Professional Documents
Culture Documents
Obstructive Jaundice
Uploaded by
Fenny Noor AidaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Obstructive Jaundice
Uploaded by
Fenny Noor AidaCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/343617705
Obstructive Jaundice: Understanding the pathophysiology
Article in International Journal of Surgery and Medicine · August 2020
DOI: 10.5455/ijsm.2020-07-061-jaundice
CITATION READS
1 6,606
1 author:
Ketan Vagholkar
Padmashree Dr. D.Y. Patil University
213 PUBLICATIONS 256 CITATIONS
SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Hydatid cysts of liver View project
All content following this page was uploaded by Ketan Vagholkar on 16 August 2020.
The user has requested enhancement of the downloaded file.
SURGERY | REVIEW ARTICLE
OBSTRUCTIVE JAUNDICE: UNDERSTANDING THE
PATHOPHYSIOLOGY
Ketan Vagholkar∗,1
∗ Department of Surgery, D.Y.Patil University school of Medicine, Navi Mumbai-400706. MS. India.
ABSTRACT Jaundice is one of the most prevalent symptom in hepatobiliary disorders. The nature of jaundice may vary
from hepatocellular to obstructive pattern. In a few cases, it may be haemolytic in nature. Identifying and ascertaining
the type is pivotal for further investigation. A combination of haematological and radiological investigations will not
only provide information on the severity and the impact of obstructive jaundice on various organ systems of the body
but also help in determining the prognosis. Endoscopy can also provide diagnostic as well as a therapeutic benefit in
obstructive jaundice. The pathophysiology, clinical evaluation and investigations in a case of obstructive jaundice is
discussed in this paper.
KEYWORDS Jaundice, obstructive, causes, complications, investigations
of Luschka are small biliary ducts that lie in the gall bladder
fossa and connect the liver and gall bladder directly. The normal
Introduction thickness of the gall bladder wall is less than 4 mm. Therefore
obstruction can occur at any level. It may be intraluminal or
Obstructive jaundice is one of the most challenging types of jaun- due to extrinsic compression. Backpressure leads to dilatation
dice. It can be treated successfully once the cause is ascertained. of the passages. Identifying the level and cause for obstruction
Understanding the basic physiology of bilirubin metabolism and is, therefore, the main aim of clinical evaluation and imaging.
the structure of the extrahepatic biliary passages is essential for
the adequate diagnostic evaluation of a patient presenting with
obstructive jaundice. [1] Physiology of bilirubin metabolism
Bilirubin is of two types, direct which is water soluble and indi-
Surgical anatomy of the extrahepatic biliary passages rect, which is water insoluble. Identifying the rise of each type
is essential in the evaluation of the type of jaundice. Hence it is
The intrahepatic ducts converge to form the right and left hepatic essential to review the normal process of bilirubin formation and
ducts which exit from the liver and join to form the common hep- clearance from the gastrointestinal tract. Fragile and senescent
atic duct. The cystic duct emerges from the gall bladder and joins RBC’s are broken down in the spleen. When the RBC membrane
the common hepatic duct which then descends as the common ruptures, haemoglobin is released. The macrophages of the retic-
bile duct. The common bile duct has four parts, supraduodenal, uloendothelial system phagocytose this. Haemoglobin is further
retroduodenal, intrapancreatic and intraduodenal. The common broken down into heme and globin. The heme component is
bile duct is joined by the main pancreatic duct to open into the then further broken into free iron which combines with ferritin
ampulla of Vater situated in the second part of the duodenum. and the straight remnant chain of four pyrrole nuclei that serves
The diameter of the normal CBD is less than 8mm, and the di- as a substrate for the formation of bile pigments.
ameter of the main pancreatic duct is less than 4 mm. The ducts Biliverdin is formed which then gets converted into bilirubin.
Copyright © 2020 by the Bulgarian Association of Young Surgeons Bilirubin is released into the plasma. In the plasma, it is bound
DOI:10.5455/ijsm.2020-07-061-jaundice to albumin and transported to the liver. There it gets absorbed
First Received: July 11, 2020 across the hepatic cell membrane. During this process, it is
Accepted: July 23, 2020 released from the albumin but remains attached to two proteins
Associate Editor: Ivan Inkov (BG);
1
Annapurna Niwas, 229 Ghantali Road. Thane 400602. MS. India; E mail:
Y and Z proteins inside the hepatocytes. Soon the bilirubin
kvagholkar@yahoo.com; Mobile: 9821341290 is detached from these proteins and is conjugated. The end
Ketan Vagholkar / International Journal of Surgery and Medicine (2020) 6(4):26-31
products are bilirubin glucuronide (80%), bilirubin sulphate This includes sump syndrome seen in a side to side choledo-
(10%), and other substances (10%). An active transport process choduodenostomy in which food, stones or debris accumulate
then excretes bilirubin glucuronide into the bile canaliculi. in the CBD and obstruct the normal biliary outflow. The other
A small quantity of conjugated bilirubin enters the plasma. such cause is seen in Roux-en Y limb wherein stasis may cause
Through the extrahepatic biliary passages, it inters into the in- biliary obstruction after biliary enteric anastomosis. [8]
testine. Conjugated bilirubin is acted upon by the bacteria con-
verting it into urobilinogen. Urobilinogen undergoes oxidation Effects of biliary obstruction:
to stercobilinogen which is excreted into the stools as stercobilin.
Stercobilin imparts the yellowish colour to normal stools. A Complications of cholestasis are proportional to the duration
part of urobilinogen is absorbed and passes to the kidneys from and intensity of jaundice. Jaundice has a negative impact on
where it is excreted into the urine as urobilin which imparts a various organ systems of the body.
yellowish colour to normal urine.
