Professional Documents
Culture Documents
Antibiotic Prophylaxis Orthopaedic Surgery
Uploaded by
DonOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Antibiotic Prophylaxis Orthopaedic Surgery
Uploaded by
DonCopyright:
Available Formats
ANTIBIOTIC PROPHYLAXIS IN ORTHOPAEDIC SURGERY
The aim of surgical prophylaxis is to reduce rates of surgical site and healthcare-associated infections and so reduce surgical morbidity and mor tality. There is however growing evidence that
aspects of prescribing practice may themselves be associated with health-care associated infections and antimicrobial resistance. The Scottish Antimicrobial Prescribing Group (SAPG), along
with the Scottish Government, monitors antimicrobial prescribing including surgical prophylaxis in order to reduce the rates of resistance and C.difficile. SIGN guideline 104 published in July
2008, and updated in April 2014, has outlined which surgical procedures require prophylactic antibiotics based on a review of the available ev idence. Principles of prophylaxis have also been
outlined, including timing and duration of antibiotic administration. In conjunction with the surgical specialties within NHS Tayside the Antimicrobial Management Group has under taken to
review local prophylaxis policy and to for mulate a uniform policy.
Principles of Antibiotic Prophylaxis Policy
1. Indication for prophylaxis should comply with SIGN 104 guideline i.e. when ‘highly recommended’, ‘recommended’ or ‘considered’ w ithin guideline.
2. Timing of antibiotic(s):
• Optimum timing is intravenous dose given or infusion completed ≤ 60 minutes prior to skin incision
• Sub-optimal if >1 hour prior to skin incision or post-skin incision
• The exception is co- trimoxazole which is a one hour infusion. The window for this is within 2 hours of knife to skin (or the application of a tour niquet where used).
3. Recording of antibiotic prescription in ‘once only’ section of medicine char t to avoid multiple dosing
4. Frequency of administration should be single dose only unless:
• > 1.5 litres intra-operative blood loss - re-dose following fluid replacement (see administration guidance table)
• operation prolonged (see administration guidance table)
• specifically stated in follow ing guidelines
5. Documentation in medical notes of reason for antibiotic administration beyond single dose or state intention for antibiotic treatment cour se
6. Choice of agent should:
• Avoid cephalosporins and quinolones wherever possible
• Use narrow spectrum agents when possible to minimise impact on resistance and CDI
• Take into account local resistance patterns
• Provision of alternatives for beta-lactam allergy
7. De-colonisation therapy/MRSA patients
• If a patient is identified as MRSA positive from screening swabs within 3 weeks of anticipated date of elective surgery then a decolonisation program
should be star ted as per MRSA protocol. For surgical prophylaxis for primary operations vancomycin infusion should be used. If they have an MRSA infection prior to
elective surgery the approach is the same as for any other infection. Fur ther advice is available from Infection Control and Microbiology.
8. Complex individual prophylaxis issues e.g. where patient has had an ESBL previously should be discussed with Microbiology or Infectious Diseases pre-operatively and recorded
in medical notes.
9. Compliance with local policy is required and monitored by NHS Tayside. Any deviation from policy must be recorded in the appropriate medical records.
For details of administration of antibiotics see last page.
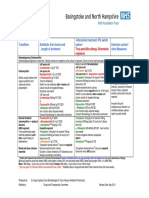
Type of Surgery Procedure SIGN 104 Recommendation Antibiotic(s) Comments
MRSA positive – add vancomycin to surgical
prophylaxis regime – see dosing in table on last
page
Previous ESBL – ask Micro for advice on
appropriate surgical prophylaxis
Orthopaedic Arthroplasty (including revisions ‘Highly Recommended’ Co-amoxiclav 1.2g IV 2 additional doses of Co-amoxiclav 1.2g (regardless of BMI) should
where no infection is suspected) Antibiotic loaded cement is be given at 8 hourly intervals ( i.e. at 8 hours and 16 hours post
recommended in addition to IV Hip Arthroplasty induction)
antibiotics and BMI ≥ 30:
Co-amoxiclav 1.2g IV In penicillin allergic patients use co- trimoxazole 960mg. 1 additional
+ dose should be given at 12 hours post induction.
Amoxicillin 1g IV
Open fracture ‘Highly Recommended’ Co-amoxiclav 1.2g IV In penicillin allergic patients use co- trimoxazole 960mg 12 hourly and
(including open hand fractures) every 8 hours metronidazole 500mg 8 hourly to ensure adequate cover.
