Professional Documents
Culture Documents
First Semester 2020-2021 Study Guide: University of The Cordilleras
Uploaded by
Jonalyn EtongOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
First Semester 2020-2021 Study Guide: University of The Cordilleras
Uploaded by
Jonalyn EtongCopyright:
Available Formats
RLE Skills Lecture
First Semester 2020-2021
Study Guide
University of the Cordilleras
College of Nursing
Hanna Lee H Antonio- UC Faculty
Oropharyngeal and Endotracheal Suctioning
UC-CON NCM 112 lecture Course
RLE Skills Lecture
Introduction
Suctioning is one of the nursing roles which is important in promoting patent
airway for clients and preventing ventilator associated pneumonia (VAP). The
upper airway warms, cleans and moistens the air we breathe. The trach tube
bypasses these mechanisms, so that the air moving through the tube is cooler,
dryer and not as clean. In response to these changes, the body produces
more mucus. Suctioning clears mucus from the tracheostomy tube and is
essential for proper breathing. Also, secretions left in the tube could become
contaminated and a chest infection could develop. Avoid suctioning too
frequently as this could lead to more secretion buildup.
Learning objectives
1. After the course the students will be able to:
a. Perform oropharyngeal suctioning
b. Perform endotracheal suctioning
c. Maintain aseptique technique in all procedures
2. Students will understand deeply the importance of nursing
interventions and their roles as nurses in the management of of
clients with endotracheal or tracheostomy tubes.
3. Identify the interventions and precautionary measures in
performing correct procedures when doing suctioning.
4. Students will be able to conduct health promotion activities in
combating the spread of infectious disease as well as practicing
infection control.
Key concepts
Tracheostomy tube:
UC-CON NCM 112 lecture Course
RLE Skills Lecture
Suction machine and suction
tip
Oropharyngeal and Nasopharyngeal Suctioning
The nurse sometimes needs to do suctioning to clear the airway (oropharynx
and nasal passages) for those who have difficulty swallowing and
expectorating secretions.
Suctioning: This is the process of aspirating secretions, often through a rubber
or polyethylene catheter connected to a suction machine or wall outlet.
Note: It is recommended that sterile technique be used for all suctioning, so
that microorganisms are not introduced into the pharynx where bacteria can
multiply and move into the trachea and bronchi causing infections or
complications. This is particularly important to delibitated clients, who are
more susceptible to infections.
UC-CON NCM 112 lecture Course
RLE Skills Lecture
Types of catheter:
1. Open-tipped: has an opening at the end and several along the sides to
distribute the negative pressure of the suction over the wide area, thus
preventing irritation of the respiratory mucosa. This effective for thick mucus
plugs but can irritate tissues.
2. Whistle-tipped: This has a slanted opening at the tip.
Note: Most catheters have a thumb port on the side, which is used to control
suctions.
The suction apparatus includes:
Collection bottle
Tubing system connected to the suction catheter
Gauge that registers the degree of suction
Deeper suctioning (called endotracheal suctioning): removes secretions from
the trachea and the bronchi. This requires more skill and usually carried by a
critical nursing specialist or an experienced nurse.
Suctioning of the upper airways is indicated to:
Inability to cough secretions
Unable to swallow
Makes light bubbling or rattling breath sounds
Possible complications of suctioning:
Irritation of the mucous membranes by suction (increase secretions)
Cause hypoxia
Purposes of suctioning:
Remove secretions tat obstruct the airways
To facilitate respiratory ventilation
To obtain secretions for diagnostic purposes
To prevent infections from accumulated secretions
Note: Sterile suction catheter sizes: #12- #18 Fr.- adults, #8-#10 Fr.- children,
#5-#8 Fr.- infants
TWO methods of suctioning:
see link at https://tracheostomyeducation.com/suctioning/
The two methods of ET tube suctioning are the open-suctioning method and
the closed-suctioning method. Open suctioning involves a sterile, single-use
catheter and sterile gloves The catheter is attached to suction tubing that
UC-CON NCM 112 lecture Course
RLE Skills Lecture
connects to a suction regulator. Open suctioning requires disconnecting the
neonate from the ventilator.
