Professional Documents
Culture Documents
Shortness of Breath in A 74-Year-Old Woman
Uploaded by
Nicole Villanueva, BSN - Level 3AOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Shortness of Breath in A 74-Year-Old Woman
Uploaded by
Nicole Villanueva, BSN - Level 3ACopyright:
Available Formats
case study [chemistry] Results of Additional Diagnostic Procedures and
Tests
Shortness of Breath A chest X-ray revealed bilateral pleural effusions. An
in a 74-Year-Old Woman electrocardiogram showed normal sinus rhythm. A
Sean M. Hussey, MD, Frank H. Wians, Jr., PhD, MT(ASCP), transthoracic echocardiogram revealed a dilated left
DABCC, FACB atrium, an increase in right-sided filling pressure, and
Department of Pathology, University of Texas Southwestern mild to moderate mitral regurgitation. The left ventricular
Medical Center, Dallas, TX ejection fraction (LVEF) was within normal limits.
DOI: 10.1309/YDG28LC23XQJ0MMV
Questions:
Patient 1. What is (are) this patient’s most striking clinical and
74-year-old Caucasian woman. laboratory result(s)?
Downloaded from https://academic.oup.com/labmed/article/35/7/408/2504416 by guest on 03 September 2021
2. How do you explain the patient’s most striking clinical
Chief Complaint and laboratory result(s)?
Progressive increase in episodic shortness of breath for 3. What condition(s) does this patient’s laboratory and
the past 2 weeks. other findings suggest?
4. What is the pathophysiology of this patient’s disease?
History of Present Illness 5. What are the clinical manifestations of this patient’s
The patient had been in her normal state of health until 2 disease?
weeks ago when she noticed that she had difficulty catching 6. What is the prognosis for this patient?
her breath while walking. She was used to walking 2 miles 7. What is the most appropriate treatment for this patient?
without difficulty, but was now becoming short of breath
after just 100 yards. The symptoms were progressing and
over the past 3 days the patient stated that she was short of
breath lying down. She had always slept with only 1 pillow,
Principal Laboratory Findings
Test Patient’s “Normal”
T1
but was now requiring 2 pillows. The patient also reported
Result Reference Range
an 8 to 10 pound weight gain over the past 6 weeks.
Hematology
WBC count 9.7 4.1-11.1 x103/µL
Past Medical History RBC count 4.19 4.01-5.31 x103/µL
Moderately controlled hypertension for the past 50 years. Hemoglobin 12.0 12.1-16.1 g/dL
Hematocrit 38.3 36.8-48.7%
Platelet count 244 174-404 x103/µL
Past Surgical History Differential: Neutrophils 62 35-80%
Benign parotid gland tumor removed in 1963. Lymphocytes 33 20-50%
Monocytes 4 2-12%
Eosinophils 1 0-7%
Drug History Basophils 0 0-2%
Diovan HCT, once a day; aspirin, 325 mg tablet, prn. Coagulation
PT 10.3 9.8-11.9 sec
INR 0.9
Family/Social History PTT 31.8 23.0-32.5 sec
The patient’s father died at age 56 from a heart attack sec- D-Dimer 0.7 0-3 mg/L
ondary to coronary artery disease. Her mother died at age 77 Chemistry
Sodium 136 135-145 mEq/L
secondary to colon cancer. Her brother died at age 49 from Potassium 3.6 3.6-4.0 mEq/L
an unknown cancer, and her sister died at age 68 from acute Chloride 101 98-109 mEq/L
renal failure secondary to diabetes mellitus. The patient has 4 CO2 25 22-31 mEq/L
BUN 11 7-21 mg/dL
children, all of whom are alive and healthy. She had no his- Creatinine 0.5 0.6-1.2 mg/dL
tory of smoking, alcohol abuse, or blood transfusion. AST 34 13-40 U/L
ALT 28 10-40 U/L
Total protein 7.1 6.3-8.2 g/dL
Physical Examination Albumin 4.2 3.5-5.2 g/dL
408 Vital signs: temperature, 35.8°C; heart rate, 82 beats per Total bilirubin 0.7 0.2-1.3 mg/dL
minute; respiratory rate, 18 breaths per minute; blood Direct bilirubin 0.1 0.0-0.3 mg/dL
BNP 827 <100 pg/mL*
pressure, 157/64 mmHg. The patient was well-nourished
and in no acute respiratory distress (oxygen saturation of *A BNP value <100 pg/mL is generally not consistent with a diagnosis of decompen-
sated heart failure; a BNP value >400 pg/mL is often seen in patients with advanced
95% on room air). Her current weight was 126 pounds. or decompensated heart failure due to left ventricular systolic or diastolic dysfunc-
The patient’s physical exam was normal with clear respi- tion; a BNP value between 100 pg/mL and 400 pg/mL may be difficult to interpret in
patients with concomitant diseases that can affect BNP levels, such as COPD and PE;
ratory sounds and no lower extremity edema. and, BNP results must always be evaluated in concert with other patient-specific clin-
ical and laboratory findings.
