Professional Documents
Culture Documents
Risk Factors Related To Falling in Stroke Patients: A Cross-Sectional Study
Uploaded by
Zilbran BerontaxOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Risk Factors Related To Falling in Stroke Patients: A Cross-Sectional Study
Uploaded by
Zilbran BerontaxCopyright:
Available Formats
J. Phys. Ther. Sci.
Original Article 27: 1751–1753, 2015
Risk factors related to falling in stroke patients:
a cross-sectional study
K ihun Cho, PT, PhD1), Jaeho Yu, PT, PhD2), Hyeonsook R hee, OT, PhD3)*
1) Department of Rehabilitative and Assistive Technology, Korea National Rehabilitation Research
Institute, Republic of Korea
2) Department of Physical Therapy, Sun Moon University, Republic of Korea
3) Department of Occupational Therapy, Shin Sung University: 1 Daehack-ro, Jungmi-myun,
Dangjin-city, Chungnam 343-861, Republic of Korea
Abstract. [Purpose] The purpose of this study was to investigate a comprehensive understanding of the fac-
tors associated with falls in poststroke patients. [Subjects] Forty-eight stroke patients (22 males and 26 females;
age 63.79 years) participated in this study. [Methods] This study applied a cross-sectional design. Fear of falling
[Falls Efficacy Scale (FES)], balance function [Berg Balance Scale (BBS) and Modified Rivermead Mobility Index
(MRMI)], ADL performance level [Modified Barthel Index (MBI)] and cognitive function [Loewenstein Occupa-
tional Therapy Cognitive Assessment for Geriatric Populations (LOTCA-G)] were assessed. [Results] Falls efficacy
was moderately correlated with ADL performance, balance, and cognition. In addition, stepwise linear regression
analysis revealed that ADL performance was the explanatory variable closely associated with falls efficacy in stroke
patients. [Conclusion] ADL performance was the primary explanatory variable of falls efficacy according to regres-
sion analysis. Thus, we suggest that these results may be used as basic data for developing rehabilitation programs
for prevention of falls in stroke patients.
Key words: Activities of daily living, Fall, Stroke
(This article was submitted Jan. 19, 2015, and was accepted Feb. 14, 2015)
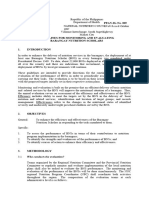
INTRODUCTION ly understand the factors associated with falls in poststroke
patients.
Falling is one of the most common complications of
stroke patients1, 2), and falling can lead to reduction of inde- SUBJECTS AND METHODS
pendence of activities of daily living such as eating, bathing,
dressing, toileting, and transferring in patients3). In addition, This study was a cross-sectional study using retrospective
falling is a leading cause of fractures for 23–50% of stroke analysis of records from patients admitted to a rehabilitation
patients4). Thus, understanding of falls risk is necessary department. Fifty-four stroke patients participated in this
for prevention of dependent ADL and secondary injuries. study. All patients underwent a standardized rehabilitation
Pevious studies demonstrated that depression and cogni- program consisting of physical and occupational therapy.
tive and physical function were associated with falling in The objectives and requirements of the study were ex-
stroke patients2, 4, 5). Krishchiunas and Savitskas reported plained to all patients, and they signed informed consent
that falls can interfere with functional recovery in stroke forms. This study, a retrospective review of the patients’
patients6), and Cho and Lee demonstrated that impaired medical records, was approved by the Institutional Re-
dynamic balance ability is associated with falls in stroke view Board of SunMoon University (SM-201410-030-2).
patients2). In particular, falling leads to the fear of falling Initial screening was performed using a medical chart.
and serious injuries such as a hip fracture and head injury7). Participants with a previous history of dementia, signifi-
Although some factors associated with falling of stroke cant difficulties in language expression or comprehension,
patients have been identified, the factors that can predict presence of other neurological disease, or inability to
prevented falls in stroke patients are still unclear. Thus, the provide informed consent were excluded. Six participants
purpose of this study was to investigate and comprehensive- were excluded because of difficulties in language ex-
pression (n=2), previous history of dementia (n=2), and
the inability to provide informed consent (n=2). Thus,
*Corresponding author. Hyeonsook Rhee (E-mail: eyerhee@ 48 participants were included in the final analysis.
hanmail.net) The fear of falling and balance were evaluated by
©2015 The Society of Physical Therapy Science. Published by IPEC Inc. physical therapists, and ADL performance and cogni-
This is an open-access article distributed under the terms of the Cre- tive function were evaluated by occupational therapists.
