Professional Documents
Culture Documents
Module 1 (Lesson 1)
Uploaded by
Jovencio Jr. Milo MilanCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Module 1 (Lesson 1)
Uploaded by
Jovencio Jr. Milo MilanCopyright:
Available Formats
1
MODULE I
INTRODUCTION TO PHARMACOLOGY
Lesson 1 Principles of Pharmacology
Lesson 2 Pharmacological
Considerations in IVT
Lesson 3 Law, Medicine and the
Midwife
J. Milan Jr. Module I
2
MODULE I
INTRODUCTION TO PHARMACOLOGY
INTRODUCTION
This module sets the scene by describing the state of the evidence based in midwifery
pharmacology; it continues with an account of pharmacological principles, terms and definitions
as they relate to midwifery practice. It also outlines the extra considerations involved when
intravenous (IV) drug administration is undertaken outside specialist intensive care facilities.
Lastly, it describes the statutory framework for the control of medicines and discusses the
implications for midwives.
LEARNING OUTCOMES
After studying the module, you should be able to:
1. Discuss the foundations of pharmacology.
2. Explain the interactions between the drug and its recipient.
3. Explain the rights and route of drug administration.
4. Apply properly the steps of IV cannulation following the healthcare process.
5. Determine the possible complications of IV therapy and its management.
6. Explain the legal regulations of pharmacology in the Philippines.
DIRECTIONS/ MODULE ORGANIZER
There are three (3) lessons in Module 1. Read the lesson carefully then answer the given
exercise after each lesson. This is to assess your understanding and/or to augment your
learnings. Work on these exercises carefully and submit your output as advised by your
instructor.
In case you encounter difficulty, discuss this with me anytime via messenger or email.
If not, set an appointment with me to talk your concerns at the CCHAMS faculty office.
Good luck and enjoy while learning.
J. Milan Jr. Module I
3
Lesson 1
PRINCIPLES OF PHARMACOLOGY
Pharmacology
The study of the actions of drugs, incorporating knowledge from other interrelated
sciences, such as pharmacokinetics (how the body absorbs, distributes, metabolizes, and
excretes a drug) and pharmacodynamics (a drug’s mechanism of action and effect on an
organism).
The three basic concepts of pharmacology:
1. Pharmacokinetics—the absorption, distribution, metabolism, and excretion of drugs
by the body
2. Pharmacodynamics—the biochemical and physical effects of drugs and the
mechanisms of drug actions
3. Pharmacotherapeutics—the use of drugs to prevent and treat diseases.
The other important aspects of pharmacology, include:
• How drugs are named and classified
• How drugs are derived
• How drugs are administered
Drug Classifications
Drugs are classified by how they affect certain body systems, such as the use of
bronchodilators for respiratory conditions; by their therapeutic use, such as anti-nausea; or
based on their chemical characteristics, such as beta-blockers.
Drug Names
Midwives must know both the trade name of a drug, which is assigned by the
pharmaceutical company that manufactures the drug, and the generic name, which is the
official drug name and is not protected by trademark.
Drug Nomenclature
Every drug has (at least) three names:
1. Chemical Name – a scientific name that precisely describes the drug’s atomic
and molecular structure.
2. Generic Name or nonproprietary name or official name - an abbreviation of the
chemical name and it refers to a common established name regardless of its
manufacturer. There is only one generic name for a drug.
3. Brand Name (there can be one or more proprietary or trade names) – it is selected
by the drug company selling the product. Trade names are protected by
copyright. The symbol ® after a trade name indicates that the name is registered
by and restricted to the drug manufacturer.
Drugs Derivation
Drugs and biologic products are derived from 4 main sources:
1. Plants: examples of which are digitalis
2. Animals and human: from which drugs such as insulin, epinephrine are obtained
3. Minerals or mineral products: examples such as iodine and iron
4. Chemicals: made in laboratories
Route of Drug Administration
The various routes of administrations are classified into local route and systemic route.
