Professional Documents
Culture Documents
Covidarticle
Uploaded by
Angellie Laborte0 ratings0% found this document useful (0 votes)
10 views1 pageCovid article
Original Title
covidarticle.-
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCovid article
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
10 views1 pageCovidarticle
Uploaded by
Angellie LaborteCovid article
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 1
%
Philippines poorly prepared to
deal with COVID-19, report says
Download PDF Copy
By Angela Betsaida B. Laguipo, BSN
Jun 13 2021
Reviewed by Benedette Cuffari, M.Sc.
Despite an early coronavirus disease (COVID-
19) response against the severe acute
x
We use cookies to enhance your experience. By
respiratory
continuing tosyndrome
browse this coronavirus
site you agree2to(SARS-
our use
CoV-2),
of theFind
cookies. Philippines
out more
more.continues to grapple
with skyrocketing cases, which have reached
over 1.3 million
Cookie total casesAccept
Settings as ofAllJune 15,
Cookies
#
2021. $ ( * +
Study: Early response to COVID-19 in the
Philippines. Image Credit: aldarinho /
Shutterstock.com
Researchers at the College of Medicine at the
University of the Philippines Manila, along
with collaborators at the School of Medicine
and Public Health at the Ateneo de Manila
University, described the challenges and early
response of the Philippines to COVID-19. To
this end, the researchers focused on travel
restrictions, community interventions, risk
communication, and testing between January
30, 2020, which was when the first case in the
country was reported, and March 21, 2020.
In this peer-reviewed study, which was
published in the World Health Organization
(WHO)’s Western Pacific Surveillance and
Response Journal (WPSAR), the authors
discuss the surveillance of and response to
public health events in the Western Pacific
Region. Ultimately, the researchers concluded
that the Philippines’s initial response to the
COVID-19 pandemic lacked organizational
preparedness.
Public health emergencies in the
Philippines
As a developing country, the Philippines
experienced some improvements in its
healthcare system over the past decade.
Despite this, the country continues to face
various challenges in its response to public
health emergencies.
It is estimated that the Philippines has about
10 hospital beds and six doctors per 10,000
people which, taken together, amounts to
only 2,335 critical beds nationwide. Mainly,
the available healthcare resources are
focused in urban areas, while rural areas
experience a lack of available physicians.
Within these rural areas, only one physician is
available for a population of 20,000 people,
with only one bed available for a population
of 1,000.
Although community health centers and local
healthcare workers comprise the primary care
system in the nation, they are often poorly
resourced with limited surge capacity.
Furthermore, while local government has
disaster preparedness plans, these plans are
designed for natural calamities, which the
country often experiences, rather than for
disease outbreaks.
Travel restrictions
The first COVID-19 case in the Philippines was
reported on January 30, 2020. By March, the
cases rose significantly, which prompted the
government to put the northern part of the
country, Luzon, in an enhanced community
quarantine (ECQ) or lockdown by March 15.
The Philippine government implemented
travel restrictions as early as January 28, 2020.
While this prevented the spread of the virus,
travelers from areas that were not included
on the list of restricted countries were not
subject to stringent screening and quarantine
protocols. Meanwhile, those from restricted
countries were subjected to a 14-day
quarantine, testing, and contact tracing.
In the first few weeks after these restrictions
were put in place, the COVID-19 spread was
delayed. However, as time passed, COVID-19
cases began to rise due to viral transmission
within communities, particularly from people
who had no prior travel history.
Community interventions
RELATED STORIES
Mu SARS-CoV-2 variant highly resistant to
neutralization by convalescent and vaccinated
sera
Does SARS-CoV-2 natural infection immunity
better protect against the Delta variant than
vaccination?
What might the third wave of COVID-19 in India
look like?
When the lockdown or ECQ was implemented
in Luzon, which included Metro Manila,
families were placed on strict home
quarantine. This quarantine consisted of strict
home quarantine in all households, with the
exception of when individuals needed to
acquire essential food and health services.
Additional measurements that were
implemented during this time included work-
from-home schemes, suspension of classes
and distance learning instruction, closure of
public transport and non-essential business
establishments, as well as physical distancing
and the prohibition of public gatherings.
