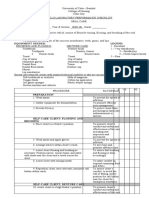
Bicol University
COLLEGE OF NURSING
Legazpi City
Name of Student : __________________________________ Date :_____________________
Name of CI: _________________________________ Level & Group : _____________
NCM 112 SKILLS LABORATORY
PERFORMANCE CHECKLIST FOR
INITIATING A BLOOD TRANSFUSION
PURPOSES:
Restore blood volume
Replace clotting factors
Improve oxygen carrying capacity
Restore blood elements that are depleted
Prevent complications
To raise the hemoglobin level
To provide antibodies
MATERIALS/EQUIPMENT NEEDED
250 ml Normal Saline Solution
Blood product
IV pole
Tape/Plaster
Alcohol pads
Blood administration set
Chlorhexidine Solution
Venipuncture set
Clean gloves
Procedure Mentioned Not Remarks
Mentioned
Perform hand hygiene and observe other appropriate infection
prevention procedures.
Prepare the infusion equipment. Ensure that the blood filter inside
the drip chamber is suitable for the blood components to be
transfused. Attach the blood tubing to the blood filter, if necessary.
Rationale: Blood filters have a surface area large enough to allow he
blood components through easily but are designed to trap clots.
Written consent for transfusion is required. Check policy and obtain
as indicated
Preparation
1. Prepare the client
Introduce yourself, verify client’s identity
Assist the client to a comfortable position, either sitting or lying.
Expose the IV site but provide for client privacy.
Explain the procedure and Purpose
Explain to the client what you are going to do, why it is necessary,
and how he or she can participate. Instruct the client to report
promptly any sudden chills, nausea, itching, rash, dyspnea, back
pain, or other unusual symptoms.
Check the needle & solution are appropriate
1. If the client has an IV solution infusing, check whether the IV
catheter and solution are appropriate to administer blood.
Page 1 of 5
� 2. The IV catheter size ranges between #18 and #20 gauge, and
the solution must be normal saline. Solutions other than
saline can cause damage to the blood components.
3. If the client does not have an IV solution infusing, check
agency policies. In some agencies an infusion must be
running before the blood is obtained from the blood bank. In
this case, you will need to perform a venipuncture on a
suitable vein and start an IV infusion of normal saline.
2. Obtain for the correct blood component
Check the doctor’s order with requisition
Check requisition form with blood bag label
check the client’s name, identification number, blood type (A, B, AB,
or O) and Rh group, the blood donor number, and the expiration
date of the blood. Observe the blood for abnormal color, RBC
clumping, gas bubbles, and extraneous material. Return outdated or
abnormal blood to the blood bank.
With another nurse (most agencies require an RN), verify the following
before initiating the transfusion
a. Order: Check the blood or component against the primary care
provider’s written order.
b. Transfusion consent form: Ensure the form is completed per facility
policy.
c. Client identification: The name and identification number on the
client’s identification band must be identical to the name and number
attached to the unit of blood.
d. Unit identification: The unit identification number on the blood
container, the transfusion form, and the tag attached to the unit must
agree.
e. Blood type: The ABO group and Rh type on the primary label of the
donor unit must agree with those recorded on the transfusion form.
f. Expiration: The expiration date and time of the donor unit should be
verified as acceptable.
g. Compatibility: The interpretation of compatibility testing must be
recorded on the transfusion form and on the tag attached to the unit.
h. Appearance: There should be no discoloration, foaming, bubbles,
cloudiness, clots or clumps, or loss of integrity of the container
• If any of the information does not match exactly, notify the charge nurse
and the blood bank. Do not administer blood until discrepancies are
corrected or clarified.
• Sign the appropriate form with the other nurse according to agency policy.
Sign the appropriate form with another nurse
Assure blood is at room temperature for not more than 30 minutes
before starting the transfusion. Agencies may designate different times
at which the blood must be returned to the blood bank if it has not been
started. Rationale: As blood components warm, the risk of bacterial
growth also increases.
If the start of the transfusion is unexpectedly delayed, return the blood
to the blood bank after 30 minutes. Do not store blood in the unit
refrigerator. Rationale: The temperature of unit refrigerators is not
precisely regulated and the blood may be damaged.
3. Set the infusion pump
Ensure that the blood filter inside the chamber is suitable for the
blood component to be transfused.
Attach the blood tubing to the blood filter, if necessary. Rationale:
Blood filters have a surface area large enough to allow the blood
components through easily but are designed to trap clots.