The local route is the simplest mode of administration of a drug at the site where the desired
action is required. When the systemic absorption of a drug is desired, medications are usually
administered by two main routes: the enteral route and the parenteral route.
J. Milan Jr. Module I
4
Figure 1. Routes of Drug Administration
I. Local Route: applied to a localized area of the body or to the surface of a body part
regardless of the location of the effect.
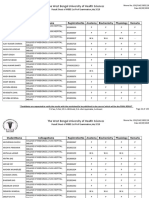
Table 1. Local Route
Route Description
Topical • Drugs are applied into the skin or mucous membrane of the eye, ear,
nose, mouth, vagina etc., mainly for local action.
• It provides a high local concentration of the drug without affecting the
general circulation.
• Drugs that are absorbed into the circulation after local administration
may then have systemic effects.
• Drugs for topical applications are usually available as creams, ointment,
liniment and drops.
II. Enteral Routes: any administration that makes use of the GIT to administer the drug
Figure 1. Enteral Routes of Drug Administration
J. Milan Jr. Module I
5
Table 2. Enteral Routes
Route Description
Oral • The most frequently used route and the first choice for drug
administration as much as possible.
• Drugs administered orally are placed in the mouth and swallowed.
Rectal • The rectal mucosa is capable of absorbing many soluble drugs into the
circulation.
• Rectal medication may be in suppository form or in liquid form to be
administered as a retention enema.
Sublingual/Buccal • The drug is placed under the tongue (sublingual route) or between gums
and inner lining of the cheek (buccal route).
• In both cases, the drug is allowed to dissolve, avoiding swallowing as far
as possible.
• The drug is rapidly absorbed through the mucosa into circulation,
thereby bypassing the portal circulation and, thus, the first-pass
metabolism in the liver.
II. Parenteral Routes: any administration that avoids the used of the GIT to administer
the drug
Figure 2. Parenteral Routes of Drug Administration
Table 3. Parenteral Routes
Route Description
Subcutaneous (SC) • Administration beneath the skin; hypodermic.
• Synonymous with the term subdermal or hypodermal.
Intramuscular (IM) • Administration within a muscle.
Intradermal (ID) • Administration within the dermis.
Intravenous (IV) • Administration within or into a vein or veins.
Intra-arterial (IA) • Administration within an artery or arteries.
Intrathecal (IT) • Administration within the cerebrospinal fluid at any level of the
cerebrospinal axis, including injection into the cerebral ventricles
Intraperitoneal (IP) • Administration within the peritoneal cavity.
Intravitreal • Administration within the vitreous body of the eye.
J. Milan Jr. Module I
6
Transdermal • Commonly referred to as “the patch”.
• Drugs administered must be highly lipophilic.
Inhalation • Also known as pulmonary route.
• A common route, both for local and for systemic actions.
• Drugs may be inhaled as gases (e.g., nitrous oxide) and enter the
bloodstream by diffusing across the alveolar membrane.
Figure 3. Injection Sites (Ruiz and Montoto. 2018)
The Evidence-Based for Pharmacologic Intervention
All treatments and their effects are multidimensional. When assessing the contribution
made by drugs to health care, we could consider the available evidence under the headings:
• magical/placebo and nocebo effects
• empirical evidence
• rational/scientific evidence
Drug Therapy
The interactions between the drug and the person receiving it can be divided into four
stages:
• Getting the drug into the body – pharmaceuticals
• Getting the drug around, about and out of the body – pharmacokinetics
• Actions of the drug on the body – pharmacodynamics
• Effects of the drug on the person – therapeutics
Figure 3. Drug Therapy
J. Milan Jr. Module I
7
Pharmaceuticals: getting the drug into the body
Two issues are considered here:
a) Compliance
Compliance or concordance with medication is the extent to which clients
adhere to prescribed regimens and the associated professional advice.
