Professional Documents
Culture Documents
Handout # 10 Part 4
Handout # 10 Part 4
Uploaded by
Ram AugustCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Handout # 10 Part 4
Handout # 10 Part 4
Uploaded by
Ram AugustCopyright:
Available Formats
1
Handout #10 2. Ambulation has also been found to decrease the
need for analgesia, decrease incidence of FHT
(Part 4) abnormalities and to promote comfort
LABOR AND DELIVERY Enema
• 1. Enema is a procedure of emptying the colon
of fecal matter to:
• Stimulate uterine contractions
Uterine Phases of Parturition (childbirth)
• Prevent infection- expulsion of feces during the
second stage predispose mother and infant
Phase 0
infection
• This extends from the time before implantation
• Facilitate descent of fetus
until late in pregnancy when the uterus is
2. Enema is not a routine procedure in the preparation
relaxed & the cervix is firm & rigid.
of woman in labor. Commonly used enemas are tap
Phase 1
water enema, fleet enema and prepacked disposable
• This is the time when the uterus & cervix
type enema. Soap suds enema is not recommended
undergo several changes in preparation for
because they have been associated with several
labor.
complications. Suppositories are also used.
Phase 2
3. Contraindications to enema:
• This is the time of active labor when the
• Not given during active phase and ruptured
contents of the uterus are expelled.
BOW
• It is divided into 3 stages:
• Vaginal bleeding
• a.) cervical stage
• Abnormal fetal presentation and position
• b.) expulsive stage
• Fetus not yet engaged
• c.) placental stage
• Premature labor because of the danger of cord
Phase 3
prolapsed
• This is the time when the newly delivered
• Abnormal fetal heart rate pattern
mother recovers from the effects of pregnancy
& childbirth.
Transfer to Delivery Room
• 1. Primiparas are transferred to the delivery
room when the cervix is fully dilated and
CARE OF PARTURIENT IN THE FIRST STAGE
perineum is bulging.
• 2. Multiparas are moved to DR when cervix is
Care of the Bladder
8cm dilated
1. A woman in labor should be encouraged to void
frequently, at least every 2 hours to prevent bladder
distention because a full bladder:
CARE OF PARTURIENT IN THE SECOND STAGE
Delay fetal descent
Increases discomfort of labor
• The second stage of labor begins as soon as the
Predispose to urinary tract infection
cervix is fully dilated and is completed with the
Can be traumatized during labor
birth of the baby.
2. A distended bladder can be palpated above the
• Never leave the patient alone once she is
symphysis pubis as it bulges or protrudes.
transferred to the delivery room.
• Never turn your back on the perineum because
Foods & Fluids
the baby could push through the vaginal
1. Early in labor, clear fluids may be allowed. If not, the
opening while your back is turned.
woman may be given ice chips to prevent drying of the
mouth and for comfort.
• During active labor, foods and oral fluid should
PREPARE DELIVERY EQUIPMENTS
be withheld because gastric emptying is
• Place the instrument table near the delivery
prolonged. Foods taken stays in the stomach
table and uncover it.
longer which the woman may vomit and
• Prepare instruments to be needed by the
aspirate especially if she has been given
newborn. Turn on radiant warmer and place
anesthetics and analgesics.
receiving blanket under it to warm.
Ambulation
• Ready resuscitation equipment.
1. Encourage woman to ambulate during the latent
• Prepare also forms and charts that must be
phase of labor to shorten first stage if membranes are
filled up in delivery room.
still intact. When the woman stands or squats, the
diameter of the inlet is increased making the passage of
the fetus through the birth canal faster and easier.
2
DELIVERY POSITION
1. Lithotomy position - Procedure: PREVENTING INFECTION
– Cover legs of woman with sterile cotton • Persons with infection or have been exposed to
leggings and raise them up to the infections or communicable disease are not
stirrups at the same time. allowed to enter the DR.
