Professional Documents
Culture Documents
The Reproductive System The Reproductive System: © 2018 Pearson Education, Ltd. 1
Uploaded by
lourd nabOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Reproductive System The Reproductive System: © 2018 Pearson Education, Ltd. 1
Uploaded by
lourd nabCopyright:
Available Formats
Chapter 16
The Reproductive System
The Reproductive System
• Gonads—primary sex organs
• Testes in males
• Ovaries in females
• Gonads produce gametes (sex cells) and secrete hormones
• Sperm—male gametes
• Ova (eggs)—female gametes
Anatomy of the Male Reproductive System
• Testes
• Duct system
• Epididymis
• Ductus (vas) deferens
• Urethra
Anatomy of the Male Reproductive System
• Accessory organs
• Seminal glands (vesicles)
• Prostate
• Bulbourethral glands
• External genitalia
• Penis
• Scrotum
Testes
• Each testis is connected to the trunk via the spermatic cord, which houses:
• Blood vessels
• Nerves
• Ductus deferens
• Coverings of the testes
• Tunica albuginea—capsule that surrounds each testis
• Septa—extensions of the capsule that extend into the testis and divide it into
lobules
© 2018 Pearson Education, Ltd. 1
Testes
• Each lobule contains one to four seminiferous tubules
• Tightly coiled structures
• Function as sperm-forming factories
• Empty sperm into the rete testis
• Sperm travels from the rete testis to the epididymis
• Interstitial cells in the seminiferous tubules produce androgens such as testosterone
Duct System
• The duct system transports sperm from the body and includes:
• Epididymis
• Ductus deferens
• Urethra
Duct System
• Epididymis
• Highly convoluted tube 6 m (20 ft) long
• Found along the posterior lateral side of the testis
• First part of the male duct system
• Temporary storage site for immature sperm
• Sperm mature as they journey through the epididymis
• During ejaculation, sperm are propelled to the ductus deferens
Duct System
• Ductus (vas) deferens
• Runs from the epididymis via the spermatic cord through the inguinal canal
and arches over the urinary bladder
• Ampulla—end of the ductus deferens, which empties into the
ejaculatory duct
• Ejaculatory duct—passes through the prostate to merge with the
urethra
• Moves sperm by peristalsis into the urethra
Duct System
• Ductus (vas) deferens (continued)
• Ejaculation—smooth muscle in the walls of the ductus deferens create
peristaltic waves to squeeze sperm forward
• Vasectomy—cutting of the ductus deferens at the level of the testes prevents
transportation of sperm (form of birth control)
2 © 2018 Pearson Education, Ltd.
Duct System
• Urethra
• Extends from the base of the urinary bladder to the tip of the penis
• Carries both urine and sperm
• Sperm enters from the ejaculatory duct
Duct System
• Urethra regions
1. Prostatic urethra—surrounded by prostate gland
2. Membranous urethra—prostatic urethra to penis
3. Spongy (penile) urethra—runs the length of the penis to the external urethral
orifice
• Ejaculation causes the internal urethra sphincter to close
• Prevents urine from passing into the urethra
• Prevents sperm from entering the urinary bladder
Accessory Glands and Semen
• Seminal vesicles
• Prostate
• Bulbourethral glands
Accessory Glands and Semen
• Seminal vesicles
• Located at the base of the bladder
• Produce a thick, yellowish secretion (60% of semen) that contains:
• Fructose (sugar)
• Vitamin C
• Prostaglandins
• Other substances that nourish and activate sperm
• Duct of each seminal vesicle joins that of the ductus deferens on each side to
form the ejaculatory duct
Accessory Glands and Semen
• Prostate
• Encircles the upper (prostatic) part of the urethra
• Secretes a milky fluid
• Helps to activate sperm
• Fluid enters the urethra through several small ducts
© 2018 Pearson Education, Ltd. 3
Accessory Glands and Semen
• Bulbourethral glands
• Pea-sized glands inferior to the prostate
• Produce a thick, clear mucus
• Mucus cleanses the spongy (penile) urethra of acidic urine prior to
ejaculation
• Mucus serves as a lubricant during sexual intercourse
Accessory Glands and Semen
• Semen
• Milky white mixture of sperm and accessory gland secretions
• Components of accessory gland secretions
• Liquid portion acts as a transport medium to dilute sperm
• Sperm are streamlined cellular “tadpoles”
• Fructose provides energy for sperm cells
• Alkalinity of semen helps neutralize the acidic environment of vagina
• Semen inhibits bacteria
External Genitalia
• Scrotum
• Penis
External Genitalia
• Scrotum
• Divided sac of skin outside the abdomen that houses the testes
• Viable sperm cannot be produced at normal body temperature
• Maintains testes at 3°C lower than normal body temperature
External Genitalia
• Penis
• Male organ of copulation that delivers sperm into the female reproductive
tract
• Regions of the penis
• Shaft
• Glans penis (enlarged tip)
• Prepuce (foreskin)
• Folded cuff of skin around proximal end
• Often removed by circumcision
4 © 2018 Pearson Education, Ltd.
