Professional Documents
Culture Documents
REviewarticle
Uploaded by
Imin BuntaraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
REviewarticle
Uploaded by
Imin BuntaraCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/342437204
Management of Postoperative Neurosurgical Patients
Article in Journal of Neuroanaesthesiology and Critical Care · June 2019
DOI: 10.1055/s-0039-1689055
CITATIONS READS
2 2,568
3 authors, including:
Nidhi Panda Rajeev Chauhan
Postgraduate Institute of Medical Education and Research Postgraduate Institute of Medical Education and Research
128 PUBLICATIONS 698 CITATIONS 80 PUBLICATIONS 43 CITATIONS
SEE PROFILE SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Letter to Editor View project
Intracranial Anuerysm View project
All content following this page was uploaded by Rajeev Chauhan on 25 June 2020.
The user has requested enhancement of the downloaded file.
Published online: 06.06.2019
THIEME
80 Review Article
Management of Postoperative Neurosurgical Patients
Nidhi B. Panda1 Shalvi Mahajan2 Rajeev Chauhan3
1 Division of Neuroanaesthesia, Department of Anaesthesia and Address for correspondence Nidhi B. Panda, MBBS, MD Anesthesia,
Intensive Care, Post Graduate Institute of Medical Education & Division of Neuroanaesthesia, Department of Anaesthesia and
Research (PGIMER), Chandigarh, Punjab, India Intensive Care, Post Graduate Institute of Medical Education &
2 Department of Anesthesia and Intensive Care, Fortis Hospital, Research (PGIMER), Chandigarh 160012, Punjab, India
Mohali, Punjab, India (e-mail: nidhibp@gmail.com).
3 Department of Anaesthesia and Intensive Care, Post Graduate
Institute of Medical Education & Research (PGIMER), Chandigarh,
Punjab, India
J Neuroanaesthesiol Crit Care 2019;6:80–86
Abstract Neurosurgical patients are a special subset of patients requiring postoperative care.
Challenging neurosurgical disease processes, advanced surgical techniques, and unique
individual patient requirements advocate the need for meticulous postoperative care to
ensure safe transition toward recovery. Timely detection of systemic and neurological
changes allows early diagnostic and therapeutic interventions. The mainstay of
Keywords postoperative care revolves around airway, maintenance of hemodynamics, sedation,
►►neurocritical care analgesia, nutrition, fluid management, and management of disease-specific
►►aneurysmal subarach- complications. In addition to standard monitoring, multimodal neuromonitoring
noid hemorrhage should be used in neurosurgical patients. Hence, four key elements in the postoperative
►►traumatic brain injury management of neurosurgical patients involve profound insight, rapid response, good
►►neurosurgery communication skills, and team collaboration.
Introduction surgery (>6 hours) and major blood loss with hemodynamic
instability, extensive posterior fossa surgery involving cranial
The concept of dedicated neurocritical care (NCC) unit was nerves and brain stem, arteriovenous malformation (AVM)
conceived late back in the 1900s.1 NCC is a specialized critical resection with chances of postoperative malignant edema, and
care unit staffed by a team comprising neurosurgeons, neu- vascular surgery with significant brain ischemia.
rointensivists, neurophysiologists, specialized nursing staff, Although the incidence of perioperative mortality is less
physiotherapists (respiratory and rehabilitation), and nutri- than 2%, medical and neurologic complications may occur
tionists. Studies have reported positive results and better in the postoperative period in up to 30% of cases. Therefore,
outcomes in patients managed postoperatively in NCC with perioperative complications must be identified and managed
aneurysmal subarachnoid hemorrhage (aSAH), stroke, before the patient’s neurologic and medical status is irreversibly
traumatic brain injury (TBI), and spine surgeries in terms of compromised. Various postoperative complications following
intensive care unit (ICU) stay and hospital discharge.2 brain surgery require admission in the NCC unit (►Table 1).
Criteria for Admission of Postoperative Assessment of Postoperative Neurosurgical
Neurosurgical Patients in NCC Unit Patients
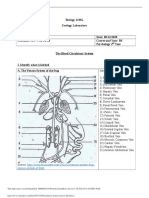
Postoperative neurosurgical patients can be grouped into Standardized systemic examination, neurological assess-
elective and emergency categories based on their presenta- ment, and neuromonitoring are valuable to recognize early
tion. Admission in the NCC unit following neurosurgical deterioration in the postoperative period (►Fig. 1).
procedure is dictated by patient’s neurologic and medical General physical examination and close monitoring
condition. Certain preoperative and intraoperative factors may of electrocardiogram (ECG), peripheral capillary oxygen
determine the need for postoperative ICU care, which include saturation (SpO2), blood pressure (invasive and noninva-
preoperative altered consciousness, prolonged duration of sive), temperature, central venous pressure along with
received DOI https://doi.org/ Copyright ©2019 Indian Society of
April 3, 2019 10.1055/s-0039-1689055 Neuroanaesthesiology and Critical
accepted after revision ISSN 2348-0548. Care
April 5, 2019
published online
June 6, 2019
Management of Postoperative Neurosurgical Patients Panda et al. 81
Table 1 Postoperative complications in neurosurgical patients It measures cerebral blood flow velocities and other derived
indices (pulsatility index) which help in the diagnosis of
Systemic Neurological
cerebral vasospasm and hyperemia.7 TCD can also be used
Hypoxia Cerebral edema to assess pressure autoregulation, cerebrovascular carbon
Hypotension/hypertension Hematoma/rebleeding dioxide reactivity, and noninvasive estimation of ICP.
Hypocapnia/hypercapnia Hydrocephalus Cerebral oxygenation can be assessed using jugular venous
Hyperthermia Pneumocephalus oximetry, cerebral oximetry, and brain tissue oxygenation.8
Jugular venous oximetry is an invasive method to measure
Hyperglycemia/hypoglycemia Seizures
oxygen saturation of the venous blood at the jugular bulb
Hyponatremia/hypernatremia Delayed cerebral and provides information of global oxygen extraction of the
ischemia
cerebral tissues. Cerebral oximetry is a noninvasive continuous
Coagulation disorders Central nervous system technique to measure regional cerebral oxygenation using
infections
near-infrared spectroscopic technique. Brain tissue oxygen
Thromboembolic events (DVT/PE) monitoring represents oxygen available at focal cerebral
Anemia mitochondrial level for oxidative phosphorylation.
