Professional Documents
Culture Documents
Predictors and Outcome of Acute Kidney Injury in Children With Diabetic Ketoacidosis
Uploaded by
MarcelliaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Predictors and Outcome of Acute Kidney Injury in Children With Diabetic Ketoacidosis
Uploaded by
MarcelliaCopyright:
Available Formats
RESEARCH PAPER
Predictors and Outcome of Acute Kidney Injury in Children with Diabetic
Ketoacidosis
MULLAI BAALAAJI, MURALIDHARAN JAYASHREE, KARTHI NALLASAMY, SUNIT SINGHI AND ARUN BANSAL
From the Pediatric Emergency and Intensive Care Units, Department of Pediatrics, Post Graduate Institute of Medical Education
and Research, Chandigarh, India.
Correspondence to: Dr Jayashree Objective: To identify predictors and outcome of acute kidney injury (AKI) in children with
Muralidharan, Professor and Chief, diabetic ketoacidosis (DKA) admitted to a Pediatric Intensive Care Unit (PICU). Methods:
Pediatric Emergency and Intensive Retrospective case review of 79 children with DKA admitted between 2011-2014. Results: 28
children developed AKI during the hospital stay; 20 (71.4%) recovered with hydration alone.
Care Units, Department of Pediatrics,
Serum chloride at 24 hours was independently associated with AKI. Children with AKI had
Post Graduate Institute of Medical prolonged acidosis, longer PICU stay, and higher mortality. Conclusions: Majority of children
Education and Research, Chandigarh, with AKI and DKA recover with hydration. Hyperchloremia at 24 hours had independent
India. mjshree@hotmail.com association with AKI, although cause-effect relation could not be ascertained.
Received: March 01, 2017; Keywords: Diabetes, Hyperchloremia, Outcome, Renal failure.
Initial review: June 19, 2017;
Accepted: January 23, 2018.
Published online: February 09, 2018. PII:S097475591600113
D
iabetic ketoacidosis (DKA) is a life- pRIFLE classification using estimated creatinine
threatening complication of diabetes with a clearance (eCCl), as urine output criterion is unreliable in
reported frequency ranging from 15-70% the setting of osmotic diuresis [7]. The patients were
across different study populations. Mortality classified into one of the three pRIFLE categories at three
from DKA in developing countries is still high (3.4%- time points viz, admission, 12 hours and 24 hours.
13%), due to putative reasons like cerebral edema, sepsis, Children with pRIFLE category 0-1 were labelled as ‘No
venous thrombosis and dyselectrolytemias [1-3]. AKI’ and those with pRIFLE category 2-3 at admission
Although renal injury is frequently encountered in were labelled as ‘AKI at admission’. Children who
hyperglycemic hyperosmolar state, it is not so well progressed from ‘No AKI’ at admission to pRIFLE 2-3
reported in DKA [4]. Furthermore, renal injury can be during hospital stay were labelled as ‘AKI progression’.
masked in children with DKA, due to osmotic diuresis
Univariate and multivariate analyses was done to
and spurious elevations in creatinine secondary to
compare demographic and biochemical characteristics
ketonemia. We undertook this study to evaluate the
between ‘No AKI’ and ‘AKI progression’ groups. P value
predictors and outcome of AKI in children with DKA
<0.05 was considered significant.
admitted to a Pediatric Intensive Care Unit (PICU).
RESULTS
METHODS
Of 79 children enrolled, 56 (71%) were new onset
Electronic medical records of children with DKA
diabetes presenting as DKA. In children with
admitted consecutively to our PICU from 2011-2014
documented healthcare contacts prior to referral (n=51),
were accessed retrospectively after seeking ethical
DKA was diagnosed only in 18 (35.3%), of which just 8
clearance. DKA was diagnosed using standard definitions
(44.4%) received appropriate fluids and insulin prior to
[5]. Rehydration was based on sum of 6.5% deficit and
referral. Majority of the children (n=59, 75%) had
maintenance over 36 hours. Additional bolus of 20 mL/kg
presented as severe DKA.
