Professional Documents
Culture Documents
Multiple Sclerosis Neurogenic Bladder 10.1038@nrurol.2016.53
Uploaded by
Putri Rizky AmaliaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Multiple Sclerosis Neurogenic Bladder 10.1038@nrurol.2016.53
Uploaded by
Putri Rizky AmaliaCopyright:
Available Formats
REVIEWS
Management of neurogenic bladder
in patients with multiple sclerosis
Véronique Phé1,2, Emmanuel Chartier–Kastler1 and Jalesh N. Panicker2
Abstract | Lower urinary tract (LUT) dysfunction is common in patients with multiple sclerosis and is
a major negative influence on the quality of life of these patients. The most commonly reported
symptoms are those of the storage phase, of which detrusor overactivity is the most frequently
reported urodynamic abnormality. The clinical evaluation of patients’ LUT symptoms should include
a bladder diary, uroflowmetry followed by measurement of post-void residual urine volume,
urinalysis, ultrasonography, assessment of renal function, quality-of‑life assessments and sometimes
urodynamic investigations and/or cystoscopy. The management of these patients requires a
multidisciplinary approach. Intermittent self-catheterization is the preferred option for management
of incomplete bladder emptying and urinary retention. Antimuscarinics are the first-line treatment
for patients with storage symptoms. If antimuscarinics are ineffective, or poorly tolerated, a range of
other approaches, such as intradetrusor botulinum toxin A injections, tibial nerve stimulation and
sacral neuromodulation are available, with varying levels of evidence in patients with multiple
sclerosis. Surgical procedures should be performed only after careful selection of patients. Stress
urinary incontinence owing to sphincter deficiency remains a therapeutic challenge, and is only
managed surgically if conservative measures have failed. Multiple sclerosis has a progressive course,
therefore, patients’ LUT symptoms require regular, long-term follow‑up monitoring.
Multiple sclerosis is the commonest progressive neuro Expanded Disability Status Scale (EDSS) is a useful tool
logical disorder in young people, with a mean age at to guide the measurement of progression of neurologi
onset of 30 years, and a prevalence of 108 cases per cal disability and includes an assessment of pyramidal,
100,000 people in Europe1. Multiple sclerosis has a cerebellar, brainstem, sensory, bowel, bladder, visual and
progressive course, of which four major subtypes have cerebral functions5. Disease-modifying treatments are
been identified. A relapse–remitting course is most currently available to prevent progression in patients
commonly reported, in 85% of patients with multiple with relapse–remitting multiple sclerosis. Until the past
sclerosis. Nearly 50% of these individuals develop a decade only IFN‑β and glatiramer were available. Now,
progressive course (described as secondary progres newer molecules have become available such as natali
sion) over a median time period of 11 years2. Less com zumab, as well as oral medications such as fingolimod6.
1
Pitié-Salpêtrière Academic monly, patients might have a primary progressive course, These treatments prevent relapses and the possible accu
Hospital, Department of characterized by progressive symptoms from the onset of mulation of neurological disability, however, uncertainty
Urology, Assistance-Publique- disease, or have a progressive, relapsing course. Chronic remains as to whether or not these treatments delay
Hôpitaux, 47–83 boulevard autoimmune T‑cell-mediated inflammation of the progression of non-motor manifestations such as lower
de l’hôpital, 75651 Paris
Cedex 13, France.
central nervous system (CNS), resulting in disruption urinary tract (LUT) dysfunction.
2
Department of Uro- of myelin sheaths, is the pathological hallmark of this LUT symptoms are reported by >80% of patients
Neurology, The National disorder (FIG. 1). Relapse–remitting multiple sclerosis is with multiple sclerosis. Symptoms might occur during
Hospital for Neurology characterized by the appearance of new and active focal the early stages of the neurological disease and some
and Neurosurgery and
inflammatory demyelinating lesions in the white matter, times might be reported at initial presentation7. Clinical
UCL Institute of Neurology,
33 Queen Square, whereas progressive multiple sclerosis is characterized evidence suggests that LUT symptoms most often result
London WC1N 3BG, UK. by diffuse injury of normal-appearing white matter, from spinal cord lesions and, indeed, a correlation exists
Correspondence to V.P. cortical demyelination and axonal loss3,4. between LUT symptoms and the degree of pyramidal
veronique.phe@aphp.fr Owing in part to spinal cord involvement, the inevi symptoms observed in the lower limbs8,9. However,
doi:10.1038/nrurol.2016.53 table progression of multiple sclerosis symptoms leads LUT symptoms might also result from cognitive prob
Published online 31 Mar 2016 to increased disability and a decline in mobility. The lems (memory loss, amotivation, apraxia and language
NATURE REVIEWS | UROLOGY ADVANCE ONLINE PUBLICATION | 1
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Key points Considering the widespread distribution of lesions
throughout the CNS in patients with multiple sclerosis,
• Lower urinary tract (LUT) symptoms are common in patients with multiple sclerosis; the establishing a precise correlation between neurological
exact symptoms vary in type and severity, and can evolve with progression of the disease lesions and LUT dysfunction is often difficult; how
• The management of LUT dysfunction in these patients requires a consensual approach, ever, the prevalence of LUT dysfunction increases with
with cooperation between different medical professionals, and should take into longer disease duration and greater physical disability22.
consideration possible progression of the disease Furthermore, the presence of LUT symptoms might
• Intermittent self-catheterization is essential for the management of patients with be overlooked in the clinical management of patients
voiding symptoms, but might also have a role in management of those with with multiple sclerosis. Indeed, results of a survey con
storage symptoms
ducted by the North American Research Committee
• Intradetrusor botulinum toxin A injections are a highly effective and minimally invasive On Multiple Sclerosis, published in 2010, revealed that
treatment of storage dysfunctions
only 43% of patients with the disease with moderate to
• Surgical options include augmentation cystoplasty, cutaneous continent diversion and severe overactive bladder symptoms had their symptoms
ileal conduit surgery, and should be performed only after careful selection of patients
evaluated by a urologist22.
• Multiple sclerosis has a progressive course and, therefore, patients with multiple
sclerosis who also have LUT symptoms require regular long-term follow‑up monitoring
Urodynamic presentation
Urodynamic investigations enable precise evaluation
of the functional pathophysiology of patients’ specific
dysfunction), additional localized causes (bladder out LUT dysfunction and of the risk factors for urinary
let obstruction, urinary tract infection or stress incon tract damage in patients with multiple sclerosis, thus
tinence), functional incontinence (reduced mobility helping clinicians to plan the optimal management
or general debilitation) or medications (such as opioid of LUT symptoms. Detrusor overactivity is the most
analgesics or tricyclic antidepressants). LUT symptoms, frequently reported urodynamic abnormality, with a
like cognitive symptoms, also progressively worsen, and prevalence of 34–91%8,14–18,23. Detrusor underactivity
become more difficult to manage with increasing dis is reported in ≤37%, and low bladder compliance in
ability. Furthermore, LUT symptoms negatively influ 2–10% of patients with multiple sclerosis14,18,23. Detrusor
ence patients’ quality of life. Data from several studies activity can also be normal in 3–34% of patients with
have shown that, in terms of patients’ overall quality of multiple sclerosis reporting LUT symptoms14,18,23. The
life, urinary incontinence is considered to be one of the reported prevalence of detrusor–sphincter dyssyner
worst aspects of living with this disease10,11. In a self- gia (DSD) in these patients ranges from 5–60%14–18,23
selected group of patients with multiple sclerosis who and this variation probably reflects the patient group
responded to a questionnaire, 70% of patients consid studied and/or technical difficulties in detecting abnor
ered the disruptive effect of LUT symptoms on their mal detrusor–sphincter contraction. With a median
life as ‘high’ or ‘moderate’ (REF. 11). Several therapeutic prevalence of 35%, DSD becomes more common if
options are currently available to treat LUT symptoms in patients’ symptoms are monitored over a longer period
patients with multiple sclerosis. The aim of this Review of time24. Urodynamic abnormalities also often coexist:
is to describe the diagnosis and management of LUT DSD can be combined with either detrusor overactiv
dysfunction in patients with multiple sclerosis. ity in 43–80% of patients or with detrusor underactivity
in 5–9%, resulting in incomplete bladder emptying24.
Presentation of LUT dysfunction However, urodynamic abnormalities can also be identi
Clinical presentation fied in patients who are asymptomatic15. Urodynamic
Over 80% of patients with multiple sclerosis report the abnormalities can also change with time in any given
incidence of LUT symptoms. This figure can vary, how patient with the evolution of the disease. Following a
ever, according to the severity of the neurological dis urodynamic study of 22 patients, with a mean follow‑up
ability of patients in the study cohort12,13. LUT symptoms duration of 42 months, investigators reported that 12
generally appear after a mean of 6 years of evolution of of these 22 patients, whose symptoms were assessed
the neurological disease13 and might be reported as a using repeated cystomanometric tests, had changes
presenting complaint in 10% of patients. Patients with in their bladder capacity, contractility, pressure or
multiple sclerosis can present with a wide range of LUT detrusor compliance during the follow‑up period25.
symptoms. Of these, symptoms of the storage phase Only those with DSD, which was observed in 13
(overactive bladder symptoms) are the most frequently of the patients, had stable urological symptoms during
reported. Indeed, increased urinary urgency is observed the follow‑up period25.
in 38–99% of patients with multiple sclerosis, increased No evidence exists that a patient’s age or type of
urinary frequency in 26–82% and urge incontinence multiple sclerosis (remittent or progressive) has any
in 27–66%8,14–18. Stress urinary incontinence (SUI) is influence on their urodynamic presentation. However,
also frequently reported with a prevalence of 56%, and a patient’s gender might independently influence uro
patients often report mixed urinary incontinence19. By dynamic presentation, with a significant increase in
contrast, symptoms of the voiding phase are less fre the maximum amplitude of uninhibited detrusor con
quent, with a prevalence of 6–49%8,17,18. Symptoms of tractions, of the detrusor leak-point pressure (defined
both the storage and voiding phases can coexist in 50% as the lowest detrusor pressure at which urine leakage
of patients20,21. occurs in the absence of either a detrusor contraction
2 | ADVANCE ONLINE PUBLICATION www.nature.com/nrurol
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
a Inflammatory neuronal damage b Non-inflammatory neuronal damage
Oligodendrocyte
Microglia
Pro-inflammatory and
cytotoxic molecules Neuronal connectivity
Macrophage
Activated
microglia
Damage
CD4+ B cell Retrograde Anterograde
CD8+ T cell degeneration Wallerian
T cell degeneration
Degeneration
Pycnotic nuclei
Anterograde Wallerian Neuronal dying back Retrograde Anterograde
degeneration degeneration Wallerian
degeneration
Figure 1 | Mechanisms of neuronal injury and degeneration in patients with multiple sclerosis. a | Proinflammatory
and cytotoxic molecules released by inflammatory cells within subarachnoid or intracortical immune Nature Reviews
infiltrates, | Urology
as well as
cell contact-dependent mechanisms of T-cell mediated damage, might lead to microglia and/or macrophage activation
and oligodendrocyte injury. This process can directly or indirectly lead to death of the neuronal cell body and nuclei
(lower panel). Such cell death leads to morphological alterations, such as the characteristic pycnotic nuclei, shrinkage of
dendrites and axonal degeneration in the cerebral cortex. This could in turn lead to dysfunction of the downstream
neuronal network via anterograde trans-synaptic (Wallerian) degeneration. b | Undisturbed neuronal connectivity, and its
related functions, could be impaired by retrograde degeneration propagating backwards in cortical neurons whose axons
have been damaged in white matter lesions or along white matter tracts such as the corticospinal tract. This white matter
tract damage can lead to microglial activation and retrograde neuronal cell death. Reproduced with permission obtained
from Nature Publishing Group © Calabrese, M. et al. Nat. Rev. Neurosci. 16, 147–158 (2015).
or increased abdominal pressure) and of the maximum overactivity and DSD (FIG. 2). However, considering the
detrusor pressure in men compared with women14. The multitude of lesions that characterize this condition,
prevalence of DSD increases with the duration of mul establishing the relative contributions of individual
tiple sclerosis. Thus, DSD is present in 13% of patients lesions to LUT dysfunction is often not possible. In gen
after 48 months of evolution of multiple sclerosis, in eral, lesions that are more caudally placed have a greater
15% of patients between 48 months and 109 months, effect on LUT dysfunction and LUT dysfunction arises
and in 48% of patients 109 months after diagnosis20. most often following spinal cord involvement. In a few
The correlation between detrusor overactivity and a studies, investigators have attempted to evaluate the
higher EDSS score or pyramidal damage seems prob association between the site of the lesion and the spe
able14,26 and a correlation between DSD and pyramidal cific LUT dysfunction. Indeed, the presence of DSD has
damage or the degree of disability has also been sug been reported to be indicative of cervical spinal cord
gested8,14,20. However, no correlation between detrusor lesions, and detrusor hyporeflexia to be indicative of a
underactivity and neurological symptoms has, thus far, pontine lesion23.
been reported15.