ative Commons Attribution Non-Commercial No Derivatives (by-nc- Fear of Falling was evaluated using the Falls Efficacy
nd) License <http://creativecommons.org/licenses/by-nc-nd/3.0/>. Scale (FES). The FES was designed to assess the degree
1752 J. Phys. Ther. Sci. Vol. 27, No. 6, 2015
of perceived efficacy at avoiding a fall during each of 10 RESULTS
relatively non-hazardous activities of daily living (tak-
ing a bath or shower, reaching into cabinets or closets, The clinical characteristics of the patients (22 females
preparing meals that do not require carrying heavy or hot and 26 males; average age 63.79 years) are shown in Table
objects, walking around the house, getting in and out of 1. Correlations between falls efficacy and variables are sum-
bed, answering the door or telephone, getting in and out marized in Table 2. Falls efficacy was moderately correlated
of a chair, getting dressed and undressed, light housekeep- with ADL performance (r=0.782, p<0.001), balance (BBS:
ing, and simple shopping). Each response was scored on r=0.669, p<0.001; MRMI: r=0.545, p<0.001), and cognition
a scale of 1 (completely confident) to 10 (no confidence), (r=0.667, p<0.001). In addition, stepwise linear regres-
with a high score indicating low falls self-efficacy8). sion analysis revealed that ADL performance (r2=0.758,
Balance was evaluated using the Berg Balance Scale (BBS) F=37.742, p<0.001) was the explanatory variable closely
and Modified Rivermead Mobility Index (MRMI). The BBS associated with falls efficacy in stroke patients.
is a valid and reliable instrument for measurement of both
the static and dynamic aspects of balance in elderly people DISCUSSION
after stroke9). The MRMI assesses 8 aspects of mobility
ranging from turning over in bed to managing stairs. Lennon Falls are common and recurrent problem in stroke
and Johnson tested the MRMI for face and content validity, patients and older adults4, 13). In particular, in the field of
and found that it had responsiveness (effect size = 1.15), stroke rehabilitation, it is important to consider a variety
test-retest reliability (r = 0.731), inter-rater reliability (ICC = of factors that can lead to a fall, such as the fear of fall-
0.98), and internal consistency (Cronbach’s alpha = 0.93)10).
ADL performance level was evaluated using the Modified
Barthel Index (MBI). The MBI is a measure of ADL that
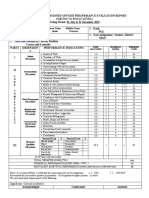
Table 1. Demographic data of the subjects (N=48)
shows the degree of independence of a patient. It covers 10
domains of functioning (activities): bowel control, bladder Variables Mean±SD
control, grooming, toilet use, feeding, transfers, walking, Gender
dressing, climbing stairs, and bathing11). Cognitive function Female /male (%) 22/26 (54.2/45.8)
was evaluated using the Loewenstein Occupational Therapy Affect side
Cognitive Assessment for Geriatric Populations (LOTCA- Left / right (%) 24/24 (50/50)
G). The LOTCA-G provides information about the patient’s
Type of stroke
abilities and deficiencies and about their capacity to cope with
Infarction/ hemorrhage (%) 31/17 (64.6/35.4)
daily and occupational tasks12). LOTCA-G consists of 7 major
areas containing 24 items. The areas investigated include ori- Age, years 63.7±10.7
entation, perception, praxis, visuomotor organization, think- Duration, days 389.1±236.1
ing operation, memory, attention, and concentration. Each MAS-U/E (0/1/1+/2) 26/12/5/5
subset is scored, and the total score ranges from 24 to 104. MAS-L/E (0/1/1+) 32/8/8
Data were analyzed using SPSS for Windows version 12.0 LOTCA -G, points 87.5±11.9
(SPSS Inc., Chicago, IL, USA). Pearson correlation coef- MBI, points 58.6±13.7
ficients were used to evaluate the relationships among the FES, points 64.1±18.5
variables. Stepwise linear regression analysis was used to
MRMI, points 34.1±4.4
elucidate the explanatory factor associated with falling.
BBS, points 37.2±11.1
Statistical significance was accepted for values of p < 0.05.
