Professional Documents
Culture Documents
Docetaxel - 40mg/ml Injection: Instruction
Uploaded by
ywOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Docetaxel - 40mg/ml Injection: Instruction
Uploaded by
ywCopyright:
Available Formats
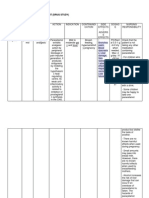
Docetaxel - 40mg/ml Injection
Instruction
Route of administration: IV
Final infusion concentration shall be less than 0.74mg/ml.
Premedication: PO dexamethasone for 3 days (the day before, during and the day after
docetaxel administration). Premedication helps to reduce the frequency and severity
of fluid retention and hypersensitivity reactions.
Storage
Store in a refrigerator and protect from light.
Dispense in non-PVC container. After dilution, use within 8 hours (bolus: in
refrigerator) or 4 hours (infusion: in room temperature).
Precaution:
Use with caution in hepatic impairment. May need dose modification.
Pregnancy Risk Factor: D
Drug-Drug Interaction
Ketoconazole: May decrease metabolism of docetaxel.
Ritonavir: May increase haematological toxicity.
Sorafenib: May increase docetaxel toxicity.
Drug-Herb
Echinacea: May diminish therapeutic effect of docetaxel.
St. John's Wort: May increase metabolism of docetaxel.
Side Effects
Haematologic toxicities (neutropenia, anaemia, thrombocytopenia).
Cardiotoxicity (fluid retention).
Skin toxicities (alopecia, cutaneous reaction, nail changes - usually transient and
disappear with treatment withdrawal).
GI toxicities (mucositis, diarrhoea, low: nausea and vomiting).
Hypersensitivity reaction (hypotension, bronchospasm, generalised rash).
Neurotoxicity (peripheral neuropathy: related to cumulative dose).
Ocular toxicity (lacrimation of eyes: transient, reversible, visual disturbances). Treat
with antibiotic and steroid.
Pulmonary toxicities (dyspnoea, epistaxis), hepatotoxicity (elevated LFT).
General (fatigue, fever, infection).
Doxorubicin - 2mg/ml Injection
Instruction
Route of administration: IV
Do not administer IT, IM or SC.
To avoid doxorubicin flare, IV bolus should be infused over 3-10 minutes.
Maximum lifetime cumulative dose: 300-550mg/m2.
Storage
Store in a refrigerator and protect from light.
Storage of vials of solution under refrigeration may result in formation of a gelled
product. If gelling occurs, place vials at room temperature for 2 to 4 hours to return
the product to a slightly viscous, mobile solution.
Precaution
Hepatic impairment (contraindicated in Child-Pugh class C or bilirubin >5 mg/dL).
Patients who have received other anthracyclines and contraindicated in patients with
history of cardiovascular disease (may cause cardiac toxicity).
Avoid pregnancy while on therapy and for at least 6 months following discontinuation
of therapy. Pregnancy Risk Factor: D
Use non-hormonal contraception in breast cancer patient.
May cause sterility in men and menopause in women. Discuss with doctor if plan to
have children.
Extravasation injury: May cause severe tissue necrosis.
Drug-Drug Interaction
Calcium channel blocker (verapamil, nifedipine) : May increase cardiotoxicity of
doxorubicin.
Barbiturates (phenobarbital): May decrease the effect of doxorubicin.
Bevacizumab: May increase doxorubicin induced cardiotoxicity.
Cyclosporin: May increase pharmacological effect of doxorubicin.
Quinolone (ciprofloxacin): May decrease quinolone absorption.
Stavudine: May decrease the active form of stavudine.
Trastuzumab: May increase cardiotoxicity.
Drug-Food/Herb
Curcumin: May decrease doxorubicin effect.
Avoid foods or products containing turmeric (curcumin).
Side Effects
Cardiotoxicity (ECG changes, cardiomyopathy, arrhythmia). Cardiac assessment
should be done at baseline and throughout therapy.
