Professional Documents
Culture Documents
Neonatal Lab Interpretation
Uploaded by
Widelmark FarrelOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Neonatal Lab Interpretation
Uploaded by
Widelmark FarrelCopyright:
Available Formats
Neonatal Laboratory Interpretation
Linda J. Juretschke, PhD, RNC-NPT, APN/NNP-BC, CCNS
Founder/President, NICU Solutions, Inc.
Neonatal Nurse Practitioner
The Ronald McDonald Children’s Hospital at Loyola University Medical Center
Objectives
At the end of this lecture, the participant will be able to:
1. identify appropriate laboratory tests for patient care,
2. describe normal laboratory values in the newborn period, and
3. formulate a plan of care for infants undergoing laboratory data monitoring.
I. Introduction
A variety of laboratory tests are done in the neonatal period on a routine basis, many as point-of-
care testing. Nurses often are the first health care providers to view the results of these tests.
Therefore, an understanding of the various blood tests obtained in the neonatal period, along with
the ability to interpret the clinical significance of these results is imperative in the provision of
care.
II. Blood Tests Commonly Drawn in the Newborn Period
Blood Glucose
CBC with Differential
Acute Phase Reactants/C-Reactive Protein
Blood Cultures
Blood Type and Rh
Coombs Test
Blood Gases
Bilirubin
Electrolytes/Calcium/Magnesium
III. Blood Sampling Sites
Heel Stick
o Appropriate Heel Stick Sites
Venipuncture
o Venipuncture Technique
Arterial Puncture
o Modified Allen's Test
© 2017 NICU Solutions, Inc.
http://www.nicusolutions.com
IV. Clinical Laboratory Tests
A. Blood Glucose
Primary fuel source for the developing brain
Accounts for more than 90% of total body oxygen consumption in early
fasting
Infants have a greater glucose requirement than adults because of their larger
brain-to-body size ratio
While all organs need glucose, the brain exclusively uses glucose for energy
The liver plays a role in glucose homeostasis by mobilizing glucose stored
within hepatocytes as glycogen and/or by converting lactate, glycerol, and
amino acids into glucose (this is known as gluconeogenesis)
In the newborn, hepatic (liver) glucose production rates are
~ 6 mg/kg/minute (3 to 6 times greater than in the adult)
Normal blood glucose levels in a term newborn:
o 0 - 24 hours: > 35 mg/dL
o > 24 hours: > 45 mg/dL
o Many now use 50 mg/dL as the cutoff value
Hypoglycemia:
o If glucose production does not meet glucose requirements, plasma glucose
concentration falls, and this eventually leads to brain energy shortage due
to hypoglycemia
o Babies most at risk for hypoglycemia include:
Infant of a diabetic mother (IDM); due to too much insulin production
Small for gestational age (SGA) babies; due to poor glycogen stores
Premature babies (< 37 weeks); due to poor glycogen stores, immature
hepatic function, decreased intake
o Other causes of Hypoglycemia
Inborn errors of metabolism
Increased glucose utilization
Altered hormone regulation
Severe hemolytic disease
Asphyxia
Cold stress
Sepsis
Liver disease
Some birth defects
© 2017 NICU Solutions, Inc.
http://www.nicusolutions.com
o Symptoms of Hypoglycemia
Apnea
Tremors/jitteriness
Sweating
Hypothermia
Lethargy
Abnormal cry
Poor feeding
Poor tone
Tachypnea/respiratory distress
Tachycardia
Cyanosis
Seizures
o Treatment for Hypoglycemia
D10W at 2 mL/kg slow IV Push
May also use glucagon (converts glycogen to blood sugar)
If otherwise healthy, might just feed and recheck
Important to follow unit protocols strictly; especially with checking
and documenting follow-up levels
B. Complete Blood Count (CBC) with Differential
Indications for obtaining a CBC:
o Check for anemia (low RBC count)
o Look for thrombocytopenia (TCP; low platelet count)
o Evaluate for sepsis
Measures:
o Red blood cells (RBCs) (Erythrocytes)
Needed to carry oxygen to the tissues
o White blood cells (WBCs) (Leukocytes)
Fight infection and invasion by foreign materials
o Hemoglobin (Hgb)
Iron-containing protein in the RBCs that carries oxygen; also carries
carbon dioxide and nitric oxide
o Hematocrit (Hct)
Percentage of red blood cells in the full volume of blood
o Platelets (Plts) (Thrombocytes)
Help with clotting
Also a natural source of growth factors
The differential measures all WBC types:
Granulocytes (Neutrophils, Basophils, Eosinophils)
Agranulocytes (Lymphocytes, Monocytes, Macrophages)
© 2017 NICU Solutions, Inc.