Prophylaxis should be started as soon as possible after injury and
ideally within 3 hour s of trauma, and continued until soft tissue
closure or for a maximum of 72 hours, whichever is sooner.
(Ref BOA 2009)
Open surgery for closed fracture ‘Highly Recommended’ Co-amoxiclav 1.2g IV All single doses only (no fur ther doses required)
In penicillin allergic patients use co- trimoxazole 960mg.
Hip fracture ‘Highly Recommended’ Co-amoxiclav 1.2g IV 2 additional doses of Co-amoxiclav 1.2g should be given at 8 hourly
intervals ( i.e. at 8 hours and 16 hours post induction)
In penicillin allergic patients use co- trimoxazole 960mg. 1 additional
dose should be given at 12 hours post induction
Orthopaedic surgery without implant ‘Not Recommended’
Lower limb amputation See Vascular surgical prophylaxis
guidance
Soft tissue surgery of the hand Locally not routinely recommended
(not trauma surgery)
Spinal surgery with implant Locally recommended Co-amoxiclav 1.2g IV 2 additional doses of Co-amoxiclav 1.2g should be given at 8 hourly
intervals ( i.e. at 8 hours and 16 hours post induction)
In penicillin allergic patients use co- trimoxazole 960mg. 1 additional
dose should be given at 12 hours post induction
Spinal surgery without implant Locally recommended Co-amoxiclav 1.2g IV All single doses only (no fur ther doses required)
Type of Surgery Procedure SIGN 104 Antibiotic(s) Comments
Recommendation Previous ESBL – ask Micro for advice on
appropriate surgical prophylaxis
Orthopaedic Revision ar throplasty Locally recommended in THEATRE: Choice of antimicrobial is based on a number of factors:
Ciprofloxacin 400mg IV one dose • Locally increasing number of gram negative
+ infections
DAIR procedure Vancomycin IV • Pseudomonas should be covered until microbiology
Give LOADING dose in theatre after results or indicators deter mine this is not required
• Locally a number of teicoplanin resistant but
Removal of other implant samples taken: vancomycin sensitive coagulase negative
Based on actual body weight staphylococci infections
<40kg 750mg over 90 minutes
Applies to procedures where 40-59kg 1g over 2 hours • It is essential that dosing of
infection is suspected 60-90kg 1.5g over 3 hours vancomycin is sufficient to treat
>90kg 2g over 4 hours
infection
Antibiotics should not be given until samples have been taken
then continue on the WARD:
for culture and sensitivity.
IV Vancomycin MAINTENANCE dose 12- Aim for pre dose vancomy cin level of 15-20mg/L
24 hours after loading dose calculated as per
local vancomycin guidance or calculator
+
ORAL ciprofloxacin 500mg bd
(750mg bd only if Pseudomonas confir med)
STOP ciprofloxacin after 48 hours if no gram
negative bacteria on cultures. Continue
vancomycin alone until cultures available then
discuss with infection specialist.
IV Antibiotic Administration Guidance:
Antibiotic Dose Administration Prolonged surgery >1.5L blood loss redose
(time from administration of initial dose) after fluid replacement
Co-amoxiclav 1.2g Bolus over 3-5 minutes 1.2g to be repeated every 4 hours* 1.2g
Co-trimoxazole 960mg Infusion over 60 minutes Redose 480mg after 8 hours ** 480mg
Dilute each 480mg/5ml vial in
125ml sodium chloride 0.9%
Metronidazole 500mg Infusion over 20 minutes Redose 500mg after 8 hours 500mg
Vancomycin*** 1g Infusion over 100 - 120 minutes Redose 1g after 12 hours 500mg
(FOR PRIMARY in 250ml sodium chloride 0.9%
SURGERY)
Ciprofloxacin 400mg Infusion over 60 minutes Redose 400mg after 8 hours 200mg
See Fluoroquinolones
warnings document
Vancomycin*** Treatment dose required to ensure sufficient levels Continue treatment dose as calculated from local 50% of dose given initially
(FOR REVISION vancomycin guidance after 12 hours
SURGERY) LOADING dose in THEATRE as per infor mation in table above
MAINTENANCE doses on WARD 12-24 hours after loading dose calculated as per
guidance or calculator
* Locally it has been agreed that if the routine practice of the surgeon is to re-dose co-amoxiclav IV 1.2g after 2 hours or, in the case of a bilateral hip procedure, prior to incision on the 2nd
side, this is acceptable. The 2 additional doses at 8 and 16 hours post induction should also be given where indicated for the procedures above.
