Professional Documents
Culture Documents
Ignatius Yansen: RSU Kabupaten Tangerang
Uploaded by
Fitria Arifin0 ratings0% found this document useful (0 votes)
8 views28 pagesOriginal Title
3. RBBB
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
8 views28 pagesIgnatius Yansen: RSU Kabupaten Tangerang
Uploaded by
Fitria ArifinCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 28
Ignatius Yansen
RSU Kabupaten Tangerang
Intrinsic impairment of conduction in the right
bundle branches
Can be chronic or intermittent
Can be rate dependant
Can be present without cardiac disease
Most often due to CAD or HTN causing ischemic or
degenerative changes
Best recognized in precordial leads V1-V6
Wide QRS complex > 0.12 s
V1:
Large terminal R’ waves with rR’ or rsR’ configuration
Onset of intrinsicoid deflection (R peak time) > 0.05 s
V6:
Wide terminal S waves are present
Septal q waves are preserved
No Axis changing
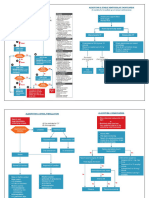
Physiologically On ECG
Unblocked R
ventricle R’
Blocked
ventricle
Two QRS’s out of ‘sync’ Single, wide QRS
• The initial QRS deflection
represents the septum
depolarizing from left to right.
This conduction is mediated by
the septal fascicle arising from
the left bundle branch
• The initial QRS is unchanged in
RBBB because conduction is
independent of the right bundle
branch
• Following the initial QRS, the left
ventricle rapidly depolarizes via
conduction from the LAF and LPF.
• The right ventricle is delayed.
• This produces a QRS vector oriented
to the left and posterior.
• The left ventricle is normally
dominant during the QRS and thus
the EKG still shows no abnormally
• Following left ventricular depolarization,
there continues to be delayed
depolarization of the right ventricle via
slow myocyte-to-myocyte spread.
• The right ventricle is now the dominate
electrical force and therefore the
terminal QRS vector is oriented to the
right and anterior. This shows on an ECG
as an additional tall upright R’ wave in V1
and a deep S wave in V6.
Initial QRS remains
normal
Middle portion of
QRS remains normal
Terminal QRS is
sluggish and
dominated by right
ventricular forces
V1 = rSR’
V6 = qRS
Uncomplicated: ST segment and T waves
normally discordant and opposite in direction
to the terminal portion of QRS complex.
Myocardial abnormality: ST and T waves are
concordant with the terminal portion of QRS
complex cardiomyopathy, myocardial
ischemia
Incomplete RBBB has all the features of RBBB
except duration of QRS complex < 0.12 s
RBBB often intermittent before it becomes
fixed. Usually rate related
Incidence increases with age
Can occur as a normal variant
Most common cause is CAD (LAD)
Other causes include both structural and functional causes
Structural: anything causing RV dilatation or
hypertrophy, (acute PE, cor pulmonale, DCM, ect),
trauma (right heart cath, steering wheel, CABG,
ablation)
Functional: rate-related bundle branch block
Myocardial infarction
Pulmonary embolism
Chronic obstructive lung disease/cor pulmonale
Pulmonary hypertension (primary or secondary)
Hypertensive heart disease
Degenerative disease of the conduction system
Brugada syndrome
Arrhythmogenic RV dysplasia
Cardiomyopathy
Chagas disease
Congenital heart disease (eg, Ebstein anomaly)
Prognosis depends on underlying etiology
Worse prognosis for patients with type II second
degree atrioventricular (AV) block or
multifascicular block
Generally good prognosis for patients without
underlying heart disease
NO treatment necessary for isolated asymptomatic
RBBB
Pacing may be necessary for symptomatic patients
or those with other AV or multifascicular block
Ectopic Ventricular impulses
Ventricular tachycardia
Accelerated idioventricular rhythm
True RBBB
Sinus or supraventricular
RBBB and stress testing still reliable
RBBB and MI : RBBB does not concealed the
ECG changes associated in Q wave MI.
