Professional Documents
Culture Documents
Penetrating Abdominal Injury Diagnosis
Uploaded by
Raquel Reyes0 ratings0% found this document useful (0 votes)
78 views3 pages You should proceed with exploratory laparotomy. While the patient is now normotensive, penetrating abdominal trauma with signs of peritonitis warrant exploration to identify and repair any injuries found. Waiting further risks delaying treatment and potential complications. Proceeding with laparotomy allows for direct visualization and control of any active bleeding or injuries present.
Original Description:
Original Title
Basic Emergency Skills in Trauma Part 3_ Penetrating Abdoninal Injury_ Dr. Oliver Belarma
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Document You should proceed with exploratory laparotomy. While the patient is now normotensive, penetrating abdominal trauma with signs of peritonitis warrant exploration to identify and repair any injuries found. Waiting further risks delaying treatment and potential complications. Proceeding with laparotomy allows for direct visualization and control of any active bleeding or injuries present.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
78 views3 pagesPenetrating Abdominal Injury Diagnosis
Uploaded by
Raquel Reyes You should proceed with exploratory laparotomy. While the patient is now normotensive, penetrating abdominal trauma with signs of peritonitis warrant exploration to identify and repair any injuries found. Waiting further risks delaying treatment and potential complications. Proceeding with laparotomy allows for direct visualization and control of any active bleeding or injuries present.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 3
SURGERY
Basic Emergency Skills in Trauma (Part 3)
Penetrating Abdominal Injury
Oliver I. Belarma, MD | June 5, 2021
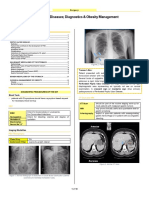
OUTLINE: ● X-Ray = pneumoperitoneum or foreign body
I. Objectives ● Blood in orifices (NGT, Foley catheter); Blood for NGT or
II. Penetrating Abdominal Injury IGT can be iatrogenic
III. Clinical Vignette
IV. Management of Colonic Injuries
If with indications in doing surgery: DECIDE
● Is the wound penetrating the peritoneum?
OBJECTIVES: ● Is there intraperitoneal injury?
● Interpret abdominal physical findings in penetrating
abdominal injury Q1: IF THE PATIENT CANNOT TELL IF THE TENDERNESS
● Understand and apply the different diagnostic modalities used IS COMING FROM THE WOUND OR INSIDE THE ABDOMEN,
in penetrating injury to the abdomen WHAT TO DO NEXT?
• Management will depend on the availability and skills of the
PENETRATING ABDOMINAL INJURY surgeons in the area.
● Penetrating Abdominal Injury
o penetrating injury entering the peritoneal space to a. Serial PE of the abdomen
retroperitoneum inflicting damage to the abdominal i. Doing the abdomen PE every 30mins for 2-3x
cnotents done by one examiner only.
● Entry wounds of abdominal injury extends in the 5th ii. Patient develops tenderness away from the entry
intercostal space up to the respective lobe causing wound or diffusely tender; do exploratory
penetrating abdominal injury laparotomy
● Most patients with penetrating abdominal injury require
laparotomy with difference in management between b. Perform wound exploration of the epigastric wound
projectile (gunshot) and non-projectile (stab). i. Single anterior abdominal wound
● Any wound in the area between the nipple line, (T4) and ii. PERFORM via the GUIDELINES, if wound
groin anteriorly and from T4 to the 3rd iliac crest the exploration is positive (penetration of fascia)
posteriorly = potential abdominal injury iii. If negative, admit for 24 hrs and do PE every 3 hrs
