Professional Documents
Culture Documents
(PHA6118 LEC) Pharmacokinetics and Pharmacodynamics FINAL
Uploaded by
christian redotaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
(PHA6118 LEC) Pharmacokinetics and Pharmacodynamics FINAL
Uploaded by
christian redotaCopyright:
Available Formats
PHARMACOLOGY I
Lecture \ SECOND SEMESTER
UNIT/LESSON XX: PHARMACOKINETICS AND PHARMACODYNAMICS
OUTLINE • Makes possible the calculation of loading and maintenance
doses
I. Pharmacokinetics EFFECTIVE DRUG CONCENTRATION
II. Effective Drug Concentration • Concentration of a drug at the receptor site (in contrast to
III. Plasma Concentration drug concentrations that are more rapidly measured, e.g.,
IV. 2 Basic Parameters blood)
V. Clearance (CL) PLASMA CONCENTRATION
VI. Half Life (T ½)
• Rate of input of the drug (by absorption) into the plasma
VII. Steady State Concentration
VIII. Bioavailability • Rate of distribution to peripheral tissue (including the target
organ)
IX. Routes of Administration, Bioavailability, and
General Characteristics. • Rate of elimination, or loss, from the body
X. Area Under the Curve (AUC) 2 BASIC PARAMETERS
XI. Time Course of Drug Effects • Unique for a particular drug in a particular patient
XII. Determinants of Absorption • Average values in large populations that can be used to
XIII. Determinants of Distribution predict concentrations
XIV. Cumulative Disease o VOLUME OF DISTRIBUTION (Vd)
XV. Extraction o CLEARANCE (CL)
XVI. Target Concentration VOLUME OF DISTRIBUTION (VD)
XVII. Dosage Regimens
• Measure of apparent space in the body available to contain
XVIII. Therapeutic Drug Monitoring
the drug
XIX. Steady State Concentration
o Amount of drug in the body to the plasma/serum
XX. Therapeutic Window concentration
XXI. Peak and Through Concentration o Intracellular and extracellular compartments
• When a drug is avidly bound in peripheral tissues, it’s
PHARMACOKINETICS concentration in plasma may drop to very low values even if
the total amount in the body is large
• “The goal of therapeutics is to achieve a desired beneficial o High volume of distribution (Vd) (overall amount of
effect with minimal adverse effects” the drug in the body)
• when a medicine has been selected for a patient, the doctor • When a drug is completely retained in the plasma
must determine always the dose that closely achieves this goal compartment
• Pharmacokinetics - Dose-concentration relationship o Volume of distribution is equal to the plasma
(absorption, distribution, elimination determine how rapidly/ how long volume
the drug will appear at the target organ)
• Pharmacodynamics - Dose-effect relationship (magnitude
of the effect of a particular concentration)
EFFECT OF DRUG BINDING IN VOLUME DISTRIBUTION
• Drug A does not bind to macromolecules, diffuses freely
between 2 compartments
• Drug B binds avidly to proteins in the blood, diffusion is much
more limited (low volume of distribution; the lower the value,
• 3 primary processes of pharmacokinetics: Input, Distribution,
the more the drug that is present)
Elimination
PHARMACOKINETICS
• Dose-concentration relationship
• Effects of the biologic system on drugs
• Deals with the processes of absorption, distribution and • In each case, the amount of the drug in the body are the
elimination of drugs same, but the apparent volume of distribution are different
(still relatively low volume of distribution because it is <42)
MEL, JCM, BGT, EFL, CJC | 2F-PH 1
PHARMACOLOGY I
Lecture \ SECOND SEMESTER
UNIT/LESSON XX: PHARMACOKINETICS AND PHARMACODYNAMICS
• Example: Drug C is avidly bound to molecules in peripheral HALF LIFE (T ½)
tissues, so that a larger total dose (200 units) is required to • Time it takes for the amount or concentration of a drug to fall
achieve measurable plasma concentrations At equilibrium, to 50% of an earlier measurement
198 units are found in the peripheral tissues and only 2 units
in the plasma, so that the calculated volume of distribution • Drugs eliminated by first-order kinetics
is greater than the physical volume of the system (To have o Constant regardless of concentration
a good plasma concentration, you need to have a higher • Drugs eliminated by zero-order kinetics
dose of drug because most of the drugs are bound to your o Particularly useful
peripheral tissues and only 2 units are in the plasma. 100= o Not constant
the drug has a high value of distribution.) o Slower clearance
• High value of distribution: most of the drug are present in the o Example of drugs that follow zero-order kinetics
peripheral tissues, in the cells, fats, organs and only few of include phenytoin, anticonvulsant, alcohol
them are in the vascular component. (konti lang yung • Derived parameter from the volume of distribution and
nagccirculate na blood) clearance
• This will affect the half-life and the dosing of the drug. The o Vd is important in half-life determination
higher the volume of distribution = the longer the half-life of • Determines the rate at which blood concentration rises
our medications (because there are a lot of drug remained during a constant infusion and falls after administration is
in our tissues) stopped
• If you have a high vloume of distrubution, you need to have
higher frequency of giving the medication so that you can
achieve a steady concentration of the drug in your blood.