These measures successfully slowed the
spread of the virus; however, it was difficult
for the government to enforce these
restrictions for extended periods of time
because of their severe economic impacts.
Though the lockdown order was just for
Luzon Island, health systems were not
overwhelmed. In fact, the quarantine
regulations gave the Philippines the
opportunity to mobilize resources and
organize its pandemic response.
Risk communication
During the lockdown, the Philippine
government ensured that all plans and
information about the COVID-19 pandemic
would be distributed to all residents and
citizens. The government also strengthened
its national risk communication plans through
press briefings, internet advertisements,
health-related television advertisements, and
infographics on social media.
Despite these efforts, misinformation and
conspiracy theories about COVID-19 emerged
in the Philippines.
Testing
Many countries that were successful in
containing the COVID-19 pandemic
implemented widespread testing. While
testing is key to controlling the pandemic, the
Philippines only performed COVID-19 testing
on a small scale. More specifically, the authors
of the current paper found that by March 19,
2020, fewer than 1,200 people in this nation
had been tested for COVID-19, with the
Research Institute for Tropical Medicine in
Metro Manila being the only institution that
was capable of performing these tests. Due to
the limited capacity of the healthcare system
to conduct mass testing, the Department of
Health (DOH) recommended rationed testing,
wherein strict protocols were implemented.
Study takeaways
The authors of the current study concluded
that the Philippines was not ready for a
pandemic. The disease surveillance system
could conduct contact tracing and, for several
months at the beginning of the pandemic,
only one laboratory was available for COVID-
19 testing. Furthermore, the primary
healthcare system did not serve as a primary
line of defense, which led infected people to
flock to hospitals in cities, thus overwhelming
the healthcare system and critical care
capacity.
&
“The lack of pandemic preparedness had
left the country poorly defended against
the new virus and its devastating effects.
Investing diligently and consistently in
pandemic prepared.”
Taken together, the researchers noted that
the lack of pandemic preparedness had left
the Philippines poorly protected from the
effects of SARS-CoV-2. The pandemic,
therefore, taught the Philippines, as well as
many other nations around the world, that
increasing its investment in the
modernization of hospitals and clinics is
crucial for protecting its citizens against
disease outbreaks in the future. This
investment should also be accompanied by
the development of adequate surveillance,
testing, and contact tracing services.
Journal reference:
Amit, A.M., Pepito, V.C., and Dayrit, Manuel.
(2021). Early response to COVID-19 in the
Philippines. World Health Organization
(WHO)’s Western Pacific Surveillance and
Response Journal (WPSAR) 12(2).
doi:10.5365/wpsar.2020.11.014.
https://ojs.wpro.who.int/ojs/index.php/wps
ar/article/view/725.
Written by
Angela Betsaida B. Laguipo
Angela is a nurse by profession and a writer by
heart. She graduated with honors (Cum
Laude) for her Bachelor of Nursing degree at
the University of Baguio, Philippines. She is
currently completing her Master's Degree
where she specialized in Maternal and Child
Nursing and worked as a clinical instructor
and educator in the School of Nursing at the
University of Baguio.
" Add a comment
Download PDF Copy
Citations ○
! back to top
# $
News-Medical.Net provides this medical information
service in accordance with these terms and conditions.
Please note that medical information found on this
website is designed to support, not to replace the
relationship between patient and physician/doctor and
the medical advice they may provide.
This site complies with the HONcode standard for
trustworthy health information: verify here.