http://www.nicusolutions.com
Total WBC Count
No established norms
5,000 to 30,000 mm3 as a general guide
♦ Preterm: 6,000 – 19,000 mm
3
♦ Term: 10,000 – 26,000 mm
3
Limited value in diagnosing infection
Very low WBC counts may be more concerning than high WBC counts
Differential (Granulocytes, Monocytes, Lymphocytes)
Granulocytes
st
♦ Neutrophils: 70% during 1 few weeks, then lymphocytes
predominate
Primary defense against bacteria; often seen during acute bacterial
infection
Go to the inflamed area and engulf the organism (phagocytosis)
It takes the body ~ 13 – 15 days to release a mature neutrophil; a “left
shift” follows the development of a neutrophil:
Myeloblast
Promyelocyte
Myelocyte
Metamyelocyte
Band
Segmented Neutrophil
To calculate the Immature/Total (I/T) Neutrophil Ratio:
Add up all the immatures and divide by the total
Example: Neutrophils = 35% Segs
15% Bands
3% Metas
53%
Immature Neutrophils (bands + metas + myelos)
All Neutrophils (segs + bands + metas + myelos)
15 (bands) + 3 (metas) _
35 (segs) + 15 (bands) + 3 (metas)
18
53 = 0.34
♦ < 0.2 is normal
♦ > 0.2 – 0.25 may be suggestive of infection
♦ > 0.8 carries a higher risk of death
© 2017 NICU Solutions, Inc.
http://www.nicusolutions.com
To calculate absolute neutrophil count (ANC) (cells/mm3):
Multiply WBC by all neutrophil percentages
Example: WBC = 10,000
Neutrophils = 35% Segs
15% Bands
3% Metas
53%
10,000 x 0.53 = 5,300
0 – 24 hours: > 2,000
After 24 hours: > 7,000
A count < 1500 is suggestive of infection
(Sources vary; some say < 2000; some say < 1000)
♦ Eosinophils: 1% – 3%
Seen with allergic response, parasitic infections
♦ Basophils: < 1%
Seen with allergic response; during healing phase of inflammation
Monocytes: 4% – 8%
2nd line of defense against bacterial infections
engulf invaders and destroy with powerful enzymes
seen in response to viral and chronic bacterial infections
Lymphocytes: 30%; increases to 60% in 1st few weeks
Increased with viral infections
Provide cellular (T cells) and humoral (B cells = antibiotics) immunity
IgG – crosses the placenta, protects babies in the 1st months, major
immunoglobulin – about 75%
IgM – about 10%, early antibody, produced by fetus in response to
intrauterine infection
IgA – about 20%, predominantly seen in mucous/saliva, secretions,
passed in human milk
IgD – < 1% - unknown function
IgE – trace, exact function unknown
© 2017 NICU Solutions, Inc.
http://www.nicusolutions.com
Platelets
Help with clotting
Mostly stored in the bone marrow, liver, and spleen
150,000 – 450,000 mm3 (same as adult values)
On day 3 – 5, may be only > 80,000 mm3
Non-specific, late sign of infection
May be decreased with fungal infections
C. Acute Phase Reactants: C-Reactive Protein (CRP)
Measures the amount of protein in the blood, signaling acute inflammation
CRP is one of the first serum acute phase reactants to rise in response to sepsis
Generally returns to normal within 2 – 7 days of successful treatment
A persistent rise may indicate a persistent infection; may also indicate
meningitis
Used by many to help monitor therapy and determine the length of antibiotic
treatment
D. Blood Cultures
Obtained when evaluating for sepsis
Drawn using venipuncture or arterial puncture technique
Minimum of 1 mL blood should be collected
Gram Stain
Divides organisms into 2 main groups: Gram Positive or Gram Negative
Identifies the shape of the organism: Rods or Coccus
Classifies the organism so antibiotic therapy can be started
Gram + Cocci in Pairs: Strep or Staph
Gram + Cocci in Chains: Strep
Gram + Cocci in Clusters: Staph
Gram – Club-shaped rods: E. Coli
Gram – Diploid: Neisseria
Timeline
By day 1 → early, preliminary report of culture
Will be read at specific intervals: 24, 48, 72 hours; with a final report on day
5 – 14 (depending on the lab)
Once the organism is identified, sensitivity testing is done
The organism is tested against certain antibiotics to see which one will
effectively inhibit it
© 2017 NICU Solutions, Inc.