– Adjust the stirrups so that the legs are • No one should be permitted in the DR without a
not widely separated and so that both sub suit, mask covering mouth and nose and
legs are of the same height. cap that completely covers hair. Anything that
– Elevate the head portion of the table to touches the patient’s perineum should be
enable the woman to push effectively. sterile.
• Indication: This position is used when surgical • Ideally, nurses and midwives attending delivery
procedures, such as forceps and episiotomy are must wear eye shields, gowns and gloves to
to be performed. protect themselves from accidental splashing of
• Advantage: This position gives easy access to blood and body fluids.
the perineum providing the birth attendant with • During labor, the nurse-midwife should perform
good control of the delivery of the baby. handwashing before and after patient care,
• Disadvantages: when providing care between patients and
– Supine hypotensive syndrome whenever there is contact with blood and body
– Positioning injuries: Clot formation due fluids.
to compression, muscle strain when • In addition, the nurse-midwife should also wear
legs are improperly placed on stirrups. gloves at all times that there is possibility of
touching body fluids and when performing any
2.Dorsal Recumbent procedure at or near the perineum.
• Procedure: • When handling perineal pads, they should be
– The head of the bed is 35 to 45 degrees handled from ends using gloved hands and not
elevated, knees are flexed and feet flat in the middle area.
on bed. This position facilitates the
pushing effort of the mother.
• Indication: Home delivery ASSISTING MOTHER IN THE DELIVERY ROOM
• Advantage: This position gives easy access to 1. Coach mother to push effectively, instruct her:
the perineum providing the birth attendant with – To avoid the Valsalva maneuver, this
good control of the delivery of the baby. involves holding breath and tightening
• Disadvantages: Supine hypotensive syndrome the abdominal muscles while pushing.
and may be uncomfortable. Valsalva maneuver decreases blood
returning to the heart, increases venous
3. Side-lying position pressure and increases intrathoracic
• Procedure: The woman is placed on her side pressure which consequently,
• Indication: Heart disease diminishes blood supply to placenta and
• Advantage: This position increase comfort to fetus.
the mother and avoids supine hypotension There are two methods of pushing:
syndrome. • Urge to push method when the
• Disadvantages: woman pushes only when the
– Less control of delivery and decreased urge to push is felt and relaxes
access to the perineum. completely after a contraction
– Danger of woman losing balance during to replenish her energy.
delivery. • Open-glottis pushing when the
woman pushes during uterine
contraction with open glottis so
air is released as she pushes.
• The woman may use any
method but she should never
be left alone when doing
pushing.
– To grasp below the knees or other hard
objects as she bears down.
3
– To push 3 to 5 times with each
contraction but push no longer than 5
to 6 seconds.
11. Place the infant over the mother’s abdomen to help
2. To avoid exhaustion, instruct the woman to pant contract the uterus.
(rapid shallow breathing) during some contraction. If • Clamping the cord:
woman complains of lightheadedness and tingling – Usually, the cord is clamped after
sensations on fingers (this is respiratory alkalosis) let pulsation has stopped to allow
her breathe through a paper bag or cupped hand. transfusion of about 50 mL of extra
blood from placenta to infant. This
3. The woman may complain of leg cramps. This is due practice provides additional iron and
to the pressure exerted by the fetal head against the helps prevent iron deficiency anemia.
pelvic nerves. Provide relief by dorsiflexing the affected – Clamp the cord twice and cut in
foot and straightening the leg until the cramps between, about 8 to 10 inches from the
disappear. umbilicus.
4. As the presenting part moves towards the outlet, – After cutting the cord, count blood
perform ironing on vaginal orifice to stretch and vessels, there should be two arteries
prepare soft tissues. and one vein. The vein is larger than the
two arteries.
