Professional Documents
Culture Documents
10.1038@s41598 020 65019 8
Uploaded by
bouchra8blsOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
10.1038@s41598 020 65019 8
Uploaded by
bouchra8blsCopyright:
Available Formats
www.nature.
com/scientificreports
OPEN An Extended Duration of the
Pre-Operative Hospitalization is
Associated with an Increased Risk
of Healthcare-Associated Infections
after Cardiac Surgery
Patrick Sulzgruber1,5 ✉, Sebastian Schnaubelt 2,5, Lorenz Koller1, Günther Laufer3,
Arnold Pilz1, Niema Kazem1, Max-Paul Winter1, Barbara Steinlechner4, Martin Andreas3,
Tatjana Fleck3, Klaus Distelmaier1, Georg Goliasch1, Aurel Toma1, Christian Hengstenberg1 &
Alexander Niessner1
Nosocomial infections are a common complication in clinical practice with major impact on surgical
success and patient outcome. The probability of nosocomial infections is rapidly increasing during
hospitalization. Therefore, we investigated the impact of a prolonged pre-operative hospital stay on
the development of post-operative infection. Within this prospective observational study, 200 patients
scheduled for elective cardiac surgery were enrolled. Patients were followed during hospital admission
and screened for the development of nosocomial infection. Logistic regression analysis was used to
assess the impact of a prolonged pre-operative hospital stay on the development of infection. A total of
195 patients were suitable for the final analysis. We found a strong and direct association of the duration
of pre-operative hospital stay and the number of patients developing infection (+23.5%; p = 0.006).
Additionally, the length of patients’ pre-operative hospital stay was independently associated with
the development of post-operative nosocomial infection, with an adjusted OR per day of 1.38 (95%CI:
1.02–1.86; p = 0.036). A prolonged pre-operative hospital stay was significantly associated with the
development of nosocomial infection after cardiac surgery. Those findings need to be considered in
future clinical patient management in order to prevent unnecessary antibiotic use and potential harm to
patients.
Healthcare-associated infections (HAIs) are a common complication in clinical practice associated with increased
hospitalization-related costs and worse patient outcome. Recent data of the World Health Organization (WHO)
revealed a global burden of HAIs of up to 15% among all hospitalized individuals, with more than 30% in inten-
sive care patients1. Of alarming importance, the development of HAI proved to be directly associated with both
short and long-term mortality in affected individuals2. It is well established that the probability of HAI develop-
ment rapidly increases during hospital stay in general, and data also suggests the pre-operative length of stay to
be a risk factor3,4. Especially extensive surgical procedures such as cardiac surgical interventions proved to have
an increased risk for the development of infectious disease during post-operative patient care5, in particular for
mediastinitis6. Despite the achievements of disinfection, sterilization and antibiotic therapy, the incidence of
HAIs is still increasing within the western society. This subsequently underlines a major need to identify potential
influencing and easily adjustable factors for HAI development. Whereas it is well-known that infection influences
the length of hospital stay, vice-versa data on the impact of the duration of the pre-operative hospitalization has
1
Division of Cardiology, Department of Internal Medicine II, Medical University of Vienna, Vienna, Austria.
2
Department of Emergency Medicine, Medical University of Vienna, Vienna, Austria. 3Division of Cardiac Surgery,
Department of Surgery, Medical University of Vienna, Vienna, Austria. 4Department of Anesthesia, General Intensive
Care and Pain Management, Medical University of Vienna, Vienna, Austria. 5These authors contributed equally:
Patrick Sulzgruber and Sebastian Schnaubelt. ✉e-mail: patrick.sulzgruber@muv.ac.at
Scientific Reports | (2020) 10:8006 | https://doi.org/10.1038/s41598-020-65019-8 1
www.nature.com/scientificreports/ www.nature.com/scientificreports
Figure 1. The incidence of post-operative healthcare-associated infections significantly increased with
increasing prolongation of a pre-operative hospitalization (p = 0.006).
not been fully investigated so far7. It seems intuitive that an extended pre-operative hospitalization increases
the individual exposition to potential pathogens, posing an elevated risk for HAIs in the post-operative state8.
Therefore, we aimed to investigate the impact of a prolonged pre-operative hospital stay on HAI development
after cardiac surgery.
Methods
In this prospective cohort study, a total of 200 patients with structural heart disease and/or stable coronary vessel
disease (CVD) scheduled for elective cardiac valve and/or coronary artery bypass graft surgery (CABG) at the
Department of Cardiac Surgery of the Medical University of Vienna (Austria) were enrolled. Enrollment was
conducted between 5/2013 and 4/2015 at the time of the patients’ hospital admission. All patients were contin-
uously followed up during the entire hospitalization and screened for the development of any nosocomial infec-
tion. HAI was defined in accordance to established criteria of the International Nosocomial Infection Control
Consortium (INICC) as an evident infection with the associated clinical symptoms developed after day three
of hospitalization9. The study protocol complies with the Declaration of Helsinki and was approved by the local
ethics committee of the Medical University of Vienna (EK 1110/2013). All patients gave written informed consent
for participation. Data reporting was performed according to the STROBE and MOOSE guidelines.
