Professional Documents
Culture Documents
Role of Laparoscopic Common Bile Duct Exploration in The Management of Choledocholithiasis
Role of Laparoscopic Common Bile Duct Exploration in The Management of Choledocholithiasis
Uploaded by
clara baezOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Role of Laparoscopic Common Bile Duct Exploration in The Management of Choledocholithiasis
Role of Laparoscopic Common Bile Duct Exploration in The Management of Choledocholithiasis
Uploaded by
clara baezCopyright:
Available Formats
Submit a Manuscript: http://www.wjgnet.
com/esps/ World J Gastrointest Surg 2016 May 27; 8(5): 376-381
Help Desk: http://www.wjgnet.com/esps/helpdesk.aspx ISSN 1948-9366 (online)
DOI: 10.4240/wjgs.v8.i5.376 © 2016 Baishideng Publishing Group Inc. All rights reserved.
MINIREVIEWS
Role of laparoscopic common bile duct exploration in the
management of choledocholithiasis
Nikhil Gupta
Nikhil Gupta, Department of Surgery, PGIMER Dr RML optimal treatment till date. With refinements in techni
Hospital, Delhi 110001, India que and expertise in field of minimal access surgery,
many centres in the world have started offering one
Author contributions: Gupta N solely contributed to this paper. stage management of choledocholithiasis by LC with
laparoscopic common bile duct exploration (LCBDE).
Conflict-of-interest statement: No potential conflicts of
interest. No financial support. Various modalities have been tried for entering into
concurrent common bile duct (CBD) [transcystic (TC) vs
Open-Access: This article is an open-access article which was transcholedochal (TD)], for confirming stone clearance
selected by an in-house editor and fully peer-reviewed by external (intraoperative cholangiogram vs choledochoscopy),
reviewers. It is distributed in accordance with the Creative and for closure of choledochotomy (T-tube vs biliary
Commons Attribution Non Commercial (CC BY-NC 4.0) license, stent vs primary closure) during LCBDE. Both TC
which permits others to distribute, remix, adapt, build upon this and TD approaches are safe and effective. TD stone
work non-commercially, and license their derivative works on extraction is involved with an increased risk of bile leaks
different terms, provided the original work is properly cited and
and requires more expertise in intra-corporeal suturing
the use is non-commercial. See: http://creativecommons.org/
licenses/by-nc/4.0/ and choledochoscopy. Choice depends on number of
stones, size of stone, diameter of cystic duct and CBD.
Correspondence to: Dr. Nikhil Gupta, MS, MRCSEd, FAIS, This review article was undertaken to evaluate the role
FMAS, FIAGES, MNAMS, Assistant Professor, Department of LCBDE for the management of choledocholithiasis.
of Surgery, PGIMER Dr RML Hospital, B-406 Panchsheel
Apartments, Plot-9, Sector-10, Dwarka, Delhi 110001, Key words: Laparoscopic common bile duct exploration;
India. nikhil_ms26@yahoo.co.in Choledochoscopy; Cholangiogram; Choledocholithiasis;
Telephone: +91-011-45526090 Primary closure
Fax: +91-011-45526090
© The Author(s) 2016. Published by Baishideng Publishing
Received: July 29, 2015
Group Inc. All rights reserved.
Peer-review started: September 1, 2015
First decision: December 7, 2015
Revised: February 5, 2016 Core tip: Various treatment modalities are available
Accepted: February 23, 2016 for management of choledocholithiasis. Laparoscopic
Article in press: February 24, 2016 common bile duct exploration offers one stage mana
Published online: May 27, 2016 gement of cholelithiasis with choledocholithiasis. This
review article was undertaken to evaluate this techni
que and its various aspects.
Abstract
Gupta N. Role of laparoscopic common bile duct exploration
Surgical fraternity has not yet arrived at any consensus
in the management of choledocholithiasis. World J Gastrointest
for adequate treatment of choledocholithiasis. Sequential
Surg 2016; 8(5): 376-381 Available from: URL: http://www.
treatment in the form of pre-operative endoscopic
wjgnet.com/1948-9366/full/v8/i5/376.htm DOI: http://dx.doi.
retrograde cholangio-pancreatography followed by
org/10.4240/wjgs.v8.i5.376
laparoscopic cholecystectomy (LC) is considered as
WJGS|www.wjgnet.com 376 May 27, 2016|Volume 8|Issue 5|
Gupta N. Role of laparoscopic CBD exploration
stone clearance rate, hospital stay, and complications.
INTRODUCTION [7]
Liu et al did a meta-analysis and found that there
The incidence of gallstones varies from 6%-10% in was no significant difference between laparoscopic
[1]
adult population . Three percent to 14.7% of patients CBD exploration group and pre-operative endoscopic
of gallstones have concurrent common bile duct (CBD) sphincterotomy group in terms of complications or
[2]
stones as well . “Gold Standard” for management of retained stones (P > 0.05). Success rate was higher in
gallstones is laparoscopic cholecystectomy (LC) but LCBDE group with reduced hospital expenses, mean
there is no consensus for treatment of CBD stones. In operative time and duration of hospitalization (P <
the era of open surgery, treatment was straight-forward; 0.05) .
[7]
open cholecystectomy with open CBD exploration Another meta-analysis done by Nagaraja et al ,
[8]
though it carried high morbidity and mortality. With the reported higher incidence of ERCP related complications
advent of non invasive and minimal invasive techniques, in patients undergoing pre-operative ERCP [odds ratio
option of pre-operative endoscopic retrograde cholangio- (OR) = 2.40, 95%CI: 1.21-4.75].
pancreatography (ERCP) followed by LC emerged as [9]
Costi et al performed a case-control study
adequate treatment. Major disadvantages of ERCP are comparing a single stage laparoscopic approach (n =
that it is a two stage procedure and is associated with 22) with sequential treatment (n = 15). They found
life threatening complications like pancreatitis, bleeding two groups to be similar in terms of early and late
and duodenal perforation. It has also been reported complications. The postoperative hospitalization was
that sphincterotomy may cause papillary stenosis and [9]
significantly less in the single stage group . Bansal
[2,3]
increased risk of bile duct cancer . et al
[10]
conducted a prospective randomized trial
With refinements in technique and expertise in comparing single stage laparoscopic treatment with
field of minimal access surgery, many centres in the sequential treatment of CBD stones. Fifteen patients
world have started offering one stage management were randomized to each group. Stone clearance rates
of choledocholithiasis by LC with laparoscopic CBD and complications were similar in both groups. They
exploration (LCBDE). Only few randomized trials are concluded that single stage approach seems to be
available comparing pre-operative ERCP followed by LC better due to smaller number of procedures and hospital
[4,5]
with single stage LC and LCBDE . There is no consensus [10]
visits .
even for the technique of LCBDE. Various modalities Cochrane systematic review was done by Dasari
have been tried for entering into CBD [transcystic et al
[11]
in 2013. They included five trials (n = 580).