(mas maraming beses magbibigay ng gamot para mareach
mo yung intended concentration mo sa blood)
• Summary: it can affect the half-life and the dosing frequency
of your drug
STEADY STATE CONCENTRATION
• Rate of drug administration is equal to rate of elimination
o need to have at least 5 half-lives to reach 100% of
your steady state
• Dose in = dose out
• Rate of steady state = rate of elimination
CLEARANCE (CL)
• Rate of elimination compared to plasma concentration
• Depends on the drug and the organs of elimination in the
patient
• Drugs eliminated with first-order kinetics
• Clearance is constant
BIOAVAILABILITY
• Elimination rate is equal to clearance times plasma
concentration
• Fraction of the administered dose of the drug that reaches
• Elimination will be rapid at first and slow as the concentration the systemic circulation
decreases
o Example: 5 units/ h (after an hour) -> 2.5 units/h -> • Equal to the amount absorbed over the amount
1.25 units/h and so on until eliminated. (depending administered
on the drug characteristic) • Intravenous administration
o Unity or 100% bioavailability because it will bypass
1st-pass metabolism
• Administration by other routes
o Reduced by incomplete absorption
o 1st-pass metabolism
▪ When the drug is taken orally, it will first
pass through portal circulation in the
liver to metabolize other drugs, hence,
the amount of drug taken will not fully go
to systemic circulation.
o Distribution into other tissues before the drug
enters the systemic circulation
MEL, JCM, BGT, EFL, CJC | 2F-PH 2
PHARMACOLOGY I
Lecture \ SECOND SEMESTER
UNIT/LESSON XX: PHARMACOKINETICS AND PHARMACODYNAMICS
o Drugs are more absorbed in the small intestines for lack of first-
because it has a larger surface area pass effect;
▪ Example: enteric coated and extended prolonged
release drugs duration of action
▪ Stomach acids may damage drugs more (skin -> slower
-> less absorption absorption)
• To offset low bioavailability • Dependent on
o Sublingual o Extent of absorption
▪ Principle: it bypasses 1st-pass effect o 1st pass effect
because the sublingual veins drain to o Rate of absorption
lingual veins to internal jugular veins that o Site of administration [e.g., topical drugs
will drain to subclavian veins down to (ointments) which have very slow rate of
superior vena cava (will not pass thru absorption
liver) and will be pumped through AREA UNDER THE CURVE (AUC)
systemic circulation. • The area under the curve (AUC) is used to calculate
o Rectal - 50% probability of bypassing the 1st - the bioavailability of a drug.
pass effect
▪ Good route of administration because it
is blood-vessel rich = greater absorption • Bioavailability is calculated from AUC(route)/AUC(IV)
▪ Example: Suppositories
▪ must be correctly inserted in • AUC can be derived from either a single dose or
the inferior part of the rectum, multiple dose.
then it will be drained to the
internal iliac vein to superior
vena cava to the heart, so it
will bypass portal circulation
(liver).