5. When the head is crowning (largest diameter of the – Later in the nursery, the cord is cut
head encircles the vulvar ring): again and umbilical cord clamp
– Instruct mother to pant and not to push (Hollister, Double Grip Umbilical Clamp)
to prevent rapid expulsion of the baby is applied about 2 to 3 cm from the
and to avoid lacerations. Rapid abdomen.
expulsion will result in sudden change – Wrap the infant in sterile diaper, show
of intracranial pressure which can cause to mother or let her hold the baby
cerebral hemorrhage in infant. (depending on institution’s policy). Be
– Episiotomy if necessary is performed at sure to establish eye contact between
this time by the doctor to prevent mother and baby to promote bonding
lacerations. before bringing newborn to nursery.
12. Information to include in the notes are:
6. Perform Ritgen’s maneuver while delivering the head. – Exact date and time of delivery.
Place a sterile towel over the rectum and apply forward – Sex of the infant.
pressure on the chin while the other hand presses – Condition of the infant (APGAR) after
downward the occiput. Ritgen’s maneuver will: birth.
– Facilitates extension of the head – Position of the infant at delivery.
– Slows down deliver of the head – Type of episiotomy, lacerations.
– Let the smallest diameter of the head to – Spontaneous or forceps delivery.
be born. – Use of oxygen and suction on the
infant.
7. Deliver the head slowly in between contractions. – Number of vessels in the cord.
Immediately after the delivery of the head: – Any or other pertinent facts about the
– Wipe the nose and mouth of secretions, delivery.
suction with bulb syringe to establish
patent airway. METHODS OF PLACENTAL SEPARATION
– Insert fingers into vagina and feel for • Schultz Mechanism – Separation of the
cord looped around the neck (nucchal placenta starts from the center. The shiny
cord). If present, slip cord down the smooth fetal side is delivered first in this type of
shoulder or over the baby’s head. If separation. About 80% of placental separation
tight, clamp twice and cut in between. occurs by Shultz Mecahnism.
• Duncan Mechanism – Separation begins from
8. Holding the sides of the head with two hands, apply a the edges of placenta. The maternal side is
slight downward push to deliver the anterior shoulder, delivered first. About 20% of separation occurs
and then elevate the head to deliver the posterior by Duncan Mechanism.
shoulder. The rest of the body follows without difficulty
after the delivery of the shoulder.
9. Take note of the exact time of baby’s birth. A child is
considered born when the whole body is delivered.
10. Immediately after birth of baby, place newborn in
dependent position to facilitate drainage of secretions.
4
MATERNAL ASSESMENT much more dilute solution by continuous
1. Monitor vital signs every 15 minutes. intravenous infusion. Oxytocin should not be
2. Monitor time interval between birth of the baby and given intravenously as a large bolus because it
the placenta. causes titanic uterine contractions and
• Normally, the placenta is delivered within 5 to hypotension. Its major adverse effect is
20 minutes after baby’s birth. antidiuresis or fluid retention.
• If a longer period of time elapsed before the
placenta is delivered, the mother is at risk of
losing greater than normal amount of blood in Care when administering oxytocin:
the third stage. • Never leave client unattended.
3. Watchful waiting: If the uterus remains contracted • Have oxygen and emergency equipment
and there is no severe bleeding, watchful waiting is available.
employed until the placenta is delivered. • Use infusion control device for IV
– Do not hurry placental delivery. No administration.
fundal push, no uterine massage and no • Discontinue if abnormal UC occur.
pulling of the cord. These actions can • Assess BP and pulse every 15 minutes.
result in uterine inversion. • Monitor FHR.
– Rest one hand over the fundus to make
sure the uterus remains firm and does
not fill with blood. Record the following information in the notes:
– Wait for signs of placental separation: – Time the placenta is delivered.
• Calkin’s sign is usually the first – How delivered (spontaneously or
sign of placental separation. manually removed by the physician).
The uterus becomes firm and – Type, amount time and route of
globular rising to the level of administration of oxytocin. Oxytocin is
umbilicus. never administered prior to delivery of
• Sudden gush of blood from the the placenta because the strong uterine
vagina. contractions could harm the fetus.