External Genitalia
• Penis (continued)
• Internally there are three areas of spongy erectile tissue around the urethra
• Erections occur when this erectile tissue fills with blood during sexual
excitement
Male Reproductive Functions
• Chief roles of the male in the reproductive process
• Produce sperm
• Produce a hormone, testosterone
Spermatogenesis
• Sperm production
• Begins at puberty and continues throughout life
• Millions of sperm are made every day
• Sperm are formed in the seminiferous tubules of the testis
• Spermatogonia (primitive stem cells) begin the process by dividing rapidly
• During puberty, follicle-stimulating hormone (FSH) is secreted in increasing
amounts
Spermatogenesis
• Each division of a spermatogonium stem cell produces:
• Type A daughter cell, a stem cell, that continues the stem cell population
• Type B daughter cell, which becomes a primary spermatocyte, destined to
undergo meiosis and form four sperm
Spermatogenesis
• Meiosis
• Special type of nuclear division that differs from mitosis
• Occurs in the gonads
• Includes two successive divisions of the nucleus (meiosis I and II)
• Results in four daughter cells (gametes)
Spermatogenesis
• Gametes are spermatids with 23 chromosomes
• 23 chromosomes are half the usual 46 found in other body cells
• 23 is known as the haploid number (n)—half the genetic material as other
body cells
• Union of a sperm (23 chromosomes, n) with an egg (23 chromosomes, n) creates a
zygote (2n, or 46 chromosomes)
© 2018 Pearson Education, Ltd. 5
Spermatogenesis
• Spermiogenesis
• Spermatids are nonmotile and not functional as sperm
• A streamlining process is needed to strip excess cytoplasm from a spermatid
and modify it into a sperm
• A sperm has three regions: head, midpiece, tail
• Acrosome sits anterior to the sperm head (nucleus)
• The entire process of spermatogenesis, including spermiogenesis, takes 64
to 72 days
Testosterone Production
• During puberty:
• Follicle-stimulating hormone (FSH) begins prodding seminiferous tubules to
produce sperm
• Luteinizing hormone (LH) begins activating the interstitial cells to produce
testosterone
Testosterone Production
• Testosterone
• Most important hormonal product of the testes
• Stimulates reproductive organ development
• Underlies sex drive
• Causes secondary sex characteristics
• Deepening of voice
• Increased hair growth
• Enlargement of skeletal muscles
• Increased bone growth and density
Anatomy of the Female Reproductive System
• Ovaries
• Duct system
• Uterine (fallopian) tubes
• Uterus
• Vagina
• External genitalia
Ovaries
• Ovaries
• Produce eggs (ova) and hormones (estrogen and progesterone)
• Each ovary houses ovarian follicles consisting of:
• Oocyte (immature egg)
• Follicle cells—layers of different cells that surround the oocyte
6 © 2018 Pearson Education, Ltd.
Ovaries
• Ovarian follicles
• Primary follicle—contains an immature oocyte
• Vesicular (Graafian) follicle—growing follicle with a maturing oocyte
• Ovulation—the follicle ruptures when the egg is mature and ready to be
ejected from the ovary; occurs about every 28 days
• The ruptured follicle is transformed into a corpus luteum
Ovaries
• Ovary support
• Suspensory ligaments secure the ovaries to the lateral walls of the pelvis
• Ovarian ligaments anchor ovaries to the uterus medially
• Broad ligaments, a fold of peritoneum, enclose and hold the ovaries in place
Duct System
• Uterine (fallopian) tubes
• Uterus
• Vagina
Duct System
• Uterine (fallopian) tubes (continued)
• Form the initial part of the duct system
• Receive the ovulated oocyte from the ovaries
• Provide a site for fertilization
• Empty into the uterus
• Little or no contact between ovaries and uterine tubes
• Supported and enclosed by the broad ligament
Duct System
• Uterine (fallopian) tube structure
• Infundibulum
• Distal, funnel-shaped end
• Fimbriae
• Fingerlike projections of the infundibulum
• Receive the oocyte from the ovary
• Cilia located inside the uterine tube transport the oocyte
Duct System
• Uterus
• Situated between the urinary bladder and rectum
• Size and shape of a pear, in a woman who has never been pregnant
• Receives, retains, nourishes a fertilized egg
© 2018 Pearson Education, Ltd. 7
Duct System
• Uterine support
• Broad ligament suspends the uterus in the pelvis
• Round ligament anchors the uterus anteriorly
• Uterosacral ligament anchors the uterus posteriorly
Duct System
• Regions of the uterus
• Body—main portion
• Fundus—superior rounded region above where uterine tube enters
• Cervix—narrow outlet that protrudes into the vagina
Duct System
• Layers of the uterus
• Endometrium
• Inner layer (mucosa)
• Site of implantation of a fertilized egg
• Sloughs off if no pregnancy occurs (menstruation or menses)
• Myometrium is the middle layer of smooth muscle that contracts during labor
• Perimetrium (visceral peritoneum) is the outermost serous layer of the uterus
Duct System
• Vagina
• Passageway that extends from cervix to exterior of body and is located
between urinary bladder and rectum
• Serves as the canal that allows a baby or menstrual flow to leave the body
• Female organ of copulation
• Receives the penis during sexual intercourse
• Hymen—partially closes the vagina until it is ruptured
External Genitalia and Female Perineum
• The female external genitalia, or vulva, includes:
• Mons pubis
• Labia
• Clitoris
• Urethral orifice
• Vaginal orifice
• Greater vestibular glands
8 © 2018 Pearson Education, Ltd.