Data are presented as the mean with standard deviation (SD) SD: standard deviation; Duration: Days between stroke
onset and assessment; MAS: Modified Ashworth Scale;
values. LOTCA-G: Loewenstein Occupational Therapy Cogni-
tive Assessment for Geriatric Population; MBI: Modified
Barthel Index; FES: Falls Efficacy Scale; MRMI, Modi-
fied Rivermead mobility Index; BBS: Berg Balance Scale
Table 2. Correlation between variables (N=48)
FES BBS MRMI LOTCA-G MBI
FES
BBS 0.669**
MRMI 0.545** 0.703**
LOTCA-G 0.667** 0.425** 0.409**
MBI 0.782** 0.558** 0.372** 0.462**
FES: Falls Efficacy Scale; BBS: Berg Balance Scale; MRMI: Modified Rivermead mobility In-
dex; LOTCA-G: Loewenstein Occupational Therapy Cognitive Assessment for Geriatric Popu-
lation; MBI: Modified Barthel Index
**p<0.01
1753
ing, balance impairment, and cognitive dysfunction4, 14). 2) Cho K, Lee G: Impaired dynamic balance is associated with falling in
post-stroke patients. Tohoku J Exp Med, 2013, 230: 233–239. [Medline]
In addition, better understanding of the factors related to [CrossRef]
prevention of falling may assist in the development of stroke 3) Krebs HI, Mernoff S, Fasoli SE, et al.: A comparison of functional and
rehabilitation strategies and enhancement of independent impairment-based robotic training in severe to moderate chronic stroke: a
pilot study. NeuroRehabilitation, 2008, 23: 81–87. [Medline]
ambulation4, 6). Thus, the current study examined the
4) Harris JE, Eng JJ, Marigold DS, et al.: Relationship of balance and mobil-
risk factors associated with falling in poststroke patients. ity to fall incidence in people with chronic stroke. Phys Ther, 2005, 85:
In the current study, falls efficacy was positively correlated 150–158. [Medline]
with ADL performance, balance, and cognition. These find- 5) Teasell R, McRae M, Foley N, et al.: The incidence and consequences of
falls in stroke patients during inpatient rehabilitation: factors associated
ings are consistent with previous results indicating that with high risk. Arch Phys Med Rehabil, 2002, 83: 329–333. [Medline]
impairment of cognitive function and impairment of balance [CrossRef]
and self-care are the risk factors associated with falls15, 16). 6) Krishchiunas AI, Savitskas RI: [Falls in early in-patient rehabilitation of
Another interesting finding of the current study was that stroke patients]. Zh Nevrol Psikhiatr Im S S Korsakova, 2004, (Suppl 11):
47–50. [Medline]
regression analysis revealed that ADL performance was the 7) Dennis MS, Lo KM, McDowall M, et al.: Fractures after stroke: frequency,
primary explanatory variable of falls efficacy. The ultimate types, and associations. Stroke, 2002, 33: 728–734. [Medline] [CrossRef]
goal of stroke rehabilitation is for stroke patients to be able 8) Tinetti ME, Richman D, Powell L: Falls efficacy as a measure of fear of
falling. J Gerontol, 1990, 45: 239–243. [Medline] [CrossRef]
to independently perform ADL after returning to their com-
9) Blum L, Korner-Bitensky N: Usefulness of the Berg Balance Scale in
munities and homes17, 18), and prevention of falls is one of stroke rehabilitation: a systematic review. Phys Ther, 2008, 88: 559–566.
the most important factors for recovery of independent ADL [Medline] [CrossRef]
performance14). Thus, we suggest that detailed assessment 10) Lennon S, Johnson L: The modified rivermead mobility index: validity and
reliability. Disabil Rehabil, 2000, 22: 833–839. [Medline] [CrossRef]
of the ability of stroke patients to perform ADL is necessary, 11) Mahoney FI, Barthel DW: Functional evaluation: the Barthel Index. Md
and ADL training should be emphasized for prevention of fall State Med J, 1965, 14: 61–65. [Medline]
in stroke rehabilitation. In particular, monitoring of the ADL 12) Katz N, Itzkovich M, Averbuch S, et al.: Loewenstein Occupational Ther-
apy Cognitive Assessment (LOTCA) battery for brain-injured patients:
level may be helpful for predicting falls in stroke patients.
