Professional Documents
Culture Documents
International Journal of Anesthetics and Anesthesiology Ijaa 7 118
Uploaded by
Ferdy RahadiyanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
International Journal of Anesthetics and Anesthesiology Ijaa 7 118
Uploaded by
Ferdy RahadiyanCopyright:
Available Formats
ISSN: 2377-4630
Sezen et al. Int J Anesthetic Anesthesiol 2020, 7:118
DOI: 10.23937/2377-4630/1410118
Volume 7 | Issue 4
International Journal of Open Access
Anesthetics and Anesthesiology
Original Article
The Effect of Single-Dose Preemptive Intravenous Ibuprofen on the
Intraoperative Hemodynamic Parameters, Recovery Characteristics,
and Acute Pain after Laparoscopic Cholecystectomy: A Randomized
Double-Blind, Placebo-Controlled Clinical Trial
Ozlem Sezen, MD* , Banu Cevik , MD and Kemal Tolga Saracoglu , MD Check for
updates
University of Health Sciences, Kartal Dr.Lutfi Kırdar Training and Research Hospital, Turkey
*Corresponding author: Ozlem Sezen, MD, University of Health Sciences, Kartal Dr. Lutfi Kırdar Training and Research
Hospital, Istanbul, Turkey, Tel: 90216-441-39-00; +90532-391-82-98
Abstract Results: There was no difference between the groups in
terms of hemodynamic findings before anesthesia induction
Background/aims: The aim of this study was to investigate and in the peroperative period. The time until Aldrete score
the effects of the preemptive administration of a single dose of 9 was statistically significantly shorter in Group I (Group
of intravenous (IV) ibuprofen on the intraoperative hemody- I 3.8 ± 1.4 min, and Group C 6.3 ± 1.9 min, p < 0.001).
namic parameters, recovery characteristics, and postopera- Sevoflurane consumption was lower in the group given pre-
tive pain management in patients undergoing laparoscopic emptive single dose IV ibuprofen, but the time to first po-
cholecystectomy. The time to first analgesic requirement stoperative analgesic requirement was longer (p < 0.001).
during postoperative period was the main goal of this study. Total analgesic consumption was highest in Group C (p <
Material and methods: Following ethical committee ap- 0.001).
proval, sixty patients scheduled for laparoscopic cholecy- Conclusion: Preemptive single dose i.v. ibuprofen (400
stectomy with American Society of Anesthesiologists (ASA) mg) can be used in laparoscopic cholecystectomy with the
physical status I-II and aged 30-65 years of either genders advantages of reducing the consumption of peroperative
were included in this prospective, randomized, place- sevoflurane, providing better VAS scores, shortening the
bo-controlled double blinded study. Patients were randomly time to the first postoperative analgesic requirement and
divided into two groups. reducing analgesic consumption.
The study group (group I) received 400 mg ibuprofen in 100
Keywords
ml IV saline 15 min before anesthesia induction, whereas
the placebo group (group C) received IV 100 ml saline only. Ibuprofen, Preemptive analgesia, Laparoscopic cholecy-
The study drug and the saline were administered by an stectomy, Postoperative analgesia
anesthesia nurse blinded to the study. The same general
anesthesia protocol was applied in both groups. Hemody-
namic parameters (non-invasive systolic (SAP), diastolic Introduction
(DAP) and mean (MAP) arterial pressure, heart rate (HR),
bispectral index (BIS) values and SpO2 values were recor-
Laparoscopic cholecystectomy is a widely preferred
ded before induction (baseline) and after induction, perope- minimally invasive surgical technique for gallstone dis-
rative 10, 20, 30, minutes., before extubation. The time to eases due to its shorter hospitalization, faster healing,
achieve a modified Aldrete score of ≥ 9 was recorded as the a better cosmetic outcome, and less postoperative pain
recovery time. During postoperative period, the time to first
characteristics. The pain after laparoscopic cholecystec-
analgesic requirement and the total amount of analgesics
within 24 hours was recorded. Patients were asked to give a tomy is regarded as visceral, quite complex and result-
number between from 1 to 5 for the satisfaction assessment ed from the insufflation of carbon dioxide into the peri-
for the anesthesia management. toneal cavity, abdominal distension, port-site incisions
Citation: Sezen O, Cevik B, Saracoglu KT (2020) The Effect of Single-Dose Preemptive Intravenous Ibu-
profen on the Intraoperative Hemodynamic Parameters, Recovery Characteristics, and Acute Pain af-
ter Laparoscopic Cholecystectomy: A Randomized Double-Blind, Placebo-Controlled Clinical Trial. Int J
Anesthetic Anesthesiol 7:118. doi.org/10.23937/2377-4630/1410118
Accepted: December 29, 2020: Published: December 31, 2020
Copyright: © 2020 Sezen O, et al. This is an open-access article distributed under the terms of the
Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction
in any medium, provided the original author and source are credited.
Sezen et al. Int J Anesthetic Anesthesiol 2020, 7:118 • Page 1 of 7 •
DOI: 10.23937/2377-4630/1410118 ISSN: 2377-4630
and patient factors [1]. Although the pain intensity and Materials and Methods
duration are less than the open surgical approach, the
This prospective, randomized, placebo-controlled
optimum analgesic modality has remained a challenging
double blinded study was conducted after receiving the
issue. Multimodal analgesia regimen combining opioids,
approval of the ethics committee (2020/514/170/24)
non-steroidal anti-inflammatory drugs, and local anes-
and the written, informed consent of all of the partici-
thetic infiltration to the port sites are the most recom-
pants, according to the Good Clinical Practice guidelines
mended treatment of choices for postoperative pain
and the principles of the Declaration of Helsinki. Sixty
management after laparoscopic cholecystectomy [2].
patients scheduled for laparoscopic cholecystectomy
Preemptive use of systemic analgesics combined with American Society of Anesthesiologists (ASA) phys-
with the general anesthesia has some beneficial effects ical status I-II and aged 30-65 years of either genders
such as blocking nociceptive pathways, reducing the were included the study.
