Professional Documents
Culture Documents
Receive Weekly Emails on Phantom Limb Pain
Uploaded by
Peter AgabaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Receive Weekly Emails on Phantom Limb Pain
Uploaded by
Peter AgabaCopyright:
Available Formats
Sign up to receive ATOTW weekly - email worldanaesthesia@mac.
com
PHANTOM LIMB PAIN
ANAESTHESIA TUTORIAL OF THE WEEK 229
27TH JUNE 2011
Dr Alison Kearsley, Speciality Registrar in Anaesthesia
Ninewells Hospital, Dundee, UK
Correspondence to a.kearsley@nhs.net
Dr Michael J.E. Neil, Consultant in Anaesthetics and Pain
Medicine
Ninewells Hospital and Medical School, Dundee, UK.
Correspondence to: mneil@nhs.net
QUESTIONS
Answer true or false
1. Phantom pain
a. Occurs in around 50% of patients after amputation
b. Reduces in incidence with time
c. Is usually a constant pain
d. Is commonly experienced by people with congenitally absent limbs
e. Is more common in patients with persistent stump pain
2. Recognised treatments include
a. Non-steroidal anti-inflammatories
b. Paracetamol
c. NMDA Antagonists
d. Sodium channel blockers
e. Tricyclic antidepressants
INTRODUCTION
Sensation experienced in an amputated limb was first described in 1551 by Ambroise Paré, a French
military surgeon. Subsequently, in 1871 during the American Civil War, the term ‘phantom limb’ was
first recorded by the neurologist Silas Weir Mitchell. Despite increased clinical recognition of
phantom pain since that time, the mechanisms underlying the phenomenon remain poorly understood.
The pathogenesis of phantom pain is complex, including both peripheral and central neural processes
and is still the subject of on-going study. Phantom pain is a form of neuropathic pain and, once
established, can be extremely difficult to treat.
DEFINITIONS
Following amputation, patients experience a number of different forms of pain. Nociceptive pain in the
amputated stump is a normal and predictable response to the surgical insult. Early post-operative
perception of non-painful sensations in the amputated limb are common (phantom sensation) and
should be regarded as normal following amputation. However, phantom pain is the perception of pain
in the amputated limb.
These different forms of pain must be distinguished by taking a careful history from the patient as
treatment varies depending on the predominant nature of the pain described.
ATOTW 229 – Phantom pain, 27/06/2011 Page 1 of 7
Sign up to receive ATOTW weekly - email worldanaesthesia@mac.com
Phantom sensation: Any sensation in the absent body part,
except pain.
Phantom pain: Painful sensations referred to the absent
body part.
Stump pain: Pain localized in the stump.
FEATURES
Phantom sensations
Phantom sensation and phantom pain commonly co-exist. Phantom sensation occurs in most amputees,
and is experienced as resembling the pre-amputation limb in shape and size and may include feelings
of posture and movement. Patients may describe feelings of warmth, cold, itching, tingling or electric
sensations. Phantom sensation usually appears soon after amputation and can last from weeks to years,
but is not experienced as being painful.
Some patients also describe the phenomenon of ‘telescoping’. This is where the distal part of the
phantom limb is felt to be closer to the stump or within the stump itself. For example, forearm
amputees may describe feeling that their amputated hand is attached to their elbow stump. This
probably occurs because the cortical magnification of the hand is proportionally over represented on
the somatosensory cortex.
Figure 1. The Homunculus; A pictoral view of the somatosensory map with body parts scaled
in sizes proportional to their cortical representation (reproduced with permission from Posit
Science Corporation)
ATOTW 229 – Phantom pain, 27/06/2011 Page 2 of 7
Sign up to receive ATOTW weekly - email worldanaesthesia@mac.com
Phantom pain
Around 60 – 80% of amputees will experience phantom pain in the early post-operative period with the
incidence decreasing with time following amputation. The incidence of phantom limb pain appears to
be independent of age, gender and level or side of amputation. 75% of patients will develop phantom
pain within the first few days after amputation but the first emergence of phantom pain may be delayed
and develop several years later. Phantom pain is often regarded as a chronic pain problem lasting for
many years following amputation. Several studies, however, have shown a reduction in pain over
periods of 2 – 5 years post amputation, although most continue to experience some pain beyond this.
