Professional Documents
Culture Documents
CDC Report of Aug. 24, 2021
Uploaded by
Algernon D'AmmassaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CDC Report of Aug. 24, 2021
Uploaded by
Algernon D'AmmassaCopyright:
Available Formats
Morbidity and Mortality Weekly Report
Early Release / Vol. 70 August 24, 2021
Effectiveness of COVID-19 Vaccines in Preventing SARS-CoV-2 Infection
Among Frontline Workers Before and During B.1.617.2 (Delta) Variant
Predominance — Eight U.S. Locations, December 2020–August 2021
Ashley Fowlkes, ScD1; Manjusha Gaglani, MBBS2; Kimberly Groover, PhD3; Matthew S. Thiese, PhD4;
Harmony Tyner, MD5; Katherine Ellingson, PhD6; HEROES-RECOVER Cohorts
During December 14, 2020–April 10, 2021, data from extraction from electronic medical records or state immuniza-
the HEROES-RECOVER Cohorts,* a network of prospec- tion registries. Among 4,217 participants, 3,483 (83%) were
tive cohorts among frontline workers, showed that the Pfizer- vaccinated; 2,278 (65%) received Pfizer-BioNTech, 1,138
BioNTech and Moderna mRNA COVID-19 vaccines were (33%) Moderna, and 67 (2%) Janssen (Johnson & Johnson)
approximately 90% effective in preventing symptomatic and COVID-19 vaccines. Cox proportional hazards models were
asymptomatic infection with SARS-CoV-2, the virus that causes used to calculate ratios of unvaccinated to fully vaccinated
COVID-19, in real-world conditions (1,2). This report updates (≥14 days after receipt of all recommended COVID-19 vac-
vaccine effectiveness (VE) estimates including all COVID-19 cine doses) infection rates, adjusted for occupation, site, and
vaccines available through August 14, 2021, and examines local viral circulation (6), and weighted for inverse probability
whether VE differs for adults with increasing time since comple- of vaccination using sociodemographic characteristics, health
tion of all recommended vaccine doses. VE before and during information, frequency of close social contact, and mask use.
SARS-CoV-2 B.1.617.2 (Delta) variant predominance, which This activity was reviewed by CDC and was conducted con-
coincided with an increase in reported COVID-19 vaccine sistent with applicable federal law and CDC policy.§
breakthrough infections, were compared (3,4). During the 35-week study period, 4,136 participants with
Methods for the HEROES-RECOVER Cohorts have no previous laboratory-documented SARS-CoV-2 infection
been published previously (1,2,5). Health care personnel, contributed a median of 20 unvaccinated days per participant
first responders, and other essential and frontline workers (interquartile range [IQR] = 8–45 days; total = 181,357 days),
in eight U.S. locations across six states were tested weekly during which 194 SARS-CoV-2 infections were identified;
for SARS-CoV-2 infection by reverse transcription–poly- 89.7% of these infections were symptomatic. A total of 2,976
merase chain reaction (RT-PCR)† and upon the onset of participants contributed a median of 177 fully vaccinated days
any COVID-19–like illness. Weeks when the Delta variant (IQR = 115–195 days; total = 455,175 days) with 34 infec-
accounted for ≥50% of viruses sequenced, based on data tions, 80.6% of which were symptomatic. Adjusted VE against
from each respective location, were defined as weeks of SARS-CoV-2 infection was 80% (95% confidence interval
Delta variant predominance. Vaccination was documented [CI] = 69%–88%). The VE point estimate was 85% among
by self-report and verified by provision of vaccine cards or participants for whom <120 days had elapsed since comple-
tion of full vaccination compared with 73% among those for
* Arizona Healthcare, Emergency Response and Other Essential Workers whom ≥150 days had elapsed; however the VE 95% CI were
Surveillance Study (HEROES) conducted in Phoenix, Tucson, and other
noncentrally located areas in Arizona; Research on the Epidemiology of overlapping, indicating the difference was not statistically
SARS-CoV-2 in Essential Response Personnel (RECOVER) conducted in significant (Table).
Miami, Florida; Duluth, Minnesota; Portland, Oregon; Temple, Texas; and
Salt Lake City, Utah. § 45 C.F.R. part 46.102(l)(2), 21 C.F.R. part 56; 42 U.S.C. Sect 241(d); 5 U.S.C.
† RT-PCR was conducted using the Quidel Lyra SARS-CoV-2 Assay (before
Sect 552a; 44 U.S.C. Sect 3501 et seq.
November 2020) or TaqPath COVID-19 Combo Kit (Applied Biosystems) at
the Marshfield Clinic Research Institute (Marshfield, WI).