Put on gloves
Close all clamps on Y- set
Insert the piercing pin into a container of 0.9 saline solution
Page 2 of 5
� Hang the container on the IV pole (about 1 meter on the venipuncture
site)
4. Prime the tubing
Open the upper clamp on the normal saline tubing & squeeze the drip
chamber until it covers the filter & 1/3 of the drip chamber above the
filter
Tap the filter chamber to expel any residual air in the filter
Too much air may cause further complication
Remove the adapter cover at the tip of the blood administration set
Open the main flow rate clamp, and prime the tubing with saline
Close both clamp
5. Start the saline solution
If the iv solution is incompatible with the blood, stop & discard the
solution & tubing
Attach the blood tubing primed with normal saline to the IV catheter
Open the saline & main flow rate clamps, adjust the flow rate
Allow a small amount of solution to infuse to make sure there are no
problems with flow/site. Rationale: infusing normal saline before
initiating the transfusion also clears the IV catheter of incompatible
solutions and medications.
6. Prepare the blood bag
Invert the blood bag gently several times to mix the cells with the
plasma. Rationale: Rough handling can damage the cells.
Expose the port on the blood bag by pulling back the tabs
Insert the remaining Y-set into the blood bag
Suspend the blood bag
Close the upper clamp below the IV saline solution on the Y-set
Open the clamp on the blood arm of the Y-set & prime the tubing
7. Establish the blood transfusion
The blood will run into the saline filled drip chamber. Squeeze the
drip chamber to reestablish the liquid level with drip chamber 1/3 full
The blood will run into the saline-filled drip chamber. If necessary,
squeeze the drip chamber to reestablish the liquid level with the drip
chamber one third full.
Tap filter to remove residual air within the filter
Readjust the flow rate with the main clamp
Make sure that it is properly regulated
1 unit of blood must be consumed within not longer than 4hrs
Remove and discard gloves.
Perform hand hygiene.
8. Observe the client closely for the 1st 5-10 minutes
Run the blood slowly for the 1st 15 minutes at 20 gtts/min
Note adverse reactions such as chilling, nausea, vomiting, skin rash,
tachycardia. Rationale: The earlier a transfusion reaction occurs, the
more severe it tends to be. Identifying such reactions promptly helps
to minimize the consequences.
Remind the client to call a nurse immediately if any unusual
symptoms are felt such as chills, nausea, itching, rash, dyspnea, or
back pain if any of these occur,
Report to the charge nurse of any reactions and take appropriate
nursing action.
9. Document relevant data
Record starting the blood, vital signs, blood type, blood unit number,
sequence number , site of the venipuncture, size of the catheter, and
drip rate.
10. Monitor the client
15 minutes after initiating the transfusion, check the vital signs. In
absence of reaction, regulate the flow rate as ordered. Most adults
can tolerate receiving one unit of blood in 1.5 to 2 hours. Do not
transfuse a unit of blood for longer than 4 hours.
Assess the client including V/S every 30 minutes or more often, until
one-hour post transfusion.
If the client has reaction, discontinue the blood, send the blood bag
and tubing to the laboratory for investigation of the blood
Page 3 of 5
� 11. Terminate the transfusion
Put on clean gloves
Clamp the tubing and remove the needle, if no transfusion to follow.
If there is another transfusion, clamp the blood tubing and open the
saline infusion. BT set are changed within 24 hours or after 4-6 units
of blood per agency protocol
If no infusion is to follow, clamp the blood tubing. Check if the blood
component bag needs to be returned or if the blood bag and tubing
can be disposed of in a biohazard container. The IV line can be
discontinued or capped with an adapter or a new infusion line and
solution container may be added. If another transfusion is to follow,
clamp the blood tubing and open the saline infusion arm. Check
agency protocol. A new blood administration set is to be used with
each component
If the primary IV is to be continued, flush the maintenance line with
saline solution. Disconnect the blood tubing system and reestablish
the IV infusion using new tubing. Adjust the drip to the desired rate.
Often a normal saline or other solution is kept running in case of
delayed reaction to the blood.
Remove gloves
Monitor vital signs
12. Follow agency protocol for appropriate disposition of the used
supplies.
• Discard the administration set according to agency practice.
• Dispose of blood bags and administration sets.
a. On the requisition attached to the blood unit, fill in the time the
transfusion was completed and the amount transfused.
b. Attach one copy of the requisition to the client’s record and
another to the empty blood bag if required by agency policy.
c. Agency policy generally involves returning the bag to the blood
bank for reference in case of subsequent or delayed adverse
reaction.
• Remove and discard gloves.
• Perform hand hygiene.
13. Document relevant data.
• Record completion of the transfusion, the amount of blood
absorbed, the blood unit number, and the vital signs. If the primary
IV infusion was continued, record connecting it. Also record the
transfusion on the IV flow sheet and intake and output record.
Total Score= 110
1. Total Rating = Raw score /Total Score x 50 + 50= Total Grade
Reference: Kozier and Erb’s,8th Edition, Fundamentals of Nursing Practice Prepared by : Bibeth B. Monsalve,M.N.
_________________________________________ _______________________________________________
Signature of Student Signature of Clinical Instructor
Page 4 of 5
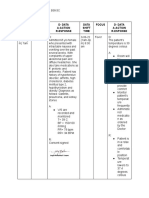
�1386 1393
Page 5 of 5