A number of factors have been shown to be predictive of the onset of phantom limb pain post-
operatively. Patients found to be most at risk are those who have severe pain in the amputated limb pre-
operatively, patients undergoing bilateral amputation and patients with persisting stump pain. The
incidence of phantom limb pain is however lower in paediatric amputees and very rare in those with
congenitally absent limbs.
Phantom pain is most commonly thought of as occurring following amputation of a limb but it is also
well recognised following amputation of other bodily parts including testis, penis, breast, eye or
tongue. The incidence of phantom pain following mastectomy is quoted as high as 15% but is a poorly
recognised and seldom acknowledged sequelae of this type of operation.
Phantom pain is usually felt as being located in the distal part of the amputated limb and is often
described as being gripping, burning, shooting or cramping in character. Unlike many forms of
neuropathic pain, phantom limb pain is commonly intermittent although some patients will experience
constant pain. Once established, phantom limb pain can be very resistant to treatment; for instance
dense regional anaesthetic blockade provides only limited benefit. Indeed, a number of cases have
been reported of patients developing phantom limb pain for the first time while under spinal
anaesthetic and also of patients experiencing exacerbations of pre-existing phantom pain with spinal
and epidural anaesthesia. This reinforces the view that phantom limb pain is not solely a phenomenon
of the peripheral nervous system but involves more widespread and complicated central processes.
Stump pain
Stump pain is common in the early post-operative period. This is an acute nociceptive pain that
usually resolves as the wound heals. Stump pain may persist in 5 – 10% of patients due to on-going
local pathology or an acute neuropathic process. Sensory examination of the stump at this time may
demonstrate hyperalgesia and allodynia. Surgical revision should be avoided if at all possible and is
only indicated for localised pathology such as osteomyelitis or abscess. Persistent stump pain may be a
risk factor for phantom pain.
At a later stage, once the patient begins rehabilitation and mobilisation, stump pain may develop or be
exacerbated due to a poorly fitting prosthesis.
AETIOLOGY OF PHANTOM PAIN
The exact mechanism of phantom limb pain is unknown but it is believed to involve both peripheral
and central changes to the nervous system that occur following nerve injury during amputation.
Peripheral mechanisms
Amputation results in the severing of peripheral nerve axons and the formation of neuromas, which are
enlarged, disorganised endings of C-fibres and demyelinated A fibres. Neuromas have been shown to
demonstrate abnormal spontaneous and evoked activity that is thought to be due to fundamental
changes in ion channel function. Altered sodium channel expression has been particularly implicated
in this process. There are also changes to dorsal root ganglion cells that display abnormal spontaneous
activity and increased sensitivity to mechanical and chemical stimulation. The sympathetic nervous
system is also thought to be involved in the pathogenesis and persistence of phantom pain.
ATOTW 229 – Phantom pain, 27/06/2011 Page 3 of 7
Sign up to receive ATOTW weekly - email worldanaesthesia@mac.com
Spinal mechanisms
After nerve injury there is an increase in excitability of spinal cord neurons characterised by abnormal
spontaneous activity and exaggerated response to mechanical and thermal stimuli. Sensitisation of
dorsal horn neurons occurs in response to increased painful stimulus from the amputation site and is
mediated by the release of pro-nociceptive agents such as glutamate and neurokinins. This
hyperexcitability may result in the clinical picture of mechanical hyperalgesia.
Key to the phenomenon of spinal sensitisation is increased activity in N-methyl D-aspartate (NMDA)
receptor mediated systems. These systems are important in the phenomenon of neuronal plasticity
whereby the receptive field of a particular neurone is widened by forming new cross-links with
adjacent afferent neurones in different laminae within the spinal cord. Other neurotransmitters such as
substance P and calcitonin gene-related peptide have also been implicated in this process
Cerebral mechanisms
Soon after amputation there is a reorganisation of primary somatosensory and motor cortices and
subcortical structures. Areas of somatosensory cortex which previously corresponded to the missing
limb subsequently receive sensory information from other areas of the body that synapse at adjacent
areas on the somatosensory cortex. It is thought that phantom pain may be a consequence of errors
occurring in this remapping process.
The degree of reorganisation is related to perceived pain intensity and reduces with effective treatment
of pain. This can be demonstrated by clinical examination of sensation, which may show a
somatotropic representation of the phantom limb on the chest wall, in the stump or on the face.