▪ Otherwise, if inserted to the
superior rectal vein, it will go
to the mesenteric vein, hence
directly drain to the portal
circulation so there is 1st-pass DETERMINANTS OF ABSORPTION
effect. 1. ROUTE OF ADMINISTRATION
o Inhalation or nasal • IV route: fastest absorption rate
▪ Similar to sublingual • Oral route: slowest absorption rate
o Transdermal patches 2. BLOOD FLOW
▪ Occurs in the capillaries of the skin • Influences absorption from IM, subcutaneous, and
in shock
ROUTE OF ADMINISTRATION, BIOAVAILABILITY, AND o in shock: low blood pressure = lesser
GENERAL CHARACTERISTICS blood flow in organs = lesser
absorption
Routes of Administration, Bioavailability, and General • High blood flow maintains a high drug depot-to-
Characteristics blood concentration gradient
Route Bioavailability (%) Characteristics • Maximizes absorption
Intravenous 100 (by definition) Most rapid onset 3. CONCENTRATION
(IV) • Concentration gradient
Intramuscular 75 to 100 Large volumes
(IM) often feasible;
• Major determinant of the rate of absorption (Fick’s
law)
may be painful
Subcutaneous 75 to 100 Smaller volumes • ↑ concentration = ↑ rate of absorption
(SC) than IM; may be DETERMINANTS OF DISTRIBUTION
painful 1. SIZE OF THE ORGAN
Oral (PO) 5 to <100 Most convenient; • Size of the organ determines the concentration
first-pass effect gradient between blood and the organ
may be important
Rectal (PR) 30 to <100 Less first-pass
• E.g., skeletal muscle and brain
effect than oral • ↑size of organ = ↑distribution
Inhalation 5 to <100 Often very rapid 2. BLOOD FLOW
onset • Important determinant of the rate of uptake
Transdermal 80 to 100 Usually very slow • ↑ blood flow = ↑distribution
absorption; used
MEL, JCM, BGT, EFL, CJC | 2F-PH 3
PHARMACOLOGY I
Lecture \ SECOND SEMESTER
UNIT/LESSON XX: PHARMACOKINETICS AND PHARMACODYNAMICS
• Well-perfused organs (Brain, heart, kidneys, o Most common process
splanchnic organs) o Followed by most drugs
• ↑amount of blood supply = ↑distribution
3. SOLUBILITY
• If the drug is very soluble in cells, the
concentration in the perivascular space will be
lower and diffusion from the vessel into the
extravascular tissue will be facilitated
4. BINDING
• Binding of drugs to macromolecules in the blood or
tissue compartment will tend to increase the drug’s
concentration in that compartment
• For example, if a drug is more bound to a specific
protein in the blood, the drug concentration in the
blood will be higher, resulting in a lower volume of
distribution. 2. ZERO ORDER ELIMINATION
• Amount of drug in the body to the concentration in • Rate of elimination is constant regardless of
the plasma
5. APPARENT VOLUME OF DISTRIBUTION concentration
• Amount of drug in the body to the concentration in • Occurs with drugs that saturate their elimination of
the plasma mechanism at concentrations of clinical interest
METABOLISM OF DRUGS • Concentration of such drugs in plasma decrease in
1. AS MECHANISM OF TERMINATION OF DRUG ACTION
linear fashion over time
• Action of many drugs is terminated before they are excreted
• With higher doses, there will be bigger chances of
• Metabolized to biologically inactive derivatives toxic effect because the patient may not be able to
• Conversion to a metabolite is a form of elimination eliminate it (E.g., Alcohol, Phenytoin, Aspirin)
2. AS MECHANISM OF DRUG ACTIVATION
• Prodrugs
o Inactive as administered and must be metabolized
in the body to become active
▪ Ex: Risperidone (Active constituent:
Paliperidone)
o Many drugs are active as administered and have
active metabolites as well
▪ Have long duration of action
▪ Some benzodiazepines (but not all)
• Lorazepam, Oxazepam, Temazepam:
benzodiazepines that become inactive
when metabolized
• Midazolam , Diazepam, Clonazepam: TIME COURSE OF DRUG EFFECTS
benzodiazepines with active • IMMEDIATE EFFECT
metabolites even when metabolized
o Directly related to concentration
3. DRUG ELIMINATION WITHOUT METABOLISM
o In the simplest case, drug effects are directly
• Drugs not modified by the body related to plasma concentrations, but this does not
• Continue to act until they are excreted (E.g., Lithium– necessarily mean that effects simply parallel the
used for bipolar disorder) time course of concentrations. Because the
ELIMINATION OF DRUGS relationship between drug concentration and effect
1. FIRST ORDER ELIMINATION is not linear, the effect will not usually be linearly
proportional to the concentration.
