Professional Documents
Culture Documents
Radiation Therapy Overview
Uploaded by
Mae CeaesarOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Radiation Therapy Overview
Uploaded by
Mae CeaesarCopyright:
Available Formats
PPT 9 – Radiation Therapy
RADIATION THERAPY
• Is a local treatment modality for cancer and it is the destruction of cancer cells by ionizing radiation
• Purpose: is to destroy malignant cells which are more sensitive to radiation than are normal cells without
permanent damage to adjacent body tissues
Discussions:
• A component of treatment for ½-2/3 of all patients with cancer
May be used as a Primary, Adjuvant, or a Palliative treatment modality - can be used to relieve pain caused by
obstruction, pathologic fractures, spinal cord compression and metastases.
Discussions:
• PRIMARY - (e.g., early-stage skin cancer, Hodgkin’s disease, carcinoma of the cervix.
• ADJUVANT - it can be used in conjunction with chemotherapy to enhance destruction of cancer cells.
Methods of Delivering Radiation Therapy
Radiation Therapy is used two different ways;
To cure cancer:
• Destroy tumors that have not spread to other body parts.
• Reduce risk that cancer will return after surgery or chemotherapy
To reduce symptoms;
• Shrink tumors affecting quality of life, like a lung tumor that is causing shortness of breath.
• Alleviate pain by reducing the size of tumor.
Types of Radiation Therapy
Externally (Teletherapy, DXT) – external beam radiation
– Delivers radiation using a linear accelerator
– This is administered through a high – energy X-ray or gamma x-ray machine*
– The major advantage of high-energy radiation is its skin – sparing effect.
Discussions:
• * (e.g., linear accelerator, cobalt, betatron, or a machine containing radioisotope).
• * The maximum effect of radiation occurs at tumor deep in the body, not on the skin surface.
• * There is no need for isolation.
Specialized Types of External Beam Radiation Therapy
Three-dimensional conformal radiation therapy (3D-CRT)
– Uses CT or MRI scans to create a 3-D picture of the tumor.
– Beams are precisely directed to avoid radiating normal tissue
Intensity Modulated Radiation Therapy (IMRT)
– A specialized form of 3D-CRT
– Radiation is broken into many “beamlets” and the intensity of each can be adjusted individually
Proton Beam Therapy
– Uses protons rather than x-rays to treat certain types of cancer.
– Allows doctors to better focus the dose on the tumor with the potential to reduce the dose to
nearby healthy tissue
Neutron Beam Therapy
– A specialized form of radiation therapy that can be used to treat certain tumors that are very
difficult to kill using conventional radiation therapy
Stereotactic Radiotherapy
– Sometimes called stereotactic radiosurgery
– This technique allows the radiation oncologist to precisely focus beams of radiation to destroy
certain tumors, sometimes in only one treatment
– Stereotactic radiosurgery (SRS) is a non-surgical radiation therapy used to treat functional
abnormalities and small tumors of the brain.
– It can deliver precisely targeted radiation in fewer high-dose treatments than
traditional therapy, which can help preserve healthy tissue.
PPT 9 – Radiation Therapy
Systems which produce different types of radiation for external beam therapy include:
A) orthovoltage x-ray machines,
B) Cobalt-60 machines,
C) linear accelerators,
D) proton beam machines, and
E) neutron beam machines.
Internally (Brachytherapy or Seed implants) – internal radiation therapy
– Involves placing radioactive sources inside the patient.
– Places radioactive material into tumor or surrounding tissue
– Also called Brachytherapy – brachy Greek for “short distance”
– Radiation sources placed close to the tumor so large doses can hit the cancer cells
– Allows minimal radiation exposure to normal tissue
– the radioisotope is placed in needles, beads, seeds, ribbons, or catheters, which are then implanted
directly into the tumor*
Discussions:
• This can be either permanently or temporarily placed in the body
THE MAJOR TYPES OF INTERNAL RADIATION THERAPY
A. SEALED SOURCE – (brachytherapy) the radioisotope is placed within or near the tumor.
• is used for both intracavitary and interstitial therapy
Discussions:
• The radioactive material is enclosed in a sealed container.
o INTRACAVITY RT is used to treat cancers of the uterus and cervix. The radioisotope is placed in the
body cavity, generally for 24 to 72 hrs.
o INTERSTITIAL THERAPY, the radioisotope is placed in needles, beads, seeds, ribbons, or catheters,
which are then implanted directly into the tumor
Discussions:
• In sealed sources of internal radiation, the radioisotope cannot circulate through the client’s body, nor can it
contaminate the client’s urine, sweat, blood or vomitus. *
• However, radiation exposure can result from direct contact with the sealed radioisotope, such as touching the
container with bare hands or from lengthy exposure to the sealed radioisotope.