Complications of LUT dysfunction
Pathophysiology of LUT dysfunction Urological complications are less frequently reported
In the pathophysiology of multiple sclerosis, lesions in patients with multiple sclerosis compared with those
of the CNS result in a characteristic pattern of LUT with other neurological disorders, such as traumatic
dysfunction according to the specific location of these spinal cord injury or spina bifida, but they are certainly
lesions. Whereas subcortical white-matter lesions not rare14,20. Potential urological complications include
result in detrus or overactivity, lesions of the spinal pyelonephritis (9% of patients), upper tract dilata
cord result in the combined occurrence of detrusor tion (8%), bladder stones (5%), kidney stones (5%),
NATURE REVIEWS | UROLOGY ADVANCE ONLINE PUBLICATION | 3
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
vesicoureteral reflux (5%), renal failure (2–3%) and Assessment of quality of life
bladder cancer (0.29%), although this risk increases (to Many questionnaires are available to assess
5.7%) in regular catheter users16,27–30. Hence, urological LUT-symptom-related quality of life. However only
complications are probably the most common cause Qualiveen® (MAPI research trust, Lyon, France)34 is
of hospitalization in patients with multiple sclerosis14. validated for evaluation of the quality of life of patients
In an epidemiological study, the risk of renal failure in with neurological disease and is recommended by the
patients with multiple sclerosis was found to be equiv European Association of Urology (EAU)35. This ques
alent to the risk reported in the general population20,31. tionnaire comprises 30 items and covers bother (nine
Identified risk factors for complications included detru items), constraints (eight items), fears (eight items) and
sor overactivity, elevated intravesical pressure, the pres feelings (five items). Each item is scored from 0–4. Each
ence of an indwelling catheter and the duration of the of the four scales are scored from 0–100, with lower
neurological disease20,32. scores indicating a better quality of life (meaning fewer
limitations, fears, constraints or negative feelings) and
Clinical investigations higher scores indicating a worse quality of life. The
The evaluation of patients with multiple sclerosis report Qualiveen® questionnaire is currently translated into
ing LUT symptoms should include use of a bladder diary, six different languages.
uroflowmetry followed by measurement of post-void
residual volumes, urinalysis, ultrasonography, assess Urinalysis
ment of renal function and sometimes a urodynamic Findings from urinalysis help to provide evidence of
study and /or cystoscopy. An assessment of a patient’s any urinary tract infections and urinalysis should be
quality of life is an integral part of the evaluation20. performed in all patients during their initial evaluation
or, subsequently, when reporting the occurrence of new
Bladder diary symptoms. Negative urinalysis findings (for example,
The International Continence Society (ICS) recom revealing a lack of leukocyte esterases and/or nitrites)
mends the use of a bladder diary in the clinical assess are useful in excluding the possibility that symptoms are
ment of patients with LUT symptoms. The bladder caused by infections as this test has a high negative pre
diary is an extension of history taking and provides a dictive value (>98%). However, the positive predictive
prospective, real-time assessment of LUT symptoms, value is low (around 50%)36. Thus, when an infection
fluid intake and baseline LUT symptoms before man is suspected, midstream or catheter urine specimens
agement, and also helps to evaluate the outcomes of any should be sent for microbiological culture. For patients
treatment33 (FIG. 3). who perform intermittent self-catheterization (ISC) or
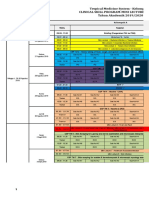
Suprapontine lesion Over-
• History: predominantly storage symptoms active
• Ultrasound: insignificant PVR urine volume
• Urodynamics: detrusor overactivity
Normo-active
Spinal (infrapontine-suprasacral) lesion Over-
• History: both storage and voiding symptoms active
• Ultrasound: PVR urine volume usually raised
• Urodynamics: detrusor overactivity, detrusor-sphincter dyssynergia
Overactive
Under- Under-
Sacral/infrasacral lesion active active
• History: predominantly voiding symptoms
• Ultrasound: PVR urine volume raised
• Urodynamics: hypocontractile or acontractile detrusor
Normo-active Underactive
Figure 2 | Patterns of lower urinary tract dysfunction following neurological disease. The pattern of lower urinary
Nature Reviews | Urology
tract dysfunction following neurological disease is determined by the site and nature of the lesion. The blue box denotes
the region above the pons and that in green denotes the sacral cord and infrasacral region. Figures on the right show the
expected dysfunctional states of the detrusor–sphincter system. PVR, post-void residual. Reproduced with permission
obtained from Elsevier © Panicker, J. et al. Lancet Neurol. 14, 720–732 (2015).
4 | ADVANCE ONLINE PUBLICATION www.nature.com/nrurol
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
The management pf patients with multiple sclerosis and LUT symptoms treatment or if the patient has had recurrent urinary
tract infections, measurement of the post-void residual
Assessment
volume should be repeated.
• History • Urinalysis/culture
• General assessment, quality • Urinary tract imaging,
of life, expectations from measures of renal function Urodynamics
treatment • Measuring post-void Urodynamic techniques, including uroflowmetry and
• Bladder diary residual volume
• Physical examination • Urodynamics filling cystometry, with or without additional synchro
nous fluoroscopic screening (videourodynamics), are
all useful methods of examining LUT function, ena
Storage symptoms bling evaluations of the pressure–volume relationship
Detrusor overactivity during non-physiological filling of the bladder and
during voiding.
The need to perform a urodynamic investigation in all
Disability
Increased post-void Normal post-void
residual volume residual volume patients with multiple sclerosis during initial assessment
is currently under debate, as the risk of damage to the
upper urinary tract is considered to be lower in patients
Learn ISC Treatment options with multiple sclerosis compared with that of those with
other neurological disorders, such as spinal-cord injury
or spina bifida20,31,40,41. Guidelines published by The UK
Behavioural therapies National Institute for Health and Care Excellence (NICE)
and a Turkish consensus statement provide guidance on
the management of patients with urinary incontinence
Antimuscarinics owing to neurological disease; both guidelines recom
mend not to offer urodynamic investigations (such as fill
Tibial nerve stimulation Intradetrusor
ing cystometry and/or pressure–flow studies) routinely
sacral neuromodulation? BoNT-A injections to patients with neurological disease who are known to
have a low risk of renal complications (for example, most
patients with multiple sclerosis)40,42. By contrast, the
Yes International Francophone Neuro-Urological Expert
ISC possible? Study Group (GENULF) recommends using urodynam
No ics in the initial diagnosis of patients20. The inclusion of
urodynamics in the routine assessment of patients with
Augmentation Incontinent urinary diversion– Indwelling urethral/ multiple sclerosis is, therefore, determined by the avail
cystoplasty option in selected patients suprapubic catheter
able local guidance; however, urodynamic investigations
Figure 3 | Algorithm for the management of storage symptoms in patients with are generally recommended in patients with risk factors
Natureof
multiple sclerosis. Maintaining quality of life, including preservation Reviews | Urology
renal function predisposing to upper urinary tract damage such as in
is the primary aim of management of these symptoms. At initial presentation, the most those with concomitant SUI, in those whose symptoms
conservative approaches should be considered the primary treatments of storage have failed to respond to first-line treatment or if surgical
symptoms; although, as patients’ disease progresses, more invasive management treatment is being considered9,43.
approaches might be required. BoNT-A, botulinum neurotoxin A; ISC, intermittent self
catherization; LUT, lower urinary tract. Assessment of renal function
Creatinine clearance, calculated based upon analysis of a
24‑hour urine sample, is a more accurate method of esti
have an indwelling catheter, findings of microbiologi mating kidney function than serum creatinine level or
cal urinalysis will almost invariably be positive owing the estimated glomerular filtration rate44.
to chronic bacteriuria. Thus, periodically sending urine
samples for culture should be discouraged in the absence Other investigations
of fresh neurological or urological symptoms37–39. Other investigations, such as cystoscopy or retrograde
ureterocystography might be required and the need
Ultrasonography for these should be assessed on a case‑by‑case basis.
Findings of renal ultrasonography in patients with Cystoscopy might be indicated in individuals with recur
multiple sclerosis can be entirely normal but can also rent urinary tract infections to investigate the presence of
sometimes reveal the presence of hydronephrosis and/or stones or diverticulae, or if risk factors for bladder c ancer
stones, both of which require a specific management are present20. Retrograde cystography is performed to
plan. Measurements of the post-void residual volume assess any vesicoureteral reflux, although, this might also
form part of the initial assessment, and this is measured be identified using videourodynamics45.
either using ultrasonography, or alternatively using a
single in–out catheterization, followed by measurement Management
of the subsequent volume of urine. Furthermore, if the The management of LUT symptoms in patients
clinician has reason to suspect a patient has developed with multiple sclerosis requires a multidisciplinary
incomplete bladder emptying owing to the effects of a approach involving the input of urologists, neurologists,
NATURE REVIEWS | UROLOGY ADVANCE ONLINE PUBLICATION | 5
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
rehabilitation physicians, continence advisers and the were randomly allocated to one of two groups. Group
various stakeholder groups that represent patients35. one, in which patients received pelvic floor muscle train
In patients with multiple sclerosis, the overall, long-term ing, electromyography biofeedback and placebo neuro
aims of management are to protect the upper urinary muscular electrical stimulation (n = 37), and group two,
tract, to achieve continence and to improve the patient’s in which patients received pelvic floor muscle training,
overall quality of life. The management strategy has to electromyography biofeedback and active neuromuscular
take both the neurological disability and the patient’s electrical stimulation (n = 37). After 9 weeks of treatment,
living environment into consideration. Furthermore, the mean number of incontinence episodes observed in
considerations should be given to urinary and bowel group two was significantly greater than that observed
functions together if both systems are affected, as both in group one (by 85% versus 47% of baseline levels,
symptoms and treatments of one system might also influ respectively; P = 0.0028)49. However, despite these encour
ence the other43. In patients presenting with both storage aging results, concomitant treatment with antimuscarinics
and voiding LUT symptoms, the management strategy was maintained in the majority of studies in this area54.
should combine the treatments available for storage Consequently the exact effects of isolated use of physical
symptoms and the treatments for voiding symptoms. treatments cannot be accurately assessed.
Management of storage symptoms Medical treatment
General measures and physical treatments Antimuscarinics
A fluid intake of 1.5–2 l per day is recommended in the Antimuscarinics and/or intermittent self catheterization
general population and, although not specifically recom (ISC) are the cornerstone of LUT symptom management
mended, this level of intake should also apply to patients in patients with early-stage multiple sclerosis55. The use
with multiple sclerosis. Furthermore a reduction in caf of antimuscarinics results in a decreased sensation of uri
feine intake below 100 mg per day has been shown to nary urgency, an improvement in continence, an increase
reduce symptoms of the storage phase46. in bladder capacity, a significant reduction of maximum
Physical therapy can be effective for the treatment of detrusor pressure and a significant improvement in qual
LUT symptoms in patients with multiple sclerosis with ity of life of patients with a variety of neurological dis
mild disability 47–51. In our own clinical experience of such eases56–58. In patients with multiple sclerosis, the evidence
an approach, bladder retraining involves the patient vol base supporting the clinical use of antimuscarinics is
untarily ‘holding on’, or refraining from voiding with a limited. Not all currently available antimuscarinics have
fairly full bladder for increasingly longer periods of time, been systematically investigated in patients with multi
often as part of an incremental programme supervised ple sclerosis and their use is often based upon inferences
by specialist continence advisers or physiotherapists. Of of efficacy from data from other patient groups58. The
course, these interventions can only be expected to be efficacy, tolerability and safety of anticholinergic drugs
effective in patients with intact neural control of their pel among patients with multiple sclerosis was assessed in
vic floor muscles; therefore, an assessment of a patient’s a Cochrane review published in 2009 (REF. 59). However,
control of their pelvic floor muscles should be made this review included data from only three single-centre
before initiating treatment. Such interventions are often randomized crossover trials that were either placebo-
difficult to initiate in patients with cognitive impairments. controlled or designed to compare the effects of two
Regular pelvic floor exercises can enhance the inhibitory or more treatments57,60,62. In the Cochrane review59, the
effect of pelvic floor contractions on the detrusor52. authors did not find sufficient evidence to prove any sig
A prospective trial was conducted to investigate the nificant benefit of antimuscarinics in patients with mul
effects of pelvic floor rehabilitation as a treatment of tiple sclerosis. The authors also noted a high incidence of
detrusor overactivity in 30 female patients with multiple adverse effects (such as dry mouth or constipation) with
sclerosis53. In 25 of these 30 patients, the strength of the more than one in five trial participants having to with
pelvic floor was significantly improved after one month draw from antimuscarinic treatment59. Findings of sys
of regular exercises (P <0.001). A significant increase in tematic reviews do not support the superiority of any one
mean functional bladder capacity, as read from patients’ drug over another. However, the most clinically relevant
voiding charts, was also observed (from 173.8 +/– 53.9 differences between antimuscarinics are in the adverse
to 208.5 +/– 57.6 cm3; P = 0.005). Furthermore, the mean event profile. For example, tolterodine, when used at self-
urinary frequency decreased significantly (from 12.7 +/– selected doses, is comparable with oxybutynin in terms
3.6 to 9.1 +/– 2.6 voids per day; P <0.01) as did the mean of increasing patients’ bladder capacities and improving
number of daily episodes of incontinence (from 2.8 +/– continence, but with less dry mouth62. The intravesical
1.3 to 1.5 +/– 1.5 episodes per day; P <0.01)49. Moreover, administration of atropine is an interesting approach that
combining active neuromuscular electrical stimulation has been reported to be as effective as oral oxybutinin,
with pelvic floor muscle training and electromyography with fewer adverse effects57. However, the limited avail
(EMG) biofeedback can result in a substantial reduction ability of atropine and the necessity to visit the clinic for
in the severity of LUT symptoms53. each instillation is a major inconvenience, which restricts
Further evidence for the combination of pelvic floor the use of this approach.