Intestines:
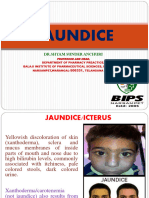
Pathophysiology of Jaundice Bile and bile acids have essential functions in maintaining the
Jaundice is best described as yellowish discolouration of the normal integrity and function of the intestines. Bile and bile
sclera. Obstructive jaundice results from obstruction to the acids contribute significantly to the normal gut barrier function.
free flow of bile from the liver to the gall bladder and then It has positive effects on the intestinal immune function. In
to the small intestine. Jaundice or raised total bilirubin may be experimental studies, it affects homing and distribution of T
due to an increase in either conjugated or unconjugated compo- lymphocytes in the gut-associated lymphatic tissue. Absence
nent. This depends upon the level at which the normal bilirubin of bile acids in the gut causes a fall in the CD4+ and CD8+
metabolism is altered. This can happen at three levels Pre hep- lymphocytes. It exerts a trophic effect on the intestinal mucosa
atic wherein there is increased production of bilirubin which by increasing the villous density and inducing hypertrophy of
exceeds the capability of the liver to conjugate the bilirubin and various components of the intestinal wall. Bile acids inhibit
excrete it into the gut. There is a predominant increase in the the growth of certain bacteria such as Bacteroides, clostridia,
unconjugated bilirubin. The most frequent prehepatic cause is lactobacillus and streptococci. [9]
haemolytic anaemia, where there is an excessive breakdown of Absence of bile in the intestine has a series of deleterious
heme. [2] effects leading to septicaemia. Absence of bile salts leads to
Intrahepatic cause for hyperbilirubinaemia is usually due disturbance of intestinal bacterial balance with overgrowth of
to parenchymal liver disease, thereby causing an inability to gram-negative bacteria. There is an alteration of intestinal tight
either conjugate or excrete bilirubin. This may initially cause a junction expression and increased intestinal apoptosis, causing
transient increase in the conjugated component, followed by the significant alterations in the intestinal oxidative state, thereby
indirect component. This is seen in viral hepatitis, drug-induced exacerbating the gut injury. There is increased intestinal perme-
and primary biliary cirrhosis. [3] ability causing bacterial and endotoxin translocation leading to
Post hepatic causes lead to an impediment to the flow of bile, septic and renal complications. Absence of bile causes suppres-
which may be either due to partial or complete obstruction of the sion of clearing capacity of Kupffer cells, the main hepatocyte
extrahepatic biliary passages between the liver and duodenum. macrophage population due to accumulation of bile acids in
There is predominantly conjugated hyperbilirubinaemia. This is the liver thereby permitting spillover of endotoxins from the
a characteristic feature of obstructive jaundice. [3] portal circulation into the systemic circulation with the release
of pro-inflammatory cytokines. These lead to the development
Aetiology of biliary obstruction of “gut-derived sepsis”. [10, 11, 12]
Biliary obstruction may either be intrahepatic or extrahepatic in
Coagulation system:
origin. [4] Intrahepatic cholestasis could be at the level of the
hepatocyte or the canalicular bile membrane. The causes include The liver has a significant synthetic role to play in the coagu-
hepatitis (hepatitis A, B & C) leading to inflammation of the lation system. It synthesizes fibrinogen, prothrombin, factors
liver with necrosis, cirrhosis (primary biliary cirrhosis) leading II, VII, IX and X. The production of these factors is dependent
to nodular regeneration and scarring, drug-induced (anabolic on vitamin K, which is a fat-soluble vitamin requiring bile in
steroids, chlorpromazine) and space-occupying lesions of the the intestine for absorption. Due to the absence of bile in the
liver such as cysts, abscesses and tumours. [5] intestine, this vitamin cannot be absorbed, leading to deficiency.
Extrahepatic causes can further be classified as intraductal, Hence glycosylation of lysyl residues cannot take place in the
which include choledocholithiasis, neoplasms (cholangiocarci- liver, thereby leading to deficiency of factors II, VII, IX and X.
nomas), biliary strictures and parasitic infestations (ascariasis, This causes disturbances in the extrinsic pathway of coagulation.
liver flukes). [6] For better understanding extrahepatic causes of The liver also manufactures natural anticoagulants such as an-
obstructive jaundice can be classified into four types (Table 1) tithrombin III, protein C, protein S and heparin cofactor II. With
Extra ductal causes include neoplasms, pancreatitis, pseu- respect to the fibrinolytic system, it produces plasminogen and
docysts of pancreas and portal hilar lymphadenopathy. Tu- alpha two anti-plasmin. Therefore alteration in liver function
mours causing extra ductal compression deserve special men- can lead to serious coagulation defects. If septic and pancreatic
tion. These include pancreatic head tumours, cholangiocarci- complications develop then a prothrombotic state may develop
noma, ampullary carcinomas, gall bladder carcinomas extending initially. Mucinous adenocarcinomas of the pancreas and hepa-
up to the CBD and metastatic lymphadenopathy. [7] Choledo- tocellular carcinomas can induce activation of the haemostatic
cholithiasis, biliary strictures and malignant tumours are the system. Thromboembolic events usually follow. Unresolved
most important and common causes of obstructive jaundice. Un- cholestasis leads to a generalized alteration in the haemostatic
common postoperative causes need to be considered as well. system. The effects are thrombocytopenia, decreased synthesis
Ketan Vagholkar / International Journal of Surgery and Medicine (2020) 6(4):26-31
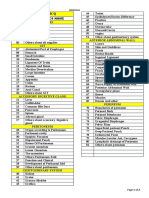
Table 1 Classification of obstructive jaundice (Benjamin).
Type I : Complete obstruction
Tumours of the head of pancreas
Ligation of the CBD
Cholangiocarcinoma
Parenchymal liver disease
Type II: Intermittent obstruction
Choledocholithiasis
Cholodochal cyst
Duodenal diverticulum
Intrabiliary parasites
Haemobilia
Type III : Chronic incomplete obstruction
Strictures of the CBD
Stenosed biliary enteric anastomosis
Chronic pancreatitis
Stenosis of the sphincter of Oddi
Type IV: Segmental obstruction
Traumatic
Sclerosing cholangitis
Intrahepatic stones
Cholangiocarcinoma
Table 2 Types of jaundice.
