Professional Documents
Culture Documents
Neuro Optha Mariano 6
Uploaded by
Dey SibalOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Neuro Optha Mariano 6
Uploaded by
Dey SibalCopyright:
Available Formats
Quid Refert, Dummodo non Desinas, Tardius Ire
Neuro-Optha
Opthalmology Dr. Mariano
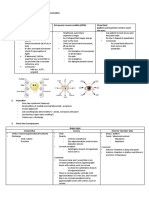
BASIC NEURO-OPTHALMOLOGY All cranial nerves are at the brainstem or anteriorly at the cavernous
sinus
AFFERENT (light going in to EFFERENT (for ocular movement)
occipital lobe)
Retina CN 3, 4, 6
Optic n. Ocular muscles
Chiasm Brainstem
Tract Pursuit & Saccadic
Cortex pathways
Common Problems Seen
Loss of vision (transient, constant, mono/binocular)
Diplopia
Ptosis
Visual disturbance
pupillary light reflex→ it ends in the pretectal nucleus and it does not go
Pupil irregularities
all the way to the occipital lobe, so you can be occipitally blind but you
Motility disorders
still have pupillary reaction.
Eyelid or facial spasms
Direct - constrict SAME side
Consensual - constrict DIFFERENT side
Considerations
If you shine a light and it doesn't constrict: problem is AFFERENT first,
Where/What is the lesion (read visual fields, interpret, and be able
maybe there's a problem in transmission, the way for you to know is to
to localize the lesion)
check the Consensual, if it doesn’t constrict in consensual then then
o bitemporal hemianopsia → lesion at optic chiasm, nearest to
problem really is AFFERENT
the pituitary so consider a sellar mass
Torch test (swinging penlight test): do it one eye at a time, look for your
When did it start
direct and consensual, what we look at is how brisk, how fast it constricts
How did it present
and re-dilate
o Patient may come to you that her vision is frosted or under
water
Urgent/Emergent
PUPILLARY LIGHT REFLEX PATHWAY
Light shined on one eye
↓
Retina
↓ Sudden & Acute → Vascular
Optic nerve Gradual, progressive → tumor (something that’s compressing)
↓ Long duration + associated pain → Inflammatory
Optic chiasm
↓ RELATIVE AFFERENT PUPILLARY DEFECT (RAPD)
Optic tract
↓ to occipital lobe Normal response
Lateral geniculate nucleus There’s consensual light reflex but there’s NO DIRECT light reflex on the
↓ affected eye
Pretectal nucleus Can be caused by
↓ Optic neuritis or
Edinger-Westphal nucleus on both sides Tumor anterior to the chiasm
↓ To test, ask the Px to look at a distance and do it fast (Marcus Gunn
Constriction of both pupils test/Swing light test)
Normal reaction → when light is shined on one eye → both eye
If a pupil doesn't constrict: Problem in EFFERENT (CN 3) constricts
While shining a light, don’t put it straight away, start underneath
because when you put it straight → the eye converges
Ang pagmamalaskit hindi nakikita ng mata,
kundi sa puso nadarama… Page 1 of 6 Miki
When the eyes look at a near object, three responses occur – OCCULOMOTOR NERVE (CN 3) PALSY
accommodation, convergence, and constriction ofthe pupil –
bringing a sharp image into focus on corresponding retinal points. eye is looking down and out + ptosis “No one loves you when you’re
(Video showing R. Eye with direct response and L. Without direct down and out”
response) → RAPD check for pupillary light reflex → will tell you the urgency of the case
If px complains of blurring of vision, and patient reads 20/400 and other if pupils are dilated → think of an aneurysm
eye is 20/20 and you check the pupil but didnt see an RAPD -- px thinks patient may have aneurysm ..and the first sign of aneurysm is a CN3
its an optic neuropathy (optic nerve problem) → Isometropic amblyopia problem + pupillary involvement and the most common site of aneurysm
(lazy eye) problem is in the connection - the brain is trying not to use one is at the junction of the PCOMM. (posterior communicating artery
eye aneurysm)