• Rate of elimination is proportionate to the
concentration (i.e., the higher the concentration, the
greater the amount eliminated per unit time)
• Drug’s concentration in plasma decreases
exponentially with time
• Half-life of elimination is constant regardless of
amount of drug in the body
• Concentration of such drug in the blood will decrease
by 50% for every half-life
MEL, JCM, BGT, EFL, CJC | 2F-PH 4
PHARMACOLOGY I
Lecture \ SECOND SEMESTER
UNIT/LESSON XX: PHARMACOKINETICS AND PHARMACODYNAMICS
• DELAYED EFFECT • CL - clearance; TC -total concentration; Foral -
o Can be due to distributional delay or delayed bioavailability during oral route
expression of the physiologic substance needed for
the effect LOADING DOSE
o Changes in the drug effects are often delayed in • For drugs with long half-lives and longer time to reach a
relation to changes in plasma concentration. steady state
o This delay may reflect the time required for the drug o Drugs with long half-lives have a slower
to distribute from plasma to the site of the action. therapeutic effect
o This will be the case for almost all drugs.
o The delay due to distribution is a pharmacokinetic • Given to promptly raise the concentration of the drug to the
target concentration
phenomenon that can account for delays of a few
minutes. o To have a faster therapeutic effect
• If the therapeutic concentration must be achieved rapidly and
• CUMULATIVE EFFECTS the volume distribution os large, a larger loading dose is
needed at the onset of therapy
o For constant infusion
o Aminoglycosides causes renal toxicity if given • Volume of distribution (Vd) is important
constantly o Higher Vd, higher loading dose
o That’s why some of the drugs are given in o Loading dose may not be needed if Vd is low
intermittent dosing schedules only
o The effect of many drugs used to treat cancer also
reflects a cumulative action—eg, the extent of
binding of a drug to DNA is proportional to drug
concentration and is usually irreversible. The effect
on tumor growth is therefore a consequence of
cumulative exposure to the drug.
EXTRACTION
• Fraction of the drug removed from the perfusing blood during
passage to the organ
• Measure of the elimination of the drug by that organ
• Drugs with high hepatic extraction ratio have large 1st - pass
effect (in turn, their bioavailability is lower) THEREPEUTIC DRUG MONITORING
TARGET CONCENTRATION PHARMACOKINETIC VARIABLES
ABSORPTION
• Desired therapeutic effects are produced
DOSAGE REGIMENS o Compliance of patient is important
o Variation in bioavailability are usually due to variation in
• Plan for drug administration over a period of time metabolism during absorption
• Achievement of therapeutic levels of the drug in the body CLEARANCE
without exceeding the minimum toxic concentration (includes
the concept of therapeutic window and toxic dose)
o Most important parameter in designing a dosage regimen
o Creatinine clearance - can be computed
MAINTENANCE DOSE
▪ Creatinine - waste product excreted through the urine in
• Dose needed to maintain a steady state of concentration normal healthy individuals; can be measured in blood and
o It will maintain plasma concentration within a urine, but usually in blood
specified range over long periods of therapy o Good indicator of renal function - raised levels may indicate
o Enough drugs to replace eliminated drugs damaged kidney
• Clearance is the most important parameter in defining o Adjust the dosage of the drug - lower dose is needed for patients
rational drug dosage with kidney problems to avoid toxicity
o No reliable indicator for liver function
VOLUME OF DISTRIBUTION
o Decreased Vd - binding to plasma proteins
o Increased Vd - binding to tissues
o Increased Vd - drug distributed to body waters, extracellular
accumulation of body fluids
HALF-LIFE
o Clearance and volume of distribution
PHARMACODYNAMIC VARIABLES
MAXIMUM EFFECT
o Emax
o No more increase in effect even if the concentration is
increasing