reliability and validity. Am J Occup Ther, 1989, 43: 184–192. [Medline]
Present study has several limitations. First, because a [CrossRef]
small number of subjects were recruited, the results of 13) van Helden S, Wyers CE, Dagnelie PC, et al.: Risk of falling in patients
this study cannot be generalized to all stroke patients. with a recent fracture. BMC Musculoskelet Disord, 2007, 8: 55. [Medline]
[CrossRef]
Second, despite the fact that several factors, such as 14) Rensink M, Schuurmans M, Lindeman E, et al.: [Falls: incidence and risk
changes in level of awareness, use of medication, lack factors after stroke. A systematic literature review]. Tijdschr Gerontol
of incontinence in the environment, and increased age, Geriatr, 2009, 40: 156–167. [Medline] [CrossRef]
may contribute to falling19), it was not considered in this 15) Chen X, Van Nguyen H, Shen Q, et al.: Characteristics associated with
recurrent falls among the elderly within aged-care wards in a tertiary hos-
study. Further investigation is required on this issue. pital: the effect of cognitive impairment. Arch Gerontol Geriatr, 2011, 53:
In conclusion, we found that the ADL level may be useful e183–e186. [Medline] [CrossRef]
for monitoring falls in poststroke patients. We suggest that 16) Campbell GB, Matthews JT: An integrative review of factors associated
with falls during post-stroke rehabilitation. J Nurs Scholarsh, 2010, 42:
these results may be used as basic information for develop-
395–404. [Medline] [CrossRef]
ing rehabilitation programs for prevention of falls in stroke 17) Ozdemir F, Birtane M, Tabatabaei R, et al.: Cognitive evaluation and func-
patients. tional outcome after stroke. Am J Phys Med Rehabil, 2001, 80: 410–415.
[Medline] [CrossRef]
18) Cho K, Lee W: Cognitive factors associated with activities of daily living
REFERENCES
in post-stroke patients. J Phys Ther Sci, 2012, 24: 779–782. [CrossRef]
19) Diccini S, de Pinho PG, da Silva FO: Assessment of risk and incidence
1) Shim S, Yu J, Jung J, et al.: Effects of dual-task performance on postural of falls in neurosurgical inpatients. Rev Lat Am Enfermagem, 2008, 16:
sway of stroke patients with experience of falls. J Phys Ther Sci, 2012, 24: 752–757. [Medline] [CrossRef]
975–978. [CrossRef]
You might also like
- Geriatric Anxiety Scale v2.0 FINALDocument2 pagesGeriatric Anxiety Scale v2.0 FINALpujipurwaningsih67% (3)
- Bates-Jensen Wound Assessment Tool (BWAT)Document4 pagesBates-Jensen Wound Assessment Tool (BWAT)Jamie OngNo ratings yet
- CS1 Assignment Y2 2020 Answer Booklet 12345Document4 pagesCS1 Assignment Y2 2020 Answer Booklet 12345Deepanshu Sharma0% (1)
- Cambridge CertificateDocument2 pagesCambridge Certificateapi-322275865No ratings yet
- Developing A Utility Index For The Aberrant Behavior Checklist (ABC-C) For Fragile X SyndromeDocument10 pagesDeveloping A Utility Index For The Aberrant Behavior Checklist (ABC-C) For Fragile X SyndromeIke Kashaka TshikungNo ratings yet
- Lesson Plan For Introduction To Vector MathDocument1 pageLesson Plan For Introduction To Vector MathLeonardo MuñozNo ratings yet
- Research Article: Prognostic Factors of Functional Recovery From Left Hemispheric StrokeDocument8 pagesResearch Article: Prognostic Factors of Functional Recovery From Left Hemispheric Strokepokharelriwaj82No ratings yet
- Adobe Scan 02 Mar 2023Document18 pagesAdobe Scan 02 Mar 2023ciptakarwanaNo ratings yet
- Mckee 2012Document10 pagesMckee 2012Reda SoNo ratings yet
- Roy Adaptation Model Extremities Amputation PDFDocument7 pagesRoy Adaptation Model Extremities Amputation PDFIntan SariNo ratings yet
- 6-1Document8 pages6-1Elahe SadeqiNo ratings yet
- Rotator Cuff Repair vs. Nonoperative Treatment - 2021 (Tema 3)Document12 pagesRotator Cuff Repair vs. Nonoperative Treatment - 2021 (Tema 3)Carlos NoronaNo ratings yet
- Gum Mess On 2003Document6 pagesGum Mess On 2003fajarcolzzzNo ratings yet
- Stroke 32Document8 pagesStroke 32pokharelriwaj82No ratings yet