If you dont see RAPD → there's NO problem in the visual pathway Ruptured aneurysm 70% mortality
If with RAPD - problem in the VISUAL Pathway
If you see a problem with the swinging light test, and it patient saw a ABDUCENS NERVE (CN 6) PALSY
very red color but other eye saw a faded red and you see an RAPD →it is
really a problem with the optic nerve
Anatomical facts:
In examining pupils, you can have anisocoria- unequal sized pupils; few
Origin of CN 6 w/c innervates lateral rectus but also gives fibers
things to consider
w/c eventually end at the contralateral medial rectus
1. Is this an emergency
Most common nerve affected or sensitive by raised pressure (swollen
2. If an emergency, you can see a neuro-ophthalmologist from 1-2wks
optic nerve)
pupillary emergencies: if one pupil is bigger than the other and
Diplopia at distance → face turn toward same side will relieve double
accompanied by a motility problem (if pupil is dilated and is not
vision
moving) also if there’s a pupil abnormality together with ptosis→
immediate imaging & referral to neuro-opthalmologist
TROCHLEAR NERVE (CN 4) PALSY
EFFERENT SYSTEM DISEASES
Only CN which exits dorsally, “stupid nerve” – it can go straight but
Diplopia
instead goes down and up again then to other side
CN palsy
Thinnest (slender)
Multiple CN palsy
Longest intracranial course 75mm
Abnormal eye movement
Only CN which crosses opposite side
Myasthenia gravis
Oblique diplopia
Patient will complain that one image is HIGHER than the other
DIPLOPIA To relieve double vision → Patient will tilt their head (if acute, px may
Key question: not present with head tilt)
Is it only in one eye? Parks-Bielschowski 3-step test
Does it go away when you close either eye? Commonly associated with brain tumors that’s NOT associated with
If a Px come to you with a complaint of double vision and raised pressure
disappears after covering one eye → investigate.
If double vision still persist → can be an Error of Refraction MULTIPLE CRANIAL NERVE NEUROPATHIES (3, 4, 6)
Mononuclear diplopia is always refractive in origin
Cataract & astigmatism Important here is AGE of the patient
Examine lids and pupils in addition to eye movement
<50yo – NOT hypertensive, NOT diabetic → Immediate imaging
Examine all CN >50yo – known hypertensive & diabetic, smokes, drinks, if only 1
Check V1 (corneal sensation), consider cavernous sinus problem CN affected you can only observe
Ischemic CN neuropathies are almost always isolated
CN 3, 4, 6 (for ocular motility) If multiple simultaneous CN, suspect lesion in posterior orbit/cavernous
sinus region
Usually d/t mass lesion
Cranial nerves are all bunched up in the brainstem and the cavernous
sinus, so any lesion affecting these areas will also affect cranial nerves
Differentiate if lesion is from the brainstem or cavernous sinus
Cerebellum is beside brainstem → px w/ brainstem problem will
also present with cerebella problem
If NO cerebellar problems → think of a cavernous sinus problem
(think of a cavernous sinus THROMBOSIS)
MYASTHENIA GRAVIS
great mimicker → can mimic any cranial nerve problem
hallmark: variability and fatigability
mechanism: autoantibodies directed against Ach
receptors are produced and destroy and block a lot of receptors
Ocular myasthenia gravis
Can be a vasculopathic cranian nerve neuropathy Myasthenic signs restricted to ocular muscles
Demyelinating disease Fatiguable diplopia & ptosis
Compressive First sign of MG >70% are with eye sign
Trauma ICE TEST or REST TEST in the clinic demonstrate improvement (Ice
↑ ICP test in the → (+) if Px can open their eyes after application of ice)
CN 4 & 6 = will always complain of DIPLOPIA Ach receptor antibodies (+) in 50% only
Complete CN 3 palsy = will complain of diplopia because he has ptosis Single fiber EMG