Data acquisition. Patient data were assessed at the time of study inclusion and inserted into a pre-defined
record abstraction form. Values of routine laboratory parameters were assessed at the time of hospital admission,
immediately after surgery and prior to hospital discharge. Levels of C-reactive protein (CRP) were assessed daily
during the hospital stay to elucidate the baseline level and the maximum increase after surgery in accordance to
the local laboratory standards of the Medical University of Vienna (Roche Diagnostics, Switzerland).
Statistical analysis. For statistical analysis patients were stratified into groups depending on their length
of pre-operative hospital stay in ≤ 2 days (surgery on time), 2–7 days (delayed surgery) and >7 days (extensive
delay of surgery). Categorical data are presented as counts and percentages and were analyzed using a test for
linear association (Maentel–Haenszel chi-square test). Continuous data are illustrated as medians and the respec-
tive interquartile range using Kruskal–Wallis test for testing within the subgroups. A logistic regression model
for the association of the duration of the patients’ pre-operative hospitalization on the development of HAI was
performed. Continuous variables were log-transformed prior to their analysis in the regression model in order to
adjust data more closely to normal distribution. Data were presented as odds ratio (OR) and the respective 95%
confidence interval (CI) per one day increase for continuous variables as the standard outcome value for logistic
regression models. The multivariate model was adjusted for “type of surgery” and “Euro Score II”. Two-sided
p-values of <0.05 were chosen as statistically significant. Statistical analysis was performed using SPSS 22.0 (IBM,
USA).
Results
Five out of 200 enrolled participants (2.5%) already presented with elevated CRP values and/or fever prior to
the cardiac surgical procedure and were therefore excluded for the final analysis, resulting in 195 individuals.
After stratification according to the duration of the pre-operative hospital stay, we found that 28.7% of patients
(n = 56) received surgical intervention on time (<2 days). One third of all individuals (32.3%; n = 63) had a pro-
longed pre-operative stay (3–7 days) and 39.0% had an extensive delay (>7 days) – with a total median duration
of pre-operative hospitalization of 14 days (Supplementary Table). Patients were followed-up daily during the
pre-operative course of hospitalization. There were no events detected that might explain both an increased risk
for HAI or prolongation of the pre-operative hospitalization.
A total of 75 patients (38.5%) developed any infection after cardiac surgery. We found a strongly increased
overall infection rate with prolongation of pre-operative hospitalization when comparing patients that received
a surgical intervention on time and individuals with an extensive delay (28.5% vs. 52.0%; p = 0.006; Fig. 1).
Scientific Reports | (2020) 10:8006 | https://doi.org/10.1038/s41598-020-65019-8 2
www.nature.com/scientificreports/ www.nature.com/scientificreports
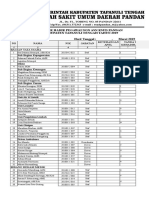
Total ≤2 days 3–7 days >7 days p-value OR (95% CI) p-value *Adj. OR (95%CI) p-value
Any Infection, n (%) 75 (38.5) 16 (28.5) 20 (31.7) 39 (52.0) 0.006 1.45 (1.08–1.95) 0.013 1.33 (1.01–1.12) 0.039
Surgical Site Infection, n (%) 9 (4.6) 0 (–) 3 (4.8) 6 (7.9) 0.034 1.57 (0.76–3.22) 0.222 ns.
Central Venous Catheter Infection, n (%) 37 (19.0) 9 (16.1) 10 (15.9) 18 (23.7) 0.245 1.19 (0.84–1.71) 0.319 ns.
Pneumonia, n (%) 17 (8.7) 4 (7.1) 2 (3.2) 11 (14.5) 0.049 1.27 (0.76–2.09) 0.358 ns.
Urinary Tract Infection, n (%) 24 (12.3) 6 (10.7) 6 (9.5) 12 (15.8) 0.346 1.19 (0.78–1.83) 0.417 ns.
Mortality, n (%) 6 (2.6) 0 (—) 0 (—) 6 (6.6) 0.019 1.13 (1.04–1.22) 0.003 1.19 (0.98–1.17) 0.110
Table 1. Nosocomial Infections and In-Hospital Mortality for the entire study population and stratified by days
of pre-operative hospitalization and Logistic Regression Analysis for the Association of the Total Pre-Operative
Hospital Stay on Infection and Mortality. Categorical data are presented as counts and percentages, continuous
data as medians and IQRs. Categorical data are analyzed using a test for linear association (Maentel–Haenszel
chi-square test), continuous data using Kruskal–Wallis test for testing within the subgroups. Logistic regression
model for the association of the total duration of the patients’ pre-operative hospital stay on the development of
infections and major adverse events within the total study population. Odds ratios (OR) for continuous variables
refer to an increase per day. *The multivariate model was adjusted for: Type of surgery and EuroScore II.
Interestingly, stratified by the respective types of infection, there was a significant absolute increase in surgical site
infection (0.0% vs. 7.9%; p = 0.034) and pneumonia (7.1% vs. 14.5%; p = 0.049). No difference was found for cen-
tral venous catheter infections (p = 0.245) and urinary tract infections (p = 0.346). Moreover, the duration of the
pre-operative hospitalization proved to be directly associated with HAIs with a crude OR per day of 1.45 (95%CI:
1.08–1.95; p = 0.013). The observed effect remained stable even after adjustment for potential cofounders, show-
ing a strong and independent association with HAIs (adjusted OR per day of 1.33 [95%CI:1.01–1.12; p = 0.039]).