Closed suctioning (Ballard) involves insertion of a Y-connector into the
ventilator circuit without t disconnection from the ventilator.2 Closed suction
technique uses a specially designed, multiple-use catheter that is enclosed in
a sterile plastic sleeve and attaches to suction tubing that is connected to a
suction regulator. The catheter is placed inline between the ventilator circuit
and the ET tube. Disconnecting the neonate from the ventilator results in loss
of positive end-expiratory pressure (PEEP) and risk of contamination of the
system, leading to ventilator-associated pneumonia. The closed suction
system maintains PEEP and prevents contamination.
Note:
Closed suctioning is helpful when frequent suctioning is required.
The inability to pass a suction catheter indicates the airway is not patent.
The entire tracheostomy tube may need to be changed if replacing the
inner cannula still does not allow the suction catheter to pass.
Nursing Interventions
1. Prepare the client
a. explain procedure (invasive, painless, relieves BOB, and stimulates
cough, gag, or sneeze reflex
b. position conscious person with functional gag reflex in semi-Fowler’s
with the head turned on the side for ORAL suctioning
c. place with the neck hyperextended fro nasal suctioning
Note: positioning of clients prevents aspiration of secretions
d. position unconscious clients in lateral position facing the nurse; then
place towel or moisture resistant pad over the pillow or under the
chin
Note: This allows the tongue to fall forward, so that it will not
obstruct the catheter on insertion. This facilitates drainage of
secretions from the pharynx and prevents aspiration.
2. Prepare the equipment
a. Set the pressure gauge
Wall unit
Adult: 100-120 mmHg
Child: 95-110 mmHg
Infant: 50-95 mmHg
Portable unit
Adult: 10-15 mmHg
Child: 5-10 mmHg
Infant: 2-5 mmHg
b. Sterile technique at all times
UC-CON NCM 112 lecture Course
RLE Skills Lecture
3. Make an appropriate measure of the depth for the insertion of the catheter
and test the equipment.
a. Measure the distance between the tip of the nose and the earlobe
(about 13 cm or 5 in for an adult).
b. Mark position of the tube
c. Check patency of catheter
4. Lubricate and introduce the catheter
a. Nasopharyngeal suction: lubricate with sterile water, saline, or
water-based lubricant
b. Oropharyngeal suction: moisten the tip with sterile water or saline
(reduces friction and eases insertion)
Note:
DO NOT apply pressure during insertion of the suction
NEVER force to advance against an obstruction
Direct the catheter along the sides of the mouth in
oropharyngeal to prevent gagging
5. Perform suctioning
a. Apply suction and gently rotate the catheter (prevents trauma)
b. Intermittent suction for 5-10 seconds (rotate and remove hand from
suction control before removing)
6. Clean the catheter, and repeat the suctioning
a. Flash and clean with saline water
b. Use different suctions for the nasal and oral
c. Alternate nares for repeated suctioning
7. Encourage the client to breathe deeply and to cough between secretions
Note: Coughing and deep breathing help carry secretions from the trachea
and bronchi to the pharynx for easier suctioning.
8. Obtain specimen if required.
a. Use a sputum trap: this will collect mucus during suctioning
9. Promote client comfort.
a. Offer oral and nasal hygiene
b. Position to facilitate breathing
10. Dispose of equipment and ensure availability for the next suction
11. Assess effectiveness of suctioning
a. Auscultate breath sounds
12. Document relevant data
a. Amount, consistency, color, and odor of sputum
Endotracheal Suctioning
UC-CON NCM 112 lecture Course
RLE Skills Lecture
Is similar to pharyngeal suctioning but catheter is inserted further to the
trachea and the bronchi. For an adult, it is usually inserted 20 cm or 8 in. To
ascertain correct procedures for nasal tracheal suctioning:
a. MEASURE distance from the tip of the nose to the earlobe and their along side
of the neck to the thyroid cartilage (Adams apple); for ORAL tracheal
suctioning, measure from the mouth to the midsternum.
Note: Always premeasured to get correct length and avoid trauma during
cautioning specially to children.
b. Have the client INHALE while you INSERT the catheter facilitates entry to the
trachea making the epiglottis open during inhalation.
c. HYPEREXTENDING the neck and extending the tongue open places the glottis
in line with the trachea rather that the esophagus.
d. If the catheter needs to be inserted on one or both of the bronchi: turn the
client’s head into the left for the left bronchi and right for the right bronchi.