WBC, white blood cell; RBC, red blood cell; PT, prothrombin time; INR, International
Principal Laboratory Results Normalized Ratio; PTT, partial thromboplastin time; BUN, blood urea nitrogen; AST, aspar-
[T1]. tate aminotransferase; ALT, alanine aminotransferase; BNP, B-type natriuretic peptide.
laboratorymedicine> july 2004> number 7> volume 35 ©
Possible Answers: Characteristics of Pleural Fluid
1. A progressive dyspnea on exertion (the patient was un-
able to walk 100 yards without getting short of breath);
Transudates and Exudates
PF Characteristic Transudate Exudate
T2
orthopnea; a chest X-ray with bilateral pleural effusions;
an increased right-sided filling pressure on Protein, g/dL <3
LD, U/L <200 >200
echocardiogram; and a markedly increased EDTA-plasma Glucose, mg/dL >60
B-type natriuretic peptide (BNP) level. WBC count/mm3 <1,000
Cholesterol, mg/dL <45 >45
[Protein]PF:[Protein]S <0.5 >0.5
2. Dyspnea on exertion. The causes of shortness of [LD]PF:[LD]S <0.6 >0.6
breath during physical exertion include: 1) pulmonary dis- [Glucose]PF:[Glucose]S 1.0
ease [eg, malignancy, asthma, chronic obstructive Associated diseases Biventricular HF Pneumonia
with venous HTN Lung abscess
pulmonary disease (COPD), pulmonary embolus (PE)]; 2) Nephrotic syndrome Pancreatitis
Downloaded from https://academic.oup.com/labmed/article/35/7/408/2504416 by guest on 03 September 2021
cardiac disease [eg, congestive heart failure (CHF), mitral Peritoneal dialysis Pancreatic pseudocyst
valve prolapse]; 3) deformity of the chest wall; and 4) dis- Atelectasis TB
Urinothorax Actinomycosis
eases associated with weakness of the respiratory muscles. Pleurisy
Orthopnea. Orthopnea, or shortness of breath while lying Asbestosis
down that is relieved with elevating the head, is most Malignant
mesothelioma
often secondary to left ventricular cardiac failure. Other Lymphoma
etiologies include pulmonary congestion, asthma, COPD, Meigs syndrome*
pulmonary infection, chronic cough, obesity, and abdomi- Lung cancer
Pneumothorax
nal distension. Pleural effusions on X-ray. The differen-
tial diagnosis of a pleural effusion is extensive; however, *Triad of benign fibroma (or other ovarian tumors) with ascites and large pleural effu-
sions. PF, pleural fluid; LD, lactate dehydrogenase; WBC, white blood cell; S, serum;
thoracentesis to obtain pleural fluid and analysis of the HF, heart failure; HTN, hypertension; TB, tuberculosis.
fluid for certain constituents allows the fluid to be catego-
rized as a transudate or an exudate [T2]. Transudates
occur when there is an imbalance between hydrostatic and
oncotic pressures (eg, in patients with heart failure in and vasodilation. Among the natriuretic peptides however,
whom the hydrostatic pressure of the fluid in the BNP has been shown to be the most stable to
peritoneal tissue becomes higher than the oncotic pressure degradation, and the most diagnostically specific for
of the fluid in the pleural space causing the movement of identifying patients with CHF and abnormal left ventricu-
fluid from the peritoneum into the pleural space), while lar function.3,4 The right ventricle of the heart pumps
exudates are defined by the presence of at least 1 of the blood directly to the lungs against a much lower resist-
following criteria: 1) [protein]pleural fluid:[protein]serum ratio ance to blood flow compared to the left ventricle which
> 0.5; 2) [LD]pleural fluid:[LD]serum ratio > 0.6; 3) [LD]pleural must pump blood to all other parts of the body against a
1
fluid >200 U/L. The classification of a pleural fluid as a much greater resistance to blood flow. Thus, patients with
transudate or exudate can be useful in suggesting CHF can have abnormal left ventricular function or mitral
additional testing for differentiating between various diag- regurgitation [ie, failure of the mitral (or bicuspid) valve
noses. In the case of this patient, the effusions were too to prevent blood from flowing back into the left atrium
small to warrant a thoracentesis. Therefore, the differential from the left ventricle]. The principal hemodynamic
diagnosis must include conditions associated potentially measure of left ventricular function is the left ventricular
with either a transudative or an exudative pleural fluid, ejection fraction (LVEF). The LVEF is determined by M-
including CHF, liver cirrhosis, nephrotic syndrome, infec- mode or 2D echocardiography and a normal functioning
tion (bacterial, viral, mycobacterial), drug-induced (the left ventricle ejects through the aorta >50% of its end di-
most common being treatment with amiodarone or nitro- astolic blood volume. Both BNP and NT-proBNP are ele-
furantoin), sarcoidosis, systemic lupus erythematosis vated in patients with signs and symptoms of HF and
(SLE), rheumatoid arthritis, pancreatitis, and PE. abnormal left ventricular function (LVF) [F2 and F3] or