• Lengthening of the cod as the – If the placenta is delivered complete
placenta separates from the and intact or in fragments.
uterus.
• Appearance of the placenta at
the vaginal opening.
• Inspect for completeness of cotyledons right CARE OF PARTURIENT IN THE FOURTH STAGE
after placental delivery. Retained placental
fragments can cause severe hemorrhage by • The main danger during the fourth stage is
preventing the uterus to contract. hemorrhage. Therefore the goal of care during
4. Massage the uterus to keep it contracted. this period is to prevent bleeding from uterine
5. Oxytoxic agents are drugs that stimulate the uterus to atony and birth canal lacerations sustained
contact. It is given to: during labor.
– Initiate labor – Given slowly and in small REPAIR OF LACERATIONS
doses until desired UC are achieved. • 1. Right after the birth of placenta, the
– Used to augment weak UC that has perineum is inspected carefully for lacerations
already begun. and necessary repairs are made. During
– Used to control postpartum atony – episioraphy (repair of episiotomy and
May be given rapidly as a bolus to lacerations) a local anesthesia is injected to the
immediately control bleeding. area to be repaired.
• When the uterus feels firm but there is
continuous oozing of bright red blood, suspect
lacerations.
• To stop the bleeding, these lacerations must be
repaired.
• If lacerations are discovered after the patient is
transferred to the recovery room or her private
room, return woman immediately to the
delivery room for repair.
• Oxytocin (Pitocin, Syntocinon) 10 units: It is 2.Classifications of perineal lacerations:
ideally given IM in a dose of 10 USP units or as a
5
• First degree: Involves the fourchette, vaginal 1. Check fundus for consistency every 15 minutes
mucous membrane, perineal skin during the first hour or until it no longer tends to relax.
• Second degree: Involving fourchette vaginal The first action to take when a baggy or relaxed uterus
mucous membrane, perineal skin, muscles of is noted is to massage the fundus gently to stimulate
perineal body uterine contraction. If the fundus does not respond to
• Third degree: Involves fourchette, vaginal massage and bleeding continues, report to physician
mucous membrane, perineal skin, muscles of right away.
perineal body and anal sphincter 2. Massage the fundus every 15 minutes during
• Fourth degree: Involves fourchette, vaginal the first hour, every 30 minutes during the next hour,
mucous membrane, perineal skin, muscles of and then, every hour.
perineal body, anal sphincter and mucous
membrane of rectum 3. Locate fundal height. Immediately after
placental delivery, it is located between the umbilicus
and the symphysis. It gradually rises to the level of the
umbilicus afterwards. It should be located at midline
and firm. If the fundus deviates from the middle, check
for fullness of the bladder which is usually the cause.
4. Assess the bladder when assessing the fundus.
Bladder distention displaces the uterus and prevents
proper uterine contraction. This can cause bleeding.
ASSESSMENT OF LOCHIA FLOW
1. Record the number of pads soaked with lochia
during recovery.
2. Assess color, amount, smell, presence of clots.
3. Observe for constant trickle of bright red lochia.
If fundus is firm, this may be caused by lacerations.
4. Observe lochia flow when the fundus is
massaged.
3. Midwifery care: PROVIDING COMFORT AND PAIN RELIEF
• Perineal care: Clean the perineum with an • During the immediate postpartum period, the
antiseptic solution and apply a sterile sanitary woman may experience pain and discomfort for
pad on the perineum. An ice pack may be several causes which include cramping from
applied to the perineum to reduce swelling uterine contractions and perineal pain from
from episiotomy especially if a fourth degree episiotomy and delivery trauma.
tear has occurred. • Relief can be provided by providing pain
• Lowe legs from the stirrups at the same time medications and applying ice compress over the
and remove soiled drapes and linens. Change perineum.
mother into clean gown.