(elevate that lid and look if dilated) TENSILON TEST (Give atropine bec. one S/E is cardiac arrest) – done
rarely, costs 40k, double vision disappears, effect is around 30s
Ang pagmamalasakit hindi nakikita ng mata,
kundi sa puso nadarama Page 2 of 6 Miki
Natural pattern
¼ present w/ diplopia or ptosis
80% may start to develop systemic weakness within 2yrs
Optical Treatment
Prisms
Occlusion
Medical
Pyridostigmine (Mestinon) – anticholinesterase
Prednisone – suppresses autoimmune process
Steroid-sparing drugs
Surgical
Thymectomy
Ptosis & Strab – must be stable, longer, better & must be informed
properly
CLUES in DIAGNOSING DIPLOPIA
Variability & Fatigability → MG Macular sparing → OCCIPITAL
Distance → CN 6, IIH, ↑ICP Meyers Loop - while it goes to the optic radiation. Some fibers go up
Near → CN3, INO to parietal lobe and some fibers go down to temporal lobe then
Down and out → CN3
meet at the occipital cortex
Monocular → Error of Refraction
Occipital lobe function is purely visual – Px would come to you
Tilting → CN 4
with Hx of bumping onto objects
Multiple CN → MG, CST
Temporal & Parietal are integrators- they let their vision come
from the optic nerve to the cortex, it gives visual cues: the WHAT &
VISUAL FIELD DEFECTS WHERE
There’s one px, wherein she couldn’t read the Snellen but when
Only the NASAL optic nerve traverses to the other side whereas the shown a single letter, vision was 20/20 → Simultagnosia (MRI
TEMPORAL doesn't, that's why posteriorly (beyond the chiasm), a lesion showed affecting the parietal, px presents w/ diffulties in
will manifest on both parts of the visual field will be affected comprehensionalso)
Any lesion posterior to the chiasm → always HOMONYMOUS
Anterior to the chiasm → only ONE eye is affected
PIE in the SKY defect (SUPERIOR quadrantinopsia) → lesion in TEMPORAL
Can either be occipital/temporal but NEVER Parietal
PIE in the FLOOR defect (INFERIOR quadrantinopsia) → lesion in
PARIETAL
Always parietal or occipatl but NEVER Temporal
Confrontation Field test
Make sure you cover one eye and eye-level with the examiner
Draw confrontation field (baliktad) on how patient sees it NOT how
you see it
If field defect is on the L. side – look for it at the R. side of brain
More congruous homonymous hemianopsia → lesion in OCCIPITAL
Ang pagmamalasakit hindi nakikita ng mata,
kundi sa puso nadarama Page 3 of 6 Miki
AFFERENT SYSTEM DISEASES TYPICAL OPTIC NEURITIS
Optic neuritis Inflammation of the optic nerve, often caused by demyelinating event (in
Ischemic optic neuropathy (arteritic vs. non arteritic) the US), in the Philippines it is purely inflammation or caused by bleeding
Toxic optic neuropathy (e.g. ethambutol toxicity) sudden vision loss with optic disc swelling
other optic neuropathies (compressive, papilledema, inflammatory, CARDINAL sign is decreased vision (especially color), seeing faded color
hereditary) suggests optic nerve problem
chiasmopathies/chiasmal disorders pain with eye movements
stroke that causes defects in the visual field females > males
RAPD present
OPTIC DISC Optic disc normal (2/3)
brown hair, blue eyes → observe for few weeks
Look for disc borders, hemorrhage, color (if pale), cup-disc ration typically found in Caucasian people
(reported as 0.3, 0.5 etc.) age b/w 15-45y/o
Pale optic disc → atophy (20% have tumor) it is associated with MS (Multiple Sclerosis) – sakit ng mga people away
In papilledema, there should be increase ICP, if there is no from the equator
mentioned increase ICP, label it as optic head swelling or disc In the Phil’s, most common cause is inflammatory or infectious
edema (normal ICP = 15-25 mmHg) Unilateral
pallor – vision affected > 6 weeks Pain
o On eye movements
o First symptom to appear & disappear (when pain disappears, vision
would drop)
R’s in Optic Neuritis
Radiology
o MRI is only done to see White matter lesions to confirm MS
