Professional Documents
Culture Documents
MIB - Internal Medicine 2 Semester 8 Updated March 2021
MIB - Internal Medicine 2 Semester 8 Updated March 2021
Uploaded by
Kavin VarmaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
MIB - Internal Medicine 2 Semester 8 Updated March 2021
MIB - Internal Medicine 2 Semester 8 Updated March 2021
Uploaded by
Kavin VarmaCopyright:
Available Formats
TUSOM PHASE – II PROGRAMME INT.
MED 2
Bachelor of Medicine
&
Bachelor of Surgery
(MBBS) Programme
MODULE INFORMATION BOOKLET
Semester 8, Year 4
INTERNAL MEDICINE 2
August 2019 Page 1
TUSOM PHASE – II PROGRAMME INT.MED 2
Contents:
1. Names of academic staff…………………………………………………………………3
2. Synopsis………………………………………………………………………………………….4
3. Rationale of inclusion of the module………….…………………………………..5
4. Module and Year offered………………………………………………………………..5
5. Student learning time in hours………………………………………………………..5
6. Credit value…………………………………………………………………………………….5
7. Pre-requisite……………………………………………………………………………………5
8. Duration………………………………………………………………………………………….5
9. Programme learning outcomes (PLO)…….……………………………………….6
10.Course learning outcomes (CLO)….………………………………………………….7
11.Mapping of PLOs with the CLOs……………………………………………………….7
12.Posting Objectives.………………………………………………………………………….8
13.Posting Outcomes…………..……………..……………………………………………….8
14.Taylor’s Graduate Capabilities…………………………………………………………9
15.Knowledge and skills matched with TGC…………………………………………10
16.Generic weekly time table………………………………………………………………11
17.Teaching-Learning strategy………………………….…………………………………11
18.Delivery methods and abbreviations used………………………………………12
19.Assessment strategy……………………………………………………………………….15
20.Tools of assessment………………………………………………………………………. 16
21.Core topics and mode of delivery……………………………………………………17
22.Assessment methods and types……………………………………………………..22
23.Reading list…………………………………………………………………………………….22
August 2019 Page 2
TUSOM PHASE – II PROGRAMME INT.MED 2
Names of Academic Staffs:
TAYLOR’S UNIVERSITY:
Full Time:
Dr. Benjamin Samraj Prakash Earnest, Senior Lecturer and Physician
Assoc Prof Dr. Abdul Kareem Meera Mohaideen [Radiology]
Dr. Lim Su Yin, Senior Lecturer and Neurologist [Clinical Skills Session]
Part Time:
Prof Dato’ Dr. Mohd Tahir Md Azhar, Emiritus Professor of Medicine and Physician
Prof Datuk Dr. Christopher Lee K C, Professor of Medicine and Physician
HOSPITAL SUNGAI BULOH (HSB):
Dr. Suresh Kumar C, HOD, Medicine, Hospital Sungai Buloh
Dr. E Chia Qi, Consultant Physician
Dr. Pearly, Consultant Physician
Dr. Thomas Koshy, Consultant Physician
Dr. Norli Marwayne, Dermatologist
Adminstrative Matters:
Director of the Clinical Campus
Professor Dr Lai Nai Ming
(NaiMing.Lai@taylors.edu.my)
Tel: 03-56296634
Phase II Program Director
Assoc. Professor Dr Win Min Thien
(MinThein.Win@taylors.edu.my)
Tel: 03-56296632
Phase II Assessment Coordinator
Assoc. Professor Dr Loh Keng Yin
(KengYin.Loh@taylors.edu.my)
Tel: 03-56296633
Stream (Year 4) Coordinator
Dr. Lim Su Yin,
SuYin.Lim@taylors.edu.my
Tel: 03-56296633
Posting Coordinator
Dr. Benjamin Samraj Prakash Earnest
BenjaminSamrajPrakash.Earnest@taylors.edu.my
Tel: 03-56296639
August 2019 Page 3
TUSOM PHASE – II PROGRAMME INT.MED 2
Senior Nursing Officer
Matron Chithradevi Kannan
Chithradevi.Kannan@taylors.edu.my
Tel: 03-56296633
Nursing Officer, Clinical Skills
Norisah Ab Latif
Norisah.AbLatif@taylors.edu.my
Tel:03-56296635
Administrative Executives:
Ms Noorhayati Kardi
Noorhayati.Kardi@taylors.edu.my
Tel:03-56296633
Ms Noorain Ibrahim
Noorain.Ibrahim@taylors.edu.my
Tel: 03-56296633
Synopsis:
The Internal Medicine 2 includes a 6-week posting in Semester 8. This posting is designed as an
extension of the Year-3 Semester-5 Internal Medicine to provide continuous learning by re-
enforcement of learning outcomes achieved in Year-3. The posting will emphasise more on
detailed steps of management and preventive measures of common medical illnesses. The
Semester-8 Medicine posting allows students to pursue a clinical senior clerkship program with
the basic experience of obtaining systematic history from and performing physical examination
on patients with common clinical problems and understanding the relevant principles of
management. Concurrently this clinical rotation will continue to inculcate humanistic values
related to the practice of medicine. These postings are designed to provide students with a
variety of experiences and opportunities essential in Internal Medicine.
Students will participate in ward work such as following ward rounds, observing clinical
procedures, attending bedside clinical teaching and participating in clinical case discussions
under the direction of a clinical supervisor. The students will also attend lectures, seminars,
case-based learning sessions and clinical skills sessions. The clinical supervisor/s will provide
mid and end of posting feedback on the students’ course work, behaviour and professionalism.
The students will also undertake the discipline specific end-of-posting and integrated end-of-
semester exams.
August 2019 Page 4
TUSOM PHASE – II PROGRAMME INT.MED 2
Rationale of the inclusion of the course/module in the programme:
Internal Medicine, being a major subject and speciality, is reinforced in the posting of Internal
Medicine 2 in Year 4.
The objectives of the posting are such that the students are to strengthen and consolidate the
knowledge, skills and behavioural attributes essential to the practice of medicine that were
acquired in Internal Medicine 1 in year 3.