Cerebral microdialysis allows monitoring of metabolic
Abbreviations: DVT, deep vein thrombosis; PE, pulmonary embolism.
milieu of brain tissue (glucose, lactate, pyruvate, glycerol,
measurement of serum electrolytes, osmolality, blood glutamate, cytokines, neurotrophic, and other neuronal
glucose, and arterial blood gases are necessary. Priority markers). However, it is not widely used for clinical purposes.9
management in NCC is prompt stabilization of all vital
parameters to prevent secondary neurological insult. General Management Goals of Postoperative
Neurological examination involves assessment of general Patients in Neurocritical Care Units
responsiveness (by Glasgow Coma Score [GCS], full outline
Postoperative complications following neurosurgical pro-
of unresponsiveness [FOUR] score), pupils, cranial nerve
cedures are mainly associated with the basic pathology
function, reflexes, and motor power. The functional scoring
of the disease or the sequel of intraoperative surgical and
systems are indispensable since they help in assessing neuro-
anesthetic techniques. Inability to rescue a patient from
logical status quantitatively and comparing neurological status
potentially reversible complications is an important reason
with previous assessment. The most commonly used score in
of perioperative morbidity and mortality (►Fig. 2).
neurological patients is GCS.3 The FOUR score was introduced
by Dr. Eelco F. M. Wijdicks for the assessment of patients with
impaired level of consciousness. It offers information about
brainstem reflexes (pupil, corneal, and cough), respiration
(breathing patterns, respiratory drive while on ventilator),
visual tracking (eye component), and motor response.4 It does
not take into account verbal component as in GCS.
Neuromonitoring: The concept of modern multimodal
neuromonitoring has shifted from rigid physiological
target-based approach to a more patient-specific approach.
Multimodal neuromonitoring helps in early identification
of pathophysiological indicators of secondary brain injury.
Hence, it is imperative for the neurointensivist to intervene
at the earliest before permanent neural cell death occurs.
Intracranial pressure (ICP), cerebral blood flow, brain
Fig. 1 Postoperative monitoring in neurosurgical patients. FOUR,
oxygenation, electrophysiology, and neuroimaging are full outline of unresponsiveness; GCS, Glasgow Coma Score; ICP,
indispensable components of neuromonitoring. intracranial pressure.
In many intracranial events, raised ICP and low cerebral
perfusion pressure (CPP) cause cerebral ischemia. ICP
monitoring is an important component of multimodal
neuromonitoring and helps in maintaining CPP. There are
both invasive and noninvasive monitoring techniques.
The gold standard technique is intraventricular pressure
monitoring, which has the added advantage of draining
cerebrospinal fluid (CSF) and administering intraventricular
medications.5 The commonly used noninvasive method of
ICP monitoring is measurement of optic nerve sheath
diameter using ultrasound.6
Cerebral blood flow can be monitored noninvasively in Fig. 2 Key elements in the management of postoperative neuro-
the postoperative period using transcranial Doppler (TCD). surgical patients.
Journal of Neuroanaesthesiology and Critical Care Vol. 6 No. 2/2019
82 Management of Postoperative Neurosurgical Patients Panda et al.
Airway Management and Ventilation Postoperative hypotension should be adequately treated
In patients with preoperative GCS < 8, lower cranial nerve with fluids and vasopressors. Hypotension causes a decrease
dysfunction, and weak gag and cough reflexes, the airway in the cerebral blood flow and CPP, which results in reflex
may need to be secured. Airway obstruction may be seen vasodilatation, increased cerebral blood volume, and high
in the postoperative period in acromegaly patients (due to ICP. Both increase in ICP and decrease in CPP in the
macroglossia and obstructive sleep apnea). Postoperative postoperative period are disastrous in terms of neurological
patients following anterior cervical spine surgery or carotid outcome.
endarterectomy may also present with airway obstruction Cardiac changes are well-known after acute brain insult.15
due to edema or hematoma. Irregular breathing pattern is Meticulous monitoring of ECG for arrhythmias and myocardial
common postoperatively in patients with posterior fossa or ischemia should be done. Biomarkers of cardiac injury
brain stem lesions. Acute brain insult may cause neurogenic (cardiac troponin I, creatine phosphokinase-myocardial
pulmonary edema (NPE).10 fraction [CK-MB], and serum B-type natriuretic peptide) can
The benefit of securing airway and elective ventilation be elevated after neurosurgeries. Cardiac troponin I is more
is to avoid hypoxia and hypercapnia, both of which aggra- sensitive for the detection of left ventricle dysfunction than
vate neuronal injury in postoperative period. Hence, CK-MB and high levels are associated with poor functional
arterial oxygen and carbon dioxide levels must be outcome in survivors. Partial or even complete resolution of
monitored regularly. A single episode of hypoxemia (SpO2 cardiac changes follows decrease in ICP. Echocardiography
< 90%, partial pressure of oxygen [PaO2] < 60 mm Hg) can show regional wall motion abnormalities, transient
increases the chance of adverse outcome by 40%11 left ventricular wall motion abnormalities involving apical
Partial pressure of carbon dioxide (PaCO2) is a powerful or mid-ventricular segments that extend beyond single
modulator of cerebrovascular resistance. Ventilation aims epicardial coronary artery distribution in SAH.16 Increased
to maintain PaCO2 levels within the normocapnic range. sympathetic activity seen in paroxysmal sympathetic
Hypoventilation may lead to cerebral hyperemia with hyperactivity has been associated with poor outcomes.17
increase in the cerebral blood volume and rise in ICP, while
hyperventilation increases the risk of vasoconstriction Postoperative Analgesia and Postoperative Nausea and
and tissue hypoxia. In the management of intracranial Vomiting
hypertension, hyperventilation strategies are useful to Most of the patients experience moderate-to-severe pain
decrease ICP. Hyperventilation is only useful as a short-term following major intracranial surgery for the first 48 hours.
strategy as pH of CSF gradually normalizes over 6 to 8 hours Patients undergoing foramen magnum decompression and
as a result of extrusion of bicarbonate. Volume-controlled acoustic neuroma resection are at a high risk to develop severe
ventilatory modes may be better for minimizing variations pain in the postoperative period.18 Adequate pain control
in PaCO2 levels. Positive end expiratory pressure (PEEP) of 5 ensures patient’s comfort, facilitates accurate neurological
to 8 cm H2O can be administered safely to prevent atelectasis. assessment, prevents increase in blood pressure, and allows
Patients with concurrent acute pulmonary injury need early recovery. Multimodal treatment with paracetamol,
protective pulmonary ventilation strategy with small tidal opioids, local anesthetic infiltration, and scalp block provides
volume and PEEP (up to 15 cm H2O).12 In patients with normal adequate analgesia in the postoperative period.
respiratory compliance, high PEEP increases intrathoracic The overall incidence of postoperative nausea and vomiting
pressure and jugular venous pressure, and decreases venous (PONV) following craniotomies is around 50%.19 PONV is
return (cardiac output) which can lead to decrease in CPP if common, especially after infratentorial surgery (foramen
cerebral autoregulation is impaired.13 But in patients with magnum decompression and acoustic neuroma resection).20
low respiratory compliance, significant effects of PEEP are Vomiting causes a rise in ICP due to systemic hypertension and
not seen on systemic and cerebral hemodynamics.14 increase in abdominal and intrathoracic pressure. Medications
Head up position: In neurosurgery patients, it is such as ondansetron, dexamethasone, cyclizine, and even
advantageous to keep patients in slight (15–30°) head up hyoscine patch can be used to prevent and treat PONV.
position so as to promote venous drainage and decrease
the risk of increase in ICP. Also, it helps in reducing risk of Postoperative Fluid and Electrolyte Disturbances
aspiration. Neurosurgical patients often exhibit changes in intravascular vol-
ume owing to use of potent diuretics, prolonged fasting, vomit-
Cardiovascular Changes and Management ing (raised ICP), hemorrhage, and electrolyte disturbances. The
Postoperative hypertension can precipitate cerebral edema, movement of water between brains extracellular area and ves-
intracranial hemorrhage as well as extracranial hemorrhage. sels is primarily driven by osmotic gradient. Use of hypo-osmo-
Therefore, strict control of blood pressure is essential in lar fluids such as 5% dextrose and 0.45% saline potentiate brain
hypertensive patients who have undergone intracranial edema, while hyperosmolar agents such as mannitol, glycer-
vascular surgery. Hypertension may be a part of Cushing ol, and hypertonic saline decrease cerebral edema. Hence in
reflex, or consequent to acute pain or hypercarbia. It is postoperative period, fluid status should be monitored using
reasonable to use invasive blood pressure monitoring in dynamic hemodynamic parameters, and isotonic crystalloids
such conditions in the postoperative period. should be used to maintain euvolemia.
