Professional Documents
Culture Documents
Case Study Pressure Ulcer Student
Uploaded by
Kuro HanabusaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Case Study Pressure Ulcer Student
Uploaded by
Kuro HanabusaCopyright:
Available Formats
lOMoARcPSD|8858835
Case study pressure ulcer Student
Concepts of Medical Surgical Nursing (Galen College of Nursing)
StuDocu is not sponsored or endorsed by any college or university
Downloaded by KATHLEEN JOSOL (kathleen.josol@urios.edu.ph)
lOMoARcPSD|8858835
Name _________________________________ Class/Group _______________ Date
_______________
Scenario
You are a nurse working on the unit and take the following report from the emergency department
(ED) nurse: “We have a patient for you: R.L. is an 81-year-old frail woman who has been in a nursing
home. Her primary admitting diagnoses are sepsis, pneumonia, and dehydration, and she has a
known stage 3 right hip pressure injury. Past medical history includes remote cerebrovascular
accident with residual right-sided weakness and paresthesia, remote myocardial infarction, and
peripheral vascular disease. She is a full code. Her vital signs are 98/62, 88 and regular, 38 and
labored, 100.4° F (38° C). Lab work is pending; she has oxygen at 4 L per nasal cannula and an IV
of D5.45 at 100 mL/hr. We just inserted an indwelling catheter. The infectious disease doctor has
been notified, and respiratory therapy is with the patient—they are just leaving the ED and should
arrive shortly.”
1. What major factors increase risk for developing a pressure injury?
Mobility, Sensory, Moisture, Nutrition, Friction, and Shear
2. Each health care setting should have a policy that outlines how to assess patients’ risk for
developing a pressure injury. What should be included in that assessment?
Activity and mobility level
General condition of the skin
Presence of coexisting physical conditions, including diabetes, cardiovascular instability, low
BP, and oxygen use
Nutritional status, including hemoglobin, anemia, serum albumin levels, and weight
Fecal and urinary incontinence and general skin moisture
3. As part of R.L.’s admission assessment, you conduct a skin assessment. What areas of R.L.’s
body will you pay particular attention to?
Right side, bony prominences, sacrum, heels
4. What are the advantages of using a validated risk assessment tool to document her skin condition
on admission?
Braden Scale, Joint Commission’s patient safety goals
5. How often should patients be reassessed for the risk of developing an injury?
Every shift
Downloaded by KATHLEEN JOSOL (kathleen.josol@urios.edu.ph)
lOMoARcPSD|8858835
CASE STUDY PROGRESS
During your assessment, you note that R.L. has very dry, thin, almost transparent skin. She has
limited mobility from her stroke and is currently bedridden. There are several areas of ecchymosis on
her upper extremities. She is alert and oriented to person only. You review the transfer summary
from the long-term care facility and note she has a history of urinary and fecal incontinence.
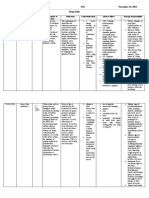
6. Evaluate R.L. with the Norton risk assessment scale.
Physical Mental Condition Activity Mobility Incontinence
Condition
Date Good 4 Alert 4 Ambulant 4 Full 4 Not 4 Total
Fair 3 Apathetic 3 Walk/help 3 Slightly Limited 3 Occasional 3 Score
Poor 2 Confused 2 Chair bound 2 Very limited 2 Usually/urine 2 7
Very 1 Stupor 1 Bed rest 1 Immobile 1 Urinary and 1
bad fecal
7. Knowing that R.L. is frail, has right-sided weakness, and has a pressure injury, what consultations
or referrals could you initiate?
PT/OT, wound care, speech therapy, infectious disease, Nutrition, Respiratory
CASE STUDY PROGRESS
As you are completing R.L.’s assessment, the wound nurse specialist comes in. She knows R.L.
from a prior admission; as soon as she received the request for a wound care consultation, she
ordered a specialty mattress. She says an air overlay should be delivered to your unit before your
shift ends.