● If the wound is projectile, the penetrating injury could result iv. DISADVANTAGE: No practical use for multiple
to wounds present in any part of the body. abdominal wounds
● 4 important parts: v. For upper abdominal wounds, inadvertently enter
o Between the ant abdomen between the anterior the chest
axillary line bound by costal margin superiorly and vi. Low utility in stab wounds
the groin distally
o The thoracoabdominal area superiorly delimited by c. Diagnostic peritoneal lavage
the 4th intercostal space anteriorly, 6th intercostal i. For single and multiple anterior abdominal wounds
space laterally, 8th intercostal space posteriorly and ii. Do exploratory laparotomy if positive (with feces
inferiorly delimited by costalmargins. and bile on your DPL; if RBC > 100,000; WBC
o Back >500 on fluid; food particles)
o Flank iii. Negative: discharge the patient if no associated
injury
iv. Advantage: High false positive result, increase
CLINICAL VIGNETTE: non-therapeutic laparotomy
● 30/M came in 8 hours post-injury after sustaining multiple
abdominal stab wounds d. Perform laparoscopy
● BP: 100/70 mmHg; HR: 98/min; RR: 18/min i. Diagnostic laparoscopy
● Pink palpebral conjunctiva, clear breath sounds, distinct ii. Open laparotomy: if positive (with penetration of
heart sounds abdominal wall, presence of bowel or vascular
● PHYSICAL EXAMINATION: injuries, isolated diaphragmatic injury cannot be
o ABDOMEN: (+) multiple stab wounds, repaired laparoscopically)
▪ 1 Epigastric area iii. Negative: admit for 24 hours
▪ 2 Left lower quadrant iv. Disadvantages: surgical expertise exhausted,
▪ 3 Right lumbar area laborious preparation
▪ (+) direct tenderness on the epigastric
area e. UTZ
▪ (-) rebound (-) guarding i. Focused abdominal sonography on trauma
o RECTAL EXAM: (-) blood, (-) gross hematuria
ii. POSITIVE: free intraperitoneal fluid or presence of
any solid organ injury
Cite signs and symptoms to determine if it warrants iii. NEGATIVE: patient discharge in absence of other
immediate surgery injury
● Signs of hemodynamic stability associated with abdominal iv. DISADVANTAGE: operator-dependent; hollow
injury injuries can be missed; needs 50cc of
● Early Abdominal contents intraperitoneal fluid to be sonographically visible;
● Peritoneal signs conclusive of a hemoperitoneum (+) with 5mL of fluid
● Gunshot wound or Intraperitoneal penetration
● Lower extremity ischemia (vascular injury)
OMMC Surgery Rotators (Group 6 Post Graduate Interns) 1 of 3
SURGERY
Penetrating Abdominal Injury
v. CT Scan to assess the inferior and lateral posterior
abdominal wounds
vi. POSITIVE: (+) free intraabdominal and/or
peritoneal fluid or presence of any solid organ
injury, hollow viscous injury
vii. NEGATIVE: patient discharge
viii. DISADVANTAGE: edxpensive and needs 50 cc to
become positive
f. Do outright exploratory laparotomy
i. If A-E cannot be done, proceed to ex-lap
Colostomy
Q2: WHILE DOING ONE OF THE ABOVE PROCEDURES,
THE PATIENT BP WENT DOWN TO 80/60 MMHG, HOW WILL
YOU RESUSCITATE THE PATIENT?
• Hemorrhage: MOST COMMON CAUSE OF SHOCK IN
TRAUMA PATIENTS
• Patient’s Case: Class III (31-40% blood loss) before
hypotensive, hypovolemic
YOU WOULD RESUSCITATE BY:
a. Giving boluses of crystalloid (1L only)
b. Transfusing with fresh whole blood (< 24hrs)
c. Transfusing PRBC (if FWB no available within 24hrs)
d. Giving colloids while awating for blood
o Should be minimal in hypovolemic patients with
shock (up to 1L)
Q3: AFTER RESUSCITATION, BP ROSE TO 100/80 MMHG,
HR=115/MIN. ONE SHOULD:
a. Proceed with exploratory laparotomy (since patient is
normotensive already) Steps:
b. Continue resuscitation and wait for blood a. Exteriorization of the injured chronic segment.