exercises with neuromuscular electrical stimulation is pro Cognitive impairment is reported in patients with
vided by a randomized controlled trial: 74 patients with multiple sclerosis, especially as the disease advances,
multiple sclerosis who presented with LUT dysfunction and the choice of antimuscarinic should, therefore, be
6 | ADVANCE ONLINE PUBLICATION www.nature.com/nrurol
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
guided by the potential risk of adverse effects on the trial with a cohort of 647 patients with multiple scler
CNS. Medications such as trospium chloride are, rela os is, oral administration of a cannabis extract or
tive to oxybutynin, tolterodine and solifenacin, less likely Δ9‑tetrahydrocannabinol (Δ9‑THC) reduced the fre
to cross the blood–brain barrier and might be a medica quency of urge incontinence episodes (by 38%, 33% and
tion to consider in patients with advanced-stage multiple 18%, respectively; P = 0.05 and 0.039 for comparisons of
sclerosis. Darifenacin, a selective antagonist of the M3 cannabis extract or Δ9‑THC with placebo, respectively)
receptor, which is not known to be involved in cogni and pad weight (mean reduction of 44.7 ml, 43.2 ml and
tion, provides an alternative to trospium41. However, 43.9 ml for cannabis extract, Δ9‑THC or a combination
studies supporting the use of darifenacin specifically of treatments, respectively, versus a mean increase of
in patients with multiple sclerosis are currently lacking. 8.3 ml for placebo; combined mean difference versus
Combinations of regular doses of two different anti placebo of 52.1 ml, 95% CI 13.4–90.9 ml; P = 0.001)74.
muscarinics have been shown to be effective and well In a small open-label trial including 21 patients with
tolerated in a few patients63. advanced-stage multiple sclerosis, the safety, tolerability,
In conclusion, antimuscarinics remain widely pre dose range and efficacy of two whole-plant extracts of
scribed agents despite the availability of only limited cannabis sativa was evaluated. Patients received extracts
evidence of their efficacy or effectiveness in patients containing Δ9‑THC and cannabidiol (CBD; 2.5 mg of
with multiple sclerosis. Use of these agents can improve each per spray) for 8 weeks followed by Δ9‑THC only
symptoms of the storage phase and patients’ quality of (2.5 mg THC per spray) for a further 8 weeks, and then
life. However, patients must be informed of the poten entered into a long-term extension phase. Urinary
tial long-term adverse effects, including the risk of an urgency, the number and volume of incontinence epi
increased post-void residual volume, which then might sodes, urinary frequency and the number of episodes
require ISC. of nocturia all decreased significantly following treat
ment (P <0.05). However, daily total volume voided,
Desmopressin catheterized, and urinary incontinence pad weights
Treatment with the synthetic antidiuretic hormone des also decreased significantly in patients who received
mopressin, used orally or intranasally at different doses both extracts75.
(from 10–100 μg), has been shown to reduce night time Data from a multicentre, double-blind, placebo-
urinary frequency in patients with multiple sclerosis64–71. controlled trial evaluating the efficacy of sublingual
Some of these data are from randomized-controlled Sativex® (GW pharmaceuticals, Cambridge, UK),
trials, and some from other studies. These investiga which is an endocannabinoid modulator consisting of
tions64–71 generally included only small numbers of THC and cannabidiol, in a 1:1 ratio, in patients with
patients with multiple sclerosis and had short (<6‑week) advanced-stage multiple sclerosis demonstrated some
durations of both treatment and follow‑up monitoring. improvements in the frequency of episodes of urinary
If taken during the day, similar doses of desmopressin incontinence, daytime urinary frequency and nocturia76.
to those used at night can also provide relief from LUT However, no significant differences in the frequency of
symptoms for up to 6 hours without rebound nocturia72. episodes of urinary incontinence was observed between
Moreover, the use of desmopressin is associated with res patients who received Sativex® and those who received
toration of sleep patterns and substantial improvements placebo after 8 weeks of treatment, despite this being the
in LUT symptoms, as determined using the International primary endpoint of the study76. A license was granted in
Consultation on Incontinence Questionnaire– 2010 for the use of Sativex® to treat spasticity in patients
Overactive Bladder questionnaire72. However, hypo with multiple sclerosis in the UK; although, this license
natraemia is a serious adverse effect of desmopressin, does not apply to the treatment of LUT symptoms.
and serum sodium levels should be checked before the
drug is administered to establish a baseline level, and Intravesical treatments
at day 3 and day 7 after commencing daily administra Onabotulinum toxin A (BoNT‑A), which is commer
tion72. Thus, desmopressin is not recommended for use cially available as BOTOX® (Allergan, Irvine, California,
more than once daily, and should be used with caution USA) has been licensed since 2012 in several countries
in elderly patients (defined as those >65 years of age). for use in patients with treatment-refractory neurogenic
Other adverse effects of desmopressin include headaches detrusor overactivity owing to multiple sclerosis or spi
(3.2–18.7%), nausea (3.2–10.5%), fluid retention (36.8%) nal cord injury. BoNT‑A is the only type of botulinum
and rhinitis and/or epistaxis (3.2–10.5%)64–71. toxin to be evaluated for the management of any LUT
dysfunction in large, multicentre, randomized controlled
Cannabinoids trials77–80. However, the use of abobotulinum toxin A,
Some evidence exists supporting the use of cannabinoids which is commercially available as Dysport® (Ipsen,
in the management of LUT symptoms in patients with Paris, France) as a treatment of neurogenic detrusor
multiple sclerosis. The rationale for cannabinoid use in overactivity but not other forms of LUT dysfunction, is
the control of LUT symptoms stems from the established also supported by a high level of evidence81.
expression of cannabinoid receptors of both subtypes BoNT‑A has several putative mechanisms of action;
(CB1 and CB2) in the urothelium and afferent nerves in addition to inhibiting the release of vesicular neuro
of the human bladder, similar to those of several other transmitters from parasympathetic nerve terminals
experimental animals73. In a large, placebo-controlled of the detrusor smooth muscle, this toxin is also
NATURE REVIEWS | UROLOGY ADVANCE ONLINE PUBLICATION | 7
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
likely to inhibit the release of transmitters involved in with end-stage multiple sclerosis, that intradetrusor
afferent signalling pathways in the bladder mucosa82. injections of BoNT‑A might provide some benefit to
Intradetrusor injections of BoNT‑A are highly effective patients with an indwelling urethral catheter who report
in reducing the incidence of urinary incontinence, in urine leakage owing to catheter bypassing87.
improving patients’ urodynamic parameters and, there
fore, their quality of life77–79,83. Two doses of BoNT‑A, Neuromodulation
200 units versus 300 units, have been tested in two Stimulation of the tibial nerve or sacral nerve root S3
double-blind, placebo-controlled randomized trials has proven to be successful in managing overactive
with cohorts of patients with neurogenic detrusor over bladder symptoms. The exact mechanisms of action of
activity owing to either multiple sclerosis or spinal cord this approach remain uncertain but are thought to be
injury78,79. Data from both studies did not reveal any a result of modulation of spinal pelvic reflexes through
significant differences in efficacy between doses; how activation of inhibitory interneurons88.
ever, the need to initiate ISC after injections was higher
in those receiving 300‑unit injections than in those Tibial nerve stimulation. Tibial nerve stimulation can
receiving 200‑unit injections or placebo (12%, 30% and be administered either using a needle to deliver electri
42%79 and 10%, 35% and 42%79 of patients not already cal stimulation (the percutaneous approach) or using
using ISC required ISC after receiving placebo, 200‑unit an electrode patch (the transcutaneous approach).
or 300‑unit injections, respectively). The effects of The transcutaneous method has the advantage that it
BoNT‑A injections usually last for 6–9 months, there can be easily used at home, either by the patient or by
fore, repeated injections are often necessary. All patients their carer, in comparison to the percutaneous method,
with multiple sclerosis should have been taught, or which requires the insertion of a needle close to the tibial
agreed to learn to do ISC before being treated with nerve by a health-care professional. Percutaneous tib
BoNT‑A injections as 88% of patients need to perform ial nerve stimulation has been shown to be effective in
de novo ISC83. However, the need for ISC did not affect managing storage symptoms and improving urodynamic
quality of life outcomes83. parameters in patients with multiple sclerosis89–91. Initial
Mehnert et al.84 investigated the effects of 100‑unit percutaneous stimulation is usually delivered during
injections of BoNT‑A in 12 patients with multiple scler 30‑min, weekly sessions, over a period of 10–12 weeks,
osis and overactive bladder symptoms. Follow‑up visits and generally followed in responders by a period of
were planned 6–7 and 12–14 weeks after injections. maintenance therapy, of which the optimal characteris
Investigators found that 6–7 weeks following the injec tics are poorly defined. This therapy is safe, the patients’
tion, maximum bladder capacity increased significantly reported subjective and objective cure rates are between
(P = 0.034), and maximum detrusor pressure (P = 0.004), 60–80%, patients’ treatment satisfaction is generally high
daytime urinary frequency (P = 0.004), urinary urgency (70%) and their overall quality of life is usually improved
(P = 0.008) and pad use (P = 0.011) all decreased sig substantially89,91–94. Data from a study of 19 patients with
nificantly. Furthermore, daytime urinary frequency multiple sclerosis who received weekly, 30‑min percu
(P = 0.002), night time urinary frequency (P = 0.005), taneous stimulation of the tibial nerve for 12 weeks
urinary urgency (P = 0.013) and pad use (P = 0.02) all revealed a significant improvement in urodynamic
decreased significantly 12–14 weeks following injec parameters, including maximum cystomanometric
tions. Post-void residual volume significantly increased capacity (increased from 199.7 to 266.8 ml; P < 0.001),
in these patients following 100‑unit BoNT‑A injections, maximum detrusor pressure at maximum cystoman
and reached 222 ml initially but decreased progressively ometric capacity (decrease from 48.8 to 35.8 cm H2O;
for 12 weeks post-treatment; overall, three patients P = 0.001), maximum flow rate (increased from 11.6
needed to perform de novo ISC84. Further studies, with to 13.2 ml; P = 0.003) and post-void residual v olume
larger populations and longer follow‑up durations are (decreased from 82.9 to 48 ml; P = 0.006)95.
required to investigate the benefits of a lower dose of The efficacy of transcutaneous tibial nerve stimula
BoNT‑A in patients with multiple sclerosis who are not tion has been proven in a multicentre study of a cohort
willing or able to self-catheterize. An alternative option of 70 patients with multiple sclerosis and symptoms of
for patients who cannot reach the urethra to perform overactive bladder96. All patients received transcutan
ISC is to control LUT symptoms using intradetrusor eous tibial nerve stimulation for 20 minutes per day, for
BoNT‑A injections and create a continent urinary diver a period of 3 months. Clinical improvement in symp
sion using a catheterizable channel (Mitrofanoff, Monti toms was observed in 82.6% and 83.3% of the patients
or Casale’s principles)85. In our own clinical experience, on day 30 and day 90, respectively, with significant
BoNT‑A injections do have to be repeated following sur improvements in urinary urgency, frequency, patients’
gery, although generally, the patient can still perform ISC self-reported symptoms, continence and quality of life
using this continent stoma. observed between day 0 and day 90 of the study (P <0.05
Furthermore, the use of BoNT‑A injections has also for all changes)96. The initial acute cystometric response
been shown to decrease the incidence of symptomatic (defined as a >30% increase in cystometric capacity
urinary tract infections. This effect seems to be related and/or reflex volume) to the first session of transcu
to improvement in urodynamic parameters, reflecting taneous stimulation was positive in 51.2% of patients,
improved reservoir capacity at low bladder pressures86. without any notable correlations with longer-term clini
Finally, evidence exists, from a series of three patients cal effectiveness of the treatments96. Further studies are
8 | ADVANCE ONLINE PUBLICATION www.nature.com/nrurol
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
required in order to assess the long-term effects of per 62 patients with a neurological condition (among them
cutaneous neuromodulation and to better understand 13 had multiple sclerosis) receiving sacral neuromodu
the need for ‘top up’ to maintain these effects. lation therapy, the reported revision and explantation
The safety of tibial nerve stimulation is particularly rates were 10.4% and 12.5% respectively. Complications
useful to patients who are disabled, who might be more included wound seroma (0.8%), wound infection (4.1%),
susceptible to the deleterious adverse effects of anti back pain (0.8%), leg pain (1.2%), implantable perma
muscarinics than those with a lower level of disability. nent generator site pain (8.2%), a sensation of shock
In our own clinical experience, in such populations, the upon stimulation (0.8%), lead breakage (2.5%), lead
use of tibial nerve stimulation as the first-line treatment migration (0.8%) and device malfunction (3.3%)101.
can be considered appropriate; although, this sugges Published data are available from other studies in this
tion is not supported by any published evidence, thus area, however, these studies included only small num
far. The advantage, to the clinicians, of the percutan bers of patients with multiple sclerosis and are highly
eous approach over the transcutaneous method is that heterogeneous102–106: most of the series were retrospective
patients’ symptoms can be monitored on a weekly basis and data from patients with multiple sclerosis were gen
by the health-care team. However, patients might con erally not analysed separately from data from patients
sider a weekly visit to be a constraint, especially if they with other neurological conditions. Currently, no data
are disabled. Use of the transcutaneous method has from randomized controlled trials are available in this
the advantage that patients can benefit from receiv area, and the types of patients who are most suitable for
ing the treatment at home, but without the possibility sacral neuromodulation is also largely unknown.
of checking if the stimulation they are receiving is opti
mally conducted. By contrast, the lack of any proven Surgery
ameliorative effects on increased detrusor pressures Surgical treatments of LUT dysfunction in patients with
might be a limitation of the percutaneous approach in multiple sclerosis are appropriate in certain situations:
patients with severe neurogenic detrusor overactivity when conservative therapies have failed; when ISC
and high detrusor pressures, which increase the risk of through the urethra is not possible; or in patients with
damage to the upper urinary tract. serious complications such as sepsis, urethral or perineal
fistulae, renal failure or severe urinary incontinence.