Journal of Neuroanaesthesiology and Critical Care Vol. 6 No. 2/2019
Management of Postoperative Neurosurgical Patients Panda et al. 83
Sodium disturbance, either hypo- or hypernatremia, is Blood glycemic control: Extreme levels of blood glucose
the most common electrolyte disturbance in neurosurgical influence neurological outcome negatively. Glycemic control
patients.21 Intracranial diseases involving surgeries of the is affected in patients who receive corticosteroids as a part of
hypothalamus, pituitary, or cerebral trauma may cause hormone replacement therapy or as a decongestive measure
diabetes insipidus (DI). It is characterized by polyuria, to decrease vasogenic edema. Blood glucose management
hypernatremia, increased plasma osmolarity, decreased in neurosurgery tends toward moderate plasma glucose
urine specific gravity and osmolarity. Management involves level goals (140–180 mg/dL). The exact mechanism how
fluid and antidiuretic hormone (ADH) supplementation. hyperglycemia exacerbates ischemic neuronal injury is
Following brain insult (trauma or SAH), patients may suffer not clearly known but oxidative stress at cellular level is
from syndrome of inappropriate ADH secretion (SIADH) or implicated. Oxidative stress due to production of advanced
cerebral salt wasting syndrome (CSWS). SIADH is a volume glycosylated end-products, polysols, and hexosans lead to
expanded state characterized by oliguria, weight gain, elevation of inflammatory cytokines and suppression of
low serum sodium, and high urine sodium (>25 mmol/L), immune system. Also, hyperglycemia is associated with
whereas CSWS manifests as hyponatremia, dehydration, release of excitatory neurotransmitter glutamate in the
and high urine sodium (>50 mmol/L). In both conditions, neocortex. During ischemia, neuronal glucose (stored in
hyponatremia is seen but the management is entirely hyperglycemic phase) results in increased intracellular
different. Treatment of SIADH depends on fluid restriction lactate. The intracellular lactate is neurotoxic and is believed
(<1 L/24 h), sodium supplementation (3% hypertonic saline), to enhance neuronal injury.
while CSWS requires isotonic sodium solutions to re-establish
circulating volume.
Common Intracranial Postoperative
Postoperative venous thromboembolism: It includes
Complications Seen in NCC Units
deep vein thrombosis (DVT) and pulmonary embolism.
Cumulative incidence varies from 20 to 50% after neurosurgical Cerebral edema: Risk factors causing edema may include
procedures. Dehydration (use of mannitol/furosemide), preoperative cerebral edema, prolonged duration of
immobility, paralysis, TBI (release of procoagulant), stroke, surgery, excessive brain retraction, following AVM
and certain brain lesions (meningioma) are considered as risk resection and redo surgeries. Treatment involves use
factors for the development of thromboembolism. Prophylaxis of dexamethasone to decrease vasogenic edema, use of
includes limb physiotherapy, mechanical devices (intermittent osmotic agents, adequate analgesia/sedation, normoventi-
pneumatic devices, graduated compression stockings), and lation to mild hyperventilation, and use of iso-osmolar to
pharmacological anticoagulants (unfractionated or low mild hyperosmolar fluids.
molecular weight h eparin). Pharmacological prophylaxis is Intracranial hemorrhage: Postoperative risk of intracranial
usually started after 48 hours of surgery when risk for bleed- hemorrhage increases in patients with hypertension, coag-
ing or increase in size of hematoma is low. ulopathy and poor surgical homeostasis. Once suspected,
Hormone replacement: In pituitary surgery almost all noncontrast computed tomography (CT) scan is indicated
patients receive corticosteroid coverage until testing indi- and depending on the site and size of the hematoma, emer-
cates an intact pituitary–adrenal axis. Thyroid hormone gent evacuation may be required. Mannitol and reintubation
replacement is reserved for patients with preoperative may be required to stabilize the patient’s condition.
hypothyroidism. Hydrocephalus: After intraventricular bleed or in
Antibiotics: Postoperative antibiotic prophylaxis is posterior fossa surgery, there are chances of development
usually not recommended except in cases where foreign of hydrocephalus. It may require external ventricular drain
materials are implanted (such as intracranial electrodes in insertion in the postoperative period.
deep brain stimulation or epilepsy surgery), or continuous Seizures: Cortical pathology has a higher chance of
ICP monitoring is done using invasive methods. Similarly, developing seizures. Patients with epilepsy, brain tumor, aneu-
it is indicated in cases of contaminated wounds such as in rysmal SAH and intracranial hemorrhage are prone to developing
TBI, or when the risk of introducing infection is high like seizures. Postoperative drop in the functional neurological score
in CSF leak. could be due to convulsive or nonconvulsive seizures. Routine
Temperature management: Euthermia should be main- seizure p rophylaxis is generally not recommended for most
tained in the postoperative period. Hypothermia in cases intra-cranial tumors unless there is evidence of seizures. In
of prolonged surgery and exposure to cold environment postoperative seizures, phenytoin or levetiracetam can be used.
(catheterization laboratory or magnetic resonance imaging Phenytoin is used with a loading dose 10 to 20 mg phenytoin
suit) delays recovery and increases the risk of developing equivalents (PE)/kg over 30 minutes, maximum rate 150 mg
postoperative infections. Postoperative shivering increases PE/minute intravenously, no faster than 50 mg/minute in an
body oxygen consumption by up to 300 to 400%.22 adult; followed by infusion of 5 to 7 mg/kg/day. Fosphenytoin
Hyperthermia in neurosurgical cases is equally detrimental. is given at a loading dose of 15 to 20 mg/kg intravenously, no
Nutrition status: Feeding should be started at the earliest faster than 100 to 150 mg/minute, followed by an infusion of
in the postoperative period, either by oral, nasogastric, or 4 to 6 PE/kg/day. L evetiracetam is used in doses of 1000 mg/day
transgastric route, along with prophylaxis for stress ulcer. to 3000 mg/day in two d ivided dosages.
Journal of Neuroanaesthesiology and Critical Care Vol. 6 No. 2/2019
84 Management of Postoperative Neurosurgical Patients Panda et al.
Cerebrospinal fluid leak: CSF leak is commonly seen oral fluids. If it has to be replaced intravenously, hypotonic
after trans-sphenoidal pituitary surgery, TBI, or incisional solutions such as 0.45% sodium chloride (NaCl) can be given.