isotonic saline was administered in first hour to children
with hypoperfusion or hypotension. Isotonic saline was Twenty eight (35%) children were diagnosed with
continued until the blood glucose fell to ≤13.9 mmol/L AKI; 13 (46.4%) at admission and rest within 24 hours of
(250 mg/dL) after which fluid was changed to N/2 saline hospital stay. The number (proportion) of children
with 5% Dextrose. Insulin was started after first hour at a categorized into pRIFLE-0,1,2,3 at admission and end of
rate of 0.05- 0.1 U/kg/hour [6]. AKI was defined by 24 hours were 35 (44.3%), 31 (39.2%), 11 (13.9%), 2
INDIAN PEDIATRICS 311 VOLUME 55__APRIL 15, 2018
Copyright of Indian Pediatrics 2018
For personal use only. Not for bulk copying or unauthorized posting to listserv/websites
BAALAAJI, et al. AKI IN DIABETIC KETOACIDOSIS
(2.5%) and 54 (68.4%), 10 (12.6%), 9 (11.4%) and 6 TABLE II COMPARISON OF ‘NO AKI’ AND ‘AKI PROGRESSION’ –
(7.6%), respectively. Twenty (71.4%) children recovered MULTIVARIATE ANALYSIS
with hydration alone while 8 (28.6%) required renal Characteristics Adjusted OR (95% CI) P value
replacement therapy (RRT).
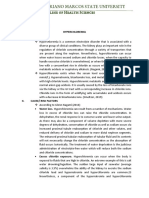
PRISM III Score 1.07 (0.96, 1.2) 0.20
None of the admission variables could predict AKI. 24 hours serum corrected 0.70 (0.39, 1.26) 0.24
However on multivariable analysis, elevated chloride sodium (mmol/L)
levels at 24 hours had an independent association 24 hours serum effective 1.19 (0.89, 1.57) 0.23
with AKI progression [Adjusted OR 1.14 (95% CI osmolality (mmol/kg)
1.04-1.27), P=0.007] (Table I and II). Serum chloride 24 hours serum chloride 1.20 (1.05, 1.37) 0.008
>112 mmol/L at 24 hours had a sensitivity, specificity and (mmol/L)
area under ROC curve of 73.3%, 82.4% and 0.835, AKI: acute kidney injury.
respectively for development of AKI (P<0.001).
DISCUSSION
Time to resolution of acidosis was significantly
longer in those with AKI than those without [Median One-third of our patients with DKA had AKI at some
(IQR) 31 (24, 77) vs 26 (20, 35) hours, P=0.006]. point during their PICU stay, with nearly half of them
Children with AKI had higher odds for needing having AKI at presentation. Majority of the children were
vasoactive drugs and ventilation, and developing new-onset DKA, who remained undiagnosed prior to
cerebral edema. Those with AKI had prolonged PICU referral and tended to present as severe DKA . This trend
stay [Median (IQR) 3 (2, 5) vs 2 (1, 2) days, P<0.001] and was similar to our previous observations [1,2] and in
lesser likelihood to survive to hospital discharge sharp contrast to the data from the developed world [8].
(Table III). Those with missed diagnosis had more likelihood of
TABLE I COMPARISON OF ‘NO AKI’ AND ‘AKI PROGRESSION’ – UNIVARIATE ANALYSIS
Variable No AKI (n=51) Mean (SD) AKI progression (n=15) Mean (SD) P value
Age (years) 7.3 (3.6) 8.2 (3.6) 0.37
PRISM III Score 23 (7) 27 (8) 0.07
At admission
- Blood glucose (mmol/L) 25.3 (6.8) 23.7 (9.2) 0.44
- Blood urea nitrogen (mmol/L) 2.6 (1.2) 3 (1) 0.19
- Serum creatinine (µmol/L) 53 (26.5) 75 (26.5) 0.01
- Corrected serum sodium (mmol/L) 139 (6) 142 (12) 0.53
- Serum Chloride (mmol/L) 101 (8) 107 (13) 0.09
- Blood bicarbonate (mmol/L) 6 (3) 5 (2) 0.18
- Blood pH 7.05 (0.12) 6.99 (0.13) 0.14
- Serum effective osmolality (mmol/kg) 293.3 (12.4) 296.3 (23.5) 0.64
At 24 hours
- Blood glucose (mmol/L) 11.3 (4.4) 13.8 (4.4) 0.01
- Blood urea nitrogen (mmol/L)* 3.5 (2.1) 8.1 (5.2) <0.001
- Serum creatinine (µmol/L)# 41 (18) 124 (86) <0.001
- Corrected serum sodium (mmol/L) 138.7 (5.9) 145.7 (10.5) 0.001
- Serum chloride (mmol/L) 106.6 (7.2) 118.6 (10.3) 0.001
- Blood bicarbonate (mmol/L) 15.8 (3.4) 10.9 (4.8) <0.001
- Blood pH 7.25 (0.14) 7.13 (0.13) 0.003
- Serum effective osmolality (mmol/kg) 285.5 (12.5) 301 (21.1) 0.001
*24 hours Blood urea nitrogen (mmol/L) expressed as Median (IQR) among No AKI vs. AKI progression: 2.8 (2,4.8) vs. 6 (5,9.3); P<0.001; #Median
(IQR) 24 hours creatinine (µmol/L) No AKI vs AKI progression: 35 (27,49) vs. 97 (57,124); P<0.001.