Module and year offered:
Semester 8, Year 4
Mode of Delivery and Contact hours
Topics/Domains Mode of Contact Independent Total Learning
delivery hours learning time (IL) in Time (TLT) in
hours hours
1. Management of heart
1 2 3
failure
2. Management of atrial
1 2 3
fibrillation
3. Clinical interpretation of Lecture
1 2 3
liver function tests (5)
4. Clinical interpretation of
1 2 3
renal function tests
5. Clinical interpretation of
1 2 3
pulmonary function tests
15
1. HIV & AIDS 1 1 2
2. Epilepsy 1 1 2
3. Brief clinical approach to Clinical
1 1 2
quadriplegia and paraplegia discussion
4. Renal replacement (CD)
1 1 2
therapy (5)
5. Renal involvement in
1 1 2
systemic disorders
10
1. Syncope 2 4 6
2. Hypertension Case Based 2 4 6
3. Diabetes Learning (CBL) 2 4 6
August 2019 Page 5
TUSOM PHASE – II PROGRAMME INT.MED 2
4. Anaemia (5) 2 4 6
5. Infections 2 4 6
30
1. Recognizing abnormal
heart sounds (OS, clicks and 2 4 6
rubs) and murmurs
2. Recognizing abnormal
2 4 6
breath sounds
3. ECG interpretation –
2 4 6
review
4. Radiological
interpretation of common 2 4 6
Clinical skills
CVS & RS conditions
(7)
5. Radiological
interpretation of common 2 4 6
neurological conditions
6. Advanced procedures
-Lumbar puncture, pleural 2 4 6
tapping and paracentesis
7. Medical simulation using
SIMMAN-Approach to Chest 2 4 6
pain
42
1. Movement disorders 2 4 6
2. Dementia Seminar 2 4 6
(3)
3. Common skin disorders 2 4 6
18
Bed side Clinic teaching:
Bedside/Clinic
Presentation & discussion
teaching 40 20 60
(2 hours/session
(20)
Total: 20 sessions)
60
1. Approach to a patient Problem 6 6 12
with heart murmur Solving
2. Investigations in heart Exercises
disease [DSL]
3. Approach to a patient (2)
with GI bleeding
4. Management of
rheumatoid arthritis and SLE
5. Gastrointestinal infections
& irritable bowel syndrome
6. Pericarditis and Pericardial
August 2019 Page 6
TUSOM PHASE – II PROGRAMME INT.MED 2
effusion
7. Pulmonary hypertension
and cor pulmonale
8. Common Geriatric
problems
9. Approach to common
oncological conditions
10. Neuromuscular junction
disorders
11. Approach to abdominal
distension and pain
11
Ward work (2 hours/session) 25 sessions 50 - 50
50
Case write-up 2 - 6 6
6
On-call 5 0 15 15
Assessment 4 12 16
Self-study 10 0 10 10
Total: 140 144 284
Credit value: 7
August 2019 Page 7
TUSOM PHASE – II PROGRAMME INT.MED 2
Student Learning Time (SLT) in hours
Teaching-Learning Mode Contact Hours Independent LT Total Student Learning Time (SLT)
Ward work 2 x 25 = 50 - 50
Bedside teaching 2 x 20 = 40 20 60
Lecture 1X5=5 10 15
Clinical discussion 1x5=5 5 10
Clinical skills session 2 x 7 = 14 28 42
Case based learning 2 x 5 = 10 20 30
Seminar 2x3=6 12 18
Case write-ups 0 2x3=6 6
Self-study (SDL) 0 10 10
Problem Solving Exercises (DSL) 6 6 12
On-call 0 3 x 5 = 15 15
Continuous assessment EOP 4 12 16
(Theory + Clinical)
TOTAL 140 144 284
Credit Value: 7 credit hours
Prerequisite:
To have successfully completed Year 3 and also End of Year 3 exams of the MBBS Programme
Duration: 6 weeks in Semester 8
TAYLOR’S MBBS PROGRAMME LEARNING OUTCOMES (PLOs)
PLO 1 Knowledge
August 2019 Page 8
TUSOM PHASE – II PROGRAMME INT.MED 2
Have sound knowledge on the foundations of medicine, including established and
evolving biomedical, clinical, epidemiological, social and behavioural sciences, as well
as humanities.
PLO 2 Practical Skills
Be competent at clinical management of acute and chronic health problems, promotion
of health and prevention of disease.
PLO 3 Social skills, Teamwork and Responsibility
Be caring and compassionate; incorporating individual, local as well as global
perspectives in making healthcare decisions.
PLO 4 Values, Ethics, Moral and Professionalism
Be committed to the overall well-being of patients and society through ethical practice,
professionalism, accountability and compliance to regulations.
PLO 5 Lifelong Learning Skills
Be aware of the need for life-long learning and continuous self-improvement.
PLO 6 Leadership Skills
Be able to promote mutual respect and foster collaborative relationship within the
healthcare team in the role of leader or member.
PLO 7 Managerial and Entrepreneurial skills
Utilise time and available resources efficiently to deliver high quality and cost-effective
care.
PLO 8 Communication Skills
Be proficient at effective communications to facilitate the gathering and sharing of
information with patients, their families, healthcare team members and the community
for the delivery of effective healthcare.
PLO 9 Information Management
Utilise technological advances effectively to retrieve information, maintain patient
records and conduct research.
PLO 10 Thinking, Scientific and Research skills
Demonstrate critical, constructive, research-oriented thinking in the delivery of
effective healthcare.
Note: The main titles above the PLOs are derived to match the Malaysian Ministry of Education
Learning Outcome Domains.
INTERNAL MEDICINE 2 COURSE LEARNING OUTCOMES (CLOs)
CLO 1 Obtain complete and comprehensive history using efficient communication skills and
August 2019 Page 9
TUSOM PHASE – II PROGRAMME INT.MED 2
structured and systematic questions in all the systems
CLO 2 Develop the knowledge and skills to perform systematic examination and eliciting
physical signs by observing bedside etiquettes to make a provisional diagnosis and
problem list.
CLO 3 Correlate the important points in the history with the examination findings to make a
provisional diagnosis or formulate a list of differential diagnoses.
CLO 4 Discuss the relevant investigations that is deemed necessary for the common medical
conditions and interpret the laboratory and imaging reports and clinically correlate to
achieve the final confirmatory diagnoses
CLO 5 Discuss the essential steps of management of the patients with common medical
conditions admitted in the ward including both non-pharmacological and
pharmacological forms of treatment
CLO 6 Observe/assist (under supervision) common clinical procedures like pleural tapping,
Paracentesis, lumbar puncture, bone marrow aspiration/biopsy, liver biopsy.
