadiNo ratings yet
- Third Ventricular Papillary MeningiomaDocument4 pagesThird Ventricular Papillary MeningiomaArif Susilo RahadiNo ratings yet
- Jadwal Jaga Triase IGD April 2021Document2 pagesJadwal Jaga Triase IGD April 2021Arif Susilo RahadiNo ratings yet
- Translated Laporan Kasus Meningioma Spinal en Plaque IDEM Dengan KalsifikasiDocument7 pagesTranslated Laporan Kasus Meningioma Spinal en Plaque IDEM Dengan KalsifikasiArif Susilo RahadiNo ratings yet
- Tbi & Glasgow Coma Scale: Mandy FreemanDocument23 pagesTbi & Glasgow Coma Scale: Mandy FreemanArif Susilo RahadiNo ratings yet
- Kurva LubchencoDocument3 pagesKurva LubchencoDanil Armand67% (3)
- The Direction of The Wind and Its Effect On HealthDocument1 pageThe Direction of The Wind and Its Effect On HealthAnurag ChandNo ratings yet
- Brilliance iCT Technical BackgrounderDocument2 pagesBrilliance iCT Technical Backgroundermedgadget100% (4)
- Approach To The Patient With Facial Erythema PDFDocument38 pagesApproach To The Patient With Facial Erythema PDFFilipa FigueiredoNo ratings yet
- Cloning of Hybridoma Cell Lines by Limit PDFDocument2 pagesCloning of Hybridoma Cell Lines by Limit PDFMaha MardenliNo ratings yet
- Case Study For DMDocument5 pagesCase Study For DMJermeLou Bao100% (1)
- TMJ SlidesDocument113 pagesTMJ SlidesRah Ma GhassanNo ratings yet
- Ajnr Benign Enhancing Lesion of Foramen MagnumDocument5 pagesAjnr Benign Enhancing Lesion of Foramen Magnumapi-288086961No ratings yet
- Management of C Shaped Canals: 3 Case ReportsDocument3 pagesManagement of C Shaped Canals: 3 Case ReportsTaufiqurrahman Abdul Djabbar100% (1)
- Tren Tata Laksana Kanker Prostat PDFDocument18 pagesTren Tata Laksana Kanker Prostat PDFShannia FrnsNo ratings yet
- Epidemiology Sample QuestionsDocument2 pagesEpidemiology Sample QuestionsMoff NyabutoNo ratings yet
- Basic First Aid (Bfa)Document118 pagesBasic First Aid (Bfa)Hamza Moussa100% (1)
- Oral Care ProtocolDocument8 pagesOral Care ProtocolQonitaNurMiladiNo ratings yet
- Osce Notes - Rac - Safina AdatiaDocument35 pagesOsce Notes - Rac - Safina AdatiaTraventure 2000No ratings yet
- Complete Protein Antigens and Low - Molecular-Weight Substances - Complete Protein Antigens, Such As AnimalDocument1 pageComplete Protein Antigens and Low - Molecular-Weight Substances - Complete Protein Antigens, Such As AnimalApple BananaNo ratings yet
- Microbiology PneumoniaDocument31 pagesMicrobiology PneumoniaKartika Rezky100% (1)
- Algorithm GERD Primary Care Pathway Ahs SCN DH 2020 15262Document7 pagesAlgorithm GERD Primary Care Pathway Ahs SCN DH 2020 15262Mihaela ShimanNo ratings yet
- Hepatitis B: What Is It?Document2 pagesHepatitis B: What Is It?DrBertram ForerNo ratings yet
- Drug InteractionDocument151 pagesDrug Interactionapi-3724213100% (1)
- Es I Algorithm PosterDocument2 pagesEs I Algorithm Posterkusdiyah ningrumNo ratings yet
- 2011-2012 Annual Report Department of Pediatrics Saint Louis University School of MedicineDocument131 pages2011-2012 Annual Report Department of Pediatrics Saint Louis University School of Medicineslusompeds0% (1)
- Viral Skin InfectionsDocument28 pagesViral Skin Infectionstolesadereje73No ratings yet
- MS SDS SR Repo Ort: Name of S Model SampleDocument7 pagesMS SDS SR Repo Ort: Name of S Model SampleCamilo WispNo ratings yet
- Sesi 15-Making Your Hospital Baby FriendlyDocument47 pagesSesi 15-Making Your Hospital Baby FriendlySiti HajarNo ratings yet
- Cycles and Cycle Safety: Pegasus PharmaceuticalsDocument25 pagesCycles and Cycle Safety: Pegasus PharmaceuticalsMahmoud El Mohamdy100% (2)
- Health: Deepen: Vitex Negundo or Lagundi (Dangla)Document1 pageHealth: Deepen: Vitex Negundo or Lagundi (Dangla)Jio RillorazaNo ratings yet
- Science Form 3 PPTnewDocument9 pagesScience Form 3 PPTnewRedzuan SulaimanNo ratings yet
- TympanoplastyDocument4 pagesTympanoplastyMelly Selvia ANo ratings yet
- Canadian Pharmacy Review Ver1Document6 pagesCanadian Pharmacy Review Ver1Dr-Usman Khan30% (10)
- NOAC Trong Rung NhĩDocument23 pagesNOAC Trong Rung NhĩToan ngoNo ratings yet