INDIAN PEDIATRICS 312 VOLUME 55__APRIL 15, 2018
Copyright of Indian Pediatrics 2018
For personal use only. Not for bulk copying or unauthorized posting to listserv/websites
BAALAAJI, et al. AKI IN DIABETIC KETOACIDOSIS
WHAT THIS STUDY ADDS?
• 24-hour serum chloride was an independent predictor of acute kidney injury in children with diabetic ketoacidosis.
TABLE III PICU NEEDS, COMPLICATIONS AND OUTCOME OF due to the retrospective nature of our data. Use of
CHILDREN WITH DKA AND AKI balanced crystalloids with lower chloride content have
Characteristics Odds ratio P value been studied in adults with DKA [14,15], but mostly in
(95% CI) relation to hyperchloremia induced normal anion gap
acidosis.
Vasoactive requirement 5.1 (1.5-17) 0.005
Mechanical ventilation requirement 7.6 (1.8-31) 0.002 There is, thus, a need for for future prospective
studies on risk factors of AKI, cause-effect relationship
Cerebral edema 7.6 (1.8-31) 0.002
between AKI and type of fluid, and role of balanced salt
Mortality in PICU 13.6 (1.5-120) 0.004
solutions in preventing AKI in children with DKA.
Survival to hospital 0.07 (0.01-0.6) 0.004
Contributors: MB: study conceptualization, data collection,
statistical analysis, drafting the manuscript; MJ: study
conceptualization, supervised data collection and statistical
complications like cerebral edema (CE) and AKI,
analysis, critical review of the manuscript; KN, SS, AB: data
possibly related to uncorrected hypovolemia [2]. The analysis, critical review of the manuscript, drafted the manuscript.
small proportion in whom AKI did not revert with fluids, All authors approved the final version of the manuscript.
needed RRT, indicating that factors other than Funding: None; Competing Interest: None stated.
hypovolemia could have contributed to AKI.
REFERENCES
Although children with ‘AKI progression’ had higher
1. Jayashree M, Singhi S. Diabetic ketoacidosis: predictors of
PRISM III and admission chloride levels, only the 24
outcome in a pediatric intensive care unit of a developing
hours serum chloride was independently associated with country. Pediatr Crit Care Med. 2004;5:427-33.
‘AKI progression’. Independent association of 24 hour 2. Tiwari LK, Jayashree M, Singhi S. Risk factors for cerebral
serum chloride rather than admission value leads one to edema in diabetic ketoacidosis in a developing country.
believe that hyperchloremia could have been an Pediatr Crit Care Med. 2012;13:e91-6.
iatrogenic element caused by the type of intravenous 3. Poovazhagi V. Risk factors for mortality in children with
fluids received. Though the current guidelines favour diabetic ketoacidosis from developing countries. World J
isotonic saline as the initial fluid in DKA, the Diabetes. 2014;5:932-8.
recommended duration of infusion is not clear. Since half 4. Zeitler P, Haqq A, Rosenbloom A, Glaser N; Drugs and
Therapeutics Committee of the Lawson Wilkins Pediatric
normal saline without dextrose was not easily available in
Endocrine Society. Hyperglycemic hyperosmolar
our setup, children continued to receive isotonic saline till syndrome in children: pathophysiological considerations
blood glucose fell to 250 mg/dL. and suggested guidelines for treatment. J Pediatr.
Hyperchloremia, in many clinical settings has been 2011;158:9-14,14.e1-2.
5. Wolfsdorf JI, Allgrove J, Craig ME, Edge J, Glaser N, Jain
hypothesised to cause renal hypoperfusion and AKI by
V, et al. ISPAD Clinical Practice Consensus Guidelines
virtue of its renal vascular smooth muscle constrictor 2014. Diabetic Ketoacidosis and Hyperglycemic
effect [9,10]. Hursh, et al. [1] reported AKI in a high Hyperosmolar State. Pediatr Diabetes. 2014;15:154-79.
proportion of children with DKA (64.2%) using Kidney 6. Nallasamy K, Jayashree M, Singhi S, Bansal A. Low-dose
Disease/Improving Global Outcomes criteria, but none in insulin vs standard-dose insulin in pediatric diabetic
association with hyperchloremia. Although studies from ketoacidosis–A randomized clinical trial. JAMA Pediatr.
developing world have reported about 4-11% incidence 2014;168:999-1005.