Note: Tracheal and bronchial suctioning should be done INTERMITTENTLY, and
the catheter should remain on the client not more than 10 secs to prevent
hypoxemia and cardiopulmonary complications.
Artificial airways: are inserted to maintain a patent airway during obstruction.
The common types of intubation:
1. Oropharyngeal intubation: done frequently for clients who are on general
anesthesia, semiconscious and are likely to obstruct their own airways through
their tongue. In some instance, are inserted for pharyngeal suctioning.
Note: It is NOT inserted to conscious clients because it stimulates the gag
reflex causing vomiting. Usually an S-shaped and made of plastics. Inserted
into the mouth and terminates in the posterior pharynx.
Nursing interventions
a. Maintain the client into a lateral or semi-prone position so that
blood, vomitus, and mucus will drain out of the mouth and prevent
aspirations.
b. Remove he airway once the client has regained consciousness and
has the swallow, GAG, and cough reflexes.
2. Nasopharyngeal intubation: is carried out if the oropharygeal route is
contraindicated, for example, following oral surgery, or to protect the nasal
and pharyngeal mucosa during nasopharyngeal or nasotracheal
suctioning.the tube is inserted through the nostrils and terminates into the
pharynx, below the upper edge of the epiglottis. To insert the tube, lubricate
entire tube with topical anesthesia to prevent irritation and discomfort.
Nursing interventions:
UC-CON NCM 112 lecture Course
RLE Skills Lecture
a. Remove tube, and insert in the other nostril at least every 8 hours, or
as ordered by the physician, or more often to prevent irritation of
the mucosa.
b. Provide nasal hygiene every 4 hours or more often if needed.
c. Monitor the client closely for stimulation of the vagus nerve if
nasotracheal suctioning is carried out. Vagal stimulation can lead
to cardiac arrest.
3. Endotracheal tubes: are most commonly inserted for clients in general
anesthetics or for those emergency situations where mechanical ventilation is
required. The tube is inserted through either the mouth of the nose and into
the trachea with the aid of a laryngoscope. The tube terminates just superior
to the bifurcation of the trachea into the bronchi. Because an ET passes
through the epiglottis and splits it open, an inflated cuff is needed to close the
system.
Note: Only nurses with special preparation are allowed to perform ET
intubation.
Nursing interventions
a. Maintain the client in a lateral or semiprone position so that blood, vomitus, or
secretions can drain from the mouth and are not aspirated.
b. Provide nasal or oral hygiene every 3 hours or as needed.
c. For an oral insertion, provide a bite block so that the client cannot bite the
tube and occlude the airway.
d. Assess the condition of the nasal or oral mucosa for irritation, and notify the
physician should the need to change a nasal ET arise; reposition an oral ET
from one side of the mouth to the other every 8 hours as required.
e. Closely monitor the air pressure in the ET cuff. If it is greater than 20 mmHg,
necrosis of the tracheal tissues may result.
f. Tape the airway in place to prevent accidental slippage or extubation.
g. Change the tape daily, and position the tube on the opposite side at each
change.
h. Provide continous humidification or aerosaol therapy to prevent undue drying
and irritation of the mucosa if the tube is left more than days or weeks.
i. Deflate and reinflate the cuff according to the manufaturer’s directions.
j. Communicate frequently with the client, and provide notepad or other
means for the client to communicate. Most clients cannot speak with the
inflated cuff, because no air can Passover the vocal chords.
4. Tracheostomy tubes: are inserted to provide and maintain a patent airway, to
remove tracheobronchial secretions from the clients unable to cough, to
replace ETs, to permit the use of positive pressure ventilation, and to prevent
unconscious clients from aspirating secretions. A tracheostomy tube is a curve
tube inserted into a tracheostomy, a surgical incision in the trachea just below
the first or second tracheal cartilage. The tube extends to through the
tracheostomy stoma into the trachea.