Sacral neuromodulation. Sacral nerve stimulation is a
minimally invasive treatment that can be used to treat Augmentation cystoplasty. In highly-motivated patients
patients with treatment-refractory LUT symptoms where ISC can be achieved in the long term, but whose
owing to a range of different underlying neurological LUT symptoms are refractory to more-conservative
diseases97. Similar to other forms of neuromodulation, treatments, augmentation cystoplasty is recommended.
the exact underlying neurophysiological mechanisms of The goal of an augmentation cystoplasty procedure,
action are complex and currently not fully understood. which involves surgically enlarging the bladder, is to
Neuromodulation might exert its effect through acti restore a low-pressure and compliant reservoir and, thus,
vation of afferent pathways that modulate the activity achieve urinary continence. This procedure is often per
of other neural pathways within the spinal cord and formed using a segment of detubularized ileon to aug
higher centres98. Results of a study, published in 2000, ment the urinary bladder. Zachoval et al.107 reported the
show that urodynamic parameters improve from base outcomes of augmentation ileocystoplasty performed in
line to 6 months post-implantation, including maximum nine patients with multiple sclerosis, of whom eight had
bladder capacity (from 244 ml to 377 ml), volume at first detrusor hyperreflexia that was refractory to conserva
uninhibited contraction (from 214 ml to 340 ml) and the tive treatment and one had renal insufficiency. With
average number of voids per day (from 16.1 voids to 8.2 a follow‑up duration of 6–19 months, investigators
voids)97. The findings of a meta-analysis published in recorded an increase in the maximum mean detrusor
2010 indicate that sacral neuromodulation might be capacity from 105 to 797 ml and a decrease in the maxi
effective (in terms of reduced incontinence and fewer mum detrusor pressure from 53 cm H2O to 30 cm H2O.
voids per day) and safe in patients with neurogenic LUT A substantial improvement in LUT symptoms was
dysfunctions99. Elsewhere, in a retrospective case series observed in all patients and the quality-of‑life score, as
of 33 patients with neurogenic LUT dysfunctions, 31 assessed using a questionnaire with a 0–6 scale (0 indi
reported satisfaction with their treatment100. However, cating excellent quality of life, six indicating unbear
the course of the underlying neurological disorder has able), improved from a mean of five to 0.7 (REF. 107).
been shown to adversely influence the ability to derive Importantly, the patient who had renal insufficiency
long-term benefits from sacral neuromodulation101,102. had a decrease in serum creatinine from 286 μmol/l to
As a result, some authors have proposed that sacral 150 μmol/l, suggesting that this surgery had a renopro
neuromodulation should be used in patients with mul tective effect in this patient108. Elsewhere, in more var
tiple sclerosis of a relapse–remitting course, who have ied but larger patient cohorts, the rates of continence
not had a relapse for at least 2 years101. The incidence (78% for patients with neuropathic bladders and 93%
of complications after sacral neuromodulation seems for those with detrusor instability) 3 years after augmen
not to be significantly different from that of the general tation are high, as are the patient satisfaction rates108,109.
population of patients with LUT dysfunctions with no Therefore, augmentation ileocystoplasty is an effective
established neurogenic aetiology103. In a study enrolling surgical approach for patients with multiple sclerosis
NATURE REVIEWS | UROLOGY ADVANCE ONLINE PUBLICATION | 9
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
who also have treatment-refractory neurogenic blad haemorrhagic shock (n = 2), the surgical procedure did
der, provided that patients are able to self-catheterize, significantly improve the mean overall Qualiveen® score
and this approach can improve patients’ LUT-specific (from 2.1 before surgery to 1.16 after surgery; P = 0.02).
quality of life. The investigators found that the postoperative morbid
Augmentation cystoplasty is currently feasible using a ity rate was 18.2%. Interestingly, limitations (1.64 ± 1.38
robot-assisted laparoscopic approach110; although, com before surgery versus 0.60 ± 0.69 after surgery; P = 0.005),
parative studies are needed to confirm the results and the constraints (2.91 ± 1.01 before surgery versus 2.07 ± 0.93
reduced morbidities observed following use of this pro after surgery; P = 0.16) and specific urinary impact index
cedure in comparison with those obtained with the open (1.86 ± 0.96 before surgery versus 1.25 ± 0.71 after sur
approach. Augmentation cystoplasty procedures can also gery; P = 0.024) subscores of the Qualiveen® were sig
be performed concomitantly with a cutaneous continent nificantly improved at 6 months after surgery116. In a
urinary diversion in circumstances where the patient is prospective study, authors reported the quality-of‑life
unable to perform ISC through the urethra. For cosmetic outcomes of 44 patients with multiple sclerosis who
reasons, the umbilicus is often used as the stoma site in underwent laparoscopic ileal conduit surgery to treat
these patients. The short-term continence rates achieved their LUT dysfunction117. The authors found that the
with augmentation cystoplasty in combination with a postoperative morbidity rate was 18.2%. Minor (Clavien
continent urinary diversion are >80% and good protec grade ≤2) and major (Clavien grade ≥3) complications
tion of the upper urinary tract is usually achieved111–113. occurred in 13.6% and 6.8% of patients, respectively.
An improvement in quality of life, as assessed using the Noted complications included asymptomatic ureteroileal
Qualiveen® questionnaire, has also been reported114; stenosis (n = 6) and pyelonephritis (n = 3).
furthermore, the reported rates of continence (86%), as
well as satisfaction with both functional and aesthetic Management of SUI
outcomes (88% and 92%, respectively) are high after a SUI owing to sphincter deficiency that does not respond
mean follow‑up duration of 21.6 months114. However, to behavioural modifications requires a specialised man
all of these patients have a high risk of complications, agement approach. Social continence, where symptoms
including stomal leakage or stenosis. Regular clinician are controlled to the extent that patients’ quality of life
visits to monitor patients’ adherence and continence is largely unaffected, can be achieved by collecting urine
status are, therefore, required. during incontinence episodes using pads, for example.
In our own clinical experience, condom catheters with
Non-continent urinary diversion. Despite the availabil urine collection devices are also a practical method for
ity of procedures to create a catheterizable outlet, some managing SUI in men as these tend to result in fewer
patients remain unable or unwilling to perform ISC. hygiene issues, and are more affordable than pads. Use
Quadriplegia, limited dexterity and/or devastating cog of a penile clamp is contraindicated in patients with
nitive impairment are the main causes of this inability. detrusor overactivity or low bladder compliance owing
In order to restore a low-pressure reservoir without the to the risk of developing high intravesical pressures36.
use of an indwelling urethral, or suprapubic catheter Neurogenic SUI remains a therapeutic challenge: cur
and to improve quality of life, a noncontinent cutan rently, no nonsurgical treatments for this condition exist,
eous diversion using an ileal conduit and a urine collect and the armamentarium for management comprises
ing device can be performed115. Ultimately, use of such midsuburethral synthetic slings, fascial slings, artificial
an approach could be considered in patients who are urinary sphincters, periurethral bulking agents and ure
wheelchair-bound or bedridden (including in those with thral closure116. No published data on neurogenic SUI
skin ulcers), with intractable and/or untreatable incon specifically in patients with multiple sclerosis currently
tinence, in patients with devastating LUT symptoms, exist. Therefore, selection of the most appropriate treat
when the upper urinary tract is severely c ompromised ment should be made on a case‑by‑case basis, consider
or in patients who refuse other therapies. ing the patient’s ability to perform ISC and the extent of
A cystectomy is usually performed as a first-line any cognitive impairment.
approach to prevent pyocystitis. Much of the data on
the outcomes of patients who underwent ileal conduit Management of voiding symptoms
surgery are from patients who underwent this procedure Intermittent catheterization
after pelvic cancer surgery. Regarding patients with ISC is the preferred method for the treatment of incom
neurological diseases, some studies have provided data plete bladder emptying or urinary retention in patients
on the outcomes of ileal conduit surgery among patients with neurogenic bladder35. This approach to manage
with multiple sclerosis. In a retrospective study, investi ment of incomplete bladder emptying was originally
gators reported the functional outcomes of ileal conduit described by Lapides and colleagues118, in 1971, in a
procedures performed in a population of 53 patients woman with multiple sclerosis. ISC has to be initi
with multiple sclerosis with neurogenic bladder116. ated in patients whose incomplete bladder emptying
Despite the fact that ileal conduit surgery was found to is reflected by the presence of a high residual volume.
be associated with substantial perioperative morbidi This high residual volume is generally accepted to be
ties, including blood loss requiring transfusion (n = 17), >100 ml, however the exact volume depends upon the
pneumonia (n = 3), pyelonephritis (n = 3), pelvic abscess characteristics of the individual patient. Actually, no
(n = 1), wall abscess (n = 2), septicaemia (n = 1) and evidence-based cut off post-void residual value exists for
10 | ADVANCE ONLINE PUBLICATION www.nature.com/nrurol
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
the recommendation to start clean intermittent catheter should be discussed with the patient and alternatives
ization in patients with multiple-sclerosis-related LUT should be presented; this is a grade A recommendation
dysfunction41. The average frequency of catheterization provided by the EAU35.
per day is 4–6 times, as bladder volume at catheteriza
tion should ideally, as a rule, not exceed 400–500 ml119. Management of DSD
ISC is rarely necessary in the early stages of multiple Urethral sphincterotomy. The main objectives of the
sclerosis but becomes increasingly likely to be needed treatment of DSD are to improve voiding function, to
as a patient’s mobility deteriorates. The introduction of decrease voiding pressures and to avoid the need for
self-catheterization can be challenging in patients with indwelling catheters. However, the possibility of using
multiple sclerosis, therefore, training and support from a condom catheter and the existence of efficient blad
the health-care team is required. The ability of patients der contractions are a prerequisite. Moreover, long-
with multiple sclerosis to learn ISC might be influenced term follow‑up monitoring is absolutely necessary,
by the extent of symptoms, as indicated by the EDSS; by owing to the risk of reflex voiding, leading to a rise in
contrast, cognitive decline seems not to limit a patient’s intravesical pressure, which could potentially damage
ability to learn ISC120. When having to perform ISC, the upper urinary tract. Urethral sphincterotomy, a
patients with multiple sclerosis might face several bar procedure designed to weaken the contractions of the
riers: patient-related factors include physical disabilities urethral sphincter, can be conducted using one of sev
and psychological factors, and external factors include eral different techniques, including laser and electrode
access to public toilets. These factors have to be indi endoscopic sphincterotomy133, sphincteric stent prosthe
vidually addressed121. Use of ISC decreases the risk of sis133 and dilatation using a balloon. Regardless of the
urinary tract infections and upper urinary tract dam technique used, sphincterotomy should only be focused
age, promotes urinary continence and, in some studies, on the striated sphincter. The effectiveness of sphincter
has been demonstrated to improve patients’ quality of otomy has been demonstrated in a prospective study of
life32,122–125. For patients with multiple sclerosis who also patients with DSD owing to spinal cord injury: 83.7%
have severe limb spasticity and poor mobility, a willing of patients had a decrease in voiding pressure, subjective
carer can be taught to catheterize the patient. autonomic dysreflexia was resolved in 93.2% of patients
Some patients are unable to reach their urethra, and febrile urinary tract infections disappeared in 76.7%
which is necessary in order to self-catheterize, owing to of patients134.