of renal injury in children with DKA [12,13] neither 7. Akcan-Arikan A, Zappitelli M, Loftis LL, Washburn KK,
standard definitions were used nor association with Jefferson LS, Goldstein SL. Modified RIFLE criteria in
critically ill children with Acute kidney injury. Kidney Int.
hyperchloremia was reported. The disparity in incidence
2007;71:1028-35.
of AKI between studies is largely related to use of 8. Jefferies C, Cutfield S, Derraik JG, Bhagvandas J, Albert
different definitions. Though we demonstrated a BB, Hofman PL, et al. 15-year incidence of diabetic
significant association between hyperchloremia at 24 hrs ketoacidosis at onset of type 1 diabetes in children from a
and AKI in our study, a causal link cannot be ascertained regional setting (Auckland, New Zealand). Sci Rep.
INDIAN PEDIATRICS 313 VOLUME 55__APRIL 15, 2018
Copyright of Indian Pediatrics 2018
For personal use only. Not for bulk copying or unauthorized posting to listserv/websites
BAALAAJI, et al. AKI IN DIABETIC KETOACIDOSIS
2015;5:10358. 12. Kanwal SK, Bando A, Kumar V. Clinical profile of
9. Marrttinen M, Wilkman E, Petaja L, Suojaranta-Ylinen R, diabetic ketoacidosis in Indian children. Indian J Pediatr.
Pettila V, Vaara ST. Association of plasma chloride values 2012;79:901-4.
with acute kidney injury in the critically ill – a prospective 13. Asl AS, Maleknejad S, Kelachaye ME. Diabetic
observational study. Acta Anaesthesiol Scand. ketoacidosis and its complications among children. Acta
2016;60:790-9. Med Iran. 2011;49:113-4.
10. Zhang Z, Xu X, Fan H, Li D, Deng H. Higher serum 14. Chua HR, Venkatesh B, Stachowski E, Schneider AG,
chloride concentrations are associated with acute kidney Perkins K, Ladanyi S, et al. Plasma-Lyte 148 vs 0.9% saline
injury in unselected critically ill patients. BMC Nephrol. for fluid resuscitation in diabetic ketoacidosis. J Crit Care.
2013;14:235. 2012;27:138-45.
11. Hursh BE, Ronsley R, Islam N, Panagiotopoulos C. Acute 15. Basnet S, Venepalli PK, Andoh J, Verhulst S, Koirala J.
kidney injury in children with type 1 diabetes hospitalized Effect of normal saline and half normal saline on serum
for diabetic ketoacidosis. JAMA Pediatr. 2017; electrolytes during recovery phase of diabetic ketoacidosis.
171:e170020. J Intensive Care Med. 2014;29:38-42.
INDIAN PEDIATRICS 314 VOLUME 55__APRIL 15, 2018
Copyright of Indian Pediatrics 2018
For personal use only. Not for bulk copying or unauthorized posting to listserv/websites
You might also like
- 0.9% Saline Versus Plasma-Lyte As InitialDocument10 pages0.9% Saline Versus Plasma-Lyte As InitialYogiPrimaZulkifliNo ratings yet
- Markers of Disease Severity and Prolonged Length of Stay For Paediatric Diabetic KetoacidosisDocument6 pagesMarkers of Disease Severity and Prolonged Length of Stay For Paediatric Diabetic KetoacidosisSSR-IIJLS JournalNo ratings yet
- Jurna Aki, MalariaDocument7 pagesJurna Aki, MalariaDewy TerangNo ratings yet
- Anemia in Pre-School Children-Does Time Change Anything?Document5 pagesAnemia in Pre-School Children-Does Time Change Anything?NZ FreelancersNo ratings yet
- Can Lactate Clearance Predict Mortality in Critically Ill Children?Document6 pagesCan Lactate Clearance Predict Mortality in Critically Ill Children?Sam Aguilar FigueroaNo ratings yet
- 406-01. Manuscript (Article Text) - 1308-1-10-20130405Document4 pages406-01. Manuscript (Article Text) - 1308-1-10-20130405Jeffrey RamosNo ratings yet
- Jurnal GEADocument5 pagesJurnal GEARian KurniawanNo ratings yet
- Metabolic Syndrome Components and Age-RelatedDocument8 pagesMetabolic Syndrome Components and Age-RelatedOki LambeNo ratings yet
- Diagnosis and Treatment of Acute Kidney Injury in PediatricsDocument13 pagesDiagnosis and Treatment of Acute Kidney Injury in PediatricsagungNo ratings yet