Haematologic toxicity (leucopenia).
GI toxicities (high to moderate: nausea and vomiting, mucositis, diarrhoea).
Skin toxicities (alopecia, hyperpigmentation of nail beds).
General (urine discoloration: urine maybe pink or reddish for 1-2 days after therapy).
Metabolism and nutrition disorders (hyperuricaemia).
Cyclophosphamide - 200mg, 1000mg Injection; 50mg Tablet
Instruction
Route of administration: PO, IV
PO: Take with food or on an empty stomach. Preferable morning
administration to ensure adequate hydration throughout the day. Do not administer at bed
time.
Storage
Injection: Store at room temperature.
Tablet: Store at room temperature not more than 30°C.
Precaution
Use with caution in renal impairment. May need dose modification.
Pregnancy Risk Factor: D
May impair fertility; sterility in men and menopause in women. Discuss
with doctor if plan to have children.
Drug-Drug Interaction
Allopurinol: May increase cyclophosphamide effect.
Warfarin: May increase the effect of warfarin.
Digoxin: May decrease the effect of digoxin.
Drug-Herb Interaction
Avoid black cohosh and dong quai in oestrogen-dependent tumours.
Side Effects
Renal toxicity (haemorrhagic cystitis in high dose and or long term therapy). May be
minimised by adequate hydration and/or with mesna).
Haematologic toxicities (anaemia, neutropenia, thrombocytopenia).
GI toxicities (moderate to high: nausea and vomiting, mucositis,
diarrhoea).
Skin toxicities (alopecia, hyperpigmentation of nail or skin).
Cardiotoxicities: With high dose HSCT therapy (arrhythmias, cardiac
tamponade, CHF, haemorrhagic myocarditis, myocardial necrosis).
Pulmonary toxicity (high dose therapy: pulmonary fibrosis).
Hepatotoxicity (high dose therapy: veno-occlusive liver disease).
Nasal congestion due to rapid administration of cyclophosphamide.
General Counselling Points for Patients During Chemotherapy
a) Avoid crowded areas.
b) Wear protective mask.
c) Go to the nearest hospital if there are signs of fever, prolonged bleeding or unexplained
fatigue.
d) Avoid smoking or alcohol consumption.
e) Avoid uncooked food, eat a well-balanced diet and drink plenty of water.
f) Get plenty of rest and sleep.
g) Perform daily activities and exercise as tolerated.
h) Consult doctor for choice of contraception measures. Discuss with doctor if plan to get
pregnant.
i) Discuss with the doctor or pharmacist before taking any other medicines, vitamins, mineral
supplements, traditional or complementary medicines. Some may seriously interfere with the
treatment that has been prescribed.
j) Discuss with the healthcare provider regarding side effects encountered during
chemotherapy. Consult doctor if wish to stop therapy for any reason.
General Precautions for Patients During Chemotherapy
a) Check with doctor or pharmacist before start taking any new drugs (including over-the
counter, nutritional supplements, vitamins, and herbal drugs). Discuss with doctor before
receiving any immunisation. This is to prevent drug-induced immunosuppression.
b) Inform doctor immediately if patient or partner becomes pregnant; may cause foetal harm.
c) Breastfeeding is not encouraged during treatment as it may harm the baby.
d) Inform doctor or dentists if on chemotherapy.
e) Avoid alcohol. It may interfere with the way some chemotherapy drugs work.
Important Medication Counselling Points for Patients During Chemotherapy
a)5R: The right patient, medicines, dose, route and time of administration (in regards to food
intake).
b)The name and indications of their medications, including supportive medications.
c) Treatment schedule; when to start, stop and interval between doses as well as duration of
each cycle and total number of cycle.
d) Common and significant side effects and the treatment managements.
e) Steps to be taken in the event of fever or other signs of infection.
f) Any drug or food interactions.
g) The arrangements for resupply either from the hospital, health clinic or retail pharmacy;
supply adequate quantity for each cycle only, advice to return any unused or extra
medication.
h) Storage instructions and emphasise on keeping out of children’s reach.
i) Any handling or safety precautions; cytotoxic drugs should not be handled by pregnant
women.
j) “Do not cut/ crush / chew”
k) Any issues on fertility.
l) Clear advice if the patient misses a dose or vomits shortly after the dose is taken:
• Take the medication at the same time each day.