U.S. Department of Health and Human Services
Centers for Disease Control and Prevention
Early Release
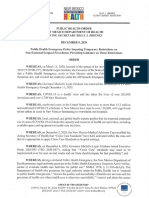
TABLE. Effectiveness of COVID-19 vaccines against any SARS-CoV-2 infection among frontline workers, by B.1.617.2 (Delta) variant predominance
and time since full vaccination — eight U.S. locations, December 2020–August 2021
No. of contributing Total no. of No. of SARS-CoV-2 Adjusted VE,†
Period and vaccination status participants* person-days Median days (IQR) infections % (95% CI)
Full cohort to date
Unvaccinated 4,136 181,357 20 (8–45) 194 N/A
Fully vaccinated§ 2,976 454,832 177 (115–195) 34 80 (69–88)
14–119 days after full vaccination 2,923 284,617 106 (106–106) 13 85 (68–93)
120–149 days after full vaccination 2,369 66,006 30 (30–30) 3 81 (34–95)
≥150 days after full vaccination 2,129 104,174 52 (37–64) 18 73 (49–86)
Pre-Delta variant predominance
Unvaccinated 4,137 156,626 19 (8–43) 175 N/A
Fully vaccinated 2,875 329,865 124 (95–149) 10 91 (81–96)
Delta variant predominance
Unvaccinated 488 24,871 43 (37–69) 19 N/A
Fully vaccinated 2,352 119,218 49 (35–56) 24 66 (26–84)
Abbreviations: CI = confidence interval; IQR = interquartile range; N/A = not applicable; SMD = standardized mean difference; VE = vaccine effectiveness.
* Person-days between the date of any dose of COVID-19 vaccine and fully vaccinated status were excluded from VE models because of indeterminate immune status.
Participants with SARS-CoV-2 infection during this period were also excluded; in the pre-Delta period, 47 participants were excluded, and in the Delta period, two
participants were excluded. Contributing participants in vaccination categories also do not equal the total number of participants in the cohort.
† Adjusted VE was inversely weighted for probability of being vaccinated and adjusted for local virus circulation, study location, and occupation. Delta variant models
were additionally adjusted for ethnicity. All Cox regression models met the proportional hazards assumption. To calculate the probability of being vaccinated for
each period, boosted regression models were fit including covariates for site, sociodemographic characteristics, health information, frequency of close social contact,
mask use, and local virus circulation. In the full cohort to date and the pre-Delta cohort, all covariates met balance criteria of SMD<0.2 after weighting except mask
use at work (SMD = 0.227 and 0.207, respectively) but was not found to change VE estimates by ≥3% when added to the models. In the Delta predominant cohort
occupation, ethnicity, influenza vaccination, and mask use at work did not meet balance criteria (SMD range = 0.206–0.288); influenza vaccination and mask use at
work did not change VE estimates by ≥3%; however, occupation and ethnicity did change VE by ≥3% and were therefore included as covariates in the Cox regression
model for VE.
§ Fully vaccinated was defined as ≥14 days after receipt of all recommended COVID-19 vaccine doses.
During Delta variant–predominant weeks at study will be monitored continuously. Although these interim
sites, 488 unvaccinated participants contributed a median findings suggest a moderate reduction in the effectiveness of
of 43 days (IQR = 37–69 days; total = 24,871 days) COVID-19 vaccines in preventing infection, the sustained two
with 19 SARS-CoV-2 infections (94.7% symptomatic); thirds reduction in infection risk underscores the continued
2,352 fully vaccinated participants contributed a median of importance and benefits of COVID-19 vaccination.
49 days (IQR = 35–56 days; total = 119,218 days) with 24
Acknowledgments
SARS-CoV-2 infections (75.0% symptomatic). Adjusted
VE during this Delta predominant period was 66% Mark G. Thompson, Lauren Grant, Julie Mayo Lamberte,
(95% CI = 26%–84%) compared with 91% (95% CI = 81%– Young M. Yoo, Gregory Joseph, Josephine Mak, Monica Dickerson,
96%) during the months preceding Delta predominance. Suxiang Tong, John Barnes, Eduardo Azziz-Baumgartner,
During December 14, 2020–August 14, 2021, full vaccina- Melissa L. Arvay, Preeta Kutty, Alicia M. Fry, Lenee Blanton,
Jill Ferdinands, Anthony Fiore, Aron Hall, Adam MacNeil,
tion with COVID-19 vaccines was 80% effective in preventing
L. Clifford McDonald, Mary Reynolds, Sue Reynolds,
RT-PCR–confirmed SARS-CoV-2 infection among frontline St e p h a n i e S c h r a g , No n g S h a n g , R o b e r t S l a u g h t e r,