amount of pharmacological agents needed to maintain
the general anesthesia, and decreasing the time to re- Exclusion criteria
cover from the drug-induced central nervous system Patients with a body mass index of more than 30 kg/
depression [3]. Adequate preemptive analgesia has two m2, pregnancy, cardiac or renal failure, mental distur-
basic requirements; verification of the effectiveness of bance, neurological disease, communication difficulties,
the direct pharmacological effect of treatment and the being unable to comprehend visual analogue scale, pre-
extension of an antinociceptive treatment into the ini- vious clinical history of chronic pain, a history of long-
tial postoperative period [4]. term or during recent 24 h nonsteroidal anti-inflamma-
Nonsteroidal anti-inflammatory drugs (NSAIDs) are tory drug use, a history of peptic ulcer, gastrointestinal
the good treatment of choices for the postoperative bleeding or inflammatory bowel disease, known allergy
pain unless contraindicated due to its opioid-sparing to ibuprofen or other nonsteroidal anti-inflammatory
effect and minimizing the opiate-induced adverse reac- drugs were excluded.
tions [5]. The guideline of the American Society of An- Randomization was achieved by using a comput-
aesthesiologist, Task Force on Acute Pain Management er-generated randomization program operated by an-
recommends that this group of drugs have a significant other clinician blinded to the study and the patients
role in postoperative multimodal pain management [6]. were allocated into two groups to receive either pre-
Like other NSAIDs, ibuprofen has anti-inflammatory, emptive single dose IV ibuprofen (Intrafen 400 mg/4 ml,
antipyretic, and analgesic properties. It causes a rap- en İlaç Ve Sağlık Ürünleri San. Ve Tic. Ltd. Sti., Ankara,
id, reversible and competitive inhibition of the cycloo- Türkiye) (Group I = 30) or IV saline (100 ml) (Group C =
xygenase (COX) isoenzymes. The analgesic property is 30).
related to the inhibition of COX-2, whereas the inhibi- Anesthesia procedure
tion of COX-1 isoenzyme results in the gastrointestinal
Patients were interviewed preoperatively to explain
or kidney side effects [7]. This drug is a propionic acid
the study and introduced to the concept of the visual
derivative and the oral form has been widely used for
analog scale (VAS), with a 10-cm vertical score ranged
many years. By the introduction of ready-to-adminis-
from 0 = no pain to 10 = worst pain imaginable. The pa-
tration intravenous ibuprofen solution, it’s increasingly
tients fasted for both solids and clear liquids at least 8
been used in multimodal analgesia for the management
hours prior to the surgical procedure. No premedication
of postoperative pain [8]. It’s been shown that the use
was applied.
of intravenous (IV) ibuprofen is a safe and effective drug
to reduce the severity of pain, and opioid consumption On arrival to the preoperative care unit, IV access
in surgical interventions such as bariatric, orthopedic, was established with an 18-G IV cannula. The study
abdominal, and gynecologic surgeries [9-12]. The ef- group received 400 mg ibuprofen in 100 ml IV saline 15
fect of NSAIDs on wound healing is a debating issue min before anesthesia induction, whereas the placebo
and animal studies indicated that non-selective NSAIDs group received IV 100 ml saline only. The study drug and
generally inhibit wound healing. However, either COX- the saline were administered by an anesthesia nurse
1 or COX-2 selective NSAIDs tend to show no effect on blinded to the study.
wound healing [13]. Before induction of anesthesia, a bispectral index
The aim of this study was to investigate the effects sensor (BIS Quatro; Medtronic plc, Dublin, Republic of
of the preemptive administration of a single dose of IV Ireland) was placed on the patient’s forehead and con-
ibuprofen on the intraoperative hemodynamic param- nected to a BIS Vista monitor (Medtronic plc, Dublin,
eters, recovery characteristics, and postoperative pain Republic of Ireland). Following standard monitoring in-
management. The time to first analgesic requirement cluded a 3-lead electrocardiogram (ECG) with continu-
during postoperative period was the main goal of this ous ST-segment analysis, peripheral oxygen saturation
study. (SpO2), and non-invasive blood pressure, anesthesia in
Sezen et al. Int J Anesthetic Anesthesiol 2020, 7:118 • Page 2 of 7 •
DOI: 10.23937/2377-4630/1410118 ISSN: 2377-4630
both groups was established with IV 1 µg/kg fentanyl Statistical analysis
and 2-2.5 mg/kg propofol. Endotracheal intubation was
The demographic characteristics and collected data
facilitated by the administration of IV rocuronium 0.6
of the patients were entered into IBM® SPSS® (the Sta-
mg/kg. Anesthesia was maintained with sevoflurane of
tistical Package for the Social Sciences) Statistics version
2-3% in 50% oxygen-air mixture in a fresh gas flow of 2
23. Variables were characterized using mean, maximum
L/minute.
and minimum values, and percentage values were used
Hemodynamic goals were to maintain the intraoper- for qualitative variables. Normal distributions were
ative mean arterial pressure and heart rate within 20% reported as mean ± SD and Student's t-test was used
of the pre-induction values. If the mean arterial pres- for comparisons between groups. For the analysis of
sure and heart rate increased more than 20%, supple- qualitative variables Pearson chi-square test was used
mentary dose of 1 µcg/kg fentanil was applied. In case if the group was small, Fisher's exact test was used.
of decreasing more than 20%, 5 mg IV ephedrine was Nonparametric continuous variables were recorded as
administered. Sevoflurane was titrated to maintain a median and intermittent distribution and compared us-
BIS value between 40 and 60. ing Mann-Whitney U tests. In the comparison of both
groups in terms of VAS, two-way ANOVA test was used
Surgical procedure
for the change in time. p < 0.05 value was considered
Laparoscopic cholecystectomy was performed with statistically significant.
four-port standard technique by highly experienced
surgeons in laparoscopic interventions. After insertion Results
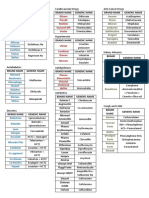
of a subumblical 10-mm port, pneumoperitoneum was Totally 60 patients were recruited into the study (Fig-
created by placing a Veress needle and the intraabdom- ure 1). Patients’ characteristics were shown in Table 1.
inal pressure was maintained at 10-12 mmHg. The op-
There was no difference between the groups in terms
eration table was positioned in reverse Trendelenburg
of hemodynamic findings before anesthesia induction
and sided to the left. A 10-mm trocar was placed in the
and in the peroperative period. However, BIS values
epigastrium to the right of the falciform ligament with
were found to be higher in Group I from the 20th minute
two additional 5-mm ports in the right upper abdomen.