Elevated BNP. B-type (or brain, the tissue in which it was LVEF [F4A and F4B] according to the scheme for evaluat-
first discovered) natriuretic peptide (BNP) is a small pro- ing the severity of CHF developed by the New York Heart 409
tein (32 amino acids) produced following the cleavage of Association (NYHA).3-5 However, mitral regurgitation,
a larger precursor protein (proBNP) that yields the physio- trauma, abdominal or thoracic surgery, subarachnoid hem-
logically inactive N-terminal proBNP molecule (NT- orrhage, certain brain disorders, and diabetic nephropathy
proBNP) and the physiologically active hormone, BNP have all been shown to raise natriuretic peptide levels.6
[F1]. The family of natriuretic peptides includes atrial na- Moreover, elevated BNP levels (>80 pg/mL) in patients
triuretic peptide (ANP), BNP, and C-type natriuretic pep- with an acute coronary syndrome are associated with a
tide (CNP), all of which are involved in the regulation of higher incidence of death, new or progressive CHF, and
blood pressure and fluid homeostasis.2 The basic functions new or recurrent myocardial infarction.7 Our patient had a
of the natriuretic peptide hormones are: natriuresis, diuresis, normal LVEF, but mild to moderate mitral regurgitation,
© laboratorymedicine> july 2004> number 7> volume 35
D R I S
9 M S
0 K S
R
S
1
C
G
H 2N-
H F
P L C C L 10 0
G S
1
P G
S A 0
proBNP G
C
K
S 7 S V
0 8 G L
Q 10 8
Y T L 0 V R
R A 7 K M R
P 6 P H — C OOH
R S
Cleavage
Downloaded from https://academic.oup.com/labmed/article/35/7/408/2504416 by guest on 03 September 2021
D R I S
M S
K S
R S
C
G
F
1 1
0
7
0
7
6
C C L
H 2N- H P L G S P G S A S Y T L R A P R —C OOH C
S G K
V
G
Q L
V R
M R
NT-proBNP P K BNP H —C OOH
H 2N- S
(physiologically inactive) (physiologically active)
[F1] Formation of BNP (32 amino acids) and NT-proBNP (76 amino acids) from cleavage of the proBNP (108 amino acids) precursor molecule.
thus accounting for her markedly elevated EDTA-plasma primary care patients than in individuals selected from a
BNP level. The diagnostic accuracy of BNP as a screening cross-section of a community or general population [T3].8
test for CHF depends on the nature of the population being
screened. As expected, the diagnostic accuracy (ie, sensitiv- 3. Most likely diagnosis: congestive heart failure (CHF).
ity and specificity) of BNP in identifying patients with heart The constellation of our patient’s clinical and laboratory find-
failure or LV systolic dysfunction is higher in symptomatic ings, including dyspnea on exertion, orthopnea, bilateral
Healthy De
cre
as
Asymptomatic
ing
LV
No SOB w/ or w/o exercise F an
Normal LVF dI
NYHA I nc
rea
Asymptomatic w/LVD sin
gS
Asymptomatic ev
No SOB w/ or w/o exercise eri
ty
Abnormal LVF of
NYHA II HF
Compensated CHF
Asymptomatic
SOB w/exercise
Abnormal LVF NYHA III
Decompensated CHF
410
Symptomatic
Marked SOB w/exercise
Abnormal LVF
NYHA IV
Refractory CHF
Symptomatic at rest
SOB w/o exercise
Abnormal LVF even w/R x
[F2] The evolution of the clinical stages of congestive heart failure (CHF) according to the classification scheme developed by the New York
Heart Association (NYHA). SOB, shortness of breath; LVD, left ventricular dysfunction; LVF, left ventricular function; Rx, therapy.
laboratorymedicine> july 2004> number 7> volume 35 ©
pleural effusions, increased right-sided cardiac filling pres-
1600
[Natriuretic Peptide], pg/mL
sure, mild to moderate mitral regurgitation, and an elevated NT-proBNP
plasma BNP level makes CHF the most likely diagnosis. 1200
BNP
4. Pathophysiology of CHF. Congestive heart failure is 800
the result of an alteration of Starling forces in the cardiac
contractile myocytes. This alteration is most often related 400
to an index event. That event could be acute, as occurs
0
with an acute myocardial infarction, or chronic, such as Healthy HTN I II III IV
long-standing hypertension or mitral valve disease. The [CHF Classification, NYHA Class]
patient had both chronic hypertension and mitral regurgi-
tation. With mitral valve insufficiency, increased loading
[F3] Relative concentrations of B-type natriuretic peptide (BNP) and
Downloaded from https://academic.oup.com/labmed/article/35/7/408/2504416 by guest on 03 September 2021
conditions (ie, increased blood requirements by the tissues N-terminal pro-BNP (NT-proBNP) in healthy patients, patients with
brought on by increased exercise resulting in a higher hypertension (HTN), or congestive heart failure (CHF) of variable
heart rate as the heart works harder to keep up with the severity (Class I, least severe to Class IV, most severe) according to
demand for blood) lead to abnormal chemical signals the CHF classification scheme developed by the New York Heart
being sent to the cardiac myocytes and fibroblasts that Association (NYHA).