- Self-Efficacy in Relation To Impairments and Activities of Daily Living Disability in Elderly Patients With Stroke: A Prospective InvestigationDocument6 pagesSelf-Efficacy in Relation To Impairments and Activities of Daily Living Disability in Elderly Patients With Stroke: A Prospective InvestigationUliuliauliaNo ratings yet
- 2021 - QoL in MSisdominated by Fatigue - Disability - Sefl-EfficacyDocument7 pages2021 - QoL in MSisdominated by Fatigue - Disability - Sefl-EfficacySM199021No ratings yet
- Katzan Et AlDocument9 pagesKatzan Et Alemsutton02No ratings yet
- Acl Rehab ProtocolDocument6 pagesAcl Rehab ProtocolPricy DevNo ratings yet
- Review 2013Document11 pagesReview 2013marioNo ratings yet
- Physiotherapy Intervention in Alzheimer'sDocument12 pagesPhysiotherapy Intervention in Alzheimer'sRestu AryaNo ratings yet
- Functioning of Stroke Survivors - A Validation of The ICF Core Set For Stroke in SwedenDocument9 pagesFunctioning of Stroke Survivors - A Validation of The ICF Core Set For Stroke in SwedenMuhammadMusa47No ratings yet
- Self-Efficacy Correlates with Independence in Stroke SurvivorsDocument7 pagesSelf-Efficacy Correlates with Independence in Stroke SurvivorsSitti Rosdiana YahyaNo ratings yet
- Cirugía de HAV y Calidad de VidaDocument8 pagesCirugía de HAV y Calidad de VidaAlejandro Fernandez GibelloNo ratings yet
- Kta ArticleDocument6 pagesKta Articleapi-291380671No ratings yet
- Stroke AFRDocument9 pagesStroke AFRPrasasti 19No ratings yet
- Hospitalized Older Adult Predictors of Functional DeclineDocument10 pagesHospitalized Older Adult Predictors of Functional DeclineMauricio LorcaNo ratings yet
- ArticleDocument11 pagesArticlejesica_loNo ratings yet
- Application of Clinical Nursing Pathway Table of Pulmonary Management in Patients With Adolescent Idiopathic ScoliosisDocument6 pagesApplication of Clinical Nursing Pathway Table of Pulmonary Management in Patients With Adolescent Idiopathic Scoliosis605706503No ratings yet
- Fall Prediction in Neurological Gait Disorders DifDocument15 pagesFall Prediction in Neurological Gait Disorders DifRudolfGerNo ratings yet
- Yjmt 30 1992090Document13 pagesYjmt 30 1992090Luis Sebastian Arango OspinaNo ratings yet
- 4-1Document9 pages4-1Elahe SadeqiNo ratings yet
- Akizuki Et Al.Document6 pagesAkizuki Et Al.Dries Van ThielenNo ratings yet
- Jurnal Demensia 5Document9 pagesJurnal Demensia 5Mutiara Anak NegeriNo ratings yet
- Poststroke Depression: Prevalence and Determinants in Brazilian Stroke PatientsDocument10 pagesPoststroke Depression: Prevalence and Determinants in Brazilian Stroke PatientsGrace KahonoNo ratings yet
- Gye Yeop Kim Et Al 2014Document6 pagesGye Yeop Kim Et Al 2014maria.castiyo2002No ratings yet
- Ggi 13069Document7 pagesGgi 13069putriNo ratings yet
- PDF 60574 4818Document13 pagesPDF 60574 4818QuiroprácticaParaTodosNo ratings yet
- Lee 2018Document7 pagesLee 2018Kings AndrewNo ratings yet
- Neuromuscular Electrical Stimulation Improves Muscle Strength Biomechanicsof Movementand Functional MobilityDocument19 pagesNeuromuscular Electrical Stimulation Improves Muscle Strength Biomechanicsof Movementand Functional MobilityAmr Mohamed GalalNo ratings yet
- Frailty and Exercise Training - How To Provide Best Care After Cardiac Surgery or Intervention For Elder Patients With Valvular Heart Disease 2018Document36 pagesFrailty and Exercise Training - How To Provide Best Care After Cardiac Surgery or Intervention For Elder Patients With Valvular Heart Disease 2018Josemi Del Castillo MolinaNo ratings yet
- Aquatic Therapy For MsDocument7 pagesAquatic Therapy For MsmadeNo ratings yet
- Journal 2Document5 pagesJournal 2nandhini raguNo ratings yet
- Rehabilitation in Patients With Rheumatoid Arhtritis 61 74Document14 pagesRehabilitation in Patients With Rheumatoid Arhtritis 61 74Yustia Ika WardhaniNo ratings yet
- Do measures of reactive balance control predict falls in people with stroke returningDocument12 pagesDo measures of reactive balance control predict falls in people with stroke returningElahe SadeqiNo ratings yet
- Abstract Leftsidest SetDocument1,047 pagesAbstract Leftsidest Setpokharelriwaj82No ratings yet