to the pre-extubation period compared to Group C and
After resection of gallbladder, it was retrieved through
were statistically significant in this regard (Table 2).
the epigastric port. Nasogastric tube was used only for
decompression of the stomach and then removed. No Aldrete 0 minute scores were similar between
abdominal drainage was used to any patient. groups (7.4 ± 0.5 in Group I, and 7.2 ± 0.5 in Group C, p =
0.139). Aldrete 1st hour scores were 9 in all patients. The
At the end of the surgery, the anesthetic gas mixture
time until Aldrete score of 9 was statistically significant-
was replaced with 100% oxygen and the neuromuscular
ly shorter in Group I (Group I 3.8 ± 1.4 min, and Group C
block was reversed using a neostigmine (0.05 mg/kg)
6.3 ± 1.9 min, p < 0.001).
and atropine (0.01 mg/kg) combination. After adequate
ventilation, protective airway reflexes and the patients’ Sevoflurane consumption was lower in the group gi-
response to verbal commands were achieved, patients ven preemptive single dose IV ibuprofen, but the time
were extubated. Following transfer to the post-anes- to first postoperative analgesic requirement was longer
thesia care unit, they discharged to the general surgery (Table 3). When the total amount of analgesics used in
clinic when patients attained a modified Aldrete score the first postoperative 24 hours was compared, only 1g
of ≥ 9. i.v. paracetamol was sufficient for all patients in Group
I, whereas the control group required 1.7 ± 0.7g i.v. pa-
Data collection racetamol (p < 0.001). In addition, 100 mg i.v. tramadol
Patient characteristics of age, gender, height, weight, was administered to all patients in the control group as
and ASA physical status were recorded. Hemodynamic an additional analgesic.
parameters (non-invasive systolic (SAP), diastolic (DAP) When both groups were compared in terms of VAS
and mean (MAP) arterial pressure, heart rate (HR), scores, patients who were given preemptive single dose
bispectral index (BIS) values and SpO2 values were re- i.v. ibuprofen had significantly lower VAS scores (Table
corded before induction (baseline) and after induction, 4).
peroperative 10, 20, 30, minutes, before extubation.
Nausea and/or vomiting was not observed in any pa-
The time to achieve a modified Aldrete score of ≥ 9 tient.
was recorded as the recovery time. During postopera-
tive period, the time to first analgesic requirement and Discussion
the total amount of analgesics within 24 hours was re- The aim of this study was to evaluate the effect of
corded. Patients were asked to give a number between postoperative analgesic effectiveness of preemptive
from 1 to 5 for the satisfaction assessment for the anes- ibuprofen on peroperative hemodynamic parameters
thesia management. and recovery criteria in laparoscopic cholecystectomy.
Sezen et al. Int J Anesthetic Anesthesiol 2020, 7:118 • Page 3 of 7 •
DOI: 10.23937/2377-4630/1410118 ISSN: 2377-4630
Enrollment
Assessed for eligibility (n=60)
Excluded (n=0)
All patients completed the study
Randomized (n=60)
Allocation
Group Ibuprofen (n=30) Group Control (n=30)
Analysis
Analysed (n=30) Analysed (n=30)
Exclueded from anlaysis (n=0) Exclueded from analysis (n=0)
Figure 1: The CONSORT flowchart of the study.
Table 1: Patients characteristics.
Variables Group I Group C P value
Age (years) 1
45.5 ± 10.2 42.6 ± 9.6 0.208
Gender2 1.000
Female 16 (26.7%) 16 (26.7%)
Male 14 (23.3%) 14 (23.3%)
Weight (kg) 1
77.2 ± 14.0 71.2 ± 10.2 0.053
Height (cm)1 166.0 ± 8.4 167.5 ± 7.5 0.427
ASA physical status I/II2
10/20 16/14 0.118
Data was expressed as 1Mean ± Standard Deviation (SD); 2The number of patients (n) and the percentage (%). ASA: American
Society of Anesthesiologist’ kg: Kilograms; cm: Centimeters
As a result of the study, it was observed that the pre-op- severe pain c after laparoscopic cholecystectomy [14].
erative ibuprofen decreased peroperative sevoflurane For this reason, many analgesic drugs are applied to pa-
consumption, the time to first analgesic requirement. tients before, during or after surgery [15]. An effective
Besides, the time to recovery was shorter, and there postoperative analgesia results in early mobilization,
was a statistically significant decrease in VAS scores shortened hospital stay, and reduced costs. One meth-
compared to the control group. Also in the group given od for postoperative pain management is preemptive
ibuprofen, analgesic consumption was found to be less analgesia. This method represents analgesic administra-
in the postoperative period. tion before painful stimulation begins [16]. Local anes-
thetics such as bupivacaine, lidocaine and drugs such as
In the postoperative period, patients complain of
ibuprofen, gabapentin, pregabalin can be used [17].
Sezen et al. Int J Anesthetic Anesthesiol 2020, 7:118 • Page 4 of 7 •
DOI: 10.23937/2377-4630/1410118 ISSN: 2377-4630
Table 2: Hemodynamic parameters of the patients (mean ± SD).