- Early Acute Kidney Injury Predicts Progressive Renal Dysfunction and Higher Mortality in Severely Burned AdultsDocument23 pagesEarly Acute Kidney Injury Predicts Progressive Renal Dysfunction and Higher Mortality in Severely Burned AdultsKartika JuwitaNo ratings yet
- Paediatrica Indonesiana: Nur Rochmah, Muhammad Faizi, Netty HarjantienDocument4 pagesPaediatrica Indonesiana: Nur Rochmah, Muhammad Faizi, Netty HarjantienSafadilla ummia yolandaNo ratings yet
- Axial Myopia and Low HbA1c Level Are Correlated AnDocument8 pagesAxial Myopia and Low HbA1c Level Are Correlated AnGeert SmoldNo ratings yet
- Current Recommendations For Management of Paediatric Diabetic KetoacidosisDocument5 pagesCurrent Recommendations For Management of Paediatric Diabetic Ketoacidosisab_ghaffar_latiffi9337No ratings yet
- Management of Acute Kidney Injury in Children: Sri Lanka Journal of Child Health January 2019Document6 pagesManagement of Acute Kidney Injury in Children: Sri Lanka Journal of Child Health January 2019HannaSaskiaIINo ratings yet
- Jurnal AkiDocument8 pagesJurnal Akinelly muslimahNo ratings yet
- Acute Kidney Injury in ChildrenDocument8 pagesAcute Kidney Injury in ChildrenInfectologia ClinicaNo ratings yet
- Prediction of Severe Acute Kidney Injury Using Renal Angina Index in A Pediatric Intensive Care UnitDocument6 pagesPrediction of Severe Acute Kidney Injury Using Renal Angina Index in A Pediatric Intensive Care UnitdoctoramanphalswalNo ratings yet
- Study of Etiology, Clinical Profile and Outcome of Acute Kidney (AKI) in Medical Intensive Care UnitDocument4 pagesStudy of Etiology, Clinical Profile and Outcome of Acute Kidney (AKI) in Medical Intensive Care UnitDavid Al HavizNo ratings yet
- Pediatric Acute Kidney Injury: Focusing On Diagnosis and ManagementDocument8 pagesPediatric Acute Kidney Injury: Focusing On Diagnosis and ManagementIrkania PasangkaNo ratings yet
- Bellomo 2006Document7 pagesBellomo 2006Manal regraguiNo ratings yet
- ISPAD Clinical Practice Consensus Guidelines 2022: Diabetic Ketoacidosis and Hyperglycemic Hyperosmolar StateDocument23 pagesISPAD Clinical Practice Consensus Guidelines 2022: Diabetic Ketoacidosis and Hyperglycemic Hyperosmolar StateMarianne Joy PontigonNo ratings yet
- Electrocardiometry For Hemodynamic Categorization and Assessment of Fluid Responsiveness in Pediatric Septic Shock - A Pilot Observational StudyDocument8 pagesElectrocardiometry For Hemodynamic Categorization and Assessment of Fluid Responsiveness in Pediatric Septic Shock - A Pilot Observational StudyMarselya GaniNo ratings yet
- Characteristics of Pediatric Patients With Diarrhea in Indonesia: A Laboratory-Based ReportDocument8 pagesCharacteristics of Pediatric Patients With Diarrhea in Indonesia: A Laboratory-Based ReportDrnNo ratings yet
- RESEARCH ARTICLEOpen AccessChallenges of Acute Peritoneal Dialysis Inextremely-Low-Birth-Weight Infants - Aretrospective Cohort StudyDocument9 pagesRESEARCH ARTICLEOpen AccessChallenges of Acute Peritoneal Dialysis Inextremely-Low-Birth-Weight Infants - Aretrospective Cohort StudysavitageraNo ratings yet
- Fitzgerald 1992Document5 pagesFitzgerald 1992Quetzi Victoria Gutiérrez RayasNo ratings yet
- Chawla 2011Document9 pagesChawla 2011samuel anchondoNo ratings yet
- Jurnal ReadingDocument41 pagesJurnal ReadinghappymedlifeNo ratings yet
- Safety and Efficacy of Packed Red Blood Cell Transfusions at Different Doses in Very Low Birth Weight InfantsDocument3 pagesSafety and Efficacy of Packed Red Blood Cell Transfusions at Different Doses in Very Low Birth Weight InfantsVidini Kusuma AjiNo ratings yet
- Jurnal HighlightDocument4 pagesJurnal HighlightStrangersNo ratings yet