http://www.nicusolutions.com
Sensitivities
Minimum Inhibitory Concentration (MIC):
The least amount of antibiotic needed to inhibit bacterial growth
E. Blood Type and Rh
Four Major Blood Types:
o A, B, O, AB
o A and B are most common
Rh Factor (Rh+, Rh-)
o Refers to the D antigen (just 1 of 50 blood antigens)
o Antigens are what trigger antibodies by the immune system
Rh Incompatibility
o Rh- mother, Rh+ fetus
o Fetus’ blood enters the mother’s circulation
o The mother’s immune system treats the Rh+ fetal cells as if they were a
foreign substance and makes antibodies against them
o These anti-Rh antibodies may cross the placenta into the developing fetus,
where they destroy the fetus’ circulating red blood cells
o Leads to anemia, release of bilirubin, and jaundice in the newborn
F. Coombs Test
Includes both the indirect Coombs and the direct Coombs
The indirect Coombs is used to screen pregnant women for antibodies that
may cause hemolytic disease of the newborn (such as in the case of ABO or
Rh incompatibility)
The direct Coombs looks for autoimmune hemolytic anemia
G. Blood Gases
Normal function of all body cells depends on a narrow range of biochemical
balance
Acids (H+ Ions) are the byproducts of the metabolism of proteins, fats, and
glucose and are constantly released into the body
Measurement of free Hydrogen Ions is expressed in terms of pH
pH is the negative logarithm of the hydrogen ion concentration, therefore the
hydrogen concentration determines the pH of blood
The more Hydrogen Ions in a solution, the lower the pH (the more acid the
solution)
The fewer Hydrogen Ions in a solution, the higher the pH (the more alkalotic
the solution)
© 2017 NICU Solutions, Inc.
http://www.nicusolutions.com
Hydrogen is carried in the form of:
Carbonic Acid (H2CO3)
Fixed Acids
o Sulfuric Acid
o Lactic Acid
o Pyruvic Acid
o Phosphoric Acid
o Ketoacids
Normal pH
o Neutral: 7.0
o Normal is 7.35 – 7.45
o Acidosis: < 7.35
o Alkalosis: > 7.45
Gas exchange
o Refers to the exchange of oxygen and carbon dioxide between air and
blood and then blood and tissue
o The exchange of oxygen is reflected in the PaO2 (partial pressure of
oxygen) in arterial blood
o The exchange of PaCO2 (partial pressure of carbon dioxide) is a direct
reflection of the adequacy of alveolar ventilation
o Factors affecting gas exchange might include:
Blood flow
Cardiac output
Metabolic rate
Diffusion
Shunting
Gas concentration of inspired air
Oxygen Diffusion and Transport
o Through breathing, oxygen is transferred from the atmosphere to the
lungs, and carbon dioxide is transferred from the lungs to the atmosphere
o Oxygen diffuses into the blood in the pulmonary capillaries and is carried
throughout the body and diffuses from systemic capillary blood into the
interstitial fluid and cells
o Fetal Hemoglobin (HgbF)
HgbF has a greater affinity for oxygen, meaning that the blood is
better saturated at lower PaO2s
This allows the transfer of oxygen from the mother’s blood, which
contains adult Hgb (HgbA), and therefore a lower affinity for oxygen
The healthy term newborn replaces its HgbF with HgbA by about 6
months of age
o Hypoxemia
Decrease in the amount of oxygen in the arterial blood which may be
due to a decrease in FIO2, alveolar hypoventilation, diffusion
impairment, anatomic shunts, and ventilation/perfusion (V/Q)
mismatch
© 2017 NICU Solutions, Inc.