External Genitalia and Female Perineum
• Mons pubis
• Fatty area overlying the pubic symphysis
• Covered with pubic hair after puberty
External Genitalia and Female Perineum
• Labia—skin folds
• Labia majora
• Hair-covered skin folds
• Enclose the labia minora
• Also encloses the vestibule
• Labia minora—delicate, hair-free folds of skin
External Genitalia and Female Perineum
• Vestibule
• Enclosed by labia majora
• Contains external openings of the urethra and vagina
• Greater vestibular glands
• One is found on each side of the vagina
• Secretions lubricate vagina during intercourse
External Genitalia and Female Perineum
• Clitoris
• Contains erectile tissue
• Corresponds to the male penis
• The clitoris is similar to the penis in that it is:
• Hooded by a prepuce
• Composed of sensitive erectile tissue
• Swollen with blood during sexual excitement
• The clitoris lacks a reproductive duct
External Genitalia and Female Perineum
• Perineum
• Diamond-shaped region between the anterior ends of the labial folds, anus
posteriorly, and ischial tuberosities laterally
Female Reproductive Functions and Cycles
• The total supply of eggs is determined by the time a female is born
• Ability to release eggs begins at puberty with the onset of the menstrual cycle
• Reproductive ability ends at menopause (in female’s fifties)
© 2018 Pearson Education, Ltd. 9
Oogenesis and the Ovarian Cycle
• Oogenesis is the process of producing ova (eggs) in a female
• Oogonia are female stem cells found in a developing fetus
• Oogonia undergo mitosis to produce primary oocytes that are surrounded by
cells that form primary follicles in the ovary
Oogenesis and the Ovarian Cycle
• Primary oocytes are inactive until puberty
• Follicle-stimulating hormone (FSH) causes some primary follicles to mature each
month
• Cyclic monthly changes constitute the ovarian cycle
Oogenesis and the Ovarian Cycle
• Meiosis starts inside maturing follicle
• First meiotic division produces a larger secondary oocyte and a smaller first
polar body
• A vesicular follicle contains a secondary oocyte (maturation from a primary
follicle takes about 14 days)
• Ovulation of a secondary oocyte occurs with the release of luteinizing hormone (LH)
• Secondary oocyte is released and surrounded by a corona radiata
Oogenesis and the Ovarian Cycle
• Meiosis is completed after ovulation only if sperm penetrates the oocyte
• Ovum is produced
• Two additional polar bodies are produced
• Once ovum is formed, the 23 chromosomes can be combined with the 23
chromosomes of the sperm to form the fertilized egg (zygote)
• If the secondary oocyte is not penetrated by a sperm, it dies and does not complete
meiosis to form an ovum
Oogenesis and the Ovarian Cycle
• Meiosis
• Males—produces four functional sperm
• Females—produces one functional ovum and three tiny polar bodies
• Sex cell size and structure
• Sperm are tiny, motile, and equipped with nutrients in seminal fluid
• Egg is large, is nonmotile, and has nutrient reserves to nourish the embryo
until implantation
10 © 2018 Pearson Education, Ltd.
Hormone Production by the Ovaries
• Estrogens are produced by follicle cells
• Cause secondary sex characteristics
• Enlargement of accessory organs of the female reproductive system
• Development of breasts
• Appearance of axillary and pubic hair
• Increase in fat beneath the skin, particularly in hips and breasts
• Widening and lightening of the pelvis
• Onset of menses (menstrual cycle)
Hormone Production by the Ovaries
• Progesterone is produced by the corpus luteum
• Production continues until LH diminishes in the blood
• Does not contribute to the appearance of secondary sex characteristics
• Other major effects
• Helps maintain pregnancy
• Prepares the breasts for milk production
Uterine (Menstrual) Cycle
• Cyclic changes of the endometrium, about 28 days in length
• Regulated by cyclic production of estrogens and progesterone by the ovaries
• FSH and LH, from the anterior pituitary, regulate the production of estrogens and
progesterone by the ovaries
• Ovulation typically occurs about midway through cycle, on day 14
Uterine (Menstrual) Cycle
• Stages of the menstrual cycle
• Menstrual phase
• Proliferative stage
• Secretory stage
Uterine (Menstrual) Cycle
• Days 1–5: menstrual phase
• Functional layer of the endometrium is sloughed
• Bleeding occurs for 3 to 5 days
• Ovarian hormones are at their lowest levels
• By day 5, growing ovarian follicles are producing more estrogen
© 2018 Pearson Education, Ltd. 11
Uterine (Menstrual) Cycle
• Days 6–14: proliferative stage
• Regeneration of functional layer of the endometrium
• Endometrium is repaired, thickens, and becomes well vascularized
• Estrogen levels rise
• Ovulation occurs in the ovary at the end of this stage
Uterine (Menstrual) Cycle
• Days 15–28: secretory phase
• Levels of progesterone rise and increase the blood supply to the
endometrium, which becomes more vascular
• Endometrium increases in size and readies for implantation
Uterine (Menstrual) Cycle
• Days 15–28: secretory phase (continued)
• If fertilization does occur:
• Embryo produces a hormone that causes the corpus luteum to
continue producing its hormones
• If fertilization does NOT occur:
• Corpus luteum degenerates as LH blood levels decline
• The phases are repeated about every 28 days
Mammary Glands
• Present in both sexes, but function only in females
• Modified sweat glands
• Function is to produce milk to nourish a newborn
• Stimulated by sex hormones (mostly estrogens) to increase in size
Mammary Glands
• Parts of the mammary gland
• Areola—central pigmented area
• Nipple—protruding central area of areola
• Lobes—internal structures that radiate around nipple
• Lobules—located within each lobe and contain clusters of alveolar glands
• Alveolar glands—produce milk when a woman is lactating (producing milk)
• Lactiferous ducts—connect alveolar glands to nipple
• Lactiferous sinus—dilated portion where milk accumulates
12 © 2018 Pearson Education, Ltd.