Hepatocellular
Parameter Pre-hepatic Obstructive
(hepatic)
Haemolysis leading to excess Deficient uptake, conjugation or Deficient excretion due to
Mechanism of raised bilirubin
production excretion by hepatocytes obstruction in the biliary tract
Unconjugated+ Predominantly conjugated
Type of serum bilirubin affected Mainly unconjugated
conjugated (>50%)
Urine bilirubin absent present present
Urine urobilinogen increased variable absent
Abnormal that is not correctable Abnormal that is corrected with
Prothrombin time normal
by vitamin k vitamin k
Features of haemolysis on blood
smear Marked increase in ALT Marked increase in ALP > 3
Additional features
(reticulocytosis, low and AST times the normal upper limit
haptoglobin, low Hb)
Prototypes Haemolytic anaemia Viral hepatitis Common bile duct stones
Table 3 Prognostic factors (Pitt’s score)
Parameters (one point per factor)
Type of obstruction (benign or malignant)
Age >60 years
Serum albumin < 3gm/dl
Serum bilirubin > 10 mg%
Serum Alkaline phosphatase > 100 IU
Serum creatinine > 1.3 mg%
TLC > 10000/mm3
Haematocrit < 30%
Ketan Vagholkar / International Journal of Surgery and Medicine (2020) 6(4):26-31
Interpretation of scores
Factors Mortality
Up to 2 0%
3 4%
4 7%
5 44%
6 67%
8 100%
and clearance of coagulation factors and inhibitors, dysfibrino- Clinical evaluation:
genemia, hyperfibrinolysis, over DIC, portal vein stasis and
Jaundice is the main presenting symptom. The main aims of
thrombosis. [13, 14]
clinical evaluation are:
1. Determining the obstructive nature of jaundice.
Renal system
Jaundice alone independent of the parenchymal liver disease 2. Identifying the cause for obstructive jaundice.
affects the integrity of the cardiovascular system. [15] The effects
3. Whether the aetiology is benign or malignant in nature.
are
4. If malignant then whether the disease is metastatic in na-
1. Reduction in peripheral vascular resistance resulting in
ture.
systemic hypotension.
5. Impact of jaundice on other organ systems.
2. Depression of myocardial function.
6. The need for multiorgan system support.
3. Profound natriuresis and diuresis, leading to volume deple-
tion. 7. Postulate an investigation algorithm based on the clinical
findings.
In experimental models, renal complications are attributed to
pre-renal factors. Various factors related to liver parenchymal
damage associated with obstructive jaundice may have an inde- Jaundice can be haemolytic, hepatocellular or obstructive in
pendent contribution to the pathogenesis of arterial underfilling, nature. (Table 2) The onset duration and progress of the jaun-
which predisposes to pre-renal failure and acute tubular necro- dice is important. Rapidly developing jaundice associated with
sis. Peripheral and renal haemodynamic effects of obstructive symptoms of pruritus, the passage of clay coloured stools and
jaundice are more marked than medical jaundice. High level of high coloured urine is seen in the obstructive pattern of jaundice.
bile acids in the circulation seen in obstructive jaundice has a Significant nausea, vomiting and loose motions are suggestive
direct cardio depressant and hypovolemic effect. In addition to of medical aetiology. History of alcoholism, intravenous drug
the direct effects of bile acids on circulation, a higher concentra- abuse and multiple tattoos over the body go in favour of medi-
tion of circulating endotoxins has deleterious effects on both the cal causes of jaundice. Persistent anaemia with mild abdominal
peripheral and renal microcirculation. symptoms is suggestive of the haemolytic pattern. History of
drug ingestion followed by jaundice is seen in the hepatocel-
lular type of jaundice. Multiple blood transfusions predispose
Liver: hepatitis B and cirrhosis. [17]
High-grade biliary obstruction leads to increased intraductal Pain as an associated symptom is important in identifying
pressure. There is bacterial overgrowth leading to cholangitis the cause of obstructive jaundice. Jaundice associated with pain
which eventually culminates to septic shock. Severe functional and fever suggestive of cholangitis is seen in bile duct stones.
derangements of the hepatic function lead to alteration of liver Jaundice typically shows waxing and waning. Intermittent at-
regeneration. High-grade obstructive jaundice causes cell dam- tacks of right upper abdominal pain accompanied by vomiting
age. Bile acids cause liver cell apoptosis by directly activating is seen in cholecystitis. Severe pain and associated symptoms
death receptors inducing oxidative damage and mitochondrial suggestive of pancreatitis can also cause transient obstructive
dysfunction, which as a combination strongly sensitizes to apop- jaundice. Painless progressive jaundice related to weight loss is
tosis. The net result of gross hepatic dysfunction is endotox- highly suspicious of malignant aetiology. The previous history
aemia. Long-standing biliary obstruction leads to secondary of biliary surgery presenting as jaundice is suggestive of a biliary
biliary cirrhosis. [16] stricture. History of inflammatory bowel disease presenting as
jaundice is suggestive of primary sclerosing cholangitis. [18]
Weight loss, bone pains, and abdominal distension due to
CNS:
ascites are suggestive of malignant aetiology. History of abdom-
Long-standing jaundice leads to the formation of pseudo trans- inal masses is highly suggestive of malignancy.
mitters which predispose to precoma and finally into a hepatic Long-standing jaundice can affect other organ systems. Neu-
coma. rological symptoms are suggestive of impending coma. Renal
Ketan Vagholkar / International Journal of Surgery and Medicine (2020) 6(4):26-31
dysfunction is a common accompaniment in severe jaundice. Co- 2. Level of obstruction and degree of back pressure changes.
agulopathies are seen in advanced stages. Generalized oedema
due to hypoproteinaemia is a bad prognostic sign. 3. Status of the liver and abdominal metastases in suspected
Physical examination reveals deepening of scleral icterus. Vi- malignant obstruction.
tal parameters may be altered if the patient presents late. Fever
is an important feature. Pain, fever and jaundice is Charcot’s 4. Splenic enlargement.
triad seen in cholangitis. In addition to these, if there is hypoten-
sion and mental obtundation, then that constitutes Reynold’s 5. Ascites.
pentad. Reynold’s pentad is seen in suppurative cholangitis.