(TC) vs transcholedochal (TD)], for confirming stone Two hundred and eighty-five patients underwent LC +
clearance [intraoperative cholangiogram (IOC) vs LCBDE and 295 patients received sequential treatment
choledochoscopy], and for closure of choledochotomy in the form of ERCP + LC. There was no significant
(T-tube vs biliary stent vs primary closure). difference among two groups in terms of mortality
(0.7% vs 1%), morbidity (15% vs 135%) or incidence
of retained stones (8% vs 11%).
REVIEW OF LITERATURE A meta-analysis of single-stage vs sequential treat
Literature search was performed to answer these ment for cholelithiasis with common bile duct stones was
questions. Online search engines like PubMed, Google, carried out by Zhu et al
[12]
recently. Eight randomized
springer link library and Cochrane database systematic controlled trials, which involved 1130 patients, were
review were utilized and review articles, prospective included in this study. The meta-analysis revealed that
and retrospective studies which detailed or compared the CBD stone clearance rate in the single-stage group
the various treatment strategies for CBD stones were was higher (OR = 1.56, 95%CI: 1.05-2.33, P = 0.03).
selected and analyzed. The lengths of hospitalization (MD = -1.02, 95%CI:
-1.99 to -0.04, P = 0.04) and total operative times (MD
Sequential vs one stage management = -16.78, 95%CI: -27.55 to -6.01, P = 0.002) were
Two randomized trials have compared pre-operative also shorter in the single-stage group. There was no
ERCP followed by LC with one stage LC and LCBDE .
[4,5]
statistically significant difference among the two groups
Results of the two modalities were comparable in terms regarding postoperative morbidity (OR = 1.12, 95%CI:
of stone clearance and complications but duration of hos 0.79-1.59, P = 0.52), mortality (OR = 0.29, 95%CI:
pitalization was shorter with LCBDE in both studies .
[4,5]
0.06-1.41, P = 0.13) and conversion to other procedures
[5]
In a study done by Rogers et al , 122 patients were (OR = 0.82, 95%CI: 0.37-1.82, P = 0.62).
randomized into either group. Hospital stay was signifi
cantly shorter for LC + LCBDE [mean (SD), 55 (45) TC vs TD
[13]
h vs 98 (83) h; P < 0.001]. There was no difference Hongjun et al compared TC approach (n = 80) with
in patient acceptance and quality of life scores among TD approach (n = 209) and found that there was no
the two groups. A prospective analysis done (n = 150) significant difference between the two approaches for
[6]
by Mohamed et al showed that the laparoscopic cystic duct diameter (0.47 ± 0.09 cm vs 0.47 ± 0.08
management of CBD stones is as safe and effective as cm), procedure time (91.94 ± 34.21 min vs 96.13
the sequential ERCP followed by LC with nearly the same ± 32.15 min), complications (2.5% vs 2.87%) and
WJGS|www.wjgnet.com 377 May 27, 2016|Volume 8|Issue 5|
Gupta N. Role of laparoscopic CBD exploration
[25]
duration of hospitalization (9.82 ± 3.48 d vs 10.74 Dong et al compared primary closure (group A,
± 5.34 d) (all P > 0.05). A significant difference was n = 101) with T-tube drainage (group B, n = 93) after
noticed in terms of the common bile duct diameter (1.18 LCBDE. The mean operative time was less in group A
[13]
± 0.29 cm vs 1.04 ± 0.24 cm, P < 0.05) . than in group B (102.6 ± 15.2 min vs 128.6 ± 20.4
[14]
Wang et al reported that TC LCBDE is safe min, P < 0.05). Postoperative hospitalization was longer
and effective in elderly population. TC approach was in group B (4.9 ± 3.2 d) than in group A (3.2 ± 2.1
successful in 157 of 165 patients (95.15%). Five d). The hospital expenses were also significantly less
patients were converted to laparoscopic TD approach in group A. Three patients experienced complications
and T-tube drainage whereas three patients were in postoperative period, which were related to T-tube
[25]
managed by laparotomy and open CBD exploration. usage in group B .
[26]
No significant complications were reported in the In other study, Leida et al showed that patients
study. The mean blood loss was 43 ± 20 mL and mean with primary closure of the CBD returned to work
operative time was 102 ± 35 min. The postoperative faster (12.6 ± 5.1 d vs 20.4 ± 13.2 d). This group
[14]
hospitalization was 3 ± 0.5 d . also showed advantages of significantly lower hospital
[15]
A systematic review done by Reinders et al expenses and less postoperative complications than
[26]
included eight randomized trials with 965 patients. T-tube drainage group (15% vs 27.5%) .
[27]
Successful bile duct clearance varied between 80.4% Lyon et al compared use of biliary stent (n =
and 100% in the TC groups and 58.3% and 100% in 82) with T-tube drainage (n = 34) after LCBDE in a
the TD groups. There were more bile leaks after TD prospective non-randomized study. The duration of
stone extraction (11%) than after TC stone extraction hospitalization for patients who underwent biliary
(1.7%). They concluded that TD stone extraction is stent or T-tube insertion after LBCDE were 1 and 3.4
associated with an increased risk of bile leaks and should d, respectively (P < 0.001). In the T-tube group, two
only be done by highly experienced surgeons; TC stone patients required laparoscopic washout due to bile leaks.
extraction seems a more accessible technique with lower They concluded that ante-grade biliary stent insertion
[4,5,10,16-20]
complication rates . is associated with low hospital expenses and increased
[21]
Chander et al have concluded that TD route is patient satisfaction .
[27]
better in asian patients with multiple, large stones and Dietrich et al
[28]
compared biliary stent with T-tube
dilated CBD. drainage in a series of 48 patients who underwent
LCBDE. Patients with T-tube drainage had more pro
IOC vs choledochoscopy cedure-related complications (P < 0.0001) and a pro
Only two studies were found comparing IOC with longed hospital stay (P = 0.03).