(75% over 15yrs)
o More lesions ↑ risk of developing MS
Recover
o IV steroids only hasten recovery but not final VA outcome
Risk factors
(N. optic disc) o 20-40yo, F, white, family Hx of MS
Recurrence
In disc is swollen & with hemorrhage, bilateral already, can be o Higher with those given with oral steroids (standard doses)
hypertensive retinopathy, consider space occupying lesion →
BRAIN TUMOR Most common symptom: PAIN on EYE MOVEMENT
Most common Visual Field Defect: DIFFUSE
Typical pattern: 1-2wks – stable visual acuity, after 2wks – improved
vision
Treatment of choice for typical optic neuritis – A. IV methylprednisolone
250mg 4x/d for 3days with Oral steroids 60 mg for 11 days (eto sagot
palagi due to optic neuritis trial but not because final visual acuity of
receiving steroids vs not is the same) B. Prednisone 60mg 1x/d for 14
days C. IV dexamethasone 20mg 1x/d
Treatment of Choice → OBSERVE (improve spontaneously)
If not improving in 2wks time – then do imaging and IV steroids
Differentiate optic neuritis from papilledema; clinically, make the Px
READ
o Optic nerve swelling but Px can read 20/20 → Papilledema on
ACUTE onset, if >6wks chronic already; difficulty reading
o Subtle findings, good visual acuity with light perception → Optic
neuritis
Atypical optic neuritis: (typical occurs in ages 15-45) you’re supposed to
do imaging
PAPILLEDEMA
Disc edema d/t ↑ ICP (mass, pseudotumor cerebri), optic nerve edema
Headache, transient visual obscurations, diplopia, tinnitus (ringing
sound), complains of changes in vision
Normal visual acuity & visual fields early
Opthalmoscopy & Imaging
Ang pagmamalasakit hindi nakikita ng mata,
kundi sa puso nadarama Page 4 of 6 Miki
Px came with a (-) 300 grade meaning myopic, recently came with a shift PUPILLARY ABNORMALITIES
in refraction with (-) 100, MRI revealed a tumor, the cause of the shift is
↑ICP, optic nerve is bathed in CSF so CSF will go to the optic nerve Anisocoria – unequal pupil size
sheath, push the eyeball. myopic eye is very long, so eyeball was pushed Difference in size is:
to be smaller o more prominent in the DARK = HORNER’s (frequent board
Image below shows ill-defined borders exam question)
Papilledema is NOT a diagnosis, the prerequisite is raised ICP o more prominent in the LIGHT = ADIE’S (anisocoria with deep
tendon abnormalities)
o DARK = LIGHT → Physiologic
Anisocoria with any motility problem = consider Aneurysm
Can be accidental discovery
Physiologic in 40% of patients
It can be isolated or associated with lid or ocular motility abnormalities
Can be iatrogenic or self-induced (Pharmacologic)
HORNER’s SYNDROME
CENTRAL RETINAL ARTERY OCCLUSION (not discussed)
Painless loss of vision
May be preceded by Amaurosis Fugax
Source of emboli usually carotid or cardiac
Less common causes: vasculitis (GCA, Anti-phospholipid syndrome)
Order Carotid Doppler Study A defect in oculosympathetic flow to the eye (pupil does not dilate in
DARK)
Sympathetic innervation is affected, Muller’s muscle is sympathetically
ARTERITIC ISCHEMIC OPTIC NEUROPATHY
innervated only contributes 1mm lid elevation (slightly ptotic only)
TRIAD
patients > 60 y.o. (older age group) headache, malaise, myalgia (calf 1. Ptosis
pain), weight loss, fever, jaw claudications and transient loss of vision 2. Anhydrosis
Labs: ESR, CRP high 3. Miosis (worst in dark)
Temporal artery biopsy Internal carotid artery dissection, neck trauma or surgery, Brainstem
> 3 cm is needed due to skip lesions strokes (Wallerburg Syndrome), apical lung tumors
giant cell arteritis/Temporal cell arteritis Urgent MRI/MRA of the head and neck for ACUTE Horner’s Syndrome
Immediately give high steroids or else the px can go blind or px may die “One horny PAM from the coast”