Mammography
• Mammography is X-ray examination that detects breast cancers too small to feel
• American Cancer Society recommends mammography annually for women between
45 and 54 years old and every 2 years thereafter if the results are normal
• Breast cancer is often signaled by a change in skin texture, puckering, or leakage
from the nipple
Pregnancy and Embryonic Development
• Pregnancy—time from fertilization until infant is born
• Conceptus—developing offspring
• Embryo—period of time from fertilization until week 8
• Fetus—week 9 until birth
• Gestation period—from date of last period until birth (approximately 280 days)
Accomplishing Fertilization
• An oocyte is viable up to 24 hours after ovulation
• Sperm are viable up to 48 hours after ejaculation
• For fertilization to occur, sexual intercourse must occur no more than 2 days
before ovulation and no later than 24 hours after
• Sperm cells must make their way to the uterine tube for fertilization to be possible
• Sperm cells are attracted to the oocyte by chemicals
Accomplishing Fertilization
• When sperm reach the oocyte:
• Enzymes break down the follicle cells of the corona radiata around the oocyte
• Sperm undergo an acrosomal reaction
• Membrane receptors on the oocyte pull in the head of the first sperm cell to
make contact
• Oocyte undergoes second meiotic division to produce an ovum and a polar
body
Accomplishing Fertilization
• Fertilization occurs when the genetic material of a sperm combines with that of an
oocyte
Events of Embryonic & Fetal Development
• Zygote
• First cell of a new individual
• The zygote is the result of the fusion of DNA from sperm and egg
• The zygote begins rapid mitotic cell divisions, known as cleavage, 24 hours
© 2018 Pearson Education, Ltd. 13
after fertilization
• The zygote journeys down the uterine tube, moving toward the uterus
Events of Embryonic & Fetal Development
• Cleavage
• Rapid series of mitotic divisions that begins with the zygote
• 3 days after ovulation, the embryo reaches the uterus and floats as a morula,
a ball of 16 cells
Events of Embryonic & Fetal Development
• Blastocyst (chorionic vesicle)
• Hollow, ball-like structure of 100 cells or more
• Secretes human chorionic gonadotropin (hCG) to induce the corpus luteum to
continue producing hormones, preventing menses, until the placenta
assumes its role
Events of Embryonic & Fetal Development
• Functional areas of the blastocyst
1. Trophoblast—large fluid-filled sphere
2. Inner cell mass—cluster of cells to one side
• By day 7 after ovulation, the blastocyst has attached to the endometrium
Events of Embryonic & Fetal Development
• Inner cell mass of blastocyst develops into:
• Primary germ layers
• Ectoderm—outside layer, which gives rise to nervous system and
epidermis of skin
• Endoderm—inside layer, which forms mucosae and associated glands
• Mesoderm—middle layer, which gives rise to everything else
Events of Embryonic & Fetal Development
• After implantation, the trophoblast of the blastocyst develops chorionic villi
(projections)
• Chorionic villi combine with tissues of the uterus to form the placenta
• Once the placenta has formed, the amnion is attached to the placenta by an
umbilical cord
• Amnion is a fluid-filled sac that surrounds the embryo
• Umbilical cord is a blood vessel–containing stalk of tissue
14 © 2018 Pearson Education, Ltd.