[29]
choledochoscopy for confirming stone clearance. Topal A retrograde study done by Abellán Morcillo et al ,
[22]
et al found similar results with both techniques, compared T-tube closure (n = 36), biliary stent (n =
though operative time was longer in IOC group. Vindal 133) and primary closure (n = 16). In the stented
[23]
et al in a prospective randomized study compared group, they found an 11.6% incidence of pancreatitis
IOC (n = 65) with intra-operative choledochoscopy and a 26.1% incidence of hyperamylasemia whereas
(n = 67). Mean operative time was 170 min in group in the primary closure group, a clear improvement of
[29]
A and 140 min in group B (P < 0.001). There was no complications and hospital stay was observed .
[30]
significant difference in complications among the two Chen et al in their study observed that primary
[23]
groups . They found choledochoscopy to be better closure is safe after LCBDE (n = 194).
[31]
and less time consuming than IOC for determining bile Estellés Vidagany et al did primary closure after
duct clearance after TD LCBDE. LCBDE in 160 patients. Bile leakage was reported in 11
patients (6.8%). In 7 out of 11 patients (63.6%), no
Primary closure vs T-tube vs biliary stent further intervention was needed and the leak closed
[24]
In a retrospective study done by Yi et al , long term on its own. Six patients were reoperated (3.75%), two
results of primary closure (group P, n = 91) after LCBDE for biliary peritonitis and four for haemoperitoneum.
were compared with T-tube drainage (group T, n = 51). The success rate for stone clearance was 96.2%. No
The mean operative time was significantly less in group mortality or CBD stricture was reported in the study.
P than group T (168.9 ± 50.1 min vs 198.0 ± 59.6 They concluded that primary closure after LCBDE is a
[31]
min, P = 0.002). The duration of hospitalization was safe technique with excellent results .
[32]
significantly less in group P than in group T (8.59 ± 6.0 Hua et al studied rate of bile leak following primary
d for group P vs 14.96 ± 5.4 d for group T, P = 0.001). closure in LCBDE via TD approach. Of 157 LCBDE
The stone recurrence rates in group P and group T were procedures, 138 (87.9%) were successfully managed
4.4% and 5.9%, respectively (P = 0.722) (mean follow- with primary closure of the choledochotomy. Eight
up 48.8 mo). There was no sign of biliary stricture or patients (5.1%) underwent closure over a T-tube after
other biliary complications in follow-up in either group. LCBDE and 11 patients (7.0%) were converted to open
They concluded that primary closure after LCBDE with surgery. The success rate for CBD stone clearance was
choledochoscopy is as safe and effective as T-tube 98.1%. Postoperative bile leak was seen in 6 patients
[24]
drainage in terms of long-term results . (3.8%).
WJGS|www.wjgnet.com 378 May 27, 2016|Volume 8|Issue 5|
Gupta N. Role of laparoscopic CBD exploration
Despite the simplicity and success of LCBDE, many
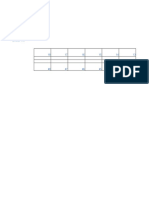
Table 1 Effective and important factors in common bile duct
stones approach surgeons across the globe are still not comfortable or
[37]
confident regarding the procedure. Petelin et al did
Factor Trans-cystic Trans-ductal a web based survey among United States surgeons
approach approach regarding their choice for managing choledocholithiasis.
Single stone Yes Yes For preoperatively known CBD calculi, 86% preferred
Multiple stones Yes Yes
preoperative ERCP. Those in metropolitan areas were
Stones < 6 mm diameter each Yes Yes
Stones > 6 mm diameter each No Yes
more likely to choose preoperative ERCP than those in
Intrahepatic stones No Yes nonmetropolitan areas (88% vs 79%, P < 0.001). For
Diameter of cystic duct < 4 mm No Yes CBD stones discovered intraoperatively, 30% chose
Diameter of cystic duct > 4 mm Yes Yes LCBDE as their preferred method of management with
Diameter of common bile duct < 6 mm Yes No
no difference between metropolitan and nonmetropolitan
Diameter of common bile duct > 6 mm Yes Yes
Suturing ability-poor Yes No areas (P = 0.335). The top reasons for not performing
LCBDE were: Availability of a reliable ERCP, lack of
equipment, and lack of skill performing LCBDE. They
Gurusamy et al
[33]
published a cochrane systematic concluded that many surgeons are uncomfortable per
review comparing T-tube with primary closure after forming LCBDE, and advanced training may be needed.
LCBDE. They included three trials randomizing 295 There is a risk of surgeons loosing the art, which may
participants: 147 to T-tube drainage vs 148 to primary still be required in cases of unavailability or failure of
[38]
closure. The operative time was significantly more in ERCP .
the T-tube drainage group compared with the primary Both TC and TD approaches are safe and effective.
closure group (MD 21.22 min; 95%CI: 12.44 to 30.00 TD stone extraction is associated with a increased
min). The duration of hospitalization was significantly risk of bile leaks and requires more expertise in intra-
[21]
more in the T-tube drainage group compared with the corporeal suturing and choledochoscopy . TC stone
primary closure group (MD 3.26 d; 95%CI: 2.49 to 4.04 extraction seems a more accessible technique with
d). According to one trial, the participants randomized to lower complication rates. Choice depends on number of
T-tube drainage took approximately eight days more to stones, size of stone, diameter of cystic duct and CBD
[39]
return to work than the participants randomized to the (Table 1) .
primary closure group (P < 0.005). They concluded that Stone clearance during LCBDE can be confirmed
T-tube drainage is associated with significantly longer by IOC or choledochoscopy. Intra-operative chole
operative time and hospital stay as compared with dochoscopy is better than IOC for determining ductal
primary closure after LCBDE. They also emphasized that clearance after TD LCBDE and is less cumbersome and
currently available evidence cannot justify the routine less time-consuming.
use of T-tube drainage after LCBDE .