cause myocyte hypertrophy and an increase in collagen
deposition in the heart wall, a process known as “remodel-
ing.”9 Myocytes elongate eccentrically and consequently natriuretic peptides increase to compensate for these
the cardiac chamber dilates. This leads to alterations in changes. Over time, however, these mechanisms may fail
the anatomical relationship between the papillary heart to relieve the stress on the heart and when this occurs, de-
muscles and the valve leaflets, which worsens both the compensated CHF of variable severity results in a medical
valve abnormality and volume overload (dilation) of the emergency requiring prompt medical intervention. The
heart chambers. Over time, the chamber dilation exceeds severity of CHF is gauged typically using the classifica-
the myocyte hypertrophy and leads to increased cardiac tion scheme developed by the New York Heart Association
wall tension and systolic dysfunction. Long-standing hy- (NYHA) [F2].
pertension, on the other hand, results as an increase in the
cross-sectional thickness of individual myocytes. Thus, 5. Clinical manifestations of CHF. Congestive heart fail-
CHF occurs when the heart is incapable of maintaining a ure can manifest itself clinically by a number of non-spe-
cardiac output sufficient to accommodate metabolic cific symptoms including fatigue, decreased appetite, and
requirements for oxygenated blood. When this occurs, increased heart rate. The principal clinical hallmarks of
heart rate, pulse rate, blood pressure, and the release of CHF include pulmonary and peripheral edema from sodium
A B
Abnormal LVEF
[BNP] = 100 pg/mL
[NT- proBNP ] = 125 pg/mL
411
[F4] A) Inverse relationship between NT-proBNP and left ventricular ejection fraction (LVEF) (modified from Reference 3; solid line corresponds
to an NT-proBNP concentration of 125 pg/mL; dotted lines encompass patient groups with an abnormal LVEF (ie, <50%). B) Inverse
relationship between BNP concentration and LVEF (modified from Reference 4; solid line corresponds to an LVEF of 50%; dotted line
corresponds to a BNP concentration of 100 pg/mL). Note that some patients with an abnormal LVEF (ie, <50%) have a BNP
concentration less than a cutoff value of 100 pg/mL.
© laboratorymedicine> july 2004> number 7> volume 35
Diagnostic Performance of BNP as increase the effectiveness of any pharmacologic treatment
a Screening Test for Heart Failure*
Type of Patient Population
T3 regimen. Multiple medications have been shown to im-
prove both cardiac function and CHF symptoms.
Angiotensin converting enzyme (ACE)-inhibitors are con-
Diagnostic Parameter General Symptomatic PC sidered by many to be the first-line of CHF therapy and
Sensitivity 76a 97b act by blocking the production of angiotensin, a hormone
Specificity 87a 84b with significant vasoconstrictor activity, thus lowering the
PPV 16 70 heart’s workload by causing vasodilation. Diuretics are
NPV 98 98
often prescribed to increase the amount of sodium and
*Modified from Reference #8. aAt a BNP cutoff value of 17.9 pg/mL. bAt a BNP cutoff water excreted by the kidneys. This will help decrease the
value of 76.8 pg/mL. BNP, B-type natriuretic peptide; PC, primary care; PPV, positive
predictive value; NPV, negative predictive value. total body fluid volume and decrease cardiac workload.
Digoxin, an inotropic agent that increases the force of the
Downloaded from https://academic.oup.com/labmed/article/35/7/408/2504416 by guest on 03 September 2021
heart’s contractions, is used to improve cardiac contractil-
and water retention. In addition, because of the inadequate ity and decrease atrial fibrillation. Other medications
supply of blood to perfuse all vital organs, blood is used in the treatment of patients with CHF include
shunted away from the periphery to compensate for this vasodilators, beta blockers, calcium channel blockers, and
deficiency. The decreased blood flow to the muscles and anticoagulants. In some patients, insertion of an
limbs leads to fatigue and peripheral edema. Moreover, the automated implantable cardioverter defibrillator (AICD),
stomach also receives less blood, which can lead to diges- or pacemaker, under the skin below the left or right collar
tive problems. Symptoms more specific for cardiac disease bone may be beneficial in reducing mortality due to car-
that are frequently seen in patients with CHF are shortness diac arrhythmias.
of breath, peripheral edema (most often in the lower ex-
tremities), wheezing, and persistent cough. As heart muscle Patient’s Treatment and Course
function declines in patients with CHF, pulmonary pres- The patient was continued on Diovan HCT and started on
sures increase, ultimately progressing to fluid accumulat- Lasix, Toprol, and daily aspirin therapy. She was referred
ing in the air spaces (alveoli) of the lung. Once this for follow-up to the cardiology service. She had several
happens, breathlessness, cough, and wheezing soon follow. follow-up BNP measurements and 6 months following the
Eventually, right-sided heart failure develops followed by initiation of her therapy, her plasma BNP level was 178
leakage of fluid into the peripheral soft tissues. In addition, pg/mL.
decreased renal function secondary to the lack of adequate
renal blood perfusion leads to sodium and water retention Keywords: congestive heart failure, dyspnea, orthop-
by the kidneys and a worsening of the pre-existing periph- nea, B-type natriuretic peptide, pleural fluid,
eral edema. transudate, exudate
6. The prognosis for patients with CHF is variable 1. Celli BR. Diseases of the diaphragm, chest wall, pleura, and mediastinum.
depending on several factors, including age, severity of In: Cecil Textbook of Medicine, 22nd ed, Goldman L, Ausiello D, eds.