- ACKD in DogsDocument9 pagesACKD in DogsGreomary Cristina MalaverNo ratings yet
- Research ArticleDocument6 pagesResearch Articlefitri asymidaNo ratings yet
- Jnma 61 258 115Document4 pagesJnma 61 258 115Nicolás Mosso F.No ratings yet
- Guia 13481Document22 pagesGuia 13481CarmenNo ratings yet
- Prevalence and Potential Risk Factors of Hypokalemia in Pediatric Patients With Diabetic KetoacidosisDocument2 pagesPrevalence and Potential Risk Factors of Hypokalemia in Pediatric Patients With Diabetic KetoacidosisAti Rahmi PurwandariNo ratings yet
- Content ServerDocument9 pagesContent ServerNourma Kusuma WinawanNo ratings yet
- 10 1016@j Ajem 2020 01 046Document7 pages10 1016@j Ajem 2020 01 046Nurul Huda KowitaNo ratings yet
- 10 1016@j Ajem 2020 01 046Document7 pages10 1016@j Ajem 2020 01 046Nurul Huda KowitaNo ratings yet
- Etm-12-02-0987 LiquidosDocument4 pagesEtm-12-02-0987 LiquidosKarenMartinezNo ratings yet
- Medicine: Congenital Chloride Losing DiarrheaDocument9 pagesMedicine: Congenital Chloride Losing DiarrheaGabriela PopescuNo ratings yet
- Pi Is 0883944117309656Document6 pagesPi Is 0883944117309656Dea PuspitaNo ratings yet
- Acut Kidney InjuryDocument12 pagesAcut Kidney InjuryorriNo ratings yet
- Risk Factors, Complications and Outcome of Cholelithiasis in Children: A Retrospective, Single-Centre ReviewDocument6 pagesRisk Factors, Complications and Outcome of Cholelithiasis in Children: A Retrospective, Single-Centre ReviewBenny KurniawanNo ratings yet
- Research Article IP FirstDocument8 pagesResearch Article IP FirstSatvik BansalNo ratings yet
- Ajkd 2023 Mortality and Major Adverse Kidney Events AkiDocument12 pagesAjkd 2023 Mortality and Major Adverse Kidney Events AkiAlexandra TofanNo ratings yet
- Guia Ispad 2022 Cetoacidosis Diabetica y Estadi HiperosmolarDocument22 pagesGuia Ispad 2022 Cetoacidosis Diabetica y Estadi HiperosmolarElizabeth Cross50% (2)
- Pediatric Diabetes - 2022 - GlaserDocument22 pagesPediatric Diabetes - 2022 - GlasersyukriNo ratings yet
- Defining Reduced Urine Output in Neonatal ICU ImpoDocument10 pagesDefining Reduced Urine Output in Neonatal ICU Impohamudek kasaNo ratings yet
- Acute Kidney Injury - Diagnosis and Management 2019Document8 pagesAcute Kidney Injury - Diagnosis and Management 2019srikandiNo ratings yet
- Baby Hug Trial - Hidroxyrea For Sickle Cell Disease in ChildrenDocument8 pagesBaby Hug Trial - Hidroxyrea For Sickle Cell Disease in ChildrenTiago UchôaNo ratings yet
- Clinical Manifestation in Sickle Cell Anemia: A Study in Chhattisgarh Institute of Medical Sciences (CIMS) Bilaspur, Chhattisgarh, India.Document4 pagesClinical Manifestation in Sickle Cell Anemia: A Study in Chhattisgarh Institute of Medical Sciences (CIMS) Bilaspur, Chhattisgarh, India.IOSRjournalNo ratings yet
- Post Partum AKIDocument5 pagesPost Partum AKISajid MehmoodNo ratings yet
- A Comparison of The RIFLE and AKIN Criteria For Acute Kidney InjuryDocument6 pagesA Comparison of The RIFLE and AKIN Criteria For Acute Kidney InjuryFranciana AzêdoNo ratings yet
- The Definition of Acute Kidney Injury and Its Use in PracticeDocument12 pagesThe Definition of Acute Kidney Injury and Its Use in PracticeErwin SiahaanNo ratings yet
- Cystatin C As A Novel Predictor of Preterm Labor in Severe PreeclampsiaDocument9 pagesCystatin C As A Novel Predictor of Preterm Labor in Severe PreeclampsiahandiNo ratings yet
- Chen 2013Document6 pagesChen 2013malaNo ratings yet
- Pediatric DiabeticDocument9 pagesPediatric Diabeticperla islasNo ratings yet
- Evolution of Haemodynamics and Outcome of Fluid Refractory Septic Shock in ChildrenDocument8 pagesEvolution of Haemodynamics and Outcome of Fluid Refractory Septic Shock in ChildrenpetrarizkyNo ratings yet