workers, further affirming the highly protective benefit of full Matthew J. Stuckey, Natalie Thornburg, Jennifer Verani, Vic Veguilla,
vaccination up to and through the most recent summer U.S. R o s e Wa n g , B a o - P i n g Z h u , W i l l i a m B r a n n e n ,
COVID-19 pandemic waves. The VE point estimates declined Stephanie Bialek, CDC; Jefferey L. Burgess, Karen Lutrick, Shawn Beitel,
from 91% before predominance of the SARS-CoV-2 Delta Patrick Rivers, Xiaoxiao Sun, Joe K. Gerald, Janko Nikolich-Žugich,
variant to 66% since the SARS-CoV-2 Delta variant became Genesis Barron, Dimaye Calvo, Esteban Cardona, Andrea Carmona,
predominant at the HEROES-RECOVER cohort study Alissa Coleman, Zoe Baccam, Emily Cooksey, Kiara Earley,
sites; however, this trend should be interpreted with caution Natalie Giroux, Sofia Grijalva, Allan Guidos, Adrianna Hernandez,
because VE might also be declining as time since vaccination James Hollister, Theresa Hopkins, Rezwana Islam, Krystal Jovel,
increases and because of poor precision in estimates due to Olivia Kavanagh, Jonathan Leyva, Sally Littau, Amelia Lobos,
limited number of weeks of observation and few infections James Lopez, Veronica Lugo, Jeremy Makar, Taylor Maldonado,
Enrique Marquez, Allyson Munoz, Assumpta Nsengiyunva,
among participants. As with all observational VE studies,
Joel Parker, Jonathan Perez Leyva, Alexa Roy, Saskia Smidt,
unmeasured and residual confounding might be present. Active Isabella Terrazas, Tahlia Thompson, Heena Timsina, Erica Vanover,
surveillance through the cohort is ongoing and VE estimates Mandie White, April Yingst, Kenneth Komatsu, Elizabeth Kim,
2 MMWR / August 24, 2021 / Vol. 70
Early Release
Karla Ledezma, University of Arizona, Arizona Department of Fiona Tsang, Maya Wheeler, Gretchen Maughan, Taryn Hunt-Smith,
Health Services; David Engelthaler, Translational Genomics Nikki Gallacher, Anika DSouza, Trevor Stubbs, Iman Ibrahim,
Research Institute; Lauren E.W. Olsho, Danielle R. Hunt, Ryder Jordin, University of Utah; Marilyn J. Odean, Whiteside
Laura J. Edwards, Meredith G. Wesley, Meghan K. Herring, Institute for Clinical Research; Allen Bateman, Erik Reisdorf,
Tyler C. Morrill, Brandon P. Poe, Brian Sokol, Andrea Bronaugh, Kyley Guenther, Erika Hanson, Wisconsin State Laboratory of
Tana Brummer, Hala Deeb, Rebecca Devlin, Sauma Doka, Hygiene; the HEROES-RECOVER participants.
Tara Earl, Jini Etolue, Deanna Fleary, Jessica Flores, Chris Flygare, Corresponding author: Ashley Fowlkes, afowlkes@cdc.gov
Isaiah Gerber, Louise Hadden, Jenna Harder, Lindsay LeClair,
1CDC COVID-19 Response Team; 2Baylor Scott and White Health, Texas
Nancy McGarry, Peenaz Mistry, Steve Pickett, Khaila Prather,
A&M University College of Medicine, Temple, Texas; 3Abt Associates, Inc.,
David Pulaski, Rajbansi Raorane, Meghan Shea, John Thacker, Rockville, Maryland; 4University of Utah, Salt Lake City, Utah; 5St. Luke’s
Matthew Trombley, Pearl Zheng, Chao Zhou, Abt Associates; Regional Health Care System, Duluth, Minnesota; 6Mel and Enid Zuckerman
Kayan Dunnigan, Spencer Rose, Tnelda Zunie, Michael E. Smith, College of Public Health, University of Arizona, Tucson, Arizona.
Kempapura Murthy, Nicole Calhoun, Claire Mathenge, Arundhati Rao, All authors have completed and submitted the International
Manohar Mutnal, Linden Morales, Shelby Johnson, Alejandro Arroliga, Committee of Medical Journal Editors form for disclosure of
Madhava Beeram, Joel Blais, Jason Ettlinger, Angela Kennedy, potential conflicts of interest. Matthew S. Thiese reports grants and
Natalie Settele, Rupande Patel, Elisa Priest, Jennifer Thomas, personal fees from Reed Group and the American College of
Baylor Scott & White Health; Allison L. Naleway, Holly C. Groom, Occupational and Environmental Medicine, outside the submitted
Jennifer L. Kuntz, Yolanda Prado, Daniel Sapp, Mi Lee, Chris Eddy, work. No other potential conflicts of interest were disclosed.
Matt Hornbrook, Danielle Millay, Dorothy Kurdyla, Ambrosia Bass,
Kristi Bays, Kimberly Berame, Cathleen Bourdoin, Carlea Buslach, References
Jennifer Gluth, Kenni Graham, Tarika Holness Enedina Luis, 1. Thompson MG, Burgess JL, Naleway AL, et al. Prevention and
Abreeanah Magdaleno, DeShaun Martin, Joyce Smith-McGee, attenuation of Covid-19 with the BNT162b2 and mRNA-1273 vaccines.