RBBB and severe HF : CRT candidate
Auscultatory findings: delayed closure of
pulmonary valves wide splitting in second
heart sound
You might also like
- ECG Interpretation UnismaDocument178 pagesECG Interpretation UnismadefinaNo ratings yet
- Quick Ekg ReferenceDocument23 pagesQuick Ekg Referencekowaikowar100% (2)
- Physician Assistant Certification and Recertification Exam Review - PANRE - PANCEDocument14 pagesPhysician Assistant Certification and Recertification Exam Review - PANRE - PANCEThe Physician Assistant Life100% (3)
- The Effects of Estrogens and ProgesteroneDocument7 pagesThe Effects of Estrogens and ProgesteroneTinke WinkeNo ratings yet
- Ekg Normal Dan Acs Sudin TimurDocument59 pagesEkg Normal Dan Acs Sudin TimurArum MaharaniNo ratings yet
- Principles of ECGDocument11 pagesPrinciples of ECGDeinielle Magdangal RomeroNo ratings yet
- ECGDocument6 pagesECGMatthew MackeyNo ratings yet
- ECG and ArrhythmiasDocument25 pagesECG and ArrhythmiasRashed ShatnawiNo ratings yet
- Dr. Anas Yasin - MDDocument58 pagesDr. Anas Yasin - MDMahfouzNo ratings yet
- ECG TerminologyDocument66 pagesECG TerminologyblndfflNo ratings yet
- Advanced ECG Interpretation: Rebecca Sevigny BSN, RN, CCRNDocument76 pagesAdvanced ECG Interpretation: Rebecca Sevigny BSN, RN, CCRNI Putu SastrawanNo ratings yet
- Recognizing Normal ECGDocument50 pagesRecognizing Normal ECGJosiephine Bucalon100% (3)
- Cardiology/EKG Board Review: Michael J. Bradley D.O. DME/Program Director Family Medicine ResidencyDocument87 pagesCardiology/EKG Board Review: Michael J. Bradley D.O. DME/Program Director Family Medicine ResidencyummimalikihamidNo ratings yet
- Anatomy, Physiology & Conduction System of The HeartDocument122 pagesAnatomy, Physiology & Conduction System of The HeartShelly Lavenia Sambodo100% (1)
- CardiologyDocument149 pagesCardiologyMuhammad SyafiqNo ratings yet
- The ElectrocardiogramDocument2 pagesThe ElectrocardiogramOh DehNo ratings yet
- Krishnan - EKG Basics Lecture NotesDocument3 pagesKrishnan - EKG Basics Lecture NotesanishdNo ratings yet
- ECG TutorialDocument40 pagesECG TutorialAnonymous HAbhRTs2TfNo ratings yet
- Cardiology Ekg BoardDocument87 pagesCardiology Ekg BoardPutri WijayaNo ratings yet
- Kuliah Ekg UnswagatiDocument75 pagesKuliah Ekg UnswagatiiikNo ratings yet
- Advanced Ecg InterpretationDocument88 pagesAdvanced Ecg Interpretationmiguel1123No ratings yet
- Suatu Alat Laboratoris Alat Bantu DiagnosisDocument78 pagesSuatu Alat Laboratoris Alat Bantu DiagnosisMohammad AlmuhaiminNo ratings yet
- ELECTROCARDIOGRAPHYDocument75 pagesELECTROCARDIOGRAPHYMeliaNo ratings yet
- EKG Interpretation Lecture 1 - Identifying The Squiggles, Developing A System For ReadingDocument6 pagesEKG Interpretation Lecture 1 - Identifying The Squiggles, Developing A System For Readingkcargen100% (1)
- Suatu Alat Laboratoris Alat Bantu DiagnosisDocument78 pagesSuatu Alat Laboratoris Alat Bantu DiagnosisAnonymous 3LwVkUsdNo ratings yet
- Ecg 1Document40 pagesEcg 1doctorhanifNo ratings yet
- Systemic Manifestations of Skin DisordersDocument41 pagesSystemic Manifestations of Skin DisordersMeighalah ArumugamNo ratings yet
- EKG Interpretation Basics Guide: Electrocardiogram Heart Rate Determination, Arrhythmia, Cardiac Dysrhythmia, Heart Block Causes, Symptoms, Identification and Medical Treatment Nursing HandbookFrom EverandEKG Interpretation Basics Guide: Electrocardiogram Heart Rate Determination, Arrhythmia, Cardiac Dysrhythmia, Heart Block Causes, Symptoms, Identification and Medical Treatment Nursing HandbookNo ratings yet
- The P WaveDocument13 pagesThe P Wave成失No ratings yet
- Teaching PlanDocument6 pagesTeaching PlanAnthony BasantaNo ratings yet