Factors associated with non-compliance include:
✓ Women in pregnancy who consider themselves to be healthy
✓ Fear of harming the unborn child
✓ Living alone
✓ Taking more than three drugs
✓ More than two drug administrations per day
✓ Reduced esophageal motility, for example dehydration
b) Drug Formulation
The storage requirements of each preparation depend on the
formulation. Therefore, the data sheet for each product and brand should be
consulted for instructions on storage.
Pharmacokinetics: how the body handles the drug
This section addresses the questions:
• Is the drug getting to the desired site of action? (absorption and distribution)
• Is the drug getting out of the body? (elimination)
• Is there a risk of accumulation and toxicity?
The LADME scheme (Figure 4) describes the pharmacokinetic processes which follow a
given dosage regimen. LADME processes can be divided into two classes, drug input (liberation
and absorption) and drug output (distribution, metabolism and excretion)
(http://www.rxkinetics.com/).
The LADME Scheme:
• Liberation – the process of release of
a drug from the pharmaceutical
formulation.
• Absorption – the process of a
substance entering the blood
circulation.
• Distribution – the dispersion or
dissemination of substances
throughout the fluids and tissues of
the body.
• Metabolism (or biotransformation, or
inactivation) – the recognition by the
organism that a foreign substance is
present and the irreversible
transformation of parent compounds
into daughter metabolites.
• Excretion – the removal of the
substances from the body. In rare
cases, some drugs irreversibly
accumulate in body tissue.
Figure 4. The LADME Scheme (wikipedia.org)
Therapeutic Range
Every drug has a therapeutic range or a desirable range for the concentration of drug in
plasma. Above the therapeutic range, toxic effects may appear. Below the therapeutic range,
the drug does not have the desired effect. For some drugs this range is very narrow, and the
therapeutic concentration is very close to the concentration at which adverse effects appear.
J. Milan Jr. Module I
8
The body handles all drugs in three stages and are affected to some extent by pregnancy.
1. Absorption
The process by which a drug is made available to the body fluids for
distribution. The absorption of a drug will depend on the route of administration,
formulation, and the way the drug molecules move across cell membranes
throughout the body. Important barriers to drug absorption and distribution
include: the gut wall, capillary walls, cell membranes, the blood/brain barrier,
the placenta, the blood/milk barrier.
2. Distribution
Distribution is the movement of the drug around the body. It is affected
by: a) plasma protein binding; b) the lipid solubility of the drug (that is whether
it dissolves in fatty tissues); c) the binding properties of the drug; d) blood flow
to the organs and the state of the circulation; e) stage of life cycle, for example
pregnancy, infancy; f) disease state, for example pre-eclampsia or heart failure
3. Elimination or Clearance
The route of elimination varies with individual drugs. Some drugs are
eliminated unchanged whereas others are extensively metabolized. Most drugs
are excreted via the kidneys, although the bile is also an important route of
excretion. Many drugs are passed into breast milk. Alcohol is unusual in that 5–
10 percent is eliminated unchanged via the lungs, sweat and urine. For most
drugs, elimination involves metabolism in the liver plus excretion by the kidneys.
Pharmacodynamics: actions of the drug on the body
This section addresses the question: what are the effects of the drug on the tissues?
Drugs work as a result of the physiochemical interactions between drug molecules and the
patient’s/recipient’s molecules. These chemical reactions may alter the way the cells are
functioning which in turn may lead to changes in the behavior of tissues, organs, and systems.
Drugs modify the existing functions of the body; they cannot introduce new functions. Most
drugs act on more than one type of cell and therefore have multiple effects on the body.
Figure 5. Pharmacokinetics vs. Pharmacodynamics
Most drug molecules work via:
• Protein receptors in cell membranes or within cells
Many drugs work by acting on specific receptor proteins. These are
components of the cell membrane which normally respond to the body’s
hormones and neurotransmitters – the endogenous ligands. Examples include
insulin receptors, opioid receptors, dopamine receptors, histamine receptors.