Out of the entire study population, a total of 6 individuals died after the surgical procedure. We found that the
duration of the pre-operative hospitalization was significantly associated with in-hospital mortality with a crude
OR of 1.13 per day (95%CI: 1.04–1.22; p = 0.003). However, this effect was lost after adjustment in the multivar-
iate model (Table 1).
Discussion
Through our analysis, we could show a strong and independent association of the duration of pre-operative hos-
pitalization and the development of post-operative HAIs in the special population of patients undergoing elective
cardiac surgery. It is well known that HAIs have an impact on the need for prolonged hospitalization, higher
readmission rates and increased mortality from both a short- and also long-term perspective10,11. Moreover, HAIs
pose a considerable economic impact on healthcare systems, and their prevention is cost-effective12. Leung et al.
could demonstrate that patients with a longer preoperative length of stay are more prone to mediastinitis after
cardiac surgery6. However, the association of the length of pre-operative hospital stay as potential factor for gen-
eral infection control in cardiac surgery patients has not yet been fully described.
Evidence-based approaches were implemented in daily clinical routine, aiming at a reduction of infection
rates and improvement of the primary patient outcome5,13–15. Many of those interventions follow an antimicrobial
approach. In accordance to local referral patterns, nasal decontamination and perioperative antibiotic prophy-
laxis with an increased dose are routinely performed16,17. Similarly, the rate of post-operative sternal infections
could be significantly reduced with local antibiotic administration18.
Patients developing HAI pose a general need for an aggravated antibiotic therapy. Facing an increasing dis-
semination of multi-resistant bacteria among healthcare institutions – mainly due to unjustified and potential
unnecessary antibiotic treatment – the prevention of HAIs poses an essential benefit against the development of
antibiotic resistances. Considering the global burden of HAIs and its strong association with patient outcome,
identification of modifiable risk factors for infection development are crucial both from a patient-centered-, and
a global environmental perspective of nosocomial infection control.
In this regard, a wide range of predisposing factors for the development of HAIs have been identified in litera-
ture, including diabetes, impaired renal function, obesity or female gender19–21. Those factors are non-modifiable
patient characteristics that increase the odds for HAI development. Therefore, the identification of adjustable
influencing variables seems of utmost importance to ensure patients’ safety and favorable outcome - such as the
limitation of the duration of the pre-operative hospitalization of patients.
Given the fact that all enrolled individuals in this analysis had medical approval for the respective elective sur-
gery at the time of admission, a delay based on a poor medical condition cannot be assumed within this analysis.
The observation that patients presenting with a higher EuroScore II experienced a prolonged pre-operative hospi-
talization, relates probably to the increased pre-operative work-up (consisting of transthoracic echocardiography,
aortic CT-scan, lung function testing, and coronary angiography). However, an optimization of variables such
as smoking status or glycemic control that is already achieved prior to hospital admission could help reducing
hospital stay duration22.
In terms of pre-operative risk stratification, we found that patients spending longer time periods in the hos-
pital in the pre-operative phase showed a tendency towards a higher Euro Score. Because of the potential asso-
ciation with patient outcome, we adjusted our regression model. Here, this result still proved to be significant.
The Euro Score as a surrogate for “riskier” surgery is a potentially adjustable risk factor - for instance this could
be addressed through a flexible team formation with only experienced surgeons operating on patients with high
Scientific Reports | (2020) 10:8006 | https://doi.org/10.1038/s41598-020-65019-8 3
www.nature.com/scientificreports/ www.nature.com/scientificreports
score values. Therefore, the composition of the surgical team could possibly influence patients’ duration of sur-
gery, hospital stay times, and also infection rates.
At the same time, a lack of both operating room and intensive care capacities for a large patient number
increases the preoperative waiting time. This could yet again lead to an increased infection rate due to various
reasons such as prolonged fasting and following poor nutritional status6. Considering the results of this analysis,
a pre-hospitalization of more than 7 days is not justifiable given the increased risk of infection. Organizational
requirements and referral patterns considering a pre-operative work-up of especially high-risk patients should be
adapted to these results and implemented in heart-team meetings of cardiologists and cardiac surgeons for ideal
patient care.
Limitations. The major limitation of this analysis represents its single center setting that alters the overall pic-
ture of our results. However, taking into consideration that patients were enrolled during a two-year observation
period, we might overcome a potential selection bias (e.g. only depicting the work of a specific team that is more
prone to postoperative infection). Moreover, our patient collective only underwent cardiac surgery – therefore,
our results cannot be applied to a general population of surgical patients. Another potentially limiting factor
is that we could not provide details on the exact timing or causative agent of infection. This could have given
additional information and data to discuss23. Lastly, other factors apart from the listed could have influenced an
increased risk for HAI, for example deconditioning in the elderly, were not taken into account and could have
biased results. Such other potentially modifiable factors should be subject of future research.