Philadelphia: Saunders. 568-576.
the heart failure, and the overall health of the patient.
2. Ruskoaho H, Leskinen H, Magga J, et al. Mechanisms of mechanical load-
Two-thirds of patients with CHF die within 5 years, while induced atrial natriuretic peptide secretion: Role of endothelin, nitric oxide,
20% of patients with CHF die within 12 months of diag- and angiotensin II. J Mol Med. 1997;75:876-885.
nosis. Moreover, the prognosis is slightly worse in men 3. Bay M, Kirk V, Parner J, et al. NT-proBNP: A new diagnostic screening
tool to differentiate between patients with normal and reduced left
than in women. The biggest medical concern in patients ventricular systolic function. Heart. 2003;89:150-154.
with CHF is lethal cardiac arrhythmia, which occurs at a 4. Valli N, Georges A, Corcuff JB, et al. Assessment of brain natriuretic
rate 9 times higher than that of the general population. peptide in patients with suspected heart failure: Comparison with
radionuclide ventriculography data. Clinica Chimica Acta. 2001;306:19-26.
Despite advances in the treatment of hypertension and
5. Maisel AS, Koon J, Krishnaswamy P, et al. Utility of B-natriuretic peptide
myocardial infarction, the survival rate for patients with as a rapid, point-of-care test for screening patients undergoing
CHF has not improved dramatically. Patients can improve echocardiography to determine left ventricular dysfunction. Am Heart J.
2001;141:367-374.
their survival by closely monitoring their diet, controlling
6. Cowe MR, Mendez GF. BNP and congestive heart failure. Prog Cardiovasc
412 their weight, and not smoking or consuming large Dis. 2002;44:293-321.
amounts of alcohol. 7. DeLemos JA, Morrow DA, Bentley JH, et al. The prognostic value of B-
type natriuretic peptide in patients with acute coronary syndromes. N Engl J
Med. 2001;345:1014-1021.
7. The appropriate treatment for patients with CHF usu- 8. Struthers AD. Heart failure: The diagnosis of heart failure. Heart.
ally consists of a combination of prescription medications 2000;84:334-338.
and lifestyle changes. Controlling dietary intake of fats, 9. Gould BE. Pathophysiology for the health professions, 2nd ed.
Philadelphia: WB Saunders Company, 2002, 284-288.
limiting alcohol intake, and smoking cessation can
laboratorymedicine> july 2004> number 7> volume 35 ©
You might also like
- Case Studies: Recurrent Fever, Chills, and Malaise in A 53-Year-Old ManDocument2 pagesCase Studies: Recurrent Fever, Chills, and Malaise in A 53-Year-Old Mansreeja maragoniNo ratings yet
- Nephrolithiasis in A 9 Year OldDocument4 pagesNephrolithiasis in A 9 Year OldJasmin Kae SistosoNo ratings yet
- Recurrent Nephrolithiasis in A 9-Year-Old Child: (University of North Carolina, Chapel Hill, NC)Document4 pagesRecurrent Nephrolithiasis in A 9-Year-Old Child: (University of North Carolina, Chapel Hill, NC)Shaysta KhanNo ratings yet
- Case Studies: Recurrent Headache and Febrile Attacks in A Young WomanDocument4 pagesCase Studies: Recurrent Headache and Febrile Attacks in A Young WomanSimran MgrNo ratings yet
- Case Studies: Fever and Petechiae in A Middle Aged MaleDocument3 pagesCase Studies: Fever and Petechiae in A Middle Aged MaleAadi VermaNo ratings yet
- Diagnostic Test: Material Needed Management of Time Task Type Notes For TeacherDocument6 pagesDiagnostic Test: Material Needed Management of Time Task Type Notes For TeacherYuni NatasyaNo ratings yet
- NCP 1Document5 pagesNCP 1Butchie's ParadiseNo ratings yet
- Fom Pedia Case AnaDocument14 pagesFom Pedia Case AnaFatima MohammedNo ratings yet
- Labmed34 0354Document4 pagesLabmed34 0354zeeshanNo ratings yet
- Data InterpretationDocument36 pagesData Interpretationaijaz.anzaNo ratings yet
- Nursing CareDocument13 pagesNursing CareKelvin TetoNo ratings yet
- 2 LK InternaDocument17 pages2 LK InternaMario KapeNo ratings yet
- Urinary Tract InfectionDocument15 pagesUrinary Tract InfectionAashlen D.No ratings yet
- Case Studies AssignmentDocument4 pagesCase Studies AssignmentCARRAO, Samuel Jr.No ratings yet