MAPPING CLOs - INTERNAL MEDICINE 2 TO PLOs
PLO 1 PLO 2 PLO 3 PLO 4 PLO 5 PLO 6 PLO 7 PLO 8 PLO 9 PLO
10
CLO
√ √ √ √ √
1
CLO
√ √ √ √ √ √
2
CLO
√ √ √ √
3
CLO
√ √ √ √ √
4
CLO
√ √ √
5
CLO
√ √ √ √
6
August 2019 Page 10
TUSOM PHASE – II PROGRAMME INT.MED 2
Posting Objectives:
1. To provide adequate clinical training experiences in Internal Medicine covering a wide
range of diseases, patient characteristics and encounter settings; thus enhancing patient
interviewing and clinical reasoning skills
2. To provide hands-on experience on clinical procedures relevant to Internal Medicine.
3. To promote practice of evidence-based medicine i.e. finding and using the best evidence
available
4. To promote professional behaviour and cultivate ethical values when interacting with
patients, colleagues and staff
Posting Outcomes:
1. Elicit a detailed and thorough history; perform a thorough and complete physical
examination including mental status examination and examination of an unconscious
patient.
2. Correlate the clinical symptoms and physical signs to make a provisional diagnosis along
with the functional disability score and suggest relevant investigations.
3. Interpret reasonably all the relevant investigations for the patient’s clinical condition.
4. Professionally present and discuss the steps in detail involved in the management of the
patient.
5. Discuss the first-line management and outline the short term and long term
management.
6. Demonstrate the skills in performing minor procedures under supervision.
August 2019 Page 11
TUSOM PHASE – II PROGRAMME INT.MED 2
August 2019 Page 12
TUSOM PHASE – II PROGRAMME INT.MED 2
Knowledge and skills (matched with Taylor’s Graduate Capabilities)
TGCs Learning outcomes for Internal Medicine 2
Elicit a detailed and thorough history; perform a thorough and
complete physical examination including mental status
examination and examination of an unconscious patient.
Correlate the clinical symptoms and physical signs to make a
provisional diagnosis along with a functional disability score and
suggest relevant investigations.
Interpret reasonably all the relevant investigations for the
patient’s clinical condition.
Professionally present and discuss the steps involved in the
management of the patient.
Discuss the first line management and outline short-term and long
term management.
Demonstrate the skills in performing minor procedures under
supervision.
August 2019 Page 13
TUSOM PHASE – II PROGRAMME INT.MED 2
Generic weekly time table:
Time / Day Monday Tuesday Wednesday Thursday Friday
Ward work / Ward work / Ward work / Ward work / Ward work
Bedside Bedside Bedside Clinical Bedside Clinical
8.00 – 12.00
Clinical Clinical Teaching (BST) Teaching (BST) Problem
Teaching Teaching Solving
(BST) (BST) Exercises
(PSEs)
CASE CASE CASE CASE CASE
DISCUSSION DISCUSSION DISCUSSION DISCUSSION DISCUSSION
12.00 – 1.00
(CD) (CD) (CD) (CD) (CD)
1.00 – 2.00 LUNCH BREAK
Self-study Self-study
2.00 – 3.00 (DSL or SDL) (DSL or SDL) INTEGRATED
CLINICAL SKILLS DISCIPLINE BLOCK /
SESSION SPECIFIC / INTEGRATED
CSS: COMMON SEMINAR /
Case-based Seminar: (S) LECTURE DISCIPLINE
3.00 – 5.00 Learning SPECIFIC
(CBL): CONCEPT
LECTURES
Teaching-learning strategy:
The bulk of learning in the Internal Medicine 2 is student centered. The students, having had a
more basic module in Internal Medicine in Year 3, are expected to further advance their
knowledge and skills, to a large extent, on their own. Students will spend a minimum of 4 hours
a day in the wards, joining ward rounds, independently clerking and following the progress of
assigned patients and observing, assisting or performing procedures. They will be supervised by
the lecturers during these periods. Most classroom based learning will be interactive; some
conducted by lecturers and others by students under the guidance of the lecturers. Specific
skills are learnt in Clinical Skills Sessions.
August 2019 Page 14
TUSOM PHASE – II PROGRAMME INT.MED 2
Delivery methods & abbreviations used:
1. Ward rounds - Wd rd
2. Ward work - Wd wk
3. Bedside teaching – BST
4. On-call duties- OD
5. Clinical discussion - CD
6. Lectures (Discipline specific Lectures, Common Lectures, Integrated lectures) – L
7. Case based learning – CBL
8. Seminars (Discipline specific Seminars + Integrated seminars) - S
9. Clinical skills session – CSS
10. Self-study (Directed self-learning – DSL & Self-directed learning - SDL)
1. Ward rounds: Students are to take part in ward rounds with consultants.Each student
group will be assigned a permanent consultant for the whole tenure of the posting.
Students will follow the consultant rounds and medical officer rounds every day from 8am
to 9am. Each student has to maintain a log of cases discussed during ward rounds. Every
student must maintain attendance for this session in the ward work diary in their log books
for these sessions which is to be signed by the consultant/specialist/TUSOM lecturer.
2. Ward work: Students will clerk and examine the patients on their own and observe
diagnostic and therapeutic procedures in the ward allotted to them from 9am to 10am.
Hospital beds are allocated to each student on a rotation basis every day. During ward work
students will clerk patients on assigned beds and give oral presentations during their
rotation for clinical presentation. Students will follow up patients and must maintain a
separate attendance for ward rounds in the clinical diary of their log books.
3. Bedside teaching (BST): A significant fraction of the core content in Year-4 Internal
Medicine is allotted for conducting bedside teaching. The whole group posted in Internal
Medicine is further divided into 2 subgroups which will be rotated in 4 different wards – 4A,
4D and 7D of Hospital Sungai buloh. There will be 1 BST daily totaling to 5 BST sessions per
week. One student will function as a student leader and will coordinate the student
activities. The student leader has to draw a roster showing the rotation of each and every
student case presentation being done every day of the week. Each student has to clerk and
examine at least 1 to 2 patients per day, write down the history and physical examination
findings in their clinical diary, and also document the name, ID, core problems and diagnosis
in their log books. As per the students’ roster, the students from two wards will combine to
form Group A and the students from the other two wards combine to form Group B and
present 2 cases (1 case from each ward) to the lecturer (either from HSB or Taylors
August 2019 Page 15
TUSOM PHASE – II PROGRAMME INT.MED 2
University). So every week, BST will be conducted in the wards, where students will present
cases clerked during ward work in beds allotted to them with the respective
lecturers/consultants. Students are required to be well equipped with all the necessary
instruments to examine all the systems.