Conclusion
The duration of the pre-operative hospitalization is a potentially adjustable factor in clinical practice. Therefore, an
optimization of internal resources as well as the enhancement of operating room and intensive care capacities may
significantly reduce the rates of nosocomial infections, extensive antibiotic drug use and hospitalization-related
mortality in patients undergoing cardiac surgery. This can increase favorable long-term patient outcome.
Received: 23 July 2019; Accepted: 4 February 2020;
Published: xx xx xxxx
References
1. WHO, World Health Organization Report on the Burden of Endemic Health Care-Associated Infection Worldwide. WHO Library
Cataloguing-in-Publication Data, (WX 167) (2011).
2. Koch, A. M. et al. Mortality related to hospital-associated infections in a tertiary hospital; repeated cross-sectional studies between
2004–2011. Antimicrob Resist Infect Control 4, 57 (2015).
3. Zimlichman, E. et al. Health care-associated infections: a meta-analysis of costs and financial impact on the US health care system.
JAMA Intern Med 173(22), 2039–46 (2013).
4. Pereira, H., Rezende, E. & Couto, B. Length of preoperative hospital stay: a risk factor for reducing surgical infection in femoral
fracture cases. Rev Bras Ortop 50(6), 638–646 (2015).
5. Gelijns, A. C. et al. Management practices and major infections after cardiac surgery. J Am Coll Cardiol 64(4), 372–81 (2014).
6. Sang, S. et al. Preoperative hospital length of stay as a modifiable risk factor for mediastinitis after cardiac surgery. J Cardiothorac
Surg 8, 45 (2013).
7. Gulack, B. C. et al. Secondary surgical-site infection after coronary artery bypass grafting: A multi-institutional prospective cohort
study. J Thorac Cardiovasc Surg 155(4), 1555–1562 (2018).
8. Bueno Cavanillas, A. et al. Preoperative stay as a risk factor for nosocomial infection. Eur J Epidemiol 7(6), 670–6 (1991).
9. Rosenthal, V. D. International Nosocomial Infection Control Consortium (INICC) resources: INICC multidimensional approach
and INICC surveillance online system. Am J Infect Control 44(6), 81–90 (2016).
10. Robich, M. P. et al. Prolonged effect of postoperative infectious complications on survival after cardiac surgery. Ann Thorac Surg
99(5), 1591–9 (2015).
11. Mazzeffi, M. et al. In-hospital mortality after cardiac surgery: patient characteristics, timing, and association with postoperative
length of intensive care unit and hospital stay. Ann Thorac Surg 97(4), 1220–5 (2014).
12. Kaier K., Wolkewitz M., Hehn P., Mutters N. T. & Heister T. The impact of hospital-acquired infections on the patient-level
reimbursement-cost relationship in a DRG-based hospital payment system. Int J Health Econ Manag. Epub ahead of print (2019).
13. Berrios-Torres, S. I. et al. Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infection 2017.
JAMA Surg. 152(8), 784–791 (2017).
14. Boltz, M. M. et al. Hospital costs associated with surgical site infections in general and vascular surgery patients. Surgery. 150(5),
934–42 (2011).
15. Perrault, L. P. et al. A Prospective Multi-Institutional Cohort Study of Mediastinal Infections After Cardiac Operations. Ann Thorac
Surg 105(2), 461–468 (2018).
16. Liu, Z. et al. Nasal decontamination for the prevention of surgical site infection in Staphylococcus aureus carriers. Cochrane
Database Syst Rev. 5, Cd012462 (2017).
17. Liu, Y. et al. The Effects of Diabetes Mellitus in Patients Undergoing Off-Pump Coronary Artery Bypass Grafting. Biomed Res Int
2016, 4967275 (2016).
18. Andreas, M. et al. Internal mammary artery harvesting influences antibiotic penetration into presternal tissue. Ann Thorac Surg
95(4), 1323–9 (2013).
19. Andreas, M. et al. Direct sternal administration of Vancomycin and Gentamicin during closure prevents wound infection. Interact
Cardiovasc Thorac Surg 25(1), 6–11 (2017).
20. Abuzaid, A. A., Zaki, M. & Al Tarief, H. Potential Risk Factors for Surgical Site Infection after Isolated Coronary Artery Bypass
Grafting in a Bahrain Cardiac Centre: A Retrospective, Case-Controlled Study. Heart Views 16(3), 79–84 (2015).
21. Meszaros, K. et al. Risk Factors for Sternal Wound Infection After Open Heart Operations Vary According to Type of Operation.
Ann Thorac Surg 101(4), 1418–25 (2016).
22. Emara, K., Hirose, C. B. & Rogero, R. What preoperative optimization should be implemented to reduce the risk of surgical site
infection/periprosthetic joint infection (SSI/PJI) in patients undergoing total ankle arthroplasty (TAA)? Foot Ankle Int. 40(1_suppl),
6S–8S (2019).
23. Wolkewitz, M., Schumacher, M., Ruecker, G., Harbarth, S. & Beyersmann, J. Estimands to quantify prolonged hospital stay
associated with nosocomial infections. BMC Med Res Methodol 19(1), 111 (2019).