Scratch marks of pruritus are commonly visible in obstructive Endoscopic ultrasound further helps in the assessment of
jaundice. Signs of hepatocellular failure are seen in advanced malignant obstruction. [20] Advantages are:
cases. Flapping tremors and mental obtundation are red flags of
poor prognosis. Fullness due to a mass in the left supraclavicular 1. Helps in evaluating the distal CBD.
region is suggestive of an inoperable malignancy.
The abdominal examination needs to be done meticulously. 2. It is accurately diagnosing CBD calculi including small cal-
Tenderness in the right hypochondrium suggests cholecystitis. A culi in a nondilated system which are missed on routine
palpable gall bladder in a jaundiced patient is highly suggestive ultrasonography.
of malignant obstruction. (Courvoisier law) Hepatomegaly may
be due to hepatitis or due to chronic cholestasis. Metastases 3. Small resectable pancreatic masses can also be identified.
in the liver can also cause hepatomegaly. A mass in continuity
with the liver can be due to an advanced gall bladder tumour. Magnetic resonance cholangiopancreatography (MRCP) is a
Free fluid in the abdomen due to ascites is a sign of advanced non-invasive investigation for evaluation of the biliary tract. It
malignant disease. has a sensitivity of 95% and a specificity of 95% as well. It helps
in diagnosing the cause and level of biliary obstruction.
Contrast-enhanced computed tomography (CECT) is the in-
Investigations: vestigation of choice for staging the disease in cases of malignant
Investigations are aimed at obstruction. [21] CECT reveals the following:
1. Determining the severity of illness 1. Site of obstruction
2. Urgency of intervention 2. Nature of obstruction, whether benign or malignant.
3. Level of care required 3. Extent or severity of backpressure changes
4. Echotexture of the liver.
Haematological investigations are very critical in the evalua-
tion of obstructive jaundice. A complete blood count will reveal
5. Presence of metastases
anaemia in malignant cases. Leucocytosis is seen in cholangitis.
Total bilirubin will be raised. There will be a predominant
increase in the direct reading component. Alkaline phosphatase 6. Ascites.
is a membrane-bound enzyme located in the bile canalicular
pole of the hepatocyte. A value of three times the upper limit 7. Vascular encasement in cases of pancreatic head cancers.
of normal value is seen in the obstructive pattern of jaundice.
It is elevated in almost all patients of biliary obstruction except
Endoscopic retrograde cholangiopancreatography (ERCP) is
for incomplete or intermittent obstruction. Gamma-glutamyl
the investigation of choice once a preliminary imaging assess-
transpeptidase is raised in bile duct obstruction. Its level paral-
ment has been done. ERCP can be both diagnostic and ther-
lels the level of alkaline phosphatase in patients with cholesta-
apeutic. The diagnostic role is to collect tissue for biopsy in
sis.
periampullary growths or brush cytology samples. The exact
Serum transaminases (ALT, AST) are mildly elevated in
level of the block and the severity of backpressure changes can
cholestasis while markedly elevated in cholangitis. PT/INR
also be ascertained. Therapeutic intervention is ideal for stones
is prolonged due to malabsorption of vitamin K. It is corrected
in the CBD, which saves unnecessary surgical exploration of the
by parenteral administration of vitamin K. If PT/INR improves
CBD. Preoperative stenting to relieve jaundice is of great help
with vitamin K injections, then it is more in favour of obstructive
in preparing the patient for surgery. In inoperable cases, pallia-
pattern while no improvement is seen in the liver parenchymal
tive stenting is useful to reduce the complications of jaundice.
disease.
However, one needs to be careful of the complications of the
Renal function is best assessed and monitored by evaluation
procedure, which include pancreatitis, perforation, haemorrhage
of serum creatinine, blood urea nitrogen and electrolytes.
and sepsis by causing cholangitis. [22]
Viral markers for hepatitis B and C should be done in all cases
Percutaneous transhepatic cholangiography (PTC) is an alter-
of obstructive jaundice.
native if ERCP fails as in hilar obstructions. It enables drainage
Ultrasound is a preliminary investigation. It enables docu-
of accumulated bile proximal to the obstruction. [23]
mentation of the presence, extent and level of obstruction. [19]
It helps in Prognosis in obstructive jaundice can be evaluated based on
haematological and radiological findings. [24] Pitt’s score can be
1. It is identifying the cause of obstruction. evaluated. Higher the score worst in the prognosis. (Table 3)
Ketan Vagholkar / International Journal of Surgery and Medicine (2020) 6(4):26-31
Conclusion 10. Bhargava SK, Usha T, Bhatt Sh, Kumari R, Bhargava S. Imag-
ing in obstructive jaundice: a review with our experience.
Understanding the pathophysiology of obstructive jaundice is
JIMSA. 2013.
essential for proper evaluation in order to prevent a delay in
the diagnosis: a careful history and physical examination help 11. Sano T, Ajiki T, Takeyama Y, Kuroda Y. Internal biliary
in ascertaining the obstructive aetiology of jaundice. Various drainage improves decreased number of gut mucosal T
imaging modalities help in confirming the benign or malignant lymphocyte and MAdCAM-1 expression in jaundiced rats.
nature of the obstruction. ERCP has an added advantage of Surgery. 2004; 136: 693-699.
therapeutic intervention especially in choledocholithiasis. Once
this road map is available the surgeon can formulate a surgical 12. Assimakopoulos SF, Scopa CD, Vagianos CE. Pathophysil-
plan for the patient. ogy of increased intestinal permeability in obstructive jaun-
dice. World J Gastroenterol. 2007; 13: 6458-6464.