Events of Embryonic & Fetal Development
• Placenta
• Forms a barrier between mother and embryo (blood is not exchanged)
• Delivers nutrients and oxygen
• Removes wastes from embryonic blood
• Becomes an endocrine organ and takes over for the corpus luteum (by end of
second month); produces estrogen, progesterone, and other hormones that
maintain pregnancy
Events of Embryonic & Fetal Development
• All organ systems are formed by the end of the eighth week
• Activities of the fetus are growth and organ specialization
• The fetal stage is one of tremendous growth and change in appearance
• Fetal changes are summarized in Table 16.1
Effects of Pregnancy on the Mother
• Pregnancy—period from conception until birth
• Anatomical changes
• Enlargement of the uterus
• Accentuated lumbar curvature (lordosis)
• Relaxation of the pelvic ligaments and pubic symphysis due to production of
the hormone relaxin
Effects of Pregnancy on the Mother
• Physiological changes
• Gastrointestinal system
• Morning sickness is common and is due to elevated progesterone and
estrogens
• Heartburn is common because of organ crowding by the fetus
• Constipation is caused by declining motility of the digestive tract
Effects of Pregnancy on the Mother
• Physiological changes (continued)
• Urinary system
• Kidneys have additional burden and produce more urine
• The uterus compresses the bladder, causing stress incontinence
© 2018 Pearson Education, Ltd. 15
Effects of Pregnancy on the Mother
• Physiological changes (continued)
• Respiratory system
• Nasal mucosa becomes congested and swollen
• Vital capacity and respiratory rate increase
• Dyspnea (difficult breathing) occurs during later stages of pregnancy
Effects of Pregnancy on the Mother
• Physiological changes (continued)
• Cardiovascular system
• Blood volume increases by 25% to 40%
• Blood pressure and pulse increase
• Varicose veins are common
Childbirth (Parturition)
• Initiation of labor
• Labor—the series of events that expel the infant from the uterus
• Rhythmic, expulsive contractions
• Operates by the positive feedback mechanism
• False labor—Braxton Hicks contractions are weak, irregular uterine
contractions
Childbirth (Parturition)
• Initiation of labor (continued)
• Estrogen levels rise
• Uterine contractions begin
• The placenta releases prostaglandins
• Oxytocin is released by the pituitary
• Combined effects of rising levels of hormones—oxytocin and prostaglandins
—initiates contractions and forces the baby deeper into the mother’s pelvis
Stages of Labor
• Dilation
• Cervix becomes dilated
• Full dilation is 10 cm
• Uterine contractions begin and increase
• Cervix softens and effaces (thins)
• The amnion ruptures (“breaking the water”)
• Longest stage, at 6 to 12 hours
16 © 2018 Pearson Education, Ltd.
Stages of Labor
• Expulsion
• Infant passes through the cervix and vagina
• Can last as long as 2 hours, but typically is 50 minutes in the first birth and 20
minutes in subsequent births
• Normal delivery is head-first (vertex position)
• Breech presentation is buttocks-first
Stages of Labor
• Placental stage
• Delivery of the placenta
• Usually accomplished within 15 minutes after birth of infant
• Afterbirth—placenta and attached fetal membranes
• All placental fragments should be removed to avoid postpartum bleeding
Developmental Aspects of the Reproductive System
• Gender is determined at fertilization
• Males have XY sex chromosomes
• Females have XX sex chromosomes
• Reproductive system structures of males and females are identical during early
development
• Gonads do not begin to form until the eighth week
• The presence or absence of testosterone determines whether male or female
accessory reproductive organs will form
Developmental Aspects of the Reproductive System
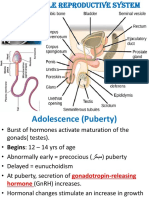
• The reproductive system is inactive during childhood
• Reproductive system organs do not function for childbearing until puberty
• Puberty usually begins between ages 10 and 15
Developmental Aspects of the Reproductive System
• Males
• Enlargement of testes and scrotum signals onset of puberty (often around
age 13)
• Females
• Budding breasts signal puberty (often around age 11)
• Menarche—first menstrual period (usually occurs about 2 years later)
© 2018 Pearson Education, Ltd. 17
Developmental Aspects of the Reproductive System
• Menopause—a whole year has passed without menstruation
• Ovaries stop functioning as endocrine organs
• Childbearing ability ends
• Hot flashes and mood changes may occur
• There is a no equivalent of menopause in males, but there is a steady decline in
testosterone
A Closer Look: Contraception
• Contraception—birth control
• Birth control pill—most-used contraceptive
• Relatively constant supply of ovarian hormones from pill is similar to
pregnancy
• Ovarian follicles do not mature, ovulation ceases, menstrual flow is reduced
A Closer Look: Contraception
• Morning-after pill (MAP)
• Taken within 3 days of unprotected intercourse
• Disrupts normal hormonal signals to the point that fertilization is prevented
• Other hormonal birth control devices cause cervical mucus to thicken
• Minipill (tablet)
• Norplant (rods placed under the skin)
A Closer Look: Contraception
• Intrauterine device (IUD)
• Plastic or metal device inserted into uterus
• Prevents implantation of fertilized egg
• Sterilization
• Tubal ligation (females)—cut or cauterize uterine tubes
• Vasectomy (males)—cut or cauterize the ductus deferens
A Closer Look: Contraception
• Coitus interruptus—withdrawal of penis prior to ejaculation
• Rhythm (fertility awareness)—avoid intercourse during period of ovulation or fertility
• Record daily basal temperature (body temperature rises after ovulation)
• Record changes in pattern of cervical mucus
18 © 2018 Pearson Education, Ltd.