Many drugs imitate the actions of the body’s own ligands. Some drugs are direct
replacements, for example insulin and epinephrine (adrenaline). Others provide
an artificial boost to certain receptors, for example opioids.
J. Milan Jr. Module I
9
Figure 6. Drug-Plasma Protein Binding (Sparreboom et al., 2001)
• Ion channels in cell membranes
Ion channels are similar to receptors in the way they bind to certain
drugs. Examples include calcium antagonists (nifedipine) and local anesthetics
such as lignocaine. However, because ion channels are present in a wide variety
of cells and tissues, the side effects of these drugs can affect several body
systems. For example, local anesthetics affect both nerves and muscles.
• Enzymes in cells or extracellular fluid
Enzymes are present in all cells, catalyzing their vital biochemical
reactions. Some drugs bind to enzymes and inhibit their actions. Examples
include, NSAIDs (non-steroidal anti-inflammatory drugs, such as aspirin,
ibuprofen), MAOIs (mono amino oxidase inhibitors for depressive illness). It is
likely that these drugs are able to interact with certain enzymes by virtue of
their shape and structure in a similar manner to the drug–receptor interaction.
• Non-specific actions
Some drugs are presumed to act by virtue of their physiochemical
properties, rather than as a result of the specific shape of their molecules. For
example, antacids such as sodium bicarbonate or aluminum hydroxide neutralize
gastric secretions without acting on the cells of the body.
Therapeutics: the effects of the drug on the person
This section addresses the questions: has the drug produced any effect on the recipient?
If so, is the result therapeutic or toxic?
Changes in Physiology of Cells, Tissues and Organs
Even if a drug is working on the body’s cells, there may be no noticeable
response. For example, due to individual differences, an oxytocic or a tocolytic may be
ineffective.
Clinical Effects
Clinical response shows considerable individual variation. This is not always
entirely predictable, and idiosyncratic reactions can occur. For example, some women
are unduly sensitive to oxytocin, and therefore infusions are commenced using a very
low dose (BNF, 2000). Clinical effects also depend upon age, gender, pregnancy, disease
J. Milan Jr. Module I
10
state, drug interactions, weight, height, and genetic make-up. For example, women
generally require lower doses of drugs than men, even when body weight is taken into
consideration.
Side Effects
Side effects are adverse drug reactions that occur within the normal range of
therapeutic doses. Most drugs have potential side effects. These can be grouped under
the headings:
• Related to the Drug’s Main Actions
These are often the drug’s main side effects. Severity is usually related
to the dose administered. Since such side effects are often highly significant
and entirely predictable, appropriate monitoring systems must be in place.
For example, unless adequate checks are undertaken anti-coagulants can
cause bleeding, and insulin can cause hypoglycemia. With other drugs, the
link between drug actions and side effects is less obvious and requires rather
more understanding of physiology.
• Unrelated to the Drug’s Main Actions:
✓ Related to Subsidiary Actions
Many drugs act on more than one type of cell receptor; this
consequence gives the potential for diverse side effects. Again, these
side effects are predictable, and the midwife should monitor or
caution the woman appropriately.
For example, oxytocin acts on the oxytocic receptors of the
uterus, but it also acts on the anti-diuretic (ADH) receptors in the
nephrons. This property gives it the potential to trigger water
retention and fluid overload. Therefore, the midwife must monitor
fluid balance.
In pregnancy, the subsidiary actions of drugs on the uterus assume
great importance. Any drugs which stimulate uterine contractility
should be avoided, including stimulant laxatives, misoprostol and all
drugs chemically related to ergotamine.
✓ Hypersensitivity Responses
A hypersensitivity response is possible with almost all drugs,
although antimicrobials are particular offenders. Individuals with a
history of atopic disorders, such as asthma or eczema, are particularly
vulnerable.
