Professional Documents
Culture Documents
Chronic Inflammation
Uploaded by
Sara Sultana0 ratings0% found this document useful (0 votes)
21 views15 pagesNotes on Chronic Inflammation from Ramdas Nayak Exam Preparatory Manual- Pathology- MBBS and BDS 2nd year students
Original Title
4. CHRONIC INFLAMMATION
Copyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentNotes on Chronic Inflammation from Ramdas Nayak Exam Preparatory Manual- Pathology- MBBS and BDS 2nd year students
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
21 views15 pagesChronic Inflammation
Uploaded by
Sara SultanaNotes on Chronic Inflammation from Ramdas Nayak Exam Preparatory Manual- Pathology- MBBS and BDS 2nd year students
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 15
4. Chronic Inflammation
27 Aprit2021— 17.27
Inflammation of prolonged duration (weeks or months} in which inflammation, tissue
damage, and healing occurs at the same time, in varying combinations.
Chronic inflammation may:
1. Follow an acute inflammation, which does not resolve (ex: chronic osteomyelitis}
or
2. Begin as insidious, low grade, chronic, response w/o any acute inflammatory
reaction,
Sequelae: chronic inflammation can cause disabling tissue damage. Ex: rheumatoid
arthritis, TB and atherosclerosis
CAUSES:
1. Persistent infections: microbes that are difficult to eradicate elicit delayed type
of hypersensitivity—produce chronic inflammation ex: mycobacteria,and certain
viruses, fungi and parasites. Some agents may cause a distinct pattern of chronic
inflammation—granulomatous reaction
2. Immune-mediated inflammatory (hypersensitivity) diseases:
+ Autoimmune di rheumatoid arthritis
+ Allergic reactions: bronchial asthma
+ Unregulated immune response: inflammatory bowel disease
3. Prolonged exposure to toxic injurious agents:
+ Exogeneous: silica—non biodegradable inanimate exogenous material. Person
exposed to silica particles for long time—inflammatory lung disease—silicosis
+ Endogenous: atherosclerosis—disease of arterial intima—represents a chronic
inflammatory process partly due to endogenous toxic plasma lipid components
Most common cause of chronic inflammation—persistent infection
MORPHOLOGIC FEATURES:
Mononuclear cells infiltrate: macrophages, lymphocytes, and plasma cells
+ Tissue destruction: by the persistence of causative agent or by the inflammatory
cells
+ Healing by fibrosis
CHRONIC INFLAMMATORY CELLS AND MEDIATOR‘
Macrophages :
Predominant cell
‘Tissue macrophage: Derived from hematopoietic stem cells in the bone marrow and
from progenitors in the embryonic yolk: sac and fetal liver during early development
MACROPHAGE EVENTS IN INFLAMMATION:
* Monocytes also emigrate into extravascular tissues early in acute inflammation—
predominant cell type within 48 hrs
* On reaching extravascular tissue—monocyte transformed into tissue
macrophage
Macrophage activation:
By 2 major pathways
© Classical macrophage activation:
-Mediators of activation: brought out mainly by:
+ Microbial products:ex: endotoxin
+ Tcell derived signals: mainly cytokines (for ex: IFN-y)
+ Foreign substances: ex: crystals and particulate matter
products of activated macrophages:
+ Lysosornal enzymes
+ Nitric oxide
+ Reactive oxygen species (ROS)
function: phagocytosis and killing/ elimination of ingested microbes
© Alternate macrophage activation:
-mediators of activation: cytokines IL-4 and IL-13 produced by T cells and other
cells
-function: initiation of the tissue repair (they are not bactericidal]
Functions of macrophages in inflammation:
‘© Phagocytosis: ingestion and elimination of microbes and necrotic tissue
© Initiation of tissue repair
© Secretion of mediators of inflammation: cytokines (TNF, IL-1, chemokines, etc]
and arachidonic acid metabolites
© Display signal to T-cells and respond signals form T-cells : responsible for the
feedback loop for defense against many microbes by cell- mediated immune
response
hocyt
‘© Band T lymphocyte: found in both antibody- mediated and cell mediated
immune reactions
© B lymphocytes: may develop into plasma cells and produce antibodies either
against foreign or self-antigens in the inflammatory site
© T lymphocytes: important being CD4+ helper T cells which has 3 subtypes
namely:
-TH1: Produce INF-y and activates macrophage in the classical pathway.