4. Case discussion (CD): Clinical case discussion is a whole-class interactive session where
common/core clinical conditions which may or may not be seen are discussed. The clinical
approach to the condition and management will be included in the discussion. Ideally the
discussion is based on a patient clerked by a student. However, in order to ensure coverage
of all common conditions, the lecturer may conduct the discussion based on a simulated
case history. CD may last for an hour from 12pm – 1pm.
5. Lectures (L): These are presented by the lecturers as formal power-point presentations and
last between 40-50 minutes on 2nd Fridays of the month. Students are encouraged to
contribute to making lectures more interactive by asking questions or seeking clarifications
during or at the end of a lecture. Lecturers may leave an electronic copy of their
presentation for the students to print out. However, power-point presentations are not
meant to contain all material that students are expected to learn. Typically, power-point
slides will contain only an outline of the material presented by the lecturer and therefore
reading a power-point presentation cannot replace attending and actively listening to
lectures. Students are advised to supplement reading of lecture notes by referring to
recommended textbooks which are listed in the latter part of this booklet (page no.15).
6. Case based learning (CBL): Similar to PBLs in Year 2, clinical cases are formulated based on
intended learning outcomes or authentic cases that would provide the basis for achieving
intended learning outcomes for Year 3 and 4. The emphasis, in Years 3 and 4, is on learning
essential core content in clinical sciences relevant to the case in question. Students are to
work in small groups of 3 to 4 on these clinical case scenarios three days prior to the CBL
session, and return to discuss their answers in the formal CBL session every Monday
afternoon from 3pm to 5pm. From 2pm to 3pm the group members will share their
thoughts, discuss relevant issues and collate information. They will then present in front of
the whole batch and the facilitator from 3pm onwards. Overall, this strategy is student-
centered and besides serving as a stimulus to foster learning of core content in the clinical
sciences, several other attributes of the PBL process such as the opportunity to think
independently, learn how to solve problems, learn collaboratively and taking ownership of
one’s learning are expected to contribute to the overall professional development of
students. However, in a significant fraction of these sessions, the students will find it more
appropriate to enhance focus on clinical reasoning as well as take a problem-solving
approach and faculty members will function as facilitators and/or resource persons.
August 2019 Page 16
TUSOM PHASE – II PROGRAMME INT.MED 2
7. Seminar (S): Students are expected to present seminars for 1 ½ to 2 hours which is another
feature of this module to enhance learning of the core contents. The specific learning
objectives and outcomes are provided to the students around 1 to 2 weeks before the date
of the seminar session. This session is student driven and faculty assisted which is to be
conducted every Tuesday from 3pm to 5pm. These seminars are discipline specific and 6
common topics will be chosen and given to different groups in a batch. The TUSOM lecturer
with the help of the student representative allots 1 seminar topic which is further broken
down into subtopics with the intended learning objectives and outcomes to a group of 3 to
4 students. Although 3 to 4 students will make the presentation, this is intended to be a
combined group effort and all students in a group are expected to be able to answer
questions from faculty members . Lecturers will review the students’ prepared powerpoint
presentation 2 days before the seminar to ensure a precise, authoritative and fluent
presentation.
8. Clinical skills sessions (CSS): Various components of clinical skills such as history taking and
physical examination of different systems can be simulated using standardized patients and
mannequins. There will be 5 CSS sessions conducted every Wednesday for a total of 3 hours
which will include a 1 hour practice session and hands on examination of mannequins with
different simulated abnormalities of the CVS,the RS, the eye, ECGs, X-rays, etc.
9. Integrated (IL) lectures: There will be a series of lectures each of 1 hour duration conducted
across the whole semester 8 on the Fridays of weeks 1, 2 and 4 of every month, as an
integrated block which will consist of clinical therapeutics, laboratory medicine and
radiology in relation to the clinical postings. Some specific topics related to these disciplines
will be covered as separate integrated lectures covering therapeutics, radiology and
laboratory medicine relevant to the overall patient management. The clinical therapeutics
lectures will be delivered by clinical pharmacologists and/or physicians of TUSOM, radiology
lectures by radiologists from HSB & TUSOM, laboratory medicine lectures by pathologists
and microbiologists from HSB & TUSOM.
10. Integrated seminar (IS): Some clinical problems which have multi-systemic features and can
be managed by multidisciplinary teams and which will involve discussion at an
interdisciplinary level (Internal Medicine + Critical Care, Surgery + Critical Care, Internal
Medicine + Ophthalmology) will be chosen and given to students to present as integrated
seminars (IS). Here the student leader will form several groups of 3 to 4 students and allot
different topics to each group with the Specific Learning Objectives (SLO) given by lecturers
to present at each IS session.The IS will be conducted on the 3rd Friday of every month in
Semester 8 in the HSB auditorium and is to be attended by all students in Semester 7. The
August 2019 Page 17
TUSOM PHASE – II PROGRAMME INT.MED 2
whole IS session will be moderated by TUSOM/HSB specialists from the clinical disciplines
involved in IS.
11. Self-study (DSL &SDL): The field of medicine is so vast that it is impossible to cover all
required material in lectures or clinical sessions. So the students should take responsibility
and ownership of what they learn. They are advised to make effective use of the facilities
and resources available like books, journals and CD-ROMs in the Taylor’s Clinical School
libraryand the hospital library, and access the internet for online databases. They are
advised to use SDL and DSL time effectively to learn and reflect on the content in lectures,
CBL and seminars as well as topics posted specifically for “directed self-learning”. Case
scenarios in the form of Problem Solving Exercises (PSEs) are used to encourage students to
learn DSL topics, which will also be tested in both formative and summative assessments
and final exams.
Assessment Strategy:
Assessment in Internal Medicine 2 Posting is in line with the general philosophy of assessment
in Phase II and includes formative and summative assessments. Both theory and clinical
components are tested in each. Assessment of the practice of evidence based medicine and
professionalism are incorporated into these components.
Formative assessment will be held during the posting and will be in the form of MCQ, MEQ and
Long Cases. These will be held during the last week of the posting. However some of the
components assessed during the posting, namely, case reports, log book and the assessment of
professionalism will contribute towards the overall marks for the semester.
The summative assessment at the end of the semester will consist of MCQ, MEQ and OSCE
covering all postings of the semester.
Tools of Assessment:
1. Multiple choice questions (MCQ):
Multiple choice questions (MCQ) in Phase II are single best answer (SBA) type questions, that
have four options within each question. The student is required to identify the best option that
fits the stem of the question. Each correct answer gains 1 mark and there is no negative
marking.