Acknowledgements
13. Parks RW, Stuart Cameron CH, Gannon CD, Pope C, Dia-
I would like to thank Parth Vagholkar for his help in typesetting mond T, Rowlands BJ. Changes in gastrointestinal morphol-
the manuscript. ogy associated with obstructive jaundice. J Pathol. 2000;
192: 526-532.
Conflict of interest
14. Assimakopoulos SF, Scopa CD, Zervoudakis G, Mylonas
None. PG, Georgiou C, Nikolopoulou VN. Bombesin and neu-
rotensin reduce endotoxemia, intestinakl oxidative stress,
Funding and apoptosis in experimentale obstructive jaundice. Ann
Nil Surg. 2005; 241: 159-167.
15. Assimakopoulos SF, Thomopoulos KC, Patsoukis N, Geor-
References giou C, Scopa CD, Nikolopoulou VN, et al. Evidence for
1. Khurram M, Durrani AA, Hasan Z, Butt Au, Ashfaq S. En- intestinal oxidative stress in patients with obstructive jaun-
doscopic retrograde cholangiopancreatographic evaluation dice. Eur J Clin Invest. 2006; 36:181-187.
of patients with obstructive jaundice. J Coll Physicians Surg
Pak. 2003; 13: 325-328. 16. Parks RW, Clements WD, Smye MG, Pope C, Rowlands
BJ, Diamond T. Intestinal barrier dysfunction in clinical
2. Ho CY, Chen TS, Chang Fy, Lee SD. Benign nontraumatic and experimental obstructive jaundice and its reversal by
inflammatory stricture of mid portion of common bile duct internal biliary drainage. Br J Surg. 1996; 83: 1345-1349.
mimicking malignant tumor: Reports of two cases. World J
Gastroenterol. 2004; 10: 2153-2155. 17. Papadopoulos V, Filippou D, Manolis E, Mimidis K.
Haemostasis impairment in patients with obstructive jaun-
3. Moghimi M, Marashi SA, Salehian MT, Sheikhvatan M. Ob- dice. J Gastrointestin Liver Dis. 2007; 16: 177-186.
structive jaundice in Iran: factors affecting early outcome.
Hepatobiliary Pancreat Dis Int. 2008; 7: 515-519. 18. Green J, Better OS. Systemic hypotension and renal fail-
ure in obstructive jaundice- mechanistic and therapeutic
4. Lapis JL, Orlando RC, Mittelstaedt CA, Staab EV. Ultra- aspects. J Am Soc Nephrol. 1995; 5: 1853-1871.
sonography in the diagnosis of obstructive jaundice. Am
Intern Med. 1978; 89: 61-63. 19. Lu Y, Zhang BY, Zhao C, Jin X. Effect of obstructive jaundice
on hemodynamics in the liver and its significance. Hepato-
5. Kumar M, Prashad R, Kumar A, Sharma R, Acharya SK, biliary Pancreat Dis Int. 2009; 8: 494-497.
Chattopadhyay TK. Relative merits of ultrasonography,
computed tomography and cholangiography in patients 20. Yang YJ, Shi JS, Xie SM, Zhang DT, Cui BS. Effects of differ-
of surgical obstructive jaundice. Hepatogastroenterology. ent drainage procedures on levels of serum endotoxin and
1998; 45: 2027-2032. tumor necrosis factor in patients with malignant obstructive
jaundice. Hepatobiliary Pancreat Dis Int. 2003; 2: 426-430.
6. Thornton JR, Loba AJ, Lintott DJ, Axon AT. Value of ultra-
sound and liver function tests in determining the need for 21. Lee JG. Diagnosis and management of acute cholangitis.
endoscopic retrograde cholangiopancreatography in unex- Nat Rev Gastroenterol Hepatol. 2009; 6: 533-541.
plained abdominal pain. Gut. 1992; 33: 1559-1561.
22. Deitch EA, Sitting K, Li M, Berg R, Specian RD. Obstructive
7. Fleischmann D, Ringl H, Schoft R, Pötzi R, Kontrus M, Henk jaundice promotes bacterial translocation from the gut. Am
C, et al. Three dimensional spiral CT cholangiography in J Surg. 1990; 159: 79-84.
patients with suspected obstructive biliary disease: compar-
ison with endoscopic retrograde cholangiopancreatography. 23. Shi Y. Mechanisms of caspase activation and inhibition dur-
Radiology. 1996; 198: 861-868. ing apoptosis. Mol Cell. 2002; 9: 459-470.
8. Heiken JR, Brink JA, Vannier MW. Spiral (helical) CT. Radi- 24. Grandic L, Perko Z, Banovic J,Pogorelic Z, Ilic N, Jukic I, et
ology. 1993; 189: 647-656. al. Our experience in the treatment of obstructive jaundice.
Acta Clin Croat. 2007; 46: 157-160.
9. Guibaud I, Bret PM, Reinhold C, Atri M, Barkun AN. Bile
duct obstruction and choledocholithiasis: diagnosis with
MR cholangiography. Radiology. 1995; 197: 109-115.