• Provide extra blanket to keep patient warm. TRANSFER TO RECOVERY OR PRIVATE ROOM
Chilling, called postpartum tremors, is common If the patient is transferred to the delivery or private
at this period and is due to the circulatory room, ensure that emergency equipment is available for
changes that occurred after delivery. possible complications.
VITAL SIGNS 1. Suction and oxygen in case patient becomes
• 1. Monitor vital sign every 15 minutes for eclamptic.
an hour then every 30 minutes for the next 2. Pitocin® is available in the event of hemorrhage.
hour. Then every hour until transferred to the 3. IV remains patent for possible use if
RR or private room. complications develop.
• 2. If the patient in stable, take them every 4. Oxygen.
2-4 hours in the succeeding hours after transfer.
If not, continue monitoring frequently. ------ End-----
• 3. The temperature may be slightly
increased during the immediate postpartum
period because of mild dehydration.
ASSESMENT OF THE FUNDUS
You might also like
- Nursing NotesDocument16 pagesNursing NotesChelzie LasernaNo ratings yet
- Complications of PregnancyDocument24 pagesComplications of PregnancyDeo Olarte100% (1)
- Abnormal Uterine ActionDocument27 pagesAbnormal Uterine Actiontanmai noolu100% (1)
- Management Normal Labor 2021 SBOGDocument118 pagesManagement Normal Labor 2021 SBOGAHMED .KNo ratings yet
- Stages of LaborDocument3 pagesStages of Labormiss RN100% (8)
- Incomplete Abortion Case StudyDocument40 pagesIncomplete Abortion Case StudyLani Michelle BelloNo ratings yet
- Activity Mark My Calendar PDFDocument2 pagesActivity Mark My Calendar PDFRey Porciuncula100% (2)
- AAP January 2024 Complete Issue NeoReviewsDocument71 pagesAAP January 2024 Complete Issue NeoReviewshabibfmNo ratings yet
- Normal Labour VIDEO + Module Final (5th June 2020)Document99 pagesNormal Labour VIDEO + Module Final (5th June 2020)Adam Chung100% (1)
- Biological ScienceDocument12 pagesBiological ScienceGrace Marie Rublica Cain100% (1)
- (Maternal) FINALSDocument86 pages(Maternal) FINALSRM DemetilloNo ratings yet
- Ncma217 Rle Day 2 - EincDocument5 pagesNcma217 Rle Day 2 - EincAbegail BalloranNo ratings yet
- EDD & AOG Computation: Expected Date of Delivery & Age of GestationDocument3 pagesEDD & AOG Computation: Expected Date of Delivery & Age of GestationRam AugustNo ratings yet
- Leopold's Maneuver and 7 Cardinal MovementsDocument5 pagesLeopold's Maneuver and 7 Cardinal MovementsMikaela Gabrielle GERALINo ratings yet
- Intrautrian Growth RetarDocument11 pagesIntrautrian Growth RetarJyoti Prem Uttam100% (3)
- Presentation Minor Discomfort .Document20 pagesPresentation Minor Discomfort .Leena BaderNo ratings yet
- Module 4 - Maternal TransespdfDocument16 pagesModule 4 - Maternal TransespdfCarl UyNo ratings yet
- 1 Stage: Dilatation/Cervical: Cesarean BirthDocument5 pages1 Stage: Dilatation/Cervical: Cesarean BirthKenji ToleroNo ratings yet
- Unit 5 Newborn ConceptsDocument5 pagesUnit 5 Newborn ConceptsEunice TrinidadNo ratings yet
- Ob-Hw 1Document8 pagesOb-Hw 1Carolina TabareNo ratings yet