• Therefore, the client’s excretions are not radioactive
B. UNSEALED SOURCE
– The radioisotopes may be administered intravenously, orally or by instillation directly into the body
cavity.
– the radioisotope circulates through the client’s body.
• Discussions:
• Therefore, the client’s urine, sweat, blood and vomitus contain the radioactive isotope.
PRINCIPLES OF RADIATION PROTECTION - DTS
D – istance
The greater the distance from the radiation source, the less the exposure dose of ionizing rays.
Maintain a distance of at least 3 feet when not performing nursing procedures.
Performed in closed proximity such as checking placement of the implant & performing nursing procedures
T – ime
Limit contact with the client for 5 minutes each time, a total of 30 minutes per 8-hour shift
Organize care to limit the amount of time spent in direct contact with the patient
Spend less time with the patient without sacrificing the quality of care given
S – hielding
PPT 9 – Radiation Therapy
Use lead shield during contact with client
Pregnant staff should not be assigned to clients receiving internal RT
If available, & no care should be delivered without wearing a film badge.
The film badge should not be shared, should not be worn other than at work, & should be returned according to
the agency’s protocol
Discussions:
• The badge (radiation dosimeter badge) will indicate cumulative radiation exposure.
Staff members caring for the client with internal RT should wear radiation dosimeter badge while in the client’s room.
Discussions:
• measures the radiation dose that the individual has received through exposure to the source
If the client with cancer of the cervix has radioisotope implant into the uterus, the following nursing interventions should
be implemented.
1. Client’s back is turned towards the door.
- To minimize exposure of healthcare staff to radioisotope entering the client’s room.
2. Encourage the client to turn to sides at regular intervals
3. The client should be on complete bed rest.
- to prevent dislodgement of the radioisotope.
4. The client should be given enema before the procedure.
- Bowel movement during the procedure may cause dislodgement of the radioisotope.
5. The client should be given low fiber diet to inhibit defecation during the procedure until the device is removed in 2-3
days.
- to prevent dislodgement of the radioisotope
6. The client should have a Foley catheter in place during the procedure.
- to prevent bladder distention and subsequently prevent irradiation of the bladder.
7. Have long forceps and lead container readily available. Use long forceps to pick up dislodged radioisotope and place it
in the lead container.
– The client receiving an unsealed source of RT: should have a private room and bath.
– All surfaces, including the floor area the client will be walking on, are covered with Chux or paper.
Foods are served on disposable plates and utensils.
Trash and linens are kept in the client’s room and are not removed until the client is ready for discharge.
- This is to minimize radiation exposure of caregivers.
The client is also instructed to rinse the sink with copious amount of water after tooth brushing and to flush the
toilet several times after each use.
- To prevent radiation contamination of other people and the environment.
Anyone entering the room wears a new pair of booties each time to prevent tracking the radioisotope out into
the hallway.
Caregivers should wear gloves when handling body fluids
Any emesis (vomiting), especially that occurs shortly after ingestion of oral radioisotope, should be covered with
absorbent pads, and the radiation safety officer should be called immediately.
TEACHING GUIDELINES REGARDING EXTERNAL RADIATION THERAPY
1. It is painless
2. Lie very still on a special table while the intervention is being given and you may be placed in a special position
to maximize tumor irradiation.
3. Each treatment usually lasts for few minutes. You may hear sounds of the machine being operated, and the
machine may move during the therapy.
4. As a safety precaution for the therapy personnel, you will remain alone in the treatment room while the
machine is in operation.
PPT 9 – Radiation Therapy
5. The technologist will be right outside your room observing you through a window or by a closed – circuit TV.
You may communicate.