c. Continue further observation b. Primary repair of the injured colon by creation of toximostoma
d. Proceed with further diagnostic work-up c. Do repair and divert
d. Do resection of colonic segment with end-colostomy or the
hartmann’s procedure
PENETRATING COLONIC INJURIES
PERITONITIS
Things to initially check:
• inflammation of the peritoneum or serosal surfaces as
1. Hypotension
evidenced by congestion and edema
2. Fecal contamination
• presence of fibrinous, purulent, or fibrino-purulent exudates,
3. Associated injuries and/or frank abscesses
4. Blood transfusion
5. Location of injury Guidelines
1. Primary repair for all non-destructive colon wounds
Colon – segment of bowel from the ileocecal valve up to the sacral
EXCEPT: PERITONITIS
promontory
2. Primary repair for DESTRUCTIVE EXCEPT: PERITONITIS,
>3 ORGANS ASSOCIATED INJURIES, SIGNIFICANT
MANAGEMENT OF COLONIC INJURY
UNDERLYING INJURIES
Primary Repair
1. Debridement with simple closure of perforation/s
2. Resection of a segment of large bowel containing the
perforation/s followed by resection and anastomosis
OMMC Surgery Rotators (Group 6 Post Graduate Interns) 2 of 3
SURGERY
Penetrating Abdominal Injury
• segmental resection and primary anastomosis: for
perforation > 50% of the bowel circumference, multiple
injuries in close proximity
MANAGEMENT OF INJURY TO THE PANCREAS
• SIMPLE REPAIR AND DRAINAGE: minor pancreatic
lacerations or contusions
• PYLORIC EXCLUSION OR DIVERTICULARIZATION:
repair of the duodenum, drainage and closure of the pylorus
with diversion of gastriccontents through a
gastrojejunolstomy
• PANCREATICODUODENAL RESECTION: indicated only
for severe injuries to the head of the pancreas and the
duodenum (rarely)
• DISTAL PANCREATECTOMY: for pancreatic injuries with
major ductal involvement
• DAMAGE CONTROL SURGERY AND POST-OPERATIVE
ERCP: for highly unstable patients
The following are done:
MANAGEMENT OF ARTERIAL INJURY • Triple shot open of the pancreas: makes the glands more
ZONES REGIONS MANAGEMENT firm
ZONE 1 Aortic hiatus to sacral All organs require
promontory divided into exploration
supra promontory and
infra promontory zones
REFERENCE:
ZONE 2 Renal hilum to pericolic Explore all penetrating
gutters (involve kidney) trauma but avoid Penetrating Abdominal Injuries
exploration of blunt Oliver I. Belarma, MD, FPCS
abdominal trauma June 5, 2021
ZONE 3 Pelvicoperitonium Explore all penetrating
Sacral promontory and trauma or all expanding
encompasses the pelvis hematoma in penetrating
trauma
Common injuries: Major arteries
MANAGEMENT OF SPLEEN INJURY
• 2nd MOST COMMONLY INJURED ORGAN FOLLOWING
BLUNT ABDOMINAL TRAUMA: SPLEEN
• Do Splenectomy: patients who are unstable and with higher
rates of injury (Grade 4 or 5)
• Splenic Digital pressure while spleen is being mobilized
• Mass tracting the hilum for hypertensive patients
MANAGEMENT OF HOLLOW VISCUS INJURY
• involves initial hemostasis and subsequent repair or
resection
• assume even number of wounds (with each entry wound
having an associated exit wound)
• Mesenteric border of the bowel, the retroperitoneal
duodenum and colon, the cardia, posterior wall, and the
greater and lesser curvatures of the stomach are areas that
might be missed.
Stomach
• primary repair for small perforations
• proximal or distal gastrectomy for extensive injuries
Small Intestines
• Primary Repair: for perforations <50% bowel circumference
OMMC Surgery Rotators (Group 6 Post Graduate Interns) 3 of 3
You might also like
- Gestroresectional SyndromesDocument18 pagesGestroresectional SyndromesAna CotomanNo ratings yet
- Schwannoma Vestibular ChristienDocument68 pagesSchwannoma Vestibular ChristienMaria Christien Agustie SitumorangNo ratings yet
- Fractures of Arm Forearm PDFDocument3 pagesFractures of Arm Forearm PDFjimNo ratings yet