- Clinical Efficacy of Mechanical Traction As Physical Therapy For Lumbar Disc Herniation - Meta AnalysisDocument8 pagesClinical Efficacy of Mechanical Traction As Physical Therapy For Lumbar Disc Herniation - Meta AnalysissamNo ratings yet
- Alp Tekin 2016Document6 pagesAlp Tekin 2016Anisah Imansari RahayuNo ratings yet
- Main 25Document6 pagesMain 25pokharelriwaj82No ratings yet
- Rheumatoid Arthritis - Assessment of Functional Performances of The PatientsDocument14 pagesRheumatoid Arthritis - Assessment of Functional Performances of The PatientsK. Vijay AnanthNo ratings yet
- Review of Effects of Physical Activity On Strength, Balance, Mobility and ADL Performance in Elderly Subjects With DementiaDocument11 pagesReview of Effects of Physical Activity On Strength, Balance, Mobility and ADL Performance in Elderly Subjects With DementiaAlejandra VasquezNo ratings yet
- ISPR8-1352: Posters (First Part) / Annals of Physical and Rehabilitation Medicine 61S (2018) E103-E308 E219Document1 pageISPR8-1352: Posters (First Part) / Annals of Physical and Rehabilitation Medicine 61S (2018) E103-E308 E219Amal VRNo ratings yet
- 2019 Comparable Walking Gait PerformanceDocument5 pages2019 Comparable Walking Gait Performancesiyueli826No ratings yet
- 2008 - Feigin - Long Term Neuropsychological Functional Outcomes StrokeDocument8 pages2008 - Feigin - Long Term Neuropsychological Functional Outcomes StrokeLourdes CFNo ratings yet
- Jurnal GerontikDocument8 pagesJurnal GerontikLIZBETH FEMMIL SAPUTRINo ratings yet
- Intervention:: American Occupational Therapy Association Evidence-Based Literature Review Project/Evidence Table.5-06Document5 pagesIntervention:: American Occupational Therapy Association Evidence-Based Literature Review Project/Evidence Table.5-06nkdewittNo ratings yet
- The Swedish Occupational Fatigue Inventory in People With Multiple SclerosisDocument7 pagesThe Swedish Occupational Fatigue Inventory in People With Multiple SclerosisikrambahariNo ratings yet
- Bab 2Document2 pagesBab 2SANDA NABILAH FATINNo ratings yet
- Rodríguez-Hernández Et Al. - 2021 - Effects of Specific Virtual Reality-Based TherapyDocument15 pagesRodríguez-Hernández Et Al. - 2021 - Effects of Specific Virtual Reality-Based TherapyMARIA TERAPEUTANo ratings yet
- Impact of Physical Activity On Disability Risk inDocument7 pagesImpact of Physical Activity On Disability Risk inLyrian LohNo ratings yet
- Stroke RehabilitationDocument10 pagesStroke RehabilitationPethuel Pomaloy100% (1)
- STROKE REHABILITATION EVIDENCEDocument36 pagesSTROKE REHABILITATION EVIDENCEMarikit2012No ratings yet
- Activities of Daily Living and Quality of Life in Persons With Muscular DystrophyDocument6 pagesActivities of Daily Living and Quality of Life in Persons With Muscular DystrophyHenry wijaya oeijNo ratings yet
- Review Article Extracorporeal Shock Wave Therapy For The Treatment of Osteoarthritis: A Systematic Review and Meta-AnalysisDocument15 pagesReview Article Extracorporeal Shock Wave Therapy For The Treatment of Osteoarthritis: A Systematic Review and Meta-Analysissymbiosis.ikfrNo ratings yet
- Interventions for Autism: Evidence for Educational and Clinical PracticeFrom EverandInterventions for Autism: Evidence for Educational and Clinical PracticeNo ratings yet
- Psychophysiological assessment of human cognition and its enhancement by a non-invasive methodFrom EverandPsychophysiological assessment of human cognition and its enhancement by a non-invasive methodNo ratings yet
- Self-directed Learning Skills in Honduras Compared to the United StatesDocument19 pagesSelf-directed Learning Skills in Honduras Compared to the United StatesZilbran BerontaxNo ratings yet
- Role of Bacterial Infections in Pancreatic Cancer: ReviewDocument5 pagesRole of Bacterial Infections in Pancreatic Cancer: ReviewZilbran BerontaxNo ratings yet
- Understanding Doctoral Nursing Students' Experiences of Blended LearningDocument8 pagesUnderstanding Doctoral Nursing Students' Experiences of Blended LearningZilbran BerontaxNo ratings yet