6. There is no residual radioactivity after radiation therapy. Safety precautions are necessary only during the time
you are receiving irradiation. You may resume normal activities of daily living.
CLIENT EDUCATION ON SKIN CARE IN EXTERNAL RADIATION THERAPY
Skin Care within The Treatment Area includes the following:
Keep your skin dry.
Do not wash the treatment area until you are instructed to do so. When permitted, wash the treated skin gently
with mild soap, rinse well, and pat dry. Use warm water or cool water, not hot water.
Do not remove the lines or ink marks (markings) placed on your skin
Avoid using powders, lotions, creams, alcohol and deodorants on the treated skin.
Wear loose – fitting clothing to avoid friction over the treatment area.
Do not apply tape to the treatment area if dressings are applied.
Shave with an electric razor. Do not use pre-shave or after-shave lotions.
Protect your skin from exposure to direct sunlight, chlorinated swimming pools, and temperature extremes*
Consult your radiation therapist or nurse about specific measures for individual skin reactions.
INTERVENTIONS FOR SIDE EFFECTS OF RADIATION THERAPY
1. SKIN REACTIONS
erythema, dry/moist desquamation
atrophy, telangiectasia, depigmentation, necrotic/ulcerative lesions.
NURSING INTERVENTIONS:
Observe for early signs of skin reaction and report to the physician.
Keep area dry.
Depigmentation telangiectasia
Washing area with water, no soap and pat dry (do not rub). Mild soap is permitted.
Do not apply ointments, powders or lotion to the area. Cornstarch may be used.
Do not apply heat; avoid direct sunshine or cold on the area.
Use soft cotton fabrics for clothing. To prevent skin irritation.
Do not erase markings on the skin. These serve as guide for areas of irradiation.
2. INFECTION
– this is due to bone marrow suppression
NURSING INTERVENTIONS:
Monitor blood counts weekly, especially WBC
Good personal hygiene, nutrition, adequate rest
Teach the client signs of infection to report to physician
3. HEMORRHAGE
Platelets are vulnerable to radiation.
NURSING INTERVENTIONS:
Monitor platelet count
Avoid physical trauma or use of aspirin(ASA)
Teach signs of hemorrhage to report (e.g., gum bleeding, nose bleeding, black stools)
Monitor stool and skin for signs of hemorrhage
Use direct pressure over injection sites until bleeding stops.
4. FATIGUE
result of high metabolic demands for tissue repair and toxic waste removal
plenty of rest and good nutrition
5. WEIGHT LOSS
anorexia, pain, and effect of cancer
6. STOMATITIS AND XEROSTOMIA (DRY MOUTH)
- Ulceration of oral mucous membrane occurs
PPT 9 – Radiation Therapy
NURSING INTERVENTIONS:
Administers analgesics before meals, as prescribed
Bland diet, avoid smoking and alcohol
Good oral hygiene with saline rinses every 2 hours
Sugarless lemon drops or mint to increase salivation
7. Diarrhea, nausea and vomiting, headache, alopecia (hair loss) and cystitis, may also occur.
8. Social isolation is also experienced by the client due to fear of contaminating others with radiation.
You might also like
- Brach y TherapyDocument3 pagesBrach y Therapydincy danielNo ratings yet
- Radiation Hazards 2Document19 pagesRadiation Hazards 2Rupender HoodaNo ratings yet
- Radiation Therapy & Nuclear MedicineDocument38 pagesRadiation Therapy & Nuclear MedicineGarima KwatraNo ratings yet
- Chapter 16 ITLS - 04-2020Document20 pagesChapter 16 ITLS - 04-2020Ahyar MohNo ratings yet
- Nursing Care Plan for Improving Social InteractionDocument3 pagesNursing Care Plan for Improving Social InteractionMae Ceaesar50% (2)
- RADIOTHERAPHYDocument20 pagesRADIOTHERAPHYMuhammad Hafiz KarimNo ratings yet
- How Does Radiation Therapy Work?Document5 pagesHow Does Radiation Therapy Work?mikeadrianNo ratings yet
- Assignment On Radiation TherapyDocument16 pagesAssignment On Radiation TherapyAxsa AlexNo ratings yet
- OPT Plus Form 2A. Municipality/City Summary Report On Operation Timbang PlusDocument6 pagesOPT Plus Form 2A. Municipality/City Summary Report On Operation Timbang PlusNutri San PabloNo ratings yet
- SMRT Radiation Therapy IntroDocument18 pagesSMRT Radiation Therapy IntroDar WebNo ratings yet
- Radiation Therapy, Nursing Care: CANDO, Precious Gia G. Ncm-105L Afpmc Prof. Dawn Capaque August 17, 2010Document10 pagesRadiation Therapy, Nursing Care: CANDO, Precious Gia G. Ncm-105L Afpmc Prof. Dawn Capaque August 17, 2010aurezeaNo ratings yet
- Radiation Therapy For CancerDocument65 pagesRadiation Therapy For CancermelNo ratings yet
- Biomedical Science Personal StatementDocument2 pagesBiomedical Science Personal StatementbidangeNo ratings yet
- Ey The Sunrise Consumer Health and Nutrition Sector ReportDocument24 pagesEy The Sunrise Consumer Health and Nutrition Sector ReportMantraa Advisory100% (1)
- Use of Radioactive in MedicalDocument28 pagesUse of Radioactive in MedicalroseyacobNo ratings yet
- Radiation Oncology: DR - Durgesh Mishra Dy - Cmo, MJPJAY, MahDocument13 pagesRadiation Oncology: DR - Durgesh Mishra Dy - Cmo, MJPJAY, MahKASATSANo ratings yet
- Radiation Therapy 2013Document59 pagesRadiation Therapy 2013AydinNo ratings yet
- Jurnal 1 MenopauseDocument7 pagesJurnal 1 MenopauseWina widiartinaNo ratings yet
- Radiation TherapyDocument9 pagesRadiation TherapyNica PinedaNo ratings yet
- RadiotherapyDocument60 pagesRadiotherapyAARYANo ratings yet
- (RADIO 250) LEC 10 Radiation OncologyDocument3 pages(RADIO 250) LEC 10 Radiation OncologyWilliam PinzonNo ratings yet
- Recent Advances in Radiation Oncology: DR M Spoorthi Shelometh Department of Radiation OncologyDocument53 pagesRecent Advances in Radiation Oncology: DR M Spoorthi Shelometh Department of Radiation Oncologyspoorthi shelomethNo ratings yet
- Radiation TherapyDocument58 pagesRadiation TherapyRichard Allan SolivenNo ratings yet
- Non Surgical Treatment Modalities of SCCHN: Presentation by Post Gradute StudentDocument113 pagesNon Surgical Treatment Modalities of SCCHN: Presentation by Post Gradute StudentZubair VajaNo ratings yet
- Acute Pain Due To Gastritis Care Plan-G.a.Document1 pageAcute Pain Due To Gastritis Care Plan-G.a.Kristin Bienvenu85% (13)
- An Overview of Measurements in Epidemiology V2 2003Document3 pagesAn Overview of Measurements in Epidemiology V2 2003Nathan AustNo ratings yet