- Abdominal Trauma Diagnosis and ManagementDocument9 pagesAbdominal Trauma Diagnosis and ManagementMyrtle Yvonne RagubNo ratings yet
- Physiologic Monitoring of The Surgical PatientDocument56 pagesPhysiologic Monitoring of The Surgical PatientSeid Adem100% (2)
- Fluid TherapyDocument10 pagesFluid Therapytaner_soysurenNo ratings yet
- Protocol Book For OBGYNDocument41 pagesProtocol Book For OBGYNShabir BadakhshNo ratings yet
- Surgical Oncology and Breast BiopsyDocument12 pagesSurgical Oncology and Breast Biopsybo gum parkNo ratings yet
- LEC 15.1 - Abdominal HerniasDocument37 pagesLEC 15.1 - Abdominal HerniasTudor CorneaNo ratings yet
- Surgery QuestionsDocument19 pagesSurgery QuestionsdocaliNo ratings yet
- Intussusception TransDocument4 pagesIntussusception TransJames Maravillas100% (1)
- Far Eastern University Medical Trauma PrinciplesDocument10 pagesFar Eastern University Medical Trauma PrinciplesMyrtle Yvonne RagubNo ratings yet
- Examination of Head and Neck SwellingsDocument22 pagesExamination of Head and Neck SwellingsObehi EromoseleNo ratings yet
- Fmge Dec 2019: QuestionsDocument16 pagesFmge Dec 2019: QuestionsSUBHADIPNo ratings yet
- Schwartz 9th Ed: Chapter Outline: The SpleenDocument22 pagesSchwartz 9th Ed: Chapter Outline: The SpleenKathryn Reunilla100% (1)
- A Disease Study On: AppendectomyDocument8 pagesA Disease Study On: Appendectomybryan leguiabNo ratings yet
- Schwartz Hour - BurnDocument62 pagesSchwartz Hour - BurnM3 SURGERY100% (1)
- 1 Inguinal Hernia EditedDocument34 pages1 Inguinal Hernia EditedNadhirah ZulkifliNo ratings yet
- Introduction To Trauma: LSU Medical Student Clerkship, New Orleans, LADocument31 pagesIntroduction To Trauma: LSU Medical Student Clerkship, New Orleans, LAnandangNo ratings yet
- Chapter 5 ATLSDocument27 pagesChapter 5 ATLSUlfaa MutiaaNo ratings yet
- 5B Surgery 1st-2nd SE #28-32 #17-18Document3 pages5B Surgery 1st-2nd SE #28-32 #17-18Liza SoberkaayoNo ratings yet
- Remove clothing, log roll, expose entire body, maintain spinal precautions and warmthDocument29 pagesRemove clothing, log roll, expose entire body, maintain spinal precautions and warmthAjay DherwaniNo ratings yet
- Operative Procedures: 1130 SRB's Manual of SurgeryDocument1 pageOperative Procedures: 1130 SRB's Manual of SurgerymadhuNo ratings yet
- Tiếng Anh dành cho giới Bác sĩ, Y tá PDFDocument248 pagesTiếng Anh dành cho giới Bác sĩ, Y tá PDFQuốc Việt100% (1)
- Drug StudyDocument13 pagesDrug StudyJaessa Feliciano50% (2)
- Breast Exam Guide for Lumps, Pain, DischargeDocument4 pagesBreast Exam Guide for Lumps, Pain, DischargekylieverNo ratings yet
- Intravenous Anesthetic Agents-1Document65 pagesIntravenous Anesthetic Agents-1Fauzan FajarNo ratings yet
- BLS Skills Checklist 2022 PDFDocument4 pagesBLS Skills Checklist 2022 PDFEvelyn EspinozaNo ratings yet
- Crit Care Nurse 2011 Grossbach 30 44Document18 pagesCrit Care Nurse 2011 Grossbach 30 44Hanik FiriaNo ratings yet
- 1.40 (Surgery) GIT Surgical Diseases - Diagnostics - Obesity ManagementDocument10 pages1.40 (Surgery) GIT Surgical Diseases - Diagnostics - Obesity ManagementLeo Mari Go LimNo ratings yet
- History Taking for Gallstones (CholelithiasisDocument6 pagesHistory Taking for Gallstones (CholelithiasisToria053No ratings yet
- INGUINAL-SCROTAL SWELLINGS GUIDEDocument23 pagesINGUINAL-SCROTAL SWELLINGS GUIDEAzmyza Azmy100% (1)
- MS SurgeryDocument118 pagesMS SurgeryLove wattaNo ratings yet
- Stages of Labor and Postpartum CareDocument7 pagesStages of Labor and Postpartum CareAkash SamuelNo ratings yet
- English-Italian Medical TermsDocument12 pagesEnglish-Italian Medical Termsionicaa3No ratings yet
- Aetiology, Pathology and Management of Enterocutaneous FistulaDocument34 pagesAetiology, Pathology and Management of Enterocutaneous Fistularoselinekhadija100% (1)