- Clinical Features and Outcomes of Children Admitted To The PICU Due To Rotavirus Infection GUNDocument5 pagesClinical Features and Outcomes of Children Admitted To The PICU Due To Rotavirus Infection GUNRoxana Ștefania DrăganNo ratings yet
- Faecal Calprotectin in Treated and Untreated Children With CoeliacDocument4 pagesFaecal Calprotectin in Treated and Untreated Children With CoeliacNejc KovačNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 1: EENT (Eyes, Ears, Nose and Throat)From EverandComplementary and Alternative Medical Lab Testing Part 1: EENT (Eyes, Ears, Nose and Throat)No ratings yet
- 2012 Gemc Res Hartmann Hemostasis OerDocument48 pages2012 Gemc Res Hartmann Hemostasis OerMarcelliaNo ratings yet
- Thrombotic Microangiopathies: T. Matthew Eison, MD Lebonheur Children'S Hospital Pediatric NephrologyDocument83 pagesThrombotic Microangiopathies: T. Matthew Eison, MD Lebonheur Children'S Hospital Pediatric NephrologyMarcelliaNo ratings yet
- Pathology Bleeding DisordersDocument67 pagesPathology Bleeding DisordersMarcelliaNo ratings yet
- 0900 0920 Antiplatelet and Anticoaulation Therapy Aleti FINALDocument31 pages0900 0920 Antiplatelet and Anticoaulation Therapy Aleti FINALMarcelliaNo ratings yet
- PAPDI DR Mardiah Suci Hardianti - Case Study ThrombocytopeniaDocument43 pagesPAPDI DR Mardiah Suci Hardianti - Case Study ThrombocytopeniaMarcelliaNo ratings yet
- Thrombocytopenia in The Intensive Care UnitDocument35 pagesThrombocytopenia in The Intensive Care UnitMarcelliaNo ratings yet
- 10.1038@s41430 019 0512 ZDocument12 pages10.1038@s41430 019 0512 ZMarcelliaNo ratings yet
- Alm037 01 02Document10 pagesAlm037 01 02MarcelliaNo ratings yet
- Proteinuria A Guide To Diagnosis and AssDocument7 pagesProteinuria A Guide To Diagnosis and AssMarcelliaNo ratings yet
- Effectiveness of Plasma and Urine Neutrophil Gelatinase-Associated Lipocalin For Predicting Acute Kidney Injury in High-Risk PatientsDocument8 pagesEffectiveness of Plasma and Urine Neutrophil Gelatinase-Associated Lipocalin For Predicting Acute Kidney Injury in High-Risk PatientsMarcelliaNo ratings yet
- Acute Kidney Injury and Diabetic Ketoacidosis in Pediatric Patients: Risk FactorsDocument4 pagesAcute Kidney Injury and Diabetic Ketoacidosis in Pediatric Patients: Risk FactorsMarcelliaNo ratings yet
- Kaewput 2020Document11 pagesKaewput 2020MarcelliaNo ratings yet
- Incidence and Characteristics of Acute Kidney Injury in Severe Diabetic KetoacidosisDocument6 pagesIncidence and Characteristics of Acute Kidney Injury in Severe Diabetic KetoacidosisMarcelliaNo ratings yet
- 192 FullDocument3 pages192 FullMarcelliaNo ratings yet
- Hemolytic Anemia Inherited: Hematologi-Onkologi Division Child Departement - Fkusu/RshamDocument56 pagesHemolytic Anemia Inherited: Hematologi-Onkologi Division Child Departement - Fkusu/RshamMarcelliaNo ratings yet
- Crystalloid and Colloid TherapyDocument11 pagesCrystalloid and Colloid TherapyAlexa UGNo ratings yet
- Fluids and Electrolytes ImbalancesDocument7 pagesFluids and Electrolytes Imbalancessinister17No ratings yet
- PUCAN, Julienne BSN III-D - NCP - HYPO&HYPERCHLOREMIADocument2 pagesPUCAN, Julienne BSN III-D - NCP - HYPO&HYPERCHLOREMIAJulienne PucanNo ratings yet
- Choice of Fluid Type Physiological Concepts and Perioperative IndicationsDocument13 pagesChoice of Fluid Type Physiological Concepts and Perioperative IndicationsCharlieBrown_QBNo ratings yet
- Reading Synthesis # 2: San Roque Extension, Roxas City, Capiz, Philippines 5800Document10 pagesReading Synthesis # 2: San Roque Extension, Roxas City, Capiz, Philippines 5800Jay VillasotoNo ratings yet
- Aguinaldo, Sophia Kaye M. Hypochloremia & HyperchloremiaDocument9 pagesAguinaldo, Sophia Kaye M. Hypochloremia & HyperchloremiaSophia Kaye AguinaldoNo ratings yet