Most drugs or their metabolites can combine with carrier proteins
in the circulation to form immunogens, substances which produce an
immune response. This may affect any one of several organs such as
skin, liver or bone marrow. The severity of the hypersensitivity
response is also variable, ranging from a temporary skin rash to life-
threatening aplastic anemia.
✓ Cell Damage
Some drugs can cause direct damage to cells. For example, in
large doses, paracetamol (acetaminophen) can damage the liver and
kidneys. Other drugs, such as components of tobacco, damage cells by
altering the DNA regulating oncogenes which control cell division.
Drug-induced teratogenesis is a result of cell damage. The risks of
fetal damage depend on several factors as well as the chemical
composition of the drug (Lipkin, 1993):
• The stage of pregnancy
• The amount of drug ingested
• The number of doses – a single dose may be less damaging than
repeated exposure
• Other agents to which mother and fetus are exposed
• The mother’s nutritional status
• The genetic makeup of mother and fetus.
J. Milan Jr. Module I
11
EXERCISE
Instruction: In a separate sheet, answer the following questions briefly.
1. In your own words, explain the following statements in 3-5 sentences:
a. Relevance of your course (Mid 201) in your profession.
b. Pharmacokinetics, Pharmacodynamics and Pharmacotherapeutics.
c. Side Effects and Adverse Reactions
2. Discuss the following:
a. Rights of drug administration
b. Advantages and disadvantages of each route of drug administration.
c. Different drug preparations
J. Milan Jr. Module I
You might also like
- Chapter 1 Pharmacology Complete Notes PDF D.Pharma ER20 PCI Noteskarts Pharmacology Notes PDFDocument16 pagesChapter 1 Pharmacology Complete Notes PDF D.Pharma ER20 PCI Noteskarts Pharmacology Notes PDFNagur123 ShaikNo ratings yet
- Introduction To PharmacologyDocument45 pagesIntroduction To Pharmacologysandeepv08No ratings yet
- Routes of Drug Administration: A Guide to Understanding Delivery MethodsDocument37 pagesRoutes of Drug Administration: A Guide to Understanding Delivery MethodsForwardNo ratings yet
- General PharmacologyDocument101 pagesGeneral PharmacologyAditya RathoreNo ratings yet
- Common Drugs Use in OphthalmologyDocument40 pagesCommon Drugs Use in Ophthalmologyณัช เกษมNo ratings yet
- Module 1 To 4Document208 pagesModule 1 To 4smbawasainiNo ratings yet
- Presented By: Imran Ahammad ChowdhuryDocument8 pagesPresented By: Imran Ahammad ChowdhurySonia BaruaNo ratings yet
- Labelling and PackagingDocument16 pagesLabelling and PackagingvyshnosudhaNo ratings yet
- Pharmacology M Pharm Syllabus KU 1Document15 pagesPharmacology M Pharm Syllabus KU 1Nagaraj YadavNo ratings yet
- Indian Public Health Standard IIDocument19 pagesIndian Public Health Standard IIKailash NagarNo ratings yet
- Pathophysiology LESSON PLANDocument9 pagesPathophysiology LESSON PLANLokesh ParmarNo ratings yet
- Anti TB PPT FinalDocument43 pagesAnti TB PPT FinalKeziah GillNo ratings yet
- Classification of Drugs According To Pharmacological ClassificationDocument1 pageClassification of Drugs According To Pharmacological ClassificationIssan Villaruel100% (1)
- Pharmacotherapy During Pregnancy, Childbirth and Lactation: Principles To ConsiderDocument7 pagesPharmacotherapy During Pregnancy, Childbirth and Lactation: Principles To Consideryuliana nurcahyatiNo ratings yet