because there is active inflammation of all blood vessels One = T1 lesion (from the posterior hypothalamus it goes all the
do temporal artery biopsy, get about 3-5cm specimen b/c there are skip way to T1 then up the carotids)
lesions Horny = Horner’s
patient always present with severe pain, headache, malaise, weight loss PAM = triad
(b/c patient has jaw claudication every time the patient tries to Coast = Pancoast Syndrome (tumor of the lungs)
eat→patient has to change his/her diet) Horner’s syndrome, SUDDEN onset + pain → Dissecting aneurysm
normally present with disc pallor (optic nerve should be orange, if pale or OCULOSYMPATHETIC PATHWAY
chalky white →optic nerve ATROPHY)
COMPRESSIVE LESIONS
slowly progressive loss of vision (in optic neuritis, it is sudden)
can be unilateral/bilateral DIAGNOSIS
pituitary tumors, craniopharyngiomas & meningiomas of the skull base Cocaine test → tell if Horner’s or NOT
require MRI for diagnosis Testing topical cocaine in the conjunctival sac differentiates
Horner's syndrome, in which the pupil does not dilate, from
physiologic anisocoria
Testing with hydroxyamphetamine drops → localize the lesion
3rd test: Apraclonidine test – get sudden result
Ang pagmamalasakit hindi nakikita ng mata,
kundi sa puso nadarama Page 5 of 6 Miki
Px with carotid dissection – manifested with Horner’s because
oculosympathetic pathway goes down and up with the carotids
ADIE’S/TONIC PUPIL
END
Black – from power point
Blue – trans from lecturer
Red – from book
Green – old trans
SEGMENTAL CONSTRICTION - Pathognomonic
Damage to the CILIARY GANGLION and/or short ciliary nerves
Sluggish or no reaction to light
Tested in a WELL-LIGHTED room
HALLMARK:
Delayed dilation after constriction (slow redilation)
Segmental constriction → BAG of WORMS
Constricts to 0.125% Pilocarpine
DTR’s may be affected → ADIE-HOLMES
Sweating only on one side of body → ADIE-ROSS-HOLMES Syndrome
LIGHT NEAR DISSOCIATION
Initially present with dilated pupil but will later become constricted
CLUES in DIAGNOSING ANISOCORIA
Dark > Bright → HORNER’S
Bright > Dark → ADIE’S
Dark = Bright = accommodation → PHYSIOLOGIC
Dark = Bright < accommodation → LIGHT NEAR DISSOCIATION
Anisocoria +/- CN3 → ANEURYSM
NOT DISCUSSED
Ang pagmamalasakit hindi nakikita ng mata,
kundi sa puso nadarama Page 6 of 6 Miki
You might also like
- Steatorrhea Medical Biochemistry ReportDocument72 pagesSteatorrhea Medical Biochemistry ReportDey Sibal80% (5)
- Steatorrhea Medical Biochemistry ReportDocument72 pagesSteatorrhea Medical Biochemistry ReportDey Sibal80% (5)
- OTR NBCOT ReviewDocument167 pagesOTR NBCOT ReviewDen Ise100% (1)
- 10 Topnotch Obstetrics Gynecology SuperExam1 PDFDocument84 pages10 Topnotch Obstetrics Gynecology SuperExam1 PDFvardhan100% (3)
- Annex 1a - School Forms Checking ReportDocument2 pagesAnnex 1a - School Forms Checking ReportQuinric Bontilao Sevillejo94% (69)
- Modified Snellen Eye Chart 6mDocument4 pagesModified Snellen Eye Chart 6mcheongiNo ratings yet
- Homonymous Visual Field Defects PDFDocument186 pagesHomonymous Visual Field Defects PDFNooramad Abbas AhmadNo ratings yet
- NeuroDocument17 pagesNeuroJack Ortega PuruggananNo ratings yet
- ProP Ophthalmic Examination Made EasyDocument5 pagesProP Ophthalmic Examination Made EasyRosario AyalaNo ratings yet
- Health Assessment - Midterm - Assessing The EyesDocument4 pagesHealth Assessment - Midterm - Assessing The Eyesaina marie templonuevoNo ratings yet
- Assessment of Neurological SystemDocument26 pagesAssessment of Neurological SystemBatiao Camille Claire100% (1)
- OPHTHA 8.0 Neuro Ophthalmology Fundamentals Dr. AtienzaDocument14 pagesOPHTHA 8.0 Neuro Ophthalmology Fundamentals Dr. AtienzaMaria Gracia YamsonNo ratings yet
- Neuro Ophtha Aillen Abines, MD: History and Physical ExaminationDocument2 pagesNeuro Ophtha Aillen Abines, MD: History and Physical ExaminationPrincess Cate MercadoNo ratings yet