News-Medical.net - An AZoNetwork Site
Owned and operated by AZoNetwork, © 2000-2021
You might also like
- Covid 19 ReportDocument4 pagesCovid 19 ReportJeancy SenosinNo ratings yet
- Position Paper - WHO PhilippinesDocument2 pagesPosition Paper - WHO PhilippinesMonica AnggiNo ratings yet
- Theo 4 ResearchDocument20 pagesTheo 4 ResearchPaulo De BorjaNo ratings yet
- Group 5humss12a Pinakafinal-Imradres03 2Document22 pagesGroup 5humss12a Pinakafinal-Imradres03 2Juliane FloresNo ratings yet
- Republic of The Philippines (Address of School) (Name of School)Document3 pagesRepublic of The Philippines (Address of School) (Name of School)siahkyNo ratings yet
- Doh Covid 19 ResponseDocument5 pagesDoh Covid 19 ResponseTheresa Mae PansaonNo ratings yet
- NCM 112 B: in Partial Fulfillment For Related Learning ExperienceDocument16 pagesNCM 112 B: in Partial Fulfillment For Related Learning ExperienceSiiti Hajar AukasaNo ratings yet
- Covid 19Document18 pagesCovid 19Jeremy FayeNo ratings yet
- Is The Pandemic Ending SoonDocument1 pageIs The Pandemic Ending SoonShela Mae Ondo CaracolNo ratings yet
- Argumentative EssayDocument5 pagesArgumentative EssayLiam GalbanNo ratings yet
- Position Paper - Whether The Government Acted Well in The COVID 19 PandemicDocument7 pagesPosition Paper - Whether The Government Acted Well in The COVID 19 PandemicSunshine ALpine100% (1)
- Vaccines and Routine Immunization Strategies During The COVID 19 PandemicDocument9 pagesVaccines and Routine Immunization Strategies During The COVID 19 PandemicMěđ SimoNo ratings yet
- Assessment 3 Miranda Bsma1 6 PDFDocument4 pagesAssessment 3 Miranda Bsma1 6 PDFEloise Dorothy PatiñoNo ratings yet
- Reporting On National and Global Health SituationsDocument9 pagesReporting On National and Global Health SituationsEvelyn MedinaNo ratings yet
- The Effects of COVID 19 Pandemic Outbreak On Food Consumption Preferences and Their Causes-With-Cover-Page-V2Document6 pagesThe Effects of COVID 19 Pandemic Outbreak On Food Consumption Preferences and Their Causes-With-Cover-Page-V2Jecel LazarraNo ratings yet
- Healthcare in Ghana Amidst The Coronavirus Pandemic: A Narrative Literature ReviewDocument5 pagesHealthcare in Ghana Amidst The Coronavirus Pandemic: A Narrative Literature ReviewSignor 2019No ratings yet
- Knowledge and Attitudes Towards COVID-19 Vaccines Among University Students, Faculty Members and StaffsDocument9 pagesKnowledge and Attitudes Towards COVID-19 Vaccines Among University Students, Faculty Members and StaffsIJPHSNo ratings yet
- Knowledge About COVID-19 Among University Students Before The Implementation of The Enhanced Community Quarantine in PhilippinesDocument8 pagesKnowledge About COVID-19 Among University Students Before The Implementation of The Enhanced Community Quarantine in PhilippinesIJPHSNo ratings yet
- SWOT of PandemicDocument4 pagesSWOT of PandemicAizeahrhey RayoNo ratings yet
- Philippines Covid-19 Emergency ResponseDocument12 pagesPhilippines Covid-19 Emergency ResponseMia Grace Edaño RosellosaNo ratings yet
- Research Chapter 1 3Document13 pagesResearch Chapter 1 3Kimberly MataviaNo ratings yet
- When Will The COVID-19 Pandemic in Indonesia End?: Dewi SusannaDocument3 pagesWhen Will The COVID-19 Pandemic in Indonesia End?: Dewi SusannatiaranindyNo ratings yet