http://www.nicusolutions.com
o Hypoxia
Decrease in the amount of oxygen available to the tissues; four
categories:
o Hypoxemic hypoxia
o Anemic hypoxia
o Circulatory hypoxia
o Histologic hypoxia
Carbon Dioxide Transport
o Carbon dioxide diffuses from the cells through the interstitial fluid to the
blood in systemic capillaries, and to the lungs where it diffuses into
alveolar gas
Normal Blood Gas Values
o pH: 7.35 – 7.45
↓ pH = acidosis
↑ pH = alkalosis
o PaCO2: 35 – 45 mmHg
↑ PaCO2 = respiratory acidosis
The baby is not breathing effectively enough; needs to blow off
more CO2
Need to help the baby breathe (ventilate)
↓ PaCO2 = respiratory alkalosis
The baby is breathing too hard or too fast (labored breathing;
tachypnea)
Need to calm the baby down, slow down his breathing, wean
ventilator support
o PaO2: 50 – 80 mmHg (term)
o PaO2 : 45 – 65 mmHg (preterm)
o HCO3-: 22 – 26 mEq/L
Bicarb is a buffer that keeps the blood in a normal acid-base balance
In newborns, we often see low bicarb due to renal immaturity (they are
peeing out their bicarb)
Usually will resolve in a few days when renal function improves
↑ HCO3- = metabolic alkalosis
↓ HCO3- = metabolic acidosis
o Base Deficit/Excess: -2 – +2 mEq/L
Base excess (a positive number) indicates too much buffer (metabolic
alkalosis)
Base deficit (a negative number) indicates too little buffer (metabolic
acidosis)
o O2 Saturation: 92% – 94%
© 2017 NICU Solutions, Inc.
http://www.nicusolutions.com
Metabolic Acidosis
Occurs when a disorder adds acid to the body or causes alkali to be lost faster than
the buffer system, lungs or kidneys can regulate the load. Characterized by:
pH
normal CO2
HCO3-
Causes of Metabolic Acidosis
Diarrhea Lactic Acidosis
Small bowel drainage Tissue Hypoxia
Hyperalimentation Sepsis
Ingestion of Chloride- Neonatal Cold Stress
containing compounds Ketoacidosis
Renal Tubular Acidosis Diabetes Mellitus
Renal Failure Starvation
Carbonic Anhydrase Ingestion of Toxins
Deficiency Inborn Errors of Metabolism
Metabolic Alkalosis
Occurs whenever acid is excessively lost or alkali is excessively retained.
Characterized by:
pH
normal CO2
HCO3-
Causes of Metabolic Alkalosis
Vomiting Bartter’s Syndrome
Nasogastric Suctioning Sodium Bicarbonate Use
Congenital Chloride-Wasting Hypokalemia
Diarrhea Hypochloremia
Dehydration Chewing Tobacco
Diuretic Therapy Massive Blood Transfusion
Steroid Therapy Cystic Fibrosis Infants Fed
Cushing’s Syndrome Regular Formula or BM
© 2017 NICU Solutions, Inc.
http://www.nicusolutions.com
Respiratory Acidosis
Occurs when CO2 is not adequately removed by the lungs. Characterized by:
pH
CO2
normal HCO3-
Causes of Respiratory Acidosis
Lung Disease Impaired Lung Motion
Upper Airway Obstruction Pleural Effusion
Small Airway Obstruction Pneumothorax
Chronic Obstructive Disease Thoracic Cage Abnormalities
Pneumonia Apnea
Pulmonary Edema Neurologic or Neuromuscular
RDS, ARDS Disorders Affecting
Aspiration Respiration
Pulmonary Hypoplasia
Respiratory Alkalosis
Occurs when CO2 is excreted by the lungs in excess of its production.
Characterized by:
pH
CO2
normal HCO3-
Causes of Respiratory Alkalosis
Anxiety Central Nervous Syndrome
Fever Disorders
Sepsis Liver Failure
Hypoxemia Reye’s Syndrome
Pneumonia Hyperthyroidism
Atelectasis Salicylate Poisoning
Pulmonary Emboli Mechanical Ventilation
Congestive Heart Failure
Asthma
© 2017 NICU Solutions, Inc.
http://www.nicusolutions.com
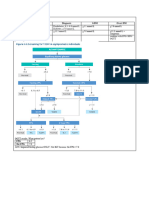
Blood Gas Practice Examples
© 2017 NICU Solutions, Inc.