Scientific Reports | (2020) 10:8006 | https://doi.org/10.1038/s41598-020-65019-8 4
www.nature.com/scientificreports/ www.nature.com/scientificreports
Author contributions
All listed authors have made substantial contributions to the conception or the design of the manuscript. PS
and SS have acquired and analyzed data and created the overall manuscript. L.K., A.P., N.K., M.P.W., M.A., T.F.,
K.D., G.G. and A.T. have further analyzed and interpreted data and made substantial revisions of the manuscript.
G.L., B.S., C.H. and A.N. have supervised the manuscript creation process and have designed and crafted the
final version of the manuscript. All listed authors have agreed to be accountable for their contribution and have
approved the submitted version of the manuscript.
Competing interests
The authors declare no competing interests.
Additional information
Supplementary information is available for this paper at https://doi.org/10.1038/s41598-020-65019-8.
Correspondence and requests for materials should be addressed to P.S.
Reprints and permissions information is available at www.nature.com/reprints.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and
institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International
License, which permits use, sharing, adaptation, distribution and reproduction in any medium or
format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Cre-
ative Commons license, and indicate if changes were made. The images or other third party material in this
article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the
material. If material is not included in the article’s Creative Commons license and your intended use is not per-
mitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the
copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
© The Author(s) 2020
Scientific Reports | (2020) 10:8006 | https://doi.org/10.1038/s41598-020-65019-8 5
You might also like
- Swedish Massage InfoDocument5 pagesSwedish Massage InfoJoy CelestialNo ratings yet
- SHCDocument58 pagesSHCElizabethmike100% (4)
- Prevention of Hospital-Acquired Infections A Practical Guide 2nd EditionDocument72 pagesPrevention of Hospital-Acquired Infections A Practical Guide 2nd EditionAndreah YoungNo ratings yet
- Prevention of Hospital-Acquired Infections A Practical Guide 2nd EditionDocument72 pagesPrevention of Hospital-Acquired Infections A Practical Guide 2nd EditionAndreah YoungNo ratings yet
- Surgical Site InfectionDocument8 pagesSurgical Site Infection1234chocoNo ratings yet
- AngioedemaDocument15 pagesAngioedemaYuni IHNo ratings yet
- Order of Duties of Ophthalmic Assitants Under NPCB&VIDocument3 pagesOrder of Duties of Ophthalmic Assitants Under NPCB&VISathishNo ratings yet
- Contracted COVID-19 at Wuhan Military Games - Multiple Athletes, The WeekDocument2 pagesContracted COVID-19 at Wuhan Military Games - Multiple Athletes, The WeekKevin SteinerNo ratings yet
- CopdDocument60 pagesCopdRizqy Shofianingrum100% (1)
- 2011 - Sspe PDFDocument230 pages2011 - Sspe PDFJean Michael Castillo100% (1)
- Postoperative Infection and Mortality Following Elective Surgery in The International Surgical Outcomes Study (ISOS)Document32 pagesPostoperative Infection and Mortality Following Elective Surgery in The International Surgical Outcomes Study (ISOS)Antonio Carlos Betanzos PlanellNo ratings yet
- HHS Public Access: A Simple Prediction Score For Developing A Hospital-Acquired Infection After Acute Ischemic StrokeDocument28 pagesHHS Public Access: A Simple Prediction Score For Developing A Hospital-Acquired Infection After Acute Ischemic StrokeGustiAngriAngalanNo ratings yet
- Research Article: Neutropenic Sepsis in The ICU: Outcome Predictors in A Two-Phase Model and Microbiology FindingsDocument9 pagesResearch Article: Neutropenic Sepsis in The ICU: Outcome Predictors in A Two-Phase Model and Microbiology Findings28121998No ratings yet
- RVM y MedistinitisDocument5 pagesRVM y MedistinitisMartha CeciliaNo ratings yet
- Infection Is Acommonproblem ForDocument11 pagesInfection Is Acommonproblem ForDitaMayasariNo ratings yet
- JPAM Vol 14 Issue1 P 609-614Document6 pagesJPAM Vol 14 Issue1 P 609-614Tira Alfiani LaariyaNo ratings yet
- JournalDocument5 pagesJournalAde Bagus PermanaNo ratings yet
- DE LA CRUZ Prevención de Infección Del Sitio Quirúrgico - ArtDocument6 pagesDE LA CRUZ Prevención de Infección Del Sitio Quirúrgico - ArtJOSE FERNANDO DE LA CRUZ SILVANNo ratings yet
- Vardi 2013Document7 pagesVardi 2013Damian CojocaruNo ratings yet