MCQs will be used to assess factual knowledge, analytical skills, critical thinking and medical
ethics.
August 2019 Page 18
TUSOM PHASE – II PROGRAMME INT.MED 2
2. Modified essay questions (MEQ):
Modified essay questions (MEQ) are designed to assess your ability to retain important
information, evaluate clinical situations and retrieve relevant information in response to
specific lines of enquiry. They differ from traditional essay questions, which are mostly open
ended, in that specific aspects of a topic are focused on. Furthermore each question (which
may have subsections) is of shorter duration, (typically 10 minutes) as opposed to essay
questions which are of 20 to 30 minutes duration.
3. Long case clinical assessment:
Long cases are used for formative assessment at the end of the posting. These assess the
student’s ability to extract relevant information from the patient, elicit the physical signs,
formulate provisional/differential diagnoses and plan for appropriate investigations and
management. Students are required to recognize issues pertaining to the community and
ethics. Students independently see a patient and discuss findings with the examiners. Marking
is done using a rubric for long case assessment.
4. Objective Structured Clinical Examination (OSCE):
In OSCEs students are assessed on their skills in establishing rapport with patients, the
communications skills needed to obtain relevant medical information from them, giving them
advice, basic skills of examining patients and carrying out some essential procedures. Real
patients, simulated patients or mannequins will be used in OSCEs.
The ability to interpret clinical investigative reports will also be tested.
OSCEs will be conducted at the End of Semester examination.
5. Case write-ups:
Students must write 1 clinical case every 2 weeks totaling to 3 case write ups with all the
necessary details in the following format:
Patients data with the name hidden or expressed as short forms
Chief complaints
History of presenting illness
Past history
Treatment /Drug history
Social/Personal history
Family history
Review of systems
Summary of history
General examination with vital signs
Systemic examination
Provisional diagnosis
August 2019 Page 19
TUSOM PHASE – II PROGRAMME INT.MED 2
Differential diagnoses and their clinical relevance
Investigations and their clinical relevance
Management
Discussion/Learning issues
References – using Vancouver format
Each case write-up is word processed using Times New Roman, font size 12 and spacing
of 1.5 with a maximum word limit of 1500 – 2000.
6. Log book:
Students are monitored and assessed throughout the module by the clinical supervisors and
coordinator through log books which is a documentary evidence of their teaching and learning
activities from the start to end of the module.
7. Assessment of Professionalism:
Students are also monitored for Professionalism by the following ways: attendance, punctuality
(daily clock-in), attentiveness in classes and behaviour (participation, teamwork, etc).
Core topics and Mode of Delivery:
MODE OF
DOMAINS CORE TOPICS
DELIVERY
ASSESSMENT
Pulmonary hypertension Formative CA:
and corpulmonale DSL
SBA type MCQs
Pericarditis and DSL
Pericardial effusion +/- SAQs (Short
Approach to the patient DSL answer questions)
with heart murmur , Log books
Interpretation of 12-lead CSS
ECG - Review Clinical
Management of heart LEC assessments –
CARDIOVASCULAR DISORDERS
failure
Management of atrial LEC Long Case
fibrillation
Investigation of heart CSS & BST
disease
Hypertension CBL
Recognition of abnormal CSS
heart sounds
Medical Simulation: CSS
August 2019 Page 20
TUSOM PHASE – II PROGRAMME INT.MED 2
Scenario of acute
coronary syndrome
Syncope CBL
Clinical approach to DSL
interstitial and infiltrative
lung disease
Approach to a patient IB-LEC
with haemoptysis
Recognition of abnormal
lung sounds CSS
RESPIRATORY DISORDERS
Video demo of
thoracocentesis
Acute respiratory distress SDL
syndrome (ARDS) and
respiratory failure
Interpretation of LEC
Pulmonary function tests
Interpretation of CSS
abnormal chest X-rays
GASTROINTESTINAL DISORDERS Approach to patient with DSL
abdominal pain &
distension
Inflammatory bowel SDL
disorders
Gastrointestinal BST & DSL
infections
Irritable bowel syndrome DSL/SDL
Malabsorption BST, SDL
syndromes
Approach to Upper BST & DSL
Gastrointestinal bleeding
Lower Gastrointestinal
bleeding
Infiltrative diseases of SDL
the liver
Interpretation of CSS
abnormal GI radiography
Interpretation of liver LEC
function test
Paracentesis CSS
Video demo of CSS
abdominal paracentesis
August 2019 Page 21
TUSOM PHASE – II PROGRAMME INT.MED 2
Brain abscess, BST & SDL
Tuberculoma and
neurocysticercosis
Epilepsy BST & CD
Brief clinical approach to CD
paraplegia &
quadriplegia
Degenerative diseases of SDL
NEUROLOGICAL DISORDERS the nervous system:
dystrophies,
spinocerebellar ataxia
Degenerative disease of SDL
the nervous system:
motor neurone disease
and myopathies
Video demo of lumbar CSS
puncture
Interpretation of CSS
abnormal neuroimaging
Dementias SEM
Multiple sclerosis & other DSL
demyelinating disorders
Movement disorders BST & SEM
Epilepsy CD
Disorders of sleep, BST
speech and vision
Neuromuscular junction DSL
disorders
RENAL & UROGENITAL Polycystic kidney disease BST & SDL
DISORDERS & inherited disorders of
kidney
Infections of the kidney BST & SDL
and urinary tract
Renal replacement BST & CD
therapy
Renal involvement in BST & CD
systemic disorders
Interpretation of renal LEC/BST
function test
Tubulo-interstitial BST
disorders & Renovascular
disorders
Urinary tract calculi and BST
Tumours of kidney
August 2019 Page 22
TUSOM PHASE – II PROGRAMME INT.MED 2
Diabetic retinopathy and
neuropathy
Diabetic nephropathy BST & CBL
and management
Diabetes – chronic
macrovascular
complications and
management
Thyroid disorders – BST
management
Disorders of calcium, DSL & IL
phosphorous metabolism
and Parathyroid glands
Disorders of adrenal BST
ENDOCRINE DISORDERS &
hyper and hypo-function
DISORDERS OF METABOLISM Disorders of pituitary BST
hyper and hypo-function
Hyperlipidemias BST
Diabetes insipidus and BST
SIADH
Myeloproliferative BST
disorders (Leukaemias)
Lymphoproliferative BST
disorders (Lymphomas)
Approach to common DSL
oncological conditions
Other hematological BST
malignancies
HAEMATOLOGY AND ONCOLOGY (Myelodysplastic
syndromes, Multiple
Myeloma, etc.)