- Bacolod, Queen Elizabeth G. Bsn3A ESSAY About Community Health Network System in The PhilippinesDocument2 pagesBacolod, Queen Elizabeth G. Bsn3A ESSAY About Community Health Network System in The PhilippinesQueenie BacolodNo ratings yet
- Case-Analysis-Grp9-Bsn-3-C 2Document11 pagesCase-Analysis-Grp9-Bsn-3-C 2api-529900010100% (1)
- OIQAG X LGSO Reasearch Study - COVID 19 PandemicDocument47 pagesOIQAG X LGSO Reasearch Study - COVID 19 PandemicNikko Valle100% (1)
- GovernanceDocument3 pagesGovernanceCris Joy BiabasNo ratings yet
- The Information-Seeking Behavior and Levels of Knowledge, Precaution, and Fear of College Students in Iloilo, Philippines Amidst The COVID-19 PandemicDocument15 pagesThe Information-Seeking Behavior and Levels of Knowledge, Precaution, and Fear of College Students in Iloilo, Philippines Amidst The COVID-19 PandemicBarangay MotibotNo ratings yet
- CASE STUDY. Government ResponsesDocument24 pagesCASE STUDY. Government ResponsesjoloaretaNo ratings yet
- PR 1 PT1 OUTLINE 1lesson 1Document4 pagesPR 1 PT1 OUTLINE 1lesson 1Rosalie CondezaNo ratings yet
- Effectiveness of Covid 19 ResearchDocument9 pagesEffectiveness of Covid 19 ResearchAinah Faith LegaspiNo ratings yet
- Final Requirement (FINAL EXAM)Document4 pagesFinal Requirement (FINAL EXAM)KATHLEEN JOSOLNo ratings yet
- Management of Parenting Preparedness at Home in COVID-2019 Pandemic Based On Individual and Family Self - Management Theory (IFSMT) : A Systematic ReviewDocument10 pagesManagement of Parenting Preparedness at Home in COVID-2019 Pandemic Based On Individual and Family Self - Management Theory (IFSMT) : A Systematic Reviewsha ditaNo ratings yet
- Narrative ReportDocument56 pagesNarrative ReportJesus MananganNo ratings yet
- Elizabeth C. BernardinoDocument6 pagesElizabeth C. BernardinoKiko BernardinoNo ratings yet
- PHM Philippines Case Study For PHM Health Systems Circle Oct 16 2020Document16 pagesPHM Philippines Case Study For PHM Health Systems Circle Oct 16 2020Aleonore EscaladesNo ratings yet
- Tan-Contemp World Final ProductDocument6 pagesTan-Contemp World Final Productjemimahvlogs11No ratings yet
- Philippine's Healthcare System During The PandemicDocument1 pagePhilippine's Healthcare System During The PandemicMaria Erica Jan MirandaNo ratings yet
- CITATION Bau21 /L 1033Document3 pagesCITATION Bau21 /L 1033Kainan Ni BaTangNo ratings yet
- Assignment No. 29Document4 pagesAssignment No. 29Chilton John DuatNo ratings yet
- AM-On Suspension of Classes Due To COVID-19Document6 pagesAM-On Suspension of Classes Due To COVID-19Zeyt MayNo ratings yet
- Como A Pandemia de COVID-19 Mudou As Atitudes de Vacinação Contra A Gripe Entre Os Profissionais de Saúde de Um Centro de Câncer ItalianoDocument7 pagesComo A Pandemia de COVID-19 Mudou As Atitudes de Vacinação Contra A Gripe Entre Os Profissionais de Saúde de Um Centro de Câncer ItalianoArquivo FisioNo ratings yet
- Corona VirusDocument7 pagesCorona VirusAndreNo ratings yet
- Epidemiological Characteristics of An Outbreak of Coronavirus Disease 2019 in The PhilippinesDocument6 pagesEpidemiological Characteristics of An Outbreak of Coronavirus Disease 2019 in The PhilippinesherrerachaimNo ratings yet
- Factors Affecting COVID-19 Vaccine Hesitancy Among Senior High Schools StudentsDocument18 pagesFactors Affecting COVID-19 Vaccine Hesitancy Among Senior High Schools StudentsNicko TabanaoNo ratings yet
- Journal 2Document2 pagesJournal 2Atabay, Jessie Rey R.No ratings yet