- Easy Way To Understand Stewart DR George Handbook 2015 PDFDocument48 pagesEasy Way To Understand Stewart DR George Handbook 2015 PDFAnonymous SMLzNANo ratings yet
- Pediatrics SLE MCQ From 2018-2014Document61 pagesPediatrics SLE MCQ From 2018-2014Asif Newaz67% (3)
- Sir David Cuthbertson Medal Lecture - Fluid, Electrolytes and Nutrition: Physiological and Clinical AspectsDocument15 pagesSir David Cuthbertson Medal Lecture - Fluid, Electrolytes and Nutrition: Physiological and Clinical AspectsThinh VinhNo ratings yet
- Fluid and Hyponatremia Management: by Craig B. Whitman, Pharm.D., BCPS, BCCCPDocument16 pagesFluid and Hyponatremia Management: by Craig B. Whitman, Pharm.D., BCPS, BCCCPAleksandar Dimovski100% (1)
- Hyperchloremia Is Associated With Complicated Course and Mortality in Pediatric Patients With Septic ShockDocument6 pagesHyperchloremia Is Associated With Complicated Course and Mortality in Pediatric Patients With Septic ShockKhairul AsriNo ratings yet
- Easy Way To Understand Stewart Acidbase George 2015 PDFDocument48 pagesEasy Way To Understand Stewart Acidbase George 2015 PDFGarry100% (2)
- Elderly Cholera Electrolyte Disturbances JASN 1995Document5 pagesElderly Cholera Electrolyte Disturbances JASN 1995PILARICA201263No ratings yet
- Electrolytes & FluidimbalancesDocument80 pagesElectrolytes & FluidimbalancesDennis Nyambane MomanyiNo ratings yet
- Hartmann's Solution and Ringer's Lactate - Targeting The Fourth Space (RLVSNS)Document2 pagesHartmann's Solution and Ringer's Lactate - Targeting The Fourth Space (RLVSNS)jmagn0070% (1)
- Patient Scenario, Chapter 45, Nursing Care of A Family When A Child Has A Gastrointestinal DisorderDocument93 pagesPatient Scenario, Chapter 45, Nursing Care of A Family When A Child Has A Gastrointestinal DisorderDay MedsNo ratings yet
- Test Bank For Medical Surgical Nursing 7th Edition Adrianne Dill LintonDocument10 pagesTest Bank For Medical Surgical Nursing 7th Edition Adrianne Dill LintonAlbertSmitheozmw100% (23)
- Intravenous Maintenance Fluid Therapy in The Pedia PDFDocument18 pagesIntravenous Maintenance Fluid Therapy in The Pedia PDFAdrianRuizNo ratings yet
- Hyperchloremia PDFDocument2 pagesHyperchloremia PDFChezer KiethNo ratings yet
- Plasma-Lyte 148 A Clinical ReviewDocument18 pagesPlasma-Lyte 148 A Clinical ReviewSofia NormanNo ratings yet
- Chloride The Queen of Electrolytes 2012Document9 pagesChloride The Queen of Electrolytes 2012Carlos PalominoNo ratings yet
- Fluids and Electrolytes in ElderlyDocument7 pagesFluids and Electrolytes in ElderlyDithaNo ratings yet
- Handout 9 Introduction To Fluids and ElectrolytesDocument22 pagesHandout 9 Introduction To Fluids and ElectrolytesGrape JuiceNo ratings yet
- Reading Synthesis # 2: San Roque Extension, Roxas City, Capiz, Philippines 5800Document15 pagesReading Synthesis # 2: San Roque Extension, Roxas City, Capiz, Philippines 5800Jay VillasotoNo ratings yet
- 3.1 Hypochloremia & HyperchloremiaDocument3 pages3.1 Hypochloremia & HyperchloremiaBooz Waief CaluzaNo ratings yet
- Electrolytes Part 2Document54 pagesElectrolytes Part 2Vincent ReyesNo ratings yet
- Anion Gap Negative Salicylates AJM 21Document5 pagesAnion Gap Negative Salicylates AJM 21anderson roberto oliveira de sousaNo ratings yet
- PUCAN, Julienne BSN III-D - SGD - HYPO&HYPERCHLOREMIADocument10 pagesPUCAN, Julienne BSN III-D - SGD - HYPO&HYPERCHLOREMIAJulienne PucanNo ratings yet
- Huet Et Al-2023-Critical Care1675545774850Document9 pagesHuet Et Al-2023-Critical Care1675545774850Taís FigueiredoNo ratings yet
- Table of Commonly Used IV SolutionsDocument2 pagesTable of Commonly Used IV Solutionslynch4614No ratings yet