Anaemia CBL
Disorders of coagulation BST
and venous thrombosis
Blood products and BST
blood transfusion
Scleroderma, SDL
Polymyositis and
RHEUMATOLOGY AND Dermatomyositis
IMMUNOLOGY Ankylosing spondylitis, SDL
spondyloarthritis and
other seronegative
arthritis
Sarcoidosis and BST
Amyloidosis
Inflammatory muscle BST
August 2019 Page 23
TUSOM PHASE – II PROGRAMME INT.MED 2
disease and fibromyalgia
Management of RA & SDL
SLE
Polyarthralgia BST & SDL
Transplantation and BST
immunosuppression
Helminthic & systemic BST
fungal infections
Protozoal infections Part- BST
1&2
Pulmonary and Extra BST
INFECTIOUS DISEASES pulmonary Tuberculosis
HIV & AIDS BST & CD
Infections CBL
Approach to a patient IB-LEC
with pyrexia of unknown
origin
Common Cutaneous CLINIC /
fungal infections WARD
Common skin disorders:
Major manifestations of SEM
skin diseases and their
clinical approach
infections and
infestations - scabies,
pyoderma, systemic
candidiasis, etc.
Allergic skin reactions:
Eczema, psoriasis, etc.
DERMATOLOGY
Cutaneous drug
reactions
Disorders of CLINIC /
pigmentation WARD
Disorders of the nails
Skin manifestations of
systemic diseases
Approach to a patient
with skin rash
GERIATRICS Common Geriatric PSE/DSL/BST
problems
August 2019 Page 24
TUSOM PHASE – II PROGRAMME INT.MED 2
Assessment Methods and Types:
1. The End of Posting (EOP) Summative CA comprises of the following:
- Theory Paper : 30 MCQs – single best answer with 4 options for 55 minutes and
Clinical Long Case Assessment (50%)
- Marks are allotted as per the rubric (Long case assessment form, the sample is given
in Log book) and the overall results are graded as A, B+, B, C+ C, D
Feedback is given at the end of posting based on the above as well as the Mid & End of Posting
reviews by the clinical supervisors.
2. End of Year (EOY) Summative CA is to be conducted at the end of Year 4:
The EOY examination assesses all the postings of Semester 7 and Semester 8 and the
details of this, students are referred to the Phase II student handbook.
August 2019 Page 25
TUSOM PHASE – II PROGRAMME INT.MED 2
Reading List:
Core Text:
1. Nicki R. Colledge, Brian R. Walker, Stuart H. Ralston. Davidson’s Principles and Practice
of Medicine, Elsevier Saunders
2. Kumar PJ and Clarke M. Kumar and Clarke’s Clinical Medicine, Elsevier Saunders
Clinical Methods:
1. Glynn M, Drake W. Hutchison’s Clinical Methods, Elsevier Saunders
2. Douglas G, Fiona Nicol, Colin Robertson. Macleod’s Clinical Examination, Elsevier
Saunders
References
1. Dan Longo, Anthony Fauci, Dennis Kasper, Stephen Hauser, J. Jameson, Joseph
Loscalzo Harrison’s Principles of Internal Medicine, 2 volumes, McGraw Hill.
2. Talley NJ and O'Connor S. Clinical Examination. A Systematic Guide to Physical
Diagnosis. Sydney: Churchill Livingston, Elsevier,
3. Alagappan. R. Manual of Practical Medicine, Jaypee Digital
4. Murray Longmore, Ian Wilkinson, Edward Davidson, Alexander Foulkes, and Ahmad
Mafi Oxford handbook of clinical medicine, Oxford University Press
5. Hampton J, The ECG Made Easy, Elsevier
6. Clarke C & Dux A, X-rays for Medical Students Wiley Blackwell
7. Foster C, Mistry N, The Washington Manual® of Medical Therapeutics, Wolters Kluwer
& Lippincott Williams & Wilkins
Online references:
1. Clinical key: www.clinicalkey.com
2. BMJ: www.bmj.com , www.learning.bmj.com , www.bestpractice.bmj.com ,
www.onexamination.com
3. Medscape & emedicine: www.emedicine.medscape.com
4. The New England Journal of Medicine: www.nejm.org
August 2019 Page 26
You might also like
- Clinical Medicine Ashok ChandraDocument52 pagesClinical Medicine Ashok ChandraVaishnavi Agrawal100% (1)
- 4 Respiratory Study GuideDocument32 pages4 Respiratory Study GuideShariq KhattakNo ratings yet
- Letter To The Editor NotesDocument4 pagesLetter To The Editor NotesDiane ShellyNo ratings yet
- ECS HFC-227ea - Owner's Manual - February 2001-06-236118-001 - Rev - AADocument36 pagesECS HFC-227ea - Owner's Manual - February 2001-06-236118-001 - Rev - AAgilangolandiaNo ratings yet
- Textbook of Practical Physiology110718 PDFDocument25 pagesTextbook of Practical Physiology110718 PDFLalit Narayana0% (2)
- 2 Blood and Immunology Module Study GuideDocument37 pages2 Blood and Immunology Module Study GuideMaryam FidaNo ratings yet
- Chronic Kidney Disease Case StudyDocument96 pagesChronic Kidney Disease Case StudyJUDE ARIZALANo ratings yet
- Lumbar PunctureDocument23 pagesLumbar Puncturemamoon100% (2)
- Semiologie Medicala Sem IDocument6 pagesSemiologie Medicala Sem IDana LebadaNo ratings yet
- Syllabus NCM 103Document11 pagesSyllabus NCM 103ivanguzman86No ratings yet
- Kidney Block Book 2017 For Student PDFDocument39 pagesKidney Block Book 2017 For Student PDFHarsya Parma PhastikaNo ratings yet
- 306 PathologyDocument16 pages306 PathologyHSm FbtNo ratings yet
- Appendicitis Case StudyDocument35 pagesAppendicitis Case StudyWilliam Soneja CalapiniNo ratings yet
- Adult Health Nursing Course Grid - Yr II Sem IIDocument43 pagesAdult Health Nursing Course Grid - Yr II Sem IIHamayun Khan100% (2)