- Predictors of Surgical Site Infection in Laparoscopic and Open Ventral Incisional Herniorrhaphy - 2010 - Journal of Surgical ResearchDocument6 pagesPredictors of Surgical Site Infection in Laparoscopic and Open Ventral Incisional Herniorrhaphy - 2010 - Journal of Surgical ResearchJose Manuel Luna VazquezNo ratings yet
- 10 1155@2019@1438793Document7 pages10 1155@2019@1438793bouchra8blsNo ratings yet
- 55-Article Text-103-1-10-20200408Document7 pages55-Article Text-103-1-10-20200408Kshitiz112No ratings yet
- Risk Factors For Wound InfectionsDocument11 pagesRisk Factors For Wound InfectionsIve PeraltaNo ratings yet
- Surgical-Site Infections Within 60 Days of Coronary Artery By-Pass Graft SurgeryDocument11 pagesSurgical-Site Infections Within 60 Days of Coronary Artery By-Pass Graft SurgeryMartha CeciliaNo ratings yet
- Pneumonia in Patients With Diabetes Mellitus: A Single-Center ExperienceDocument5 pagesPneumonia in Patients With Diabetes Mellitus: A Single-Center ExperienceNoer Sidqi MNo ratings yet
- Incidence and Risk Factors For Ventilator Associated Pneumon 2007 RespiratorDocument6 pagesIncidence and Risk Factors For Ventilator Associated Pneumon 2007 RespiratorTomasNo ratings yet
- Effect of Implementation of A Surgical Safety Checklist On Perioperative and Postoperative Complications at An Academic Institution in North AmericaDocument14 pagesEffect of Implementation of A Surgical Safety Checklist On Perioperative and Postoperative Complications at An Academic Institution in North AmericaMuhammad BasharatullahNo ratings yet
- Infeccion Nosocomial en UciDocument7 pagesInfeccion Nosocomial en UciPaul SalazarNo ratings yet
- Monitoring The One Year Postoperative Infection Rate After Primary Total Hip ReplacementDocument7 pagesMonitoring The One Year Postoperative Infection Rate After Primary Total Hip ReplacementChebbah MahmoudNo ratings yet
- In Critically Ill Adult Patients Community-Acquired Bloodstream InfectionDocument12 pagesIn Critically Ill Adult Patients Community-Acquired Bloodstream InfectionNeliel NoraNo ratings yet
- Saar 2016Document7 pagesSaar 2016iinmsNo ratings yet
- Nosocomial Bloodstream Infection and Clinical SepsisDocument6 pagesNosocomial Bloodstream Infection and Clinical SepsiswintannNo ratings yet
- Ijccm 19 14Document7 pagesIjccm 19 14SahasraNo ratings yet
- Intqhc mzv068 FullDocument7 pagesIntqhc mzv068 FullherryNo ratings yet
- 1 s2.0 S0039606007003480 MainDocument8 pages1 s2.0 S0039606007003480 MainAna MîndrilăNo ratings yet
- Control of Hospital Acquired Infections in The ICU: A Service PerspectiveDocument5 pagesControl of Hospital Acquired Infections in The ICU: A Service PerspectiveAndriyanto HermawanNo ratings yet
- Efficacy and Safety of Restrictive Blood TransfusiDocument4 pagesEfficacy and Safety of Restrictive Blood TransfusiJustin Jay Dar INo ratings yet
- Covid 1 PDFDocument17 pagesCovid 1 PDFPrajawira Smanti CilacapNo ratings yet
- Rba 0 AheadOfPrint 6036c54fa95395582f07f644Document5 pagesRba 0 AheadOfPrint 6036c54fa95395582f07f644STRMoch Hafizh AlfiansyahNo ratings yet
- Antibiotics 02 00001Document10 pagesAntibiotics 02 00001Jenny AlmagroNo ratings yet
- Sharshar 2009 Debil y EstadiaDocument7 pagesSharshar 2009 Debil y EstadiaStefania Anahi MartelNo ratings yet
- Sepsis in Icu GreeceDocument9 pagesSepsis in Icu GreeceChrysiida DelimitrouNo ratings yet
- Infection Control in The ICU: ChestDocument37 pagesInfection Control in The ICU: ChestAditi MehraNo ratings yet
- Video 4 PDFDocument9 pagesVideo 4 PDFMirza RisqaNo ratings yet
- HSR2 5 E649Document9 pagesHSR2 5 E649Samsul BahriNo ratings yet
- 2017 Article 66Document8 pages2017 Article 66Zuhratul LathifaNo ratings yet
- Infection As An Independent Risk Factor For Mortality in The Surgical Intensive Care UnitDocument6 pagesInfection As An Independent Risk Factor For Mortality in The Surgical Intensive Care UnitTito Ahmad RizkiawanNo ratings yet
- Abdominal Sepsis Prognostic FactorDocument6 pagesAbdominal Sepsis Prognostic FactorPrasojo JojoNo ratings yet
- Association Between Perioperative Fluid Management and Patient Outcomes: A Multicentre Retrospective StudyDocument10 pagesAssociation Between Perioperative Fluid Management and Patient Outcomes: A Multicentre Retrospective Studyana mariaNo ratings yet
- art3A10.10072Fs10096 013 2026 2Document7 pagesart3A10.10072Fs10096 013 2026 2mekonen fisehaNo ratings yet
- SepsisScreenTreatmentAlgorithm BaylorUMedicalCenter PDFDocument66 pagesSepsisScreenTreatmentAlgorithm BaylorUMedicalCenter PDFFanie BeatriceNo ratings yet
- EtopxidoDocument28 pagesEtopxidoNatalia ValenzuelaNo ratings yet