Ketan Vagholkar / International Journal of Surgery and Medicine (2020) 6(4):26-31
View publication stats
You might also like
- Gastrointestinal SystemDocument218 pagesGastrointestinal Systemnursereview92% (12)
- Cholelithiasis Case 1Document21 pagesCholelithiasis Case 1Arvin F. LansangNo ratings yet
- Case Study CholecystitisDocument27 pagesCase Study Cholecystitisyhanne98% (225)
- Protein Digestion and AbsorptionDocument7 pagesProtein Digestion and AbsorptionSIJINo ratings yet
- Hepatic Fibrosis, (Liver Cirrhosis) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHepatic Fibrosis, (Liver Cirrhosis) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- GERDDocument32 pagesGERDlumina.sNo ratings yet
- Ebook Sleisenger and Fordtrans Gastrointestinal and Liver Disease PDF Full Chapter PDFDocument67 pagesEbook Sleisenger and Fordtrans Gastrointestinal and Liver Disease PDF Full Chapter PDFronald.hartford579100% (25)
- Obstructive JaundiceDocument18 pagesObstructive JaundiceBellinda PaterasariNo ratings yet
- Case Study - BronchopneumoniaDocument108 pagesCase Study - BronchopneumoniaAnthony WallNo ratings yet
- Hematuria, (Blood in Urine) A Simple Guide to The Condition, Related Diseases And Use in Diagnosis of DiseasesFrom EverandHematuria, (Blood in Urine) A Simple Guide to The Condition, Related Diseases And Use in Diagnosis of DiseasesRating: 5 out of 5 stars5/5 (2)
- Anal Rectal MalformationsDocument64 pagesAnal Rectal Malformationsdevtario100% (1)
- Obstructive JaundiceDocument7 pagesObstructive JaundiceNatalindah Jokiem Woecandra T. D.No ratings yet
- Obstructive Jaundice BMJlearningmoduleDocument26 pagesObstructive Jaundice BMJlearningmodulesamudraandiNo ratings yet
- Oj 2 PDFDocument6 pagesOj 2 PDFAnisah Maryam DianahNo ratings yet
- Biliary Atresia 2024Document11 pagesBiliary Atresia 2024Dayana FajardoNo ratings yet
- Biliary Obstruction - 2022Document13 pagesBiliary Obstruction - 2022Ana Itzel Carlon ChavezNo ratings yet
- Dissertation ON A Clinical Study On Obstructive JaundiceDocument66 pagesDissertation ON A Clinical Study On Obstructive JaundicePravat SatpathyNo ratings yet
- PBL Icterus 3Document23 pagesPBL Icterus 3MelanSeptianyNo ratings yet
- 5 и 6 Lectures Gall Stone Disease, Acute Cholecystitis, Obstuctive Jaundice, Postcholecystectomy Syndrome 2019-1Document115 pages5 и 6 Lectures Gall Stone Disease, Acute Cholecystitis, Obstuctive Jaundice, Postcholecystectomy Syndrome 2019-1HashmithaNo ratings yet
- Peadiatrics 3Document27 pagesPeadiatrics 3skNo ratings yet
- 33 34 IV 12 Atresia BiliarisDocument13 pages33 34 IV 12 Atresia BiliarisTasia AmeliaNo ratings yet
- Pathology of The Liver: Systems Pathology II-PA5402 Dr. Khan T-W-RDocument78 pagesPathology of The Liver: Systems Pathology II-PA5402 Dr. Khan T-W-RCrystal Lynn Keener SciariniNo ratings yet
- Bile Peritonitis 2021Document6 pagesBile Peritonitis 2021Brvo CruzNo ratings yet
- Razeen - Surgery Research GALLSTONE DISEASEDocument23 pagesRazeen - Surgery Research GALLSTONE DISEASERazeen RiyasatNo ratings yet
- Clase 3 HepatogramaDocument9 pagesClase 3 HepatogramajuanpbagurNo ratings yet
- Liver Function - Assignment 1Document7 pagesLiver Function - Assignment 1Michelle Mae JulianaNo ratings yet
- Surgical JaundiceDocument15 pagesSurgical Jaundicedrrohit1756No ratings yet
- GallstonesDocument6 pagesGallstonesricky aditNo ratings yet
- Jaundice Revisited: Recent Advances in The Diagnosis and Treatment of Inherited Cholestatic Liver DiseasesDocument13 pagesJaundice Revisited: Recent Advances in The Diagnosis and Treatment of Inherited Cholestatic Liver Diseasesmiss betawiNo ratings yet
- Cholelithiasis: A Brief Review On Diagnostic Approach and Management in Clinical PracticeDocument6 pagesCholelithiasis: A Brief Review On Diagnostic Approach and Management in Clinical PracticeWarda SariNo ratings yet
- Kidney Disease Presentation, Princess ChiomaDocument14 pagesKidney Disease Presentation, Princess ChiomaNwigwe Promise ChukwuebukaNo ratings yet
- Surgery JournalDocument23 pagesSurgery JournalRazeen RiyasatNo ratings yet
- Incidentally Exploration of The Fusiform Cystic Duct 2024 International JourDocument4 pagesIncidentally Exploration of The Fusiform Cystic Duct 2024 International JourRonald QuezadaNo ratings yet
- A Liver Manifestation Hepatic CirrhosisDocument11 pagesA Liver Manifestation Hepatic CirrhosisAjit SinghNo ratings yet
- HepatolithiasisDocument5 pagesHepatolithiasisAndrean HeryantoNo ratings yet
- Sas S8Document10 pagesSas S8Ralph Louie ManagoNo ratings yet
- CholedocholithiasisDocument3 pagesCholedocholithiasisPao AcelajadoNo ratings yet
- Pruebas de Función RenalDocument10 pagesPruebas de Función RenalTito AboNo ratings yet
- At Two: Was SeDocument3 pagesAt Two: Was Seida ayu agung WijayantiNo ratings yet
- Jaundice - StatPearls - NCBI BookshelfDocument11 pagesJaundice - StatPearls - NCBI BookshelfCONSTANTIUS AUGUSTONo ratings yet