- Renal, Endocrine and ReproductionDocument33 pagesRenal, Endocrine and ReproductionAbdurehman ShahNo ratings yet
- GIT & Hepatobilliary-II Module (Block-K)Document36 pagesGIT & Hepatobilliary-II Module (Block-K)F ParikhNo ratings yet
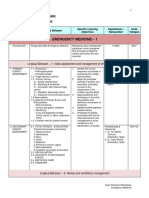
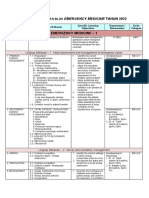
- Lingkup Bahasan Blok Emergerncy Medicine 2019Document14 pagesLingkup Bahasan Blok Emergerncy Medicine 2019Juang ZebuaNo ratings yet
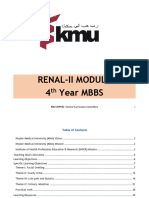
- RENAl SyllabusDocument33 pagesRENAl SyllabusArmaghan GulNo ratings yet
- Syllabus NCM 104Document10 pagesSyllabus NCM 104ivanguzman860% (1)
- Medicine II MODLUE BOOK Spring 2023Document4 pagesMedicine II MODLUE BOOK Spring 2023Osama MalikNo ratings yet
- Git & Hepatobiliary-Ii 4 Year MBBS: KMU (IHPER) - Central Curriculum CommitteeDocument50 pagesGit & Hepatobiliary-Ii 4 Year MBBS: KMU (IHPER) - Central Curriculum CommitteeF ParikhNo ratings yet
- Lingkup Bahasan Blok Emergency Medicine 2022Document13 pagesLingkup Bahasan Blok Emergency Medicine 2022emma19No ratings yet
- Specifications: 'LFRT,"Document82 pagesSpecifications: 'LFRT,"waled badawyNo ratings yet
- Ablist Modul Final JakartaDocument750 pagesAblist Modul Final JakartaardianNo ratings yet
- NRS 205 Advanced Nursing Part B SP 17Document22 pagesNRS 205 Advanced Nursing Part B SP 17james jonhsonNo ratings yet
- MD - Peadiatrics - (Revised) - Copy ExportDocument37 pagesMD - Peadiatrics - (Revised) - Copy Exportpradeepgullipalli.1089No ratings yet
- Semiologie Medicala SEM IIDocument8 pagesSemiologie Medicala SEM IIDana LebadaNo ratings yet
- Roberts Miebaka La1 - 161BDocument2 pagesRoberts Miebaka La1 - 161BbrightagbotuiNo ratings yet
- NRSG 352 Course SpecificationDocument7 pagesNRSG 352 Course SpecificationDrmirfat AlkashifNo ratings yet
- PhysiologyDocument12 pagesPhysiologyrajan guptaNo ratings yet
- FEX 2007.1Document18 pagesFEX 2007.1j.jk.jk.17No ratings yet
- Physiology 2Course Specifications Template Updated PTDocument6 pagesPhysiology 2Course Specifications Template Updated PTmariemebrahem404No ratings yet
- DM Pulmonary MedicineDocument7 pagesDM Pulmonary MedicineAJITH KUMARNo ratings yet
- Fourth ClassDocument71 pagesFourth Classhomamamm7No ratings yet
- MED 507 - Pediatrics IDocument14 pagesMED 507 - Pediatrics Iعبد المجيد محمد صالح الفقيهNo ratings yet
- University of Nevada, Reno School of Medicine Syllabus: Internal Medicine Clerkship, Elko Imed 651 Elko, NevadaDocument29 pagesUniversity of Nevada, Reno School of Medicine Syllabus: Internal Medicine Clerkship, Elko Imed 651 Elko, NevadaAna CanastraNo ratings yet
- PHARMACY PRACTICE & CLINICAL PHARMACY dEPARTMENT (PDFDrive) PDFDocument83 pagesPHARMACY PRACTICE & CLINICAL PHARMACY dEPARTMENT (PDFDrive) PDFDinesh Kumar YadavNo ratings yet
- Principles of Family Medicine TextbookDocument137 pagesPrinciples of Family Medicine TextbookbunnyhopkinNo ratings yet
- 1pediatrc Training LogbookDocument20 pages1pediatrc Training Logbookareen saberNo ratings yet
- Log Book PediatricsDocument22 pagesLog Book Pediatricsرافت العواضيNo ratings yet
- LECTURE 1 (August 4, 2022) - AM SESSION: Dopamine - Can Help Contract The HeartDocument344 pagesLECTURE 1 (August 4, 2022) - AM SESSION: Dopamine - Can Help Contract The HeartMeanie ManszNo ratings yet
- An Introduction To AnaemiaDocument77 pagesAn Introduction To AnaemiaLinux LinuxNo ratings yet
- FerrAurum-22: NanoSystem For Control of Symptomatic Diabetes MellitusDocument42 pagesFerrAurum-22: NanoSystem For Control of Symptomatic Diabetes MellitusdrashtiNo ratings yet
- MBBS Scheme Feb2014Document23 pagesMBBS Scheme Feb2014Sasikala MohanNo ratings yet
- Group2 End Stage Renal Disease Case PresentationDocument106 pagesGroup2 End Stage Renal Disease Case PresentationDoneva Lyn MedinaNo ratings yet
- Elective Course Topics-1Document9 pagesElective Course Topics-1Rebecca WongNo ratings yet
- Immersion Course Specifications V2020-EngDocument8 pagesImmersion Course Specifications V2020-EngDrmirfat AlkashifNo ratings yet
- Endocrinology Module Study Guide 2023 FinalDocument24 pagesEndocrinology Module Study Guide 2023 Finaldomitam105No ratings yet
- Internship LogbookDocument9 pagesInternship Logbooksarhang talebaniNo ratings yet
- YL8 Case Presentation and Patient Charting Rating Scale PDFDocument1 pageYL8 Case Presentation and Patient Charting Rating Scale PDFJenLNo ratings yet
- Semiologie Medicala Sem IDocument6 pagesSemiologie Medicala Sem IAndaDiaconuNo ratings yet
- Neurosciences 1 Module Study Guide 2023Document22 pagesNeurosciences 1 Module Study Guide 2023faariyaabdullah03No ratings yet
- Concordia CollegeDocument14 pagesConcordia CollegeChristian PaulNo ratings yet
- MD Physiology 1Document13 pagesMD Physiology 1arunadavis3No ratings yet
- The Treatment of Chronic Low Back Pain Following The Principles of The Fascial Distortion ModellDocument74 pagesThe Treatment of Chronic Low Back Pain Following The Principles of The Fascial Distortion ModellsimonyanNo ratings yet
- 1.1 Nursing Care of A Patient Assessment Tool - Version 2 - 2014Document3 pages1.1 Nursing Care of A Patient Assessment Tool - Version 2 - 2014danielndaa51No ratings yet