Martha Perley, Sam Peterson, Aaron Piepert, Krystil Phillips, N Engl J Med 2021;385:320–9. PMID:34192428 https://doi.
Joanna Price, Sperry Robinson, Katrina Schell, Emily Schield, Natosha org/10.1056/NEJMoa2107058
2. Thompson MG, Burgess JL, Naleway AL, et al. Interim estimates of
Shirley, Anna Shivinsky, Britta Torgrimson-Ojerio, Brooke Wainwright, vaccine effectiveness of BNT162b2 and mRNA-1273 COVID-19
Shawn Westaway, Kaiser Permanente Northwest; Jennifer Meece, vaccines in preventing SARS-CoV-2 infection among health care
Elisha Stefanski, Lynn Ivacic, Jake Andreae, Adam Bissonnette, personnel, first responders, and other essential and frontline workers—
Krystal Boese, Michaela Braun, Cody DeHamer, Timothy Dziedzic, eight U.S. locations, December 2020–March 2021. MMWR Morb Mortal
Joseph Eddy, Heather Edgren, Wayne Frome, Nolan Herman, Wkly Rep 2021;70:495–500. PMID:33793460 https://doi.org/10.15585/
mmwr.mm7013e3
Mitchell Hertel, Erin Higdon, Rosebud Johnson, Steve Kaiser, 3. Herlihy R, Bamberg W, Burakoff A, et al. Rapid increase in circulation
Tammy Koepel, Sarah Kohn, Taylor Kent, Thao Le, Carrie Marcis, of the SARS-CoV-2 B.1.617.2 (Delta) variant—Mesa County, Colorado,
Megan Maronde, Isaac McCready, Nidhi Mehta, Daniel Miesbauer, April–June 2021. MMWR Morb Mortal Wkly Rep 2021;70:1084–7.
Anne Nikolai, Brooke Olson, Lisa Ott, Cory Pike, Nicole Price, PMID:34383734 https://doi.org/10.15585/mmwr.mm7032e2
Christopher Reardon, Logan Schafer, Rachel Schoone, Jaclyn Schneider, 4. Brown CM, Vostok J, Johnson H, et al. Outbreak of SARS-CoV-2
infections, including COVID-19 vaccine breakthrough infections,
Tapan Sharma, Melissa Strupp, Janay Walters, Alyssa Weber, associated with large public gatherings—Barnstable County, Massachusetts,
Reynor Wilhorn, Ryan Wright, Benjamin Zimmerman, Marshfield July 2021. MMWR Morb Mortal Wkly Rep 2021;70:1059–62.
Clinic Research Laboratory; Angela Hunt, Jessica Lundgreen, PMID:34351882 https://doi.org/10.15585/mmwr.mm7031e2
Karley Respet, Jennifer Viergutz, Daniel Stafki, St. Luke’s Regional 5. Lutrick K, Ellingson KD, Baccam Z, et al. COVID-19 infection,
Health Care System; Alberto J. Caban-Martinez, Natasha Schaefer-Solle, reinfection, and vaccine effectiveness in a prospective cohort of Arizona
frontline/essential workers: the AZ HEROES research protocol. JMIR
Paola Louzado Feliciano, Carlos Silvera, Karla Montes, Cynthia Beaver, Res Protoc 2021. Epub May 26, 2021. PMID:34057904 https://doi.
Katerina Santiago, University of Miami; Sarang K. Yoon, Kurt Hegmann, org/10.2196/28925
Andrew L. Phillips, Rachel T. Brown, Camie Schaefer, Arlyne Arteaga, 6. US Department of Health and Human Services. HHS protect public data
Matthew Bruner, Daniel Dawson, Emilee Eden, Jenna Praggastis, hub. Washington, DC: US Department of Health and Human Services;
Joseph Stanford, Jeanmarie Mayer, Marcus Stucki, Riley Campbell, 2021. Accessed August 16, 2021. https://protect-public.hhs.gov/
Kathy Tran, Madeleine Smith, Braydon Black, Madison Tallman,
Chapman Cox, Derrick Wong, Michael Langston, Adriele Fugal,
Readers who have difficulty accessing this PDF file may access the HTML file at https://www.cdc.gov/mmwr/volumes/70/wr/mm7034e4.
htm?s_cid=mm7034e4_w. Address all inquiries about the MMWR Series, including material to be considered for publication, to Editor,
MMWR Series, Mailstop V25-5, CDC, 1600 Clifton Rd., N.E., Atlanta, GA 30329-4027 or to mmwrq@cdc.gov.