- Health Promotion During Pregnancy 1Document2 pagesHealth Promotion During Pregnancy 1Christian Jay AlbarracinNo ratings yet
- Stages of LaborDocument6 pagesStages of LaborShaii Whomewhat GuyguyonNo ratings yet
- Complications of Intrapartum and Post PartumDocument8 pagesComplications of Intrapartum and Post PartumMikasa AckermanNo ratings yet
- HIGH RISK AND SICK MOTHER 5PsDocument16 pagesHIGH RISK AND SICK MOTHER 5Psbaracream.exeNo ratings yet
- Chapter 3 Theories of Labor Onset and Signs of LaborDocument1 pageChapter 3 Theories of Labor Onset and Signs of LaborChristian Jay AlbarracinNo ratings yet
- CMCALEC Lesson9MDocument14 pagesCMCALEC Lesson9Mluisgregory113No ratings yet
- NCM 107 Module 4FDocument25 pagesNCM 107 Module 4FNotur BarbielatNo ratings yet
- L1 - L5 CmcaDocument18 pagesL1 - L5 CmcaRose Anne AbivaNo ratings yet
- Puerperium and ManagementDocument38 pagesPuerperium and ManagementWadhha AlsenaidiNo ratings yet
- Shoulder Dystocia NCPDocument6 pagesShoulder Dystocia NCPNicole Genevie MallariNo ratings yet
- Semis - MCN RLEDocument12 pagesSemis - MCN RLEKorean GirlNo ratings yet
- Gestational Conditions-1Document8 pagesGestational Conditions-1jimwelluismNo ratings yet
- Assesment and Monitoring During 2nd Stage of LabourDocument11 pagesAssesment and Monitoring During 2nd Stage of LabourPragati BholeNo ratings yet
- Prenatal Period 1st PartDocument18 pagesPrenatal Period 1st PartCrystal MaidenNo ratings yet
- Preterm Labor: Group 6Document13 pagesPreterm Labor: Group 6Evelyn MedinaNo ratings yet
- Chapter V D. Stages of LaborDocument3 pagesChapter V D. Stages of LaborStefanie TerminezNo ratings yet
- NFDN 2004 - Unit 4.3 - JLB StudentDocument43 pagesNFDN 2004 - Unit 4.3 - JLB StudentkendrabooboooNo ratings yet
- Hydramnios or PolyhydramniosDocument4 pagesHydramnios or PolyhydramniosAngel MoncadaNo ratings yet
- CHN Lec - Nursing Care of A Family During Labor & BirthDocument9 pagesCHN Lec - Nursing Care of A Family During Labor & BirthMark VincentNo ratings yet
- Complication During Labor and BirthDocument4 pagesComplication During Labor and BirthlizafyelcsNo ratings yet
- Intrapartum 111: 1. Examine The Woman For Emergency SignsDocument7 pagesIntrapartum 111: 1. Examine The Woman For Emergency SignsJane MartinNo ratings yet
- DystociaDocument46 pagesDystociacoco brillqnteNo ratings yet
- Birth TermsDocument36 pagesBirth Termskamaljit kaurNo ratings yet
- Reviewer in NCMDocument12 pagesReviewer in NCMtamsmadjad18No ratings yet
- Complications With The PowerDocument4 pagesComplications With The PowerAllyssa Leila Estrebillo OrbeNo ratings yet
- NCM 107 Module 4FDocument25 pagesNCM 107 Module 4F1B - Zafra, RamoneNo ratings yet
- Second Stage of LaborDocument25 pagesSecond Stage of LaborAna67% (6)
- Operative Obstetrics: DR - Hanan Mohamed Abdelaziz Ass. Prof Obgyn AuwDocument23 pagesOperative Obstetrics: DR - Hanan Mohamed Abdelaziz Ass. Prof Obgyn AuwÃsmäå MøhãmmëdNo ratings yet
- Lecture 5 - Obsteric Emergencies-1Document103 pagesLecture 5 - Obsteric Emergencies-1Priscilla Sarah PayneNo ratings yet