- College of Health Sciences Nursing Care Plan for Fractured FemurDocument5 pagesCollege of Health Sciences Nursing Care Plan for Fractured FemurMae CeaesarNo ratings yet
- Laser / IPL Technology for Skin Care: A Comprehensive Technical and Informative TextbookFrom EverandLaser / IPL Technology for Skin Care: A Comprehensive Technical and Informative TextbookRating: 4 out of 5 stars4/5 (8)
- The Philippine Health AgendaDocument32 pagesThe Philippine Health Agendajustbeingclever100% (2)
- Brachytherapy 140129094056 Phpapp02Document77 pagesBrachytherapy 140129094056 Phpapp02KAZOBA FRANCISNo ratings yet
- Principles of Cancer TreatmentDocument73 pagesPrinciples of Cancer Treatmentmaria erika100% (1)
- Nursing ManagementDocument19 pagesNursing ManagementAbby Trisha MadularaNo ratings yet
- Principles of Diathermy, Radiotherapy and Anesthesia: Dr. Amar KumarDocument18 pagesPrinciples of Diathermy, Radiotherapy and Anesthesia: Dr. Amar KumarSudhanshu ShekharNo ratings yet
- Radiation TherapyDocument4 pagesRadiation Therapypanniyin selvanNo ratings yet
- Handout in MPN 1 Prelims AY 2021-2022: Short TermDocument7 pagesHandout in MPN 1 Prelims AY 2021-2022: Short TermGlory Anne Joy WillyNo ratings yet
- Radiation TherapyDocument7 pagesRadiation TherapyMeenakshi VyasNo ratings yet
- RT 307Document153 pagesRT 307Lyht TVNo ratings yet
- Palliative Radiation TherapyDocument7 pagesPalliative Radiation TherapyJohnasse Sebastian NavalNo ratings yet
- Radiation Therapy: Group 4 and 5Document29 pagesRadiation Therapy: Group 4 and 5Anonymous 596wAK78eCNo ratings yet
- Internal Radiotherapy TreatmentDocument5 pagesInternal Radiotherapy TreatmentWindy HardiyantyNo ratings yet
- Radiotherapy: Hemraj SainiDocument27 pagesRadiotherapy: Hemraj SainiAnuj AryanNo ratings yet
- RT 313 Final NotesDocument38 pagesRT 313 Final NotesGiralph NikkoNo ratings yet
- RT For General PublicDocument24 pagesRT For General Publicraheel252100% (1)
- Cancer Therapy Modalities & Side EffectsDocument9 pagesCancer Therapy Modalities & Side EffectsNeweeJoonYowNo ratings yet
- Clinical Practice 4: Radiotherapy Lecture 5 & 6Document28 pagesClinical Practice 4: Radiotherapy Lecture 5 & 6allordNo ratings yet
- An Assignment: Course Name: Course No.: PHY-5213Document5 pagesAn Assignment: Course Name: Course No.: PHY-5213Tonmoy PaulNo ratings yet
- Managments in Oncology 13OCTDocument49 pagesManagments in Oncology 13OCTM ANo ratings yet
- Ways Radiation Is Used in Medicine - Cobalt 60 Radiotherapy MachineDocument22 pagesWays Radiation Is Used in Medicine - Cobalt 60 Radiotherapy MachineKavidu KeshanNo ratings yet
- Radiation TherapyDocument28 pagesRadiation Therapypalakkhurana012No ratings yet
- Understanding Radiation TherapyDocument24 pagesUnderstanding Radiation Therapyabhilashreddy45No ratings yet
- Title - BT Treatment Procedure For Vaginal CarcinomaDocument21 pagesTitle - BT Treatment Procedure For Vaginal CarcinomaparvezNo ratings yet
- Positive effects of electromagnetic radiationDocument8 pagesPositive effects of electromagnetic radiationTyrone Stavros BarracaNo ratings yet
- Radiation TherapyDocument6 pagesRadiation TherapyKaren Joyce MagtanongNo ratings yet
- Radiation TherapyDocument11 pagesRadiation Therapyrnnr2159No ratings yet
- Radiation Protection in Nuclear MedicineDocument6 pagesRadiation Protection in Nuclear MedicineRamon De GuiaNo ratings yet
- RadiotherapyDocument5 pagesRadiotherapyHertina SilabanNo ratings yet
- Radiation Therapy Chemotherapy Stem Cell Transplantation Biologic Therapy Gene TherapyDocument14 pagesRadiation Therapy Chemotherapy Stem Cell Transplantation Biologic Therapy Gene TherapyPebbles PangilinanNo ratings yet