- Choose 2 From The Disease Below That Are Emerging in The PhilippinesDocument4 pagesChoose 2 From The Disease Below That Are Emerging in The PhilippinesMICHELLE BIANCA PATRICE CRUZNo ratings yet
- Impact of Pandemic in The Lives of Filipinos': Final Project in NSTP 1Document15 pagesImpact of Pandemic in The Lives of Filipinos': Final Project in NSTP 1Jashi SiosonNo ratings yet
- Impact of Pandemic in The Lives of Filipinos': Final Project in NSTP 1Document15 pagesImpact of Pandemic in The Lives of Filipinos': Final Project in NSTP 1Jashi SiosonNo ratings yet
- Coronavirus - The Situation in Philippines: Learning Activity Sheet #03Document9 pagesCoronavirus - The Situation in Philippines: Learning Activity Sheet #03Juliana SottoNo ratings yet
- Title: The Acceptance and Attitudes of Students Toward Covid-19 VaccineDocument5 pagesTitle: The Acceptance and Attitudes of Students Toward Covid-19 VaccineJoanah Nichole TinoyNo ratings yet
- Activity 1 DRRRDocument2 pagesActivity 1 DRRRFried ChickenNo ratings yet
- Caring Amidst The Pandemic: Struggles of The Medical Frontliners in A Designated Covid-19 Hospital in The PhilippinesDocument7 pagesCaring Amidst The Pandemic: Struggles of The Medical Frontliners in A Designated Covid-19 Hospital in The PhilippinesEden LacsonNo ratings yet
- Chapter I IiDocument26 pagesChapter I IiAron JaroNo ratings yet
- The Major Effects of Covid-19 in The PhilippinesDocument8 pagesThe Major Effects of Covid-19 in The PhilippinesRafael ArchieNo ratings yet
- Apa 109 1932Document2 pagesApa 109 1932Gabriela Wakim SchiesslNo ratings yet
- Ged104 Module1 PaperDocument3 pagesGed104 Module1 PaperAdolf HitlerNo ratings yet
- Villaflor Draft Med ResDocument3 pagesVillaflor Draft Med ResAileen SiaNo ratings yet
- Degree of Acceptance of Residents Barangay Bibincahan To Vaccination Program of The Philippine GovernmentDocument6 pagesDegree of Acceptance of Residents Barangay Bibincahan To Vaccination Program of The Philippine GovernmentRJ DealcaNo ratings yet
- Covid 19 Last Patients Leave Hospital AfterDocument2 pagesCovid 19 Last Patients Leave Hospital AfterAngellie LaborteNo ratings yet
- Analysis Paper: Christ The King College de Maranding Inc. Maranding, Lala, Lanao Del NorteDocument10 pagesAnalysis Paper: Christ The King College de Maranding Inc. Maranding, Lala, Lanao Del NorteAngellie LaborteNo ratings yet
- Crisis Since World War II. Imagine That It Killed 274,898 People Worldwide in SixDocument2 pagesCrisis Since World War II. Imagine That It Killed 274,898 People Worldwide in SixAngellie LaborteNo ratings yet
- TREN CorporationDocument2 pagesTREN CorporationAngellie Laborte100% (1)
- Financial Management Their AnalysisDocument22 pagesFinancial Management Their AnalysisAngellie LaborteNo ratings yet
- 22-05-2021 HMB EnglishDocument137 pages22-05-2021 HMB EnglishKiran SNNo ratings yet
- 24-06-2020 HMB EnglishDocument20 pages24-06-2020 HMB EnglishRakshith GowdaNo ratings yet
- 3 Artikel Pak WiDocument3 pages3 Artikel Pak WiMirken DebyNo ratings yet
- What Else? 2 SentencesDocument3 pagesWhat Else? 2 SentencesMarvin Medem LaquidanNo ratings yet
- Maklumat Vaksinasi: Vaccination DetailsDocument2 pagesMaklumat Vaksinasi: Vaccination DetailscottonNo ratings yet
- President Rodrigo DuterteDocument1 pagePresident Rodrigo DuterteBea Garcia AspuriaNo ratings yet