limited hand dexterity or other physical limitations, such
as obesity. For such patients, a continent catheterizable BoNT‑A. A few published reports exist from studies
tube is created using various surgical techniques, includ designed to investigate the outcomes of intraurethral
ing the appendix (Mitrofanoff ’s principle) or a portion injections of BoNT‑A for the treatment of DSD. In a
of small intestine (Yang-Monti and Casale’s principles)85. multicentre, randomized double-blind study, investi
Data from a study of a small cohort of patients with gators evaluated the efficacy and safety of 100‑unit
multiple sclerosis reveal that use of α‑adrenoceptor antag injections of BoNT‑A into the striated sphincter as a
onists reduces post-void residual volumes126; although, treatment of DSD in 86 patients with multiple scler
the experience in clinical practice indicates that many osis135. The authors administered the treatment as a
patients fail to derive any consistent benefits from this single transperineal injection using striated sphincter
approach. However, symptoms of poor voiding owing to electromyography: the coaxial needle was inserted on the
outflow obstruction might be caused by prostate enlarge median line 2 cm above the anal margin in men, or in the
ment in men, or a pelvic-organ prolapse in women. The upper external or internal quarter, above the urethral
possible presence of one of these two conditions should meatus in women, thus enabling the striated sphincter
be assessed during initial clinical examination. to be localized135. The injection was delivered after first
having verified that the needle was not inserted into a
Long-term indwelling catheterization blood vessel. Compared with placebo, BoNT‑A injec
For patients with a substantially increased post-void tions significantly increased the voided volume (by 54%;
residual volume who are unwilling or unable to con P = 0.02) and reduced both the premicturition and maxi
duct ISC, or who have incontinence that is refractory mal detrusor pressures (by 29% and 21%, respectively;
to treatment, a long-term indwelling transurethral or both P = 0.02). By contrast, BoNT‑A injections had no
suprapubic catheter is often used to ensure that the significant effect upon post-void residual v olumes and
bladder empties and to provide urinary continence. both treatments were equally well tolerated135.
However, long-term indwelling catheter use “should be Following a randomized-controlled double-blind
avoided when possible” (REF. 35) because this might lead study designed to compare the efficacy and tolerability
to a range of complications including recurrent urinary of transperineal injections of BoNT‑A versus those of
tract infections, catheter blockages, catheter bypass lidocaine, including three patients with multiple scler
ing, urethral destruction, bladder stones and bladder osis in a cohort of 13 patients, investigators reported
cancer127–131. Despite these possible complications, how that post-void residual volume was significantly
ever, long-term catheterization does not substantially decreased (by 141.4 ml 7 days after treatment; P <0.03);
alter a patient’s quality of life132. A suprapubic catheter DSD and patient satisfaction were both improved
is recommended over a transurethral catheter for long- in the BoNT‑A but not in the lidocaine group136. In
term use9,42; however, the potential for complications another report, investigators described similar results
NATURE REVIEWS | UROLOGY ADVANCE ONLINE PUBLICATION | 11
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
in a prospective nonrandomized study with a cohort evaluation is advocated, including use of a 3‑day bladder
of 21 patients, eight of whom had multiple sclerosis137; diary and uroflowmetry with measurement of the post-
however, data from patients with multiple sclerosis void residual volume. The International Francophone
were not analysed separately in this study. Moreover, in Neurourological Expert Study Group20 recommends a
both studies136,137, contrary to the study by Gallien and urodynamic investigation every 3 years, whereas the UK
colleagues135, electromyography was not used to locate consensus on the management of the bladder in multiple
the striated sphincter. Results from studies with small sclerosis recommends urodynamic investigations only in
patient cohorts, which have a high risk of bias relative the event of second-line or intravesical treatment being
to those with larger cohorts, have revealed evidence of required, or when a patient is considered to be at risk of
limited quality, suggesting that intraurethral BoNT‑A damage to the upper urinary tract9.
injections given as a treatment of functional blad For patients who are deemed to have a higher risk of
der outlet obstruction in adults with neurogenic bladder rapid worsening of LUT symptoms, the annual evalu
dysfunction improve certain urodynamic parameters ation should be more complete, and should include ultra
30 days after treatment; these parameters include sonography of the urinary tract, measurement of renal
higher voided urine volumes and lower premaximal creatinine clearance and a quality-of‑life assessment.
and maximal detrusor pressures, as summarized in a The urodynamic follow‑up should be systematic. The
meta-analysis138. In conclusion, only limited evidence specific choice of investigations should be determined
is available to support the use of intraurethral BoNT‑A in discussions among an expert m ultidisciplinary team.
injections in the treatment of DSD in patients with mul
tiple sclerosis. Moreover, the need for reinjections is a Conclusions
major drawback138. LUT symptoms are common in patients with multiple
sclerosis and can negatively affect patients’ quality of
Follow‑up monitoring life. During the early stages of LUT dysfunction, anti
Patients with multiple sclerosis should have their symp muscarinic medications and ISC are the first-line treat
toms reviewed regularly as both the type and severity ments. Treatment pathways are now available that offer
of LUT dysfunction can change with neurological pro guidance on selecting the most appropriate manage
gression9,20,40. Recommendations exist for long-term ment strategy. Patients should be assessed and m anaged
urological follow‑up monitoring, taking into account by health-care professionals with a suitable level of
the presence of specific risk factors: duration of multi experience, who can offer at least one of the number
ple sclerosis >15 years, presence of an indwelling cath of effective treatment options. Long-term monitoring of
eter, ample uninhibited detrusor contractions, high patients with multiple sclerosis is essential as the type
detrusor pressure or DSD9,20,40. For patients who are and severity of LUT dysfunction can change with
risk-free according to these criteria, a systematic annual neurological progression.
1. Multiple Sclerosis International Federation. Atlas 11. Hemmett, L., Holmes, J., Barnes, M. & Russell, N. What 21. Panicker, J. & Haslam, C. Lower urinary tract
of MS 2013: mapping multiple sclerosis around the drives quality of life in multiple sclerosis? QJM 97, dysfunction in MS: management in the community.
world. [online], http://www.msif.org/wp-content/ 671–676 (2004). Br. J. Community Nurs. 14, 474–480 (2009).
uploads/2014/09/Atlas-of-MS.pdf (2013). 12. Marrie, R. A., Cutter, G., Tyry, T., Vollmer, T. 22. Mahajan, S. T., Patel, P. B. & Marrie, R. A. Under
2. Confavreux, C., Aimard, G. & Devic, M. Course and & Campagnolo, D. Disparities in the management treatment of overactive bladder symptoms in
prognosis of multiple sclerosis assessed by the of multiple sclerosis-related bladder symptoms. patients with multiple sclerosis: an ancillary analysis
computerized data processing of 349 patients. Neurology 68, 1971–1978 (2007). of the NARCOMS Patient Registry. J. Urol. 183,
Brain J. Neurol. 103, 281–300 (1980). 13. Mayo, M. E. & Chetner, M. P. Lower urinary tract 1432–1437 (2010).
3. Kutzelnigg, A. et al. Cortical demyelination and dysfunction in multiple sclerosis. Urology 39, 67–70 23. Araki, I., Matsui, M., Ozawa, K., Takeda, M.
diffuse white matter injury in multiple sclerosis. (1992). & Kuno, S. Relationship of bladder dysfunction to
Brain J. Neurol. 128, 2705–2712 (2005). 14. Giannantoni, A. et al. Urological dysfunctions and upper lesion site in multiple sclerosis. J. Urol. 169,
4. Furby, J. et al. Magnetic resonance imaging measures urinary tract involvement in multiple sclerosis patients. 1384–1387 (2003).
of brain and spinal cord atrophy correlate with clinical Neurourol. Urodyn. 17, 89–98 (1998). 24. Porru, D. et al. Urinary tract dysfunction in multiple
impairment in secondary progressive multiple 15. Koldewijn, E. L., Hommes, O. R., Lemmens, W. A. J. G., sclerosis: is there a relation with disease-related
sclerosis. Mult. Scler. 14, 1068–1075 (2008). Debruyne, F. M. J. & Van Kerrebroeck, P. E. V. parameters? Spinal Cord 35, 33–36 (1997).
5. Kurtzke, J. F. Rating neurologic impairment in multiple Relationship between lower urinary tract abnormalities 25. Ciancio, S. J., Mutchnik, S. E., Rivera,
sclerosis: an expanded disability status scale (EDSS). and disease-related parameters in multiple sclerosis. V.M. & Boone, T. B. Urodynamic pattern changes in
Neurology 33, 1444–1452 (1983). J. Urol. 154, 169–173 (1995). multiple sclerosis. Urology 57, 239–245 (2001).
6. Derfuss, T., Bergvall, N. K., Sfikas, N. & Tomic, D. L. 16. Gallien, P. et al. Vesicourethral dysfunction and 26. Giannantoni, A. et al. Lower urinary tract dysfunction
Efficacy of fingolimod in patients with highly active urodynamic findings in multiple sclerosis: a study and disability status in patients with multiple
relapsing-remitting multiple sclerosis. Curr. Med. Res. of 149 cases. Arch. Phys. Med. Rehabil. 79, 255–257 sclerosis. Arch. Phys. Med. Rehabil. 80, 437–441
Opin. 31, 1687–1691 (2015). (1998). (1999).
7. Nortvedt, M. W. et al. Prevalence of bladder, bowel 17. Kasabian, N. G., Krause, I., Brown, W. E., Khan, Z. 27. De Ridder, D. et al. Bladder cancer in patients with
and sexual problems among multiple sclerosis & Nagler, H. M. Fate of the upper urinary tract in multiple sclerosis treated with cyclophosphamide.
patients two to five years after diagnosis. Mult. Scler. multiple sclerosis. Neurourol. Urodyn. 14, 81–85 J. Urol. 159, 1881–1884 (1998).
13, 106–112 (2007). (1995). 28. Desgrippes, A., Meria, P., Cortesse, A.,
8. Betts, C. D., D’Mellow, M. T. & Fowler, C. J. Urinary 18. Amarenco, G., Kerdraon, J. & Denys, P. Bladder and Cochand-Priollet, B. & Cariou, G. Epidermoid
symptoms and the neurological features of bladder sphincter disorders in multiple sclerosis. Clinical, carcinoma of the bladder [French]. Prog. Urol. 8,
dysfunction in multiple sclerosis. J. Neurol. Neurosurg. urodynamic and neurophysiological study of 225 cases. 321–329 (1998).
Psychiatry 56, 245–250 (1993). Rev. Neurol. (Paris) 151, 722–730 (in French) (1995). 29. Hennessey, A., Robertson, N. P., Swingler, R.
9. Fowler, C. J. et al. A UK consensus on the 19. Murphy, A. M., Bethoux, F., Stough, D. & Compston, D. A. Urinary, faecal and sexual
management of the bladder in multiple sclerosis. & Goldman, H. B. Prevalence of stress urinary dysfunction in patients with multiple sclerosis.
J. Neurol. Neurosurg. Psychiatry 80, 470–477 incontinence in women with multiple sclerosis. J. Neurol. 246, 1027–1032 (1999).
(2009). Int. Neurourol. J. 16, 86–90 (2012). 30. Perrigot, M., Richard, F., Veaux-Renault, V.,
10. Khan, F., Pallant, J. F., Shea, T. L. & Whishaw, M. 20. de Seze, M. et al. The neurogenic bladder in multiple Chatelain, C. & Küss, R. Bladder sphincter disorders
Multiple sclerosis: prevalence and factors impacting sclerosis: review of the literature and proposal of in multiple sclerosis: symptomatology and evolution.
bladder and bowel function in an Australian community management guidelines. Mult. Scler. 13, 915–928 100 cases [French]. Sem. Hôp. 58, 2543–2546
cohort. Disabil. Rehabil. 31, 1567–1576 (2009). (2007). (1982).
12 | ADVANCE ONLINE PUBLICATION www.nature.com/nrurol
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
31. Lawrenson, R., Wyndaele, J. J., Vlachonikolis, I., 54. de Sèze, M. & Gamé, X. Multiple sclerosis and 77. Schurch, B. et al. Botulinum toxin type a is a safe
Farmer, C. & Glickman, S. Renal failure in patients pelviperineology: urinary and sexual dysfunctions and effective treatment for neurogenic urinary
with neurogenic lower urinary tract dysfunction. and pregnancy [French]. Prog. Urol. 24, 483–494 incontinence: results of a single treatment,
Neuroepidemiology 20, 138–143 (2001). (2014). randomized, placebo controlled 6‑month study. J. Urol.