8. Why is a specialty mattress used for immobile or compromised patients?
The help reduce pressure, provide comfort, and eliminate bottoming out
9. Why are patients placed on specialty mattresses still at risk for skin breakdown?
Because they will still need to be turned q2 hours, friction and shearing,
10. Why do the heels have the greatest incidence of breakdown, even when the patient is on a
specialty mattress?
Heels are covered by a thin layer of skin and fat, so they are a high risk for breakdown
11. What intervention can you initiate to protect R.L.’s heels?
Apply heel protectors, Monitor skin on feet and ankles daily, elevate her calves on pillow position
lengthwise to help relieve any pressure.
Downloaded by KATHLEEN JOSOL (kathleen.josol@urios.edu.ph)
lOMoARcPSD|8858835
12. Compare friction and shear.
Friction is the force of rubbing two surfaces against one another. Shear is a gravity force of pushing
down on the patient’s body with resistance between the patient and the chair and or bed.
13. What risk factor does using a draw sheet prevent or minimize?
Using a draw sheet to reposition or move the patient will help to distribute the pressure and help to
minimize sheering forces to the skin that can result in skin tears.
14. Describe 6 interventions aimed at minimizing friction and shear.
Establish a risk assessment per facility protocol, Pads and protect vulnerable arears, Use heel or
elbow protectors, utilize positioning devices in wheelchairs or chairs to reduce shearing
15. Elevated skin temperature and perspiration increase risk for pressure injury. Write 4 specific
measures to manage the microclimate.
Apply skin barrier creams in sensitive areas, Apply dressings to manage drainage from wounds,
Maintain a mild climate in the environment by avoiding excessive heat and humidity, Wear
breathable clothing and change undergarments regularly.
16. Which instructions will you give to the UAP helping you care for R.L.? Select all that apply.
a.Assess R.L.’s skin status every shift
b.Develop an every-2-hour turn schedule
c.Use the appropriate sheets on the airflow bed
d.Keep R.L.’s head of bed below a 30-degree angle
e.Assist with hygiene measures when R.L. is incontinent
f. Empty and measure output in the urine collection device
17. Write an outcome related to R.L.’s skin integrity.
CASE STUDY PROGRESS
The wound nurse needs to evaluate the preexisting pressure injury. She gently removes the old
dressing, using the push-pull method and adhesive remover wipes. After taking off the outside
Downloaded by KATHLEEN JOSOL (kathleen.josol@urios.edu.ph)
lOMoARcPSD|8858835
dressing, or the secondary dressing, she pulls out the primary dressing and states that R.L. has a
tunneled wound that was “packed too hard.”
18. What problems can be created by packing a wound too full?
If too much gauze is packed into the wound, it may create an environment that is too dry to allow the
wound to heal, prompting the wound to remain concave and possibly exacerbate. Too much packing
may also create more pressure within the healing wound, forcing it to extend further than its original
edges.
19. The nurse systematically assesses the injury and confirms the presence of a stage 3 wound with
moderate yellow drainage. There is no tissue necrosis or debris. What does it mean to “stage” a
wound?
Base Staging on the type of tissue visualized or palpated. Once you stage a wound it cannot be
reversed when documenting a healing pressure ulcer.
20. What would you expect a stage 3 pressure injury to look like?
Full thickness tissue loss, subcutaneous fat may be visible, but bone, tendon, or muscle are not
exposed. Some slough may be present.
21. What is a tunneling wound? What risk factors are associated with tunneling?
A tunneling wound is any wound that has a channel that tunnels from the wound into/through the
muscle or subcutaneous tissue.
Risk Factors: Smoking, putting too much weight on the wound, corticosteroids, chemotherapy or
immunosuppressant, Infection that has caused the destruction of tissue.