Group I Group C p
Preoperative
SAB (mmHg) 142.3 ± 14.8 140.5 ± 14.0 0.589
DAB (mmHg) 84.5 ± 7.7 82.3 ± 9.2 0.304
MAP (mmHg) 107.0 ± 10.4 106.4 ± 14.2 0.525
HR (beats/minute) 83.7 ± 10.4 84.5 ± 12.6 0.734
SpO2% 99.1 ± 0.8 99.4 ± 0.8 0.072
BIS 96.6 ± 2.3 97.2 ± 1.4 0.388
After induction
SAB 124.5 ± 24.5 125.2 ± 20.0 0.706
DAB 76.0 ± 18.1 74.5 ± 18.0 0.663
MAP 94.4 ± 18.8 93.7 ± 18.9 0.929
HR 87.0 ± 13.7 88.9 ± 13.6 0.679
SpO2 99.6 ± 0.7 99.5 ± 0.8 0.224
BIS 33.2 ± 9.2 33.5 ± 8.2 0.766
Peroperative 10. minute
SAB 114.4 ± 17.1 112.9 ± 18.6 0.853
DAB 71.1 ± 17.4 70.7 ± 19.7 0.935
MAP 86.4 ± 16.9 87.0 ± 19.6 0.767
HR 81.9 ± 14.0 80.9 ± 19.5 0.953
SpO2 99.1 ± 0.9 99.0 ± 0.7 0.529
BIS 36.1 ± 8.9 34.3 ± 6.2 0.445
Peroperative 20. minute
SAB 117.8 ± 18.8 117.8 ± 19.1 0.773
DAB 74.5 ± 18.3 73.4 ± 17.8 0.790
MAP 90.0 ± 17.5 93.1 ± 19.4 0.554
HR 76.9 ± 12.8 78.4 ± 12.6 0.756
SpO2 99.1 ± 0.8 99.0 ± 0.7 0.918
BIS 40.7 ± 7.2 35.2 ± 8.4 0.019*
Peroperative 30. minute
SAB 130.3 ± 20.4 122.9 ± 19.2 0.164
DAB 80.7 ± 12.9 73.7 ± 13.3 0.067
MAP 97.0 ± 14.3 94.7 ± 15.6 0.336
HR 73.8 ± 10.3 76.6 ± 13.4 0.549
SpO2 99.2 ± 0.8 99.2 ± 0.6 0.974
BIS 43.8 ± 6.0 38.6 ± 7.2 0.009*
Before extubation
SAB 127.9 ± 16.8 124.0 ± 20.6 0.399
DAB 81.9 ± 14.5 72.4 ± 14.9 0.062
HR 75.6 ± 12.3 75.4 ± 13.0 0.801
SpO2 99.4 ± 0.6 99.3 ± 0.6 0.748
BIS 47.5 ± 9.3 40.0 ± 7.0 0.001*
*p < 0.001 statistically highly significant
Table 3: Consumption of the anesthesia drug and time to first analgesic requirement.
Group I Group C p
Sevoflurane consumption % 1
8.5 ± 3.1 20.1 ± 5.8 0.006*
The time to first analgesic requirement1 (hours) 19.4 ± 3.1 1.2 ± 0.4 0.001*
Mean ± Standard Deviation (SD); *p < 0.001 statistically highly significant.
1
Sezen et al. Int J Anesthetic Anesthesiol 2020, 7:118 • Page 5 of 7 •
DOI: 10.23937/2377-4630/1410118 ISSN: 2377-4630
Table 4: The comparison of VAS values between Group I, Group C.
VAS Group I Group C p
VAS 1 minute1 0.00 ± 0.00 3.06 ± 1.50 0.00*
VAS 1st hour1 0.43 ± 0.89 5.76 ± 1.79 0.00*
VAS 2nd hour1 0.53 ± 1.00 3.50 ± 1.83 0.00*
VAS 6th hour1 0.70 ± 1.11 4.96 ± 1.69 0.00*
VAS 12th hour1 1.20 ± 1.47 4.86 ± 1.67 0.00*
1
Mean ± Standard Deviation (SD); *p < 0.001 statistically highly significant.
VAS: Visual analog pain scale
To reduce postoperative opioid consumption, anal- There are some limitations for this study. First, ibu-
gesic and/or anti-inflammatory drugs and opioids are profen 400 mg was used as a single dose regardless of
used before and during surgery. Among these drugs patients' weight. Different results and a different side
most commonly paracetamol and ibuprofen with low effect profiles may have been obtained with a dose of
potential for side effects are used [8]. 800 mg. The second limitation is that the 400 mg dose
was used only before surgery and not after surgery. We
In a study evaluating the effect of ibuprofen on post-
aimed to evaluate the effectiveness of the preemptive
operative pain, 800 mg ibuprofen was found to reduce
dose. Third, the effect on the length of hospital stay has
postoperative opioid consumption [18]. In another
not been evaluated.
study, preemptive analgesia together with postopera-
tive primary care analgesic treatment has been shown In conclusion, preemptive single dose i.v. ibuprofen
to reduce opioid use more effectively [19]. (400 mg) reduced analgesic consumption in the first
24 hours postoperatively in patients undergoing lapa-
Gazal, et al. found lower VAS scores in their group
roscopic cholecystectomy. Preemptive single dose of
given ibuprofen and attributed this to anti-inflamma-
ibuprofen (400 mg) can be used in laparoscopic chole-
tory activity of the drug [20]. Moss, et al. showed that
cystectomy with the advantages of reducing the con-
single dose i.v. ibuprofen significantly reduced opioid
sumption of peroperative sevoflurane, providing better
consumption in the postoperative period in children un-
VAS scores, shortening the time to the first postopera-
dergoing tonsillectomy [21]. In our study, VAS scores,
tive analgesic requirement and reducing analgesic con-
postoperative analgesic need together with the time to
sumption.
first analgesic need of the group who were given pre-
emptive i.v. ibuprofen were comparatively lower. References
Southworth, et al. stated that ibuprofen is a good op- 1. Protic M, Veljkovic R, Bilchik AJ, Popovic A, Kresoja M, et
tion because of its analgesia and balanced anti-inflam- al. (2017) Prospective randomized controlled trial compa-
ring standard analgesia with combined intra-operative cy-
matory effect [22]. In another study, it was reported stic plate and port-site local anesthesia for post-operative
that preoperative i.v. ibuprofen reduces stress response pain management in elective laparoscopic cholecystec-
in laparoscopic cholecystectomies [23]. tomy. Surg Endosc 31: 704-713.
In their meta-analysis Moore, et al. emphasized that 2. Amornyotin S (2019) Anesthetic Management for Laparo-
scopic Cholecystectomy.
ibuprofen had a stronger analgesic effect compared to
ibuprofen and paracetamol. However, in their study, 3. Kaufman E, Epstein JB, Gorsky M, Jackson DL, Kadari A
(2005) Preemptive analgesia and local anesthesia as a
oral forms of drugs were used [24]. The i.v. form of ibu- supplement to general anesthesia: A review. Anesth Prog
profen has been evaluated in different studies as for 52: 29-38.
postoperative pain management. 4. Kissin I (2000) Preemptive analgesia. Anesthesiology 93:
In a study evaluating the effectiveness of i.v. ibupro- 1138-1143.
fen and paracetamol for postoperative pain manage- 5. Gupta A, Bah M (2016) NSAIDs in the Treatment of Posto-
ment in laparoscopic cholecystectomies, 800 mg i.v. perative Pain. Curr Pain Headache Rep 20: 62.
ibuprofen has been shown to result in lower pain scores 6. (2012) Practice guidelines for acute pain management in
and opioid consumption [25]. It has been reported that the perioperative setting: An updated report by the ame-
rican society of anesthesiologists task force on acute pain
i.v. ibuprofen is very safe and effective in patients who management. Anesthesiology 116: 248-273.
will undergo orthopedic surgery [26].