A Closer Look: Contraception
• Barrier methods
• Diaphragms
• Cervical caps
• Condoms
• Spermicidal foams
• Gels
• Sponges
A Closer Look: Contraception
• Abortion—termination of pregnancy
• Miscarriage—spontaneous abortion is common and frequently occurs before a
woman knows she is pregnant
• RU486, or “abortion pill”—induces miscarriage during first 7 weeks of pregnancy
© 2018 Pearson Education, Ltd. 19
You might also like
- Bio Concept MapDocument33 pagesBio Concept MappullaiNo ratings yet
- The Cardiovascular System: Lecture Presentation by Patty Bostwick-Taylor Florence-Darlington Technical CollegeDocument124 pagesThe Cardiovascular System: Lecture Presentation by Patty Bostwick-Taylor Florence-Darlington Technical Collegelourd nabNo ratings yet
- Biology Investigatory Project On GametogenesisDocument20 pagesBiology Investigatory Project On GametogenesisAshwin Rockzz46% (13)
- The Reproductive System The Reproductive System: © 2018 Pearson Education, Inc. 1Document19 pagesThe Reproductive System The Reproductive System: © 2018 Pearson Education, Inc. 1valjulene monteNo ratings yet
- 2020 - Reproductive System - Lecture NotesDocument18 pages2020 - Reproductive System - Lecture Notesinsight scienceNo ratings yet
- MF009 6B Human Reproduction System James LDocument26 pagesMF009 6B Human Reproduction System James LPikuNo ratings yet
- Anatomy of The Male and Female Reproductive SystemDocument13 pagesAnatomy of The Male and Female Reproductive SystemThrecia RotaNo ratings yet
- BIO 282 Male Reproductive System - FINALDocument46 pagesBIO 282 Male Reproductive System - FINALLira PagaraNo ratings yet
- Science 10 - Reproductive SystemDocument32 pagesScience 10 - Reproductive SystemHanabi Scarlet ShadowNo ratings yet
- Biology 2 Lecture 10 - Reproductive SystemDocument42 pagesBiology 2 Lecture 10 - Reproductive SystemRYLE IBANEZNo ratings yet
- Repro SsystemDocument6 pagesRepro SsystemGuenNo ratings yet
- Human Male Reproductive SystemDocument45 pagesHuman Male Reproductive Systemcyber secNo ratings yet
- Reproductive System Male and FemaleDocument61 pagesReproductive System Male and FemaleAsad KHAN100% (1)
- A P Powerpoint10Document61 pagesA P Powerpoint10AbdiwaliNo ratings yet
- 11 Reproductive SystemDocument51 pages11 Reproductive Systemamare mitkuNo ratings yet
- Male Reproductive SystemDocument30 pagesMale Reproductive SystemChinju Jose SajithNo ratings yet
- Safe Environment ContractDocument37 pagesSafe Environment Contractdipanjang panjanginNo ratings yet
- 5a. Male & Female Reproductive AnatomyDocument119 pages5a. Male & Female Reproductive AnatomyvictorNo ratings yet
- Male SubfertilityDocument41 pagesMale SubfertilityIshaThapaNo ratings yet
- Sistem Reproduksi PriaDocument87 pagesSistem Reproduksi PriaAnonymous uLcvBr5ywNo ratings yet
- Ch. 28 Reproductive Part IDocument20 pagesCh. 28 Reproductive Part Imfoley11No ratings yet
- Human Reproductive SystemDocument43 pagesHuman Reproductive Systembabaaijaz01No ratings yet
- Anatomy 2nd-U-6 Reproductive SystemDocument134 pagesAnatomy 2nd-U-6 Reproductive Systemsinte beyuNo ratings yet
- Chapter 3 - Human Reproduction - STUDY RATEDocument14 pagesChapter 3 - Human Reproduction - STUDY RATEsriharshitha darapuNo ratings yet
- Rhsi, LSDocument56 pagesRhsi, LSMary AkellaNo ratings yet
- Human Reproduction: 3.1: Male Reproductive SystemDocument27 pagesHuman Reproduction: 3.1: Male Reproductive SystemAvik BhaumikNo ratings yet
- Anatomy and Physiology of The Male Reproductive SystemDocument81 pagesAnatomy and Physiology of The Male Reproductive SystemMj BrionesNo ratings yet
- 24 Lecture PPT - Reproductive SystemDocument47 pages24 Lecture PPT - Reproductive Systemjohnjay3110100% (2)
- Sexual Reproductive SystemDocument46 pagesSexual Reproductive Systemred JimNo ratings yet
- Basic Steps in Human ReproductionDocument14 pagesBasic Steps in Human ReproductionMauz KhanNo ratings yet
- 1 Anatomy and Physiology of ReproductionDocument31 pages1 Anatomy and Physiology of Reproductionjose mari chanNo ratings yet
- Male Reproductive SystemDocument34 pagesMale Reproductive Systemelia watiNo ratings yet
- Anatomy of The Male Reproductive SystemDocument70 pagesAnatomy of The Male Reproductive SystemDaniel HikaNo ratings yet