MMWR / August 24, 2021 / Vol. 70 3
You might also like
- MD1187 Recruit Vaccination Form E-Version 13Document2 pagesMD1187 Recruit Vaccination Form E-Version 13Isara Nimcharoen100% (1)
- PSAAI Position Statements on COVID-19 VaccinesDocument25 pagesPSAAI Position Statements on COVID-19 VaccinesMonica LowinskiNo ratings yet
- Pepsi Project Ed 220Document13 pagesPepsi Project Ed 220api-511143214No ratings yet
- What Is HomeoprophylaxisDocument6 pagesWhat Is HomeoprophylaxiswrestlerloverNo ratings yet
- J Parenter Enteral Nutr - 2022 - Flordel S Lasierra - Enteral Nutrition in Critically Ill Patients Under Vasoactive DrugDocument11 pagesJ Parenter Enteral Nutr - 2022 - Flordel S Lasierra - Enteral Nutrition in Critically Ill Patients Under Vasoactive DrugROBERTO CARLOS BLANQUICETT CORTINANo ratings yet
- Spibey Et Al., 2008Document8 pagesSpibey Et Al., 2008Mimmo RussoNo ratings yet
- Vaccines For Severe Acute Respiratory Syndrome Virus and Other CoronavirusesDocument30 pagesVaccines For Severe Acute Respiratory Syndrome Virus and Other Coronavirusesluis echeverryfNo ratings yet
- Sero-Epidemiology of Early Rubella Infection Among Young Nulliparous Women in Abonnema, Rivers State, NigeriaDocument9 pagesSero-Epidemiology of Early Rubella Infection Among Young Nulliparous Women in Abonnema, Rivers State, Nigeriaijmb333No ratings yet
- Integrase Inhibitor RaltegravirDocument15 pagesIntegrase Inhibitor RaltegravirNovi SilitongaNo ratings yet
- NarrativeReview - Fluid Management in Children With Severe DengueDocument14 pagesNarrativeReview - Fluid Management in Children With Severe DenguePamela JumpNo ratings yet
- Couden - Final Chikungunya Health Impact Framework PaperDocument15 pagesCouden - Final Chikungunya Health Impact Framework Paperapi-449016836100% (1)
- BullDocument7 pagesBullhawkssensNo ratings yet
- Iu Lawsuit RulingDocument101 pagesIu Lawsuit RulingjasonmoverholtNo ratings yet
- Trump Campaign New Mexico LawsuitDocument42 pagesTrump Campaign New Mexico LawsuitAlgernon D'AmmassaNo ratings yet
- Spaceport Authority - Investigation of Complaint Final ReportDocument362 pagesSpaceport Authority - Investigation of Complaint Final ReportAlgernon D'AmmassaNo ratings yet
- Thirdperiodictest (2022 2023)Document4 pagesThirdperiodictest (2022 2023)Mary Lyn ObejasNo ratings yet
- OET Nursing - Official OET Practice Book 1Document229 pagesOET Nursing - Official OET Practice Book 1vidyaNo ratings yet
- Prevalence and Pattern of Maternal Malaria in Owerri, NigeriaDocument8 pagesPrevalence and Pattern of Maternal Malaria in Owerri, Nigeriaijmb333No ratings yet
- Dengue LancetDocument16 pagesDengue LancetJorge Ricardo Uchuya GómezNo ratings yet
- Relationship Between Glycated Haemoglobin and Renal Function in Diabetic Patients in Port Harcourt J NigeriaDocument8 pagesRelationship Between Glycated Haemoglobin and Renal Function in Diabetic Patients in Port Harcourt J Nigeriaijmb333No ratings yet
- Questions and Answers: Results of Study On Sars-Cov-2 in White-Tailed DeerDocument2 pagesQuestions and Answers: Results of Study On Sars-Cov-2 in White-Tailed DeerCaleb HollowayNo ratings yet
- CCVD OieDocument13 pagesCCVD OieMiftahuddin MadjidNo ratings yet
- Pertusis TreatmentDocument20 pagesPertusis TreatmentJaipratap SinghNo ratings yet
- Ao2021 0045Document14 pagesAo2021 0045che_c812125No ratings yet
- Guang 2020Document6 pagesGuang 2020VANESSA CARIÑONo ratings yet
- Measures of Disease Frequency NOTESDocument22 pagesMeasures of Disease Frequency NOTESSJ JungNo ratings yet
- NURS702 Critique 2Document9 pagesNURS702 Critique 2natalie nodayNo ratings yet
- Lockdown Added Little or Nothing Bristol Did Covid-19 Infections Decline Before Uk LockdownDocument7 pagesLockdown Added Little or Nothing Bristol Did Covid-19 Infections Decline Before Uk LockdownGala LindvallNo ratings yet
- 14 Antiviral TherapyDocument1 page14 Antiviral TherapyPhạm Ngọc MinhNo ratings yet