- Andrew Idoko Radiology GROUP 332 1. The Concept of Radical and Palliative Treatment. Indications, Contraindications Dose Limits. ExamplesDocument5 pagesAndrew Idoko Radiology GROUP 332 1. The Concept of Radical and Palliative Treatment. Indications, Contraindications Dose Limits. ExamplesdreNo ratings yet
- RT 313 Prelim NotesDocument13 pagesRT 313 Prelim NotesGiralph NikkoNo ratings yet
- Stimulus Material (3 Sources)Document6 pagesStimulus Material (3 Sources)Isaac JTNo ratings yet
- Radiation TherapyDocument6 pagesRadiation TherapyLorraine Padlan BaysicNo ratings yet
- OverviewDocument6 pagesOverviewarakbaeNo ratings yet
- Radiography Safety ProcedureDocument9 pagesRadiography Safety ProcedureأحمدآلزهوNo ratings yet
- NCM106-Cellular Aberrations-Module1-Lesson 4Document10 pagesNCM106-Cellular Aberrations-Module1-Lesson 4Esmareldah Henry SirueNo ratings yet
- Cold & Decrease Pain For Circulation - WarmDocument3 pagesCold & Decrease Pain For Circulation - Warmmyer pasandalanNo ratings yet
- Clinical Practice 4: RadiotherapyDocument27 pagesClinical Practice 4: RadiotherapyallordNo ratings yet
- AFCC Working With RadiationDocument35 pagesAFCC Working With RadiationMoch Irvan BadriNo ratings yet
- Medical Uses of Ionizing Radiation: Dr. Ali Sid AhmedDocument17 pagesMedical Uses of Ionizing Radiation: Dr. Ali Sid AhmedX x A7md x XNo ratings yet
- Radiation Therapy Techniques for Gynecological Cancers: A Comprehensive Practical GuideFrom EverandRadiation Therapy Techniques for Gynecological Cancers: A Comprehensive Practical GuideKevin AlbuquerqueNo ratings yet
- Activity No 4Document1 pageActivity No 4Mae CeaesarNo ratings yet
- Activity No 5 PPD UNFINISHEDDocument1 pageActivity No 5 PPD UNFINISHEDMae CeaesarNo ratings yet
- Activity No 3 PPD18Document1 pageActivity No 3 PPD18Mae CeaesarNo ratings yet
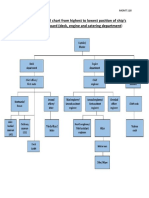
- An Organizational Chart From Highest To Lowest Position of ShipDocument1 pageAn Organizational Chart From Highest To Lowest Position of ShipMae CeaesarNo ratings yet
- Activity No 5 PPD UNFINISHEDDocument1 pageActivity No 5 PPD UNFINISHEDMae CeaesarNo ratings yet
- 112 HTP - HypertensionDocument4 pages112 HTP - HypertensionMae CeaesarNo ratings yet
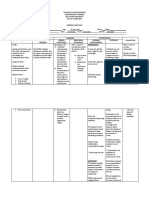
- College of Health Sciences Nursing Care PlanDocument3 pagesCollege of Health Sciences Nursing Care PlanMae CeaesarNo ratings yet
- Reflection About Confidentiality and Privacy in HealthcareDocument1 pageReflection About Confidentiality and Privacy in HealthcareMae CeaesarNo ratings yet
- 112 - Drug Study Naquila Irish May 3EDocument13 pages112 - Drug Study Naquila Irish May 3EMae CeaesarNo ratings yet
- Reflection About Confidentiality and Privacy in HealthcareDocument1 pageReflection About Confidentiality and Privacy in HealthcareMae CeaesarNo ratings yet
- 112 - Drug Study Naquila Irish May 3EDocument20 pages112 - Drug Study Naquila Irish May 3EMae CeaesarNo ratings yet
- Naquila 3E Anemia DISCHARGE INSTRUCTIONS FORMDocument2 pagesNaquila 3E Anemia DISCHARGE INSTRUCTIONS FORMMae CeaesarNo ratings yet
- Reflection 3Document1 pageReflection 3Mae CeaesarNo ratings yet
- Two Assessment Tool 112Document1 pageTwo Assessment Tool 112Mae CeaesarNo ratings yet
- Reflection 5Document1 pageReflection 5Mae CeaesarNo ratings yet
- Reflection 1Document1 pageReflection 1Mae CeaesarNo ratings yet
- Reflection 4Document1 pageReflection 4Mae CeaesarNo ratings yet