- Part 8 - Human Male Reproductive SystemDocument19 pagesPart 8 - Human Male Reproductive SystemAmal Naeem JHNo ratings yet
- Reproductive System - Bio 2Document56 pagesReproductive System - Bio 220181539No ratings yet
- The Reproductive SystemDocument36 pagesThe Reproductive SystemKem Marian MauricioNo ratings yet
- Chap 19 - The Reproductive SystemDocument46 pagesChap 19 - The Reproductive SystemHATLERNo ratings yet
- Histologi Reproduksi PriaDocument45 pagesHistologi Reproduksi Priablack junoNo ratings yet
- Male Reproduction I (Spring2020)Document48 pagesMale Reproduction I (Spring2020)Sahil ParikhNo ratings yet
- Basic Human AnatomyDocument43 pagesBasic Human AnatomyZirah Lee ValledorNo ratings yet
- Histology Exam IV Review Part 2Document26 pagesHistology Exam IV Review Part 2ashdmb217No ratings yet
- Lesson 4 Anatomy and Physiology of ReproductionDocument16 pagesLesson 4 Anatomy and Physiology of ReproductionAngel AsisNo ratings yet
- 02 Overview of The Male and Female Reproductive SystemsDocument30 pages02 Overview of The Male and Female Reproductive SystemsOsman Saidu SesayNo ratings yet
- Male Reproductive SystemDocument31 pagesMale Reproductive SystemGeorge Allen VisperasNo ratings yet
- Oleza Cannery S. Reproductive SystemDocument16 pagesOleza Cannery S. Reproductive SystemCannery OlezaNo ratings yet
- Human Reproduction (Edustudy Point)Document10 pagesHuman Reproduction (Edustudy Point)Vishal UpadhyayNo ratings yet
- ReproDocument80 pagesReprocream o100% (1)
- Human ReproductionDocument11 pagesHuman ReproductionAdesh BhullarNo ratings yet
- Reproductive SystemDocument219 pagesReproductive Systemtzushka_vipNo ratings yet
- Reproductive System NotesDocument40 pagesReproductive System Notesakhtardilshad009No ratings yet
- Reproductive SystemDocument26 pagesReproductive SystemViscount MalamiNo ratings yet
- Male Reproductive SystemDocument30 pagesMale Reproductive SystemRaisashimi M.S.100% (1)
- Reproductive System: Endocrinology of ReproductionDocument40 pagesReproductive System: Endocrinology of ReproductiongerginNo ratings yet
- Human Sexuality Unit: Reproductive SystemsDocument38 pagesHuman Sexuality Unit: Reproductive SystemsMary Grace CacalNo ratings yet
- Male Female Anatomy ReproductivDocument44 pagesMale Female Anatomy ReproductivWiedNo ratings yet
- CH3 Human ReproductionDocument34 pagesCH3 Human ReproductionArmanNo ratings yet
- Repro LecDocument18 pagesRepro LecApril NojaraNo ratings yet
- Human ReproductionDocument94 pagesHuman ReproductionDivya AgarawalNo ratings yet
- Repro A 2017Document94 pagesRepro A 2017Ruvarashe MutadzaNo ratings yet
- Reproductive System Lecture WebsiteDocument35 pagesReproductive System Lecture Websiteapi-295110496No ratings yet
- Male Reproductive SystemDocument47 pagesMale Reproductive SystemLiezel CauilanNo ratings yet
- Guided Lecture Notes, Chapter 2, Community-Based Nursing PracticeDocument3 pagesGuided Lecture Notes, Chapter 2, Community-Based Nursing Practicelourd nabNo ratings yet
- Guided Lecture Notes, Chapter 1, Health Care Delivery and Evidence-Based Nursing PracticeDocument3 pagesGuided Lecture Notes, Chapter 1, Health Care Delivery and Evidence-Based Nursing Practicelourd nabNo ratings yet
- BSN 3 ProceduresDocument128 pagesBSN 3 Procedureslourd nabNo ratings yet
- The Urinary System Functions of The Urinary System: © 2018 Pearson Education, Ltd. 1Document13 pagesThe Urinary System Functions of The Urinary System: © 2018 Pearson Education, Ltd. 1lourd nabNo ratings yet
- The Respiratory System Organs of The Respiratory System: © 2018 Pearson Education, Ltd. 1Document13 pagesThe Respiratory System Organs of The Respiratory System: © 2018 Pearson Education, Ltd. 1lourd nabNo ratings yet
- The Cardiovascular System The Cardiovascular System: EpicardiumDocument17 pagesThe Cardiovascular System The Cardiovascular System: Epicardiumlourd nabNo ratings yet
- CH - 03 The CellDocument29 pagesCH - 03 The Celllourd nabNo ratings yet
- The Skeletal System The Skeletal System: © 2018 Pearson Education, Ltd. 1Document16 pagesThe Skeletal System The Skeletal System: © 2018 Pearson Education, Ltd. 1lourd nabNo ratings yet
- The Muscular System The Muscular System: © 2018 Pearson Education, Ltd. 1Document14 pagesThe Muscular System The Muscular System: © 2018 Pearson Education, Ltd. 1lourd nabNo ratings yet