- Trends in Copper Versus Hormonal Intrauterine Device Breakage (Contraception 2022)Document3 pagesTrends in Copper Versus Hormonal Intrauterine Device Breakage (Contraception 2022)Jessica A. BotelhoNo ratings yet
- Epidemio - Clinical Profile and Management of Female Infertility in The City of IsiroDocument5 pagesEpidemio - Clinical Profile and Management of Female Infertility in The City of IsiroInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Symptoms of RabiesDocument47 pagesSymptoms of RabiesJuri GallosNo ratings yet
- Manage Animal Bites & Prevent RabiesDocument10 pagesManage Animal Bites & Prevent RabiesWilly WizeNo ratings yet
- Hiv PPDocument37 pagesHiv PPJitendra YadavNo ratings yet
- Measuring Disease As SGTDocument5 pagesMeasuring Disease As SGTItharshan Indreswaran33% (3)
- COVID-19 Vaccination Requirements For City EmployeesDocument4 pagesCOVID-19 Vaccination Requirements For City EmployeesKristina KoppeserNo ratings yet
- Emergency Meeting Information Memo 11092021Document2 pagesEmergency Meeting Information Memo 11092021NEWS CENTER MaineNo ratings yet
- Week 4 CPH LEC - Introduction To Epidemiology: Fundamentals of Epidemiology in Public Health PracticeDocument11 pagesWeek 4 CPH LEC - Introduction To Epidemiology: Fundamentals of Epidemiology in Public Health PracticeQueency DangilanNo ratings yet
- Assessment of Immunization Coverage and Its Determinants in Urban Slums of Raipur City, Chhattisgarh Surendra Kumar Painkra, Nirmal Verma, Dhiraj Bhawnani, G.P. SoniDocument7 pagesAssessment of Immunization Coverage and Its Determinants in Urban Slums of Raipur City, Chhattisgarh Surendra Kumar Painkra, Nirmal Verma, Dhiraj Bhawnani, G.P. Soninjmdr100% (1)
- 2011 Nosocomial Infections - Knowledge and Source of Information Among Clinical Health Care Students in GhanaDocument4 pages2011 Nosocomial Infections - Knowledge and Source of Information Among Clinical Health Care Students in GhanaMostafa AbdelrahmanNo ratings yet
- Final SBAM Report-CompressedDocument83 pagesFinal SBAM Report-CompressedCraig MaugerNo ratings yet
- Knowledge and Practices of Umbilical Cord Care Among Mothers Attending Post Natal Clinic at Kampala International University Teaching Hospital, Bushenyi DistrictDocument7 pagesKnowledge and Practices of Umbilical Cord Care Among Mothers Attending Post Natal Clinic at Kampala International University Teaching Hospital, Bushenyi DistrictKIU PUBLICATION AND EXTENSIONNo ratings yet
- Signed PSYCHOSOCIAL CARE IN PALIIATIVE CAREDocument10 pagesSigned PSYCHOSOCIAL CARE IN PALIIATIVE CAREMarianne LayloNo ratings yet
- Knowledge and Risk Factors of Dengue Fever Among Blood DonorsDocument8 pagesKnowledge and Risk Factors of Dengue Fever Among Blood Donorsijmb333No ratings yet
- MDR GNR PreventionDocument45 pagesMDR GNR Preventiondjdiek100% (1)
- HIV/AIDS Quiz - Test Your KnowledgeDocument6 pagesHIV/AIDS Quiz - Test Your KnowledgeSp PpvNo ratings yet
- NYSDOH Weekly Flu RPT 20211204 1639165910938 0Document6 pagesNYSDOH Weekly Flu RPT 20211204 1639165910938 0News10NBCNo ratings yet
- PolicyLab Guidance in Person Education K-12 Educational Settings January 2022Document2 pagesPolicyLab Guidance in Person Education K-12 Educational Settings January 2022Kristina KoppeserNo ratings yet
- 2021 Covid-19 Vaccination Guidance v3-0Document12 pages2021 Covid-19 Vaccination Guidance v3-0lucaste50No ratings yet
- COVID-19 Guidance For Operating Schools Safely 728838 7Document3 pagesCOVID-19 Guidance For Operating Schools Safely 728838 7WXYZ-TV Channel 7 DetroitNo ratings yet
- BANS-184 Important QuestionsDocument31 pagesBANS-184 Important QuestionsRahul Singh RajputNo ratings yet
- 8.23.21 DRAFT of Safe Return To In-Person Learning Plan 21-22Document7 pages8.23.21 DRAFT of Safe Return To In-Person Learning Plan 21-22Hannah Shirley100% (1)
- Seminar Report Final Year CT ScanDocument13 pagesSeminar Report Final Year CT ScanKapil SidhpuriaNo ratings yet
- 20210511-Press Release MR G. H. Schorel-Hlavka O.W.B. Issue - THE LIVING DEADDocument7 pages20210511-Press Release MR G. H. Schorel-Hlavka O.W.B. Issue - THE LIVING DEADGerrit Hendrik Schorel-HlavkaNo ratings yet