[33]
Choledochotomy after LCBDE (TD approach) is
Podda et al
[34]
did a meta-analysis of all studies conventionally managed by T-tube closure. Primary
comparing primary duct closure and T-tube drainage closure of choledochotomy is a safe and effective option
after LCBDE (total 16 studies, 1770 patients). Primary with less operative time and hospital stay. Biliary stent
duct closure showed a significant advantage over T-tube also reduces cost and hospital stay as compared to
in terms of postoperative bile peritonitis (P = 0.02), T-tube. There is lack of randomized trial comparing
operative time, duration of hospitalization, and median primary closure with biliary stent.
hospital cost (all P < 0.00001). In patients having cholangitis, it is advisable to go
for drainage of biliary obstruction by ERCP followed
by LC. LCBDE can be offered to all other patients with
DISCUSSION [21]
CBD stones if expertise is available . If laparoscopic
Pre-operative ERCP followed by LC is the most com exploration fails, it is prudent to convert it to open bile
monly used treatment modality for management of duct exploration and removal of ductal stones.
choledocholithiasis. ERCP carries a high rate of morbidity
and mortality mostly due to post-procedure pancreatitis,
duodenal perforation and bleeding. It also causes injury REFERENCES
to sphincter of oddi which should be avoided in younger 1 Sharma A, Dahiya P, Khullar R, Soni V, Baijal M, Chowbey PK.
patients. LCBDE offers a one stage treatment with Management of common bile duct stones in the laparoscopic era.
Indian J Surg 2012; 74: 264-269 [PMID: 23730054 DOI: 10.1007/
similar or better stone clearance rate and with a shorter s12262-012-0593-6]
hospital stay. It also preserves function of sphincter of 2 Shojaiefard A, Esmaeilzadeh M, Ghafouri A, Mehrabi A. Various
[2,3]
oddi and hence prevents reflux related complications . techniques for the surgical treatment of common bile duct stones: a
LCBDE has been found to be safe even in elderly meta review. Gastroenterol Res Pract 2009; 2009: 840208 [PMID:
population
[14,35]
. A Cochrane systematic review by Martin 19672460 DOI: 10.1155/2009/840208]
[36] 3 Lee HM, Min SK, Lee HK. Long-term results of laparoscopic
et al concluded that a single-stage treatment in the common bile duct exploration by choledochotomy for choledo
form of LCBDE via TC approach is the procedure of cholithiasis: 15-year experience from a single center. Ann Surg
choice for intraoperatively discovered CBD calculi. Treat Res 2014; 86: 1-6 [PMID: 24761400 DOI: 10.4174/astr.2014.
WJGS|www.wjgnet.com 379 May 27, 2016|Volume 8|Issue 5|
Gupta N. Role of laparoscopic CBD exploration
86.1.1] [PMID: 16041208 DOI: 10.1097/01.sla.0000171035.57236]
4 Cuschieri A, Lezoche E, Morino M, Croce E, Lacy A, Toouli J, 18 Sgourakis G, Karaliotas K. Laparoscopic common bile duct
Faggioni A, Ribeiro VM, Jakimowicz J, Visa J, Hanna GB. E.A.E.S. exploration and cholecystectomy versus endoscopic stone extraction
multicenter prospective randomized trial comparing two-stage vs and laparoscopic cholecystectomy for choledocholithiasis. A
single-stage management of patients with gallstone disease and prospective randomized study. Minerva Chir 2002; 57: 467-474
ductal calculi. Surg Endosc 1999; 13: 952-957 [PMID: 10526025 [PMID: 12145577]
DOI: 10.1007/s004649901145] 19 Noble H, Tranter S, Chesworth T, Norton S, Thompson M. A
5 Rogers SJ, Cello JP, Horn JK, Siperstein AE, Schecter WP, randomized, clinical trial to compare endoscopic sphincterotomy
Campbell AR, Mackersie RC, Rodas A, Kreuwel HT, Harris HW. and subsequent laparoscopic cholecystectomy with primary
Prospective randomized trial of LC+LCBDE vs ERCP/S+LC laparoscopic bile duct exploration during cholecystectomy in
for common bile duct stone disease. Arch Surg 2010; 145: 28-33 higher risk patients with choledocholithiasis. J Laparoendosc Adv
[PMID: 20083751 DOI: 10.1001/archsurg.2009.226] Surg Tech A 2009; 19: 713-720 [PMID: 19792866 DOI: 10.1089/
6 Mohamed MA, Bahram MA, Ammar MS, Nassar AH. One- lap.2008.0428]
Session Laparoscopic Management of Combined Common Bile 20 ElGeidie AA, ElShobary MM, Naeem YM. Laparoscopic
Duct and Gallbladder Stones Versus Sequential ERCP Followed exploration versus intraoperative endoscopic sphincterotomy for
by Laparoscopic Cholecystectomy. J Laparoendosc Adv Surg common bile duct stones: a prospective randomized trial. Dig Surg
Tech A 2015; 25: 482-485 [PMID: 25951293 DOI: 10.1089/ 2011; 28: 424-431 [PMID: 22236538 DOI: 10.1159/000331470]
lap.2014.0582] 21 Chander J, Vindal A, Lal P, Gupta N, Ramteke VK. Laparoscopic
7 Liu JG, Wang YJ, Shu GM, Lou C, Zhang J, Du Z. Laparoscopic management of CBD stones: an Indian experience. Surg Endosc
versus endoscopic management of choledocholithiasis in patients 2011; 25: 172-181 [PMID: 20535498 DOI: 10.1007/s00464-010-1
undergoing laparoscopic cholecystectomy: a meta-analysis. 152-5]
J Laparoendosc Adv Surg Tech A 2014; 24: 287-294 [PMID: 22 Topal B, Aerts R, Penninckx F. Laparoscopic common bile duct
24809784 DOI: 10.1089/lap.2013.0546] stone clearance with flexible choledochoscopy. Surg Endosc