~TH2: Produce IL-4, IL-5 and IL-13 which recruit and activate eosinophils and
activate macrophages through alternate pathway. Involved in defense against
helminthic infestation and allergic reaction.
-THI7: Produce IL-17 and other cytokines which recruit neutrophils and
monocytes.
Other cells:
‘© Plasma cells: derived from activated B lymphocytes and produce antibodies
either against foreign or self-antigens
© Eosinophils: seen in immune reactions mediated by IgE and in parasitic
infections. Chemokine which attracts eosinophil recruitment- eotaxin. Eosinophil
granules contain major basic protein—toxic to parasites and also destroy the
epithelial cells
© Mast cells: distributed in CTs and participate in both acute and chronic
inflammatory reactions. Seen in allergic reactions to foods, insect venom or
drugs.
TYPES OF CHRONIC INFLAMMATIO!
1. Chronic non-specific inflammation
2. Granulomatous inflammation
Eosinophils seen in’
+ Hypersensitivity reactions
+ Parasitic infestations
GRANULOMATOUS INFLAMMATION:
Granuloma—distinctive type of chronic inflammation characterized by
microscopic aggregation of activated macrophages (that are transformed into
epithelium like/ epithelioid cells] with scattered lymphocytes
+ Older granulomas—rim of fibroblasts and CT as the outermost layer
+ Structurally, granuloma consists of
+ Epithelioid cells: modified macrophages which resemble epithelial cells
-Pale pink granular cytoplasm—indistinct cell borders—appearing to merge into
one another
-Nucleus—oval or elongate—may show folding of the nuclear membrane—less
dense nucleus than lymphocyte
+ Giant cells: epithelioid cells fuse to form giant cells—found in the periphery or
sometimes in the center of the granulomas
-May attain diameters of 40-50 pm and have many small nuclei
-Nuclei—20 or more—may be arranged either peripherally (Langhans-type giant
cell] or haphazardly (foreign body-type giant cell]
+ Lymphocytes: cell mediated immune reaction to antigen, lymphocytes form an
integral part of granulomatous inflammation
+ Necrosis: sometimes granulomas are associated with central necrosis (ex: TB)
~Granulomas in Crohn disease, sarcoidosis, and foreign body reactions does not
have necrotic centers—non caseating granulomas
+ Fibrosis: granulomas may heal by producing extensive fibrosis
‘TYPES OF GRANULOMAS:
Depending on the pathogenesis—2 types:
Foreign body granulom:
+ Develops against relatively inert foreign bodies which do not incite any specific
inflammatory ot immune response (absence of T-cell mediated immune
responses)
+ Foreign body which elicit granuloma—suture materials, talc (associated with iv
drug abuse}, or other fibers that are large enough to be phagocytosis by a
macrophage
+ Foreign material—in the center of the granuloma—if seen with polarized light
Immune granuloma:
+ Caused by agents /microbes capable of inducing a persistent T-cell-mediated
immune response
+ Develop when the inciting agent is difficult to eradicate, such as a persistent
microbe (ex: Mycobacterium tuberculosis) or a self- antigen
+ Macrophages activate T cells to produce cytokines, such as IL-2—in turn
activates other T cells, perpetuating the response, and IFN-y, which activates the
macrophages
+ Granuloma in TB—tubercle - central caseous necrosis (due to a combination of
hypoxia and free radical mediated injury}
+ Additional tests / investigations to identify the etiologic agent
~ Special stains, e.g, acid-fast stains for tubercle bacilli — Culture methods, e.g. in
tuberculosis and fungal diseases
~ Molecular techniques (e.g. the polymerase chain reaction in tuberculosis)
~ Serologic studies [e.g, in syphilis)
Examples of granulomatous inflammation:
ee ; BOK 4.1:Types of giant cells
Fg. 42: Varousypesct gars
GRANULOMATOUS DISEASES:
+ Mycobacterium -- slender aerobic rods—straight or branching chains—have a
waxy cell wall composed of mycolic acid—responsible for their acid fast nature—
weakly gram +ve
+ Acid fast—mycobacteria retain stain even on treatment with a mixture of acid
and alcohol
LEPROSY:
+ Hansen disease
+ Chronic, granulomatous, slowly progressive, destructive infection caused by
Mycobacterium leprae
+ Sites of involvement—peripheral nerves, skin and mucous membranes (nasal)
and results in disabling deformities
Mycobacterium Leprae:
+ Slender, weakly acid fast intracellular bacillus
Resembles Mycobacterium tuberculosis but is less acid fast
Froliferates at low temperature of the human skin
Cannot be cultured on artificial media or in cell culture
Lepra bacilli grow at sites where temperature is below that of the internal organs
Ex: foot pads of mice, ear lobes of hamsters, rats and other rodents
Antigen in lepra bacilli: cell wall—2 antigens—M. Leprae specific phenolic
glycolipid (PGL-1] and lipoarabinomannan [LAM]
+ Mode of transmission: low communicability
+ M, leprae: Grows best in cooler tissues: (1] Skin, (2) Peripheral nerves, (3)
Anterior chamber of eye, (4) Upper respiratory tract and (5) Testis.