- Jurnal LainDocument22 pagesJurnal LainBudi ArsanaNo ratings yet
- Preoperative Assessment of The Risk For Multiple Complications After SurgeryDocument10 pagesPreoperative Assessment of The Risk For Multiple Complications After SurgerylaisNo ratings yet
- Journal Pre-Proof: Mayo Clinic ProceedingsDocument26 pagesJournal Pre-Proof: Mayo Clinic Proceedingssameer sahaanNo ratings yet
- Epidemiology of Surgical Site Infection in A Tertiary Care Centre in North IndiaDocument7 pagesEpidemiology of Surgical Site Infection in A Tertiary Care Centre in North IndiaIJAR JOURNALNo ratings yet
- Aiken 2013Document6 pagesAiken 2013gdakmlMKLNo ratings yet
- Incidence of Surgical Site Infection in Abdominal Surgery in A Tertiaty Care Center in AssamDocument6 pagesIncidence of Surgical Site Infection in Abdominal Surgery in A Tertiaty Care Center in AssamIJAR JOURNALNo ratings yet
- Hospital-Acquired Pneumonia in Critically Ill Children: Incidence, Risk Factors, Outcome and Diagnosis With Insight On The Novel Diagnostic Technique of Multiplex Polymerase Chain ReactionDocument7 pagesHospital-Acquired Pneumonia in Critically Ill Children: Incidence, Risk Factors, Outcome and Diagnosis With Insight On The Novel Diagnostic Technique of Multiplex Polymerase Chain ReactionadhitiaNo ratings yet
- Development and Validation of A Nomogram Using On Admission Routine Laboratory Parameters To Predict In-Hospital Survival of Patients With COVID-19Document23 pagesDevelopment and Validation of A Nomogram Using On Admission Routine Laboratory Parameters To Predict In-Hospital Survival of Patients With COVID-19dariusNo ratings yet
- Boutolleau 2021Document9 pagesBoutolleau 2021nathalialusman98No ratings yet
- Infection Prevention in The Neurointensive Care Unit: A Systematic ReviewDocument15 pagesInfection Prevention in The Neurointensive Care Unit: A Systematic ReviewDžiugas KrNo ratings yet
- 2 Infection Control in The ICU (PDFDrive)Document35 pages2 Infection Control in The ICU (PDFDrive)Lutfi Kumala BaitiNo ratings yet
- Prevention of Infection in Patients With Cancer Evidence Based Nursing InterventionsDocument10 pagesPrevention of Infection in Patients With Cancer Evidence Based Nursing InterventionsAkshayNo ratings yet
- Posters: A Sample of 156 of 232 Nurses Answered An Anonymous QuestionDocument7 pagesPosters: A Sample of 156 of 232 Nurses Answered An Anonymous QuestionFiras DrNo ratings yet
- Ak 2011Document6 pagesAk 2011bouchra8blsNo ratings yet
- Ibi JurnalDocument9 pagesIbi JurnalRiski Pradika 2017No ratings yet
- Infections in Surgery: Prevention and ManagementFrom EverandInfections in Surgery: Prevention and ManagementMassimo SartelliNo ratings yet
- Characterization of Compression BandageDocument21 pagesCharacterization of Compression Bandagebouchra8blsNo ratings yet
- Characterization of Compression BandageDocument21 pagesCharacterization of Compression Bandagebouchra8blsNo ratings yet
- Dr. Lojpur - Dressing and BandageDocument9 pagesDr. Lojpur - Dressing and BandageJayvie Gacutan100% (1)
- Classification of Compression Bandages PDocument10 pagesClassification of Compression Bandages Pbouchra8blsNo ratings yet
- Compression Under Dynamic StateDocument15 pagesCompression Under Dynamic Statebouchra8blsNo ratings yet
- Dr. Lojpur - Dressing and BandageDocument9 pagesDr. Lojpur - Dressing and BandageJayvie Gacutan100% (1)
- Compression Under Dynamic StateDocument15 pagesCompression Under Dynamic Statebouchra8blsNo ratings yet
- The Impact of Gown-Use Requirement On Hand Hygiene ComplianceDocument7 pagesThe Impact of Gown-Use Requirement On Hand Hygiene Compliancebouchra8blsNo ratings yet
- Classification of Compression Bandages PDocument10 pagesClassification of Compression Bandages Pbouchra8blsNo ratings yet
- The Impact of Gown-Use Requirement On Hand Hygiene ComplianceDocument7 pagesThe Impact of Gown-Use Requirement On Hand Hygiene Compliancebouchra8blsNo ratings yet
- Haley 1991Document7 pagesHaley 1991bouchra8blsNo ratings yet
- Nosocomial Infections Epidemiology Prevention Control and SurveillanceDocument21 pagesNosocomial Infections Epidemiology Prevention Control and SurveillanceFelicia BulaiNo ratings yet
- Prevention of Hospital-Acquired Infections: Review of Non-Pharmacological InterventionsDocument16 pagesPrevention of Hospital-Acquired Infections: Review of Non-Pharmacological Interventionsbouchra8blsNo ratings yet
- To Lera 2020Document7 pagesTo Lera 2020bouchra8blsNo ratings yet