** There is no requirement to re dose co- trimoxazole at 2 hours or before incision on second side because it has a very long half life (9-11 hours at least). Developed by: AMG/Orthopaedic s
Approv ed: Nov 2012
*** Note if vancomycin is being used to treat a presumed or known infection the dosing should be as per the vancomycin guideline to ensure sufficient levels Updated: March 2013, May 2014 , March
2015, July 2015, Sept 2017
Rev iew: Sept 2019
Amended as per SAPG updated guidance
May 2019
References:
• SAPG Good Practice Recommendations for Surgical and Procedural Antibiotic Prophylaxis in Adults in NHS Scotland. https://www.sapg.scot/media/4109/good-practice-
recommendations- for-surgical-and-procedural-antibiotic-prophylaxis-in-adults-in-nhs-scotland.pdf [Accessed May 2019]
• SAPG Recommendations for Re-dosing Antibiotics for Surgical Prophylaxis. https://www.sapg.scot/media/4105/good-practice-recommendations-for-re-dosing-antibiotics-for-surgical-
prophylaxis.pdf [Accessed May 2019]
You might also like
- PDF Surgical Prophylaxis Poster Dec 2021Document1 pagePDF Surgical Prophylaxis Poster Dec 2021Midhun KishorNo ratings yet
- Surgical Site Infection (SSI)Document3 pagesSurgical Site Infection (SSI)Sahrul RiadiNo ratings yet
- AHS антибиотики рекомендацDocument42 pagesAHS антибиотики рекомендацMaksym DemianchukNo ratings yet
- Antibiotic PolicyDocument10 pagesAntibiotic Policykrutarth shahNo ratings yet
- Antibiotic Prophylaxis in Gustilo Grade I To III Open Fractures of The Lower LimbV5 - April18th2012Document1 pageAntibiotic Prophylaxis in Gustilo Grade I To III Open Fractures of The Lower LimbV5 - April18th2012Yopi ArdhiaswariNo ratings yet
- Antibiotics-Generation OperationDocument5 pagesAntibiotics-Generation OperationZamzami Ahmad FahmiNo ratings yet
- Guideline For Antimicrobial Use in The Orthopaedic and Trauma Department..Document8 pagesGuideline For Antimicrobial Use in The Orthopaedic and Trauma Department..Long Nguyễn HoàngNo ratings yet
- Antimicrobial Dosage Adjustments in Renal Impairment For FormularyDocument20 pagesAntimicrobial Dosage Adjustments in Renal Impairment For Formularyangkatanjuli2019No ratings yet
- SHC Open Fracture ABX Prophylaxis GuidelineDocument2 pagesSHC Open Fracture ABX Prophylaxis GuidelineAulia OkhidNo ratings yet
- Paediatric Cardiac Surgical Antibiotic Prophylaxis: PurposeDocument9 pagesPaediatric Cardiac Surgical Antibiotic Prophylaxis: PurposeZamzam DomaNo ratings yet
- Salbutamol Inhaler and Nebulizer InformationDocument36 pagesSalbutamol Inhaler and Nebulizer InformationlolabayNo ratings yet
- CH 8Document12 pagesCH 8Олександр РабошукNo ratings yet
- AntibiocardDocument25 pagesAntibiocardchildicuNo ratings yet
- Seminar On Standing Orders and Protocols and Use of Selected Life SavingDocument18 pagesSeminar On Standing Orders and Protocols and Use of Selected Life SavingmalathiNo ratings yet
- Antibiotics in NeurosurgeryDocument12 pagesAntibiotics in Neurosurgerylouglee9174100% (1)
- Paediatric Bone Infection GuideDocument11 pagesPaediatric Bone Infection GuideDorica GiurcaNo ratings yet
- Open Fracture Antibiotic RecommendationDocument16 pagesOpen Fracture Antibiotic RecommendationRana ScrubsNo ratings yet
- Rabbit Formulary: Inhalation AnestheticsDocument3 pagesRabbit Formulary: Inhalation AnestheticsMiriam CervantesNo ratings yet
- Pharmacology AnalgesicsDocument14 pagesPharmacology Analgesicsamasoud96 amasoud96No ratings yet