- Anatomy and Physiology: The CellDocument8 pagesAnatomy and Physiology: The Celllourd nabNo ratings yet
- The Endocrine System The Endocrine System: © 2018 Pearson Education, Ltd. 1Document12 pagesThe Endocrine System The Endocrine System: © 2018 Pearson Education, Ltd. 1lourd nabNo ratings yet
- Test II Anatomy LabelingDocument7 pagesTest II Anatomy Labelinglourd nabNo ratings yet
- Cell JunctionsDocument11 pagesCell Junctionslourd nabNo ratings yet
- ABG Quiz by GroupDocument13 pagesABG Quiz by Grouplourd nabNo ratings yet
- Anatomical PrinciplesDocument4 pagesAnatomical Principleslourd nabNo ratings yet
- Head, Face and NeckDocument50 pagesHead, Face and Necklourd nabNo ratings yet
- Muscles in Alphabetical OrderDocument2 pagesMuscles in Alphabetical Orderlourd nabNo ratings yet
- Health Education NotesDocument5 pagesHealth Education Noteslourd nab50% (2)
- Human ReproductionDocument107 pagesHuman ReproductionYashNo ratings yet
- The International Glossary On Infertility and Fertility Care, 2017Document14 pagesThe International Glossary On Infertility and Fertility Care, 2017Zurya UdayanaNo ratings yet
- The Effects of Diabetes On Male Fertility and Epigenetic Regulation During SpermatogenesisDocument6 pagesThe Effects of Diabetes On Male Fertility and Epigenetic Regulation During SpermatogenesisSephendra LutfiNo ratings yet
- Comprehensive GynaecologyDocument716 pagesComprehensive GynaecologyCharity AtsuNo ratings yet
- All Est Real Biology Exams by Dr. Mai Abd El SalamDocument153 pagesAll Est Real Biology Exams by Dr. Mai Abd El SalamNancy MohamedNo ratings yet
- 61 Sharma and Agarwal Spermiogenesis - An OverviewDocument26 pages61 Sharma and Agarwal Spermiogenesis - An Overviewjohairah merphaNo ratings yet
- Spermatogenesis 4BIO9Document31 pagesSpermatogenesis 4BIO9CourtneyNo ratings yet
- Human ReproductionDocument41 pagesHuman ReproductionMmabatho VilakaziNo ratings yet
- CAPE Biology 2013 U1 P2Document18 pagesCAPE Biology 2013 U1 P2Reggie ThorpeNo ratings yet
- Isbn 93-8551658-2Document252 pagesIsbn 93-8551658-2Zehra Aybüke CEYLANNo ratings yet
- A Practical Approach To Testicular BiopsyDocument8 pagesA Practical Approach To Testicular BiopsyNazaqat FarooqNo ratings yet
- Andrology - 2017 - Semet - The Impact of Drugs On Male Fertility A ReviewDocument24 pagesAndrology - 2017 - Semet - The Impact of Drugs On Male Fertility A ReviewAbhishek RampalNo ratings yet
- AUBF - Amniotic Fluid and Semen Study MaterialDocument10 pagesAUBF - Amniotic Fluid and Semen Study MaterialVienna Jamaica Be Cari-CariNo ratings yet
- Fisiologi Genital SherwoodDocument80 pagesFisiologi Genital SherwoodBeatrix RoriNo ratings yet
- Ahds 242 Objective Questions 2Document9 pagesAhds 242 Objective Questions 2std21376No ratings yet
- Animal ReproductionDocument10 pagesAnimal ReproductionAnugat JenaNo ratings yet
- Functions of The Reproductive SystemDocument3 pagesFunctions of The Reproductive SystemVernice OrtegaNo ratings yet
- Ameliorating Effect of Olive Oil On Fertility of Male Rats Fed On Genetically Modified Soya BeanDocument6 pagesAmeliorating Effect of Olive Oil On Fertility of Male Rats Fed On Genetically Modified Soya Bean--No ratings yet
- Sexual Reproductive HealthDocument29 pagesSexual Reproductive HealthAlen VukosavljevicNo ratings yet
- Anatomy & Physiology: Male Reproductive SystemDocument7 pagesAnatomy & Physiology: Male Reproductive Systemkristel ludangcoNo ratings yet
- Anatomy and Physiology of The Reproductive System in BullsDocument18 pagesAnatomy and Physiology of The Reproductive System in BullsnayayathNo ratings yet
- Zoology MCQsDocument26 pagesZoology MCQsUmair KhalidNo ratings yet
- Anatomy & Physiology of Farm AnimalsDocument116 pagesAnatomy & Physiology of Farm AnimalsJayson BasiagNo ratings yet
- 2nd Year Mcqs - Mcqs Physiology MedicalDocument4 pages2nd Year Mcqs - Mcqs Physiology MedicalKhadijaSarwarNo ratings yet
- Diagestive, Urinary and Reproductive SystemDocument39 pagesDiagestive, Urinary and Reproductive SystemCarolina Calle HerreraNo ratings yet
- SCIENCE 8 Q4 Weeks1to4 Binded Ver10-1Document41 pagesSCIENCE 8 Q4 Weeks1to4 Binded Ver10-1EFREN REYESNo ratings yet
- GynecologyDocument124 pagesGynecologyrajkumar871992No ratings yet
- 10 1111@and 13509Document22 pages10 1111@and 13509Theylor RibeiroNo ratings yet