- Gilbert2021 Article A17-year-oldBoyWithProgressiveDocument2 pagesGilbert2021 Article A17-year-oldBoyWithProgressivefatinarmiantoNo ratings yet
- Educational Case: Kidney Transplant Rejection: Kevin Kuan, MD and Daniel Schwartz, MDDocument7 pagesEducational Case: Kidney Transplant Rejection: Kevin Kuan, MD and Daniel Schwartz, MDL ANo ratings yet
- STUDENT COPD Pneumonia FUNDAMENTAL - Reasoning PDFDocument8 pagesSTUDENT COPD Pneumonia FUNDAMENTAL - Reasoning PDFYeny PenaNo ratings yet
- ProstateDocument7 pagesProstateGabriela ValdiviaNo ratings yet
- LK IcuDocument9 pagesLK IcuMario KapeNo ratings yet
- Case #4 Asthma (BSN3F, Group3)Document19 pagesCase #4 Asthma (BSN3F, Group3)Eduard GarchitorenaNo ratings yet
- Aac 28 2 347Document2 pagesAac 28 2 347Sat ezNo ratings yet
- Case HipotiroidDocument3 pagesCase HipotiroidVivi DeviyanaNo ratings yet
- XcaretDocument9 pagesXcaretmubarek abdurohemanNo ratings yet
- Clinical Conference 21 August 2022: Eria (New Case)Document16 pagesClinical Conference 21 August 2022: Eria (New Case)mujahidah nursinNo ratings yet
- Case Protocol Kawasaki DiseaseDocument5 pagesCase Protocol Kawasaki DiseaseFranz SalazarNo ratings yet
- Icu Fluids JCDocument3 pagesIcu Fluids JCapi-611386981No ratings yet
- Arciaga, FG - SGDPara 051221Document4 pagesArciaga, FG - SGDPara 051221FG ArciagaNo ratings yet
- Is It Always Anterior Chest Pain Angina Pectoris?Document7 pagesIs It Always Anterior Chest Pain Angina Pectoris?Diana MinzatNo ratings yet
- Educational Case: Anemia in A Neonate: Megan E. Kachur, MD and Benjamin J. Rosen, DODocument9 pagesEducational Case: Anemia in A Neonate: Megan E. Kachur, MD and Benjamin J. Rosen, DOL ANo ratings yet
- Case Report: Grace Y. Kim, MD Helen Anaedo, MD Sahar Nozad, MD Tipu Nazeer, MD Hassan Shawa, MDDocument6 pagesCase Report: Grace Y. Kim, MD Helen Anaedo, MD Sahar Nozad, MD Tipu Nazeer, MD Hassan Shawa, MDPedro Gómez RNo ratings yet
- Marine-Lenhart Syndrome Case ReportDocument5 pagesMarine-Lenhart Syndrome Case ReportEliana InsaurraldeNo ratings yet
- Hypomagnesemia and Prolonged Hospital Stay: A Case Report and Literature ReviewDocument6 pagesHypomagnesemia and Prolonged Hospital Stay: A Case Report and Literature ReviewIJAR JOURNALNo ratings yet
- Ahmad Basori VidiDocument30 pagesAhmad Basori VidiIka AyuNo ratings yet
- Pengantar Modul 2016Document52 pagesPengantar Modul 2016ahmad syaifulNo ratings yet
- Tuberculous Meningitis: Dr. Irbab HawariDocument46 pagesTuberculous Meningitis: Dr. Irbab Hawarimaya raufNo ratings yet
- PBL Als 02Document7 pagesPBL Als 02Danial MazukiNo ratings yet
- PBL Als 02Document7 pagesPBL Als 02Danial MazukiNo ratings yet
- Grand Case FinalDocument13 pagesGrand Case FinalArianne Nicole PinuelaNo ratings yet
- Sepsis E.C Mrss Infection in Patient With Cva: Tropic Infection-1 Case DiscussionDocument47 pagesSepsis E.C Mrss Infection in Patient With Cva: Tropic Infection-1 Case DiscussionIswanto Korompot MonoarfaNo ratings yet
- Perinatal Transient Myeloproliferative Disorder in Trisomy 21Document11 pagesPerinatal Transient Myeloproliferative Disorder in Trisomy 21Carina SuarezNo ratings yet
- Lung Lobe Torsion in Seven Juvenile DogsDocument7 pagesLung Lobe Torsion in Seven Juvenile DogsKelvinSueyzyNo ratings yet
- Student Pain Management Fundamental ReasoningDocument7 pagesStudent Pain Management Fundamental ReasoningSharon TanveerNo ratings yet
- CMC Cns Infection 2023Document5 pagesCMC Cns Infection 2023Juan RecyNo ratings yet
- Bao 2012Document3 pagesBao 2012Salim MichaelNo ratings yet
- NCA BurrholeDocument14 pagesNCA BurrholePhatsee PangilinanNo ratings yet
- Labmed38 0610Document3 pagesLabmed38 0610الشهيد محمدNo ratings yet
- RCT EvinacumabDocument13 pagesRCT EvinacumabMamoNo ratings yet
- Hypokalemic NephropathyDocument7 pagesHypokalemic NephropathyGoris HariyadiNo ratings yet
- NC - Alief Gibran - ERIADocument24 pagesNC - Alief Gibran - ERIADodi DiNo ratings yet
- RHU Case Analysis - Patient XYZDocument17 pagesRHU Case Analysis - Patient XYZaasimon2466cabNo ratings yet
- Case Report Incomplete AbortionDocument26 pagesCase Report Incomplete Abortionrian mourbasNo ratings yet