32. Castel-Lacanal, E. et al. Urinary complications and risk 55. De Ridder, D. et al. Conservative bladder management 174, 196–200 (2005).
factors in symptomatic multiple sclerosis patients. Study in advanced multiple sclerosis. Mult. Scler. 11, 78. Cruz, F. et al. Efficacy and safety of
of a cohort of 328 patients. Neurourol. Urodyn. 34, 694–699 (2005). onabotulinumtoxinA in patients with urinary
32–36 (2015). 56. Madhuvrata, P., Singh, M., Hasafa, Z. & Abdel- incontinence due to neurogenic detrusor overactivity:
33. Abrams, P., Cardozo, L., Khoury, S. & Wein, A. (eds) Fattah, M. Anticholinergic drugs for adult neurogenic a randomised, double-blind, placebo-controlled trial.
Incontinence 5th edn (ICUD press, 2013). detrusor overactivity: a systematic review and meta- Eur. Urol. 60, 742–750 (2011).
34. Bonniaud, V. et al. Quality of life in multiple sclerosis analysis. Eur. Urol. 62, 816–830 (2012). 79. Ginsberg, D. et al. Phase 3 efficacy and tolerability
patients with urinary disorders: discriminative validation 57. Fader, M. et al. Intravesical atropine compared to study of onabotulinumtoxinA for urinary incontinence
of the English version of Qualiveen. Qual. Life Res. 14, oral oxybutynin for neurogenic detrusor overactivity: from neurogenic detrusor overactivity. J. Urol. 187,
425–431 (2005). a double-blind, randomized crossover trial. J. Urol. 2131–2139 (2012).
35. Blok, B. et al. Guidelines on neuro-urology. European 177, 208–213 (2007). 80. Ehren, I. et al. Efficacy and impact of botulinum toxin A
Association of Urology [online], http://uroweb.org/ 58. van Rey, F. & Heesakkers, J. Solifenacin in on quality of life in patients with neurogenic detrusor
wp-content/uploads/21-Neuro-Urology_LR2.pdf (2015). multiple sclerosis patients with overactive bladder: overactivity. Scand. J. Urol. Nephrol. 41, 335–340
36. Fowlis, G. A., Waters, J. & Williams, G. The cost a prospective study. Adv. Urol. 2011, 834753 (2011). (2007).
effectiveness of combined rapid tests (Multistix) in 59. Nicholas, R. S., Friede, T., Hollis, S. & Young, C. A. 81. Mangera, A. et al. Contemporary management of
screening for urinary tract infections. J. R. Soc. Med. 87, Anticholinergics for urinary symptoms in multiple lower urinary tract disease with botulinum toxin A:
681–682 (1994). sclerosis. Cochrane Database Syst. Rev. 1, CD004193 a systematic review of botox (onabotulinumtoxinA)
37. Khasriya, R. et al. The inadequacy of urinary dipstick (2009). and dysport (abobotulinumtoxinA). Eur. Urol. 60,
and microscopy as surrogate markers of urinary tract 60. Gajewski, J. B. & Awad, S. A. Oxybutynin versus 784–795 (2011).
infection in urological outpatients with lower urinary tract propantheline in patients with multiple sclerosis 82. Apostolidis, A., Dasgupta, P. & Fowler, C. J. Proposed
symptoms without acute frequency and dysuria. J. Urol. and detrusor hyperreflexia. J. Urol. 135, 966–968 mechanism for the efficacy of injected botulinum toxin
183, 1843–1847 (2010). (1986). in the treatment of human detrusor overactivity.
38. Schwartz, D. S. & Barone, J. E. Correlation of urinalysis 61. Hebjorn, S. Treatment of detrusor hyperreflexia Eur. Urol. 49, 644–650 (2006).
and dipstick results with catheter-associated urinary in multiple sclerosis: a double-blind, crossover clinical 83. Kalsi, V. et al. Botulinum injections for the treatment
tract infections in surgical ICU patients. Intensive Care trial comparing methantheline bromide (Banthine), of bladder symptoms of multiple sclerosis. Ann. Neurol.
Med. 32, 1797–1801 (2006). flavoxate chloride (Urispas) and meladrazine tartrate 62, 452–457 (2007).
39. Mimoz, O., Bouchet, E., Edouard, A., Costa, Y. (Lisidonil). Urol. Int. 32, 209–217 (1977). 84. Mehnert, U., Birzele, J., Reuter, K. & Schurch, B. The
& Samii, K. Limited usefulness of urinary dipsticks to 62. Ethans, K. D., Nance, P. W., Bard, R. J., Casey, A. R. effect of botulinum toxin type a on overactive bladder
screen out catheter-associated bacteriuria in ICU & Schryvers, O. I. Efficacy and safety of tolterodine in symptoms in patients with multiple sclerosis: a pilot
patients. Anaesth. Intensive Care 23, 706–707 (1995). people with neurogenic detrusor overactivity. J. Spinal study. J. Urol. 184, 1011–1016 (2010).
40. Cetinel, B. et al. Management of lower urinary tract Cord Med. 27, 214–218 (2004). 85. Karsenty, G. et al. A novel technique to achieve
dysfunction in multiple sclerosis: a systematic review 63. Amend, B. et al. Effective treatment of neurogenic cutaneous continent urinary diversion in spinal cord-
and Turkish consensus report. Neurourol. Urodyn. 32, detrusor dysfunction by combined high-dosed injured patients unable to catheterize through native
1047–1057 (2013). antimuscarinics without increased side-effects. urethra. Spinal Cord 46, 305–310 (2007).
41. Panicker, J. N., Fowler, C. J. & Kessler, T. M. Lower Eur. Urol. 53, 1021–1028 (2008). 86. Gamé, X. et al. Botulinum toxin A detrusor injections
urinary tract dysfunction in the neurological patient: 64. Valiquette, G., Herbert, J. & Maede‑D’Alisera, P. in patients with neurogenic detrusor overactivity
clinical assessment and management. Lancet Neurol. Desmopressin in the management of nocturia in significantly decrease the incidence of symptomatic
14, 720–732 (2015). patients with multiple sclerosis. A double-blind, urinary tract infections. Eur. Urol. 53, 613–618
42. The National Institute for Health and Care Excellence. crossover trial. Arch. Neurol. 53, 1270–1275 (1996). (2008).
Urinary incontinence in neurological disease: assessment 65. Eckford, S. B., Kohler-Ockmore, J. & Feneley, R. C. 87. Lekka, E. & Lee, L. K. Successful treatment with
and management. [online], https://www.nice.org.uk/ Long-term follow‑up of transvaginal urethral closure intradetrusor botulinum‑A toxin for urethral urinary
guidance/cg148 (2012). and suprapubic cystostomy for urinary incontinence leakage (catheter bypassing) in patients with end-
43. Abrams, P. et al. 4th International Consultation on in women with multiple sclerosis. Br. J. Urol. 74, staged multiple sclerosis and indwelling suprapubic
Incontinence. Recommendations of the international 319–321 (1994). catheters. Eur. Urol. 50, 806–810 (2006).
scientific committee. Evaluation and treatment of urinary 66. Kim, J.-H. in Primer on Multiple Sclerosis (ed. 88. Stoller, M. Afferent nerve stimulation for pelvic floor
incontinence, pelvic organ prolapse and faecal Giesser, B. S.) Ch. 15, 197–206 (Oxford Univ. Press, dysfunction. Eur. Urol. 35 (Suppl. 2), 16 (1999).
incontinence. Neurourol. Urodyn. 29, 213–240 (2010). 2011). 89. Kabay, S. C., Kabay, S., Yucel, M. & Ozden, H. Acute
44. Mingat, N. et al. Prospective study of methods of renal 67. Zahariou, A., Karamouti, M., Karagiannis, G. urodynamic effects of percutaneous posterior tibial
function evaluation in patients with neurogenic bladder & Papaioannou, P. Maximal bladder capacity is nerve stimulation on neurogenic detrusor overactivity in
dysfunction. Urology 82, 1032–1037 (2013). a positive predictor of response to desmopressin patients with Parkinson’s disease. Neurourol. Urodyn.
45. Caramella, D. et al. Videourodynamics in patients with treatment in patients with MS and nocturia. 28, 62–67 (2009).
neurogenic bladder due to multiple sclerosis: our Int. Urol. Nephrol. 40, 65–69 (2008). 90. Kabay, S. C., Yucel, M. & Kabay, S. Acute effect of
experience. Radiol. Med. 116, 432–443 (2011). 68. Tubridy, N., Addison, R. & Schon, F. Long term use posterior tibial nerve stimulation on neurogenic
46. Bryant, C. M., Dowell, C. J. & Fairbrother, G. Caffeine of desmopressin for urinary symptoms in multiple detrusor overactivity in patients with multiple sclerosis:
reduction education to improve urinary symptoms. sclerosis. Mult. Scler. 5, 416–417 (1999). urodynamic study. Urology 71, 641–645 (2008).
Br. J. Nurs. 11, 560–565 (2002). 69. Hoverd, P. A. & Fowler, C. J. Desmopressin in the 91. Gobbi, C. et al. Percutaneous posterior tibial nerve
47. Klarskov, P., Heely, E., Nyholdt, I., Rottensten, K. treatment of daytime urinary frequency in patients stimulation as an effective treatment of refractory
& Nordenbo, A. Biofeedback treatment of bladder with multiple sclerosis. J. Neurol. Neurosurg. lower urinary tract symptoms in patients with multiple
dysfunction in multiple sclerosis. A randomized trial. Psychiatry 65, 778–780 (1998). sclerosis: preliminary data from a multicentre,
Scand. J. Urol. Nephrol. Suppl. 157, 61–65 (1994). 70. Fredrikson, S. Nasal spray desmopressin treatment of prospective, open label trial. Mult. Scler. 17,
48. Vahtera, T., Haaranen, M., Viramo-Koskela, A. L. bladder dysfunction in patients with multiple sclerosis. 1514–1519 (2011).
& Ruutiainen, J. Pelvic floor rehabilitation is effective Acta Neurol. Scand. 94, 31–34 (1996). 92. Andrews, B. J. & Reynard, J. M. Transcutaneous
in patients with multiple sclerosis. Clin. Rehabil. 11, 71. Hilton, P., Hertogs, K. & Stanton, S. L. The use of posterior tibial nerve stimulation for treatment of
211–219 (1997). desmopressin (DDAVP) for nocturia in women with detrusor hyperreflexia in spinal cord injury. J. Urol.
49. McClurg, D., Ashe, R. G. & Lowe-Strong, A. S. multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 170, 926 (2003).
Neuromuscular electrical stimulation and the treatment 46, 854–855 (1983). 93. Govier, F. E., Litwiller, S., Nitti, V., Kreder, K. J. Jr
of lower urinary tract dysfunction in multiple sclerosis — 72. Bosma, R., Wynia, K., Havlíková, E., De Keyser, J. & Rosenblatt, P. Percutaneous afferent
a double blind, placebo controlled, randomised clinical & Middel, B. Efficacy of desmopressin in patients with neuromodulation for the refractory overactive
trial. Neurourol. Urodyn. 27, 231–237 (2008). multiple sclerosis suffering from bladder dysfunction: bladder: results of a multicenter study. J. Urol. 165,
50. McClurg, D., Ashe, R. G., Marshall, K. & Lowe- a meta-analysis. Acta Neurol. Scand. 112, 1–5 1193–1198 (2001).
Strong, A. S. Comparison of pelvic floor muscle training, (2005). 94. van Balken, M. R., Vergunst, H. & Bemelmans, B. L. H.
electromyography biofeedback, and neuromuscular 73. Hedlund, P. Cannabinoids and the endocannabinoid Prognostic factors for successful percutaneous tibial
electrical stimulation for bladder dysfunction in people system in lower urinary tract function and dysfunction. nerve stimulation. Eur. Urol. 49, 360–365 (2006).
with multiple sclerosis: a randomized pilot study. Neurourol. Urodyn. 33, 46–53 (2014). 95. Kabay, S. et al. The clinical and urodynamic results
Neurourol. Urodyn. 25, 337–348 (2006). 74. Freeman, R. M. et al. The effect of cannabis on urge of a 3‑month percutaneous posterior tibial nerve
51. Lucio, A., D’Ancona, C., Lopes, M., Perissinotto, M. incontinence in patients with multiple sclerosis: stimulation treatment in patients with multiple
& Damasceno, B. The effect of pelvic floor muscle a multicentre, randomised placebo-controlled trial sclerosis-related neurogenic bladder dysfunction.
training alone or in combination with electrostimulation (CAMS-LUTS). Int. Urogynecol. J. Pelvic Floor Neurourol. Urodyn. 28, 964–968 (2009).
in the treatment of sexual dysfunction in women with Dysfunct. 17, 636–641 (2006). 96. de Seze, M. et al. Transcutaneous posterior tibial nerve
multiple sclerosis. Mult. Scler. 20, 1761–1768 (2014). 75. Brady, C. M. et al. An open-label pilot study of stimulation for treatment of the overactive bladder
52. Deffieux, X. et al. Pelvic floor rehabilitation for female cannabis-based extracts for bladder dysfunction syndrome in multiple sclerosis: results of a multicenter
urinary incontinence: mechanisms of action [French]. in advanced multiple sclerosis. Mult. Scler. 10, prospective study. Neurourol. Urodyn. 30, 306–311
Prog. Urol. 23, 491–501 (2013). 425–433 (2004). (2011).