1. Inoculation /inhalation: person to person through aerosols form asymptomatic
lesions in the upper respiratory tract
+ Inhaled M. leprae—taken up by alveolar macrophages and disseminates through
the blood—replicates only in relatively cool tissues of the skin and extremities
2. Intimate contact: many years with untreated leprosy patients—shed many
bacilli from damaged skin, nasal secretions, mucous membrane of mouth and
hair follicles
Source of infection: nasal secretions or ulcerated lesions of patients
Only bacterium that invades peripheral nerves,
Incubation period—5-7 years
CLASSIFICATIO
‘A. Ridley and Jopling classification:
Depends on the clinicopathological spectrum of the disease—determined by the
immune resistance of the host
5 groups—2 extremes or polar forms—tuberculoid and lepromatous
aseyctngclsstcaon
Secor astcaton of eposy
f T + 1 ihe and oping satiation
a Es ee
tprenr tt) | fptmiotet) (68) Wren
Fig 43:8 sets
Tuberculoid leprosy (TT): polar form that has maximal immune response.
Borderline tuberculoid (BT): immune response b/w BB and TT
Borderline leprosy [BB]: exactly b/w the two polar forms of leprosy
Borderline lepromatous (BL): immune response b/w BB and LL
Lepromatous leprosyiLL}: least immune response
Variants of leprosy:
+ Indeterminate leprosy: initial non specific type of leprosy
+ Pure neural leprosy—neurologic involvement is the main feature
+ Histoid leprosy: variant of lepromatous leprosy—skin lesions grossly resemble
nodules of dermatofibroma and microscopically shows numerous lepra bacilli
ohewe
B. WHO classification
Paucibacillary and muttibacillary
+ Paucibacillary—all cases of tuberculoid leprosy and some cases of borderline type
+ Multibacillary—all cases of lepromatous leprosy and some cases of borderline
type
PATHOGENESIS:
‘Mycobacterium leprae- does not secrete any toxins—virulence depends on
properties of its cell wall (similar to M. tuberculosis
+ Immunization with BCG may provide some protection against M. leprae infection
+ Tuberculoid leprosy—strong TH1 response compared to weak TH1 response in
lepromatous leprosy
+ Cell mediated immunity—reflected by delayed-type hypersensitivity reactions to
dermal injections of a bacterial extract called lepromin
+ T-helper (TH1] lymphocyte response to M. leprae, determines whether an
individual develop tuberculoid or lepromatous type of leprosy.
-Tuberculoid leprosy patients—TH1 response—secretes IL-2 and IFN-y. IFN-y is
essential for an effective host macrophage response
-Lepromatous leprosy—weak TH1 response and, in some a relative increase in
the TH2 response --results in a poor cell-mediated immunity --proliferation of
lepra bacilli
Sometimes antibodies produced against M. leprae antigens, but usually not
protective.