MEL, JCM, BGT, EFL, CJC | 2F-PH 5
PHARMACOLOGY I
Lecture \ SECOND SEMESTER
UNIT/LESSON XX: PHARMACOKINETICS AND PHARMACODYNAMICS
o Example: Emax = 1000mg at 95%; increasing the dose will not • Average total amount of drug in the body does not change
increase the effect over multiple dosing intervals
SENSITIVITY • Rate of drug input equals the rate of elimination
o Increased, exaggerated response to small doses • Condition in 3 to 4 t½ must elapse before checking drug
blood concentration
PLASMA BINDING PROTEIN • Drugs given intermittently are in steady state of
• More highly protein bound drug will displace the less protein concentration
bound drug
• Inert
• A - 90% protein bound
• B - 50% protein bound
• A will displace B
• More unbound drug to act on the receptor site
o Pag hindi naka-bind sa protein, mas maraming mag-bind
sa receptor site
o More protein bound, less therapeutic effect
• Acidic drugs bind to albumin
• Graph:
o Relationship of frequency of dosing and maximum
• Basic drugs bind to alpha 1 acid glycoprotein and minimum plasma concentrations when a
• Most appropriate time to measure drug concentration steady state of the drug (Theophylline) plasma
o Absorption is complete level of 10mg/L is desired
o 2 hours after the dose o Black line - plasma concentration achieved with an
STEADY STATE CONCENTRATION intravenous infusion of 28 mg/hr; mean steady
state
• Graph:
o Orange line - 224mg/8hr
o Time course of the drug accumulation and elimination o Blue line - 672 mg/24hr
o Red line - plasma concentrations reflecting the drug
accumulation during a constant rate infusion of a drug THERAPEUTIC WINDOW
▪ 50% of the steady state concentration is reached • Safe “opening” between the MEC and the MTC of the drug
after one half-life • Used to determine the range of plasma levels that is
▪ 75% of the steady state concentration is reached acceptable when designing a dosing regimen
after two half-lives
▪ Over 90 of the steady state concentration is PEAK AND THROUGH CONCENTRATION
reached after three to four half-lives • Safe “opening” between the MEC and the MTC of the drug
▪ 100% steady state concentration is reached after
five half-lives
• Used to determine the range of plasma levels that is
acceptable when designing a dosing regimen
▪ If the drug’s half-life is 12 hours, steady-state
concentration and full therapeutic effect will be • MEC determines the desired trough levels of a drug given
reached after 2.5 days intermittently
o Dash-lines - after a constant rate of infusion of a drug • MTC determines the permissible peak plasma concentration
has reached the steady state • Maximum and minimum drug concentrations – in plasma or
▪ After 5 half-lives, the drug will be eliminated blood measured during cycles of repeated dosing
▪ Dose in dose out
o Rule of thumb - after 4 half-lives (at fifth half-life), it must
elapse first after the starting drug dosing regimen before
the full effects will be seen on the approach of the
accumulation curve to over 90% of the final steady state
concentration
MEL, JCM, BGT, EFL, CJC | 2F-PH 6
You might also like
- Kinetik LengkapDocument133 pagesKinetik Lengkapreczky HasanNo ratings yet
- 02. Individualisasi DosisDocument30 pages02. Individualisasi DosisSoshi DaysNo ratings yet
- 2.1 Pharmacokinetics Distribution and MetabolismDocument4 pages2.1 Pharmacokinetics Distribution and MetabolismLloyd Selorio ArboledaNo ratings yet
- Pharmacology Block 1.4 - PharmacokineticsDocument9 pagesPharmacology Block 1.4 - Pharmacokineticsdaleng subNo ratings yet
- introduction (1) (1)Document56 pagesintroduction (1) (1)samrawitmekonnen16No ratings yet
- Biomedical Nanotechnology: Lecture 17: Nanopharmacology & Drug TargetingDocument65 pagesBiomedical Nanotechnology: Lecture 17: Nanopharmacology & Drug TargetingDURGA DEVI T 037 BMENo ratings yet
- Pharma Chapter 5 PDFDocument60 pagesPharma Chapter 5 PDF爾雅雷No ratings yet
- Lec1 - Introduction To Pharmacology - 1Document38 pagesLec1 - Introduction To Pharmacology - 1ABDALRHMAN ABU ZAIDNo ratings yet