Parts of tracheostomy tube:
UC-CON NCM 112 lecture Course
RLE Skills Lecture
a. Outer tube: usually have ties to secure it around the neck, although plastic
tubes are cuffed with a soft balloon that can be inflated to hold the tube in
place.
b. Inner tube or inner cannula: fitted inside the outer tube (some plastic sets do
not have this because it is unnecessary to change the tube, and are called
single cannula tubes). In double cannula sets, the inner cannula is inserted
and locked in place after the obturator is removed; it acts as a removable
liner for the more permanent, or removable cannula. The inner tube is
withdrawn only for brief periods to be cleaned.
c. Obturator: only used to insert the outer tube and then removed once in
placed.
Things to remember:
Cuffed tracheostomy tubes: surrounded by inflatable cuff that
produces an airtight seal between the tube and the trachea.
This seal prevents aspiration of oropharyngeal secretions and air
leakage between the tube and the trachea. Cuffed tubes are
often used immediately after a tracheostomy in adults and
infants and are essential when ventilating a tracheostomy client
with a ventilator. Children do not require cuffed tubes, because
their trachea is resilient enough to seal the air space around the
tube.
Some tubes have high pressure cuffs; others have low pressure
cuffs; these can be inflated alternately to alter the pressure
points on to the trachea and prevent tracheal irritation and
tissue damage. Alternate inflation also allows uninterrupted
respirator function for people using ventilators.
Cuffs that are bonded to the tracheostomy tube eliminate the
risk of accidental detachment inside the trachea.
Low- pressure cuffs are costly but distribute a low, even pressure
against the tracheal wall decreasing risk for necrosis. They do
not need to be deflated periodically and prevents pressure to
the tracheal walls.
Double cuffed- high-pressure-tubes may reduce the risk of tissue
necrosis with alternate inflation of cuffs, but only if there is
adherence to the alternate inflation schedules. If tracheal
damage does occur, a larger area of the trachea is involved
with a double-cuffed tube.
Foam cuff does not require injected air; instead when the port is
opened. Ambient air enters the balloon, which then confirms to
the client’s trachea. The physician removes air from the cuff
prior to insertion or removal of the tube.
Complications of suctioning:
1. Hypoxemia
2. Trauma to the airway
3. Nosocomial infection
4. Cardiac dysrhythmia
5. Stimulates cough reflex resulting to increase secretions
UC-CON NCM 112 lecture Course
RLE Skills Lecture
Note: For the endotracheal and tracheostomy suctioning, the diameter of the
suction catheter should be about half the inside diameter of the
tracheostomy tube so that the hypoxia can be prevented. The nurse should
use sterile technique to prevent infection of the respiratory tract.
SUCTIONING A TRACHEOSTOMY
1. Prepare the client
Intermittent coughing
DBE: semi-fowlers position
2. Prepare the equipment
3. Flush and lubricate the catheter
4. If the client does not have copious secretions, hyperventilate the resuscitation
bag before suctioning.
5. If the client has copious secretions, DO NOT hyperventilate INSTEAD: Keep the
regular oxygen delivery device on, and increase the liter flow for few minutes
before suctioning. HYPERVENTILATING can force the secretions deeper into
the lungs.
6. Quickly, but gently, insert the catheter without applying any suction.
7. Perform suctioning.
8. If secretions are thick, flush the catheter and perform tracheal lavage
according to the agency protocol.
9. Reassess the client’s oxygenation status, and repeat suctioning as above.
10. 10. Dispose of equipment and ensure availability for the next suction.
11. 11. Provide client comfort and safety.
12. Document relevant data.
Learning resources
1. https://www.youtube.com/watch?v=zFq63SA7jsE
2. https://www.youtube.com/watch?v=IftM_1TNaWE
3. https://www.youtube.com/watch?v=TUxQCPhaYbc
4. Fundamental of Nursing by Kozier, 5th edition
Study questions
The students will be asked of the following to identify their ideas about the
procedures.
1. What is Suctioning?
2. What are the indications when to perform suctioning?
3. What are the expected complications?
4. What are the nurse’s important roles and interventions in caring
a client with tracheostomy?
Learning activities
Activity 1: Assignment
Watch the video on Endotracehal suctioning for pediatric clients by
accessing
UC-CON NCM 112thelecture
link provided
Course below. What are the observations you
have notice when they perform these procedures? Make a
comparison on the differences and similarities.