- Antivenom Therapy SBG2021Document5 pagesAntivenom Therapy SBG2021anju sulishaNo ratings yet
- 5 TFC 3 Ig PDFDocument49 pages5 TFC 3 Ig PDFLMadeiraNo ratings yet
- Tramadol Plus ParacetamolDocument2 pagesTramadol Plus ParacetamolKeir Mrls ForcadillaNo ratings yet
- Use of Muscle Relaxants in Feline Ophthalmic Anesthesia - Surgery - Veterinary Anesthesia Update - VINDocument3 pagesUse of Muscle Relaxants in Feline Ophthalmic Anesthesia - Surgery - Veterinary Anesthesia Update - VINCristian FloreaNo ratings yet
- Surgical Antibiotic Prophylaxis Guideline 220719Document7 pagesSurgical Antibiotic Prophylaxis Guideline 220719MuathNo ratings yet
- P - O M I S: OST P Edication Nformation HeetDocument1 pageP - O M I S: OST P Edication Nformation HeetSarah Catherine WalkerNo ratings yet
- Amoxicillin - Drug Information - UpToDateDocument47 pagesAmoxicillin - Drug Information - UpToDateMikaela lNo ratings yet
- Antibiotic Prophylaxis in Orthopedic Surgery: GeneralDocument4 pagesAntibiotic Prophylaxis in Orthopedic Surgery: GeneralWiindha Tahta Alfina CiigejeeNo ratings yet
- 2010 Guías de Manejo de Anticoag en Proced EndoscópicosDocument15 pages2010 Guías de Manejo de Anticoag en Proced EndoscópicosSantiago AlonsoNo ratings yet
- TCCC Guidelines August 2011Document12 pagesTCCC Guidelines August 2011OnTheXNo ratings yet
- SQC ABx Guidelines 2-21-2011 PDFDocument2 pagesSQC ABx Guidelines 2-21-2011 PDFMinh SteveNo ratings yet
- Recommendation For The Use of Antibiotics For The Treatment of InfectionDocument5 pagesRecommendation For The Use of Antibiotics For The Treatment of InfectionGem BorjaNo ratings yet
- Pediatric Guidelines For Medications PDFDocument24 pagesPediatric Guidelines For Medications PDFLaylatan NurNo ratings yet
- Indocollyre 0.1% Eye Drops Summary of Product CharacteristicsDocument6 pagesIndocollyre 0.1% Eye Drops Summary of Product CharacteristicsUpik MoritaNo ratings yet
- Antibiotic Guidelines For BONE AND JOINT INFECTIONSDocument3 pagesAntibiotic Guidelines For BONE AND JOINT INFECTIONSKhurram NadeemNo ratings yet
- Bone and Joint Infection Treatment GuidelinesDocument3 pagesBone and Joint Infection Treatment GuidelinesDanissa Fidia PuteriNo ratings yet
- 15.guidelines COPDDocument5 pages15.guidelines COPDRed DevilNo ratings yet
- Antimicrobial Drug Interactionstable220716 PDFDocument4 pagesAntimicrobial Drug Interactionstable220716 PDFBhavin DesaiNo ratings yet
- Effects of atracurium besylateDocument3 pagesEffects of atracurium besylateWidya WidyariniNo ratings yet
- Complications of Chemotherapeutic DrugsDocument64 pagesComplications of Chemotherapeutic DrugsJulienne Sanchez-SalazarNo ratings yet
- Face Fracture Treatment & Management: Prehospital CareDocument7 pagesFace Fracture Treatment & Management: Prehospital Caremafoel39No ratings yet
- Clinical Pharmacology - Minimizing Adverse Effects of DrugsDocument7 pagesClinical Pharmacology - Minimizing Adverse Effects of DrugshalesNo ratings yet
- ANTIBIOTIC POLICY FOR Sassoon Hospital & BJGMC, PuneDocument32 pagesANTIBIOTIC POLICY FOR Sassoon Hospital & BJGMC, Puneshah007zaadNo ratings yet
- Addison's Surgicalguidelines BWDocument1 pageAddison's Surgicalguidelines BWHanifan AuliaNo ratings yet
- Antibiotics in Surgery: July 2010Document31 pagesAntibiotics in Surgery: July 2010louglee9174No ratings yet
- Tranexamic Acid Injection 500 MG/ 5 ML Ampoule New Zealand Data SheetDocument18 pagesTranexamic Acid Injection 500 MG/ 5 ML Ampoule New Zealand Data SheetHatim DziauddinNo ratings yet