‘These can form immune complexes with free antigens and lead to erythema
nodosum, vasculitis, and glomerulonephritis
Morphology:
‘Two extremes or polar forms ~ tuberculoid and lepromatous
1. Tuberculoid leprosy: less severe form—very slow course—most patients die
-Lesion in skin’
«Number of lesions—single or very few
= Site—face, extremities or trunk
« Type—tocalized, well demarcated, red or hypopigmented, dry , elevated, skin
patches having raised outer edges and depressed pale centers (central healing]
As they progress they develop irregular shapes with induration
-Nerve involvement:
= Dominating feature in tuberculoid leprosy
« Nerves surrounded by granulomatous inflammatory reactions and may destroy
small (ex: peripheral twigs) nerves
«Nerve involvernent—toss of sensation in skin—atrophy of skin and muscle.
Affected parts—liable to trauma, and lead to the development of chronic skin
ulcers
« Consequences: contractures, paralyses, and autoamputation of fingers or toes
Involvement of facial nerve can lead to paralysis of fingers or toes. Involvement of
facial nerve can lead to paralysis of the eyelids, with keratitis and corneal
ulcerations
-Microscopy:
«= Granuloma: well formed, circumscribed and non- caseating. In all involved sites
and in the dermis of skin, tuberculoid leprosy because the granulomas resemble
those found in TB. Composed of epithelioid cells [modified macrophages),
Langhans giant cells and lymphocytes.
= Absence of Grenz zone: granulomas in the dermis extend to the basal layer of the
epidermis [w/o a clear/ Grenz zone]
« Fite-Faraco (modified Z-N stain for demonstration of lepra bacillus} stain
generally does not show lepra bacillus, hence the name “paucibacillary” leprosy.
« Perineural (surrounding nerve fibers} inflammation: By lymphocytes
« Strong T-cell immunity: It is responsible for granulomas formation, without lepra
bacilli,
Tuberculoid leprosy:
1. Good immune response
2. Lepromin test positive
3. Noncaseating granuloma in the skin
4. Nerve involvement.
2. Lepromatous leprosy: more severe form — anergic leprosy—because of the
unresponsiveness of the host immune system.
Sites involved:
-Lesion in skin:
= Thickening of skin and multiple, symmetric, macular, papular, or nodular
lesions, Nodular skin lesions may ulcerate. Most skin lesions—hypoesthetic or
anesthetic
+ More severe involvement of the cooler areas of skin (ex: earlobes, wrists, elbows,
and knees, and feet], than warmer areas (ex: axilla and groin)
« With progression, the nodular lesions in the face and earlobes may coalesce to
produce a lion like appearance known as leonine facies. This may be
accompanied by loss of eyebrows and eyelashes.
-peripheral nerves:
= Ulnar and peroneal nerves—symmetrically invaded with mycobacteria
+ Loss of sensation and trophic changes in the hands and feet may follow the
damage to the nerves
~Testes: severely involved—destruction of the seminiferous tubules—sterility
-Other sites:
= Anterior chamber of the eye—blindness
= Upper airways—chronic nasal discharge and voice change
-Microscopy of skin lesion:
= Flattened epidermis—epidermis is thinned and flattened (loss of rete ridges) over
the nodules
= Grenz (clear] zone: a characteristic narrow, uninvolved dermis (normal collagen|--
separates the epidermis from nodular accumulations of macrophages
+ Lepra cells: nodular lesions contain large aggregates of lipid-laden foamy
macrophages (lepra cells, Virchow cells), filled with aggregates (globi) of acid fast
lepra bacilli (M.leprae)
+ Fite-Faraco (acid fast | stain—shows numerous leprabacilli (“red snappers”
within the foamy macrophages. They may be arranged in a parallel fashion like
cigarettes in a pack,
+ Due to the presence of numerous bacteria, lepromatous leprosy—muttibacillary
In advanced cases, M. leprae—in sputum and blood
Individuals with intermediate forms of disease—borderline leprosy
3. Borderline leprosy:
+ Borderline tuberculoid(BT): shows epithelioid cells and numerous lymphocytes
with a narrow clear subepidermal zone. Lepra bacilli—few—in nerves
+ Borderline lepromatous (BL): shows predominantly histiocytes, few epithelioid
cells and lymphocytes. Numerous lepra bacilli
+ Mid-borderline (BB) dimorphic form—sheets of epithelioid cells w/o any giant
cells, Few lymphocytes in the perineum. Lepra bacilli_mostly in nerves
4. Indeterminate leprosy: non-specific and few findings help in suspecting leprosy.
Include:
i, Local infiltration of lymphocytes or mononuclear cells surrounding the skin
adnexa (ex: hair follicles and sweat glands] or around blood vessels
ii, Involvement of nerve involvement (if seen strongly favors the diagnosis) and
ili, Finding of lepra bacilli (which confirms the diagnosis]
LEPROMIN TEST:
Not a diagnosis test for leprosy.