PREVENTION
Many studies have been undertaken investigating methods of preventing phantom limb pain. A popular
theory has been the use of pre-emptive analgesia. The constant, supra-normal nociceptive input from
an amputated limb is thought to contribute to the neural re-organisation which may lead to phantom
pain phenomena. It was hoped that by initiating intensive pre-operative analgesia, particularly by
afferent nerve blockade, abnormal neural reorganisation may be prevented. However, in patients who
have experienced a period of severe pain pre-operatively these changes may have already taken place.
Much of the early work in this area examined the impact of prolonged pre-operative epidural analgesia
on the incidence of phantom pain. Despite showing promising early results, it was later realised that
some studies had significant methodological problems and subsequent larger studies found no
significant benefit on the overall incidence of phantom pain with this technique. Pre-operative epidural
anaesthesia may however decrease the incidence of severe phantom pain but not the overall incidence
of phantom pain.
An alternative, and increasingly popular technique to prevent phantom pain involves the placement of
peri-neural catheters either pre or intra-operatively. Administration of local anaesthetic at the time of
amputation and as a continuous infusion for 72 hrs post operatively has been shown to be of some
benefit in helping prevent phantom pain. The addition of clonidine to a peri-neural local anaesthetic
infusion may confer an additional benefit.
TREATMENT
In common with many areas in pain medicine, there is no strong evidence base to guide treatment of
phantom pain. Many studies are of small size with differing end-points and investigate diverse patient
groups with different peri-operative anaesthetic management. Consequently, much available evidence
ATOTW 229 – Phantom pain, 27/06/2011 Page 4 of 7
Sign up to receive ATOTW weekly - email worldanaesthesia@mac.com
is based on small case-series, cohort studies and expert opinion making any firm recommendations
difficult. However, some common treatment strategies are detailed below.
Pharmacological
Antidepressants
Tricyclic antidepressants (TCA’s) such as amitriptyline and nortriptyline act by inhibiting the re-uptake
of noradrenaline and serotonin thereby potentiating the action of two important central anti-nociceptive
pathways. TCA’s have been shown in a number of randomised controlled trials to be effective in the
management of a variety of neuropathic pain conditions. Although there are no studies specifically
examining the use of TCAs in phantom limb pain, they are commonly used and thought to have modest
efficacy. TCAs have a number of side-effects including excessive sedation and anticholinergic side
effects such as dry mouth, urinary retention and constipation. These may limit their use. However,
when started at low dose, these effects can be minimised.
Duloxetine is a relatively new agent which has shown promise as an analgesic in other types of
neuropathic pain (particularly in painful diabetic neuropathy). Duloxetine also acts on serotinergic and
noradrenergic pathways similar to TCA’s. Clinical experience with this agent in phantom limb pain is
limited; however, one early case report suggests that duloxetine may be beneficial in phantom limb
pain.
Serotonin specific re-uptake inhibitors (SSRIs) are less effective in the management of neuropathic
pain and consequently are seldom used for this purpose. This lack of efficacy is likely to be a reflection
on the much narrower spectrum of action compared to TCA’s.
Sodium channel blockers and anticonvulsants
Gabapentin and pregabalin bind to voltage gated calcium channels and have been shown to be effective
in a variety of neuropathic pain problems. Evidence for their use in phantom pain is unclear, with
conflicting results from RCTs. Although generally well tolerated, the main dose-limiting side effects
of gabapentin are somnolence and dizziness which can be minimised by gradual dose titration.
Second line agents include carbamazepine and lamotrigine. These should be considered after
conventional mono and combination therapy with TCA’s and anticonvulsants has failed.
Intravenous lidocaine has been extensively reported as having good efficacy in neuropathic pain and its
oral analogue, mexiletine, has also been shown in one small study to produce pain relief in phantom
pain. This class of drug can be particularly useful as the analgesic effects are of faster onset in
comparison to standard anti-neuropathic agents with the clinical effect often significantly outlasting the
pharmacological action of the drug. These agents have a good safety profile and should be considered
at an early stage after other first-line agents have been tried.