- Staphylococcus LugdunensisDocument10 pagesStaphylococcus Lugdunensisapi-734715302No ratings yet
- NLR Bells PalsyDocument4 pagesNLR Bells PalsyIskandar HasanNo ratings yet
- CPC For Students 2016Document10 pagesCPC For Students 2016Kwadwo Sarpong JnrNo ratings yet
- Nursing Care Plan SampleDocument2 pagesNursing Care Plan Samplez6cc9vgg6nNo ratings yet
- Case 6Document16 pagesCase 6Arthur AlegriaNo ratings yet
- Labmed46 0e82Document6 pagesLabmed46 0e82FairysparklesNo ratings yet
- Group 4 Activity Ncm120Document3 pagesGroup 4 Activity Ncm120Nicole Villanueva, BSN - Level 3ANo ratings yet
- VillanuevaN Activity1 MagnaCartaofHCWDocument4 pagesVillanuevaN Activity1 MagnaCartaofHCWNicole Villanueva, BSN - Level 3ANo ratings yet
- NCM 118L/ 119L (Related Learning Experience) Day 1-ActivityDocument3 pagesNCM 118L/ 119L (Related Learning Experience) Day 1-ActivityNicole Villanueva, BSN - Level 3ANo ratings yet
- Group 4 Activity Ncm120Document3 pagesGroup 4 Activity Ncm120Nicole Villanueva, BSN - Level 3ANo ratings yet
- Ca WordDocument2 pagesCa WordNicole Villanueva, BSN - Level 3ANo ratings yet
- Importance of Transcultural NursingDocument9 pagesImportance of Transcultural NursingNicole Villanueva, BSN - Level 3ANo ratings yet
- VillanuevaNicole MidtermForum2 RizalDocument6 pagesVillanuevaNicole MidtermForum2 RizalNicole Villanueva, BSN - Level 3ANo ratings yet
- NCM 118 - Questions InterviewDocument2 pagesNCM 118 - Questions InterviewNicole Villanueva, BSN - Level 3ANo ratings yet
- VillanuevaNicole MidtermForum2 RizalDocument6 pagesVillanuevaNicole MidtermForum2 RizalNicole Villanueva, BSN - Level 3ANo ratings yet
- VillanuevaN - Transcultural NursingDefinitionsDocument4 pagesVillanuevaN - Transcultural NursingDefinitionsNicole Villanueva, BSN - Level 3ANo ratings yet
- A. Classification and Characteristics of Diabetes MellitusDocument6 pagesA. Classification and Characteristics of Diabetes MellitusNicole Villanueva, BSN - Level 3ANo ratings yet
- REVISED Group4 Congestive Heart FailureDocument64 pagesREVISED Group4 Congestive Heart FailureNicole Villanueva, BSN - Level 3ANo ratings yet
- Instrument Function Picture Cutting and Dissecting InstrumentsDocument10 pagesInstrument Function Picture Cutting and Dissecting InstrumentsNicole Villanueva, BSN - Level 3ANo ratings yet
- REVISED Group4 Congestive Heart FailureDocument64 pagesREVISED Group4 Congestive Heart FailureNicole Villanueva, BSN - Level 3ANo ratings yet
- VillanuevaN Group4 Day-3-ActivityDocument3 pagesVillanuevaN Group4 Day-3-ActivityNicole Villanueva, BSN - Level 3ANo ratings yet
- Drug Study: Loop DiureticDocument5 pagesDrug Study: Loop DiureticNicole Villanueva, BSN - Level 3ANo ratings yet
- NCM 118L/ 119L (Related Learning Experience) Day 3-ActivityDocument4 pagesNCM 118L/ 119L (Related Learning Experience) Day 3-ActivityNicole Villanueva, BSN - Level 3ANo ratings yet
- Anatomy and PhysiologyDocument3 pagesAnatomy and PhysiologyNicole Villanueva, BSN - Level 3ANo ratings yet
- Case Analysis: Managing Conflict: Leadership and Management Learning Activity 2 - October 20, 2021Document7 pagesCase Analysis: Managing Conflict: Leadership and Management Learning Activity 2 - October 20, 2021Nicole Villanueva, BSN - Level 3ANo ratings yet
- REVISED - Group 4 - Anaphylactic ShockDocument53 pagesREVISED - Group 4 - Anaphylactic ShockNicole Villanueva, BSN - Level 3ANo ratings yet
- Anaphylactic Shock PathoDocument2 pagesAnaphylactic Shock PathoNicole Villanueva, BSN - Level 3ANo ratings yet
- Pathophysiology-LCHFDocument2 pagesPathophysiology-LCHFNicole Villanueva, BSN - Level 3ANo ratings yet
- Fundamentals of Dementia Care For Health Facility PersonnelDocument40 pagesFundamentals of Dementia Care For Health Facility PersonnelNicole Villanueva, BSN - Level 3ANo ratings yet
- VillanuevaN - Transcultural NursingDefinitionsDocument4 pagesVillanuevaN - Transcultural NursingDefinitionsNicole Villanueva, BSN - Level 3ANo ratings yet
- Gender: FemaleDocument9 pagesGender: FemaleNicole Villanueva, BSN - Level 3ANo ratings yet