7. Rao P, Knaus EE (2008) Evolution of nonsteroidal anti-in-
In our study, we used a single dose of i.v. ibuprofen flammatory drugs (NSAIDs): Cyclooxygenase (COX) inhibi-
15 minutes before anesthesia induction. Our aim was tion and beyond. J Pharm Pharm Sci 11: S81-S110.
to reach peak plasma concentration at the beginning of 8. Koh W, Nguyen KP, Jahr JS (2015) Intravenous non-opioid
the surgical stimulus and to see fewer side effects with analgesia for peri-and postoperative pain management: A
scientific review of intravenous acetaminophen and ibupro-
a single dose of 400 mg.
fen. Korean J Anesthesiol 68: 3-12.
Sezen et al. Int J Anesthetic Anesthesiol 2020, 7:118 • Page 6 of 7 •
DOI: 10.23937/2377-4630/1410118 ISSN: 2377-4630
9. Gulay Erdogan Kayhana, Mukadder Sanlib, Ulku Ozgula, of intravenous ibuprofen 400 and 800 mg every 6 hours in
Ramazan Kirtekeb, Saim Yologluc (2018) Comparison of the management of postoperative pain. Clin Ther 31: 1922-
intravenous ibuprofen and acetaminophen for postoperati- 1935.
ve multimodal pain management in bariatric surgery: A ran-
19. Atkinson HC, Stanescu I, Frampton C, Salem II, Beasley
domized controlled trial. J Clin Anesth 50: 5-11.
CP, et al. (2015) Pharmacokinetics and bioavailability of a
10. De Peter KC, Blumberg SM, Dienstag Becker S, Meltzer JA fixed-dose combination of ibuprofen and paracetamol after
(2017) Does the use of ibuprofen in children with extremity intravenous and oral administration. Clin Drug Investig 35:
fractures increase their risk for bone healing complications? 625-632.
J Emerg Med 52: 426-432.
20. Gazal G, Al-Samadani KH (2017) Comparison of parace-
11. Gago Martínez A, Escontrela Rodriguez B, Planas Roca tamol, ibuprofen, and diclofenac potassium for pain relief
A, Martínez Ruiz A (2016) Intravenous Ibuprofen for Treat- following dental extractions and deep cavity preparations.
ment of Post-Operative Pain: A Multicenter, Double Blind, Saudi Med J 38: 284-291.
Placebo-Controlled, Randomized Clinical Trial. PLoS One
21. Moss JR, Watcha MF, Bendel LP, McCarthy DL, Witham
11: e0154004.
SL, et al. (2014) A multicenter, randomized, double-blind
12. Peter B Kroll, Laura Meadows, Amy Rock, Leo Pavliv placebo-controlled, single dose trial of the safety and effi-
(2011) A Multicenter, Randomized, Double-Blind, Place- cacy of intravenous ibuprofen for treatment of pain in pe-
bo-Controlled Trial of Intravenous Ibuprofen (IV-Ibuprofen) diatric patients undergoing tonsillectomy. Paediatr Anaesth
in the Management of Postoperative Pain Following Abdo- 24: 483-489.
minal Hysterectomy. Pain Pract 11: 23-32.
22. Southworth SR, Woodward EJ, Peng A, Rock AD (2015)
13. Hannah Zhao-Fleming, Audrey Hand, Kelly Zhang, Robert An integrated safety analysis of intravenous ibuprofen (Cal-
Polak, Armand Northcut, et al. (2018) Effect of non-steroi- dolor((R)) in adults. J Pain Res 8: 753-765.
dal anti-inflammatory drugs on post-surgical complications
23. Vanny Le, Lakshmi Kurnutala, Joseph Schianodi Cola,
against the backdrop of the opioid crisis. Burn Trauma 6:
Khaja Ahmed, Joel Yarmush, et al. (2016) Premedication
25.
with intravenous ibuprofen improves recovery characteristi-
14. Ahiskalioglu EO, Ahiskalioglu A, Aydin P, Yayik AM, Temiz cs and stress response in adults undergoing laparoscopic
A (2017) Effects of single-dose preemptive intravenous ibu- cholecystectomy: A randomized controlled trial. Pain Med
profen on postoperative opioid consumption and acute pain 17: 1163-1173.
after laparoscopic cholecystectomy. Medicine 96: e6200.
24. RA Moore, S Derry, PJ Wiffen, S Straube, DJ Aldington
15. Karim Saadati, Mohammad Reza Razavi, Daryoush Naze- (2015) Overview review: Comparative efficacy of oral ibu-
mi Salman, Shahrzad Izadi (2016) Postoperative pain relief profen and paracetamol (acetaminophen) across acute and
after laparoscopic cholecystectomy: Intraperitoneal sodium chronic pain conditions. Eur J Pain 19: 1213-1223.
bicarbonate versus normal saline. Gastroenterol Hepatol
25. Ekinci M, Çiftci B, Çelik EC, Köse EA, Karakaya MA, et
Bed Bench 9: 189-196.
al. (2020) A randomized, Placebo-controlled, double-blind
16. Kelly DJ, Ahmad M, Brull SJ (2001) Preemptive analgesia study that evaluates efficacy of intravenous ibuprofen and
I: Physiological pathways and pharmacological modalities. acetaminophen for postoperative pain treatment following
Can J Anaesth 48: 1000-1010. laparoscopic cholecystectomy surgery. J Gastrointest Surg
24: 780-785.
17. Argyro Fassoulaki, Konstantinos Patris, Costantine Sa-
rantopoulos, Quinn Hogan (2002) The analgesic effect of 26. Singla N, Rock A, Pavliv L (2010) A multicenter, randomi-
gabapentin and mexiletine after breast surgery for cancer. zed, double blind placebo controlled trial of intravenous ibu-
Anesth Analg 95: 985-991. profen (IV ibuprofen) for treatment of pain in postoperative
orthopedic adult patients. Pain Med 11: 1284-1293.