- ECG InterpretationDocument40 pagesECG InterpretationMuhammad BadrushshalihNo ratings yet
- Arrhythmias: M. Lacombe Mdfmr/Unecom July 22, 2009Document210 pagesArrhythmias: M. Lacombe Mdfmr/Unecom July 22, 2009Kent MaravillosaNo ratings yet
- Normal Ecg, Infarction & Arrhythmia SDocument98 pagesNormal Ecg, Infarction & Arrhythmia SAdinda GupitaNo ratings yet
- Phenytoin Drug StudyDocument3 pagesPhenytoin Drug StudyCheezy Bread100% (1)
- Widecomplex Tachycardia: Mithilesh Kumar Das,, Archana Rajdev,, Vikas KalraDocument13 pagesWidecomplex Tachycardia: Mithilesh Kumar Das,, Archana Rajdev,, Vikas KalraTor JaNo ratings yet
- Bloqueos Intraventriculares ECG UpToDateDocument16 pagesBloqueos Intraventriculares ECG UpToDateMoctezuma VeraNo ratings yet
- LI NarvinDocument14 pagesLI NarvinRosa Nurul FajriNo ratings yet
- Ventricular Arrhythmia - VT: Braghmandaru A.BDocument113 pagesVentricular Arrhythmia - VT: Braghmandaru A.BFaisol SiddiqNo ratings yet
- Normal Ecg, Infarction & Arrhythmias: Iqbal Lahmadi Departement of Internal Medicine Sintang - 2013Document98 pagesNormal Ecg, Infarction & Arrhythmias: Iqbal Lahmadi Departement of Internal Medicine Sintang - 2013Maylisa ManurungNo ratings yet
- C240 Understanding ElectrocardiographyDocument12 pagesC240 Understanding ElectrocardiographyBeauNo ratings yet
- Conduction AbnormalitiesDocument16 pagesConduction Abnormalitiesmerin sunilNo ratings yet
- KULIAH ECG Dinkes PurworejoDocument69 pagesKULIAH ECG Dinkes PurworejoSofian PalupiNo ratings yet
- KULIAH ECG Dinkes PurworejoDocument69 pagesKULIAH ECG Dinkes PurworejoVella NurfatimahNo ratings yet
- Ecg 6Document17 pagesEcg 6api-3757039No ratings yet
- Top Ten (Or 11) EKG KillersDocument84 pagesTop Ten (Or 11) EKG KillersphausknechtNo ratings yet
- Ecg Interpretation:: The BasicsDocument40 pagesEcg Interpretation:: The BasicsRavi SharmaNo ratings yet
- Ipd Kuliah Ekg Blok KegawatdaruratanDocument118 pagesIpd Kuliah Ekg Blok Kegawatdaruratansiti solikhaNo ratings yet
- Suatu Alat LaboratorisDocument78 pagesSuatu Alat LaboratorisHematology 2016No ratings yet
- Electrocardiogram (Ecg)Document31 pagesElectrocardiogram (Ecg)Suraj AgarwalNo ratings yet
- ECG LectureDocument37 pagesECG LectureAmit Pannu100% (1)
- EKG Common Clinical ArrhythmiasDocument54 pagesEKG Common Clinical ArrhythmiasFaisal AlhasNo ratings yet
- Kamis 10 September 2015 - IPD 2 - Kuliah-Ekg-Blok-KegawatdaruratanDocument118 pagesKamis 10 September 2015 - IPD 2 - Kuliah-Ekg-Blok-KegawatdaruratanIrfanArifZulfikarNo ratings yet
- ECGDocument33 pagesECGWasif RaheelNo ratings yet
- 5 Ekg PM Eng PDFDocument70 pages5 Ekg PM Eng PDFfgxNo ratings yet
- Conduction System of Heart: DR - Sruthi Meenaxshi PDF in VMCRHDocument27 pagesConduction System of Heart: DR - Sruthi Meenaxshi PDF in VMCRHsruthimeena6891No ratings yet
- Cheong Kuan Loong Medical Department Hospital Sultan Haji Ahmad Shah, Temerloh 12/5/10Document99 pagesCheong Kuan Loong Medical Department Hospital Sultan Haji Ahmad Shah, Temerloh 12/5/10Haq10No ratings yet
- Ecg Criteria SVT Vs VT: DR - Vinoth Kumar PostgraduateDocument48 pagesEcg Criteria SVT Vs VT: DR - Vinoth Kumar Postgraduatelichumo murryNo ratings yet
- 5 - Ventricular Tachyarrhythmias DoneDocument79 pages5 - Ventricular Tachyarrhythmias Doneclaimstudent3515No ratings yet
- Kursus Ekg DR Ismi-1Document78 pagesKursus Ekg DR Ismi-1Sekar Ayu WulandariNo ratings yet
- Tri Fascicular BlockDocument28 pagesTri Fascicular BlockSubhashini KNo ratings yet
- ECG ExaminationDocument70 pagesECG ExaminationPercy Caceres OlivaresNo ratings yet
- Module - 6.advance 12 Lead InterpretationDocument30 pagesModule - 6.advance 12 Lead InterpretationFerry SofyanriNo ratings yet
- How To Set TPMDocument19 pagesHow To Set TPMFitria ArifinNo ratings yet