- Antibiotics in ENT Surgery: Magdy M. Amin RIADDocument57 pagesAntibiotics in ENT Surgery: Magdy M. Amin RIAD1974sathyaNo ratings yet
- EC-DH Epirubicin Cyclophosphamide Followed by Docetaxel With Trastuzumab Protocol V1.1Document11 pagesEC-DH Epirubicin Cyclophosphamide Followed by Docetaxel With Trastuzumab Protocol V1.1smokkerNo ratings yet
- VIDE v3Document3 pagesVIDE v3gonococo29No ratings yet
- TCCC Guidelines September 2012Document14 pagesTCCC Guidelines September 2012Valentin GlezNo ratings yet
- Neuromuscular Blocking Drugs and Anticholinesterases UpdateDocument4 pagesNeuromuscular Blocking Drugs and Anticholinesterases UpdateAuliaNo ratings yet
- Efficacy of Postoperative Analgesia of Local Ketamine Wound Instillation Following Total ThyroidectomyDocument20 pagesEfficacy of Postoperative Analgesia of Local Ketamine Wound Instillation Following Total ThyroidectomyCristina RamirezNo ratings yet
- Antibiotic Prophylaxis in Surgery GuideDocument5 pagesAntibiotic Prophylaxis in Surgery GuideKhairul MustafaNo ratings yet
- 2 - RevisedJointProtocol6!26!08Document3 pages2 - RevisedJointProtocol6!26!08Julianus YudhisNo ratings yet
- Treating Tetanus: Support, Wound Care, AntitoxinsDocument11 pagesTreating Tetanus: Support, Wound Care, AntitoxinsFuad Adi PrasetyoNo ratings yet
- OB Hem Uterotonic Medications For Prevention and Treatment of PPHDocument7 pagesOB Hem Uterotonic Medications For Prevention and Treatment of PPHpwytymbm56No ratings yet
- Medical ManagementDocument2 pagesMedical ManagementnickanelNo ratings yet
- Icu Antibiotic GuidelinesDocument4 pagesIcu Antibiotic GuidelinesTia MonitaNo ratings yet
- Ultrasound and clinically guided Injection techniques on the musculoskeletal systemFrom EverandUltrasound and clinically guided Injection techniques on the musculoskeletal systemNo ratings yet
- EVALUATION OF THE INFLUENCE OF TWO DIFFERENT SYSTEMS OF ANALGESIA AND THE NASOGASTRIC TUBE ON THE INCIDENCE OF POSTOPERATIVE NAUSEA AND VOMITING IN CARDIAC SURGERYFrom EverandEVALUATION OF THE INFLUENCE OF TWO DIFFERENT SYSTEMS OF ANALGESIA AND THE NASOGASTRIC TUBE ON THE INCIDENCE OF POSTOPERATIVE NAUSEA AND VOMITING IN CARDIAC SURGERYNo ratings yet
- Bowel Prep CPG 2019Document6 pagesBowel Prep CPG 2019Ogbonnaya IfeanyichukwuNo ratings yet
- 727 Outcomes of Antibiotic Use in Ischemic ColitisDocument2 pages727 Outcomes of Antibiotic Use in Ischemic ColitisDonNo ratings yet
- Role of Postoperative Antibiotics After Appendectomy in Non-Perforated AppendicitisDocument4 pagesRole of Postoperative Antibiotics After Appendectomy in Non-Perforated AppendicitisDonNo ratings yet
- 727 Outcomes of Antibiotic Use in Ischemic ColitisDocument2 pages727 Outcomes of Antibiotic Use in Ischemic ColitisDonNo ratings yet
- 203 FullDocument7 pages203 FullDonNo ratings yet
- 203 FullDocument7 pages203 FullDonNo ratings yet
- Disaster Management-Group 2Document90 pagesDisaster Management-Group 2Kavitha ArjunNo ratings yet
- Respiratory Disease Anatomy and Phys Sheridan CollegeDocument7 pagesRespiratory Disease Anatomy and Phys Sheridan CollegeAudrey AndinoNo ratings yet
- Daftar PustakaDocument13 pagesDaftar PustakaYUNINDA LOVIANA ERSIANTINo ratings yet
- Miguel Pocholo Matundan - Life Expectancy CalculatorDocument2 pagesMiguel Pocholo Matundan - Life Expectancy CalculatorAnne Marieline BuenaventuraNo ratings yet
- AZ01-20 MediSafe Infinite+ AZ0120 Co No FA PDFDocument27 pagesAZ01-20 MediSafe Infinite+ AZ0120 Co No FA PDFMatthew Bisset TeMaroNo ratings yet