- Peptic Ulcer Disease: Causes, Symptoms and TreatmentDocument60 pagesPeptic Ulcer Disease: Causes, Symptoms and TreatmentNehimyaNo ratings yet
- Essential Drug Concept and Its Implication in NepalDocument5 pagesEssential Drug Concept and Its Implication in NepalB.pharm 16th BatchNo ratings yet
- Immunomodulators: By: Payal Suthar Department of PharmacognosyDocument26 pagesImmunomodulators: By: Payal Suthar Department of PharmacognosyHely Patel100% (1)
- Benefit vs HarmDocument3 pagesBenefit vs HarmSahrulNuhuyanan0% (1)
- Mechanisms of Drug Toxicity: Proceedings of the Third International Pharmacological MeetingFrom EverandMechanisms of Drug Toxicity: Proceedings of the Third International Pharmacological MeetingH. RaškováNo ratings yet
- Course Syllabus-Maternity TheoryDocument6 pagesCourse Syllabus-Maternity TheoryannairishybNo ratings yet
- Factors Affecting Drug Absorption PDFDocument2 pagesFactors Affecting Drug Absorption PDFRobNo ratings yet
- Vijaya College of Nursing: Course Subject Unit Bio-Psycho Social PathophysiologyDocument3 pagesVijaya College of Nursing: Course Subject Unit Bio-Psycho Social PathophysiologyReshma Rinu50% (2)
- MW3501 Pharmacology For Midwifery Practice PDFDocument2 pagesMW3501 Pharmacology For Midwifery Practice PDFLerma Navarro Reyes-Valencia100% (1)
- Pharmacotherapeutics PDFDocument30 pagesPharmacotherapeutics PDFprazol shresthaNo ratings yet
- Guideline Antibiotic RationalDocument35 pagesGuideline Antibiotic RationalIstianah EsNo ratings yet
- Emetics and Antiemetics DrugsDocument15 pagesEmetics and Antiemetics DrugsrajenderNo ratings yet
- TDM of LidocaineDocument19 pagesTDM of LidocaineNikkiiNo ratings yet
- Pharmacology For Nurses Part BDocument118 pagesPharmacology For Nurses Part BAndrea CarmenNo ratings yet
- Classification of Antibiotics by Biological Effect and Chemical StructureDocument14 pagesClassification of Antibiotics by Biological Effect and Chemical Structuredoc_abdullahNo ratings yet
- YAWS: Elimination To EradicationDocument5 pagesYAWS: Elimination To EradicationShrutiNo ratings yet
- RCH program goals for reproductive health and child survivalDocument2 pagesRCH program goals for reproductive health and child survivalAnnapurna DangetiNo ratings yet
- Oral MedicationDocument30 pagesOral MedicationPetit NacarioNo ratings yet
- Drug Used in Skin and Mucus MembraneDocument35 pagesDrug Used in Skin and Mucus MembraneMamta Yadav100% (1)
- Drug Distribution in HospitalsDocument38 pagesDrug Distribution in HospitalsVescop 18-21No ratings yet
- 05 N001 40088Document23 pages05 N001 40088hariharad sourabhNo ratings yet
- Topical AdministrationDocument8 pagesTopical AdministrationSilpa Jose TNo ratings yet
- Topical skin procedure checklistDocument5 pagesTopical skin procedure checklistpramod kumawatNo ratings yet
- Obs Seminar Evaluation FormDocument1 pageObs Seminar Evaluation Formvikash kumarNo ratings yet
- History of Pharmacology From AntiquityDocument7 pagesHistory of Pharmacology From AntiquityBryan Steven González ArévaloNo ratings yet
- Acute Critical Care AssignmentDocument15 pagesAcute Critical Care Assignmentsantosh kumarNo ratings yet
- Wound Dressing Procedure WPS OfficeDocument8 pagesWound Dressing Procedure WPS OfficeAbhishek VermaNo ratings yet