8 Nagaraja V, Eslick GD, Cox MR. Systematic review and meta- 2007; 21: 2317-2321 [PMID: 17943379 DOI: 10.1007/s00464-00
analysis of minimally invasive techniques for the management of 7-9577-1]
cholecysto-choledocholithiasis. J Hepatobiliary Pancreat Sci 2014; 23 Vindal A, Chander J, Lal P, Mahendra B. Comparison between
21: 896-901 [PMID: 25187317 DOI: 10.1002/jhbp.152] intraoperative cholangiography and choledochoscopy for ductal
9 Costi R, Mazzeo A, Tartamella F, Manceau C, Vacher B, Valverde clearance in laparoscopic CBD exploration: a prospective ran
A. Cholecystocholedocholithiasis: a case-control study comparing domized study. Surg Endosc 2015; 29: 1030-1038 [PMID:
the short- and long-term outcomes for a “laparoscopy-first” attitude 25154888 DOI: 10.1007/s00464-014-3766-5]
with the outcome for sequential treatment (systematic endoscopic 24 Yi HJ, Hong G, Min SK, Lee HK. Long-term Outcome of Primary
sphincterotomy followed by laparoscopic cholecystectomy). Closure After Laparoscopic Common Bile Duct Exploration
Surg Endosc 2010; 24: 51-62 [PMID: 19466493 DOI: 10.1007/ Combined With Choledochoscopy. Surg Laparosc Endosc
s00464-009-0511-6] Percutan Tech 2015; 25: 250-253 [PMID: 25856136 DOI: 10.1097/
10 Bansal VK, Misra MC, Garg P, Prabhu M. A prospective rando SLE.0000000000000151]
mized trial comparing two-stage versus single-stage management of 25 Dong ZT, Wu GZ, Luo KL, Li JM. Primary closure after laparo
patients with gallstone disease and common bile duct stones. Surg scopic common bile duct exploration versus T-tube. J Surg Res 2014;
Endosc 2010; 24: 1986-1989 [PMID: 20135172 DOI: 10.1007/ 189: 249-254 [PMID: 24746254 DOI: 10.1016/j.jss.2014.03.055]
s00464-010-0891-7] 26 Leida Z, Ping B, Shuguang W, Yu H. A randomized comparison of
11 Dasari BV, Tan CJ, Gurusamy KS, Martin DJ, Kirk G, McKie L, primary closure and T-tube drainage of the common bile duct after
Diamond T, Taylor MA. Surgical versus endoscopic treatment of laparoscopic choledochotomy. Surg Endosc 2008; 22: 1595-1600
bile duct stones. Cochrane Database Syst Rev 2013; 12: CD003327 [PMID: 18202889 DOI: 10.1007/s00464-007-9731-9]
[PMID: 24338858 DOI: 10.1002/14651858.CD003327.pub4] 27 Lyon M, Menon S, Jain A, Kumar H. Use of biliary stent in
12 Zhu HY, Xu M, Shen HJ, Yang C, Li F, Li KW, Shi WJ, Ji F. A laparoscopic common bile duct exploration. Surg Endosc 2015; 29:
meta-analysis of single-stage versus two-stage management for 1094-1098 [PMID: 25249145 DOI: 10.1007/s00464-014-3797-y]
concomitant gallstones and common bile duct stones. Clin Res 28 Dietrich A, Alvarez F, Resio N, Mazza O, de Santibañes E,
Hepatol Gastroenterol 2015; 39: 584-593 [PMID: 25936687 DOI: Pekolj J, Clariá RS, de Santibañes M. Laparoscopic management
10.1016/j.clinre.2015.02.002] of common bile duct stones: transpapillary stenting or external
13 Hongjun H, Yong J, Baoqiang W. Laparoscopic common bile biliary drainage? JSLS 2014; 18: [PMID: 25489219 DOI: 10.4293/
duct exploration: choledochotomy versus transcystic approach? JSLS.2014.00277]
Surg Laparosc Endosc Percutan Tech 2015; 25: 218-222 [PMID: 29 Abellán Morcillo I, Qurashi K, Abrisqueta Carrión J, Martinez Isla
25799258 DOI: 10.1097/SLE.0000000000000133] A. Laparoscopic common bile duct exploration. Lessons learned
14 Wang B, Ding YM, Nie YG, Zhang AM, Wang P, Wang WX. after 200 cases. Cir Esp 2014; 92: 341-347 [PMID: 24559592
The Clinical Evaluation of Laparoscopic Transcystic Duct DOI: 10.1016/j.ciresp.2013.02.010]
Common Bile Duct Exploration in Elderly Choledocholithiasis. 30 Chen D, Zhu A, Zhang Z. Laparoscopic transcystic chole
Hepatogastroenterology 2014; 61: 892-896 [PMID: 26158137] dochotomy with primary suture for choledocholith. JSLS 2015; 19:
15 Reinders JS, Gouma DJ, Ubbink DT, van Ramshorst B, Boerma e2014.00057 [PMID: 25848193 DOI: 10.4293/JSLS.2014.00057]
D. Transcystic or transductal stone extraction during single-stage 31 Estellés Vidagany N, Domingo Del Pozo C, Peris Tomás N, Díez
treatment of choledochocystolithiasis: a systematic review. World Ares JÁ, Vázquez Tarragón A, Blanes Masson F. Eleven years of
J Surg 2014; 38: 2403-2411 [PMID: 24705779 DOI: 10.1007/ primary closure of common bile duct after choledochotomy for
s00268-014-2537-8] choledocholithiasis. Surg Endosc 2016; 30: 1975-1982 [PMID:
16 Rhodes M, Sussman L, Cohen L, Lewis MP. Randomised trial of 26201414 DOI: 10.1007/s00464-015-4424-2]
laparoscopic exploration of common bile duct versus postoperative 32 Hua J, Lin S, Qian D, He Z, Zhang T, Song Z. Primary closure
endoscopic retrograde cholangiography for common bile duct and rate of bile leak following laparoscopic common bile duct
stones. Lancet 1998; 351: 159-161 [PMID: 9449869 DOI: 10.1016/ exploration via choledochotomy. Dig Surg 2015; 32: 1-8 [PMID:
S0140-6736(97)09175-7] 25613528 DOI: 10.1159/000368326]
17 Nathanson LK, O’Rourke NA, Martin IJ, Fielding GA, Cowen AE, 33 Gurusamy KS, Koti R, Davidson BR. T-tube drainage versus
Roberts RK, Kendall BJ, Kerlin P, Devereux BM. Postoperative primary closure after laparoscopic common bile duct exploration.