CSF leak following posterior fossa surgery. Clinical symptoms Insulin and potassium supplementation might be required
include leakage of clear, nonmucoid, watery fluid from the when dextrose-containing fluids are used, and when
nose, ear, or suture site which has positional dependency. corticosteroids are administered concomitantly. When hor-
Sometimes, it also presents as a salty postnasal drip. Further monal replacement is required, 1-deamino-8-d-arginine
testing of clear fluid mixed with blood or nasal discharge on vasopressin, a synthetic analog of the natural hormone
a filter paper shows double ring or halo or target sign. The arginine vasopressin, can be given intravenously, subcutane-
handkerchief test differentiates nasal discharge (unclear, ously, orally, or intranasally. The latter might not be feasible
sticky due to mucin secretion) and CSF (clear and nonsticky). after transnasal trans-sphenoidal pituitary surgery. The
Glucose level in CSF > 30 mg/dL indicates CSF leak. Beta-2 usual intravenous or subcutaneous dose is 0.3 µg/kg/day in
transferrin and beta-trace proteins are specific markers two divided doses. The dose of oral medication is 0.05 to
of CSF.CSF rhinorrhea predisposes patients to meningitis, 1.2 mg/day at once or divided into two or three doses. The
intracranial hypotension and leads to prolonged hospital stay. intranasal dose is 10 to 40 µg/day in one to three doses.
Early detection and repair of the leak are essential. Incisional Vision loss in the immediate postoperative period can
CSF leak requires resuturing of the wound, concomitant be due to hematoma formation compressing on the optic
CSF lumbar drainage, and administration of antibiotics. nerve or optic chiasma, which requires immediate surgical
Pneumocephalus: Patients operated in sitting or semi-sit- evacuation, while delayed loss can be due to cerebral edema,
ting positions are at risk of developing pneumocephalus. which requires supportive NCC. A thorough evaluation of
Pneumocephalus may also develop in other surgeries such postoperative rhinorrhea for CSF leak is important. CSF leak
as trans-sphenoidal surgery or chronic subdural hematoma increases risk of meningitis and secondary neurological
evacuation. Large amount of air trapping results in altered injury. Treatment options include lumbar drainage of CSF and
sensorium, seizures and coma. Tension pneumocephalus surgical repair of the defect.
requires urgent decompression. Infratentorial surgery: Patients undergoing posterior
Cranial nerve deficits: Cranial nerve deficits are common fossa surgeries may have delayed emergence due to tension
in posterior fossa surgery or skull base surgery. Injury can pneumocephalus, intracranial hemorrhage, symptomatic
cause impaired bulbar function, which requires reconsider- venous air embolism, and damage to the brain stem. Elective
ation of airway protection due to the possibility of aspiration postoperative ventilation is required in cases of bulbar
pneumonia. involvement and extensive intraoperative dissection near
Meningitis: Meningitis can be seen in postoperative cases the brain stem (central respiratory depression). Injury to
of TBI, use of intraoperative electrodes, following CSF leak, or lower cranial nerves (IX, X, and XII) may compromise the
due to failure to use sterile surgical techniques. It is important patient’s ability to maintain a patent protected airway due
to identify meningitis and promptly initiate treatment. to difficulty in swallowing and clearing secretions. Injury
to ophthalmic division of the trigeminal nerve may impair
protective reflexes of the cornea and require external
Specific Neurological Conditions
protection with an eye patch. Postoperative visual loss sub-
Supratentorial surgery: Postoperative hematoma, cerebral sequent to surgery in prone position is another devastating
edema, seizures, postcraniotomy pain, and PONV are common complication. Severe postoperative pain due to extensive
complications following supratentorial surgeries. Tumor muscle dissection and muscle spasm needs adequate anal-
bed hematoma due to incomplete hemostasis, subdural gesia to prevent development of chronic pain syndromes.
or epidural hematoma are not uncommon. Prevention of Close proximity of the surgical site to vomiting centers and
hypertension or excessive coughing and bucking during use of opioids for postoperative pain relief increase the risk
emergence is important. Management involves urgent of PONV and require multimodal a ntiemetic therapy.
noncontrast CT head, medical treatment to decrease raised Subarachnoid hemorrhage: Postoperative period follow-
ICP, hematoma evacuation, and decompressive craniectomy. ing surgical clipping in aSAH is crucial. Life-threatening vaso-
Delayed hydrocephalus may occur after resection of spasm is usually seen from 3 to 14 days after SAH. It is clinically
supratentorial malignant gliomas and should be considered identified as decrease in consciousness, disorientation, and
in cases of initial improvement followed by deterioration of appearance of new focal neurological deficits. Clinical vaso-
consciousness. Shunting of CSF in cases of communicating spasm is seen in 30% cases, while radiographic vasospasm
hydrocephalus yields satisfactory results. is seen in 70% cases.Different parameters that aid in the
Pituitary surgery: Endocrine complications following diagnosis of vasospasm include flow velocity measurement
pituitary surgery include hypocortisolism, hypothyroidism, by TCD (increased flow velocity > 120 cm/s or Lindegaard
and DI. Treatment of DI consists of hydration and hormonal ratio >3), decreased amplitude, and decreased alpha activity
supplementation. The volume and type of intravenous in electroencephalography. Digital subtraction angiography
fluids are guided by urine volume, serum electrolytes, and offers diagnostic as well as therapeutic (intra-arterial
osmolality. Free water (H2O) deficit can be estimated using nimodipine/milrinone administration) modality. Numerous
the formula: Free H2O deficit (L) = (serum Na–140) × body treatment options are available but approved treatment
weight (kg) × 0.6/140. Free water deficit can be replaced by involves use of oral nimodipine, maintenance of euvolemic
Journal of Neuroanaesthesiology and Critical Care Vol. 6 No. 2/2019
Management of Postoperative Neurosurgical Patients Panda et al. 85
status, and maintenance of mild hypertension.23 Fluid and Arteriovenous malformation: Following AVM resection
electrolyte disturbances are common in aSAH. Up to 40% or obliteration, patients are at risk of developing compli-
patients experience hyponatremia either due to CSWS or cations similar to those that occur after aneurysm surgery
SIADH. Management of CSWS and SIADH has been described (vasospasm, hydrocephalus, and seizures). In addition,
earlier. Acute hydrocephalus can occur in 20% of aSAH. these patients are at high risk of developing hyperemic
Patients may have persistent headache, loss of upward gaze, complications leading to uncontrollable cerebral swelling
and cognitive impairment, and may require CSF drainage. and hemorrhage due to transient circulatory disturbance
Traumatic brain injury: The systemic sequelae of head known as normal perfusion pressure breakthrough. This
trauma frequently become apparent in the postoperative can manifest as headache, seizures, permanent neurological
period. These include cardiac arrhythmias, disseminated disability, and even death. Treatment strategies include fluid
intravascular coagulation, adult respiratory distress restriction, prevention of systemic hypertension, controlled
syndrome, NPE, DI, SIADH, hyperglycemic hyperosmolar hyperventilation, osmotic agents, and use of anesthetic
nonketotic coma, and gastrointestinal stress ulcers and agents to prevent raised ICP.