- Drugs Affecting The Ear and Eye 2021Document88 pagesDrugs Affecting The Ear and Eye 2021renz bartolomeNo ratings yet
- Factors Affecting Drug Metabolism PDFDocument2 pagesFactors Affecting Drug Metabolism PDFPaige50% (2)
- Nursing Care of Patients Receiving Chemotherapy Ranjita Rajesh Lecturer People's College of Nursing BhopalDocument55 pagesNursing Care of Patients Receiving Chemotherapy Ranjita Rajesh Lecturer People's College of Nursing BhopalFayizatul AkmarNo ratings yet
- Mathematical Fundamental in PharmacokineticDocument21 pagesMathematical Fundamental in PharmacokineticErna PratiwiNo ratings yet
- Poisoning First AidDocument13 pagesPoisoning First AidGerra Mae Tubio CandelasaNo ratings yet
- Case Study FOR Pharmaceutical Care: Drug-Related Needs Drug-Therapy ProblemsDocument44 pagesCase Study FOR Pharmaceutical Care: Drug-Related Needs Drug-Therapy ProblemsYorry Chiristine Pamangin100% (3)
- Univ. „Ovidius” of Constanța General Medicine InjectionsDocument18 pagesUniv. „Ovidius” of Constanța General Medicine InjectionsNotInterestedNo ratings yet
- VAGINITISDocument16 pagesVAGINITISannu panchalNo ratings yet
- Routes of Drug AdministrationDocument37 pagesRoutes of Drug Administrationxq qxNo ratings yet
- The West Bengal University of Health SciencesDocument9 pagesThe West Bengal University of Health Sciencesbhaskar rayNo ratings yet
- Lecture 1, Introduction To Pharmacology (Script)Document10 pagesLecture 1, Introduction To Pharmacology (Script)JustDen09No ratings yet
- Essential Medicine List Concept and Rational UseDocument16 pagesEssential Medicine List Concept and Rational UseDixa MeNo ratings yet
- Teach ManualDocument78 pagesTeach ManualShouvik DebnathNo ratings yet
- Antepartum Haemorrhage: BY: Ms. R. Liangkiuwiliu Assistant Professor, Obg SSNSR, SuDocument44 pagesAntepartum Haemorrhage: BY: Ms. R. Liangkiuwiliu Assistant Professor, Obg SSNSR, SuLiangkiuwiliuNo ratings yet
- Management of Tuberculosis: A guide for clinicians (eBook edition)From EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)No ratings yet
- New Era University: Pharmacology For MidwiferyDocument11 pagesNew Era University: Pharmacology For MidwiferyHarriegail O. LontocNo ratings yet
- Route of Drug AdministrationDocument4 pagesRoute of Drug AdministrationMr. PREMNATH D. 930No ratings yet
- Module 1 (Lesson 2)Document11 pagesModule 1 (Lesson 2)Jovencio Jr. Milo MilanNo ratings yet
- Midwifery Practice and Legal AccountabilityDocument11 pagesMidwifery Practice and Legal AccountabilityJovencio Jr. Milo MilanNo ratings yet
- Midwifery Practice and Legal AccountabilityDocument11 pagesMidwifery Practice and Legal AccountabilityJovencio Jr. Milo MilanNo ratings yet
- Module 1 (Lesson 1)Document11 pagesModule 1 (Lesson 1)Jovencio Jr. Milo MilanNo ratings yet
- Module 1 (Lesson 2)Document11 pagesModule 1 (Lesson 2)Jovencio Jr. Milo MilanNo ratings yet
- VEDANT ChaudhariDocument31 pagesVEDANT Chaudharivedant chaudhariNo ratings yet
- Anjleen KaurDocument3 pagesAnjleen KaurAnjleen KaurNo ratings yet
- Injections and Implanted Drug ProductsDocument3 pagesInjections and Implanted Drug ProductsHAROLD TANNo ratings yet
- CHECKLIST - Administering Oral, Sublingual, and Buccal MedicationDocument4 pagesCHECKLIST - Administering Oral, Sublingual, and Buccal MedicationMichaelNo ratings yet