Used for classifying leprosy based on the immune response
Procedure: an antigen extract of M.leprae called leprornin is intradermally injected.
Mitsuda reaction’
Reaction:
+ Early positive reaction—as an indurated area in 24-48 hrs - Fernandez reaction
+ A delayed granulomatous reaction appearing after 3-4 weeks—Mitsuda reaction
Interpretation:
+ Lepromatous leprosy—shows negative lepromin test due to suppression of cell
mediated immunity
+ Tuberculoid leprosy—shoes positive lepromin test because of delayed
hypersensitivity reaction.
Lepromatous leprosy:
1. Leonine facies
2. Low resistance
3. Thinned epidermis
4. Grenz zone
5. Lepra cells filled with acid-fast bacilli
6. Lepromin test negative.
Uses of lepromin test
1. Classification of leprosy
2. Evaluation of cell-mediated immunity status in patient
3. Know the prognosis
Reactions in leprosy:
Immunity in leprosy may change spontaneously or following treatment
+ Type I reaction:
-borderline leprosy—most unstable form of leprosy where immune status may
shift up or down.
2 types:
@ Upgrading reactions: If immunity improves, the disease may shift towards
tuberculoid leprosy.
‘ Downgrading reaction: If the immunity decreases, the disease moves towards
lepromatous leprosy
+ Type II reaction or erythema nodosum leprosum:
-mostly in lepromatous leprosy—when on treatment
-clinical features: (1] Tender red plaque or nodules and (2) fever, malaise and
arthralgia
-Microscopy:
@ Necrotizing vasculitis
© Lepra bacilli in the foamy macrophages
omatos nd ier ea.
Symmetical, multiple idefined, macular, Asymmetrical, hypopigmented, wel
fined macular
nodular
Leonine facies, los of eyebrows, Minimal disfigurement
pendulous earlobes, clawhands saddle
Nerve involvement Seen, but with less severe sensory loss Common with sensory disturbances
than tuberculid
Microscopy of skin lesions
Type oflesion Nodular or difuse collections of Lepra__Noncaseating granulomas composed of.
‘els wthin dermis epithelioid cells and giant cells
‘Grenz/clearzone between inflammatory Present ‘Absent
‘ells and epidermis
Lepra bac Plenty within thelepraclisas globular Rareifany
masses (glob)
Bacilary index 4ors °
‘Other features
Immunity Suppeessed low resistance Good immunityhigh resistance
Lepromin test Negative Postive
Diagnosis of Leprosy ‘Morphological index (i):
+ Staining of smears or skin biopsy + Measure of number of acid fst bacil (AFB) n skin scrapings
= ‘eid fast Ziehl Neeser stain ‘that stan uniformly bright.
= Fte-Faraco stain + Contelates with viablty of AFB.
+ Molecular method—PCR
Bacteriological index (8): Quantifis M leprae in tissue or smears It scored from 1+ to 6+ ange from 1 to 10 baci per 100 fils to >
1000 pe fed) as mutbacilay leprosy whereas Blof +s termed paucbacilary.
DIAGNOSIS OF LEPROSY:
1. Clinical examination:
+ Sensory testing:
+ Examination of peripheral nerve
2. Demonstration of acid fast bacilli:
+ Skin smears prepared by slit and scrape method
+ Mycobacterium leprae—demonstrated in tissue sections, in split skin smears by
splitting the skin and in nasal smears by the following techniques
-Acid fast [Z-N]) staining
-Fite-Faraco staining procedure—modification of ZN procedure and is considered
vetter for more adequate staining of tissue sections
-Gomori methenamine silver (GMS} staining can also be employed
+ Nasal swabs stained by ZN method:
Staining procedure similar to M. tuberculosis but can be decolorized by lower
concentration (5%| of sulfuric acid (less acid-fast)
3. Skin biopsy: Fite-Faraco staining procedure is a modified ZN procedure and is
better for tissue sections.