• If vomiting occurs within 1 hour of taking a dose, consult doctor or healthcare
providers.
• If missed a dose, take it as soon as possible and do not double the dose.
- Once a day dosing : If it is more than 12 hours since missed dose, skip the missed dose and
go back to usual dosing time.
- Twice a day dosing : If it is more than 6 hours since missed dose, skip the missed dose and
go back to usual dosing time.
Common Counselling for Cancer Patients regarding the side effects
1. Coping with Nausea and Vomiting
-Eat and drink slowly. Try having small frequent meals throughout the day instead of usual
portion of breakfast, lunch, and dinner.
-Avoid sweet, fried, or fatty foods, as well as foods with strong smell. Eating cold foods or at
room temperature can help to avoid strong smells.
-Ensure full understanding of doctor’s and pharmacist’s instructions on taking anti-nausea
and vomiting medicines.
-Ensure a sufficient supply of the correct drugs.
-Consume adequate fluids. Ask doctor, pharmacist or dietician about proper nutrition during
this time.
-Do not starve for long periods, as this may make the nausea worsen.
-Find out from doctor or pharmacist if any other medicines taken may require special
precautions.
2. Preventing Mucositis:
-Avoid salty, spicy or dry food, avoid drinks containing caffeine or alcohol
-Eat food at room temperature rather than food served hot.
-Practice good oral hygiene to prevent infection.
-Use soft bristle toothbrush or an oral sponge (rinsing the bristles in hot water can make them
even softer).
-Gargle regularly (avoid gargles that contain alcohol).
-Drink plenty of water.
-Try sipping cups of water throughout the day to avoid dry mouth.
-If wearing dentures, remove them once mouth becomes sensitive.
-Inform doctor if experience tooth or gum problem. They can refer to dentist for further
management before chemotherapy starts.
3. Prevention of Constipation:
• Eat plenty of food with high dietary fiber (breads, grains, fruits and vegetables).
• Drink plenty of fluids.
• Make light exercise a part of everyday schedule, e.g. walk or ride an exercise bike for
15-30 mins/day
• Inform doctor or pharmacist if no bowel movement in 2 days or are passing hard
stools.
• Doctor may prescribe laxatives to prevent or treat constipation.
4. Coping with diarrhea:
• Replace lost fluids and salts.
• Drink plenty of fluids (at least 2 L).
• Take oral rehydration salt (ORS).
Consume food that is nourishing without contributing to diarrhea:
• Clear broth (soup) or porridge such as chicken, vegetable or beef.
• High-protein foods such as eggs (well cooked), lean meat, fish or poultry.
• Bananas.
• Potatoes (boiled, without the skin).
• Oatmeal.
Avoid foods and drinks that can make diarrhea worse :
• Dairy products, such as milk and cheese.
• Spicy, greasy or fried food.
• Food that cause gas, such as broccoli and cabbage.
• Food that are high in fiber, such as whole-wheat breads and bran cereals.
• Beer, wine, and other drinks with alcohol in them. Caffeinated drinks like cola,
coffee, and black tea.
-Consult doctor or pharmacist before taking medicine for diarrhea
5. Diet is an important part of cancer treatment.
There are many benefits from eating well before, during, and after treatment such as:
• Cope better with the unpleasant effect of cancer and cancer treatment.
• Faster recovery following treatment.
• Feels more energetic.
• Maintain body weight.