18. Southworth S, Peters J, Rock A, Pavliv L (2009) A mul-
ticenter, randomized, double-blind, placebo-controlled trial
Sezen et al. Int J Anesthetic Anesthesiol 2020, 7:118 • Page 7 of 7 •
You might also like
- EVALUATION OF THE INFLUENCE OF TWO DIFFERENT SYSTEMS OF ANALGESIA AND THE NASOGASTRIC TUBE ON THE INCIDENCE OF POSTOPERATIVE NAUSEA AND VOMITING IN CARDIAC SURGERYFrom EverandEVALUATION OF THE INFLUENCE OF TWO DIFFERENT SYSTEMS OF ANALGESIA AND THE NASOGASTRIC TUBE ON THE INCIDENCE OF POSTOPERATIVE NAUSEA AND VOMITING IN CARDIAC SURGERYNo ratings yet
- Top Trials in Gastroenterology & HepatologyFrom EverandTop Trials in Gastroenterology & HepatologyRating: 4.5 out of 5 stars4.5/5 (7)
- S 0042 1749386Document7 pagesS 0042 1749386wanggaNo ratings yet
- Dolor Postop, Ligamentos Cruzados, AmbulatorioDocument7 pagesDolor Postop, Ligamentos Cruzados, AmbulatorioChurrunchaNo ratings yet
- Kumar S.Document4 pagesKumar S.Van DaoNo ratings yet
- International Journal of Anesthetics and Anesthesiology Ijaa 7 112Document4 pagesInternational Journal of Anesthetics and Anesthesiology Ijaa 7 112mikoNo ratings yet
- PracticeJournal1 PutriMaharaniAndes 19-0010Document8 pagesPracticeJournal1 PutriMaharaniAndes 19-0010putri maharani andesNo ratings yet
- Analgesic Effects and Adverse Reactions of LidocaiDocument6 pagesAnalgesic Effects and Adverse Reactions of Lidocaibrendastevany23No ratings yet
- Priyanka New PPT Final 2-1Document49 pagesPriyanka New PPT Final 2-1sourabh jakharNo ratings yet
- 1 s2.0 S2468824X17300517 MainDocument5 pages1 s2.0 S2468824X17300517 MainFirah Triple'sNo ratings yet
- DR Surekha S Chavan, DR Stephan Jebaraj & DR Priya ChavreDocument10 pagesDR Surekha S Chavan, DR Stephan Jebaraj & DR Priya ChavreTJPRC PublicationsNo ratings yet
- Amalia 163216 - Journal ReadingDocument26 pagesAmalia 163216 - Journal ReadingGhifari FarandiNo ratings yet
- The Impact of Preemptive Perianal Anaesthetic Block in Open Haemorrhoidectomy - A Randomised Controlled TrialDocument3 pagesThe Impact of Preemptive Perianal Anaesthetic Block in Open Haemorrhoidectomy - A Randomised Controlled TrialhrtfdnbzvwNo ratings yet
- Randomized trial finds depth of anesthesia has no effect on postoperative painDocument6 pagesRandomized trial finds depth of anesthesia has no effect on postoperative painIntan PurnamasariNo ratings yet
- Research ArticleDocument10 pagesResearch ArticlethiaNo ratings yet
- Assessing Pain Relief Following Medical and Surgical Interventions For Lumbar Disc HerniationDocument4 pagesAssessing Pain Relief Following Medical and Surgical Interventions For Lumbar Disc HerniationInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Dr._Nataraj__EJCM-132-1888-1893-2023Document7 pagesDr._Nataraj__EJCM-132-1888-1893-2023vithz kNo ratings yet
- Journal Reading AnestesiDocument4 pagesJournal Reading AnestesiVania RNo ratings yet
- 2264-Article Text-5024-4-10-20151024Document6 pages2264-Article Text-5024-4-10-20151024shivamNo ratings yet
- Journal Homepage: - : Introduction:-ObjectiveDocument8 pagesJournal Homepage: - : Introduction:-ObjectiveIJAR JOURNALNo ratings yet
- Analgesia en Apendicitis AgudaDocument3 pagesAnalgesia en Apendicitis Agudasilvia barbosaNo ratings yet
- Ponv InternasionalDocument8 pagesPonv InternasionalRandi KhampaiNo ratings yet
- Coba 2Document6 pagesCoba 2Bianca CaterinalisendraNo ratings yet
- Auriculas AcupresurDocument6 pagesAuriculas AcupresurRahmania Kannesia DahuriNo ratings yet
- Effect Observation of Electro Acupunctute AnesthesiaDocument7 pagesEffect Observation of Electro Acupunctute Anesthesiaadink mochammadNo ratings yet
- Pain Management After Surgical Tonsillectomy: Is There A Favorable Analgesic?Document6 pagesPain Management After Surgical Tonsillectomy: Is There A Favorable Analgesic?Vladimir PutinNo ratings yet
- Effects of propofol versus sevoflurane anesthesia on postoperative pain after gastrectomyDocument33 pagesEffects of propofol versus sevoflurane anesthesia on postoperative pain after gastrectomyJuwita PratiwiNo ratings yet
- Impact of Intra-Operative Dexamethasone After Scheduled Cesarean Delivery: A Retrospective StudyDocument8 pagesImpact of Intra-Operative Dexamethasone After Scheduled Cesarean Delivery: A Retrospective StudyMiftah Furqon AuliaNo ratings yet
- Anesthesia & ClinicalDocument4 pagesAnesthesia & Clinicalreinhard fourayNo ratings yet
- The Routes of Administration For Acute Postoperative Pain MedicationDocument17 pagesThe Routes of Administration For Acute Postoperative Pain Medicationronald97hgNo ratings yet
- Journal Homepage: - : IntroductionDocument6 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- Journal of Clinical AnesthesiaDocument2 pagesJournal of Clinical AnesthesiatsalasaNo ratings yet
- 3 PBDocument7 pages3 PBDinda ArmeliaNo ratings yet
- Critical AppraisalDocument13 pagesCritical AppraisalRatna Widiyanti KNo ratings yet
- Comparison of Clonidine and Fentanyl As An Adjuvant To Bupivacaine in Unilateral Spinal AnaesthesiaDocument11 pagesComparison of Clonidine and Fentanyl As An Adjuvant To Bupivacaine in Unilateral Spinal AnaesthesiaYadin SabudiNo ratings yet