RLE Skills Lecture
UC-CON NCM 112 lecture Course
RLE Skills Lecture
Activity 2: Reading assignment
What are the complications expected when performing suctioning
procedures?
__________________________________________________________________________
__________________________________________________________________________
__________________________________________________________________________
__________________________________________________________________________
__________________________________________________________________________
__________________________________________________________________________
_______________________________________________.
Enumerate the supplies needed.
__________________________________________________________________________
__________________________________________________________________________
__________________________________________________________________________
__________________________________________________________________________
__________________________________________________________________________
__________________________________________________________________________
_______________________________________________.
How was aseptique technique demonstrated on this procedures?
__________________________________________________________________________
__________________________________________________________________________
__________________________________________________________________________
__________________________________________________________________________
__________________________________________________________________________
__________________________________________________________________________
__________________________________________________________________________
____________________.
Summary
At the end of the course the students have learned the following principles on:
1. Definition of suctioning
2. Differences of intermittent and continous suctioning
3. Identify the parts of a tracheostomy tube
4. Identify complications of suctioning
5. Enumerate the supplies needed for suctioning
6. Demonstrate proper suctioning procedures
7. Identify the appropriate nursing management throughout procedures.
UC-CON NCM 112 lecture Course
RLE Skills Lecture
References
1. https://www.youtube.com/watch?v=zFq63SA7jsE
2. https://www.youtube.com/watch?v=IftM_1TNaWE
3. https://www.youtube.com/watch?v=TUxQCPhaYbc
4. Fundamental of Nursing by Kozier, 5th edition
5. https://www.hopkinsmedicine.org/tracheostomy/living/suctioning.ht
ml
6. https://www.elsevier.com/__data/assets/pdf_file/0012/996753/Endot
racheal-Tube-Closed-Suctioning-Skill-Neonatal-_030420.pdf
7. https://tracheostomyeducation.com/suctioning/
UC-CON NCM 112 lecture Course
You might also like
- Human Biology Lecture NotesDocument6 pagesHuman Biology Lecture NotesGrace Melissa ChoiNo ratings yet
- A Mortal Man’s Guide to Building a Better Upper ChestDocument101 pagesA Mortal Man’s Guide to Building a Better Upper ChestGianniNo ratings yet
- Fundamentals of Nursing: OxygenationDocument56 pagesFundamentals of Nursing: OxygenationFEVIE ANNE BANATAONo ratings yet
- Blair Upper CervicalDocument4 pagesBlair Upper Cervicallopezhectora100% (1)
- Lalpath Shruti ThrroidDocument2 pagesLalpath Shruti ThrroidSatish SrivastavaNo ratings yet
- Evidenced Based ExercisesDocument16 pagesEvidenced Based ExercisesJonalyn EtongNo ratings yet
- Nasm-Cpt Assessment Solutions Table Cpt6-Update PDFDocument1 pageNasm-Cpt Assessment Solutions Table Cpt6-Update PDFNguyễn Tài Đức100% (2)