Tramadol
Tramadol is a synthetically produced drug that has both monoaminergic and opioid activity with less
adverse effects than strong opioids. This extended action is particularly useful for neuropathic pain that
can involve multiple receptor processes. Tolerance and dependence are uncommon. Tramadol has been
shown in a number of studies to reduce neuropathic pain including post-amputation pain.
Other drugs
One double-blind crossover study has shown calcitonin to be effective in treating phantom pain if
given early in the post-operative period. This is a clinically well tolerated agent that can be
administered as a subcutaneous injection, intravenous infusion or intra-nasal spray. It does not,
however, have any proven efficacy in treating established phantom pain.
ATOTW 229 – Phantom pain, 27/06/2011 Page 5 of 7
Sign up to receive ATOTW weekly - email worldanaesthesia@mac.com
Intravenous ketamine has been shown to reduce pain, hyperalgesia and ‘wind up’ in those with stump
pain and phantom limb pain. However, ketamine administered via the epidural route peri-operatively
does not decrease the incidence of phantom limb pain. The use of ketamine is frequently limited by
unpleasant neuro-psychiatric side-effects such as hallucinations. An alternative NMDA antagonist is
Memantine that has been shown in some small studies to be helpful in managing phantom limb pain if
used during the acute or sub-acute phase. This drug has a good pharmacokinetic profile, well suited to
pain management, with a better side-effect profile than ketamine.
Non medical treatments
Mirror box
The mirror box is a device containing a vertically placed mirror into which the amputated limb is
placed and is positioned so that a reflection of the patient’s intact limb is ‘superimposed’ onto the
perceived position of the phantom limb. It has been shown that mirrored movements activate the
contralateral sensorimotor cortex, and this is associated with a reduction in pain.
The mirror box is particularly helpful in patients who experience spasms of their phantom upper limb
perceived as involuntary clenching of the missing hand. The mirror box allows the patient to visualise
the unclenching of this limb which can help relieve the pain of these spasms.
Mental imagery
Alternative methods of stimulating the motor or sensory cortices can also achieve a reduction in
phantom limb pain. Mental imagery is the process of imagining motor sequences and is thought to
work in a similar way to the mirror box. This follows a program of imagery exercises and can be
completed by the patient at home. Studies looking at functional MRI (fMRI) in amputees before and
after training in mental imagery have shown a significant reduction in pain which is associated with a
corresponding change in cortical MRI signal. This is seen only in patients with amputation pain, and
not in amputees with no pain or controls.
Acupuncture and TENS
Other treatments which have been used include acupuncture and TENS. It is not clear where the
optimum site for placement of TENS electrodes. One approach is to apply stimulation to the
contralateral limb. There may also be benefit in placing electrodes on the chest wall or flank in patients
who display clear somatotropic representation of the limb on these areas.
Stump care
Stump care and prosthetics also have an important role. Immediate fitting of stump prosthesis can be
helpful in the management of phantom pain.
Psychology
Patients may also benefit from explanation and reassurance or therapies such as hypnosis,
psychotherapy and cognitive behavioural therapy.
Electrical stimulation
Electrical stimulation of the spinal cord, deep brain structures and motor cortex may relieve pain but its
effectiveness may decrease over time. These invasive techniques should be reserved for the most
refractory of cases.
ATOTW 229 – Phantom pain, 27/06/2011 Page 6 of 7
Sign up to receive ATOTW weekly - email worldanaesthesia@mac.com
CONCLUSION
Phantom limb pain occurs in 60 – 80% of patients following amputation as result of a combination of
peripheral, spinal and cortical changes and is often difficult to treat. Current treatments are
predominantly based on evidence from small studies and evidence of benefit in different types of
neuropathic pain. Further research is required to examine methods of preventing phantom pain
developing and to guide treatment choices in the future.
Summary
Phantom limb sensation, stump pain and phantom limb pain
often co-exist
Phantom limb pain occurs as result of a combination of
peripheral, spinal and cortical changes.
Phantom limb pain is difficult to treat
Pharmacological therapies include tricyclic antidepressants,
sodium channel blockers, anticonvulsants, NMDA
antagonists and calcitonin.
Non-drug treatments such as mirror therapy, acupuncture,
TENS, psychology and prosthetics are also important
Epidural anaesthesia may have a role in preventing phantom
limb pain but further studies are required.