- JurnalDocument6 pagesJurnalDewi NurfadilahNo ratings yet
- Initial Experience Using Incisional Anesthetic Catheter in Abdominal Wall Ambulatory SurgeryDocument6 pagesInitial Experience Using Incisional Anesthetic Catheter in Abdominal Wall Ambulatory SurgeryilhamNo ratings yet
- The Effect of Perineural Dexamethasone On Rebound Pain After Ropivacaine Single-Injection Nerve Block: A Randomized Controlled TrialDocument10 pagesThe Effect of Perineural Dexamethasone On Rebound Pain After Ropivacaine Single-Injection Nerve Block: A Randomized Controlled TrialMichael Judika Deardo PurbaNo ratings yet
- Jurnal LaparatomyDocument12 pagesJurnal LaparatomyindahmartyasNo ratings yet
- Anesth Essays ResDocument8 pagesAnesth Essays ResFi NoNo ratings yet
- Effects of Intraoperative Epidural Anesthesia During Hepatectomy On Intraoperative and Post-Operative Patient OutcomesDocument8 pagesEffects of Intraoperative Epidural Anesthesia During Hepatectomy On Intraoperative and Post-Operative Patient OutcomesAfniNo ratings yet
- Trial Egistration: Running HeadDocument31 pagesTrial Egistration: Running Headnimas putriNo ratings yet
- Anes 10 3 9Document7 pagesAnes 10 3 9ema moralesNo ratings yet
- Multimodal Postoperative Analgesia: Combinations of Analgesics After Abdominal Surgery at Chu - Jra AntananarivoDocument11 pagesMultimodal Postoperative Analgesia: Combinations of Analgesics After Abdominal Surgery at Chu - Jra AntananarivoIJAR JOURNALNo ratings yet
- Efficacy Lidocaine Endoscopic Submucosal DissectionDocument7 pagesEfficacy Lidocaine Endoscopic Submucosal DissectionAnonymous lSWQIQNo ratings yet
- Randomized-Controlled Trial of Intravenous AcetaminophenDocument6 pagesRandomized-Controlled Trial of Intravenous Acetaminophenclara giovaniNo ratings yet
- 与扑热息痛联用增效Document5 pages与扑热息痛联用增效zhuangemrysNo ratings yet
- Relationship Between The Incidence and Risk Factors of Postoperative Nausea and Vomiting in Patients With Intravenous Patient-Controlled AnalgesiaDocument6 pagesRelationship Between The Incidence and Risk Factors of Postoperative Nausea and Vomiting in Patients With Intravenous Patient-Controlled AnalgesiaRandi KhampaiNo ratings yet
- To Evaluate The Efficacy of Ultrasonography Guided Pectoral Nerve Block For Postoperative Analgesia in Breast SurgeriesDocument4 pagesTo Evaluate The Efficacy of Ultrasonography Guided Pectoral Nerve Block For Postoperative Analgesia in Breast SurgeriesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Revista Brasileira DE AnestesiologiaDocument9 pagesRevista Brasileira DE AnestesiologiayulianiNo ratings yet
- Spinal vs. General Anesthesia For Percutaneous Nephrolithotomy: A Prospective Randomized TrialDocument5 pagesSpinal vs. General Anesthesia For Percutaneous Nephrolithotomy: A Prospective Randomized TrialDella Puspita SariNo ratings yet
- Pain Management in Enhanced Recovery After Surgery (ERAS) ProtocolsDocument8 pagesPain Management in Enhanced Recovery After Surgery (ERAS) ProtocolsbokobokobokanNo ratings yet
- Original Contribution: Abd-Elazeem Elbakry, Wesam-Eldin Sultan, Ezzeldin IbrahimDocument6 pagesOriginal Contribution: Abd-Elazeem Elbakry, Wesam-Eldin Sultan, Ezzeldin IbrahimWALTER GARCÍA TERCERONo ratings yet
- Effect of Anxiolytic Dose On Incidence of Intraoperative Nausea and Vomiting in CS Under Spinal AnesthesiaDocument8 pagesEffect of Anxiolytic Dose On Incidence of Intraoperative Nausea and Vomiting in CS Under Spinal AnesthesiaCentral Asian StudiesNo ratings yet
- Aroma 1Document8 pagesAroma 1bazediNo ratings yet
- A Change in Practice From Epidural To Intrathecal Morphine For Hepato Bilio SurgDocument7 pagesA Change in Practice From Epidural To Intrathecal Morphine For Hepato Bilio Surgvalerio.messinaNo ratings yet
- Protocol oDocument8 pagesProtocol oCynthia ChávezNo ratings yet
- Comparison of Analgesic Effects of Intravenous Nalbuphine and Pentazocine in Patients Posted For Short-Duration Surgeries A Prospective Randomized Double-Blinded StudyDocument4 pagesComparison of Analgesic Effects of Intravenous Nalbuphine and Pentazocine in Patients Posted For Short-Duration Surgeries A Prospective Randomized Double-Blinded StudyMuhammad AtifNo ratings yet
- JAnaesthClinPharmacol371114-28986 000449Document5 pagesJAnaesthClinPharmacol371114-28986 000449Ferdy RahadiyanNo ratings yet
- DwefgnmjDocument8 pagesDwefgnmjfabian arassiNo ratings yet
- JAnaesthClinPharmacol371108-277131 000437Document6 pagesJAnaesthClinPharmacol371108-277131 000437Ferdy RahadiyanNo ratings yet
- JAnaesthClinPharmacol371114-28986 000449Document5 pagesJAnaesthClinPharmacol371114-28986 000449Ferdy RahadiyanNo ratings yet
- Perioperative Management For Cesarean Section in COVID 19 PatientsDocument4 pagesPerioperative Management For Cesarean Section in COVID 19 PatientsFerdy RahadiyanNo ratings yet
- JAnaesthClinPharmacol37163-254754 000414Document4 pagesJAnaesthClinPharmacol37163-254754 000414Ferdy RahadiyanNo ratings yet
- Sepsis para AnestesiologoDocument8 pagesSepsis para AnestesiologoJose ManuelNo ratings yet
- 1471 2253 14 39 PDFDocument8 pages1471 2253 14 39 PDFHannyNo ratings yet
- Journal of Clinical AnesthesiaDocument8 pagesJournal of Clinical AnesthesiaFerdy RahadiyanNo ratings yet