Types of food which should be avoided during chemotherapy:
• Raw food, raw fruits (e.g. tempoyak), raw and unpasteurized honey
• Unpasteurized milk and fresh milk product
• Salad and cheese
• Preserved food (e.g. salted fish, salted vegetable, “salai” meat, cincalok, belacan)
• Raw/half cooked fungus (e.g. mushroom)
Types of food which should be avoided during chemotherapy:
• Half cooked food
• Spicy food, oily food
• Carbonated drinks
• Drinking water:
1. Drink boiled water.
2. Filtered water which is not boiled should be avoided.
3. Wash the outer area of bottled water before opening
• Alcohol - Avoid alcohol throughout treatment period.
You might also like
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesFrom EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesRating: 4 out of 5 stars4/5 (2)
- Drug Analysis: Submitted By: GALICINAO, Gretta Shalou GDocument9 pagesDrug Analysis: Submitted By: GALICINAO, Gretta Shalou GggalicinaoNo ratings yet
- DexamethasoneDocument4 pagesDexamethasoneMits Valencia Karlsson0% (2)
- PREDNISONEDocument4 pagesPREDNISONECay SevillaNo ratings yet
- Generic Name: Albuterol Brand Name: Salbutamol, Proventil, Ventolin, Accuneb, Airet, Novo-SalbutamolDocument26 pagesGeneric Name: Albuterol Brand Name: Salbutamol, Proventil, Ventolin, Accuneb, Airet, Novo-SalbutamolAnna Joy Antone100% (1)
- Drugs For EmergencyDocument25 pagesDrugs For EmergencyJunathan L. DelgadoNo ratings yet
- Hydrocortisone TabDocument7 pagesHydrocortisone TabXee JayNo ratings yet
- Drug Study On Emergency DrugsDocument14 pagesDrug Study On Emergency DrugsRene John FranciscoNo ratings yet
- Drug Study On Emergency DrugsDocument34 pagesDrug Study On Emergency DrugsMei-mei ZhuangNo ratings yet
- Drug StudyDocument14 pagesDrug StudyKatrina EstoconingNo ratings yet
- EMERGENCY DRUGS: A Drug StudyDocument8 pagesEMERGENCY DRUGS: A Drug StudyShaine WolfeNo ratings yet
- EMERGENCY DRUGS: Aminophylline, Amiodarone, Atropine, BumetanideDocument33 pagesEMERGENCY DRUGS: Aminophylline, Amiodarone, Atropine, BumetanideNicole GarciaNo ratings yet
- Metformin Hydrochloride PDFDocument4 pagesMetformin Hydrochloride PDFHannaNo ratings yet
- Drug StudyDocument9 pagesDrug Studyjanelee2824No ratings yet
- Drug Study On Emergency DrugsDocument14 pagesDrug Study On Emergency Drugsjcarysuitos100% (4)
- DactinomycinDocument4 pagesDactinomycinKeith MadarangNo ratings yet
- Calcium Carbonate for Bone HealthDocument14 pagesCalcium Carbonate for Bone HealthBianca Freya Porral85% (13)
- Labor and Delivery MedsDocument12 pagesLabor and Delivery MedsSam DanaNo ratings yet
- Diphenhydramine Hydrochloride (Benadryl) 50mg/1mlDocument6 pagesDiphenhydramine Hydrochloride (Benadryl) 50mg/1ml'SheenMarkReal'No ratings yet
- Daunorubicin: Drug NameDocument7 pagesDaunorubicin: Drug NameEdgar Ledesma-MartínezNo ratings yet
- Nifedipine and Prednisone Drug StudyDocument5 pagesNifedipine and Prednisone Drug StudyAllyne GavinoNo ratings yet
- Respiratory Medications ReviewDocument4 pagesRespiratory Medications ReviewKevin VillaranteNo ratings yet
- Drug StudyDocument6 pagesDrug StudyNajmah Saaban100% (1)