- Self-Directed Learning Methods On Nursing Education: A Literature ReviewDocument8 pagesSelf-Directed Learning Methods On Nursing Education: A Literature ReviewZilbran BerontaxNo ratings yet
- Speech and Language Therapy For Aphasia Following Subacute StrokeDocument6 pagesSpeech and Language Therapy For Aphasia Following Subacute StrokeZilbran BerontaxNo ratings yet
- Transtition To Blended LearningDocument17 pagesTranstition To Blended LearningZilbran BerontaxNo ratings yet
- The Effects of Blended Learning On Knowledge, Skills, and Satisfaction Innursing Students A Meta-AnalysisDocument7 pagesThe Effects of Blended Learning On Knowledge, Skills, and Satisfaction Innursing Students A Meta-AnalysisZilbran BerontaxNo ratings yet
- The Self-Directed Learning Readiness Level of The Undergraduate Students of Midwife and Nurse in Terms of Sustainability in Nursing and Midwifery EducationDocument14 pagesThe Self-Directed Learning Readiness Level of The Undergraduate Students of Midwife and Nurse in Terms of Sustainability in Nursing and Midwifery EducationZilbran BerontaxNo ratings yet
- Blended Learning (Research Article)Document12 pagesBlended Learning (Research Article)Andrés Espinoza100% (1)
- The Impact of Blended Teaching On Knowledge, Satisfaction, and Self-Directed Learning in Nursing Undergraduates: A Randomized, Controlled TrialDocument7 pagesThe Impact of Blended Teaching On Knowledge, Satisfaction, and Self-Directed Learning in Nursing Undergraduates: A Randomized, Controlled TrialJefry ArieNo ratings yet
- Bencana 1Document14 pagesBencana 1Andhi SNo ratings yet
- Validation of Self-Directed LearningDocument11 pagesValidation of Self-Directed LearningZilbran BerontaxNo ratings yet
- Effectiveness of A Self-Directed LearningDocument8 pagesEffectiveness of A Self-Directed LearningZilbran BerontaxNo ratings yet
- Simulation Videos Presented in A Blended Learning Platform ToDocument27 pagesSimulation Videos Presented in A Blended Learning Platform ToZilbran BerontaxNo ratings yet
- The Impact of The Learning Contract On Self-Directed LearningDocument5 pagesThe Impact of The Learning Contract On Self-Directed LearningZilbran BerontaxNo ratings yet
- Self-Directed Learning A Tool For Lifelong LearningDocument15 pagesSelf-Directed Learning A Tool For Lifelong LearningZilbran BerontaxNo ratings yet
- Effect of Self-Directed Learning On Nursing Students' Readiness, Perception and Performance in SudanDocument10 pagesEffect of Self-Directed Learning On Nursing Students' Readiness, Perception and Performance in SudanZilbran BerontaxNo ratings yet
- LR SDL - 7. OutDocument7 pagesLR SDL - 7. OutAnggita Nandya ArdiatiNo ratings yet
- Effect of Self-Directed Learning On Nursing Students' Readiness, Perception and Performance in SudanDocument10 pagesEffect of Self-Directed Learning On Nursing Students' Readiness, Perception and Performance in SudanZilbran BerontaxNo ratings yet
- Effect of Blended Learning On Newly Nursing Student's Outcomes Regarding New Trends in Nursing Subject at Ain Shams UniversityDocument9 pagesEffect of Blended Learning On Newly Nursing Student's Outcomes Regarding New Trends in Nursing Subject at Ain Shams UniversityZilbran BerontaxNo ratings yet
- Scientific Information System: Network of Scientific Journals From Latin America, The Caribbean, Spain and PortugalDocument12 pagesScientific Information System: Network of Scientific Journals From Latin America, The Caribbean, Spain and PortugalZilbran BerontaxNo ratings yet
- Measure Nursing Student Self-Directed Learning AbilitiesDocument8 pagesMeasure Nursing Student Self-Directed Learning AbilitiesZilbran BerontaxNo ratings yet
- Concurrent Validity of Self-Rating Scale ofDocument11 pagesConcurrent Validity of Self-Rating Scale ofZilbran BerontaxNo ratings yet
- Exploratory Study of The Relationship Between Self-Directed Learning and Academic Performance in A Web - Based Learning EnvironmentDocument11 pagesExploratory Study of The Relationship Between Self-Directed Learning and Academic Performance in A Web - Based Learning EnvironmentZilbran BerontaxNo ratings yet