- Presbyopia: What Is Presbyopia? What Is Refraction?Document2 pagesPresbyopia: What Is Presbyopia? What Is Refraction?UlfNo ratings yet
- Eyes Lecture 2Document4 pagesEyes Lecture 2Rue Cheng MaNo ratings yet
- TIGAS BACA nrSENSORYDocument44 pagesTIGAS BACA nrSENSORYNiluh Putu NurindahNo ratings yet
- Ophthalmology How To Examine An Eye: Visual AcuityDocument2 pagesOphthalmology How To Examine An Eye: Visual AcuityOlalekan OgundareNo ratings yet
- Essential Guide to Strabismus ExamDocument40 pagesEssential Guide to Strabismus ExamIkmal ShahromNo ratings yet
- Oph SBR Case-QuizDocument4 pagesOph SBR Case-QuizRix tanNo ratings yet
- C 5Document9 pagesC 5Joy LayNo ratings yet
- Ca 3 4Document5 pagesCa 3 4Angel LuayonNo ratings yet
- Pupillary Pathway and Lesions GuideDocument3 pagesPupillary Pathway and Lesions GuidemiaNo ratings yet
- Type and Cause Refractive ErrorDocument7 pagesType and Cause Refractive ErrorShi YingNo ratings yet
- Neuro-ophthalmology Basics and Common FindingsDocument6 pagesNeuro-ophthalmology Basics and Common FindingsMiguel C. DolotNo ratings yet
- Nystagmus 1Document35 pagesNystagmus 1syed mohammed hussain100% (1)
- NB (047) Vision - Central Visual Pathways 1 Lecture1 DR RadwaelzanatyDocument21 pagesNB (047) Vision - Central Visual Pathways 1 Lecture1 DR RadwaelzanatyZeyad AmrNo ratings yet
- Large Pupil Small Pupil Cranial Nerve V - Trigeminal Nerve MotorDocument3 pagesLarge Pupil Small Pupil Cranial Nerve V - Trigeminal Nerve MotorKhristine Andrea RabagoNo ratings yet
- RAPD TestDocument3 pagesRAPD TestSugumar YathavanNo ratings yet
- How To Test For A Relative Afferent Pupillary Defect (RAPD) : StepsDocument2 pagesHow To Test For A Relative Afferent Pupillary Defect (RAPD) : StepsTony NgNo ratings yet
- Vision Rehabilitation Prelims LectureDocument6 pagesVision Rehabilitation Prelims LectureJxce MLeKidNo ratings yet
- Reviewer G10 Todamax - 1Document11 pagesReviewer G10 Todamax - 1Aiza Casinillo CabatinganNo ratings yet
- L9 PediaDocument47 pagesL9 PediaNawaf AleanziNo ratings yet
- NCM 116 Ee Module 4Document18 pagesNCM 116 Ee Module 4Meryville JacildoNo ratings yet
- MEDSURG II (2nd Sem - ENDTERM NOTES)Document39 pagesMEDSURG II (2nd Sem - ENDTERM NOTES)Meryville JacildoNo ratings yet
- BSN3 - MEDSURG2 RLE - Neuro Assessment & Seizure PrecautionDocument6 pagesBSN3 - MEDSURG2 RLE - Neuro Assessment & Seizure PrecautionADRIANNA NICOLE BAHALA GONZALEZNo ratings yet
- 7) Adherent LeucomaDocument6 pages7) Adherent LeucomaDasNo ratings yet
- Cranial Nerve ExaminationDocument3 pagesCranial Nerve ExaminationtomodachiNo ratings yet
- Vision Problems: Doing & ThinkingDocument43 pagesVision Problems: Doing & ThinkingHa nasserNo ratings yet
- Tamara Bystrak Pharmd CandidateDocument39 pagesTamara Bystrak Pharmd CandidatehurensohnNo ratings yet
- SodaPDF Converted Precept 2Document6 pagesSodaPDF Converted Precept 2VINSMOKE RIKUNo ratings yet
- The Eye VisionDocument7 pagesThe Eye VisionJean ReyesNo ratings yet
- S S I I P: Response Score SignificanceDocument1 pageS S I I P: Response Score Significanceyaneidys perezNo ratings yet
- Language, Orientation, Memory, Attention Span and Calculation, LOCDocument7 pagesLanguage, Orientation, Memory, Attention Span and Calculation, LOCYessamin Paith RoderosNo ratings yet
- NYSTAGMUSDocument13 pagesNYSTAGMUSwillemlrouxNo ratings yet
- PupilgameDocument55 pagesPupilgameBataa BattulgaNo ratings yet
- See, Sense and Correct: Exploring the Amazing SensesDocument14 pagesSee, Sense and Correct: Exploring the Amazing SensesaWDwaDNo ratings yet
- Perceptual DisturbancesDocument7 pagesPerceptual DisturbancesVin SageNo ratings yet
- (OPT) 1.01 Eye Symptoms and Eye Examination Aclan v2Document14 pages(OPT) 1.01 Eye Symptoms and Eye Examination Aclan v2gprint1122No ratings yet