- Head & Neck: Most CommonDocument6 pagesHead & Neck: Most CommonJüdith Marie Reyes BauntoNo ratings yet
- Principles of Neonatal SurgeryDocument44 pagesPrinciples of Neonatal Surgerykbmed2003100% (2)
- Essentials for Practice of Medicine in the Frontline: From Tropical Africa; Pleasantly Different Volume 2From EverandEssentials for Practice of Medicine in the Frontline: From Tropical Africa; Pleasantly Different Volume 2No ratings yet
- Pediatric Surgery: Review Questions: Self-Assessment in General SurgeryDocument3 pagesPediatric Surgery: Review Questions: Self-Assessment in General Surgerymkct111No ratings yet
- Functions and anatomy of the small intestineDocument8 pagesFunctions and anatomy of the small intestineErald PaderangaNo ratings yet
- Surgery Sheet SchemeDocument51 pagesSurgery Sheet SchemeReem E.MNo ratings yet
- Total Abdominal HysterectomyDocument19 pagesTotal Abdominal HysterectomyMeidina Rachma Amanda100% (1)
- (DERMA) 03 TineasDocument9 pages(DERMA) 03 TineasJolaine ValloNo ratings yet
- Surgical Anatomy of The Chest Wall, Pleura, and MediastinumDocument8 pagesSurgical Anatomy of The Chest Wall, Pleura, and MediastinumNooneNo ratings yet
- Urogenital TumorDocument71 pagesUrogenital TumorJanet UngNo ratings yet
- Intra Abdominal 2009Document8 pagesIntra Abdominal 2009Shinta Dwi Septiani Putri WibowoNo ratings yet
- SurgeryDocument14 pagesSurgeryVinit ChoudharyNo ratings yet
- Physio Ob ReviewDocument368 pagesPhysio Ob ReviewMark LopezNo ratings yet
- Systemic Surgery NuggetsDocument17 pagesSystemic Surgery NuggetsAhmad UsmanNo ratings yet
- Management of Acute Appendicitis in Adults - UpToDateDocument28 pagesManagement of Acute Appendicitis in Adults - UpToDateaulia rachman100% (1)
- 3 Surgery - Mediastinum and PleuraDocument6 pages3 Surgery - Mediastinum and PleuraCassey Koi FarmNo ratings yet
- SurgeryDocument12 pagesSurgeryManusheeNo ratings yet
- PRETEST SURGERY - TRAUMA QUESTION 2 - Dr. Mariana UngurDocument1 pagePRETEST SURGERY - TRAUMA QUESTION 2 - Dr. Mariana UngurMariana UngurNo ratings yet
- In Service Exam For Breast DR Paul BalisiDocument11 pagesIn Service Exam For Breast DR Paul BalisiAmiel Francisco ReyesNo ratings yet
- Incisional Hernia RepairDocument6 pagesIncisional Hernia RepairLouis FortunatoNo ratings yet
- Clinical Pathology Case StudiesDocument10 pagesClinical Pathology Case StudiesKwadwo Sarpong JnrNo ratings yet
- OSPE 3rd Prof Microscopic Slide of Breast BiopsyDocument144 pagesOSPE 3rd Prof Microscopic Slide of Breast BiopsyMuhammadShahzadNo ratings yet
- Malunion Delayed Union and Nonunion FracturesDocument31 pagesMalunion Delayed Union and Nonunion FracturesRasjad ChairuddinNo ratings yet
- Workshop 1: Knots: Stage 1Document4 pagesWorkshop 1: Knots: Stage 1Noora jabeenNo ratings yet
- SURGERY: Schwartz's Textbook QuestionsDocument102 pagesSURGERY: Schwartz's Textbook Questionsvaegmundig100% (1)
- OSCE Must Knows For All SubjectsDocument8 pagesOSCE Must Knows For All SubjectsPrincess Jeanne Roque GairanodNo ratings yet
- Trans Congenital MalformationsDocument10 pagesTrans Congenital MalformationsRemelou Garchitorena AlfelorNo ratings yet
- Examination of Breast Lump PDFDocument2 pagesExamination of Breast Lump PDFDanaNo ratings yet
- Done By: Abdul Hakeem Hady. Gynecology SlidesDocument16 pagesDone By: Abdul Hakeem Hady. Gynecology Slidesعمر احمد شاكرNo ratings yet
- Chronic Suppurative Otitis MediaDocument6 pagesChronic Suppurative Otitis MediaSuhas IngaleNo ratings yet
- Carcinoma Penis Management GuideDocument63 pagesCarcinoma Penis Management GuideBibek GhimireNo ratings yet
- HyphemaDocument19 pagesHyphemaLiyanti RinceNo ratings yet
- 008 Plain X-Ray AbdomenDocument7 pages008 Plain X-Ray AbdomenAthul GurudasNo ratings yet