22. What are the dimensions of R.L.’s wound?
6 cm wide and 5 cm in length
Downloaded by KATHLEEN JOSOL (kathleen.josol@urios.edu.ph)
lOMoARcPSD|8858835
CASE STUDY PROGRESS
After the wound nurse obtains a set of wound cultures, you watch as she packs the wound with
gauze. The wound nurse charts the findings and makes formal recommendations for management of
the wound to the primary care provider.
23. When collecting a wound culture with a swab, the nurse should culture the
a.Wound drainage
b.Healthy-appearing tissue
c.Most necrotic-appearing tissue
d.Very outer edges of the wound
24. Describe the technique for packing a tunneled wound.
Packing should fill the wound space completely, but not tightly. Use a cotton swab to gently guide the
packing into small or tunneled ares. Open your outer dressing material and place it on the towel.
Keep it away from the bowl, and don’t get it wet.
Downloaded by KATHLEEN JOSOL (kathleen.josol@urios.edu.ph)
lOMoARcPSD|8858835
25. What factors influence the choice of a wound dressing?
Wound and skin related factors, such as cause, severity, environment, condition of the peri wound
skin, wound size and depth, anatomic location, volume of exudate, and the risk of infection.
26. What do you feel would be the best choice for dressing R.L.’s wound?
27. What wound documentation is necessary at this time?
Location, Size, Stage, Discharge, Odor
28. Complete an example of a documentation entry for R.L.’s wound care.
Wound Location Right Side
Pressure Injury Stage 3
Stage
Wound Dimensions 6 cms width and 5 cm length
Undermining 3.5 cm
Tissue Type 60% granulation 40% slough
Drainage Slightly yellow
Periwound
Condition
Cleansing Agents Normal salin
Dressing Type Hydrogel
Applied
CASE STUDY OUTCOME
Downloaded by KATHLEEN JOSOL (kathleen.josol@urios.edu.ph)
lOMoARcPSD|8858835
Despite aggressive treatment, R.L.’s sepsis and pneumonia are overwhelming, and she dies 9 days
later from multiple organ failure.
Downloaded by KATHLEEN JOSOL (kathleen.josol@urios.edu.ph)
You might also like
- Caring for a Cast: Monitoring for ComplicationsDocument39 pagesCaring for a Cast: Monitoring for ComplicationsGrape JuiceNo ratings yet
- Nursing Care Plan for Client with Major BurnDocument2 pagesNursing Care Plan for Client with Major BurnMaricel R. ManabatNo ratings yet
- Changing Fecal Pouching Colostomy)Document48 pagesChanging Fecal Pouching Colostomy)Champola Pola Camille BernardoNo ratings yet
- Bladder IrrigationDocument19 pagesBladder IrrigationDwight Kristian CruzNo ratings yet
- Fecal Elimination and Urinary EliminationDocument6 pagesFecal Elimination and Urinary Eliminationincent100% (1)
- Hirschsprung Disease Case Study: Maecy P. Tarinay BSN 4-1Document5 pagesHirschsprung Disease Case Study: Maecy P. Tarinay BSN 4-1Maecy OdegaardNo ratings yet
- Study On Pressure UlcerDocument219 pagesStudy On Pressure UlcerThein Ko Oo100% (1)
- MCN II AntepartumDocument28 pagesMCN II AntepartumJharaNo ratings yet
- Helping a client with leg traction and impaired mobilityDocument2 pagesHelping a client with leg traction and impaired mobilityNikki GalveNo ratings yet