- The Three Layers of the Eye and Photoreceptor CellsDocument2 pagesThe Three Layers of the Eye and Photoreceptor CellsMarissa AsimNo ratings yet
- Neurological Examination: ObserveDocument9 pagesNeurological Examination: ObserveTom MallinsonNo ratings yet
- Ocular ExaminationDocument2 pagesOcular ExaminationMuhammad HaziqNo ratings yet
- Cranial Nerve: I Olfactory (S) Smell Anosmia - InabilityDocument4 pagesCranial Nerve: I Olfactory (S) Smell Anosmia - InabilityLeamy ReyesNo ratings yet
- NCLEX SimpleNursing PediatricsDocument120 pagesNCLEX SimpleNursing PediatricsOlrac Agairdam100% (4)
- The Eyes and Visual SystemDocument2 pagesThe Eyes and Visual SystemMichael Varela GuglielmelliNo ratings yet
- Pupillary Reflexes: Rohith. A Roll No-66Document34 pagesPupillary Reflexes: Rohith. A Roll No-66KarthikeyanNo ratings yet
- CN Name Type Function Testing Lesions/ResultsDocument5 pagesCN Name Type Function Testing Lesions/ResultsBen SarNo ratings yet
- Visual Acuity Examination For MNUMS 5th Course StudentsDocument14 pagesVisual Acuity Examination For MNUMS 5th Course Studentsbyambadorj.mbNo ratings yet
- Cranial Nerve Functions and Lesion SymptomsDocument4 pagesCranial Nerve Functions and Lesion SymptomsBloom DhillonNo ratings yet
- Angle Closure GlaucomaDocument21 pagesAngle Closure Glaucomasri sinagaNo ratings yet
- The Acute Painful Red Eye: History of Presenting Complaint - The Time and Speed of OnsetDocument4 pagesThe Acute Painful Red Eye: History of Presenting Complaint - The Time and Speed of Onsetleigh_zaliNo ratings yet
- From Light To Features: Dr. Sjoerd StuitDocument65 pagesFrom Light To Features: Dr. Sjoerd StuitsethNo ratings yet
- EYE ASSESSMENT TransDocument10 pagesEYE ASSESSMENT TransJennie KimNo ratings yet
- Oral Revalida Review2019: Concise Guide to Ophthalmology ExamDocument10 pagesOral Revalida Review2019: Concise Guide to Ophthalmology ExamanonymousNo ratings yet
- SquintDocument7 pagesSquintMohamed GhanemNo ratings yet
- KEJANG PADA ANAK SEMINAR IDAI (Autosaved)Document43 pagesKEJANG PADA ANAK SEMINAR IDAI (Autosaved)Olan Adjalah KeknyaNo ratings yet
- OSCE Somatosensory and Autonomics Examination PDFDocument11 pagesOSCE Somatosensory and Autonomics Examination PDFriczen vilaNo ratings yet
- Optha Anatomy DR - RamosDocument12 pagesOptha Anatomy DR - RamosDey SibalNo ratings yet
- OPHTHA - Low Vision Rehabilitation (Dr. Jimenez)Document12 pagesOPHTHA - Low Vision Rehabilitation (Dr. Jimenez)Dey SibalNo ratings yet
- Spine & Extremities / Abdomen / Neurologic Exam: PalpationDocument8 pagesSpine & Extremities / Abdomen / Neurologic Exam: PalpationBrent DizonNo ratings yet
- OPHTHA 004 - Corneal and External DiseasesDocument7 pagesOPHTHA 004 - Corneal and External DiseasesDey SibalNo ratings yet
- Juris Midterms 2021Document94 pagesJuris Midterms 2021Dey SibalNo ratings yet
- PRISMA 2020 ExamplesDocument75 pagesPRISMA 2020 ExamplesDey SibalNo ratings yet
- Basic Surgical Skill PDFDocument89 pagesBasic Surgical Skill PDFEvan AninditoNo ratings yet
- Optha Samplex and Recalls All inDocument51 pagesOptha Samplex and Recalls All inDey SibalNo ratings yet
- Clinical Medicine CVS Tabulated 2019Document5 pagesClinical Medicine CVS Tabulated 2019Justin TayabanNo ratings yet
- Legal Med T Techniques of Identification Part 2Document4 pagesLegal Med T Techniques of Identification Part 2Dey SibalNo ratings yet
- Techniques of Identification (Part 1) : (Online Class, 2020)Document3 pagesTechniques of Identification (Part 1) : (Online Class, 2020)Dey SibalNo ratings yet
- Low Vision RehabilitationDocument48 pagesLow Vision RehabilitationJuswadji SudionoNo ratings yet
- Medical Ethics & the LawDocument28 pagesMedical Ethics & the LawDey SibalNo ratings yet
- Acute AbdomenDocument1 pageAcute AbdomenDey SibalNo ratings yet