ERCP versus laparoscopic choledochotomy for clearance of selected Cochrane Database Syst Rev 2013; 6: CD005641 [PMID: 23794201
bile duct calculi: a randomized trial. Ann Surg 2005; 242: 188-192 DOI: 10.1002/14651858.CD005641.pub3]
WJGS|www.wjgnet.com 380 May 27, 2016|Volume 8|Issue 5|
Gupta N. Role of laparoscopic CBD exploration
34 Podda M, Polignano FM, Luhmann A, Wilson MS, Kulli C, Tait 37 Petelin JB. Laparoscopic common bile duct exploration. Surg
IS. Systematic review with meta-analysis of studies comparing Endosc 2003; 17: 1705-1715 [PMID: 12958681 DOI: 10.1007/
primary duct closure and T-tube drainage after laparoscopic s00464-002-8917-4]
common bile duct exploration for choledocholithiasis. Surg Endosc 38 Baucom RB, Feurer ID, Shelton JS, Kummerow K, Holzman MD,
2016; 30: 845-861 [PMID: 26092024 DOI: 10.1007/s00464-015- Poulose BK. Surgeons, ERCP, and laparoscopic common bile duct
4303-x] exploration: do we need a standard approach for common bile duct
35 Shelat VG, Chia VJ, Low J. Common bile duct exploration in stones? Surg Endosc 2016; 30: 414-423 [PMID: 26092008 DOI:
an elderly asian population. Int Surg 2015; 100: 261-267 [PMID: 10.1007/s00464-015-4273-z]
25692428 DOI: 10.9738/INTSURG-D-13-00168.1] 39 Puhalla H, Flint N, O’Rourke N. Surgery for common bile duct
36 Martin DJ, Vernon DR, Toouli J. Surgical versus endoscopic stones--a lost surgical skill; still worthwhile in the minimally
treatment of bile duct stones. Cochrane Database Syst Rev 2006; invasive century? Langenbecks Arch Surg 2015; 400: 119-127
(2): CD003327 [PMID: 16625577] [PMID: 25366358 DOI: 10.1007/s00423-014-1254-y]
P- Reviewer: Kaya M, Lee HC S- Editor: Ji FF
L- Editor: A E- Editor: Liu SQ
WJGS|www.wjgnet.com 381 May 27, 2016|Volume 8|Issue 5|
Published by Baishideng Publishing Group Inc
8226 Regency Drive, Pleasanton, CA 94588, USA
Telephone: +1-925-223-8242
Fax: +1-925-223-8243
E-mail: bpgoffice@wjgnet.com
Help Desk: http://www.wjgnet.com/esps/helpdesk.aspx
http://www.wjgnet.com
© 2016 Baishideng Publishing Group Inc. All rights reserved.
You might also like
- Pediatric Surgery Handbook For Residents and Medical Students (2017)Document428 pagesPediatric Surgery Handbook For Residents and Medical Students (2017)Oana Stefania Pintilii100% (1)
- International Journal of Surgery Open: Tariq Al-Aubaidi, Basim R. Ghadhban, Samer S. ChitheerDocument7 pagesInternational Journal of Surgery Open: Tariq Al-Aubaidi, Basim R. Ghadhban, Samer S. Chitheersamer falconNo ratings yet
- Approach Calculos Wjge 6 32 PDFDocument10 pagesApproach Calculos Wjge 6 32 PDFJavier Alonso Jara CánovasNo ratings yet
- Xanthogranulomatous Cholecystitis - What The Radiologist Should KnowDocument10 pagesXanthogranulomatous Cholecystitis - What The Radiologist Should KnowSamuel WidjajaNo ratings yet
- Conrad Et Al-2017-Journal of Hepato-Biliary-Pancreatic SciencesDocument14 pagesConrad Et Al-2017-Journal of Hepato-Biliary-Pancreatic SciencesAndra CiocanNo ratings yet
- Is Intraoperative Cholangiography Necessary During Laparoscopic Cholecystectomy For Cholelithiasis?Document16 pagesIs Intraoperative Cholangiography Necessary During Laparoscopic Cholecystectomy For Cholelithiasis?Rendy NunuhituNo ratings yet
- Madhu Sud Han 2016Document13 pagesMadhu Sud Han 2016Shivaraj S ANo ratings yet
- Advancements in Upper Gastrointestinal Endoscopic Therapy: A Comprehensive ReviewDocument12 pagesAdvancements in Upper Gastrointestinal Endoscopic Therapy: A Comprehensive ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- WarshawDocument11 pagesWarshawJuan RamirezNo ratings yet
- Cambio de Laparoscopia A Cirugia AbiertaDocument7 pagesCambio de Laparoscopia A Cirugia AbiertaJosé David Cortez Centeno 20190155No ratings yet
- 1 Bjs 10662Document8 pages1 Bjs 10662Vu Duy KienNo ratings yet
- Perforated Peptic Ulcer - An Update: ArticleDocument14 pagesPerforated Peptic Ulcer - An Update: ArticleMuhammad ibnu kaesar PurbaNo ratings yet
- Design and Preliminary Evaluation of A Self-Steering, Pneumatically Driven Colonoscopy RobotDocument15 pagesDesign and Preliminary Evaluation of A Self-Steering, Pneumatically Driven Colonoscopy RobotNguyen SyNo ratings yet
- Tugas Bahasa Inggris Temu 2: A12-B Kelompok 3Document12 pagesTugas Bahasa Inggris Temu 2: A12-B Kelompok 3Wisnu 12No ratings yet
- Laparoscopic and Endoscopic Co-Operative Surgery For Non-Ampullary Duodenal TumorsDocument9 pagesLaparoscopic and Endoscopic Co-Operative Surgery For Non-Ampullary Duodenal TumorsZikry SitaniaNo ratings yet
- Clinical and Radiological Investigations To Predict Difficult Laparoscopic CholecystectomyDocument5 pagesClinical and Radiological Investigations To Predict Difficult Laparoscopic CholecystectomySuyash GhadgeNo ratings yet
- Medscimonit 21 2607Document6 pagesMedscimonit 21 2607jsoang ooiNo ratings yet
- Anastomosis After LaparoscopicDocument16 pagesAnastomosis After LaparoscopicDuratul FahliaNo ratings yet
- Advantages of Laparoscopic Common Bile Duct Exploration in Common Bile Duct StonesDocument5 pagesAdvantages of Laparoscopic Common Bile Duct Exploration in Common Bile Duct Stonesnaili nsnNo ratings yet