4. Nerve biopsy
5, Molecular method: Polymerase chain reaction (PCR)
SYPHILIS:
+ IgM antibodies to PGL-1 antigen: Found in 95% of patients of lepromatous
leprosy and in 60% of tuberculoid leprosy
+ Caused by spirochete Treponema pallidum
+ Spirochetes—gram ve, slender corkscrew shaped bacteria covered in a
membrane called outer sheath—may mask its antigens from the host immune
response
+ Syphilis (Ilues|-- chronic, STD caused by Treponema pallidum.
ETIOLOGY:
Treponema pallidum
+ Thin, delicate, corkscrew shaped spirochete—10um long with tapering ends—10
regular spirals
Actively motile—rotation round the long axis, backward and forward motion
Can't be grown in artificial media
Doesn't stain with ordinary bacterial stains—too slender to be seen in gram stain
Visualized by silver stains, dark field examination and immunofluorescence
techniques.
+ Source of infection: open lesion of primary or secondary syphilis. Lesions in the
mucous membranes or skin of the genital organs, rectum, mouth, fingers, or
nipples.
+ Mode of transmission:
-sexual contact
-Transplacental transmission—congenital syphilis
-Blood transfusion
-Direct contact: with the open lesion—rare
BASIC MICROSCOPIC LESION:
Consists of
+ Mononuclear inflammatory infiltrate: predominantly of plasma cells and
lymphocytes
+ Obliterative endarteritis: characteristic obstructive vascular lesion in which
mononuclear infiltrates surround small arteries and arterioles (periarteritis)
STAGES OF SYPHILIS:
+ Treponema pallidum—passes from the site of inoculation to regional lymph nodes
and enters to the systemic circulation and disseminate throughout the body
+ Can be congenital or acquired
+ Course of acquired syphilis - 3 stages:
i, Primary syphilis
ii, Secondary syphilis
ili, Tertiary syphilis
seine come
a sai
=..| See |e ro
Soo lac Seiagsme | jeter
Panioss iymehadenopaty moore — Peteceis 3 Eighth-nerve deainess,
ig Ate Vasious
PRIMARY SYPHILIS.
Develops about 3 weeks after contact with an infected individual and the lesion is
primary chancre.
Primary Chancre:
Classical lesion of primary syphilis
+ Sites: penis or scrotum in men and cervix, vulva and vaginal wall in women. May
also be seen in the anus or mouth
+ Gross features: single, firm , nontender (painless), slightly raised , red papule
(chancre] up to several centimeters in diameter. Erodes to create a clean based
shallow ulcer. Because of the induration surrounding the ulcer, it is designated
as hard chancre
+ Demonstration of treponema: plenty of treponemes demonstrated in chancre by
i. Silver stains (ex: Warthin-Starry stain] or
ii, Immunofluorescence techniques or
ili, Dark field examination
+ Microscopy:
-Mononuclear infiltration: consisting of plasma cells, with scattered macrophages
and lymphocytes—also seen surrounding the blood vessels [periarteritsis}
Blood vessels with endarteritis: endothelial cell proliferation which progresses to
intimal fibrosis.
Primary syphilis: Chancre is the painless lesion seen in the external genitalia with
regional lymphadenitis.
Regional Lymphadenitis It is due to nonspecific acute or chronic inflammation.
+ Treponemes may spread throughout the body by blood and lymphatics even
before the appearance of the chancre.
+ Symptoms: Usually, painless and often unnoticed
+ Fate: It heals in 3-6 weeks with or without therapy. Secondary Syphilis
Secondary syphilis: 1. Mucocutaneous lesions 2. Generalized lymphadenopathy
SECONDARY SYPHILIS:
Secondary syphilis
1, Mucocutaneous lesions
2. Generalized lymphadenopathy
Develops 2-10 weeks after the primary chancre in approx 75% untreated patients.
Manifestations: due to systemic spread and proliferation of the spirochetes within the
skin and mucocutaneous tissues.