- Plant Cyanogenic Glycosides: An Overview: Review ArticleDocument6 pagesPlant Cyanogenic Glycosides: An Overview: Review ArticleVinz AlvarezNo ratings yet
- Single High Dose Vitamin DDocument8 pagesSingle High Dose Vitamin DFerdy RahadiyanNo ratings yet
- Anesthetics and Anesthesiology: Effect of Opioid-Free Anaesthesia On Perioperative Period: A ReviewDocument11 pagesAnesthetics and Anesthesiology: Effect of Opioid-Free Anaesthesia On Perioperative Period: A Reviewveranisa suciaNo ratings yet
- Vit D JournalDocument10 pagesVit D JournalFerdy RahadiyanNo ratings yet
- The Link Between Vitamin D and COVID-19: Distinguishing Facts From FictionDocument3 pagesThe Link Between Vitamin D and COVID-19: Distinguishing Facts From FictionFerdy RahadiyanNo ratings yet
- A Plasmid Is A Small DNA Molecule Within A Cell That Is Physically Separated From A Chromosomal DNA and Can Replicate IndependentlyDocument5 pagesA Plasmid Is A Small DNA Molecule Within A Cell That Is Physically Separated From A Chromosomal DNA and Can Replicate Independentlyyaqoob008No ratings yet
- 2ND Periodical Test in Science 6 With Tos KeyDocument9 pages2ND Periodical Test in Science 6 With Tos KeyJumaliza Francisco Paguirigan67% (3)
- RFID Chip will Poison Me and Kill me if I Disobey. Microchip Implants - RFID Brain Chip : Crime, Malpratice, Mindcontrol, Sexual Abuse, Brain Abuse, Torture Abuse, Medical Abuse, and The Silent Killers via RFID Brain ChipDocument3 pagesRFID Chip will Poison Me and Kill me if I Disobey. Microchip Implants - RFID Brain Chip : Crime, Malpratice, Mindcontrol, Sexual Abuse, Brain Abuse, Torture Abuse, Medical Abuse, and The Silent Killers via RFID Brain ChipJohanNo ratings yet
- Blood Gas AnalysisDocument28 pagesBlood Gas AnalysiskempolonNo ratings yet
- Probiotics and Preterm Infants A Position Paper.26 ShareDocument17 pagesProbiotics and Preterm Infants A Position Paper.26 Shareendy tovarNo ratings yet
- Problems faced by construction workers in Tamil NaduDocument3 pagesProblems faced by construction workers in Tamil NaduYamini HarshaNo ratings yet
- Anembryonic Pregnancy/ Gestation (O02.0)Document137 pagesAnembryonic Pregnancy/ Gestation (O02.0)Marvin Mark AbamongaNo ratings yet
- Malnutrition e BD 12Document51 pagesMalnutrition e BD 12dr.vichiayorinaNo ratings yet
- Dispensing DrugsDocument1 pageDispensing DrugsIan CalalangNo ratings yet
- Jib Achha Applied Preventive Vet MedicineDocument2 pagesJib Achha Applied Preventive Vet MedicineAweke EngdaworkNo ratings yet
- Crisis of Hypertension Revised 1Document57 pagesCrisis of Hypertension Revised 1keenmunir100% (4)
- Emma Sarbit, EPSE405 WILK, Assignment 1 Watching A MovieDocument5 pagesEmma Sarbit, EPSE405 WILK, Assignment 1 Watching A Movieesarbit1No ratings yet
- Umbilical Cord CareDocument3 pagesUmbilical Cord CareHui Li TehNo ratings yet
- Pernicious Oral Habits-1 PDFDocument35 pagesPernicious Oral Habits-1 PDFWen Shu GohNo ratings yet
- Growel Dairy Farming ManualDocument52 pagesGrowel Dairy Farming ManualGrowel Agrovet Private Limited.No ratings yet
- Test Bank For Medical Parasitology A Self Instructional Text 6th Edition Chapters 2 8 LeventhalDocument18 pagesTest Bank For Medical Parasitology A Self Instructional Text 6th Edition Chapters 2 8 LeventhalSabina Moskowitz100% (36)
- Xi Cleft (Accumulation Point) : DiagnosisDocument4 pagesXi Cleft (Accumulation Point) : DiagnosisZareen FNo ratings yet
- The Diagnostic Criteria For Chronic EndometritisDocument7 pagesThe Diagnostic Criteria For Chronic EndometritisyuriescaidaNo ratings yet
- English For Science and Technology - Paper 2Document11 pagesEnglish For Science and Technology - Paper 2Alaister Bernard JampongNo ratings yet
- Key Acupoints PDFDocument6 pagesKey Acupoints PDFthouartu50% (2)
- Dichotomous KeyDocument4 pagesDichotomous KeyJojee ErraNo ratings yet
- Cabbage & CauliflowerDocument19 pagesCabbage & CauliflowerramNo ratings yet
- Community As Partner - Chapter 2Document2 pagesCommunity As Partner - Chapter 2KTNo ratings yet
- Why Do We Dream Thesis StatementDocument8 pagesWhy Do We Dream Thesis Statementgbx272pg100% (2)
- Government College of Nursing Jodhpur: Procedure On-Cordocentesis Subject-Obstetrics & Gynecology Specialty-IDocument4 pagesGovernment College of Nursing Jodhpur: Procedure On-Cordocentesis Subject-Obstetrics & Gynecology Specialty-Ipriyanka100% (2)
- Fundamentals of NursingDocument16 pagesFundamentals of Nursingsorilla_franceschelNo ratings yet
- AdhdDocument7 pagesAdhdAnca CzifraNo ratings yet
- Correlation Between Systemic Risk Factors and Diabetic Macular Edema in Diabetes Mellitus - Dian Paramitasari 1Document8 pagesCorrelation Between Systemic Risk Factors and Diabetic Macular Edema in Diabetes Mellitus - Dian Paramitasari 1Hutami Sri UmmiyatiNo ratings yet
- A Student Manual of Clinical Skills 13 7 8Document194 pagesA Student Manual of Clinical Skills 13 7 8mofath100% (5)
- Expanding Designed Exercise Awareness and Produced by Gregory Petrovich GrabovoiDocument5 pagesExpanding Designed Exercise Awareness and Produced by Gregory Petrovich GrabovoiManojkumar NairNo ratings yet