- Reflection About Confidentiality and Privacy in HealthcareDocument1 pageReflection About Confidentiality and Privacy in HealthcareMae CeaesarNo ratings yet
- Reflection 4Document1 pageReflection 4Mae CeaesarNo ratings yet
- Reflection 1Document1 pageReflection 1Mae CeaesarNo ratings yet
- Reflection 1Document1 pageReflection 1Mae CeaesarNo ratings yet
- Nurses Progress NotesDocument3 pagesNurses Progress NotesMae CeaesarNo ratings yet
- Reflection 4Document1 pageReflection 4Mae CeaesarNo ratings yet
- Reflection 2Document1 pageReflection 2Mae CeaesarNo ratings yet
- Nurses Progress NotesDocument3 pagesNurses Progress NotesMae CeaesarNo ratings yet
- Reflection 3Document1 pageReflection 3Mae CeaesarNo ratings yet
- Thryoid Cancer NotesDocument1 pageThryoid Cancer NotesMae CeaesarNo ratings yet
- MedSurg Notes - LeukemiaDocument3 pagesMedSurg Notes - LeukemiaMae CeaesarNo ratings yet
- CAB ManagementDocument21 pagesCAB ManagementTery'sNo ratings yet
- Abbott Alinity S FactSheetDocument1 pageAbbott Alinity S FactSheetInayat UllahNo ratings yet
- 1 PDFDocument1 page1 PDFBharti sainNo ratings yet
- ConsensusStatement ChildabuseandmasksDocument4 pagesConsensusStatement ChildabuseandmasksPennLiveNo ratings yet
- Medical Waste Disposal BrochureDocument3 pagesMedical Waste Disposal BrochureRachael HernandezNo ratings yet
- If The Physician Diagnoses The Patient Wrongly He Would Get BeatenDocument4 pagesIf The Physician Diagnoses The Patient Wrongly He Would Get BeatenSheen GabatoNo ratings yet
- Equinox-Operator Quick TipsDocument2 pagesEquinox-Operator Quick TipsDr. Richard JohnsonNo ratings yet
- CA Physician Code of EthicsDocument3 pagesCA Physician Code of EthicsKev TaningcoNo ratings yet
- Tentative CML 2017 - Not Updated - 02.01.2018Document870 pagesTentative CML 2017 - Not Updated - 02.01.2018drgnans36% (11)
- Hyperbaric Versus Plain Bupivacaine For Spinal.20Document9 pagesHyperbaric Versus Plain Bupivacaine For Spinal.20Della Elvina RoeslandNo ratings yet
- PBS Test Study Guide Unit 3 Outbreaks and Emergencies: Key TermsDocument3 pagesPBS Test Study Guide Unit 3 Outbreaks and Emergencies: Key TermsJude ChartierNo ratings yet
- Week 13 CD COURSE TASK 7. Dengue Fever, Filariasis, Malaria and EncephalitisDocument5 pagesWeek 13 CD COURSE TASK 7. Dengue Fever, Filariasis, Malaria and EncephalitisRogelyn PatriarcaNo ratings yet
- Dentistry: A Case of Drug - Induced Xerostomia and A Literature Review of The Management OptionsDocument4 pagesDentistry: A Case of Drug - Induced Xerostomia and A Literature Review of The Management OptionsSasa AprilaNo ratings yet
- Psychosomatic Medicine and BalintworkDocument6 pagesPsychosomatic Medicine and Balintworkcristina sescuNo ratings yet
- Self Injection Made EasyDocument8 pagesSelf Injection Made EasyJames OkamotoNo ratings yet
- Midwife Cover LetterDocument7 pagesMidwife Cover Letterqrhxvwljg100% (1)
- Pulmonary Embolism (PE) PDFDocument9 pagesPulmonary Embolism (PE) PDFMileNo ratings yet
- Role of Pharmacist in Patient CareDocument2 pagesRole of Pharmacist in Patient CareblossomkdcNo ratings yet
- Diagnosis and Management of CowDocument31 pagesDiagnosis and Management of CowSteluta BoroghinaNo ratings yet
- Cochrane LibraryDocument59 pagesCochrane LibraryMadalina BocaNo ratings yet
- ICER ALZ Draft Evidence Report 050521Document123 pagesICER ALZ Draft Evidence Report 050521Renard ChristianNo ratings yet
- Medicare Initial Preventive Physical Examination Encounter Form ("Welcome To Medicare Physical")Document2 pagesMedicare Initial Preventive Physical Examination Encounter Form ("Welcome To Medicare Physical")B PNo ratings yet