- VOL 3 - Layout 1Document596 pagesVOL 3 - Layout 1Raluca Crina100% (1)
- Week 3Document7 pagesWeek 3Margarita Kotova100% (2)
- Nasogastric TubeDocument78 pagesNasogastric TubeQuia Benjch Uayan100% (1)
- Maternal Quiz 2Document24 pagesMaternal Quiz 2Aaron ConstantinoNo ratings yet
- Patient Positioning in Operating TheatreDocument52 pagesPatient Positioning in Operating TheatreFatkhul AdhiatmadjaNo ratings yet
- Anatomy of Nervous TissueDocument54 pagesAnatomy of Nervous TissueNand PrakashNo ratings yet
- Head and NeckDocument11 pagesHead and NeckdrsamnNo ratings yet
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Understanding the Concept of Srotas in AyurvedaDocument112 pagesUnderstanding the Concept of Srotas in AyurvedaSanjana SajjanarNo ratings yet
- EMERGENCY DRUGSDocument7 pagesEMERGENCY DRUGSJohn Balgoa100% (2)
- Basic Body Mechanics Moving & Positioning: Nursing 114A Care of The Older AdultsDocument44 pagesBasic Body Mechanics Moving & Positioning: Nursing 114A Care of The Older AdultsJonalyn EtongNo ratings yet
- ThyroidDocument84 pagesThyroidMeLissa Pearl GuillermoNo ratings yet
- Cardiac MonitoringDocument19 pagesCardiac MonitoringYaska Musa100% (1)
- MCN II AntepartumDocument28 pagesMCN II AntepartumJharaNo ratings yet
- Naso Orogastric Tube Guideline For The Care of Neonate Child or Young Person RequiringDocument12 pagesNaso Orogastric Tube Guideline For The Care of Neonate Child or Young Person RequiringmeisygraniaNo ratings yet
- 8 Irrigating A ColostomyDocument5 pages8 Irrigating A ColostomyAnn Jalover PerezNo ratings yet
- Administering Enema POWERPOINT GIVING ENEMA TO PATIENT, FOR PATIENT WITH GASTROINTESTINAL DISORDERS .. LECTURES, PRINCIPLES AND PROCEDURESDocument14 pagesAdministering Enema POWERPOINT GIVING ENEMA TO PATIENT, FOR PATIENT WITH GASTROINTESTINAL DISORDERS .. LECTURES, PRINCIPLES AND PROCEDURESPb0% (1)
- Core Elements of Evidence-Bases Gerontological Nursing PracticeDocument15 pagesCore Elements of Evidence-Bases Gerontological Nursing PracticeGrape Juice67% (3)
- National Core Competency StandardsDocument89 pagesNational Core Competency Standardsverna100% (1)
- Republic Act No. 9994 - Expanded Senior Citizens ActDocument29 pagesRepublic Act No. 9994 - Expanded Senior Citizens ActJumen Gamaru TamayoNo ratings yet
- Excretory System NotesDocument10 pagesExcretory System Noteswama ojha100% (1)
- SuctioningDocument31 pagesSuctioningmelanie silvaNo ratings yet
- Tonsillectomy - ORDocument3 pagesTonsillectomy - ORRich John Mercene-NewNo ratings yet
- 11 Core CompetenciesDocument8 pages11 Core CompetenciesJune TorrionNo ratings yet
- Socio-Cultural Aspects of Maternal and Child NursingDocument14 pagesSocio-Cultural Aspects of Maternal and Child NursingShauie CayabyabNo ratings yet
- Colostomy Irrigation ProcedureDocument24 pagesColostomy Irrigation ProcedureJan Federick Bantay100% (1)
- 3.chronic IllnessesDocument51 pages3.chronic IllnessesJonalyn EtongNo ratings yet
- Complication During PregnancyDocument43 pagesComplication During PregnancyRizza Domalaon BalangitanNo ratings yet
- Emergency NursingDocument5 pagesEmergency NursingDerick RanaNo ratings yet
- Disaster Nursing NotesDocument19 pagesDisaster Nursing NotesRoscelin LumenNo ratings yet
- Colostomy CareDocument13 pagesColostomy CareLord Pozak MillerNo ratings yet
- Cardio and Hema - DR PueyoDocument161 pagesCardio and Hema - DR Pueyoapi-3735995100% (2)
- Essential CHN Bag ContentsDocument36 pagesEssential CHN Bag ContentsRomeo RiveraNo ratings yet
- EENT Instillation and IrrigationDocument13 pagesEENT Instillation and Irrigationplebur100% (1)