- Assessment of Activities of Daily Living in Patients Post COVID-19: A Systematic ReviewDocument18 pagesAssessment of Activities of Daily Living in Patients Post COVID-19: A Systematic Reviewjavieron11No ratings yet
- Excercise 2 - Frequency MeasureDocument6 pagesExcercise 2 - Frequency MeasureAnonymous aH8gCZ7zj75% (4)
- COVID Vaccine Systematic Review Dong Dai WeiDocument14 pagesCOVID Vaccine Systematic Review Dong Dai WeiJason SnapeNo ratings yet
- Qualitative Study On Barriers To Access From The Perspective of Patients and OncologistsDocument6 pagesQualitative Study On Barriers To Access From The Perspective of Patients and OncologistsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 2020-SEBS-0956 - State of MichiganDocument3 pages2020-SEBS-0956 - State of MichiganCaleb Holloway100% (1)
- Chapter 1 The Cold ChainDocument18 pagesChapter 1 The Cold ChainCamae Echin CelisNo ratings yet
- Nciph ERIC6Document4 pagesNciph ERIC6bejarhasanNo ratings yet
- Doctrine of Corporate ResponsibilityDocument2 pagesDoctrine of Corporate ResponsibilityMar VicNo ratings yet
- Knowledge, Attitude and Practice Towards COVID-19 Vaccination Among Adults of Sullia Taluk in Dakshin Kannada District of Karnataka - A Community Based Survey)Document8 pagesKnowledge, Attitude and Practice Towards COVID-19 Vaccination Among Adults of Sullia Taluk in Dakshin Kannada District of Karnataka - A Community Based Survey)International Journal of Innovative Science and Research TechnologyNo ratings yet
- FAQ Bank - Masterlist (RD2 RELEASE) Updated As of 12 March 2021Document19 pagesFAQ Bank - Masterlist (RD2 RELEASE) Updated As of 12 March 2021Jek RicoNo ratings yet
- Covid 19 Epi Report Schools FinalDocument1 pageCovid 19 Epi Report Schools FinalSharon PfeiferNo ratings yet
- 2022 Capital Outlay Projects by CountyDocument29 pages2022 Capital Outlay Projects by CountyAlgernon D'AmmassaNo ratings yet
- New Mexico Public Health Orders Aug. 17, 2021Document11 pagesNew Mexico Public Health Orders Aug. 17, 2021Algernon D'AmmassaNo ratings yet
- "We Will Not Comply" BillDocument4 pages"We Will Not Comply" BillAlgernon D'Ammassa100% (2)
- Aug. 17 2020 New Mexico Public Health Order On VaccinesDocument7 pagesAug. 17 2020 New Mexico Public Health Order On VaccinesAlgernon D'AmmassaNo ratings yet
- Aug. 17 2021 New Mexico Public Health Order On MasksDocument4 pagesAug. 17 2021 New Mexico Public Health Order On MasksAlgernon D'AmmassaNo ratings yet
- 55 - State OF NEW Mexico - , 2022: TH Legislature Second SessionDocument3 pages55 - State OF NEW Mexico - , 2022: TH Legislature Second SessionAlgernon D'AmmassaNo ratings yet
- March 2022 OIG Report On Torrance County Detention FacilityDocument19 pagesMarch 2022 OIG Report On Torrance County Detention FacilityAlgernon D'AmmassaNo ratings yet
- COVID 19 VOC Case Report - 07.26.21Document8 pagesCOVID 19 VOC Case Report - 07.26.21Algernon D'AmmassaNo ratings yet
- 7.27.2021 Speak Easy - Cease and Desist OrderDocument13 pages7.27.2021 Speak Easy - Cease and Desist OrderJim Parker100% (1)
- Doña Ana County Return To Work Directive 05.15.2021Document2 pagesDoña Ana County Return To Work Directive 05.15.2021Algernon D'AmmassaNo ratings yet
- May 19, 2021 Legislative Hearing On Borderland Economic DevelopmentDocument15 pagesMay 19, 2021 Legislative Hearing On Borderland Economic DevelopmentAlgernon D'AmmassaNo ratings yet
- TRIP New Mexico Transportation by The Numbers Report March 2021Document19 pagesTRIP New Mexico Transportation by The Numbers Report March 2021Algernon D'AmmassaNo ratings yet
- New Mexico Public Health Order Feb. 24, 2021Document15 pagesNew Mexico Public Health Order Feb. 24, 2021Algernon D'AmmassaNo ratings yet
- Vaccine Mandate Memo 012921Document2 pagesVaccine Mandate Memo 012921Algernon D'AmmassaNo ratings yet
- Cease and Desist - Dona Ana Republican PartyDocument10 pagesCease and Desist - Dona Ana Republican PartyAlgernon D'AmmassaNo ratings yet