- Pharmacokinetics InformationDocument31 pagesPharmacokinetics InformationSyeda Ayesha FarhanaNo ratings yet
- 1 General PharmacologyDocument29 pages1 General PharmacologyAli EllaffiNo ratings yet
- Onset VS, Duration of Action Onset: The Time Required For The Drug Before A Duration of Action: The Span of Time WhereDocument4 pagesOnset VS, Duration of Action Onset: The Time Required For The Drug Before A Duration of Action: The Span of Time WhereAmaetenNo ratings yet
- TDM UtsDocument285 pagesTDM Utsnabila auliaNo ratings yet
- (Medicalstudyzone - Com) Pharmacology Image BankDocument112 pages(Medicalstudyzone - Com) Pharmacology Image BanktktanvirNo ratings yet
- _ue_migdadiu1614592452789Document32 pages_ue_migdadiu1614592452789osama2010bNo ratings yet
- 1628771279-Oral MR Systems All Slides 06dec23Document69 pages1628771279-Oral MR Systems All Slides 06dec23Riya moreNo ratings yet
- Pharmacokinetic Models MultiDocument79 pagesPharmacokinetic Models Multiuday sainiNo ratings yet
- Integrated Therapy (part-1)(2)Document350 pagesIntegrated Therapy (part-1)(2)samuel mergaNo ratings yet
- Unit-3 BPDocument48 pagesUnit-3 BPShreyas ShreyuNo ratings yet
- Therapeutic Drug Monitoring GuideDocument12 pagesTherapeutic Drug Monitoring GuideSharon GabrielNo ratings yet
- Prof. Dr. Darius P. Zlotos: Drug Substance (Active Pharmaceutical Ingredient API)Document24 pagesProf. Dr. Darius P. Zlotos: Drug Substance (Active Pharmaceutical Ingredient API)Mirette AshrafNo ratings yet
- Introduction To BiopharmaceuticsDocument29 pagesIntroduction To Biopharmaceuticssameermomin133No ratings yet
- Introduction To Biopharmaceutics and PharmacokineticsDocument29 pagesIntroduction To Biopharmaceutics and PharmacokineticsNasima Begum100% (1)
- Pharmacokinetics LectureDocument3 pagesPharmacokinetics LectureChristine Annmarie TapawanNo ratings yet
- Cc2lab TDM Part1Document3 pagesCc2lab TDM Part1Krisiah Anne HernandezNo ratings yet
- Clinical - Pharmacokinetics 3rd Year BushDocument53 pagesClinical - Pharmacokinetics 3rd Year BushBaguma MichaelNo ratings yet
- Introduction and Overview: ObjectivesDocument17 pagesIntroduction and Overview: Objectivesandreani temeNo ratings yet
- Pharmacokinetics Student VersionDocument25 pagesPharmacokinetics Student VersionShuruq SanchezNo ratings yet
- Pharmacokinetic Models: Submitted To: Dr. Satyabrata BhanjaDocument85 pagesPharmacokinetic Models: Submitted To: Dr. Satyabrata BhanjaBandameedi RamuNo ratings yet
- Physicochemical Properties of The Drug Dosage Form Route of AdministrationDocument10 pagesPhysicochemical Properties of The Drug Dosage Form Route of AdministrationFfs AccsNo ratings yet
- Compartment Modelling Upto IV InfusionDocument42 pagesCompartment Modelling Upto IV Infusionuday sainiNo ratings yet
- Introduction to PharmacologyDocument59 pagesIntroduction to PharmacologyMoza AlanziNo ratings yet
- Principles of Clinical Pharmacology: Indications For Drug Therapy: Risk VersusDocument12 pagesPrinciples of Clinical Pharmacology: Indications For Drug Therapy: Risk VersusKenneth MiguelNo ratings yet
- Principles of Pharmacokinetics AbsorptionDocument10 pagesPrinciples of Pharmacokinetics AbsorptionMikmik DGNo ratings yet
- FarmakokinetikaDocument27 pagesFarmakokinetikaRanhie Pen'ned CendhirhieNo ratings yet
- PharmacologyDocument32 pagesPharmacologyHarleanne ParkNo ratings yet
- Drug Delivery SystemDocument78 pagesDrug Delivery SystemMd. Abu Bakar Siddique Tayef100% (1)
- Pharmacokinetic processes of drug absorption, distribution, metabolism and excretionDocument31 pagesPharmacokinetic processes of drug absorption, distribution, metabolism and excretionAli ElmehdawiNo ratings yet
- Bio PharmaceuticsDocument29 pagesBio Pharmaceuticsthedud123No ratings yet
- BioavailabilityDocument35 pagesBioavailabilityDr. Bharat JainNo ratings yet
- Per 1 - 4 Farmakologi UmumDocument98 pagesPer 1 - 4 Farmakologi UmumamaliahriskaikaNo ratings yet
- AbsorptionDocument84 pagesAbsorptionDr. Bharat JainNo ratings yet