- ER Nurse ResponsibilitiesDocument2 pagesER Nurse Responsibilitiesjasnate84No ratings yet
- Singapore Nursing Board Review PointersDocument18 pagesSingapore Nursing Board Review PointersRubelyn Arriola Nioko100% (1)
- Evolution of Nursing Research and Role of The Nurse in ResearchDocument3 pagesEvolution of Nursing Research and Role of The Nurse in ResearchAlmer OstreaNo ratings yet
- Or Return Demo FinalDocument2 pagesOr Return Demo FinallemuelNo ratings yet
- Congenital GenitourinaryDocument93 pagesCongenital GenitourinaryEllen AngelNo ratings yet
- At LTC N Theories Models 1Document35 pagesAt LTC N Theories Models 1Darin BransonNo ratings yet
- Skill Performance Evaluation - Measuring Intake and OutputDocument2 pagesSkill Performance Evaluation - Measuring Intake and OutputLemuel Que100% (1)
- Esarean Ction: Cadalin, Fremelen Rose Cedamon, CarloDocument18 pagesEsarean Ction: Cadalin, Fremelen Rose Cedamon, CarloMonette Abalos MendovaNo ratings yet
- VerA Ok-Prelim Ncm104 (Autosaved) VeraDocument30 pagesVerA Ok-Prelim Ncm104 (Autosaved) Verajesperdomincilbayaua100% (1)
- MCN SF Chapter 18 QuizDocument4 pagesMCN SF Chapter 18 QuizKathleen AngNo ratings yet
- HandwashingDocument35 pagesHandwashingJoyce Catherine Buquing UysecoNo ratings yet
- Nursing Skills ChecklistDocument6 pagesNursing Skills Checklistapi-433883631No ratings yet
- Handling Instruments During The Surgical ProcedureDocument4 pagesHandling Instruments During The Surgical ProcedureR-o-N-n-e-l100% (1)
- Nursing Practice Standards2Document25 pagesNursing Practice Standards2sunielgowdaNo ratings yet
- Post Op Worksheet FinalDocument5 pagesPost Op Worksheet FinalRiza Angela BarazanNo ratings yet
- ) Administering Nasogastric Tube or Orogastric Tube FeedingDocument6 pages) Administering Nasogastric Tube or Orogastric Tube FeedingJohn Pearl FernandezNo ratings yet
- Pentagon Review - Nursing ManagementDocument5 pagesPentagon Review - Nursing ManagementJay ReanoNo ratings yet
- Leopold'S Maneuver: DefinitionDocument3 pagesLeopold'S Maneuver: DefinitionJyra Mae TaganasNo ratings yet
- Nursing Interventions CHFDocument3 pagesNursing Interventions CHFbanyenye25100% (1)
- Pediatric Oncology Case StudyDocument12 pagesPediatric Oncology Case StudyromelynNo ratings yet
- Live Preterm Baby Delivered NSDDocument13 pagesLive Preterm Baby Delivered NSDKristine Anne SorianoNo ratings yet
- Assessing Uterine Contractions and Fetal Heart Rate During LaborDocument4 pagesAssessing Uterine Contractions and Fetal Heart Rate During LaborRegNo ratings yet
- Fluid Volume Deficit and Excess: Types, Causes, Signs and Nursing ManagementDocument32 pagesFluid Volume Deficit and Excess: Types, Causes, Signs and Nursing ManagementAcohCChaoNo ratings yet
- CHN Health Care Process PDFDocument9 pagesCHN Health Care Process PDFKathleen AngNo ratings yet
- Ctu CCMC Level 3 NCM 1Document15 pagesCtu CCMC Level 3 NCM 1Divina VillarinNo ratings yet
- Acute Respiratory InfectionsDocument18 pagesAcute Respiratory InfectionsEmilyRose17No ratings yet
- Intra-Abdominal Pressure: Causes, Symptoms and TreatmentDocument29 pagesIntra-Abdominal Pressure: Causes, Symptoms and TreatmentRoshin Mae E. TejeroNo ratings yet
- NCM 107 LAB: Catheterization Factors and ProceduresDocument4 pagesNCM 107 LAB: Catheterization Factors and ProceduresCatherine PradoNo ratings yet
- Oxygen TherapyDocument3 pagesOxygen Therapymarie100% (3)
- High-Risk Pregnancy Factors & CareDocument19 pagesHigh-Risk Pregnancy Factors & CareRoger Jr PumarenNo ratings yet
- Nso AbdurasadDocument4 pagesNso AbdurasadNader AbdurasadNo ratings yet