- CHN Drug StudyDocument10 pagesCHN Drug StudyJoshua Cyryll ComiaNo ratings yet
- Paracetamol and Levofloxacin Drug StudyDocument9 pagesParacetamol and Levofloxacin Drug StudyKevin Sam AguirreNo ratings yet
- Nursing Considerations Assessment: History: Infections Kidney Disease Liver Disease, Hypothyroidism UlcerativeDocument5 pagesNursing Considerations Assessment: History: Infections Kidney Disease Liver Disease, Hypothyroidism UlcerativeSophia limNo ratings yet
- MinoxidilDocument4 pagesMinoxidilapi-3797941100% (1)
- HydrocortisoneDocument2 pagesHydrocortisoneMaggieNo ratings yet
- Drug StudyDocument6 pagesDrug StudyFloramae Celine BosqueNo ratings yet
- The 10 Most Common Emergency DrugsDocument28 pagesThe 10 Most Common Emergency DrugsKrishna BalsarzaNo ratings yet
- NizoralDocument4 pagesNizoralianecunar100% (2)
- Drug StudyDocument17 pagesDrug StudyKenneth ManalangNo ratings yet
- 9 Drug StudyDocument11 pages9 Drug StudyJessa Mae Mauricio CastilloNo ratings yet
- Doxorubicin: Mechanism of ActionDocument3 pagesDoxorubicin: Mechanism of ActionGeorge FogNo ratings yet
- Diclofenac Sodium Drug InformationDocument9 pagesDiclofenac Sodium Drug InformationAlexander Chavez Alto100% (1)
- Generic Name: Propiverine HCl Brand Name: Mictonorm Classification: Urinary AntispasmodicDocument7 pagesGeneric Name: Propiverine HCl Brand Name: Mictonorm Classification: Urinary AntispasmodicMaRic Gabutin Guerra100% (1)
- Nursing Pharmacology Handouts For ZamboDocument7 pagesNursing Pharmacology Handouts For ZamboAlexa Abidin Oldenborg100% (8)
- Drug Study NewDocument4 pagesDrug Study NewJehannah Dayanara Berdan HayudiniNo ratings yet
- Propylthiouracil DSDocument6 pagesPropylthiouracil DSAlexandrea MayNo ratings yet
- COPD Medications Reduce Inflammation Improve BreathingDocument3 pagesCOPD Medications Reduce Inflammation Improve BreathingKdamnzNo ratings yet
- Drug Study (DR)Document19 pagesDrug Study (DR)09159054476No ratings yet
- 1430 Drug CardsfinalDocument7 pages1430 Drug CardsfinalLizSherman100% (1)
- TB medications overviewDocument7 pagesTB medications overviewANNIE SHINE MAGSACAYNo ratings yet
- PLASIL antiemetics classificationDocument5 pagesPLASIL antiemetics classificationAbby MontealegreNo ratings yet
- Pharmacology EndocrineDocument29 pagesPharmacology Endocrineamasoud96 amasoud96No ratings yet
- Keterolax Trometamol Classification: Nonsteroidal Anti-Inflamatory DrugDocument7 pagesKeterolax Trometamol Classification: Nonsteroidal Anti-Inflamatory DrugEm Hernandez AranaNo ratings yet
- Drug StudyDocument5 pagesDrug StudyCrystal Joy MisaNo ratings yet
- Drug Cefaclor IsoxsuprineDocument6 pagesDrug Cefaclor IsoxsuprineJelly Ong 王金玉No ratings yet
- LIVOLIN FORTE ACTIONS AND USESDocument5 pagesLIVOLIN FORTE ACTIONS AND USESDick Morgan FerrerNo ratings yet
- Chlorpromazine Dosage GuideDocument3 pagesChlorpromazine Dosage GuideChristine Pialan SalimbagatNo ratings yet
- Drug Study Gentamicin Sulfate and SalbutamolDocument7 pagesDrug Study Gentamicin Sulfate and SalbutamolEduardNo ratings yet
- Emergency Drugs: (A Drug Study)Document13 pagesEmergency Drugs: (A Drug Study)Marichu BajadoNo ratings yet
- ImipramineDocument6 pagesImipramineMuhammed Faruk JambazNo ratings yet