- Nursing Care WithDocument14 pagesNursing Care WithSafitriNo ratings yet
- Jiaats Site Admin,+762 Article+Text 1305 1 2 20190704Document5 pagesJiaats Site Admin,+762 Article+Text 1305 1 2 20190704Dr. Kazy Habibur RahmanNo ratings yet
- Biliary SystemDocument15 pagesBiliary SystemDjabhi SpinzzNo ratings yet
- Peadiatrics Assignment - Mr. KangwaDocument11 pagesPeadiatrics Assignment - Mr. KangwaTahpehs PhiriNo ratings yet
- Jaundice Therapy 3Document24 pagesJaundice Therapy 3sn4s7nyxcbNo ratings yet
- hpb0011 0194Document9 pageshpb0011 0194ocramusNo ratings yet
- Gallbladder 101Document69 pagesGallbladder 101Gerry OshNo ratings yet
- Independent Research Assignment - GallstonesDocument3 pagesIndependent Research Assignment - Gallstonesjena DorringtonNo ratings yet
- Nihms-789481 The Molecular Pathogenesis of Cholestasis in SepsisDocument15 pagesNihms-789481 The Molecular Pathogenesis of Cholestasis in SepsisAlexis CarrelNo ratings yet
- Diagnosis and Management of Klatskin Tumor: April 2010Document6 pagesDiagnosis and Management of Klatskin Tumor: April 2010Feby Kurnia PutriNo ratings yet
- Biliary AtresiaDocument39 pagesBiliary AtresiaRamesh ReddyNo ratings yet
- Liver ThesisDocument8 pagesLiver Thesissusanandersonannarbor100% (2)
- Pathology of Liver SamDocument28 pagesPathology of Liver SamJaks RipperNo ratings yet
- Ladja, Irish V. BSN 3-C Laboratory ResultsDocument13 pagesLadja, Irish V. BSN 3-C Laboratory ResultsEzra LambarteNo ratings yet
- Bile Duct DilatedDocument4 pagesBile Duct DilatedAmit GauravNo ratings yet
- Disorders of The PancreasDocument77 pagesDisorders of The PancreasGeofry OdhiamboNo ratings yet
- BiliaryDocument41 pagesBiliaryayundyawibowoNo ratings yet
- I&IDocument7 pagesI&IJdee XNo ratings yet
- Biliary Atresia Pathology Etiology and PathogenesiDocument17 pagesBiliary Atresia Pathology Etiology and Pathogenesijohn lemonNo ratings yet
- Obstructive Jaundice Group 6Document33 pagesObstructive Jaundice Group 6Qurbon AliNo ratings yet
- Cholestasis Definisi: Penghentian Atau Supresi Aliran Empedu, Dengan Penyebab Intrahepatik Atau Ekstrahepatik EtiologiDocument18 pagesCholestasis Definisi: Penghentian Atau Supresi Aliran Empedu, Dengan Penyebab Intrahepatik Atau Ekstrahepatik EtiologiElsya ParamitasariNo ratings yet
- Liver Disorders in Childhood: Postgraduate Paediatrics SeriesFrom EverandLiver Disorders in Childhood: Postgraduate Paediatrics SeriesNo ratings yet
- Post-cholecystectomy Bile Duct InjuryFrom EverandPost-cholecystectomy Bile Duct InjuryVinay K. KapoorNo ratings yet
- The Evolving Landscape of Liver Cirrhosis ManagementFrom EverandThe Evolving Landscape of Liver Cirrhosis ManagementHitoshi YoshijiNo ratings yet
- Obstructive JaundiceDocument7 pagesObstructive JaundiceFenny Noor AidaNo ratings yet
- A Comprehensive Review of Central Post Stroke PainDocument15 pagesA Comprehensive Review of Central Post Stroke PainFenny Noor AidaNo ratings yet
- A Narrative Review of Persistent Post-Stroke Headache - ADocument12 pagesA Narrative Review of Persistent Post-Stroke Headache - AFenny Noor AidaNo ratings yet
- The Triple Elimination of Mother-to-Child Transmission of HIV, Hepatitis B and Syphilis in Asia and The Pacific, 2018-2030Document44 pagesThe Triple Elimination of Mother-to-Child Transmission of HIV, Hepatitis B and Syphilis in Asia and The Pacific, 2018-2030Sekar MentariNo ratings yet
- Intermediate UveitisDocument7 pagesIntermediate UveitisFenny Noor AidaNo ratings yet
- Vertebral Artery Dissection Presenting As Isolated Vertigo: N J Rane, D McauleyDocument1 pageVertebral Artery Dissection Presenting As Isolated Vertigo: N J Rane, D McauleyFenny Noor AidaNo ratings yet
- Management of Hepatitis B Virus Infection Updated Swedish GuidelinesDocument27 pagesManagement of Hepatitis B Virus Infection Updated Swedish GuidelinesFenny Noor AidaNo ratings yet
- Intermediate UveitisDocument7 pagesIntermediate UveitisFenny Noor AidaNo ratings yet
- Penyakit Inf Saluran Pencernaan PDFDocument9 pagesPenyakit Inf Saluran Pencernaan PDFAde PermanaNo ratings yet
- Intermediate UveitisDocument7 pagesIntermediate UveitisFenny Noor AidaNo ratings yet
- Hepatitis B and Pregnancy: Virologic and Immunologic CharacteristicsDocument15 pagesHepatitis B and Pregnancy: Virologic and Immunologic CharacteristicsFenny Noor AidaNo ratings yet
- A Narrative Review of Persistent Post-Stroke Headache - ADocument12 pagesA Narrative Review of Persistent Post-Stroke Headache - AFenny Noor AidaNo ratings yet
- Best Practice & Research Clinical Obstetrics and GynaecologyDocument12 pagesBest Practice & Research Clinical Obstetrics and GynaecologyFenny Noor AidaNo ratings yet
- A Comprehensive Review of Central Post Stroke PainDocument15 pagesA Comprehensive Review of Central Post Stroke PainFenny Noor AidaNo ratings yet
- Penyakit Inf Saluran Pencernaan PDFDocument9 pagesPenyakit Inf Saluran Pencernaan PDFAde PermanaNo ratings yet