- LEGMED - Physical Injuries 1-4Document10 pagesLEGMED - Physical Injuries 1-4Dey SibalNo ratings yet
- TR Housekeeping NC IVDocument95 pagesTR Housekeeping NC IVDey SibalNo ratings yet
- Low Vision RehabilitationDocument48 pagesLow Vision RehabilitationJuswadji SudionoNo ratings yet
- Ilovepdf MergedDocument296 pagesIlovepdf MergedDey SibalNo ratings yet
- Anatomy of The EYEDocument17 pagesAnatomy of The EYEDey SibalNo ratings yet
- MANILA - FEES - 1STSem - SY2020 - 1STYRDocument5 pagesMANILA - FEES - 1STSem - SY2020 - 1STYRDey SibalNo ratings yet
- Apply for Professional ID CardDocument1 pageApply for Professional ID CardVeraNataaNo ratings yet
- Health System in Action PDFDocument422 pagesHealth System in Action PDFDey SibalNo ratings yet
- After 2017Document2 pagesAfter 2017NonoyTaclino100% (1)
- 587 MetCon For Group M Felzmann PDFDocument4 pages587 MetCon For Group M Felzmann PDFDey SibalNo ratings yet
- Visual Illusions ExplainedDocument16 pagesVisual Illusions Explainedmagnetto123100% (1)
- Status Ujian Mata DR GilbertDocument6 pagesStatus Ujian Mata DR Gilbertanggitas2594No ratings yet
- Pupillary Pathway, Pupillary Abnormalities, RAPDDocument24 pagesPupillary Pathway, Pupillary Abnormalities, RAPD015Afeefa N ANo ratings yet
- Tonometry Dan PacymetriDocument9 pagesTonometry Dan PacymetriGusti Zidni FahmiNo ratings yet
- Color blindness affects millionsDocument3 pagesColor blindness affects millionsUugaa SoNo ratings yet
- Visual FieldsDocument86 pagesVisual FieldsoptorameshgpNo ratings yet
- Retina QuizDocument3 pagesRetina QuizGoldiee MishraNo ratings yet
- Eye Brain and Vision PDFDocument2 pagesEye Brain and Vision PDFBrett0% (1)
- Wikipedia - HemeralopiaDocument2 pagesWikipedia - HemeralopiaPablo G. BledtNo ratings yet
- Vision in Insects: Compound Eyes and Mosaic VisionDocument3 pagesVision in Insects: Compound Eyes and Mosaic VisionShubham BhartariNo ratings yet
- BioDocument21 pagesBioShweta katiyarNo ratings yet
- Metrado de Madera EdificioDocument128 pagesMetrado de Madera EdificioAlberto Falconi TapiaNo ratings yet
- Mystery of ConsciousnessDocument242 pagesMystery of ConsciousnessVered Amir100% (4)
- VBA-21-0960N-2-ARE EyesDocument10 pagesVBA-21-0960N-2-ARE EyesCombat CraigNo ratings yet
- Cataract Not FixedDocument41 pagesCataract Not FixedDeasy MirayashiNo ratings yet
- High MyopiaDocument37 pagesHigh Myopiastroma januariNo ratings yet
- Top Ophthalmology Journals Q1 & Q2Document4 pagesTop Ophthalmology Journals Q1 & Q2Peony PinkNo ratings yet
- Pupil AssessmentDocument2 pagesPupil AssessmentJiezl Abellano AfinidadNo ratings yet
- Wa0002Document3 pagesWa0002Abhinav KumarNo ratings yet
- School Nursing Abnormal Findings ReportDocument4 pagesSchool Nursing Abnormal Findings ReportBianca MaeNo ratings yet
- ECK The Little Guide To Strabismus and AmblyopiaDocument37 pagesECK The Little Guide To Strabismus and AmblyopiaAndreea MaciucNo ratings yet
- FisicaDocument3 pagesFisicaValentina CerdaNo ratings yet
- Signs and Symptom For UveitisDocument4 pagesSigns and Symptom For UveitisVan KochkarianNo ratings yet
- NCM 116 Ee Module 4Document18 pagesNCM 116 Ee Module 4Meryville JacildoNo ratings yet
- Why Red Doesn't Sound Like A Bell - Understanding The Feel of Consciousness (PDFDrive)Document287 pagesWhy Red Doesn't Sound Like A Bell - Understanding The Feel of Consciousness (PDFDrive)Roger13No ratings yet
- Orthoptic Eval and Treatment in Orbital FracturesDocument10 pagesOrthoptic Eval and Treatment in Orbital Fractureslaljadeff12No ratings yet
- Visual Functional Neuroanatomy Map: © 2000, Dennis P. Swiercinsky, PH.DDocument1 pageVisual Functional Neuroanatomy Map: © 2000, Dennis P. Swiercinsky, PH.DCristi BorceaNo ratings yet
- Anatomy of Eye: Dr. Y. Lokesh KumarDocument37 pagesAnatomy of Eye: Dr. Y. Lokesh KumarLokesh KumarNo ratings yet