- Laparoscopic Versus Open Cystogastrostomy For Pancreatic Pseudocysts A Comparative StudyDocument4 pagesLaparoscopic Versus Open Cystogastrostomy For Pancreatic Pseudocysts A Comparative StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Allison Et AlDocument9 pagesAllison Et AlChintya EltaNo ratings yet
- 9 Management of Common Bile-Duct Stones and Associated Gallbladder Stones: Surgical AspectsDocument14 pages9 Management of Common Bile-Duct Stones and Associated Gallbladder Stones: Surgical AspectsekoNo ratings yet
- Editorial: Percutaneous Drainage of Liver Hydatid Cysts: Is Evidence Enough To Accept It As First Modality of Choice?Document3 pagesEditorial: Percutaneous Drainage of Liver Hydatid Cysts: Is Evidence Enough To Accept It As First Modality of Choice?David CerrónNo ratings yet
- 10.1007@s00464 020 07698 yDocument11 pages10.1007@s00464 020 07698 yGabriel RangelNo ratings yet
- Kenny 2014Document5 pagesKenny 2014Ángel AranaNo ratings yet
- Urinary Lithiasis Conventional Open Surgery2020Revista Da Associacao Medica BrasileiraOpen AccessDocument5 pagesUrinary Lithiasis Conventional Open Surgery2020Revista Da Associacao Medica BrasileiraOpen Accessdev darma karinggaNo ratings yet
- WJG 22 4438Document9 pagesWJG 22 4438prasanna1047No ratings yet
- Cholelithiasis With Choledocholithiasis: Epidemiological, Clinical ProfileDocument3 pagesCholelithiasis With Choledocholithiasis: Epidemiological, Clinical ProfileShashank KumarNo ratings yet
- Huang2020 Article ComparisonOfEmergencyCholecystDocument14 pagesHuang2020 Article ComparisonOfEmergencyCholecystLerdsin PlasticNo ratings yet
- JMinAccessSurg114223-7427737 203757Document8 pagesJMinAccessSurg114223-7427737 203757Jonas De Oliveira MenescalNo ratings yet
- WJGS 8 106Document10 pagesWJGS 8 106thanhNo ratings yet
- 3Document8 pages3polomska.kmNo ratings yet
- Is It Necessary To Ligate Distal Common Bile Duct Stumps After Excising Choledochal Cysts?Document4 pagesIs It Necessary To Ligate Distal Common Bile Duct Stumps After Excising Choledochal Cysts?Rajarshi KumarNo ratings yet
- 10 Carcinomatoza PeritonealaDocument9 pages10 Carcinomatoza PeritonealaGabriela MilitaruNo ratings yet
- Jsls 14 2 246Document5 pagesJsls 14 2 246Maman SulaemanNo ratings yet
- Todani IVDocument3 pagesTodani IVJoshua Patrick MuljadiNo ratings yet
- Cirugía y CirujanosDocument6 pagesCirugía y CirujanosMuhammad Fuad MahfudNo ratings yet
- Optimal Approach To Lobectomy For Non-Small Cell Lung Cancer: Systemic Review and Meta-AnalysisDocument34 pagesOptimal Approach To Lobectomy For Non-Small Cell Lung Cancer: Systemic Review and Meta-AnalysissofiaNo ratings yet
- Meta 4 - de Jong DM - 2022Document13 pagesMeta 4 - de Jong DM - 2022matheus.verasNo ratings yet
- Approach To Incomplete Colonoscopy - New Techniques and Technologies - Gastroenterology & HepatologyDocument15 pagesApproach To Incomplete Colonoscopy - New Techniques and Technologies - Gastroenterology & HepatologyAhmadNassrNo ratings yet
- Bahasa IndonesiaDocument4 pagesBahasa IndonesiaNadiah Umniati SyarifahNo ratings yet
- JurnalDocument6 pagesJurnalAgamMayzulfiNo ratings yet
- 1 s2.0 S1028455922000262 MainDocument8 pages1 s2.0 S1028455922000262 MainDanica SavićNo ratings yet
- Open CholecystectomyDocument35 pagesOpen CholecystectomywqNo ratings yet
- Clinical Spotlight Review - Management of Choledocholithiasis - A SAGES PublicationDocument15 pagesClinical Spotlight Review - Management of Choledocholithiasis - A SAGES PublicationMu TelaNo ratings yet
- MOC IV 2014 Laparoscopy and Elective Colon Resection June 2012Document18 pagesMOC IV 2014 Laparoscopy and Elective Colon Resection June 2012pingusNo ratings yet
- Coloproctology: Results of Videolaparoscopic Surgical Treatment of Diverticular Disease of The ColonDocument5 pagesColoproctology: Results of Videolaparoscopic Surgical Treatment of Diverticular Disease of The ColonMaxend Arselino SilooyNo ratings yet
- The Safety and Feasibility of Laparoscopic Common Bile Duct Exploration For Treatment Patients With Previous Abdominal SurgeryDocument6 pagesThe Safety and Feasibility of Laparoscopic Common Bile Duct Exploration For Treatment Patients With Previous Abdominal SurgeryAndrei SarmientoNo ratings yet
- Esophageal Surgery in Minimally Invasive Era: Lapo Bencini, Luca Moraldi, Ilenia Bartolini, Andrea CorattiDocument14 pagesEsophageal Surgery in Minimally Invasive Era: Lapo Bencini, Luca Moraldi, Ilenia Bartolini, Andrea CorattiBerdasbi XiphoNo ratings yet
- Management of Common Bile Duct Stones at A Tertiary Care HospitalDocument5 pagesManagement of Common Bile Duct Stones at A Tertiary Care Hospitalindex PubNo ratings yet
- Is The Diverticularpapilla A Factor in The Failure of Canulation of The Common Bile Duct in Biliary Stones Pathology?Document7 pagesIs The Diverticularpapilla A Factor in The Failure of Canulation of The Common Bile Duct in Biliary Stones Pathology?IJAR JOURNALNo ratings yet
- Fonc 09 00597Document13 pagesFonc 09 00597Giann PersonaNo ratings yet
- Comparative Study of Single-Incision Laparoscopic Cholecystectomy With Four-Port Conventional Laparoscopic Cholecystectomy A Single-Center ExperienceDocument4 pagesComparative Study of Single-Incision Laparoscopic Cholecystectomy With Four-Port Conventional Laparoscopic Cholecystectomy A Single-Center Experiencerifki indiraNo ratings yet