- Unit 1, Part 4 Clin. PKDocument11 pagesUnit 1, Part 4 Clin. PKshammaNo ratings yet
- RUDs + PharmacokineticsDocument53 pagesRUDs + PharmacokineticsdaghameendoniaNo ratings yet
- Biopharmaceutics IntroductionDocument46 pagesBiopharmaceutics IntroductionMinal NadeemNo ratings yet
- Basic Concepts and Principles of PharmacokineticsDocument42 pagesBasic Concepts and Principles of PharmacokineticsSophia AgenyiNo ratings yet
- Anesthesia Pharmacology CompiledDocument106 pagesAnesthesia Pharmacology CompiledJovy Tan-AmodiaNo ratings yet
- 2021-8-31 PharmacokineticsDocument25 pages2021-8-31 PharmacokineticsNOT ZUXNo ratings yet
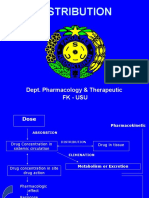
- Distribution: Dept. Pharmacology & Therapeutic FK - UsuDocument16 pagesDistribution: Dept. Pharmacology & Therapeutic FK - UsuSudirman ArbiNo ratings yet
- Concept of Drug Delivery SystemDocument60 pagesConcept of Drug Delivery SystemokNo ratings yet
- Clinical PharmacologDocument81 pagesClinical PharmacologSHILOTANo ratings yet
- 1 PHA6120 IntroductionDocument86 pages1 PHA6120 Introductionchristian redotaNo ratings yet
- Distribution: Dept. Pharmacology & Therapeutic FK - UsuDocument16 pagesDistribution: Dept. Pharmacology & Therapeutic FK - UsuagnesNo ratings yet
- Biopharmaceutics by Shehryar KhanDocument66 pagesBiopharmaceutics by Shehryar KhanAmna Saifullah100% (1)
- Cdds Unit 1.NddsDocument15 pagesCdds Unit 1.NddskblikithkumarNo ratings yet
- Adv. Biopharmaceutics All For VIvaDocument98 pagesAdv. Biopharmaceutics All For VIvaArvi KhanNo ratings yet
- Farmaco LectureDocument117 pagesFarmaco LectureanaNo ratings yet
- Pharmaco KineticsDocument427 pagesPharmaco KineticsMehrdad AvestaNo ratings yet
- Controlled Drug Delivery Systems 1.7Document35 pagesControlled Drug Delivery Systems 1.7sc5753972No ratings yet
- Pharmacology in Drug Discovery: Understanding Drug ResponseFrom EverandPharmacology in Drug Discovery: Understanding Drug ResponseNo ratings yet
- Antihypertensive AgentsDocument1 pageAntihypertensive Agentschristian redotaNo ratings yet
- Lec1 Intro To Pharmacology PD PK FinalDocument112 pagesLec1 Intro To Pharmacology PD PK Finalchristian redotaNo ratings yet
- PHA6118 Course Orientation Portfolio 2TAY2022-23 Salonga ForRevision v3Document25 pagesPHA6118 Course Orientation Portfolio 2TAY2022-23 Salonga ForRevision v3christian redotaNo ratings yet
- 1 PHA6120 IntroductionDocument86 pages1 PHA6120 Introductionchristian redotaNo ratings yet
- (PHA6118 Lec) Introduction To PharmacologyDocument5 pages(PHA6118 Lec) Introduction To Pharmacologychristian redotaNo ratings yet
- Christian's interview on Baptist beliefsDocument1 pageChristian's interview on Baptist beliefschristian redotaNo ratings yet
- 32 Redota, Christian Activity 10Document23 pages32 Redota, Christian Activity 10christian redotaNo ratings yet
- Theology 1Document3 pagesTheology 1christian redotaNo ratings yet
- ASSIGNMENT1Document1 pageASSIGNMENT1christian redotaNo ratings yet
- 32 - Redota, Christian-Activity 3Document3 pages32 - Redota, Christian-Activity 3christian redotaNo ratings yet
- 32 Redota, Christian Activity 9Document1 page32 Redota, Christian Activity 9christian redotaNo ratings yet
- 32 Redota, Christian Acitivty 8Document1 page32 Redota, Christian Acitivty 8christian redotaNo ratings yet
- pH Measurement and Buffer Preparation LabDocument32 pagespH Measurement and Buffer Preparation Labchristian redotaNo ratings yet
- 32 Redota, Christian Activity 6Document5 pages32 Redota, Christian Activity 6christian redotaNo ratings yet
- EM Activity Flow IdentificationDocument3 pagesEM Activity Flow Identificationchristian redotaNo ratings yet
- pH Measurement and Buffer Preparation LabDocument32 pagespH Measurement and Buffer Preparation Labchristian redotaNo ratings yet
- REDOTA - Globalization Around UsDocument1 pageREDOTA - Globalization Around Uschristian redotaNo ratings yet
- Amino Acids and Peptides HoDocument17 pagesAmino Acids and Peptides Hochristian redotaNo ratings yet