http://www.nicusolutions.com
H. Bilirubin
Normal breakdown product of red blood cells
Produced from the catabolism of heme-containing proteins
Hemoglobin accounts for 70% – 80% of bilirubin production
Higher in infants due to a higher turnover and shorter lifespan of RBCs
Two different forms:
o Unconjugated (indirect); Lipid Soluble
o Conjugated (direct); Water Soluble
The body can only eliminate the conjugated form, so the liver needs to convert
it first
Bilirubin Metabolism and Excretion
In utero, unconjugated fetal bilirubin is transported across the placenta and
excreted by the maternal circulation
After birth, the newborn liver must metabolize bilirubin, however, it can only
excrete conjugated bilirubin, and therefore must first convert the unconjugated
form to the conjugated form (phototherapy works by changing bilirubin to the
water soluble, or conjugated form)
Once conjugated, the bilirubin is passed through the intestines where it is
converted into urobilinogen by bacterial enzymes, then excreted
A carrier molecule (albumin) is needed to transport bilirubin to the liver
If the rate bilirubin production exceeds the liver’s ability to conjugate and
eliminate it, or if albumin binding sites are saturated or scarce, unconjugated
bilirubin will rise and jaundice will develop
I. Sodium
Normal is 135 – 145 mEq/L
Helps conduct neuromuscular impulses
Maintains intravascular osmolality
Regulates acid-base balance (NaCl-, NaHCO3-)
If abnormal, can cause seizures, venous sinus thrombosis, CNS hemorrhage
Abnormalities can be life threatening, especially if:
o < 120 mEq/L
o > 155 mEq/L
Hyponatremia
o Can be dilutional (too much fluid)
o Can be due to too little intake
o Can be due to renal losses
Renal immaturity, polyuria, diuretic therapy
o Can be due to GI losses
Vomiting, diarrhea
© 2017 NICU Solutions, Inc.
http://www.nicusolutions.com
Hypernatremia
o Can be due to excessive intake, sodium bicarb or saline administration
o Can be due to dehydration
Urinary losses
GI losses
Evaporation through the skin
J. Potassium
Normal is 3.5 – 5.5 mEq/L
Responsible for cardiac and skeletal muscle contraction
Helps maintain acid-base balance
Needed for all cell functions to take place
If abnormal, can cause weakness, arrhythmias/EKG changes, death
Hypokalemia
Can be due to too little intake
Can be due to renal losses
o Renal immaturity, polyuria, diuretic therapy
Can be due to GI losses
Vomiting, diarrhea
Hyperkalemia
o Can be due to excessive intake, blood cell hemolysis, excessive bruising,
acidosis, multiple blood transfusions
K. Chloride
Normal is 96 – 111 mmoL/L
Works with Na+ to maintain acid/base balance, transmit nerve impulses, and
regulate fluid in and out of cells
L. Calcium
Most abundant mineral in the human body
Needed for bone mineralization
99% of total Ca++ is contained in bone—this is true for all ages
The Ca++ we are measuring in serum represents just 1% of the total body Ca++
Because dietary intake is decreased in the first few days, serum concentration
decreases in the first day of life
In term infants, ICa++ reaches its nadir of 1.10 – 1.36 mmol/L at ~ 24 hours of
age; ~ 30% will develop “early” hypocalcemia (within the first 2 days of life)
For term infants, hypocalcemia is defined as:
++
♦ ICa < 1.10 mmol/L or
++
♦ Total serum Ca < 8.0 mg/dL
In preterm infants, hypocalcemia is defined as:
++
♦ ICa < 1 mmol/L or
++
♦ Total serum Ca < 7.0 mg/dL
© 2017 NICU Solutions, Inc.
http://www.nicusolutions.com
Usually temporary and will improve in 1 – 3 days due to:
Ca++ intake in feedings
Renal P excretion
Improved parathyroid function
Hypercalcemia
o Total Ca++ > 10.8 mg/dL
o Can be asymptomatic or cause nonspecific signs including:
Poor feeding
Constipation
Polyuria
Dehydration
muscle tone
Lethargy
Bradycardia
o If prolonged, can lead to metastatic calcifications; primarily
nephrocalcinosis (kidney stones)
M. Phosphorus
Normal is 5 – 7.8 mg/dL
Needed for bone mineralization, erythrocyte function, cell metabolism and the
generation and storage of energy
~ 85% of the total P is in skeleton
The remaining 15% is found in soft tissues and extracellular fluid
~ 2/3 is organic (phospholipids); the remainder is inorganic
Inorganic is what we are measuring
85% is ionized
5% is complexed
10% is protein bound
Serum concentration varies widely and is dependent on intake and renal
excretion
Levels are low at birth, but rise rapidly after birth
Higher levels are seen in formula fed babies than in breast fed babies
An inverse relationship between serum ICa++ and serum P exists
N. Magnesium
Normal is 1.6 – 2.8 mg/dL
Distributed primarily in bone and muscle
Needed for energy production, cell membrane function, and protein synthesis
~ 1% of body Mg++ is in the extracellular fluid
Hypomagnesemia
o Mg++ < 1.6 mg/dL
o Usually asymptomatic until < 1.2 mg/dL
© 2017 NICU Solutions, Inc.