ANSWERS TO MCQS
1) FTFFT
2) FFTTT
REFERENCES and FURTHER READING
1) Nikolajsen L, Jensen TS. Phantom limb pain. Br. J. Anaesth. 2001; 87 (1): 107-116.
2) Nathanson M. Phantom Limbs as reported by S.Weir Mitchell. Neurology 1988; 38:504-505
3) Spiegel DR et al. A presumed case of phantom limb pain treated successfully with duloxetine and
pregabalin. Gen Hosp Psychiatry. 2010; 32(2):228
4) Dworkin RH et al. Pharmacologic management of neuropathic pain: Evidence-based
recommendations. Pain 2007; 132 (3): 237-251
5) Jaeger H, Maier C. Calcitonin in phantom limb pain: a double‐blind study. Pain 1992; 48: 21–27
6) Diers M et al. Mirrored, imagined and executed movements differentially activate sensorimotor
cortex in amputees with and without phantom limb pain. Pain 2010; 149: 296-304
7) MacIver D, Lloyd M et al. Phantom limb pain, cortical reorganization and the therapeutic effect of
mental imagery. Brain 2008; 131 (8): 2181-2191
8) Fisher A, Meller Y. Continuous postoperative regional analgesia by nerve sheath block for
amputation surgery—a pilot study. Anesth Analg 1991; 72: 300–3
9) Churchill Pocketbook of Pain Second Edition 2004 Stannard C, Booth S
10) Jackson MA, Simpson KH. Pain after amputation. BJA: Contin Educ Anaesth Crit Care Pain 2004;
4 (1): 20-23.
11) Flor H. Phantom-limb pain: characteristics, causes, and treatment. The Lancet 2002 (1); 3:182-189
ATOTW 229 – Phantom pain, 27/06/2011 Page 7 of 7
You might also like
- PAIN: Phantom Limb PainDocument4 pagesPAIN: Phantom Limb PainIgnacio AndrésNo ratings yet
- Understanding Nociceptors and Phantom Limb PainDocument4 pagesUnderstanding Nociceptors and Phantom Limb PainluisaNo ratings yet
- Atow 438 00Document7 pagesAtow 438 00Luiza MansurNo ratings yet
- Pain Management in The AmputeeDocument51 pagesPain Management in The Amputeeptannenbaum100% (1)
- Phantom Limb Pain 2006Document10 pagesPhantom Limb Pain 2006Alejandra RomeroNo ratings yet
- Phantom Limb PainDocument10 pagesPhantom Limb PaindevrtNo ratings yet
- Traumatic Brachial Plexus Injuries GuideDocument5 pagesTraumatic Brachial Plexus Injuries GuidedoruntineNo ratings yet
- Chinese Journal of Traumatology: Phantom Limb Pain: A Literature ReviewDocument3 pagesChinese Journal of Traumatology: Phantom Limb Pain: A Literature ReviewEva Nur MalaNo ratings yet
- Report Neuro DutyDocument10 pagesReport Neuro DutyNoelle HarrisonNo ratings yet
- Phantom Limb Pain: Subtle Energy PerspectivesDocument28 pagesPhantom Limb Pain: Subtle Energy PerspectivesMircea PocolNo ratings yet
- Sindrome MiofacialDocument13 pagesSindrome MiofacialAngie Paola RodriguezNo ratings yet
- Sign up for weekly anaesthesia tutorial emailDocument8 pagesSign up for weekly anaesthesia tutorial emailAli AftabNo ratings yet
- Managing Phamtom PainDocument12 pagesManaging Phamtom PainjesusmonNo ratings yet
- Week 9 Case Study 9 Chir13009Document7 pagesWeek 9 Case Study 9 Chir13009api-479754549No ratings yet
- Adverse Neural Tissue TensionDocument60 pagesAdverse Neural Tissue TensionjoecannilloNo ratings yet
- Konsep Nyeri - Dr. SusiloDocument18 pagesKonsep Nyeri - Dr. Susilotendri ayuNo ratings yet
- Carpal Tunnel SyndromeDocument27 pagesCarpal Tunnel SyndromeSereinNo ratings yet
- Trauma Case Reports: Jugert Bango, Evan Zhang, Daniel L. Aaron, Amna DiwanDocument4 pagesTrauma Case Reports: Jugert Bango, Evan Zhang, Daniel L. Aaron, Amna DiwanCristhian Jover CastroNo ratings yet