- AVRT Treatment and AblationDocument32 pagesAVRT Treatment and AblationFitria ArifinNo ratings yet
- OCT BenyDocument23 pagesOCT BenyFitria ArifinNo ratings yet
- Machine Setup and Connection FFR and OCTDocument33 pagesMachine Setup and Connection FFR and OCTFitria ArifinNo ratings yet
- Ignatius Yansen: RSU Kabupaten TangerangDocument28 pagesIgnatius Yansen: RSU Kabupaten TangerangFitria ArifinNo ratings yet
- Suryani Rahman, SKep, Ners, MM, SPKVDocument66 pagesSuryani Rahman, SKep, Ners, MM, SPKVFitria ArifinNo ratings yet
- PT. Bina Mitra Jaya BersamaDocument25 pagesPT. Bina Mitra Jaya BersamaHADI PRAYITNONo ratings yet
- International Olympic Committee (IOC) Consensus Statement On Relative Energy de Ficiency in Sport (RED-S) : 2018 UpdateDocument16 pagesInternational Olympic Committee (IOC) Consensus Statement On Relative Energy de Ficiency in Sport (RED-S) : 2018 UpdateNicol TrujilloNo ratings yet
- Validación EPDS en Chile - 1995Document6 pagesValidación EPDS en Chile - 1995pennylane_girlNo ratings yet
- Appeal Letter FfsDocument1 pageAppeal Letter FfsAndrea LaBarberaNo ratings yet
- H PyloriDocument8 pagesH PyloriLydia KosasihNo ratings yet
- 1 PDFDocument2 pages1 PDFRAHUL RANANo ratings yet
- WHO - Therapeutic Efficacy Study - Template-Protocol-For-Tet-EnDocument49 pagesWHO - Therapeutic Efficacy Study - Template-Protocol-For-Tet-EnPrakit KitsupeeNo ratings yet
- Patient CounsellingDocument46 pagesPatient CounsellingKeith OmwoyoNo ratings yet
- Conns Current Therapy 2021 Rick D Kellerman Full ChapterDocument67 pagesConns Current Therapy 2021 Rick D Kellerman Full Chapterkelly.caughlin506100% (2)
- Jbra1117 PDFDocument4 pagesJbra1117 PDFAgusNo ratings yet
- Maturity Onset Diabetes of The Young: Clinical Characteristics, Diagnosis and ManagementDocument10 pagesMaturity Onset Diabetes of The Young: Clinical Characteristics, Diagnosis and ManagementatikahanifahNo ratings yet
- Lab Module 06Document7 pagesLab Module 06DHIRAJ DILLEP S NAIRNo ratings yet
- Atypical Extractions-Oral Surgery / Orthodontic Courses by Indian Dental AcademyDocument36 pagesAtypical Extractions-Oral Surgery / Orthodontic Courses by Indian Dental Academyindian dental academyNo ratings yet
- Blood TransfusionDocument2 pagesBlood TransfusionKomal TomarNo ratings yet
- Reproductive Arranged (MedicalBooksVN - Com)Document63 pagesReproductive Arranged (MedicalBooksVN - Com)Rabooh AyashiNo ratings yet
- First Aid Principles and PracticeDocument51 pagesFirst Aid Principles and PracticeGiselle KhrystineNo ratings yet
- Interventions For Clients Requiring Oxygen Therapy or TracheostomyDocument25 pagesInterventions For Clients Requiring Oxygen Therapy or TracheostomyFabricio Serna MarinNo ratings yet
- Acute Flaccid ParalysisDocument4 pagesAcute Flaccid ParalysisZharah RuzNo ratings yet
- Ocular Drug Delivery: Dr. Herman J. WoerdenbagDocument32 pagesOcular Drug Delivery: Dr. Herman J. Woerdenbagitung23No ratings yet
- The Essm Manual of Sexual Medicine - IndexDocument10 pagesThe Essm Manual of Sexual Medicine - IndexAbdulwahab AlhamoodNo ratings yet
- Jama Shadman 2023 RV 230004 1679344287.92157Document15 pagesJama Shadman 2023 RV 230004 1679344287.92157Alejandro PedrazaNo ratings yet
- Rawla 2018 Efficacy and Safety of Megestrol inDocument6 pagesRawla 2018 Efficacy and Safety of Megestrol inAbdallah H. KamelNo ratings yet
- Congenital CataractDocument20 pagesCongenital CataractYouhengNo ratings yet
- Single Dose VialsDocument54 pagesSingle Dose VialsKyon Asma100% (1)
- Constipation NCPDocument2 pagesConstipation NCPjudaperlNo ratings yet
- Overview of Brachytherapy Physics NathDocument6 pagesOverview of Brachytherapy Physics Nathgrounds8No ratings yet