- Lange Q&A: Radiography ExaminationDocument18 pagesLange Q&A: Radiography ExaminationSamuel JeebanNo ratings yet
- Migraine Diagnosis and TreatmentDocument19 pagesMigraine Diagnosis and TreatmentMagdalila Pua RosalesNo ratings yet
- Prescribing Information and Patient Medication Information: BuscopanDocument27 pagesPrescribing Information and Patient Medication Information: BuscopanMey KhNo ratings yet
- 2021 SAE KeyWords Email XPHS 022221Document18 pages2021 SAE KeyWords Email XPHS 022221haftomNo ratings yet
- Medication Administration QuestionsDocument17 pagesMedication Administration QuestionsJacqueline Greer100% (1)
- Ali Raza Pharma NotesDocument110 pagesAli Raza Pharma NotesMuhammad Talha100% (1)
- Routes of Administration ReferencesDocument55 pagesRoutes of Administration ReferencesVictoria Eliza InguilloNo ratings yet
- Delivery of BiopharmaceuticalDocument9 pagesDelivery of BiopharmaceuticalRabia KhattakNo ratings yet
- Smu066 PDF EngDocument9 pagesSmu066 PDF EngDEREK SANDOVALNo ratings yet
- Dosage FormDocument5 pagesDosage Formqbn9vx7t9jNo ratings yet
- Intravenous in The Management OF Gouty Arthritis : ColchicineDocument5 pagesIntravenous in The Management OF Gouty Arthritis : Colchicinejnbp1No ratings yet
- NCM 109 Rle PrelimDocument21 pagesNCM 109 Rle PrelimAllaika Zyrah FloresNo ratings yet
- KAPS Exam Guide and Sample Papers - Australian Pharmacy Council PDFDocument10 pagesKAPS Exam Guide and Sample Papers - Australian Pharmacy Council PDFShoaib BiradarNo ratings yet
- Study of Dissolution Enhancement of Furosemide by Solid Dispersion Technique Using Different PolymersDocument86 pagesStudy of Dissolution Enhancement of Furosemide by Solid Dispersion Technique Using Different PolymersTanvir halimNo ratings yet
- Types of Parenteral Products ExplainedDocument7 pagesTypes of Parenteral Products ExplainedJoginder KumarNo ratings yet
- 22 Design of Controlled-Release Drug Delivery SystemsDocument14 pages22 Design of Controlled-Release Drug Delivery Systemssantoshnaidu555No ratings yet
- Pharmacokinetic & PharmacodynamicDocument77 pagesPharmacokinetic & Pharmacodynamicdimasscrib100% (1)
- Pharmacy Paper I & II TopicsDocument2 pagesPharmacy Paper I & II TopicsShadman RhamanNo ratings yet
- Formulationandin vitroEvaluationofBuccalTabletsofPiroxicam PDFDocument11 pagesFormulationandin vitroEvaluationofBuccalTabletsofPiroxicam PDFFransisca Cornelia PutriNo ratings yet
- (PHA6118 LEC) Pharmacokinetics and Pharmacodynamics FINALDocument6 pages(PHA6118 LEC) Pharmacokinetics and Pharmacodynamics FINALchristian redotaNo ratings yet
- Chapter 5 ReviewDocument5 pagesChapter 5 Review陳宛妤No ratings yet
- Common Acronyms & AbbreviationsDocument2 pagesCommon Acronyms & AbbreviationsMayrigen DominguezNo ratings yet
- IRAN DRUG LIST - September 2009: No Drug Name Dosage Form ATC Code Description List NameDocument70 pagesIRAN DRUG LIST - September 2009: No Drug Name Dosage Form ATC Code Description List NameportosinNo ratings yet
- General PharmacologyDocument288 pagesGeneral PharmacologyFisseha AbayNo ratings yet
- 2-Principles of Antimicrobial Therapy 2 PDFDocument29 pages2-Principles of Antimicrobial Therapy 2 PDFShashidharan MenonNo ratings yet
- General Pharmacology by DR Mayur Sayta M 91044Document19 pagesGeneral Pharmacology by DR Mayur Sayta M 91044funzzNo ratings yet