hemorrhage. Moderate-to-severe head injury patients require Interventional neuroradiological procedures: These
intensive care for prevention of secondary injury, early patients should be kept in supine position till femoral
detection, and management of neurological deterioration sheath is in situ. Adequate control of blood pressure in post-
and management of ICP. operative period depends upon the type of cerebrovascular
NPE is a fulminant form of pulmonary edema, which pathology. Contrast-induced nephropathy (CIN) is the third
can progress rapidly (within hours to days) toward either most common cause of hospital-acquired renal failure. The
resolution or death. Treatment is aimed at reducing ICP, risk factors include diabetes mellitus, high dose of contrast,
reducing sympathetic hyperactivity, mainly with volume depletion, co-administration of nephrotoxic
pharmacological agents, providing respiratory supportive drugs, and pre-existing renal disease. To prevent renal
care, and inotropic therapy as needed. complications, perioperative management should be aimed
SIADH treatment consists of water restriction, use of at maintaining normovolemia using intravenous saline
loop diuretics, and hypertonic saline. In mild cases, fluid hydration and the use of low osmolality contrast medium.
restriction (1–1.5 L/day) is sufficient to correct hyponatremia. The use of N-acetylcysteine to decrease the risk of CIN is
Furosemide may be added to treat hypervolemia. Hypertonic debatable.26 In view of current evidence, it is probably not
saline is usually reserved for a serum Na < 120 mEq/L. It indicated as the standard-of-care.
is given in small amounts for a short time (1–2 mL/kg/h Spine surgery: Anterior cervical spine surgeries
for 2–3 h) after which serum sodium and osmolality are increase the risk of developing postoperative airway
measured. During the acute phase of SIADH, urine output obstruction due to pharyngeal edema, wound hematoma,
should be measured hourly, urine osmolality and specific vocal palsy, dislodgment of bone graft, or fixation plate.
gravity, and serum sodium and osmolality are measured Management involves emergency reintubation followed
every 6 to 8 hours. Serum sodium should be increased at a by hematoma evacuation. Postoperative pain management
rate of not more than 0.5 mEq/L/hour or 12 mEq/L/day. is an important aspect as it interferes with functional
Brain Trauma Foundation guideline states ICP above recovery following surgery (impaired ventilation in thoracic
22 mm Hg as threshold for treatment. The treatment of raised surgery, reduced early mobilization, increased risk of DVT,
ICP follows stepwise pattern starting with head elevation delayed bowel function, and increased risk of urinary
(30°), normoventilation (or short period of hyperventilation), infections). Multimodal pain management is an essential
adequate sedation, analgesia, and muscle paralysis (to part of postoperative care of these patients. Prolonged spine
prevent coughing and bucking on ventilator and decreas- surgeries along with immobilization and hypercoagulable
ing work of breathing). If ICP continues to be high (>25 mm states increase the risk of thromboembolic events in the
Hg), hyperosmolar therapy (mannitol/hypertonic saline) and postoperative period.
ventriculostomy can be added to the previous treatment.
Other options to decrease raised ICP include therapeutic
Conclusion
hypothermia, decompressive craniectomy, and inducing
barbiturate coma. Although hypothermia is neuroprotective, Outcome after neurosurgical procedure depends not only
therapeutic hypothermia has not been found to improve on surgical technique but also on postoperative care of
functional neurological outcomes.24,25 these patients in specialized NCC units. The postoperative
Occlusive cerebrovascular surgery: Carotid sinus management of neurosurgical patients is a complex endeavor
baroreceptor function impairment after carotid endarterectomy and it demands comprehensive knowledge of anatomical,
or angioplasty causes hypotension, hypertension, and dysrhyth- physiological, and neurological perturbations. Careful regular
mias. Mild increase in blood pressure (up to 20% above baseline assessment, multimodal neuromonitoring along with early
level) is acceptable but above this requires antihypertensive detection, and management of any complication by an
therapy. Major complications anticipated include stroke, alert neurointensivist remain cornerstone of postoperative
myocardial infarction, and hyper-perfusion syndrome. management.
Journal of Neuroanaesthesiology and Critical Care Vol. 6 No. 2/2019
86 Management of Postoperative Neurosurgical Patients Panda et al.
Conflict of Interest 14 Caricato A, Conti G, Della Corte F, et al. Effects of PEEP on
None declared. the intracranial system of patients with head injury and
subarachnoid hemorrhage: the role of respiratory system
compliance. J Trauma 2005;58(3):571–576
References 15 Zygun D. Non-neurological organ dysfunction in neurocrit-
ical care: impact on outcome and etiological considerations.
1 Lassen HC. A preliminary report on the 1952 epidemic Curr Opin Crit Care 2005;11(2):139–143
of poliomyelitis in Copenhagen with special reference to 16 Banki N, Kopelnik A, Tung P, et al. Prospective analysis
the treatment of acute respiratory insufficiency. Lancet of prevalence, distribution, and rate of recovery of left
1953;1(6749):37–41 ventricular systolic dysfunction in patients with subarachnoid
2 Mirski MA, Chang CW, Cowan R. Impact of a neuroscience hemorrhage. J Neurosurg 2006;105(1):15–20
intensive care unit on neurosurgical patient outcomes and cost 17 Meyfroidt G, Baguley IJ, Menon DK. Paroxysmal sympathetic
of care: evidence-based support for an intensivist-directed hyperactivity: the storm after acute brain injury. Lancet
specialty ICU model of care. J Neurosurg Anesthesiol Neurol 2017;16(9):721–729
2001;13(2):83–92 18 Thibault M, Girard F, Moumdjian R, Chouinard P,
3 Teasdale G, Jennett B. Assessment of coma and impaired Boudreault D, Ruel M. Craniotomy site influences postopera-
consciousness. A practical scale. Lancet 1974;2(7872):81–84 tive pain following neurosurgical procedures: a retrospective
4 Wijdicks EF, Bamlet WR, Maramattom BV, Manno EM, study. Can J Anaesth 2007;54(7):544–548
McClelland RL. Validation of a new coma scale: the FOUR 19 Latz B, Mordhorst C, Kerz T, et al. Postoperative nausea and
score. Ann Neurol 2005;58(4):585–593 vomiting in patients after craniotomy: incidence and risk
5 Miller JD. Measuring ICP in patients: its value now and in factors. J Neurosurg 2011;114(2):491–496
the future? In: Hoff JT, Betz AL, eds. Intracranial Pressure VII. 20 Kurita N, Kawaguchi M, Nakahashi K, et al. [Retrospective
Berlin: Springer-Verlag; 1989:5–15 analysis of postoperative nausea and vomiting after
6 Rajajee V, Vanaman M, Fletcher JJ, Jacobs TL. Optic nerve craniotomy]. Masui 2004;53(2):150–155
ultrasound for the detection of raised intracranial pressure. 21 Tisdall M, Crocker M, Watkiss J, Smith M. Disturbances of
Neurocrit Care 2011;15(3):506–515 sodium in critically ill neurologic patients. J Neurosurg
7 Aaslid R, Markwalder TM, Nornes H. Noninvasive transcranial Anesthesiol 2006;18:57–63
Doppler ultrasound recording of flow velocity in basal cerebral 22 Pauca AL, Savage RT, Simpson S, Roy RC. Effect of pethidine,
arteries. J Neurosurg 1982;57(6):769–774 fentanyl and morphine on post-operative shivering in man.