- Intro HoDocument14 pagesIntro Hochristian redotaNo ratings yet
- Proteins HODocument16 pagesProteins HOchristian redotaNo ratings yet
- Suvarnaprashana Therapy in Children ConcDocument3 pagesSuvarnaprashana Therapy in Children ConcBhavana GangurdeNo ratings yet
- HSS - Summer 2020 - Syllabus - ANTH 1667Document7 pagesHSS - Summer 2020 - Syllabus - ANTH 1667Bruce JobseNo ratings yet
- Nursing Care Plan For LEUKEMIASDocument12 pagesNursing Care Plan For LEUKEMIASMaverick LimNo ratings yet
- Treating Cholestatic Liver Diseases with UDCA and BeyondDocument35 pagesTreating Cholestatic Liver Diseases with UDCA and BeyondalnyhilwanyNo ratings yet
- Heart Failure - A Life Time Pills ConsumptionDocument29 pagesHeart Failure - A Life Time Pills ConsumptionTania LadoNo ratings yet
- A Industrial Training ReportDocument23 pagesA Industrial Training ReportSuzan patelNo ratings yet
- Online Book Reviews: Stockley's Drug Interactions, Eleventh EditionDocument1 pageOnline Book Reviews: Stockley's Drug Interactions, Eleventh Editionkehie HananielNo ratings yet
- Different Routes of Nursing Medication AdministrationDocument13 pagesDifferent Routes of Nursing Medication AdministrationRonica MendozaNo ratings yet
- F3 (Gangguan Suasana Perasaan - Mood)Document41 pagesF3 (Gangguan Suasana Perasaan - Mood)Nabilla RizkyNo ratings yet
- Music For Pain Relief - Binaural Beats Instant Download PDFDocument1 pageMusic For Pain Relief - Binaural Beats Instant Download PDFIoannis ManNo ratings yet
- 1 Analgetik Ketorolac: No Golongan Obat Nama GenerikDocument44 pages1 Analgetik Ketorolac: No Golongan Obat Nama GenerikHayu Ajeng A RNo ratings yet
- Management of Refeeding Syndrome in Medical Inpatients: Clinical MedicineDocument18 pagesManagement of Refeeding Syndrome in Medical Inpatients: Clinical MedicineThay SousaNo ratings yet
- Depression Since Prozac An Argument For Authenticity 2167 1044 1000298Document8 pagesDepression Since Prozac An Argument For Authenticity 2167 1044 1000298M CNo ratings yet
- Huraira Ehsan F17-0848 Bs Accounting and Finance 7 Semester Corporate Governance Sir Shiraz Ahmed 23/1/21Document9 pagesHuraira Ehsan F17-0848 Bs Accounting and Finance 7 Semester Corporate Governance Sir Shiraz Ahmed 23/1/21huraira ehsanNo ratings yet
- Toronto Sick KidsDocument13 pagesToronto Sick KidsAnonymous AuJncFVWvNo ratings yet
- Brunner and Suddarth's Textbook of Medical-Surgical Nursing 12th Ed. (Dragged) 6Document1 pageBrunner and Suddarth's Textbook of Medical-Surgical Nursing 12th Ed. (Dragged) 6jamie carpioNo ratings yet
- OETreadingVol1 2Document148 pagesOETreadingVol1 2GeorgianNeagu100% (1)
- Case Study on Chronic Pain and DepressionDocument5 pagesCase Study on Chronic Pain and DepressionClinton MandelaNo ratings yet
- Trimetazidine medication guideDocument2 pagesTrimetazidine medication guideJULIANNE BAYHON100% (1)
- Algoritma Handling NyeriDocument21 pagesAlgoritma Handling Nyeriscan resepNo ratings yet
- CHAPTER V Dangerous Drugs Full PresentationDocument105 pagesCHAPTER V Dangerous Drugs Full PresentationMark Angelo BauiNo ratings yet
- 1 Sumreen Case ReportDocument4 pages1 Sumreen Case ReportNosheen JavedNo ratings yet
- PhcogRev 3 5 143Document11 pagesPhcogRev 3 5 143yermi atiNo ratings yet
- PCOL TRivias 2Document3 pagesPCOL TRivias 2Maria Izabelle QuemiNo ratings yet
- Strategi Obat BCS IIIDocument20 pagesStrategi Obat BCS IIIVennyNo ratings yet
- St. Paul College of Ilocos SurDocument5 pagesSt. Paul College of Ilocos SurKelsey MacaraigNo ratings yet
- Iontophoresis:: Iontophoresis Along With Various Drugs UsedDocument6 pagesIontophoresis:: Iontophoresis Along With Various Drugs UsedApoorvNo ratings yet
- Biologics Immunogenicity Causes and ConsequencesDocument12 pagesBiologics Immunogenicity Causes and ConsequencesWei Sheng ChongNo ratings yet
- Allergic Rhinitis VASDocument5 pagesAllergic Rhinitis VASxtineNo ratings yet
- DiclofenacDocument14 pagesDiclofenacAyunda Nur Faiz'zaNo ratings yet