- Problem-based Approach to Gastroenterology and HepatologyFrom EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisNo ratings yet
- 3.04 Medical Ethics Trans - Human ActsDocument5 pages3.04 Medical Ethics Trans - Human ActsRaquel ReyesNo ratings yet
- Renal Anatomy and Physiology FunctionsDocument13 pagesRenal Anatomy and Physiology FunctionsRaquel ReyesNo ratings yet
- Oxygenation Hydration Posture VeggiesDocument1 pageOxygenation Hydration Posture VeggiesRaquel ReyesNo ratings yet
- ANATOMY AS Group 3b - Back and SpineDocument9 pagesANATOMY AS Group 3b - Back and SpineRaquel ReyesNo ratings yet
- 3.06 Medical Ethics Trans - ConscienceDocument5 pages3.06 Medical Ethics Trans - ConscienceRaquel ReyesNo ratings yet
- Biochem Part 2Document93 pagesBiochem Part 2Raquel ReyesNo ratings yet
- Bioethics Syllabus Explains Course ObjectivesDocument18 pagesBioethics Syllabus Explains Course ObjectivesRaquel ReyesNo ratings yet
- 3.02 Medical Ethics Trans - Introduction To BioethicsDocument4 pages3.02 Medical Ethics Trans - Introduction To BioethicsRaquel ReyesNo ratings yet
- Breezy BiochemDocument23 pagesBreezy BiochemRaquel ReyesNo ratings yet
- COMPRE REVIEW PART TWO KEY POINTSDocument26 pagesCOMPRE REVIEW PART TWO KEY POINTSRaquel ReyesNo ratings yet
- Biochem Part 3Document26 pagesBiochem Part 3Raquel ReyesNo ratings yet
- Biochem Part 2Document93 pagesBiochem Part 2Raquel ReyesNo ratings yet
- Breezy BiochemDocument23 pagesBreezy BiochemRaquel ReyesNo ratings yet
- FM CHEF CASE - January 2020 2BDocument3 pagesFM CHEF CASE - January 2020 2BRaquel ReyesNo ratings yet
- Med Paper Wards 4th ShiftingDocument9 pagesMed Paper Wards 4th ShiftingRaquel ReyesNo ratings yet
- KarunaGopal Channel6Document8 pagesKarunaGopal Channel6Ramesh GarikapatiNo ratings yet
- ABC MultimorbidityDocument4 pagesABC MultimorbidityJosef SosNo ratings yet
- Peptic Ulcer DiseaseDocument45 pagesPeptic Ulcer DiseaseKulgaurav RegmiNo ratings yet
- Materi DR. Dr. Ery Olivianto, Sp.A (K)Document39 pagesMateri DR. Dr. Ery Olivianto, Sp.A (K)utamiprakosoNo ratings yet
- Inform Concent Actemra 1Document2 pagesInform Concent Actemra 1lukiharjantiNo ratings yet
- Share SPM Problems With AnswerDocument54 pagesShare SPM Problems With AnswersanthoshNo ratings yet
- Susuk X RayDocument2 pagesSusuk X RayMasjid Bandar Bukit PuchongNo ratings yet
- Sai Kiran Hospital & Kiran Infertility Center PVT - LTD - DR Samit SekharDocument8 pagesSai Kiran Hospital & Kiran Infertility Center PVT - LTD - DR Samit SekharKiran IVFNo ratings yet
- Silingan Naka IUD, Namatay Man Gud", As Verbalized by TheDocument3 pagesSilingan Naka IUD, Namatay Man Gud", As Verbalized by TheMaxenia FaboresNo ratings yet
- PQT Updates Egypt AUG 2018Document41 pagesPQT Updates Egypt AUG 2018KaRiM NassarNo ratings yet
- UltramageDocument12 pagesUltramagegi vrgsNo ratings yet
- Dementia Drug StudyDocument2 pagesDementia Drug StudyBilljan TagapulotNo ratings yet
- English Eating Disorder Research PaperDocument7 pagesEnglish Eating Disorder Research PaperBrooke Van VeenNo ratings yet
- Diagnosis and Management of Vertebral Compression FracturesDocument7 pagesDiagnosis and Management of Vertebral Compression FracturesMayang CendikiaNo ratings yet
- Measuring Vital Signs SOPDocument3 pagesMeasuring Vital Signs SOPIffaNo ratings yet
- Heterogeneity Corrections - Treatment PlanningDocument10 pagesHeterogeneity Corrections - Treatment Planningapi-395602816100% (1)
- WBC MorphologyDocument47 pagesWBC MorphologyMuhammad ZakriaNo ratings yet
- Recover at Work Plan 5 ProposedDocument2 pagesRecover at Work Plan 5 ProposedSiosiana DenhamNo ratings yet
- DR - Rajalakshmi.C: Emergency Physician MMHRC Institute of Emergency MedicineDocument22 pagesDR - Rajalakshmi.C: Emergency Physician MMHRC Institute of Emergency MedicineP Vinod KumarNo ratings yet