8 Chieregato A, Calzolari F, Trasforini G, Targa L, Latronico N. Acta Anaesthesiol Scand 1984;28(2):138–143
Normal jugular bulb oxygen saturation. J Neurol Neurosurg 23 Connolly ES, Rabinstein AA, Carhuapoma JR, Derdeyn CP,
Psychiatry 2003;74(6):784–786 Dion J, Higashida Rt. Guidelines for the management of
9 Hillered L, Vespa PM, Hovda DA. Translational neurochemical aneurysmal Subarachnoid haemorrhage: a guideline for
research in acute human brain injury: the current status and healthcare professionals from the American Heart Association
potential future for cerebral microdialysis. J Neurotrauma /American Stroke Association. Stroke 2012;43(6):1711–1737
2005;22(1):3–41 24 Andrews PJ, Sinclair HL, Rodriguez A, et al; Eurotherm
10 Davison DL, Terek M, Chawla LS. Neurogenic pulmonary 3235 Trial Collaborators. Hypothermia for Intracranial
edema. Crit Care 2012;16(2):212 Hypertension after Traumatic Brain Injury. N Engl J Med
11 McHugh GS, Engel DC, Butcher I, et al. Prognostic value of 2015;373(25):2403–2412
secondary insults in traumatic brain injury: results from the 25 Cooper DJ, Nichol AD, Bailey M, et al. Effect of early
IMPACT study. J Neurotrauma 2007;24(2):287–293 sustained prophylactic hypothermia in neurologic outcomes
12 Davis DP. Early ventilation in traumatic brain injury. among patients with severe traumatic brain injury. JAMA
Resuscitation 2008;76(3):333–340 2018;320(21):2211–2220
13 Muench E, Bauhuf C, Roth H, et al. Effects of positive 26 Li JX, Jin EZ, Yu LH, et al; Li Jing-Xui. Oral N-acetylcysteine
end-expiratory pressure on regional cerebral blood flow, for prophylaxis of contrast-induced nephropathy in patients
intracranial pressure, and brain tissue oxygenation. Crit Care following coronary angioplasty: A meta-analysis. Exp Ther
Med 2005;33(10):2367–2372 Med 2017;14(2):1568–1576
Journal of Neuroanaesthesiology and Critical Care Vol. 6 No. 2/2019
View publication stats
You might also like
- Acute Neuro Care: Focused Approach to NeuroemergenciesFrom EverandAcute Neuro Care: Focused Approach to NeuroemergenciesPrasanna Udupi BidkarNo ratings yet
- CNCCSC 2015Document16 pagesCNCCSC 2015clauxavNo ratings yet
- Neuro in The ICUDocument4 pagesNeuro in The ICUEduardo GarciaNo ratings yet
- A Systemic Review of Functional Near-Infrared Spectroscopy For Stroke: Current Application and Future DirectionsDocument14 pagesA Systemic Review of Functional Near-Infrared Spectroscopy For Stroke: Current Application and Future DirectionsEricNo ratings yet
- Risk Factors and Associated Complications With Unplanned Intubation in Patients With Craniotomy For Brain Tumor.Document5 pagesRisk Factors and Associated Complications With Unplanned Intubation in Patients With Craniotomy For Brain Tumor.49hr84j7spNo ratings yet
- Neurocritical Care Management of The Neurosurgical Patient (PDFDrive)Document510 pagesNeurocritical Care Management of The Neurosurgical Patient (PDFDrive)Chanatthee KitsiripantNo ratings yet
- Guidelines For The Management of Brain InjuryDocument26 pagesGuidelines For The Management of Brain InjuryfathaNo ratings yet
- Postoperative Cognitive Dysfunction Preoperative Risk Assessment and Perioperative Risk Minimization A Pragmatic Review of The LitDocument5 pagesPostoperative Cognitive Dysfunction Preoperative Risk Assessment and Perioperative Risk Minimization A Pragmatic Review of The Litade_liaNo ratings yet
- 1 s2.0 S105230572300006X MainDocument14 pages1 s2.0 S105230572300006X MainIda Ayu Trisna DewiNo ratings yet
- Management Post Operative NeurosurgicalDocument6 pagesManagement Post Operative NeurosurgicalLusy Octavia SaputriNo ratings yet
- Neurocritico Nuevos ParadigmasDocument16 pagesNeurocritico Nuevos ParadigmasAlessandraCervantesNo ratings yet
- 4 Preliminary Guideline - and Pathophysiology - Base Protocols For Neurological CareDocument9 pages4 Preliminary Guideline - and Pathophysiology - Base Protocols For Neurological CareehuaniNo ratings yet
- UCNS NCS Website FAQ Sheet 9 9 20Document6 pagesUCNS NCS Website FAQ Sheet 9 9 20Lilian MariaNo ratings yet
- Medsci 11 00015 v2Document34 pagesMedsci 11 00015 v2Paulina Sobarzo VegaNo ratings yet
- Pattern and Categorisation of Neurosurgical Emergencies: Conference ProceedingDocument3 pagesPattern and Categorisation of Neurosurgical Emergencies: Conference ProceedingarshadNo ratings yet
- Update On Multimodality MonitoDocument8 pagesUpdate On Multimodality MonitoConstanza Andrea Saldivia Blanco(RedSalud Magallanes)No ratings yet
- NeuroVISION ArticleDocument8 pagesNeuroVISION ArticleDanielle de Sa BoasquevisqueNo ratings yet
- Application of Intracranial Pressure-Directed Therapy On DCIDocument9 pagesApplication of Intracranial Pressure-Directed Therapy On DCIRonaldo MofuNo ratings yet
- Neurocritical Care Management of The Neurosurgical Patient 1St Edition Edition Monisha Kumar Full ChapterDocument67 pagesNeurocritical Care Management of The Neurosurgical Patient 1St Edition Edition Monisha Kumar Full Chapteramelia.bradham272100% (9)
- PTJ 1006Document9 pagesPTJ 1006sundar_kumar0No ratings yet
- Anaesthesia For Neurosurgery PDFDocument6 pagesAnaesthesia For Neurosurgery PDFAnderson LondoñoNo ratings yet
- Baru 2Document12 pagesBaru 2Bianca CaterinalisendraNo ratings yet
- Initial Diagnosis and Management of Acutely Elevated Intracranial PressureDocument8 pagesInitial Diagnosis and Management of Acutely Elevated Intracranial PressureGlessin MurilloNo ratings yet
- Neurocritical Care Training CurriculumDocument3 pagesNeurocritical Care Training Curriculumgemmalynn sarapuddinNo ratings yet
- PCVS Nirs No 2010Document4 pagesPCVS Nirs No 2010Maximiliano OliveraNo ratings yet
- Milne (2022) - Neuromonitoring and Neurocognitive Outcomes in Cardiac SurgeryDocument16 pagesMilne (2022) - Neuromonitoring and Neurocognitive Outcomes in Cardiac SurgeryVanessaNo ratings yet