MUCOCUTANEOUS LESIONS:
Painless, superficial lesions—contain spirochetes—infectious
Skin lesion
+ Skin rashes: consist of discrete red-brown macules less than 5 mm in diameter—
may be scaly / pustular/ annular—more frequent on the palms of the hands, or
soles of the feet
+ Condylomata lata: broad based, elevated plaques with numerous spirochetes—
seen in moist areas of the skin, such as the anogenital region perineum, vulva,
and scrotum], inner thighs, and axillae.
Mucosal lesion:
Oral cavity or vagina as silvery-gray superficial erosions—contain numerous
T pallidum-- highly infectious.
Microscopy: similar to primary chancre, Le. infiltration by plasma cells and
endarteritis obliterans.
Painless lymphadenopathy:
Involves epitrochlear nodes and shows plenty of spirochetes
Symptoms: Mild fever, malaise, and weight loss—common in secondary syphilis—may
last for several weeks. Lesions subside even w/o treatment.
‘Treponema pallidurn—identified in lesions of primary or secondary syphilis
TERTIARY SYPHILI
Involves mainly CVS, CNS and focal lesions called gumma.
+ After the lesions of secondary syphilis have subsided patients enters an
asymptomatic latent phase of the disease
+ Latent period—s yrs or more even decades), but spirochetes continue to
multiply—rare if patient gets adequate treatment, but can occur in about one-
third of untreated patients
+ Focal ischemic necrosis due to obliterative endarteritis is responsible for many of
the processes associated with tertiary syphilis
Manifestations: three main manifestations—cardiovascular syphilis, neurosyphilis,
and so-called benign tertiary syphilis—may occur alone or in combination.
CARDIOVASCULAR SYPHILIS:
Most frequently invoives the aorta—syphilic aortitis
+ Syphilitic aortitis: more than 80% of cases of tertiary disease, and affects the
proximal aorta
+ Saccular aneurysm and aortic valve insufficiency:
-Occlusion of the vasa vasorum due to endarteritis leads to necrosis and scarring
of the aortic media, causing a loss of elasticity, strength and resilience.
~ Gradual weakening and slow progressive dilation of the aortic root and arch,
causes aortic valve insufficiency and aneurysms of the proximal aorta. Syphilitic
aneurysms are saccular and seen in the ascending aorta, which is unusual site
for the more common atherosclerotic aneurysms
~ On gross examination, the aortic intima appears rough and pitted (tree-bark
appearance}
+ Myocardial ischemia: Narrowing of the coronary artery ostia (at the origin from
aorta] caused by subintimal scarring may lead to myocardial ischemia/ infarction.
Cardiovascular syphilis: Involves proximal aorta and lead to saccular aneurysm of
aorta and aortic valve incompetence. Syphilis never causes aortic stenosis
NEUROSYPHILIS: asymptomatic or symptomatic
Asymptomatic neurosyphilis: detected by CSF examination—shows pleocytosis,
increased numbers of inflammatory cells), elevated protein levels, or decreased
glucose.
Antibodies also detected in CSF—most specific test for neurosyphilis
Symptomatic disease: takes one of the several forms
Chronic meningovascular disease: chronic meningitis—involves base of brain,
cerebral convexities and spinal leptomeninges
+ Tabes dorsalis: demyelination of posterior column, dorsal root and dorsal root
ganglia.
+ General paresis of insane: generalized brain parenchymal disease with
dementia—general paralysis of insane
BENIGN TERTIARY SYPHILIS
+ Formation of nodular lesions called gummas in any organ or tissue
+ Gammas reflect development of delayed hypersensitivity to the spirochete
+ Gummas—very rare—found in patients with AIDS
SYPHILITIC GUMMAS:
Central area of coagulative necrosis surrounded by plump, palisading macrophages,
fibroblasts and plenty of plasma cells
Gumma
May be single or multiple
+ White-gray and rubbery
+ Vary in size from microscopic lesions to large tumor-like masses
+ In most organs but mainly involve:
-Skin, subcutaneous tissue and the mucous membranes of the upper airway and
mouth,
~Bone and joints: It causes local pain, tenderness, swelling, and sometimes
pathologic fractures
~ In the liver, scarring due to gummas may cause a distinctive hepatic lesion
known as hepar lobatum.