- Urinary System Disorders Practice Quiz #1 (50 Questions)Document26 pagesUrinary System Disorders Practice Quiz #1 (50 Questions)Emy TandinganNo ratings yet
- SOAPIE and FDAR DocumentationDocument3 pagesSOAPIE and FDAR DocumentationDanna Kim AuxteroNo ratings yet
- Retained Placenta-OB Shock-Uterine InversionDocument38 pagesRetained Placenta-OB Shock-Uterine InversionBien Bosito0% (1)
- Care of Clients With Problem in Oxygenation Quiz 3Document5 pagesCare of Clients With Problem in Oxygenation Quiz 3marsan12No ratings yet
- Concept Map PEDocument3 pagesConcept Map PERobert MariasiNo ratings yet
- MS 3 Case Analysis DownloadableDocument1 pageMS 3 Case Analysis DownloadableCharissa Magistrado De LeonNo ratings yet
- Nursing Care of A Family With A Toddler Child: Christine M. Fiel, RN MN LPT MaedDocument25 pagesNursing Care of A Family With A Toddler Child: Christine M. Fiel, RN MN LPT MaedJrose CuerpoNo ratings yet
- A Case Study Presentation On Subarachnoid Hemorrhage: Presented byDocument78 pagesA Case Study Presentation On Subarachnoid Hemorrhage: Presented byNinaNo ratings yet
- Nursing Interventions CHFDocument3 pagesNursing Interventions CHFbanyenye25100% (1)
- Endocrine Disorder QuizDocument4 pagesEndocrine Disorder QuizBethrice MelegritoNo ratings yet
- Post-Partum Hemorrhage Pathophysiology PaperDocument5 pagesPost-Partum Hemorrhage Pathophysiology Paperapi-399619969No ratings yet
- Quiz 1Document5 pagesQuiz 1Francis Rafael PadillaNo ratings yet
- Transcultural Perspective in The Nursing Care of Adults Physiologic Development During AdulthoodDocument5 pagesTranscultural Perspective in The Nursing Care of Adults Physiologic Development During AdulthoodeuLa-mayzellNo ratings yet
- Hyperosmolar Hyperglycemic State (HHS)Document21 pagesHyperosmolar Hyperglycemic State (HHS)Malueth AnguiNo ratings yet
- Issues On Artificial ReproductionDocument46 pagesIssues On Artificial ReproductionOfficially RandomNo ratings yet
- Herniorrhaphy Procedure Repairs Hernia Through SuturesDocument2 pagesHerniorrhaphy Procedure Repairs Hernia Through SuturesSheldon Deypalubos Jr.No ratings yet
- Acute Appendicitis ExplainedDocument63 pagesAcute Appendicitis ExplainedIsis Elektra100% (1)
- GBS Management, Medications and Nursing ConsiderationsDocument4 pagesGBS Management, Medications and Nursing Considerationssouledg3100% (1)
- Principles of Casting and SplintingDocument8 pagesPrinciples of Casting and Splintingbobtaguba100% (1)
- Open Cholecystectomy Procedure OverviewDocument7 pagesOpen Cholecystectomy Procedure OverviewjosephcloudNo ratings yet
- Acute TonsillopharyngitisDocument39 pagesAcute TonsillopharyngitisCin AtianzarNo ratings yet
- INTUSSUSCEPTIONDocument3 pagesINTUSSUSCEPTIONS GNo ratings yet
- MS4 Midterm NCLEX BurnsDocument5 pagesMS4 Midterm NCLEX BurnsDebbie Dela Cruz100% (5)
- Orthopedic Splints and Traction TechniquesDocument26 pagesOrthopedic Splints and Traction TechniquesArun C RajNo ratings yet
- COAP-Medical-Surgical-Nursing-Gastrointestinal-System-30-Items-JIZ DE ORTEGADocument9 pagesCOAP-Medical-Surgical-Nursing-Gastrointestinal-System-30-Items-JIZ DE ORTEGANicole OrtegaNo ratings yet