- Effect of Blended Learning On Newly Nursing Student's Outcomes Regarding New Trends in Nursing Subject at Ain Shams UniversityDocument9 pagesEffect of Blended Learning On Newly Nursing Student's Outcomes Regarding New Trends in Nursing Subject at Ain Shams UniversityZilbran BerontaxNo ratings yet
- Blended Versus Lecture LearningDocument5 pagesBlended Versus Lecture LearningZilbran BerontaxNo ratings yet
- Blended Learning The New Normal and Emerging Technologies PDFDocument16 pagesBlended Learning The New Normal and Emerging Technologies PDFBagas Annas UtomoNo ratings yet
- Blended Learning in High School Chemistry ToDocument11 pagesBlended Learning in High School Chemistry ToZilbran BerontaxNo ratings yet
- Down Syndrome and AutismDocument8 pagesDown Syndrome and AutismChristine Joy GonzalesNo ratings yet
- IIC Annual Report 2021-22Document30 pagesIIC Annual Report 2021-22Aeronautical ACSCENo ratings yet
- Detailed Lesson Plan in Science ViDocument6 pagesDetailed Lesson Plan in Science ViJustin Ace MallorcaNo ratings yet
- Ratee's Name Last Name, Given Name Middle Name Galvez Jessie PanaresDocument2 pagesRatee's Name Last Name, Given Name Middle Name Galvez Jessie PanaresMeredith GalvezNo ratings yet
- Dualtech Training Center Presentation RVSADocument17 pagesDualtech Training Center Presentation RVSADennis SalongaNo ratings yet
- Heads Up 2023Document6 pagesHeads Up 2023api-39965614No ratings yet
- Dream Tending - What It IsDocument3 pagesDream Tending - What It IsNick JudsonNo ratings yet
- DepEd Order On Time Allotment Per Learning Areas - TeacherPHDocument1 pageDepEd Order On Time Allotment Per Learning Areas - TeacherPHsjnhs SPANo ratings yet
- Download ebook Intermediate Macroeconomics Pdf full chapter pdfDocument67 pagesDownload ebook Intermediate Macroeconomics Pdf full chapter pdfjulia.castro488100% (27)
- Report Assessment 1 CSC264 - Muhammad Hafiz Imran Bin AhmadDocument9 pagesReport Assessment 1 CSC264 - Muhammad Hafiz Imran Bin AhmadMUHD HAFIZ IMRAN BIN AHMADNo ratings yet
- Ead-519 Dress Code Case AnalysisDocument4 pagesEad-519 Dress Code Case Analysisapi-642173798No ratings yet
- NAPLAN Yr 9 Numeracy Test-3 CalcAllowedDocument11 pagesNAPLAN Yr 9 Numeracy Test-3 CalcAllowedLeezaNo ratings yet
- Bns Accomplishment ReportDocument4 pagesBns Accomplishment ReportRaquel ParcareyNo ratings yet
- Black History Month LessonDocument11 pagesBlack History Month LessonJ JohnsonNo ratings yet
- Introduction to Symposium on Public Service Motivation ResearchDocument3 pagesIntroduction to Symposium on Public Service Motivation ResearchHumberto RiveraNo ratings yet
- Applications OF Artificial Intelligence FOR Organic ChemistryDocument203 pagesApplications OF Artificial Intelligence FOR Organic ChemistryMichael RoseNo ratings yet
- Managing For Quality and Performance Excellence, 9E, © 2014 Cengage PublishingDocument46 pagesManaging For Quality and Performance Excellence, 9E, © 2014 Cengage PublishingWilsonNo ratings yet
- Week 9-Gagarin, Jophnel Noa B.Document3 pagesWeek 9-Gagarin, Jophnel Noa B.JOPHNEL NOA GAGARINNo ratings yet
- Bahasa Inggris (Iklan Pekerjaan)Document5 pagesBahasa Inggris (Iklan Pekerjaan)AndreNo ratings yet
- PEpC 1Document44 pagesPEpC 1Claudio Makarovsky100% (1)
- IntroductionDocument6 pagesIntroductionNigel KowNo ratings yet
- Create New Java Red5 Application - TsavoDocument38 pagesCreate New Java Red5 Application - TsavoFabrizio TorelliNo ratings yet
- CV AnalysisDocument6 pagesCV Analysisbaniyash1204No ratings yet
- UAE4 School List4Document82 pagesUAE4 School List4Javeed MohiuddinNo ratings yet
- IATF Internal Auditor 2019Document1 pageIATF Internal Auditor 2019Prakash kumarTripathiNo ratings yet
- Intro to Philosophy of Human Person Chapter 1Document90 pagesIntro to Philosophy of Human Person Chapter 1Adrian Nicole DionisioNo ratings yet
- Accreditation of CME Programme As Approved by Governing Body of U P Medical Council, Lucknow On 11 April 2012Document9 pagesAccreditation of CME Programme As Approved by Governing Body of U P Medical Council, Lucknow On 11 April 2012GauravChopraNo ratings yet