+ Microscopy: Center of the gummas show coagulative necrosis -surrounded by
plump, palisading macrophages, fibroblasts and plenty of plasma cells
‘Treponemes are scant in gummas
CONGENITAL SYPHILIS:
TRANSPLACENTAL TRANSMISSIOI
+ T.Pallidum can cross placenta and spread from infected mother to the fetus
[during pregnancy),
+ Transmission occurs, when mother is suffering from primary or secondary
syphilis (when the spirochetes are abundant, Because of routine serologic testing
for syphilis in done in all pregnancies) congenital syphilis is rare
Manifestations: divided into:
1. Intrauterine death and perinatal death
2. Early (infantile ) syphilis: first 2 yrs of life—nasal discharge and congestion
(snuffles}
+ A desquamating or bullous eruption/rash—- epidermal sloughing of the skin,
mainly in the hands and feet, around mouth and anus
+ Skeletal abnormalities
-Syphilitic osteochondritis: Inflammation of bone and cartilage is more distinctive
inthe nose. Destruction of the vomer causes collapse of the nasal bridge—saddle
nose deformity
-Syphilitic periostitis: involves the tibia—causes excessive new bone formation on
the anterior surfaces and leads to anterior bowing or saber shin
+ Liver: diffuse fibrosis in the liver—hepar lobaturn
+ Lungs: diffuse interstitial fibrosis—lungs appear pale and airless (pneumonia
alba]
3. Late (tardive) syphilis: manifests 2 yrs after birth. About 50% of untreated
children with neonatal syphilis will develop late manifestations
+ Manifestations: distinctive manifestation is Hutchinson's triad.
Interstitial keratitis
-Hutchinson's teeth: like small screw-drivers or peg-shaped incisors, with
notches in the enamel
-Eighth-nerve deafness
LABORATORY DIAGNOSIS:
Immunofluorescence of exudate from the chancre—impt for diagnosis in primary
syphilis
+ Microscopy and PCR useful
+ Serological tests
-Nontreponemal antibody tests: measure antibody to cardiolipin, a phospholipid
present in both host tissues and T. pallidum,
+ These antibodies—detected by the rapid plasma reagin and Venereal disease
research laboratory (VDRL] tests
+ False positive VDRL test: found in certain acute infections, collagen vascular
diseases (ex: systemic lupus erythematosus], drug addiction, pregnancy,
hypergammagiobulinemia of any cause, and lepromatous leprosy.
+ Antitreponemal antibody tests: measure antibodies which react with T.pallidum.
Include
-Fluorescent treponemal antibody absorption test [FTA] - Microhemagglutination
assay for T. pallidum antibodies.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- CONSPOSTERDocument1 pageCONSPOSTERSara SultanaNo ratings yet
- CADAVER As Our First TeacherDocument1 pageCADAVER As Our First TeacherSara Sultana80% (5)
- Document From Sara SultanaDocument49 pagesDocument From Sara SultanaSara SultanaNo ratings yet
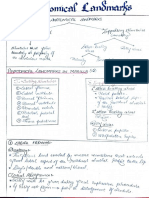
- Anatomical Landmarks - PCPDocument14 pagesAnatomical Landmarks - PCPSara Sultana0% (1)
- Cell Injury, Cell Death and AdaptationsDocument28 pagesCell Injury, Cell Death and AdaptationsSara SultanaNo ratings yet
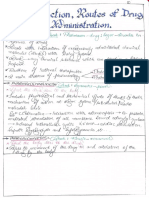
- Introduction, Routes of Drug Administration (Notes)Document24 pagesIntroduction, Routes of Drug Administration (Notes)Sara Sultana100% (1)
- William Shakespeare PoemsDocument471 pagesWilliam Shakespeare PoemsSara SultanaNo ratings yet
- Sl. No. Chapter Name Checked Questions 1 2 3 4Document4 pagesSl. No. Chapter Name Checked Questions 1 2 3 4Sara SultanaNo ratings yet
- General Anatomy Syllabus PDFDocument3 pagesGeneral Anatomy Syllabus PDFSara SultanaNo ratings yet
- Why Do We Fall IllDocument11 pagesWhy Do We Fall IllSara SultanaNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)