http://www.nicusolutions.com
o Signs/Symptoms:
Irritability
Tremors
Seizures
o Hypomagnesemia is frequently seen with hypocalcemia
Need to correct the hypomagnesemia in order to correct the
hypocalcemia
Hypermagnesemia
o Mg++ > 2.8 mg/dL
o Often due to excessive Mg++ administration
o Generally will return to normal after a few days
o Treatment:
Hydration
+/- Diuretics
© 2017 NICU Solutions, Inc.
http://www.nicusolutions.com
References
Arnon S, & Litmanovitz I (2008). Diagnostic tests in neonatal sepsis. Current Opinions
in Infectious Disease. 21(3): 223-227.
Blackburn, ST (2012). Maternal, Fetal, and Neonatal Physiology: A Clinical
Perspective (4th ed.). St. Louis: W.B.Saunders.
Browning, R (2002). CBC 101: blood count basics. Nursing Spectrum 15 (7IL): 24-26.
Farmand, M (2009). Blood gas analysis and the fundamentals of acid-base balance.
Neonatal Network 28(2): 125-128.
Fusch, C, & Jochum, F (2005). Water, sodium, potassium and chloride. In RC Tsang, R
Uauy, B Koletzko, & SH Zlotkin (Eds.) Nutrition of the Preterm Infant: Scientific Basis and
Practical Guidelines (2nd ed.), pp. 201-244. Cincinnati: Digital Educational Publishing, Inc.
Gardner, SL (Ed.) (2010). Merenstein & Gardner's Handbook of Neonatal Intensive Care
th
(7 ed.). St. Louis: Mosby.
Gunderson, LP, & Kenner, C (Eds.) (1995). Care of the 24 – 25 Week
Gestational Age Infant: A Small Baby Protocol. Petaluma, CA: NICU Ink.
Hawk, M (2008). C-reactive protein in neonatal sepsis. Neonatal Network 27(2): 117-20.
Hazinski, M (2012). Nursing Care of the Critically Ill Child (3rd ed.). Chicago, IL:
Mosby Year Book.
Ishibashi, M (2002). C-reactive protein kinetics in newborns: application of a high-
sensitivity analytic method in its determination. Clinical Chemistry 48: 1103-1106.
Kenner, C, & Lott, JW (2013). Comprehensive Neonatal Care: An Interdisciplinary
Approach (5th ed.). Philadelphia, PA: WB Saunders Company.
Lorenz, JM (1997). Assessing fluid and electrolyte status in the newborn. Clinical
Chemistry 43(1): 205-210.
Lorenz, JM, Kleinman, LI, Ahmed, G, & Markarian, K (1995). Phases of fluid and
electrolyte homeostasis in the extremely low birth weight infant. Pediatrics 96(3): 484-489
Lorenz, JM, Kleinman, LI, & Markarian, K (1997). Potassium metabolism in extremely
low birth weight infants in the first week of life. Journal of Pediatrics 131(1): 81-86.
Manroe, BL et al (1979). The neonatal blood count in health and disease. Part 1:
reference values for neutrophilic cells. Journal of Pediatrics 95 (1): 89-98.
© 2017 NICU Solutions, Inc.
http://www.nicusolutions.com
Martin, RJ, Fanaroff, AA, & Walsh, MC (Eds.) (2011). Fanaroff and Martin's Neonatal-
Perinatal Medicine: Diseases of the Fetus and Infant (9th ed.). St. Louis: Elsevier.
Pohlandt, F, Abrams, S, & Cooke, R (2005). Calcium, magnesium, phosphorus and
vitamin D. In RC Tsang, R Uauy, B Koletzko, & SH Zlotkin (Eds.) Nutrition of the Preterm
Infant: Scientific Basis and Practical Guidelines (2nd ed.), pp. 245-275. Cincinnati: Digital
Educational Publishing, Inc.