- Amniotic Sac: - The Bag of Membranes Containing The Fetus and The Amniotic Fluid. Its Functions Is To Protect The "Baby"Document35 pagesAmniotic Sac: - The Bag of Membranes Containing The Fetus and The Amniotic Fluid. Its Functions Is To Protect The "Baby"Anjali Rahul AjmeriNo ratings yet
- Breast Feeding and PostDocument4 pagesBreast Feeding and PostMichaela BernadasNo ratings yet
- Maternal and Child NursingDocument22 pagesMaternal and Child NursingCutedenNo ratings yet
- NCM 107maternal FinalsDocument84 pagesNCM 107maternal FinalsFranz goNo ratings yet
- Explain 4Document21 pagesExplain 4CHACHACHACHAAAAANo ratings yet
- INTRAPARTUMDocument174 pagesINTRAPARTUMRUSTOM JAKENo ratings yet
- Conduct of Normal LabourDocument32 pagesConduct of Normal Labourbwire innocentNo ratings yet
- NSD ChecklistDocument3 pagesNSD ChecklistChristine Evan HoNo ratings yet
- DaaanDocument19 pagesDaaanduca.danrainer02No ratings yet
- Handout # 10Document22 pagesHandout # 10Ram August100% (1)
- Normal LaborDocument27 pagesNormal LaborRamil BonifacioNo ratings yet
- Stages of Labor & Leopold's Maneuver First Stage: Dilating StageDocument11 pagesStages of Labor & Leopold's Maneuver First Stage: Dilating StagePanJan BalNo ratings yet
- Labor Delivery1Document95 pagesLabor Delivery1knotstmNo ratings yet
- Face PresentationDocument4 pagesFace PresentationRose Ann HajironNo ratings yet
- CHAPTER 23 Tilles ReviewerDocument10 pagesCHAPTER 23 Tilles Reviewercutiepie creampieNo ratings yet
- Care of Women in All Stages of LaborDocument43 pagesCare of Women in All Stages of LaborSonam SonamNo ratings yet
- Chapter 2 Lesson 3 Part 1Document14 pagesChapter 2 Lesson 3 Part 1baracream.exeNo ratings yet
- Advice To Wives On The Management Of Themselves, During The Periods Of Pregnancy, Labour And SucklingFrom EverandAdvice To Wives On The Management Of Themselves, During The Periods Of Pregnancy, Labour And SucklingNo ratings yet
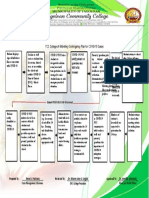
- Competency Performance Checklist: Tagoloan Community CollegeDocument2 pagesCompetency Performance Checklist: Tagoloan Community CollegeRam AugustNo ratings yet
- TCC College of Midwifery Contingency Plan For COVID-19 CasesDocument1 pageTCC College of Midwifery Contingency Plan For COVID-19 CasesRam AugustNo ratings yet
- Communication: (Verbal and Non Verbal)Document52 pagesCommunication: (Verbal and Non Verbal)Ram AugustNo ratings yet
- Handout # 10Document22 pagesHandout # 10Ram August100% (1)
- Republic Act No. 7392 An Act Revising Republic Act No. 2644, As Amended, Otherwise Known As The Philippine Midwifery ActDocument6 pagesRepublic Act No. 7392 An Act Revising Republic Act No. 2644, As Amended, Otherwise Known As The Philippine Midwifery ActRam AugustNo ratings yet
- Handout # 3 Mid 100 - 2020Document3 pagesHandout # 3 Mid 100 - 2020Ram AugustNo ratings yet
- Health Informatics Qualifications and Ehealth Literacy: Week # 9-10 HandoutDocument2 pagesHealth Informatics Qualifications and Ehealth Literacy: Week # 9-10 HandoutRam AugustNo ratings yet
- BPE Introduction To AnatomyDocument7 pagesBPE Introduction To AnatomyRam AugustNo ratings yet