- Patient ChartDocument2 pagesPatient ChartHydieNo ratings yet
- HerniaDocument11 pagesHerniaHapsari Wibawani 'winda'100% (1)
- Post-Debridement Nursing Care PlanDocument2 pagesPost-Debridement Nursing Care PlanAbdelmar SusulanNo ratings yet
- Different BandagingDocument2 pagesDifferent BandagingMarc LimNo ratings yet
- HyperpitutrismDocument41 pagesHyperpitutrismmuhammad kazimNo ratings yet
- Types of Traction and Casts Used in Fracture TreatmentDocument12 pagesTypes of Traction and Casts Used in Fracture TreatmentNoemi Nazareno MarceloNo ratings yet
- Nursing Management of Congestive Heart FailureDocument37 pagesNursing Management of Congestive Heart FailurePierre Aseron ManuelNo ratings yet
- ParkinsonDocument2 pagesParkinsongoyaNo ratings yet
- Mastectomy: Prepared By: Hilario, Eunice Lamoste, Jenebelle Lopez, Maria SofiaDocument34 pagesMastectomy: Prepared By: Hilario, Eunice Lamoste, Jenebelle Lopez, Maria SofiaSofia LopezNo ratings yet
- German MeaslesDocument8 pagesGerman MeaslesYdynn Parejas GavinaNo ratings yet
- Service Quality of Hospital Outpatient Departments: Patients' PerspectiveDocument2 pagesService Quality of Hospital Outpatient Departments: Patients' Perspectivelouie john abilaNo ratings yet
- Case 052: Biliary ColicDocument4 pagesCase 052: Biliary ColicZauzaNo ratings yet
- 51 100Document18 pages51 100Jaessa Feliciano100% (1)
- 9 Tips On How To Make A Good SOAPIEDocument7 pages9 Tips On How To Make A Good SOAPIEMagbanua Airene MarielNo ratings yet
- Acute Respiratory Distress Syndrome (ARDS): Causes, Symptoms and TreatmentDocument30 pagesAcute Respiratory Distress Syndrome (ARDS): Causes, Symptoms and TreatmentOya Zuraini KamalNo ratings yet
- F&E ExamDocument3 pagesF&E ExamDino PringNo ratings yet
- DOH ProgramsDocument6 pagesDOH ProgramsMichael VillavertNo ratings yet
- A Case Presentation On CholedocholithiasisDocument11 pagesA Case Presentation On CholedocholithiasisPaul Vincent EspereNo ratings yet
- Clinical Case StudyDocument5 pagesClinical Case Studyv2wish_iNo ratings yet
- Infertility Nursing Diagnosis and Pregnancy SymptomsDocument7 pagesInfertility Nursing Diagnosis and Pregnancy SymptomsPaolo AtienzaNo ratings yet
- Clubfoot Definition, Types, and TreatmentDocument5 pagesClubfoot Definition, Types, and TreatmentcrisolandNo ratings yet
- Fracture (Cast Care)Document6 pagesFracture (Cast Care)Vane UcatNo ratings yet
- The Nature of Nursing 2Document12 pagesThe Nature of Nursing 2twy113No ratings yet
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- Pedia Drug StudyDocument6 pagesPedia Drug StudyKuro HanabusaNo ratings yet
- Pedia Drug StudyDocument6 pagesPedia Drug StudyKuro HanabusaNo ratings yet
- CombinepdfDocument280 pagesCombinepdfKuro HanabusaNo ratings yet
- Final NCP PediaDocument2 pagesFinal NCP PediaKuro HanabusaNo ratings yet
- Placenta PreviaDocument5 pagesPlacenta PreviaKuro HanabusaNo ratings yet
- Anna Trisha B. Crosrojas N42 November 24, 2021 Drug Study: 3G IvttDocument3 pagesAnna Trisha B. Crosrojas N42 November 24, 2021 Drug Study: 3G IvttKuro HanabusaNo ratings yet