- NeuropathyDocument54 pagesNeuropathyshreyasNo ratings yet
- ELECTROACUPUNCTURE FOR ALLEVIATION OF PHANTOM LIMB PAIN : Case ReportDocument5 pagesELECTROACUPUNCTURE FOR ALLEVIATION OF PHANTOM LIMB PAIN : Case ReportrezteevicNo ratings yet
- Mike Reinold - Solving The PF MysteryDocument36 pagesMike Reinold - Solving The PF MysteryCarrie SagoNo ratings yet
- Nerve Injuries Associated With Gynecological SurgeryDocument8 pagesNerve Injuries Associated With Gynecological SurgeryLakshmi DheviNo ratings yet
- Concept of PainDocument98 pagesConcept of PainEnrico Carlo EstacioNo ratings yet
- Thesis J FleurenDocument192 pagesThesis J FleurenEniko VeghNo ratings yet
- Posterior Knee Pain and Its CausesDocument12 pagesPosterior Knee Pain and Its Causesdoos1No ratings yet
- Trigger Point Homp. TehranDocument46 pagesTrigger Point Homp. TehranKasra Chehrazy100% (1)
- Morton's NeuromaDocument3 pagesMorton's NeuromaRaymondNo ratings yet
- Week 1 and 2 PCP Workbook QuestionsDocument4 pagesWeek 1 and 2 PCP Workbook Questionsapi-479717740100% (1)
- Back Pain PathophysiologyDocument33 pagesBack Pain PathophysiologyDaryo Soemitro94% (18)
- Post-Traumatic Tremors: Francisco E.C. Cardoso, MD & Joseph Jankovic, MDDocument1 pagePost-Traumatic Tremors: Francisco E.C. Cardoso, MD & Joseph Jankovic, MDaston7776No ratings yet
- Pathophysiology Back Pain: Daryo SoemitroDocument33 pagesPathophysiology Back Pain: Daryo SoemitroNurul AiniNo ratings yet
- AnesthesiaDocument3 pagesAnesthesiaAnd OnlyJustNo ratings yet
- Spinal Cord InjuriesDocument35 pagesSpinal Cord InjuriesTitanium TssNo ratings yet
- Pathophysiology Back Pain: Daryo SoemitroDocument33 pagesPathophysiology Back Pain: Daryo SoemitroJohannah DaroNo ratings yet
- Diagnosing Pronator SyndromeDocument6 pagesDiagnosing Pronator SyndromeMplusWNo ratings yet
- Cateteres PerineuralesDocument23 pagesCateteres PerineuralesAndres Felipe Velasquez TafurNo ratings yet
- Weiss Athens2006Document11 pagesWeiss Athens2006MarceloAntonioHaradaPennaNo ratings yet
- Lumbar Laminectomy Surgery For Spinal StenosisDocument15 pagesLumbar Laminectomy Surgery For Spinal StenosisElizabeth Liles MartinezNo ratings yet
- Spinal Cord Injury RehabilitationDocument6 pagesSpinal Cord Injury RehabilitationHugh JacobsNo ratings yet
- Complications After AmputationDocument44 pagesComplications After AmputationGulzar AhmadNo ratings yet
- Auricular Therapy For Treating Phantom Limb Pain Accompanied by Jumping Residual Limb: A Short Review and Case StudyDocument11 pagesAuricular Therapy For Treating Phantom Limb Pain Accompanied by Jumping Residual Limb: A Short Review and Case StudyrezteevicNo ratings yet
- Low Back Pain PDFDocument4 pagesLow Back Pain PDFnetifarhatiiNo ratings yet
- Síndrome de Dolor MiofascialDocument7 pagesSíndrome de Dolor MiofascialAbraham SaldañaNo ratings yet
- WEISSPNEDocument4 pagesWEISSPNELauraNo ratings yet
- Peripheral Nerve Injuries - Medical ApplicationsDocument103 pagesPeripheral Nerve Injuries - Medical ApplicationsJune Epe100% (1)
- Peroneal Mononeuropathy TreatmentDocument13 pagesPeroneal Mononeuropathy TreatmentAnnisa Kinanti AstiNo ratings yet
- ElectromyographyDocument54 pagesElectromyographymohanprasannaNo ratings yet
- Musculoskeletal Disorders of Elbow, Wrist and HandsDocument59 pagesMusculoskeletal Disorders of Elbow, Wrist and Handssaroj yadavNo ratings yet