- Note: Refer To The Structures Above and Familiarize The Functions of Each PartsDocument2 pagesNote: Refer To The Structures Above and Familiarize The Functions of Each PartsRam August100% (1)
- Mpharm Year 2 Gastrointes Nal Tract Example MCQ'SDocument8 pagesMpharm Year 2 Gastrointes Nal Tract Example MCQ'SManish JainNo ratings yet
- 1 11Document12 pages1 11filipe.med.vettNo ratings yet
- Medications For FibromyalgiaDocument3 pagesMedications For FibromyalgiaAl ClarkeNo ratings yet
- Nama: Nadia Fitra RahmaDocument2 pagesNama: Nadia Fitra RahmaNadya Fitra RahmaNo ratings yet
- Antenatal Assessment ToolDocument13 pagesAntenatal Assessment ToolBlessy MadhuriNo ratings yet
- Exercise During Pregnancy and The Postpartum PeriodDocument18 pagesExercise During Pregnancy and The Postpartum PeriodSally Davies0% (1)
- Daisy's Route - Summertime Saga WikiDocument1 pageDaisy's Route - Summertime Saga WikiHaruka KobayashiiNo ratings yet
- Scope and Standards of Maternal and Child Practice in The PhilippinesDocument33 pagesScope and Standards of Maternal and Child Practice in The PhilippinesSana ChanNo ratings yet
- Hydatidiform MoleDocument19 pagesHydatidiform MoleAndre Karl FaculinNo ratings yet
- Contemporary Maternal Newborn Nursing 9th Edition Test BankDocument34 pagesContemporary Maternal Newborn Nursing 9th Edition Test BankCharlotte Reddy100% (37)
- Committee Opinion No 712 Intrapartum Management.58Document7 pagesCommittee Opinion No 712 Intrapartum Management.58Arturo Aguilar ZamoraNo ratings yet
- Neonatal Resuscitation: DR Hassan Abdullahi ElechiDocument17 pagesNeonatal Resuscitation: DR Hassan Abdullahi ElechiHadiza Adamu AuduNo ratings yet
- Rle Breast Care Health EducationDocument6 pagesRle Breast Care Health EducationCagabcab Canibel MelanyNo ratings yet
- The Phuilippine Health Statistics Definition of TermsDocument8 pagesThe Phuilippine Health Statistics Definition of Termsinno so qtNo ratings yet
- 3.0 Cytology-CELL CYCLE UphmoDocument43 pages3.0 Cytology-CELL CYCLE UphmoPatrick DingcoNo ratings yet
- Vgo Imp MCQDocument5 pagesVgo Imp MCQomprakash ChabarwalNo ratings yet
- ACOG Timing of Cesarean Delivery in Women With 2 Previous CesareanDocument10 pagesACOG Timing of Cesarean Delivery in Women With 2 Previous CesareanNica Joy DesquitadoNo ratings yet
- Eskan DR 2018Document7 pagesEskan DR 2018Jorge E. Lara CoronadoNo ratings yet
- 25 HospitalDocument5 pages25 HospitalVIRAT SINGHNo ratings yet
- Embryology 6 Limb DevelopmentDocument17 pagesEmbryology 6 Limb DevelopmentVokeh Dante MedDeeNo ratings yet
- Test Bank For Fundamentals of Corporate Finance 10th Edition Stephen A Ross Randolph W Westerfield Bradford D JordanDocument36 pagesTest Bank For Fundamentals of Corporate Finance 10th Edition Stephen A Ross Randolph W Westerfield Bradford D Jordantithly.decamplh56c7100% (41)
- Drug IntroductionDocument84 pagesDrug IntroductionMousumi DasNo ratings yet
- Examen D'anglès de La Selectivitat 2023Document8 pagesExamen D'anglès de La Selectivitat 2023RAC1No ratings yet
- Final 1 (12TH June) - 230530 - 115919Document26 pagesFinal 1 (12TH June) - 230530 - 115919Arda DumanNo ratings yet