- "Nag Dugo Akong Gums Kaduha" AsDocument3 pages"Nag Dugo Akong Gums Kaduha" AsKuro HanabusaNo ratings yet
- Filipino Value SystemDocument33 pagesFilipino Value SystemTenisha Foster95% (231)
- In Our Families and Faith CommunitiesDocument1 pageIn Our Families and Faith CommunitiesroshelleNo ratings yet
- What is Atropine and its UsesDocument3 pagesWhat is Atropine and its UsesKuro HanabusaNo ratings yet
- Cues Nursing Diagnosis Planning Interventions Rationale Evaluation SubjectiveDocument2 pagesCues Nursing Diagnosis Planning Interventions Rationale Evaluation SubjectiveKuro HanabusaNo ratings yet
- Final NCP PediaDocument2 pagesFinal NCP PediaKuro HanabusaNo ratings yet
- Naproxen Drug Study GuideDocument3 pagesNaproxen Drug Study GuideKuro HanabusaNo ratings yet
- Pedia Drug StudyDocument6 pagesPedia Drug StudyKuro HanabusaNo ratings yet
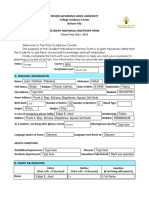
- Father Saturnino Urios University: (Name of Student)Document1 pageFather Saturnino Urios University: (Name of Student)Kuro HanabusaNo ratings yet
- Father Saturnino Urios University: (Name of Student)Document1 pageFather Saturnino Urios University: (Name of Student)Kuro HanabusaNo ratings yet
- Humoral Immunity Cell-Mediated ImmunityDocument2 pagesHumoral Immunity Cell-Mediated ImmunityKuro HanabusaNo ratings yet
- Submissions PANITIKANG FILIPINO N41 Pamprelim Na Pagsusulit Father Saturnino Urios UniversityDocument6 pagesSubmissions PANITIKANG FILIPINO N41 Pamprelim Na Pagsusulit Father Saturnino Urios UniversityKuro HanabusaNo ratings yet
- Humoral Immunity Cell-Mediated ImmunityDocument2 pagesHumoral Immunity Cell-Mediated ImmunityKuro HanabusaNo ratings yet
- Comprehensive Guide to Substance Abuse Diagnosis and TreatmentDocument3 pagesComprehensive Guide to Substance Abuse Diagnosis and TreatmentKuro HanabusaNo ratings yet
- Comprehensive Guide to Substance Abuse Diagnosis and TreatmentDocument3 pagesComprehensive Guide to Substance Abuse Diagnosis and TreatmentKuro HanabusaNo ratings yet
- What is Atropine and its UsesDocument3 pagesWhat is Atropine and its UsesKuro HanabusaNo ratings yet
- Father Saturnino Urios University College Guidance Center Butuan City Student Individual Inventory FormDocument4 pagesFather Saturnino Urios University College Guidance Center Butuan City Student Individual Inventory FormKuro HanabusaNo ratings yet
- This Study Resource WasDocument2 pagesThis Study Resource WasKuro HanabusaNo ratings yet
- NCP FormDocument2 pagesNCP FormKuro HanabusaNo ratings yet
- Resumption of Sustained PerfusingDocument14 pagesResumption of Sustained PerfusingKuro HanabusaNo ratings yet
- Re-Designing A Rapid Response System: Effect On Staff Experiences and Perceptions of Rapid Response Team CallsDocument9 pagesRe-Designing A Rapid Response System: Effect On Staff Experiences and Perceptions of Rapid Response Team CallsKuro HanabusaNo ratings yet
- Quiz 1Document3 pagesQuiz 1Kuro HanabusaNo ratings yet
- Image of A LeaderDocument1 pageImage of A LeaderKuro HanabusaNo ratings yet
- Image of A LeaderDocument1 pageImage of A LeaderKuro HanabusaNo ratings yet
- LP 21 Health Q3Document6 pagesLP 21 Health Q3Hazel Rubas SamsonNo ratings yet