- Medicine KMC SyllabusDocument28 pagesMedicine KMC SyllabusMalvika BabuNo ratings yet
- Study Guide Musculoskeletal Module: 1 Professional MBBS (Session 2018-19)Document42 pagesStudy Guide Musculoskeletal Module: 1 Professional MBBS (Session 2018-19)Shariq KhattakNo ratings yet
- 1 - Surgical Area - 2022-2023Document1 page1 - Surgical Area - 2022-2023Ana ElshekhNo ratings yet
- Course Details Module UltrasonographyDocument10 pagesCourse Details Module UltrasonographyDr. Pallavi SinghNo ratings yet
- Obs1 41 Course Specification CorrectedDocument10 pagesObs1 41 Course Specification CorrectedWek KivNo ratings yet
- Pulmonary Topics Objectives Reference: Our Lady of Fatima University Department of Internal MedicineDocument6 pagesPulmonary Topics Objectives Reference: Our Lady of Fatima University Department of Internal MedicineAlmar NuñezNo ratings yet
- Hardness Test (Lab Report)Document14 pagesHardness Test (Lab Report)Kavin VarmaNo ratings yet
- Internal Medicine 2 Case Write-Up: School of Medicine Bachelor of Medicine Bachelor of SurgeryDocument18 pagesInternal Medicine 2 Case Write-Up: School of Medicine Bachelor of Medicine Bachelor of SurgeryKavin VarmaNo ratings yet
- MEC60204 Engineering Solid Mechanics Lab Report Deflection of Tie Bar Module Coordinator: Dr. Chou Pui MayDocument17 pagesMEC60204 Engineering Solid Mechanics Lab Report Deflection of Tie Bar Module Coordinator: Dr. Chou Pui MayKavin VarmaNo ratings yet
- Final ReportDocument28 pagesFinal ReportKavin VarmaNo ratings yet
- Ethico Legal Issues Affecting Disaster Nursing ManagementDocument25 pagesEthico Legal Issues Affecting Disaster Nursing ManagementKaylaNo ratings yet
- Plank Hold: Lesson 1Document12 pagesPlank Hold: Lesson 1alallaallalaNo ratings yet
- Green Dentistry, A Metamorphosis Towards An Eco-Friendly Dentistry: A Short CommunicationDocument2 pagesGreen Dentistry, A Metamorphosis Towards An Eco-Friendly Dentistry: A Short CommunicationAlexandru Codrin-IonutNo ratings yet
- 2017-ENG-Ljiljana Stošić Mihajlović-Socijalno Preduzetništvo Podržano Kreativnom EkonomijomDocument14 pages2017-ENG-Ljiljana Stošić Mihajlović-Socijalno Preduzetništvo Podržano Kreativnom EkonomijomSandra NikolicNo ratings yet
- JEY ANN CANDAME UNDERSTANDING THE SELF Module 7Document8 pagesJEY ANN CANDAME UNDERSTANDING THE SELF Module 7ren alvaradoNo ratings yet
- Glasgow 12-Lead ECG Analysis Program Statement of Validation and Accuracy 3302436.ADocument32 pagesGlasgow 12-Lead ECG Analysis Program Statement of Validation and Accuracy 3302436.AKiattisak PrajongsinNo ratings yet
- TIMOTHYDocument3 pagesTIMOTHYShan ElahiNo ratings yet
- McDonal Data Analysis PDFDocument16 pagesMcDonal Data Analysis PDFAnandha SayanamNo ratings yet
- 1 The Ultimate Success MantraDocument25 pages1 The Ultimate Success MantraAbhishek MishraNo ratings yet
- Ecological Profile 2021Document405 pagesEcological Profile 2021mcnuquiNo ratings yet
- Elrha GapAnalysis GBV Accessible PDF 2021Document104 pagesElrha GapAnalysis GBV Accessible PDF 2021chilyata kabwalwaNo ratings yet
- La ConsolacionDocument2 pagesLa ConsolacionRex RegioNo ratings yet
- Robert Morris Relocation PlanDocument7 pagesRobert Morris Relocation PlanFOX56 NewsNo ratings yet
- Opening Toward Life Experiences of Basic Body Awareness Therapy in Persons With Major DepressionDocument14 pagesOpening Toward Life Experiences of Basic Body Awareness Therapy in Persons With Major DepressionALEJANDRA NOGUERA PEÑANo ratings yet
- My Resume 1Document5 pagesMy Resume 1api-553045669No ratings yet
- Research Ethics in Social SciencesDocument3 pagesResearch Ethics in Social SciencesGame KingNo ratings yet
- Radiographic Special Procedures: Kenneth M. Luciano, RRTDocument36 pagesRadiographic Special Procedures: Kenneth M. Luciano, RRTKaye A. JardinicoNo ratings yet
- Beer, Whiskey, Alcoholic Drinks May Come Under Food Regulator FSSAI Lens - The HinduDocument3 pagesBeer, Whiskey, Alcoholic Drinks May Come Under Food Regulator FSSAI Lens - The Hindustar childNo ratings yet
- Obstacle CourseDocument20 pagesObstacle CourseBalba ChrislynNo ratings yet
- Key Determinants of Happiness and MiseryDocument22 pagesKey Determinants of Happiness and MiseryVlastimil VohánkaNo ratings yet
- Unit 6: Q2e Listening & Speaking 3: Audio ScriptDocument8 pagesUnit 6: Q2e Listening & Speaking 3: Audio ScriptQuỳnh LươngNo ratings yet
- InfloranDocument19 pagesInfloranMuhammed AskarNo ratings yet
- Temporary Student Hub - Request LetterDocument3 pagesTemporary Student Hub - Request LetterJeofy PamaNo ratings yet
- Social Marketing: Improving The Quality of Life (2nd Edition)Document3 pagesSocial Marketing: Improving The Quality of Life (2nd Edition)narenkittuNo ratings yet
- Risk Assessment Band SawDocument5 pagesRisk Assessment Band SawybuluckNo ratings yet
- Diabetic KetoacidosisDocument21 pagesDiabetic KetoacidosisMaryam MartawigunaNo ratings yet
- Case # 4 Difficulty of BreathingDocument6 pagesCase # 4 Difficulty of BreathingGrace TanajuraNo ratings yet