- Working in A Hospital's Neurointensive Care Unit Treat Patients Suffering From Everything From Stroke To Traumatic Brain InjuriesDocument5 pagesWorking in A Hospital's Neurointensive Care Unit Treat Patients Suffering From Everything From Stroke To Traumatic Brain InjuriesRichlle CortesNo ratings yet
- Jurnal Clinical L OutcomeDocument14 pagesJurnal Clinical L OutcomeaesunnitheticNo ratings yet
- Neurointensive IndicationDocument8 pagesNeurointensive Indicationzee zeeNo ratings yet
- Establishing A Clinical Service For The Management of Sports-Related ConcussionsDocument11 pagesEstablishing A Clinical Service For The Management of Sports-Related ConcussionsPato Patiño MuñozNo ratings yet
- Neurological SurgeryDocument16 pagesNeurological Surgeryalpriani patrasNo ratings yet
- Role of Ultrasonographic Inferior Venacaval Assessment in Surgeries Conducted Under General Anaesthesia-A Prospective Observational StudyDocument6 pagesRole of Ultrasonographic Inferior Venacaval Assessment in Surgeries Conducted Under General Anaesthesia-A Prospective Observational StudyIJAR JOURNALNo ratings yet
- Traumatic Brain Injury Initial Resuscitation and TransferDocument4 pagesTraumatic Brain Injury Initial Resuscitation and TransferRielc zemartinNo ratings yet
- Stroke SimulationDocument6 pagesStroke SimulationShirsho ShreyanNo ratings yet
- Outcome in Nuerocritical CareDocument7 pagesOutcome in Nuerocritical CareParvathy R NairNo ratings yet
- Results of Assessing The Effect of Biliary Therapy On The Blood Clotting SystemDocument4 pagesResults of Assessing The Effect of Biliary Therapy On The Blood Clotting SystemCentral Asian StudiesNo ratings yet
- Preoperative Identification of Neurosurgery Patients With A High Risk of In-Hospital Complications: A Prospective Cohort of 418 Consecutive Elective Craniotomy PatientsDocument11 pagesPreoperative Identification of Neurosurgery Patients With A High Risk of In-Hospital Complications: A Prospective Cohort of 418 Consecutive Elective Craniotomy PatientsAzizi AlfyanNo ratings yet
- Good Morning EveryoneDocument6 pagesGood Morning EveryoneRichlle CortesNo ratings yet
- Multimodal and AutoregulationDocument20 pagesMultimodal and Autoregulationpraneeth reddy drNo ratings yet
- Perioperative Stroke BJA 2021Document7 pagesPerioperative Stroke BJA 2021lim sjNo ratings yet
- Early Mobilization Reduces Delirium After Coronary Artery Bypass Graft SurgeryDocument6 pagesEarly Mobilization Reduces Delirium After Coronary Artery Bypass Graft SurgeryevaNo ratings yet
- Idsa NeurocisticercosisDocument27 pagesIdsa Neurocisticercosistucto849915No ratings yet
- Sedatives in Neurocritical Care 2019 Curr Opin Crit CareDocument8 pagesSedatives in Neurocritical Care 2019 Curr Opin Crit CareCAMILO ERNESTO DAZA PERDOMONo ratings yet
- Acute Ischaemic StrokeDocument40 pagesAcute Ischaemic StrokeDana Crusoveanu100% (1)
- Assessment of The Effects of Dysphagia Therapy in Patients in The Early Post-Stroke Period: A Randomised Controlled TrialDocument7 pagesAssessment of The Effects of Dysphagia Therapy in Patients in The Early Post-Stroke Period: A Randomised Controlled TrialAlba Fernández GonzálezNo ratings yet
- Risk Factors For Prehospital Delays in Acute Stroke Patients in South IndiaDocument5 pagesRisk Factors For Prehospital Delays in Acute Stroke Patients in South IndiaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Brainsci 10 00499 v2Document9 pagesBrainsci 10 00499 v2Maudonat MegNo ratings yet
- Jnic 2019 00213 PDFDocument6 pagesJnic 2019 00213 PDFAwal13 ArigaNo ratings yet
- Original Article: ArticleinfoDocument5 pagesOriginal Article: ArticleinfoBIOMEDSCIDIRECT PUBLICATIONSNo ratings yet
- Neurocritical Care.2019 - Kosaku KinoshitaDocument225 pagesNeurocritical Care.2019 - Kosaku KinoshitaHenry Flores CallaNo ratings yet
- TB I Guidelines 2008Document32 pagesTB I Guidelines 2008tugiwiyonoNo ratings yet
- Preope Mayo Clinic 2020Document16 pagesPreope Mayo Clinic 2020claauherreraNo ratings yet
- Fisioterapia Hematoma SubduralDocument4 pagesFisioterapia Hematoma SubduralLeandro AntivilNo ratings yet
- NiceDocument7 pagesNiceRisky Ilona SaputraNo ratings yet
- Extubation Success Prediction in A Multicentric Cohort of Patients With Severe Brain InjuryDocument9 pagesExtubation Success Prediction in A Multicentric Cohort of Patients With Severe Brain InjuryEdison LucioNo ratings yet
- Prognostic Factors of Functional Outcome in Post-Acute Stroke in The Rehabilitation UnitDocument9 pagesPrognostic Factors of Functional Outcome in Post-Acute Stroke in The Rehabilitation UnitIda Ayu Trisna DewiNo ratings yet
- Monitoreo MultinodakDocument7 pagesMonitoreo Multinodakrodolfo riosNo ratings yet
- Early Acute-CPG - CPG Bladder Managmenet PDFDocument81 pagesEarly Acute-CPG - CPG Bladder Managmenet PDFesperanza asencios cernaNo ratings yet
- Anaesthesia For Neurosurgery-PIIS1472029919302656Document6 pagesAnaesthesia For Neurosurgery-PIIS1472029919302656james Wilson09No ratings yet
- Effects of Early Rehabilitation Nursing InterventionDocument9 pagesEffects of Early Rehabilitation Nursing InterventionFistalina SukmiantiNo ratings yet
- Prevalence of Malnutrition Among Hospitalized Children: June 2014Document4 pagesPrevalence of Malnutrition Among Hospitalized Children: June 2014Imin BuntaraNo ratings yet
- Brain 20 Ultrasonography 20 in 20 The 20 Premature 20 InfantDocument11 pagesBrain 20 Ultrasonography 20 in 20 The 20 Premature 20 InfantImin BuntaraNo ratings yet
- International Journal of Research PublicationsDocument3 pagesInternational Journal of Research PublicationsImin BuntaraNo ratings yet
- Transcranial Ultrasound Doppler Parameters in CereDocument7 pagesTranscranial Ultrasound Doppler Parameters in CereImin BuntaraNo ratings yet
- On The Regulation of The Blood Supply To The BrainDocument4 pagesOn The Regulation of The Blood Supply To The BrainImin BuntaraNo ratings yet
- Prophylactic Antibiotics in Pediatric Neurological SurgeryDocument6 pagesProphylactic Antibiotics in Pediatric Neurological SurgeryImin BuntaraNo ratings yet