- Drug Study, NCP, and Discharge Plan For AppendectomyDocument12 pagesDrug Study, NCP, and Discharge Plan For AppendectomyApril80% (5)
- Sinus and FistulaDocument3 pagesSinus and FistulaAndrew BonusNo ratings yet
- Pressure Sore or Decubitus Ulcer or Bed SoreDocument20 pagesPressure Sore or Decubitus Ulcer or Bed SorePrecious BlessingNo ratings yet
- Basic First AidDocument7 pagesBasic First AidCarlo LaguadorNo ratings yet
- Wfa ProductDocument14 pagesWfa ProductjhoniNo ratings yet
- Hospital Training ReportDocument30 pagesHospital Training ReportNitin Chaudhary82% (22)
- First AidDocument7 pagesFirst AidjuliaNo ratings yet
- Post-Op Instructions For Knee Debridement & MeniscectomyDocument2 pagesPost-Op Instructions For Knee Debridement & MeniscectomyMuhammad YusufNo ratings yet
- Primary Care Woundcare Formulary Final Version January 2020Document21 pagesPrimary Care Woundcare Formulary Final Version January 2020Dr Purva PaiNo ratings yet
- Infected WoundDocument23 pagesInfected WoundMohamed FarahatNo ratings yet
- Application of Bandages and Binders - StudentsDocument110 pagesApplication of Bandages and Binders - Studentsjeremiah90% (10)
- First Aid Dressings and Bandages LessonDocument7 pagesFirst Aid Dressings and Bandages LessonAliah Mae MontanoNo ratings yet
- Zhang2020 Article EvaluationOfBepanGelHydrogelEfDocument14 pagesZhang2020 Article EvaluationOfBepanGelHydrogelEfİncelus ChinusNo ratings yet
- Fundamentals of Nursing Test IIIDocument19 pagesFundamentals of Nursing Test IIIja97% (29)
- Burns Care GuideDocument106 pagesBurns Care GuideShahini PrajapatiNo ratings yet
- DURBIN MEDICAL SUPPLY CATALOGUE Consumables and General SuppliesDocument22 pagesDURBIN MEDICAL SUPPLY CATALOGUE Consumables and General SuppliesAlexander Kwaitota100% (1)
- Deceased Patient Protocol Interim GuidanceDocument15 pagesDeceased Patient Protocol Interim GuidanceAnonymous 4PZvNVWoehNo ratings yet
- HEALTH Mod. 12 Q3 LASDocument4 pagesHEALTH Mod. 12 Q3 LASHsiri IrishNo ratings yet
- S M D U: KIN Anagement Ecubitis LcerDocument77 pagesS M D U: KIN Anagement Ecubitis LcerabidNo ratings yet
- Tracheostomy Care and SuctionDocument2 pagesTracheostomy Care and SuctionMsPocketbook HoarderNo ratings yet
- Catalog NP 2018-2019Document124 pagesCatalog NP 2018-2019Angela MazónNo ratings yet
- Proper Bandaging TechniquesDocument13 pagesProper Bandaging TechniquesAnkita Bramhe100% (1)
- Minor Surgery Procedures ExplainedDocument19 pagesMinor Surgery Procedures ExplainedAudrey Austria IINo ratings yet
- Wilderness and Remote First Aid - Pocket GuideDocument16 pagesWilderness and Remote First Aid - Pocket Guide2mvp100% (1)
- Overgranulation: A. Muhammad Reva A.MDocument21 pagesOvergranulation: A. Muhammad Reva A.Mgalih widodoNo ratings yet
- Sterile ProductsDocument88 pagesSterile ProductsBadri KarkiNo ratings yet
- FIRST AID-Module OneDocument111 pagesFIRST AID-Module One@tcher96% (24)
- Burn Dressing GuidelinesDocument7 pagesBurn Dressing GuidelinesOnlyjust FormeNo ratings yet
- Home Economics For Secondary Schools Book 2Document162 pagesHome Economics For Secondary Schools Book 2EleciaNo ratings yet