- Face Masks and Respirators in The Fight Against The COVID-19 Pandemic: An Overview of The Standards and Testing MethodsDocument12 pagesFace Masks and Respirators in The Fight Against The COVID-19 Pandemic: An Overview of The Standards and Testing Methodsbouchra8blsNo ratings yet
- Pediatric Protrusion Mentioned,: Robert M.D. CityDocument2 pagesPediatric Protrusion Mentioned,: Robert M.D. Citybouchra8blsNo ratings yet
- Vieira 2011Document6 pagesVieira 2011bouchra8blsNo ratings yet
- Chauveau X 2015Document7 pagesChauveau X 2015bouchra8blsNo ratings yet
- Mechanical Properties of Orthopedic Plaster Bandages : U.S.A. Robert E. Porter?Document14 pagesMechanical Properties of Orthopedic Plaster Bandages : U.S.A. Robert E. Porter?bouchra8blsNo ratings yet
- Nosocomial Infections and Infection Control: What's New?Document5 pagesNosocomial Infections and Infection Control: What's New?bouchra8blsNo ratings yet
- Nosocomial Infections and Infection Control: What's New?Document5 pagesNosocomial Infections and Infection Control: What's New?bouchra8blsNo ratings yet
- Pediatric Protrusion Mentioned,: Robert M.D. CityDocument2 pagesPediatric Protrusion Mentioned,: Robert M.D. Citybouchra8blsNo ratings yet
- Chauveau X 2015Document7 pagesChauveau X 2015bouchra8blsNo ratings yet
- Prevention of Hospital-Acquired Infections: Review of Non-Pharmacological InterventionsDocument16 pagesPrevention of Hospital-Acquired Infections: Review of Non-Pharmacological Interventionsbouchra8blsNo ratings yet
- Prevention of Hospital-Acquired Infections: Review of Non-Pharmacological InterventionsDocument16 pagesPrevention of Hospital-Acquired Infections: Review of Non-Pharmacological Interventionsbouchra8blsNo ratings yet
- Pediatric Protrusion Mentioned,: Robert M.D. CityDocument2 pagesPediatric Protrusion Mentioned,: Robert M.D. Citybouchra8blsNo ratings yet
- Chauveau X 2015Document7 pagesChauveau X 2015bouchra8blsNo ratings yet
- Nosocomial Infections and Infection Control: What's New?Document5 pagesNosocomial Infections and Infection Control: What's New?bouchra8blsNo ratings yet
- Group 4 Case Presentation DiarrheaDocument46 pagesGroup 4 Case Presentation DiarrheaEphraim John QuichoNo ratings yet
- Deterministic Malaria Transmission Model With Acquired ImmunityDocument6 pagesDeterministic Malaria Transmission Model With Acquired ImmunityAchmad Nur AlphiantoNo ratings yet
- 4333445492022-10-25T16 28 16.773Document6 pages4333445492022-10-25T16 28 16.773Nina JordanNo ratings yet
- The Scoring Clinical Index For OnychomycosisDocument4 pagesThe Scoring Clinical Index For OnychomycosisPatricia Avalos C.No ratings yet
- Department of Medicine Report 2019Document49 pagesDepartment of Medicine Report 2019Taylor LaframboiseNo ratings yet
- Haematology Physical ExaminationDocument8 pagesHaematology Physical Examinationrodahlyu100% (1)
- Gauze-Based Negative Pressure Wound TherapyDocument20 pagesGauze-Based Negative Pressure Wound TherapyAbdilla RidhwanNo ratings yet
- Acupuntura - Puntos ImportantesDocument14 pagesAcupuntura - Puntos ImportantessanthigiNo ratings yet
- BAER - Brainstem Auditory Evoked ResponseDocument2 pagesBAER - Brainstem Auditory Evoked ResponseAhmad Badrul AminNo ratings yet
- Angels ResumeDocument4 pagesAngels Resumeapi-274792391No ratings yet
- PPR - LISTS - Registered Medicine Price List - 20211230Document333 pagesPPR - LISTS - Registered Medicine Price List - 20211230Abdulla KamalNo ratings yet
- Adults 6Document7 pagesAdults 6Bshara SleemNo ratings yet
- TESTDocument22 pagesTESTjuniati samparaNo ratings yet
- Impact of Prebiotics and Probiotics On Skin Health: F.H. Al-Ghazzewi and R.F. TesterDocument10 pagesImpact of Prebiotics and Probiotics On Skin Health: F.H. Al-Ghazzewi and R.F. TestereaudreyliaNo ratings yet
- PRELIMINARY ACTIVITY of Module 1Document3 pagesPRELIMINARY ACTIVITY of Module 1Casio, Anthony MaryNo ratings yet
- Morning Report Obs FebrisDocument10 pagesMorning Report Obs FebrisJessicaNo ratings yet
- Inside The Human BodyDocument1 pageInside The Human BodyKaravanNo ratings yet
- WedDocument6 pagesWedPratiwi IkaNo ratings yet
- MS GENEZAL EGAY PRUHealth PrimeDocument12 pagesMS GENEZAL EGAY PRUHealth PrimeAntoniette Samantha NacionNo ratings yet
- Vascular TraumaDocument16 pagesVascular TraumaAndi Suchy Qumala SarieNo ratings yet
- Physician CertificationDocument1 pagePhysician CertificationcwadotorgNo ratings yet
- World Sight Day-Activity Report - 2022-PICO PakistanDocument5 pagesWorld Sight Day-Activity Report - 2022-PICO Pakistanjibran khanNo ratings yet
- Absen Edit 2019Document29 pagesAbsen Edit 2019Judika ThampNo ratings yet