- Nhs Covid Pass - Vaccinated: Covid-19 Vaccine Astrazeneca Covid-19 Vaccine AstrazenecaDocument1 pageNhs Covid Pass - Vaccinated: Covid-19 Vaccine Astrazeneca Covid-19 Vaccine AstrazenecaSHWE LINo ratings yet
- Physical Education and Health: PretestDocument4 pagesPhysical Education and Health: PretestDemosthenes RemoralNo ratings yet
- Certificate For COVID-19 Vaccination: Beneficiary DetailsDocument1 pageCertificate For COVID-19 Vaccination: Beneficiary DetailsGlobal printNo ratings yet
- NursalamDocument2 pagesNursalamAdipar AadNo ratings yet
- Autonomous Institute Affiliated To Mumbai University: CGPA: 3.02 Grade A (Validity Extension Up To 2025-26)Document5 pagesAutonomous Institute Affiliated To Mumbai University: CGPA: 3.02 Grade A (Validity Extension Up To 2025-26)Anand PandeyNo ratings yet
- My Life With COVID-19 Comic Strip PrintableDocument13 pagesMy Life With COVID-19 Comic Strip PrintableHannah Grace VallespinNo ratings yet
- 14.falra Rachmadiva - Xii Mipa 3 - Tugas Pertemuan 4 KD 3.6Document3 pages14.falra Rachmadiva - Xii Mipa 3 - Tugas Pertemuan 4 KD 3.6TasyaNo ratings yet
- HSE Bulletin # 84: Break The Chain of Corona Virus Transmission Stay Safe & Stay at HomeDocument1 pageHSE Bulletin # 84: Break The Chain of Corona Virus Transmission Stay Safe & Stay at HomeAbdus SamadNo ratings yet
- Group 2 - Tool Practice 02Document6 pagesGroup 2 - Tool Practice 02Gian Carlo CalixtoNo ratings yet
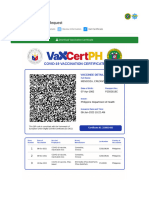
- VAXCert PHDocument2 pagesVAXCert PHvhide23No ratings yet
- Assignment On Hospitality IndustryDocument1 pageAssignment On Hospitality IndustryRohini PandeyNo ratings yet
- Navi Mumbai: Kamothe Police Conduct Raid at Hookah Parlour, 31 Including Four Women BookedDocument3 pagesNavi Mumbai: Kamothe Police Conduct Raid at Hookah Parlour, 31 Including Four Women BookedSatya YadavNo ratings yet
- Situation of Covid-19 Pandemic in The Philippines: Lyren Hope A. PujidaDocument5 pagesSituation of Covid-19 Pandemic in The Philippines: Lyren Hope A. PujidaLovella PujidaNo ratings yet
- Reflection Paper On The WebinarDocument2 pagesReflection Paper On The WebinarAngel Cuacko GacmatanNo ratings yet
- Glt1009 Final Copy RC Ebola Week 14Document4 pagesGlt1009 Final Copy RC Ebola Week 14shahiraNo ratings yet
- Covid-19 Pandemic: Jump To Navigationjump To SearchDocument4 pagesCovid-19 Pandemic: Jump To Navigationjump To SearchGoran SNo ratings yet
- CertificateDocument1 pageCertificateManish AbbaniNo ratings yet
- Format PENCATATAN TGL 11-1-2022 AKUN PUSKESMASDocument11 pagesFormat PENCATATAN TGL 11-1-2022 AKUN PUSKESMASsoebirinNo ratings yet
- Baguio City News On GuidelinesDocument2 pagesBaguio City News On GuidelinesLesly BriesNo ratings yet
- Certificate For COVID-19 Vaccination: Beneficiary DetailsDocument1 pageCertificate For COVID-19 Vaccination: Beneficiary DetailsLakshya NagotaNo ratings yet
- Certificate For COVID-19 Vaccination: Beneficiary DetailsDocument1 pageCertificate For COVID-19 Vaccination: Beneficiary Detailsuday xeroxNo ratings yet
- Safety Seal Requirements For Face-To-face Classes Sy 2021-2022 - Attachments & AnnexesDocument83 pagesSafety Seal Requirements For Face-To-face Classes Sy 2021-2022 - Attachments & AnnexesMichelle Ann SoledadNo ratings yet
- lc042 Time To Shake Hands AgainDocument2 pageslc042 Time To Shake Hands Againadulea20No ratings yet
- Coronavirus (COVID-19) RecordsDocument3 pagesCoronavirus (COVID-19) RecordsTestertNo ratings yet