© 2017 NICU Solutions, Inc.
http://www.nicusolutions.com
You might also like
- Neonatal Nurse Practitioner A Complete Guide - 2020 EditionFrom EverandNeonatal Nurse Practitioner A Complete Guide - 2020 EditionNo ratings yet
- 1513 PDFDocument397 pages1513 PDFlider68No ratings yet
- Pediatric Cardiology and Pulmonology: A Practically Painless ReviewFrom EverandPediatric Cardiology and Pulmonology: A Practically Painless ReviewNo ratings yet
- Electronic Fetal MonitoringDocument20 pagesElectronic Fetal MonitoringEagles171100% (2)
- LOW RISK NEONATAL NURSING: Passbooks Study GuideFrom EverandLOW RISK NEONATAL NURSING: Passbooks Study GuideNo ratings yet
- Central Vascular Access - 2019 PDFDocument14 pagesCentral Vascular Access - 2019 PDFSoutrik SeThNo ratings yet
- Quick Hits for Pediatric Emergency MedicineFrom EverandQuick Hits for Pediatric Emergency MedicineCristina M. Zeretzke-BienNo ratings yet
- Neonatal Care Protocols for Hospital PhysiciansDocument648 pagesNeonatal Care Protocols for Hospital PhysiciansИван Мельник100% (1)
- NEONATAL NURSE PRACTITIONER: Passbooks Study GuideFrom EverandNEONATAL NURSE PRACTITIONER: Passbooks Study GuideNo ratings yet
- ACoRN Acute Care of At-Risk Newborns A Resource and Learning Tool For Health Care Professionals 2nd EditionDocument473 pagesACoRN Acute Care of At-Risk Newborns A Resource and Learning Tool For Health Care Professionals 2nd EditionGerardo FernandezNo ratings yet
- Fetal Distress: BY: Buenafe, Drexler Justine ADocument24 pagesFetal Distress: BY: Buenafe, Drexler Justine AFaye Dianne Damian-BuenafeNo ratings yet
- How to Survive the NICU: Tips for Mothers of Premature Babies in HospitalFrom EverandHow to Survive the NICU: Tips for Mothers of Premature Babies in HospitalRating: 3 out of 5 stars3/5 (1)
- 2017 Pcep Specialized Newborn Care 4 PDFDocument171 pages2017 Pcep Specialized Newborn Care 4 PDFmagnumforce 007No ratings yet
- Fanconi Anemia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandFanconi Anemia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Kansas Pediatric Scenario GuidebookDocument82 pagesKansas Pediatric Scenario GuidebookSarah-kate PatersonNo ratings yet
- NEONATAL INTENSIVE CARE NURSING: Passbooks Study GuideFrom EverandNEONATAL INTENSIVE CARE NURSING: Passbooks Study GuideNo ratings yet
- Newborn Assessment Period: ST THDocument3 pagesNewborn Assessment Period: ST THYoussef AliNo ratings yet
- Reference Range Values For Pediatric CareDocument177 pagesReference Range Values For Pediatric CareTrish Santosidad100% (1)
- BronchiolitisDocument51 pagesBronchiolitisBranaghNo ratings yet
- Neonatal Guidelines 2019-2021Document407 pagesNeonatal Guidelines 2019-2021YUDY LORENA GIRALDO ALFONSONo ratings yet
- Routine Newborn Assessment PDFDocument17 pagesRoutine Newborn Assessment PDFYanna RizkiaNo ratings yet
- Newborn and Infant Physical Exam (NIPE) GuidelineDocument37 pagesNewborn and Infant Physical Exam (NIPE) GuidelineClara CarneiroNo ratings yet
- Bronchiolitis in Infants and Children - Clinical Features and DiagnosisDocument23 pagesBronchiolitis in Infants and Children - Clinical Features and Diagnosisjorgego95No ratings yet
- Vygon: Basic ManualDocument71 pagesVygon: Basic ManualRakhmawati WeniNo ratings yet
- Paeds Handbook Class2021 1568487638Document30 pagesPaeds Handbook Class2021 1568487638kafosidNo ratings yet
- Mac Peds Survival GuideDocument206 pagesMac Peds Survival GuideKatheryn100% (1)
- PDF - VeinsDocument3 pagesPDF - VeinsjulialeoNo ratings yet
- Common Diseases of NewbornDocument162 pagesCommon Diseases of NewbornMichelle ThereseNo ratings yet