- Colorectal Disease - 2021 - Christensen - Management Guidelines For Low Anterior Resection Syndrome The MANUEL ProjectDocument15 pagesColorectal Disease - 2021 - Christensen - Management Guidelines For Low Anterior Resection Syndrome The MANUEL ProjectRicardo QuinteiroNo ratings yet
- Quistectomía Laparoscópica en Quiste Hidatídico Hepático: Laparoscopic Cystectomy in Hidatidid CystDocument7 pagesQuistectomía Laparoscópica en Quiste Hidatídico Hepático: Laparoscopic Cystectomy in Hidatidid CystIvette AlvarezNo ratings yet
- Laparoscopic Resection of Pancreatic Neuroendocrine TumorsDocument10 pagesLaparoscopic Resection of Pancreatic Neuroendocrine TumorsWahyudi Permana DarlisNo ratings yet
- Choledocholithiasis: Evolving Standards For Diagnosis and ManagementDocument6 pagesCholedocholithiasis: Evolving Standards For Diagnosis and ManagementAngel Princëzza LovërzNo ratings yet
- Non-Invasive Tools For Compensate D Advance D Chronic Liver Disease and Portal Hypertension After Baveno VII - An UpdateDocument10 pagesNon-Invasive Tools For Compensate D Advance D Chronic Liver Disease and Portal Hypertension After Baveno VII - An UpdateValentina IorgaNo ratings yet
- Acute Pain Management in Symptomatic Cholelithiasis: Tahir Masudi, Helen Capitelli-Mcmahon, Suhail AnwarDocument7 pagesAcute Pain Management in Symptomatic Cholelithiasis: Tahir Masudi, Helen Capitelli-Mcmahon, Suhail AnwarJuan SlaxNo ratings yet
- Residual CholedocholithiasisDocument8 pagesResidual CholedocholithiasisAbu Junayed RifatNo ratings yet
- Post-cholecystectomy Bile Duct InjuryFrom EverandPost-cholecystectomy Bile Duct InjuryVinay K. KapoorNo ratings yet
- Bruxism Affects Stress Responses in Stressed RatsDocument8 pagesBruxism Affects Stress Responses in Stressed RatsJonathan GIraldo MartinezNo ratings yet
- New Test of Competence Webinar Slides 3 December 2020Document42 pagesNew Test of Competence Webinar Slides 3 December 2020Donald QuackNo ratings yet
- Physical Head-To-Toe AssessmentDocument138 pagesPhysical Head-To-Toe AssessmentCRISELLE KHATE TABAGO PAGATPATANNo ratings yet
- A Study About The Relocation of Badjao Community in Totolan 4Document17 pagesA Study About The Relocation of Badjao Community in Totolan 4welpNo ratings yet
- Diagnostic Test in Mapeh 6 Name: - Date: - Teacher: - SectionDocument5 pagesDiagnostic Test in Mapeh 6 Name: - Date: - Teacher: - SectionMelanie Joan Abao PaconNo ratings yet
- NCP Activity IntoleranceDocument1 pageNCP Activity IntoleranceBen David100% (2)
- Advanced Endoscopic TechnologiesDocument14 pagesAdvanced Endoscopic TechnologiesLeticia Fruchi CostaNo ratings yet
- MSDS Ethanol (E10) by Neste (2018)Document28 pagesMSDS Ethanol (E10) by Neste (2018)Torero02No ratings yet
- Grade 12 Pre Board I 2020 21QuPDocument17 pagesGrade 12 Pre Board I 2020 21QuPManav Ji ManavNo ratings yet
- NCP For PCAPDocument4 pagesNCP For PCAPDianeNo ratings yet
- Drexel Resident Handbook 2018-2019Document119 pagesDrexel Resident Handbook 2018-2019samNo ratings yet
- Pulmonary Function TestsDocument57 pagesPulmonary Function Testsmerin sunilNo ratings yet
- Meconium Aspiration SyndromeDocument20 pagesMeconium Aspiration SyndromeLevi PosadasNo ratings yet
- IHR Status 208 NepalDocument2 pagesIHR Status 208 NepalKeshab RijalNo ratings yet
- Regular 20 Regular 30 Regular 50 Urgent 20 Urgent 30 Urgent 50Document2 pagesRegular 20 Regular 30 Regular 50 Urgent 20 Urgent 30 Urgent 50Arwa Algezeri0% (1)
- ĐIỀN TỪ VÀO ĐOẠN VĂN - ANH 9Document5 pagesĐIỀN TỪ VÀO ĐOẠN VĂN - ANH 9nvo169007No ratings yet
- 3 - Development From Conception To BirthDocument50 pages3 - Development From Conception To BirthMa. Angelica PampagNo ratings yet
- Gi Notes: Nurs 3103 Pathophysiology Teri L. Hernandez, PHD, RNDocument4 pagesGi Notes: Nurs 3103 Pathophysiology Teri L. Hernandez, PHD, RNjuliafinnNo ratings yet
- Autotransplantation of Teeth: An: OrthodonticsDocument8 pagesAutotransplantation of Teeth: An: OrthodonticshayiarNo ratings yet
- Master Rekam Medis Nama PasienDocument24 pagesMaster Rekam Medis Nama PasienHachiNo ratings yet
- Root Coverage With Emdogain/ Alloderm: A New Way To Treat Gingival RecessionsDocument20 pagesRoot Coverage With Emdogain/ Alloderm: A New Way To Treat Gingival RecessionsAdam HusniNo ratings yet
- LALLEMAND Sel Yeast in RuminantsDocument5 pagesLALLEMAND Sel Yeast in Ruminantsأمالي أريفينNo ratings yet
- Health Maintenance of InfantDocument59 pagesHealth Maintenance of InfantMohamed Na3eemNo ratings yet
- English: Fiji Year 12 Certificate Examination 2018Document38 pagesEnglish: Fiji Year 12 Certificate Examination 2018tarusilaNo ratings yet
- Culture Effects Upon HealthDocument3 pagesCulture Effects Upon HealthTinotenda ChetenNo ratings yet
- Contributors: Consulting EditorDocument174 pagesContributors: Consulting EditorJasNo ratings yet
- The Child Survivor Healing Developmental Trauma AnDocument68 pagesThe Child Survivor Healing Developmental Trauma Anpetrila deboraNo ratings yet
- LP On Baby BathDocument11 pagesLP On Baby BathSandeep DahiyaNo ratings yet
- Everyone in Phase 1A, Groups 1,2,3 and 4 Is Eligible For The VaccineDocument3 pagesEveryone in Phase 1A, Groups 1,2,3 and 4 Is Eligible For The VaccineSinclair Broadcast Group - EugeneNo ratings yet