53. De Ridder, D., Vermeulen, C., Ketelaer, P., 76. Kavia, R. B. C., De Ridder, D., Constantinescu, C. S., 97. Chartier-Kastler, E. J. et al. Long-term results of sacral
Van Poppel, H. & Baert, L. Pelvic floor rehabilitation Stott, C. G. & Fowler, C. J. Randomized controlled trial nerve stimulation (S3) for the treatment of neurogenic
in multiple sclerosis. Acta Neurol. Belg. 99, 61–64 of Sativex to treat detrusor overactivity in multiple refractory urge incontinence related to detrusor
(1999). sclerosis. Mult. Scler. 16, 1349–1359 (2010). hyperreflexia. J. Urol. 164, 1476–1480 (2000).
NATURE REVIEWS | UROLOGY ADVANCE ONLINE PUBLICATION | 13
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
98. Craggs, M. & McFarlane, J. Neuromodulation of the 116. Legrand, G. et al. Functional outcomes after 131. West, D. A. et al. Role of chronic catheterization
lower urinary tract. Exp. Physiol. 84, 149–160 management of end-stage neurological bladder in the development of bladder cancer in patients
(1999). dysfunction with ileal conduit in a multiple sclerosis with spinal cord injury. Urology 53, 292–297 (1999).
99. Kessler, T. M. et al. Sacral neuromodulation for population: a monocentric experience. Urology 78, 132. James, R., Frasure, H. E. & Mahajan, S. T. Urinary
neurogenic lower urinary tract dysfunction: systematic 937–941 (2011). catheterization may not adversely impact quality of
review and meta-analysis. Eur. Urol. 58, 865–874 117. Guillotreau, J. et al. Prospective evaluation of life in multiple sclerosis patients. ISRN Neurol. 2014,
(2010). laparoscopic assisted cystectomy and ileal conduit 167030 (2014).
100. Wallace, P. A., Lane, F. L. & Noblett, K. L. Sacral in advanced multiple sclerosis. Urology 80, 852–857 133. Chancellor, M. B. et al. Sphincteric stent versus
nerve neuromodulation in patients with underlying (2012). external sphincterotomy in spinal cord injured men:
neurologic disease. Am. J. Obstet. Gynecol. 197, 118. Lapides, J., Diokno, A. C., Silber, S. J. & Lowe, B. S. prospective randomized multicenter trial. J. Urol. 161,
96.e1–96.e5 (2007). Clean, intermittent self-catheterization in the 1893–1898 (1999).
101. Chaabane, W. et al. Sacral neuromodulation for treatment of urinary tract disease. Trans. Am. Assoc. 134. Fontaine, E. et al. Reappraisal of endoscopic
treating neurogenic bladder dysfunction: clinical and Genitourin. Surg. 63, 92–96 (1971). sphincterotomy for post-traumatic neurogenic
urodynamic study. Neurourol. Urodyn. 30, 547–550 119. Kirchhof, K. & Fowler, C. J. The value of the Kurtzke bladder: a prospective study. J. Urol. 155, 277–280
(2011). Functional Systems Scales in predicting incomplete (1996).
102. Minardi, D. & Muzzonigro, G. Sacral neuromodulation bladder emptying. Spinal Cord 38, 409–413 135. Gallien, P. et al. Placebo controlled, randomised,
in patients with multiple sclerosis. World J. Urol. 30, (2000). double blind study of the effects of botulinum A toxin
123–128 (2011). 120. Vahter, L. et al. Clean intermittent self-catheterization on detrusor sphincter dyssynergia in multiple sclerosis
103. Peters, K. M., Kandagatla, P., Killinger, K. A., in persons with multiple sclerosis: the influence of patients. J. Neurol. Neurosurg. Psychiatry 76,
Wolfert, C. & Boura, J. A. Clinical outcomes of cognitive dysfunction. Mult. Scler. 15, 379–384 1670–1676 (2005).
sacral neuromodulation in patients with neurologic (2009). 136. de Sèze, M. et al. Botulinum A toxin and detrusor
conditions. Urology 81, 738–743 (2013). 121. Seth, J. H., Haslam, C. & Panicker, J. N. Ensuring sphincter dyssynergia: a double-blind lidocaine-
104. Minardi, D. & Muzzonigro, G. Lower urinary tract patient adherence to clean intermittent self- controlled study in 13 patients with spinal cord
and bowel disorders and multiple sclerosis: role catheterization. Patient Prefer. Adherence 8, disease. Eur. Urol. 42, 56–62 (2002).
of sacral neuromodulation: a preliminary report. 191–198 (2014). 137. Phelan, M. W. et al. Botulinum toxin urethral sphincter
Neuromodulation 8, 176–181 (2005). 122. Sand, P. K. & Sand, R. I. The diagnosis and injection to restore bladder emptying in men and
105. Marinkovic, S. P. & Gillen, L. M. Sacral management of lower urinary tract symptoms in women with voiding dysfunction. J. Urol. 165,
neuromodulation for multiple sclerosis patients multiple sclerosis patients. Dis. Mon. 59, 261–268 1107–1110 (2001).
with urinary retention and clean intermittent (2013). 138. Utomo, E., Groen, J. & Blok, B. F. Surgical
catheterization. Int. Urogynecol J. 21, 223–228 123. Yonnet, G. J., Fjeldstad, A. S., Carlson, N. G. management of functional bladder outlet obstruction
(2010). & Rose, J. W. Advances in the management of in adults with neurogenic bladder dysfunction.
106. Andretta, E., Simeone, C., Ostardo, E., Pastorello, M. neurogenic detrusor overactivity in multiple sclerosis. Cochrane Database Syst. Rev. 5, CD004927
& Zuliani, C. Usefulness of sacral nerve modulation in Int. J. MS Care 15, 66–72 (2013). (2014).
a series of multiple sclerosis patients with bladder 124. Schulte-Baukloh, H. et al. Efficacy of botulinum‑A
dysfunction. J. Neurol. Sci. 347, 257–261 toxin bladder injections for the treatment of Acknowledgements
(2014). neurogenic detrusor overactivity in multiple sclerosis V.P. acknowledges support from the European Urological
107. Zachoval, R. et al. Augmentation cystoplasty in patients: an objective and subjective analysis. Scholarship Programme
patients with multiple sclerosis. Urol. Int. 70, 21–26 Neurourol. Urodyn. 25, 110–115 (2006).
Author contributions
(2003). 125. Castel-Lacanal, E. et al. Impact of intermittent
All authors researched data for this article, and made a sig-
108. Venn, S. N. & Mundy, A. R. Long-term results of catheterization on the quality of life of multiple
nificant contribution to discussions of content. V.P. wrote the
augmentation cystoplasty. Eur. Urol. 34, 40–42 sclerosis patients. World J. Urol. 31, 1445–1450
manuscript, and all authors reviewed and/or edited
(1998). (2013).
the manuscript prior to submission.
109. Herschorn, S. Long-term outcome of augmentation 126. O’Riordan, J. I. et al. Do alpha-blockers have a role
enterocystoplasty for neurogenic bladder. J. Urol. in lower urinary tract dysfunction in multiple Competing interest statement
187, e668 (2012). sclerosis? J. Urol. 153, 1114–1116 (1995). E.C.K. has acted as a consultant of Allergan, Astellas,
110. Gould, J. J. & Stoffel, J. T. Robotic enterocystoplasty: 127. Weld, K. J. & Dmochowski, R. R. Effect of bladder Axonics, Coloplast, Medtronic and and, and has received
technique and early outcomes. J. Endourol. 25, management on urological complications in spinal honoraria from Allergan, Astellas, Coloplast, Medtronic and
91–95 (2011). cord injured patients. J. Urol. 163, 768–772 Pfizer. V.P. and J.P. declare no competing interests.
111. Liard, A., Séguier-Lipszyc, E., Mathiot, A. & (2000).
Mitrofanoff, P. The Mitrofanoff procedure: 20 years 128. Bennett, C. J., Young, M. N., Adkins, R. H. & Diaz, F. Review criteria
later. J. Urol. 165, 2394–2398 (2001). Comparison of bladder management complication A literature research was performed using searches of the
112. Moreno, J. G. et al. Improved quality of life and outcomes in female spinal cord injury patients. Medline database with the following keywords alone or in
sexuality with continent urinary diversion in J. Urol. 153, 1458–1460 (1995). combination: “multiple sclerosis”, “neurogenic bladder”,
quadriplegic women with umbilical stoma. 129. Larsen, L. D., Chamberlin, D. A., Khonsari, F. “prevalence”, “epidemiology”, “intermittent” catheterization”,
Arch. Phys. Med. Rehabil. 76, 758–762 (1995). & Ahlering, T. E. Retrospective analysis of urologic “antimuscarinics”, “desmopressin”, “botulinum toxin A”, “can-
113. Stein, R. et al. Urinary diversion and orthotopic complications in male patients with spinal cord injury nabinoids”, “tibial nerve stimulation”, “sacral neuromodula-
bladder substitution in children and young adults managed with and without indwelling urinary tion”, “augmentation cystoplasty”, “continent urinary
with neurogenic bladder: a safe option for treatment? catheters. Urology 50, 418–422 (1997). diversion”, “ileal conduit” and “sphincterotomy”. Relevant
J. Urol. 163, 568–573 (2000). 130. Mitsui, T., Minami, K., Furuno, T., Morita, H. articles that reported the prevalence of LUT symptoms
114. Vian, E., Soustelle, L., Viale, S. & Costa, P. A technique & Koyanagi, T. Is suprapubic cystostomy an optimal among patients with multiple sclerosis or the outcomes of the
of continent vesicostomy with ileocystoplasty: study of urinary management in high quadriplegics? management of LUT symptoms among patients with multiple
32 patients. Prog. Urol. 19, 116–121 (2009). A comparative study of suprapubic cystostomy sclerosis specifically were identified. The studies were limited
115. Jacques, C., David, G. & Gilles, K. (eds) Textbook of and clean intermittent catheterization. Eur. Urol. 38, to full-text articles that were published in English and in
the Neurogenic Bladder 3rd edn (CRC Press, 2011). 434–438 (2000). French until the 1st of May 2015. Case reports were excluded.