- Measles: Case Study: Hiro Landazuri Karla Gonzalez Jonathan ChenDocument12 pagesMeasles: Case Study: Hiro Landazuri Karla Gonzalez Jonathan ChenNicole Villanueva, BSN - Level 3ANo ratings yet
- Acoustic Neuroma: Virginia A. Jupiter, PHD, RNDocument18 pagesAcoustic Neuroma: Virginia A. Jupiter, PHD, RNNicole Villanueva, BSN - Level 3ANo ratings yet
- The Eye Disorders: Prof: Anna May B. Gamilla RN MANDocument8 pagesThe Eye Disorders: Prof: Anna May B. Gamilla RN MANNicole Villanueva, BSN - Level 3ANo ratings yet
- Cognitive DisordersDocument51 pagesCognitive Disordersmai-maiNo ratings yet
- UrosepsaDocument2 pagesUrosepsaHazir AziriNo ratings yet
- NursingDocument9 pagesNursingIlie SmarandacheNo ratings yet
- Speech SkincareDocument2 pagesSpeech SkincarePI40621 Fatin Alyaa Binti Abdullah ZawawiNo ratings yet
- Potential Health Benefits of Garlic Allium SativumDocument26 pagesPotential Health Benefits of Garlic Allium SativumAlyssa SagarioNo ratings yet
- Developed by The Teaching History of Pharmacy Committee of The History of Pharmacy SIG, 2017-18Document75 pagesDeveloped by The Teaching History of Pharmacy Committee of The History of Pharmacy SIG, 2017-18Durga MadhuriNo ratings yet
- Psychiatry EmergencyDocument121 pagesPsychiatry EmergencyDr. Jayesh Patidar67% (6)
- Adult Nutrition Assessment Tutorial 2012Document9 pagesAdult Nutrition Assessment Tutorial 2012Dariana floresNo ratings yet
- Meat ScienceDocument320 pagesMeat ScienceVivian Feddern100% (3)
- Critical Thinking Case Study #18:: Sickle-Cell AnemiaDocument15 pagesCritical Thinking Case Study #18:: Sickle-Cell AnemiaHakima Hadji DaudNo ratings yet
- RLE Evaluation FormDocument2 pagesRLE Evaluation Formtwothumbs100% (1)
- Vital Technical Sdn. BHD.: VT-210 High Performance SealantDocument4 pagesVital Technical Sdn. BHD.: VT-210 High Performance Sealantkhai ruleNo ratings yet
- Internship Report FormatDocument33 pagesInternship Report FormatSidra Ashraf92% (12)
- Feeding-Guide-for-Hospitalized-Dogs-and-Cats - PDF Version 1Document2 pagesFeeding-Guide-for-Hospitalized-Dogs-and-Cats - PDF Version 1Damian ChicaizaNo ratings yet
- High Frequency Oscillatory Ventilation (HFOV) تغريدDocument16 pagesHigh Frequency Oscillatory Ventilation (HFOV) تغريدtaghreednurseNo ratings yet
- PharmDos LAB - M2.2Document7 pagesPharmDos LAB - M2.2Gianna LingadNo ratings yet
- Guidelines For DNR Policies in Nursing FacilitiesDocument2 pagesGuidelines For DNR Policies in Nursing Facilitiesmichelle marquezNo ratings yet
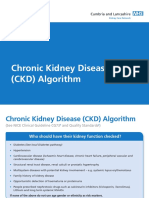
- Cumbria and Lancs KCN Algorithm PDFDocument18 pagesCumbria and Lancs KCN Algorithm PDFratih83No ratings yet
- Safety Data Sheet: K-37 Septic Tank Treatment 1. Product Identification K-37 Septic Tank TreatmentDocument7 pagesSafety Data Sheet: K-37 Septic Tank Treatment 1. Product Identification K-37 Septic Tank TreatmentRicardo AlvaradoNo ratings yet
- TOYOTA SR 09 - EngagingEmployees PDFDocument11 pagesTOYOTA SR 09 - EngagingEmployees PDFurooj salmanNo ratings yet
- Prevention of Postpartum Psychosis PDFDocument7 pagesPrevention of Postpartum Psychosis PDFAjengNo ratings yet
- PE NotesDocument20 pagesPE NotesAlma C WalshNo ratings yet
- Bpacnz Antibiotics GuideDocument40 pagesBpacnz Antibiotics GuideBulborea MihaelaNo ratings yet
- TechniquesDocument13 pagesTechniquesMirela Cojocaru StetcoNo ratings yet
- Performance Belgian Health SystemDocument117 pagesPerformance Belgian Health SystemM Faozi KurniawanNo ratings yet
- Panzi-Publication 181112 Spreads Small-2Document23 pagesPanzi-Publication 181112 Spreads Small-2johnpaul mosuelaNo ratings yet
- Ectopic PregnancyDocument4 pagesEctopic PregnancySyahriana AnaNo ratings yet
- Postoperative Phase 2021Document56 pagesPostoperative Phase 2021Jmarie Brillantes PopiocoNo ratings yet
- Scale For Ranking Family Health Problems Accdg To PrioritiesDocument3 pagesScale For Ranking Family Health Problems Accdg To PrioritiesIvan A. EleginoNo ratings yet
- Tesda Learning PortalsDocument4 pagesTesda Learning PortalsarishtenNo ratings yet