- Solu-Cortef (Hydrocortisone)Document3 pagesSolu-Cortef (Hydrocortisone)E100% (2)
- Atorvastatin CalciumDocument2 pagesAtorvastatin Calciumshiraz.aNo ratings yet
- Drug Name Action Indication Contraindication Adverse Effects Nursing ResponsibilitiesDocument5 pagesDrug Name Action Indication Contraindication Adverse Effects Nursing ResponsibilitiesJanry-Mae Escobar TumanengNo ratings yet
- Report On Suspected Adverse Drug ReactionsDocument2 pagesReport On Suspected Adverse Drug Reactionsyw100% (1)
- Cancer Drug Counselling Guide Pharmacists 2016Document154 pagesCancer Drug Counselling Guide Pharmacists 2016carmenchang93No ratings yet
- MOH Systemic Protocol 2016Document184 pagesMOH Systemic Protocol 2016ywNo ratings yet
- Manual For Sterile PreparationsDocument107 pagesManual For Sterile PreparationsywNo ratings yet
- MOH Systemic Therapy Protocol 2011Document150 pagesMOH Systemic Therapy Protocol 2011ywNo ratings yet
- Docetaxel - 40mg/ml Injection: InstructionDocument11 pagesDocetaxel - 40mg/ml Injection: InstructionywNo ratings yet
- g6pd DeficiencyDocument6 pagesg6pd DeficiencyAnonymous C7LSjfNo ratings yet
- Remember and Skip Doubling-Up If You Forget To Apply. Only For External UseDocument1 pageRemember and Skip Doubling-Up If You Forget To Apply. Only For External UseywNo ratings yet
- EPP Assignment 2 (Letter of Notification)Document1 pageEPP Assignment 2 (Letter of Notification)ywNo ratings yet
- PDFDocument791 pagesPDFNgai29100% (2)
- Planningpaper3 130814075802 Phpapp01Document32 pagesPlanningpaper3 130814075802 Phpapp01Ke Ke SawNo ratings yet
- 23 01 2015Document4 pages23 01 2015ywNo ratings yet
- Medical Surgical Questions LiverDocument17 pagesMedical Surgical Questions LiverHasan A AsFourNo ratings yet
- Passed Like A ShadowDocument15 pagesPassed Like A ShadowTimoNo ratings yet
- NPC Data PrivacyDocument2 pagesNPC Data PrivacyCess AyomaNo ratings yet
- Basic Neuroanatomy and Stroke Syndromes PDFDocument15 pagesBasic Neuroanatomy and Stroke Syndromes PDFFrancisco A. Villegas-López100% (2)
- Family Centered CareDocument7 pagesFamily Centered CareSirisha ChelvaNo ratings yet
- 00 Obs&Gyn Clerkship-1-1Document9 pages00 Obs&Gyn Clerkship-1-1samwel daniel100% (1)
- CASE STUDY (Gastro)Document3 pagesCASE STUDY (Gastro)Jake Yvan DizonNo ratings yet
- 1 Module 1 hss1010 Booklet 1Document108 pages1 Module 1 hss1010 Booklet 1api-463761938No ratings yet
- The role of Du Mai in separation from the maternal matrix and development of individual identityDocument81 pagesThe role of Du Mai in separation from the maternal matrix and development of individual identityJonathan67% (3)
- Estimating Transition Probabilities FromDocument12 pagesEstimating Transition Probabilities Fromsleepanon4362No ratings yet
- Efficacy and Safety of Very Early Mobilisation Within 24 H of Stroke Onset (AVERT) : A Randomised Controlled TrialDocument10 pagesEfficacy and Safety of Very Early Mobilisation Within 24 H of Stroke Onset (AVERT) : A Randomised Controlled TrialJohann Sebastian CruzNo ratings yet
- 665 672Document8 pages665 672Sebastián Ghiso JiménezNo ratings yet