- HNPDocument47 pagesHNPSyifa RabiahNo ratings yet
- Basic Science ART & NerveDocument56 pagesBasic Science ART & NerveStar CruiseNo ratings yet
- CRPS and Compartment SyndromeDocument19 pagesCRPS and Compartment Syndromegbc1989No ratings yet
- Managing Neuropathic PainDocument10 pagesManaging Neuropathic PainAgusBhakti100% (1)
- Femoral Neck FracturesDocument2 pagesFemoral Neck FracturesFarinaDwinandaFaisalNo ratings yet
- Nociception Neuropathic Inflammatory PainDocument1 pageNociception Neuropathic Inflammatory PainRiyad AliNo ratings yet
- MFPSDocument18 pagesMFPSएम जी एम अलाइड हेल्थ साइंसेज इंस्टिट्यूट MAHSI MGMMC IndoreNo ratings yet
- Pronator Teres Syndrome DiagnosisDocument11 pagesPronator Teres Syndrome DiagnosisNUR ZAMZAM AZIZAHNo ratings yet
- Carpal Tunnel Syndrome, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandCarpal Tunnel Syndrome, A Simple Guide To The Condition, Treatment And Related ConditionsRating: 5 out of 5 stars5/5 (1)
- Cubital Tunnel Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandCubital Tunnel Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Experience and RecollectionDocument316 pagesExperience and RecollectionPeter AgabaNo ratings yet
- Zampieri 2019Document8 pagesZampieri 2019Peter AgabaNo ratings yet
- Fluid Assessment by SonographyDocument58 pagesFluid Assessment by SonographyPeter AgabaNo ratings yet
- Vt900a User ManualDocument58 pagesVt900a User ManualdcgNo ratings yet
- Fluidos e Hipertonicos Neurocrit CareDocument5 pagesFluidos e Hipertonicos Neurocrit CareMiguelAngelEspinalLendofNo ratings yet
- Albumin Administration in The Acutely Ill: What Is New and Where Next?Document10 pagesAlbumin Administration in The Acutely Ill: What Is New and Where Next?Peter AgabaNo ratings yet
- FCEM (SA) - Part - I - Past - Papers 4Document4 pagesFCEM (SA) - Part - I - Past - Papers 4matentenNo ratings yet
- 2015 Resident ManualDocument850 pages2015 Resident ManualPeter AgabaNo ratings yet
- Peri-Operative Cardiac Arrest Secondary To Adrenal InsufficiencyDocument3 pagesPeri-Operative Cardiac Arrest Secondary To Adrenal InsufficiencyPeter AgabaNo ratings yet
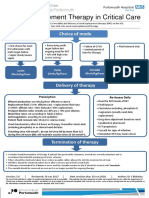
- Renal Replacement Therapy in Critical Care: Choice of ModeDocument15 pagesRenal Replacement Therapy in Critical Care: Choice of ModePeter AgabaNo ratings yet
- 171 Vapour Is at Ion and VapourisersDocument9 pages171 Vapour Is at Ion and Vapourisersdrvinodg2000No ratings yet
- Sign up for weekly anaesthesia tutorial emailDocument8 pagesSign up for weekly anaesthesia tutorial emailAli AftabNo ratings yet
- 321 Difficult Mask VentilationDocument7 pages321 Difficult Mask VentilationFajar SatriaNo ratings yet
- تعديل مناقشةDocument159 pagesتعديل مناقشةم.م حمزة عباس فاضلNo ratings yet
- AmputationDocument7 pagesAmputationAsma SaleemNo ratings yet
- Full Draft - Grace Prosthetics Fabrication, Inc.Document102 pagesFull Draft - Grace Prosthetics Fabrication, Inc.CarlNo ratings yet
- Reconstructive Surgery - Lower Extremity CoverageDocument29 pagesReconstructive Surgery - Lower Extremity Coverage정형화No ratings yet
- Stump Healing Times and Hospital Stays Compared for Soft vs Rigid Dressings After BKADocument4 pagesStump Healing Times and Hospital Stays Compared for Soft vs Rigid Dressings After BKAAris Alfaldieka CahyanaNo ratings yet