14 | ADVANCE ONLINE PUBLICATION www.nature.com/nrurol
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
You might also like
- NBME 26 Question - AnswerDocument54 pagesNBME 26 Question - AnswerAsmaaNasserNo ratings yet
- Reader's Digest USA - November 2021Document126 pagesReader's Digest USA - November 2021Reference CambridgeExams67% (3)
- Creog Urogyn ReviewDocument97 pagesCreog Urogyn ReviewAlexandriah AlasNo ratings yet
- Urodynamics (Aquick Pocket Guide)Document210 pagesUrodynamics (Aquick Pocket Guide)ZICO100% (2)
- Physical Therapy Patient Pelvic Floor Assessment FormDocument4 pagesPhysical Therapy Patient Pelvic Floor Assessment FormTopaz Company100% (1)
- Assessment WorkbookDocument48 pagesAssessment WorkbookBhinder ThindNo ratings yet
- Case Scenario-Study 2Document6 pagesCase Scenario-Study 2J100% (1)
- Neuro QuestionsDocument19 pagesNeuro Questionssarasmith1988100% (6)
- ES GastrointestinalDocument12 pagesES GastrointestinalMateus ValenteNo ratings yet
- 10 1038@nrneph 2017 85 PDFDocument13 pages10 1038@nrneph 2017 85 PDFSirGonzNo ratings yet
- Grupo 6 - Pancreatitis Crónica (01-15)Document15 pagesGrupo 6 - Pancreatitis Crónica (01-15)Romina GonzálezNo ratings yet
- Primer: Chronic PancreatitisDocument18 pagesPrimer: Chronic PancreatitisFrancisco FigueiredoNo ratings yet
- Pancreatitis 2Document8 pagesPancreatitis 2Romina GonzálezNo ratings yet
- Redefining Lupus Nephritis, Clinical Implications of Pathophysiologic Subtypes PDFDocument14 pagesRedefining Lupus Nephritis, Clinical Implications of Pathophysiologic Subtypes PDFaneliatiarasuciNo ratings yet
- Dyslipidaemia in Nephrotic Syndrome: Mechanisms and TreatmentDocument14 pagesDyslipidaemia in Nephrotic Syndrome: Mechanisms and TreatmentEss liNo ratings yet
- Membranosa 2Document17 pagesMembranosa 2Carolina CastroNo ratings yet
- Scleroderma Renal Crisis and Renal Involvement in Systemic SclerosisDocument14 pagesScleroderma Renal Crisis and Renal Involvement in Systemic Sclerosiszlaticab4246No ratings yet
- Nrgastro 2017 38Document15 pagesNrgastro 2017 38Fasya DaffaNo ratings yet
- Panes Rimola 2017Document13 pagesPanes Rimola 2017Natasya DarrelNo ratings yet
- Modelling Diabetic Nephropathy in MiceDocument9 pagesModelling Diabetic Nephropathy in MiceKarina ThiemeNo ratings yet
- Reviews: Obesity-Related Glomerulopathy: Clinical and Pathologic Characteristics and PathogenesisDocument19 pagesReviews: Obesity-Related Glomerulopathy: Clinical and Pathologic Characteristics and Pathogenesisthaynara robertoNo ratings yet
- Synovial Tissue Research State of The Art ReviewDocument13 pagesSynovial Tissue Research State of The Art ReviewDeliana Nur Ihsani RahmiNo ratings yet
- Reviews: Hirschsprung Disease - Integrating Basic Science and Clinical Medicine To Improve OutcomesDocument16 pagesReviews: Hirschsprung Disease - Integrating Basic Science and Clinical Medicine To Improve OutcomesThanh Thảo PhanNo ratings yet
- Parkinson DiseaseDocument21 pagesParkinson DiseasegabisaenaNo ratings yet
- HdhdudhdhDocument20 pagesHdhdudhdhRafaelNo ratings yet
- Reviews: A Clinicopathological Approach To The Diagnosis of DementiaDocument16 pagesReviews: A Clinicopathological Approach To The Diagnosis of DementiaLeonardo Barrera ArizaNo ratings yet
- Barturen 2018Document20 pagesBarturen 2018jezy2014No ratings yet
- Potential New Therapy For OphthalmopathyDocument1 pagePotential New Therapy For OphthalmopathyEsteban Martin Chiotti KaneshimaNo ratings yet
- Kellum 2018Document14 pagesKellum 2018hemer hadyn calderon alvitesNo ratings yet
- Reviews: Inflammation in Gout: Mechanisms and Therapeutic TargetsDocument9 pagesReviews: Inflammation in Gout: Mechanisms and Therapeutic TargetsBless MineNo ratings yet
- Nrneurol 2016 150Document15 pagesNrneurol 2016 150tonnyprogramadorNo ratings yet
- NeuroblastomaDocument21 pagesNeuroblastomaRichard DjigoNo ratings yet
- Nrneurol 2018 30 PDFDocument16 pagesNrneurol 2018 30 PDFFathan MustafidNo ratings yet
- AdrenolukodistropyDocument10 pagesAdrenolukodistropymary uwuNo ratings yet
- Loeser PDFDocument9 pagesLoeser PDFGaudeamus IgiturNo ratings yet
- Oligometastatic Prostate Cancer. Definitions, Clinical Outcomes, and Treatment Considerations (2017) .Document11 pagesOligometastatic Prostate Cancer. Definitions, Clinical Outcomes, and Treatment Considerations (2017) .Orlando SotoNo ratings yet
- Metaplasia. Nature ReviewsDocument11 pagesMetaplasia. Nature ReviewsCamila RodríguezNo ratings yet
- HVDA No Varcieal Nature 2018Document21 pagesHVDA No Varcieal Nature 2018Juan Jose SarastiNo ratings yet
- 10 1038@nrurol 2018 1Document15 pages10 1038@nrurol 2018 1cristianNo ratings yet
- Calcification AorticDocument28 pagesCalcification AorticGaal PinNo ratings yet
- Tsokos 2016Document15 pagesTsokos 2016karen rinconNo ratings yet
- Vascular Cognitive ImpairmentDocument16 pagesVascular Cognitive ImpairmentVitor Souza100% (1)
- Giant Cell Arteritis and Polymyalgia Rheumatica: Current Challenges and OpportunitiesDocument15 pagesGiant Cell Arteritis and Polymyalgia Rheumatica: Current Challenges and OpportunitiesSue BarrNo ratings yet
- MalariaDocument13 pagesMalariaAndres Felipe DuqueNo ratings yet
- Non-Variceal Upper Gastrointestinal BleedingDocument21 pagesNon-Variceal Upper Gastrointestinal BleedingSiddhartha PalaciosNo ratings yet
- Constipacion Review 2017Document19 pagesConstipacion Review 2017Ronald MoraNo ratings yet
- Nontraumatic Intracerebral Haemorrhage in Young AdultsDocument14 pagesNontraumatic Intracerebral Haemorrhage in Young AdultsAmalia Gh,No ratings yet
- Renal CellDocument10 pagesRenal CellEss liNo ratings yet
- Enfermedades Mitocondriales.Document16 pagesEnfermedades Mitocondriales.cristobalarancibia71No ratings yet
- NRDP 20174Document17 pagesNRDP 20174EccoNo ratings yet
- Mieloma Multiple Nature.Document20 pagesMieloma Multiple Nature.pacho21No ratings yet
- Lectura Seminario 3 - NF1Document17 pagesLectura Seminario 3 - NF1Diego SoteloNo ratings yet
- Escobar Mor Real e 2018Document15 pagesEscobar Mor Real e 2018HIDAYATUL RAHMINo ratings yet
- Erythematosus - 2017Document11 pagesErythematosus - 2017Matheus AugustoNo ratings yet
- Salivary Duct Stenosis Diagnosis and TreatmentDocument10 pagesSalivary Duct Stenosis Diagnosis and TreatmentYeni PuspitasariNo ratings yet
- Primer: Amyotrophic Lateral SclerosisDocument19 pagesPrimer: Amyotrophic Lateral SclerosisBerkay ALpayNo ratings yet
- Cardiomiopatia Hipertrofica 2016 PDFDocument25 pagesCardiomiopatia Hipertrofica 2016 PDFBlanca Herrera MoralesNo ratings yet
- A Systemic View of Alzheimer Disease 2017Document12 pagesA Systemic View of Alzheimer Disease 2017Jaime Arevalo PanduroNo ratings yet
- PRIMER de LES 2016 PDFDocument21 pagesPRIMER de LES 2016 PDFAndres DoblerNo ratings yet
- Manifestaciones Neurologicas VIH NatureDocument13 pagesManifestaciones Neurologicas VIH NatureGeral D. VelascoNo ratings yet
- Alzheimer e Diabetes Nature 2018Document14 pagesAlzheimer e Diabetes Nature 2018Viviane MacedoNo ratings yet
- Hepatocarcinoma 2Document23 pagesHepatocarcinoma 2NaraMayhumiDeBelenMerinoOrtizNo ratings yet
- Piezos Thrive Under PressureDocument13 pagesPiezos Thrive Under PressureВладимир ДружининNo ratings yet
- Kuner 2016Document11 pagesKuner 2016Guilherme MonteiroNo ratings yet
- Wong2016 PDFDocument17 pagesWong2016 PDFMelissa Peña LópezNo ratings yet
- Orofacial Manifestations of Systemic SclerosisDocument6 pagesOrofacial Manifestations of Systemic SclerosisIt's MeNo ratings yet
- Biochemical Correlates of Brain Structure and FunctionFrom EverandBiochemical Correlates of Brain Structure and FunctionA.N. DavisonNo ratings yet
- Consultation in Neurourology: A Practical Evidence-Based GuideFrom EverandConsultation in Neurourology: A Practical Evidence-Based GuideNo ratings yet
- prm/2018/11 4/prm 11 4 prm170481/prm 11 prm170481Document9 pagesprm/2018/11 4/prm 11 4 prm170481/prm 11 prm170481Putri Rizky AmaliaNo ratings yet
- NeurogenicbladdermanagementwithcompleteurethraldistructionDocument11 pagesNeurogenicbladdermanagementwithcompleteurethraldistructionPutri Rizky AmaliaNo ratings yet
- Outcomes of Ileal Conduit Urinary Diversion in Patients With Multiple SclerosisDocument7 pagesOutcomes of Ileal Conduit Urinary Diversion in Patients With Multiple SclerosisPutri Rizky AmaliaNo ratings yet
- Peterson 2012Document5 pagesPeterson 2012Putri Rizky AmaliaNo ratings yet
- Controversial TopicDocument11 pagesControversial TopicPutri Rizky AmaliaNo ratings yet
- Rhinitis Allergy and ElderlyDocument26 pagesRhinitis Allergy and ElderlyPutri Rizky AmaliaNo ratings yet
- Role of Rhinitis in Laryngitis: Another Dimension of The Unified AirwayDocument6 pagesRole of Rhinitis in Laryngitis: Another Dimension of The Unified AirwayPutri Rizky AmaliaNo ratings yet
- Healthcare: Allergic Rhinitis and Laryngeal Pathology: Real-World EvidenceDocument9 pagesHealthcare: Allergic Rhinitis and Laryngeal Pathology: Real-World EvidencePutri Rizky AmaliaNo ratings yet
- Literature Reading Short StatureDocument34 pagesLiterature Reading Short StaturePutri Rizky AmaliaNo ratings yet
- HHS Public Access: 236 Children With Developmental Hydrocephalus: Causes and Clinical ConsequencesDocument22 pagesHHS Public Access: 236 Children With Developmental Hydrocephalus: Causes and Clinical ConsequencesPutri Rizky AmaliaNo ratings yet
- The Half-Life of Infusion Fluids An Educational ReviewDocument8 pagesThe Half-Life of Infusion Fluids An Educational ReviewPutri Rizky AmaliaNo ratings yet
- Doctor Patient RelationshipDocument21 pagesDoctor Patient RelationshipPutri Rizky AmaliaNo ratings yet
- Epos Summary PDFDocument30 pagesEpos Summary PDFPutri Rizky AmaliaNo ratings yet
- Post Partum ComplicationDocument29 pagesPost Partum ComplicationPutri Rizky AmaliaNo ratings yet
- Jadwal Perkulihanan THN 4 2019-2020 TM-FMDocument20 pagesJadwal Perkulihanan THN 4 2019-2020 TM-FMPutri Rizky AmaliaNo ratings yet
- Pengaruh Kegel Exercise Terhadap Inkontinensia Urine Pada Ibu Postpartum MultiparaDocument8 pagesPengaruh Kegel Exercise Terhadap Inkontinensia Urine Pada Ibu Postpartum MultiparaYunita RahayuNo ratings yet
- Haylen Et Al-2016-Neurourology and UrodynamicsDocument33 pagesHaylen Et Al-2016-Neurourology and UrodynamicsanyNo ratings yet
- HysterectomyDocument10 pagesHysterectomyjhodaneNo ratings yet
- Notes On The Board of DR - Nadine's Lectures: Gynecology & Obstetrics For 5 Year Medical StudentsDocument58 pagesNotes On The Board of DR - Nadine's Lectures: Gynecology & Obstetrics For 5 Year Medical Studentssrhmd100% (2)
- Module 7 Identification of Obstetric Fistula Fistula CareDocument9 pagesModule 7 Identification of Obstetric Fistula Fistula Caregeorgeloto12No ratings yet
- DX Spine Injury PDFDocument5 pagesDX Spine Injury PDFSherree HayesNo ratings yet
- Jurnal - Postpartum Urinary RetentionDocument28 pagesJurnal - Postpartum Urinary RetentionBoyParadiseNo ratings yet
- UTI'sDocument3 pagesUTI'sElirene IrenNo ratings yet
- Perubahan Bio, Spiritual Dan Kultural Yang Lazim Terjadi Pada - Ger - Mrs Wanti - SMT Genap - March2019Document15 pagesPerubahan Bio, Spiritual Dan Kultural Yang Lazim Terjadi Pada - Ger - Mrs Wanti - SMT Genap - March2019Cahya SupriatnaNo ratings yet
- Handouts - PeriopDocument79 pagesHandouts - PerioplibalibzyrelleNo ratings yet
- Micturition 2022Document20 pagesMicturition 2022Mohammad zreadNo ratings yet
- Urinary Tract Infection in The ElderlyDocument18 pagesUrinary Tract Infection in The ElderlyNicky AlexandraNo ratings yet
- 06 Pelvic Floor Muscle Training For WomenDocument5 pages06 Pelvic Floor Muscle Training For WomenAINo ratings yet
- General Urology Question and Answer ItemsDocument13 pagesGeneral Urology Question and Answer ItemsalaamorsyNo ratings yet
- Assignment 2Document8 pagesAssignment 2Krithardh ChunchuNo ratings yet
- BLadder Outlet ObstructionDocument28 pagesBLadder Outlet ObstructionCodillia Cheong100% (1)
- Preslica Ili Rastavić Equisetum Arvense LDocument5 pagesPreslica Ili Rastavić Equisetum Arvense LtamaraiivanaNo ratings yet
- Liverpool Outcome Score (LOS) For Assessing Adults at DischargeDocument3 pagesLiverpool Outcome Score (LOS) For Assessing Adults at Dischargekartika farahdillaNo ratings yet
- Nanda 2018 2020Document7 pagesNanda 2018 2020lerma delasondraNo ratings yet
- Urinary Tract Infections in ChildrenDocument8 pagesUrinary Tract Infections in ChildrenLorelie AsisNo ratings yet
- Transurethral Resection of The ProstateDocument4 pagesTransurethral Resection of The Prostatezesty-merr-l-akut-9424No ratings yet
- Hanging Bladder Calculi Secondary To Misplaced Surgical SutureDocument3 pagesHanging Bladder Calculi Secondary To Misplaced Surgical SutureChato Haviz DanayomiNo ratings yet