- Immigration and Viral Hepatitis: Public HealthDocument8 pagesImmigration and Viral Hepatitis: Public HealthFenny Noor AidaNo ratings yet
- WHO HIV 2015.5 EngDocument10 pagesWHO HIV 2015.5 EngFenny Noor AidaNo ratings yet
- Best Practice & Research Clinical Obstetrics and GynaecologyDocument12 pagesBest Practice & Research Clinical Obstetrics and GynaecologyFenny Noor AidaNo ratings yet
- Penyakit Inf Saluran Pencernaan PDFDocument9 pagesPenyakit Inf Saluran Pencernaan PDFAde PermanaNo ratings yet
- Tabungan Fenny Noor AidaDocument1 pageTabungan Fenny Noor AidaFenny Noor AidaNo ratings yet
- Hepatitis B and Pregnancy: Virologic and Immunologic CharacteristicsDocument15 pagesHepatitis B and Pregnancy: Virologic and Immunologic CharacteristicsFenny Noor AidaNo ratings yet
- Penyakit Inf Saluran Pencernaan PDFDocument9 pagesPenyakit Inf Saluran Pencernaan PDFAde PermanaNo ratings yet
- Wellness and Healthy Magazine Wellness and Healthy Magazine Wellness and Healthy MagazineDocument5 pagesWellness and Healthy Magazine Wellness and Healthy Magazine Wellness and Healthy Magazineresty shrdNo ratings yet
- Hepatitis B and Pregnancy: An Underestimated Issue: 2009 John Wiley & Sons A/SDocument7 pagesHepatitis B and Pregnancy: An Underestimated Issue: 2009 John Wiley & Sons A/SFenny Noor AidaNo ratings yet
- Maternity Hospital PowerPoint TemplatesDocument48 pagesMaternity Hospital PowerPoint TemplatesweberNo ratings yet
- Vertebral Artery Dissection Presenting As Isolated Vertigo: N J Rane, D McauleyDocument1 pageVertebral Artery Dissection Presenting As Isolated Vertigo: N J Rane, D McauleyFenny Noor AidaNo ratings yet
- Endometriosis and Pelvic Pain Epidemiological EvidDocument13 pagesEndometriosis and Pelvic Pain Epidemiological EvidFenny Noor AidaNo ratings yet
- Penyakit Inf Saluran Pencernaan PDFDocument9 pagesPenyakit Inf Saluran Pencernaan PDFAde PermanaNo ratings yet
- Hepatitis B and Pregnancy: Virologic and Immunologic CharacteristicsDocument15 pagesHepatitis B and Pregnancy: Virologic and Immunologic CharacteristicsFenny Noor AidaNo ratings yet
- Drug-Induced Acute-onChronic Liver FailureDocument18 pagesDrug-Induced Acute-onChronic Liver FailureVerónica Bello HorizonteNo ratings yet
- Gross Anatomy of The Appendix, Colon, Rectum, and AnusDocument8 pagesGross Anatomy of The Appendix, Colon, Rectum, and Anusbo gum parkNo ratings yet
- TERMINOLOGI 2 ST - PencernaanDocument61 pagesTERMINOLOGI 2 ST - PencernaanSarah Suzanna Sitepu0% (1)
- Barium Swallow (Esophagram) :: Positions and Barium Images PurposeDocument3 pagesBarium Swallow (Esophagram) :: Positions and Barium Images PurposeAaron SmithNo ratings yet
- Hemorrhoids in PregnancyDocument3 pagesHemorrhoids in PregnancySalwa Rizky SalsabillaNo ratings yet
- Baxter 2018Document5 pagesBaxter 2018Bagus Putra KurniawanNo ratings yet
- Guia para El Manejo de La Anemia Por Deficiencia de Hierro 2017Document9 pagesGuia para El Manejo de La Anemia Por Deficiencia de Hierro 2017Walther YepesNo ratings yet
- Altered Bowel EliminationDocument1 pageAltered Bowel EliminationneoclintNo ratings yet
- NCP DiarrheaDocument2 pagesNCP DiarrheaPrincess Xzmae RamirezNo ratings yet
- Anal FissuraDocument14 pagesAnal FissuraAnonymous LoQcj2xENo ratings yet
- Nursing Care Plan Peptic UlcerDocument3 pagesNursing Care Plan Peptic UlcerJefferson Baluyot PalmaNo ratings yet
- Esophageal Involvement in Scleroderma: Gastroesophageal Reflux, The Common ProblemDocument9 pagesEsophageal Involvement in Scleroderma: Gastroesophageal Reflux, The Common ProblemVania Dwi AndhaniNo ratings yet
- Serotonin (5-HT3) Antagonist: Ondansetron SucralfateDocument6 pagesSerotonin (5-HT3) Antagonist: Ondansetron SucralfateLola LeNo ratings yet
- Harrison's Practice Abdominal Pain DefinitionDocument27 pagesHarrison's Practice Abdominal Pain Definitionearicasilla100% (2)
- Discharge Planning Diarrhea PatientDocument2 pagesDischarge Planning Diarrhea PatientSulvian ayuNo ratings yet
- Human Digestive System (Notes)Document5 pagesHuman Digestive System (Notes)emily sidantaNo ratings yet
- Chapter 005 QuestionsDocument24 pagesChapter 005 QuestionsCaitlin EsguerraNo ratings yet
- Family Medicine 19Document4 pagesFamily Medicine 19moses okumuNo ratings yet
- Insolube Fibers Group-3 PDFDocument19 pagesInsolube Fibers Group-3 PDFHind almazrouei100No ratings yet
- 8.2 # Human Digestive SystemDocument5 pages8.2 # Human Digestive SystemSara Nadeem KhanNo ratings yet
- Nutrilite FiberDocument8 pagesNutrilite FiberJignesh Dhomse100% (1)
- Stomach Ulcer TreatmentsDocument3 pagesStomach Ulcer TreatmentsplacementfriendsNo ratings yet
- LABORATORY DIAGNOSIS OF GIT AND PANCREATIC DISORDERS - PPTXDocument105 pagesLABORATORY DIAGNOSIS OF GIT AND PANCREATIC DISORDERS - PPTXVijay SudhaNo ratings yet
- A MCQ: Si - No Sub Topics NameDocument2 pagesA MCQ: Si - No Sub Topics NameInzamamul Haque ShihabNo ratings yet