- Disaster Readiness and Risk Reduction: Disasters and Its Effects Learning From Weakness Why Us? Not Others?Document8 pagesDisaster Readiness and Risk Reduction: Disasters and Its Effects Learning From Weakness Why Us? Not Others?Eli67% (12)
- Final Oral Pathology ExamDocument5 pagesFinal Oral Pathology Examsolom islamNo ratings yet
- Melinda Smith, M.A., Lawrence Robinson, and Jeanne Segal, PH.D, Sehar Shoukat, Sophia, Sarah, John M. Grohol, Psy.DDocument5 pagesMelinda Smith, M.A., Lawrence Robinson, and Jeanne Segal, PH.D, Sehar Shoukat, Sophia, Sarah, John M. Grohol, Psy.DZhang PeilinNo ratings yet
- Bailey's Head and Neck Surgery Otolaryngology - (PG 1032 - 2032)Document1,001 pagesBailey's Head and Neck Surgery Otolaryngology - (PG 1032 - 2032)loliklesmanaNo ratings yet
- Recommended Procedures For Doctors and Nurse in The Management of Kawasaki DiseaseDocument34 pagesRecommended Procedures For Doctors and Nurse in The Management of Kawasaki DiseaseJOSHUA DICHOSONo ratings yet
- Neonatal assessment essentialsDocument91 pagesNeonatal assessment essentialsSHAFIQNo ratings yet
- Hemo DynamicsDocument70 pagesHemo Dynamicsansam shawabkehNo ratings yet
- Addiction and Emotionally Focused Couple TherapyDocument218 pagesAddiction and Emotionally Focused Couple TherapyOlesya BoyerNo ratings yet
- Assessment Diagnosis Inference Planning Intervention Rationale Evaluation SubjectiveDocument4 pagesAssessment Diagnosis Inference Planning Intervention Rationale Evaluation SubjectiveDivina Gracia Vibal CieloNo ratings yet
- All BacteriaDocument14 pagesAll Bacteriamorale28100% (2)
- 7 Myths About ADHD - DebunkedDocument1 page7 Myths About ADHD - DebunkedDalila VicenteNo ratings yet
- Introduction To Technical Writing in The ProfessionsDocument22 pagesIntroduction To Technical Writing in The ProfessionsDeborah Grace ApiladoNo ratings yet
- Managing Health and Safety in HealthcareDocument56 pagesManaging Health and Safety in HealthcareKamlesh KumarNo ratings yet
- Intestinal Surgery in Small Animals - How To Prevent It Leaking?Document5 pagesIntestinal Surgery in Small Animals - How To Prevent It Leaking?Ayu DinaNo ratings yet
- Sources of Stem CellsDocument13 pagesSources of Stem CellsAnshi AroraNo ratings yet
- 10 Facts About HealthcareDocument2 pages10 Facts About HealthcareMat Domdom V. SansanoNo ratings yet
- Assessing Newborns and InfantsDocument16 pagesAssessing Newborns and InfantsCrestyl Faye R. CagatanNo ratings yet
- Rajkumari Amrit Kaur College of Nursing: Lesson Plan On Infection Prevention and Control MeasuresDocument18 pagesRajkumari Amrit Kaur College of Nursing: Lesson Plan On Infection Prevention and Control MeasuresIshwar Das100% (2)
- Hymenolepis Nana Life Cycle and TreatmentDocument2 pagesHymenolepis Nana Life Cycle and TreatmentJacque TorresNo ratings yet
- Preprints Review 1marzoDocument61 pagesPreprints Review 1marzoJorgelina BernetNo ratings yet
- Herbs CampDocument42 pagesHerbs CampJohn JohnNo ratings yet
- Treating RSV Pneumonitis in InfantsDocument6 pagesTreating RSV Pneumonitis in InfantsIja Lourice RosalNo ratings yet
- Nonalcoholic Steatohepatitis. Review JAMA March 2020Document9 pagesNonalcoholic Steatohepatitis. Review JAMA March 2020Luis Henrique SalesNo ratings yet
- Case Study 14 NAFLD Liver DiseaseDocument6 pagesCase Study 14 NAFLD Liver DiseaseRuihan LI67% (3)
- PD Week 5Document7 pagesPD Week 5DAPHNEE MAE AGUDONGNo ratings yet