- Sesi 5a - Ukuran Asosiasi 2011Document50 pagesSesi 5a - Ukuran Asosiasi 2011Tyra Septi DianaNo ratings yet
- HEMATOLOGY Chapter 20 Rodaks Hematology, 5E (2016)Document14 pagesHEMATOLOGY Chapter 20 Rodaks Hematology, 5E (2016)Sachi Xandria de LaraNo ratings yet
- Risk Assessment Form: Zibran Anwar SayyadDocument2 pagesRisk Assessment Form: Zibran Anwar SayyadMufid SatamkarNo ratings yet
- Burn Management Guidelines in EthiopiaDocument28 pagesBurn Management Guidelines in EthiopiaNEsreNo ratings yet
- A Neuro-Heuristic Approach For Recognition of Lung Diseases From X-RayDocument15 pagesA Neuro-Heuristic Approach For Recognition of Lung Diseases From X-RaySarah NixonNo ratings yet
- DOHaD and Birth Cohort ResearchDocument3 pagesDOHaD and Birth Cohort ResearchNguyễn Tiến HồngNo ratings yet
- End of Life ManualDocument238 pagesEnd of Life ManualJeffery TaylorNo ratings yet
- BODYPUMP 100 Education Only - Print ReadyDocument5 pagesBODYPUMP 100 Education Only - Print ReadyNikolas MandilarasNo ratings yet
- The Early Identification of Autism: The Checklist For Autism in Toddlers (CHAT)Document43 pagesThe Early Identification of Autism: The Checklist For Autism in Toddlers (CHAT)melaniNo ratings yet
- Professional English For Physical SciencesDocument134 pagesProfessional English For Physical SciencesRavindranathan ArumugamNo ratings yet
- PEMERINTAH KABUPATN MAMUJU TENGAH DINAS PENDIDIKAN UPTD SMP NEGERI 2 PANGALEDocument4 pagesPEMERINTAH KABUPATN MAMUJU TENGAH DINAS PENDIDIKAN UPTD SMP NEGERI 2 PANGALEFitri ShanumNo ratings yet
- Spirometry Testing - What Is A SpirometerDocument11 pagesSpirometry Testing - What Is A SpirometerFatima Sherrisa SaliNo ratings yet
- Yoga Mudras For Balancing Dosha (Vata, Pitta, & Kapha) : Home Articles Mudras Poses PranayamaDocument26 pagesYoga Mudras For Balancing Dosha (Vata, Pitta, & Kapha) : Home Articles Mudras Poses PranayamaDanaNo ratings yet
- Prostate CancerDocument5 pagesProstate CancerBrilliant Osai-OyeteNo ratings yet
- Guzom NarrativeDocument29 pagesGuzom NarrativeJoshua FloranoNo ratings yet
- Leukemia in Children: 1 Rahul Dhaker, Asst. Professor, RCNDocument41 pagesLeukemia in Children: 1 Rahul Dhaker, Asst. Professor, RCNRahul DhakerNo ratings yet
- Nisargastrikesmaharashtracoast: 2 Lac Flashpoints Are Not in List of Identified Areas Still ContestedDocument14 pagesNisargastrikesmaharashtracoast: 2 Lac Flashpoints Are Not in List of Identified Areas Still ContestedTomNo ratings yet
- FULL Download Ebook PDF Fundamentals of Health Psychology 2nd Edition PDF EbookDocument41 pagesFULL Download Ebook PDF Fundamentals of Health Psychology 2nd Edition PDF Ebookjennifer.lawver532100% (31)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (14)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (5)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (327)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- Daniel Kahneman's "Thinking Fast and Slow": A Macat AnalysisFrom EverandDaniel Kahneman's "Thinking Fast and Slow": A Macat AnalysisRating: 3.5 out of 5 stars3.5/5 (130)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisFrom EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (3)