- Fped 08 00277Document10 pagesFped 08 00277Imin BuntaraNo ratings yet
- The Incidence of Respiratory Distress Syndrome Among Preterm Infants Admitted To Neonatal Intensive Care Unit: A Retrospective StudyDocument6 pagesThe Incidence of Respiratory Distress Syndrome Among Preterm Infants Admitted To Neonatal Intensive Care Unit: A Retrospective StudyImin BuntaraNo ratings yet
- Pereira Da Silva - AmJHealthSystPharm2003Document6 pagesPereira Da Silva - AmJHealthSystPharm2003Imin BuntaraNo ratings yet
- R. Hasya Arianda BAB VIIIDocument13 pagesR. Hasya Arianda BAB VIIIImin BuntaraNo ratings yet
- Definition and Categorization of The Timing of Mother-To-Child Transmission of Sars-Cov-2Document14 pagesDefinition and Categorization of The Timing of Mother-To-Child Transmission of Sars-Cov-2Imin BuntaraNo ratings yet
- Nutrients: Congenital, Intrapartum and Postnatal Maternal-Fetal-Neonatal Sars-Cov-2 Infections: A Narrative ReviewDocument15 pagesNutrients: Congenital, Intrapartum and Postnatal Maternal-Fetal-Neonatal Sars-Cov-2 Infections: A Narrative ReviewImin BuntaraNo ratings yet
- Obesity A Risk Factor For Increased COVID 19 Prevalence, Severity and Lethality (Review)Document11 pagesObesity A Risk Factor For Increased COVID 19 Prevalence, Severity and Lethality (Review)Imin BuntaraNo ratings yet
- Clinical Manifestations of Children With COVID 19: A Systematic ReviewDocument9 pagesClinical Manifestations of Children With COVID 19: A Systematic ReviewImin BuntaraNo ratings yet
- Circulatory System Answer SheetDocument4 pagesCirculatory System Answer SheetMarlie TobiseNo ratings yet
- Respiratory Case StudiesDocument2 pagesRespiratory Case Studiesk_manchesterNo ratings yet
- File 0147Document6 pagesFile 0147Tassnime SebaeiNo ratings yet
- Neuronal Conduction1Document61 pagesNeuronal Conduction1ISHITA GOEL 19224115No ratings yet
- Body Fluid: Dr. Dr. H. Busjra M. Nur, MS Dept. Physiology FKUI/ FKK UMJDocument50 pagesBody Fluid: Dr. Dr. H. Busjra M. Nur, MS Dept. Physiology FKUI/ FKK UMJGhaidaa SadeqNo ratings yet
- 9 Heart MuscleDocument31 pages9 Heart Muscleshoeb4uNo ratings yet
- NeurotransmittersDocument39 pagesNeurotransmitterspreetie87No ratings yet
- Science (Grade 9) ModuleDocument394 pagesScience (Grade 9) Modulecaseydale_2489% (472)
- Comparative Anatomy of Heart, Circulation Aortic Arches EtcDocument36 pagesComparative Anatomy of Heart, Circulation Aortic Arches EtcNarasimha Murthy100% (4)
- Chapter 01 Introduction To PerceptionDocument48 pagesChapter 01 Introduction To PerceptionSimrat WNo ratings yet
- Medical Surgical Nursing An Integrated Approach - Compressed-554-624Document71 pagesMedical Surgical Nursing An Integrated Approach - Compressed-554-624nugrahaNo ratings yet
- Blood Oxygen & Heart Rate Monitor With MAX30100 & ArduinoDocument3 pagesBlood Oxygen & Heart Rate Monitor With MAX30100 & ArduinoHusnain AfzalNo ratings yet
- Brain Bee Sample QuestionsDocument4 pagesBrain Bee Sample QuestionsThasaRatha100% (3)
- 9 ECG Strips On The NCLEXDocument1 page9 ECG Strips On The NCLEXAlther LorenNo ratings yet
- Chapter 14 - Multiple ChoiceDocument13 pagesChapter 14 - Multiple ChoiceNicky PhakathiNo ratings yet
- Health Teaching PPT For HypertensionDocument13 pagesHealth Teaching PPT For HypertensionJeym Quinny ClapanoNo ratings yet
- Us Chughtais Lab Rate ListDocument2 pagesUs Chughtais Lab Rate Listapi-525272944No ratings yet
- MID YEAR Assessment - SCIENCE10Document5 pagesMID YEAR Assessment - SCIENCE10anelou guingueNo ratings yet
- Anaphy - Lesson 4 - Topic 4 and 5Document21 pagesAnaphy - Lesson 4 - Topic 4 and 5Rica Abigail DagosNo ratings yet
- NCP RequirementsDocument3 pagesNCP RequirementsJasmine JarapNo ratings yet
- Diabetic Ketoacidosis (DKA) VS. Hyperosmolar Hyperglycemic Syndrome (HHS)Document5 pagesDiabetic Ketoacidosis (DKA) VS. Hyperosmolar Hyperglycemic Syndrome (HHS)MrRightNo ratings yet
- V.Sowndharya MeeraDocument22 pagesV.Sowndharya MeeraGopi NathNo ratings yet
- Case Study 1 DKADocument8 pagesCase Study 1 DKALupita SolorzanoNo ratings yet
- Learner's Activity Sheet: Physical Education and Health I (Quarter I - Week 4)Document8 pagesLearner's Activity Sheet: Physical Education and Health I (Quarter I - Week 4)Ayesha MeloNo ratings yet
- Dr. Naitik Trivedi & Dr. Upama Trivedi: Haemopoietic SystemDocument22 pagesDr. Naitik Trivedi & Dr. Upama Trivedi: Haemopoietic SystemthiruklpNo ratings yet
- Pain and Pain Pathways FinalDocument56 pagesPain and Pain Pathways FinalAnji SatsangiNo ratings yet
- ANPS 020 Cornbrooks 02-07-14Document25 pagesANPS 020 Cornbrooks 02-07-14enam professorNo ratings yet
- Week 13 Endocrine 2 1 PPDocument57 pagesWeek 13 Endocrine 2 1 PPJoy KNo ratings yet
- Lee, Thonylet E. Mabinta, Dianne Melad, Maria FeDocument25 pagesLee, Thonylet E. Mabinta, Dianne Melad, Maria FeShivaveerakumar S. Chandrikimath100% (1)
- Nervous System WorksheetDocument12 pagesNervous System WorksheetLeamae ObinaNo ratings yet
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (32)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 4.5 out of 5 stars4.5/5 (82)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (46)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (4)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesFrom EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesRating: 4.5 out of 5 stars4.5/5 (1412)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (5)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisFrom EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisRating: 5 out of 5 stars5/5 (8)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Troubled: A Memoir of Foster Care, Family, and Social ClassFrom EverandTroubled: A Memoir of Foster Care, Family, and Social ClassRating: 4.5 out of 5 stars4.5/5 (27)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingFrom EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingRating: 4 out of 5 stars4/5 (1138)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)