- Pathophysiology of ArrhythmiasDocument15 pagesPathophysiology of ArrhythmiasJonathan MontecilloNo ratings yet
- Perioperative Nursing CareDocument84 pagesPerioperative Nursing CaremarkyboiNo ratings yet
- CHN RVW 2Document51 pagesCHN RVW 2Michael UrrutiaNo ratings yet
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- WEEK 2-3 Mod.Document21 pagesWEEK 2-3 Mod.Jonalyn EtongNo ratings yet
- Step 2 of 4: Sources Ofinformatlon Formr. B'S Comprehensive AssessmentDocument3 pagesStep 2 of 4: Sources Ofinformatlon Formr. B'S Comprehensive AssessmentJonalyn EtongNo ratings yet
- Suction Equipment For Airway Clearance InstructionsDocument12 pagesSuction Equipment For Airway Clearance InstructionsJonalyn EtongNo ratings yet
- Understanding The Implications of Birth Weight: 28 DaysDocument5 pagesUnderstanding The Implications of Birth Weight: 28 DaysAdib FraNo ratings yet
- Hmole Case ReviewDocument5 pagesHmole Case ReviewJonalyn EtongNo ratings yet
- Hemodialysis TemplateDocument7 pagesHemodialysis TemplateJonalyn EtongNo ratings yet
- Hmole Case ReviewDocument5 pagesHmole Case ReviewJonalyn EtongNo ratings yet
- Abnormal Breathing PatternsDocument5 pagesAbnormal Breathing PatternsJonalyn EtongNo ratings yet
- Assessing Community Health NeedsDocument6 pagesAssessing Community Health NeedsJonalyn Etong0% (1)
- Epidemiology Public-Health-Key-TermsDocument1 pageEpidemiology Public-Health-Key-TermsJonalyn EtongNo ratings yet
- 7.1 Human Endocrine System - MEMO - ONE PAGER 2020Document1 page7.1 Human Endocrine System - MEMO - ONE PAGER 2020Rudzi UdziNo ratings yet
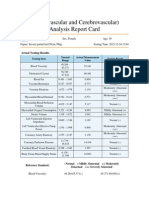
- Cardiovascular and CerebrovascularDocument6 pagesCardiovascular and CerebrovascularJoshelle B. Bancilo0% (1)
- Most Common CPT CodesDocument5 pagesMost Common CPT CodesKrishna KumarNo ratings yet
- Autonomic Nervous System (ANS)Document11 pagesAutonomic Nervous System (ANS)Prathmesh vetalNo ratings yet
- Stages of Mitosis under MicroscopeDocument21 pagesStages of Mitosis under MicroscopeOM CHAVANNo ratings yet
- Alternativas A TotalesDocument12 pagesAlternativas A TotalesJuan Jose Stuven RodriguezNo ratings yet
- HLTAAP001 Recognise Healthy Body System SAB v3.0 - THEORYDocument41 pagesHLTAAP001 Recognise Healthy Body System SAB v3.0 - THEORYSujan AdhikariNo ratings yet
- The MidbrainDocument3 pagesThe MidbrainAshly Kate AbarientosNo ratings yet
- CT of The Paranasal Sinuses Normal Anatomyvariants and PathologyDocument10 pagesCT of The Paranasal Sinuses Normal Anatomyvariants and PathologyAndi FirdaNo ratings yet
- Operative Otolaryngology Head and Neck SurgeryDocument7 pagesOperative Otolaryngology Head and Neck SurgeryTugce InceNo ratings yet
- Hierarchy of Organization: Associated SLODocument10 pagesHierarchy of Organization: Associated SLOZainne Sarip BandingNo ratings yet
- Lab Report 4 - Cardiovascular Physiology and Blood AgglutinationDocument17 pagesLab Report 4 - Cardiovascular Physiology and Blood AgglutinationHarith HaikalNo ratings yet
- Class 2 EVS (Lesson - 2) TermsDocument7 pagesClass 2 EVS (Lesson - 2) TermsRittwik MandalNo ratings yet
- Boney LandmarksDocument39 pagesBoney LandmarksStefanie Kiss-PlucasNo ratings yet
- Phono TEST 1Document2 pagesPhono TEST 1Thị Anh Thư LêNo ratings yet
- The Slump Test: Examining Spinal Pain and Range of MotionDocument5 pagesThe Slump Test: Examining Spinal Pain and Range of MotionNahu SteinmannNo ratings yet
- Week 3Document10 pagesWeek 3John Chris Villanueva100% (1)
- Physiology of Nerve Fibers: Dr. Zara BatoolDocument30 pagesPhysiology of Nerve Fibers: Dr. Zara BatoolZuhaib AhmedNo ratings yet