- Letter To Steinborn 3-18-19 Clearing InvestigationDocument1 pageLetter To Steinborn 3-18-19 Clearing InvestigationAlgernon D'AmmassaNo ratings yet
- PHO - Activation of CSC and TCADocument6 pagesPHO - Activation of CSC and TCAAlgernon D'AmmassaNo ratings yet
- PHO - Non-Essential SurgeriesDocument3 pagesPHO - Non-Essential SurgeriesAlgernon D'AmmassaNo ratings yet
- Requested Investigation Into Steinborn 2-26-19Document14 pagesRequested Investigation Into Steinborn 2-26-19Algernon D'AmmassaNo ratings yet
- 2020 07 07 Kinder Morgan Notice of ViolationDocument3 pages2020 07 07 Kinder Morgan Notice of ViolationAlgernon D'AmmassaNo ratings yet
- Well Behaved WomenDocument141 pagesWell Behaved WomenBrad GlasmanNo ratings yet
- A Somatic Symptom DisorderDocument2 pagesA Somatic Symptom DisorderAbdul Nisar JilaniNo ratings yet
- SingleSheet ISO22716 EN USLTRDocument1 pageSingleSheet ISO22716 EN USLTRPatrick FlowerdayNo ratings yet
- 01 Uk Biodata ChecklistDocument1 page01 Uk Biodata ChecklistJulie Ann BeranNo ratings yet
- Chap 2&4&5Document47 pagesChap 2&4&5Christian Philip VillaNo ratings yet
- Treatments of AutismDocument2 pagesTreatments of AutismseemabNo ratings yet
- Psychology Course OutlineDocument2 pagesPsychology Course Outlineapi-359950984No ratings yet
- Rigor Mortis in FishDocument9 pagesRigor Mortis in FishddfqclNo ratings yet
- Quarter 4 Assessment Test 4 Mapeh 7: Guipos National High School Poblacion, Guipos Zamboanga Del SurDocument2 pagesQuarter 4 Assessment Test 4 Mapeh 7: Guipos National High School Poblacion, Guipos Zamboanga Del SurCristia Marie Combalicer ColastreNo ratings yet
- Exxi 010 00 00 HS PLN 0002 1Document116 pagesExxi 010 00 00 HS PLN 0002 1USER OEMNo ratings yet
- Original Research ArticleDocument11 pagesOriginal Research ArticleswabrijNo ratings yet
- Handling of Out of Specification Results: International Journal of Pharmaceutical Quality Assurance April 2015Document8 pagesHandling of Out of Specification Results: International Journal of Pharmaceutical Quality Assurance April 2015Haroon RasheedNo ratings yet
- Contoh Kuesioner Knowledge, Attitude and Practice EnglishDocument8 pagesContoh Kuesioner Knowledge, Attitude and Practice EnglishElisabeth FransiskaNo ratings yet
- Paula Valeza, RN CVDocument1 pagePaula Valeza, RN CValraisihuman1122No ratings yet
- Mbbs Admission 2022 Student StatusDocument122 pagesMbbs Admission 2022 Student StatusShreyasNo ratings yet
- Roughan and Flecknell, 2006Document16 pagesRoughan and Flecknell, 2006Paul FlecknellNo ratings yet
- Problematizing Perfectionism - A Closer Look at The Perfectionism ConstructDocument10 pagesProblematizing Perfectionism - A Closer Look at The Perfectionism ConstructShelbi WatsonNo ratings yet
- FNCPDocument8 pagesFNCPVanessa Mae Dela CruzNo ratings yet
- Acupuncture For Primary Dysmenorrhea A Randomized Controlled TrialDocument3 pagesAcupuncture For Primary Dysmenorrhea A Randomized Controlled TrialAnnis RohmawatiNo ratings yet
- SD202005国内外康养旅游研究展望Document11 pagesSD202005国内外康养旅游研究展望Jo LNo ratings yet
- Jurnal 4Document5 pagesJurnal 4Nindita RahmaNo ratings yet
- Module 5: Understanding Global Networks: GlobalizationDocument4 pagesModule 5: Understanding Global Networks: GlobalizationKasnhaNo ratings yet
- ADAM MILO Service PortfolioDocument9 pagesADAM MILO Service Portfoliojayce100% (1)
- UNITY GMC - RFQ With DataDocument27 pagesUNITY GMC - RFQ With DataBOC ClaimsNo ratings yet
- Beyond Wedge: Clinical Physiology and The Swan-Ganz CatheterDocument12 pagesBeyond Wedge: Clinical Physiology and The Swan-Ganz Catheterkromatin9462No ratings yet
- Protocol For Prevention and Control of DiabetesDocument90 pagesProtocol For Prevention and Control of Diabetessrikanth PosaNo ratings yet
- Understanding Dry Skin and Oily Skin: Causes, Symptoms, and SolutionsDocument14 pagesUnderstanding Dry Skin and Oily Skin: Causes, Symptoms, and SolutionsSameer BisenNo ratings yet