- Cambodian School of Prosthetics and Orthotics: CSPO ManualDocument60 pagesCambodian School of Prosthetics and Orthotics: CSPO ManualBilalNo ratings yet
- Whirlp 1Document20 pagesWhirlp 1mdjgladiatorNo ratings yet
- Upper-Int 3 Lesson 7Document25 pagesUpper-Int 3 Lesson 7masc1127No ratings yet
- Chapter 46: Amputations: Multiple ChoiceDocument10 pagesChapter 46: Amputations: Multiple ChoiceStaceyNo ratings yet
- Sandra M. Nettina MSN ANP BC Lippincott Manual of Nursing Practice Handbook 2005 LWWDocument1,109 pagesSandra M. Nettina MSN ANP BC Lippincott Manual of Nursing Practice Handbook 2005 LWWJoan Ano CaneteNo ratings yet
- Osteomyoplastic Transtibial Amputation The Ertl.6Document7 pagesOsteomyoplastic Transtibial Amputation The Ertl.6alex1973maNo ratings yet
- GURPS Injuries TableDocument3 pagesGURPS Injuries Tabledenix100% (1)
- 1.5-DOH Reviewer & Examination-NurseDocument111 pages1.5-DOH Reviewer & Examination-NurseRoger CarpisoNo ratings yet
- Ankle Disarticulation Prosthetics: Course Work ManualDocument52 pagesAnkle Disarticulation Prosthetics: Course Work ManualJananthan Thavarajah67% (3)
- Mnemonic: Erotica: MGT For FractureDocument6 pagesMnemonic: Erotica: MGT For FractureBianx Flores DosdosNo ratings yet
- Abbreviations Used:: Î Blank Rubric, Rubric Having No Remedy ListDocument181 pagesAbbreviations Used:: Î Blank Rubric, Rubric Having No Remedy ListBhargavi KotaNo ratings yet
- Facilitators and Barriers That Transfemoral Amputees Experience in Their Everyday LifeDocument8 pagesFacilitators and Barriers That Transfemoral Amputees Experience in Their Everyday LifeJuciara MouraNo ratings yet
- Daftar Diagnosis Dan Tindakan Orthopaedi Ina CBG Baru Dan Plafonb - CompressDocument11 pagesDaftar Diagnosis Dan Tindakan Orthopaedi Ina CBG Baru Dan Plafonb - CompressChika HardiyantiNo ratings yet
- Critical Limb IschemicDocument27 pagesCritical Limb IschemicErik Judika2No ratings yet
- Encyclopedia of Unusual Sex Practices PDFDocument432 pagesEncyclopedia of Unusual Sex Practices PDFmspiliopoulou100% (1)
- Final 2021 Benefit Year Final HHS Risk Adjustment Model CoefficientsDocument26 pagesFinal 2021 Benefit Year Final HHS Risk Adjustment Model CoefficientsJ CHANGNo ratings yet
- DMDocument59 pagesDMfidelia adetayo CONDENo ratings yet
- Healthy Lifestyle Vocabulary Word List (306) : Unit 2-HealthDocument12 pagesHealthy Lifestyle Vocabulary Word List (306) : Unit 2-HealthTulus HikmatullohNo ratings yet
- AmputationDocument1 pageAmputationKassandra MerrillNo ratings yet
- Modul 2qquestionsDocument4 pagesModul 2qquestionsНваневу СильванусNo ratings yet
- Test Bank For Essentials of Assistive Technologies 1st Edition Albert M Cook DownloadDocument5 pagesTest Bank For Essentials of Assistive Technologies 1st Edition Albert M Cook Downloadazurawinifredupaa8mNo ratings yet
- Sister Callista RoyDocument17 pagesSister Callista RoyAbhee CalimagNo ratings yet
- Vascular Journal Reading - Rendi KurniawanDocument6 pagesVascular Journal Reading - Rendi KurniawanChristopher TorresNo ratings yet
- Lightweight Artificial Limb Production CentreDocument5 pagesLightweight Artificial Limb Production Centresahil patelNo ratings yet
- Rehabilitation For Persons With Upper Extremity AmputationDocument14 pagesRehabilitation For Persons With Upper Extremity AmputationVince ObiedoNo ratings yet