- Fetal Strip Review-Contraction ChartDocument82 pagesFetal Strip Review-Contraction Chartsanthanalakshmi100% (1)
- Neonatology AllDocument22 pagesNeonatology AllDebadutta dashNo ratings yet
- NRP Baby Saver III June 2011Document24 pagesNRP Baby Saver III June 2011nursesedNo ratings yet
- Neonatal Ventilator Vent Set-Up CheatsheetDocument1 pageNeonatal Ventilator Vent Set-Up CheatsheetRick Frea50% (2)
- Persistent Pulmonary Hypertension in Newborn: By: Dr. Abhay Kumar Moderator: Dr. Akhilesh KumarDocument31 pagesPersistent Pulmonary Hypertension in Newborn: By: Dr. Abhay Kumar Moderator: Dr. Akhilesh KumarAbhay BarnwalNo ratings yet
- 32-Week OB CheckDocument4 pages32-Week OB CheckG. Crusor-PriceNo ratings yet
- EV Neonatal JaundiceDocument24 pagesEV Neonatal JaundiceAlkrenaweeSrurNo ratings yet
- Pocketbook WHO PediatricsDocument398 pagesPocketbook WHO PediatricsNashria RusdhyNo ratings yet
- Cardiovascular: SystemDocument18 pagesCardiovascular: Systemkelsey jacksonNo ratings yet
- OB NRSNG - Com BrainsheetsDocument4 pagesOB NRSNG - Com BrainsheetsD SchwartzlerNo ratings yet
- Psychiatric Nursing ConceptsDocument28 pagesPsychiatric Nursing ConceptsCai Velasco Decena100% (1)
- Acute Respiratory Infeciton (ARI)Document19 pagesAcute Respiratory Infeciton (ARI)Haryo Prakoso Adhi PNo ratings yet
- K7 - Supraventricular Tachycardia (SVT)Document44 pagesK7 - Supraventricular Tachycardia (SVT)Zikri Putra Lan LubisNo ratings yet
- 1642 CompressedDocument246 pages1642 CompressedJasonZambranoRojasNo ratings yet
- Neonatal EmergenciesDocument123 pagesNeonatal EmergenciesMaria Babette Almazan Talavera100% (2)
- Neonatal CareDocument59 pagesNeonatal Careconsultorio la cardeneraNo ratings yet
- Electronic Fetal MonitoringDocument4 pagesElectronic Fetal MonitoringMauZungNo ratings yet
- Newborn Care Hnadbook by 2019 ClassDocument267 pagesNewborn Care Hnadbook by 2019 Classknowledge chanall chanallNo ratings yet
- Enuresis in Children - A Case - Based ApproachDocument9 pagesEnuresis in Children - A Case - Based ApproachBogdan NeamtuNo ratings yet
- PAT - Remick Spring CE 2014Document50 pagesPAT - Remick Spring CE 2014Nadar RizatullahNo ratings yet
- Neonatal SubgalealDocument6 pagesNeonatal SubgalealIrenLayNo ratings yet
- The Kids Are Alright Pediatric Trauma PearlsDocument21 pagesThe Kids Are Alright Pediatric Trauma PearlsDaniel Torres CutivaNo ratings yet
- Care of The Normal Newborn: M. Rogers-Walker, MSN/Ed, RNDocument28 pagesCare of The Normal Newborn: M. Rogers-Walker, MSN/Ed, RNyanetp01No ratings yet
- Newborn Care Free Online EditionDocument452 pagesNewborn Care Free Online EditionMayeso E. ChikwalikwaliNo ratings yet
- Newborn AssessmentDocument5 pagesNewborn Assessmentlanilyn aquinoNo ratings yet
- Family Medicine 33: 28-Year-Old Female With Dizziness: Learning ObjectivesDocument6 pagesFamily Medicine 33: 28-Year-Old Female With Dizziness: Learning ObjectivesAndrea Kristin OrigenesNo ratings yet
- Pediatric Assessment TriangleDocument31 pagesPediatric Assessment TriangleblairNo ratings yet
- AirCare Pediatric Reference GuideDocument8 pagesAirCare Pediatric Reference GuideN/ANo ratings yet
- PEDIA 4.1 NephrologyDocument7 pagesPEDIA 4.1 NephrologyAngela CaguitlaNo ratings yet
- Manual of Ambulatory PediatricsDocument624 pagesManual of Ambulatory PediatricsArvin E. PamatianNo ratings yet
- Mood Disorders: Advanced Practice Education AssociatesDocument11 pagesMood Disorders: Advanced Practice Education AssociatesAndrea100% (1)
- Ventricular Septal DefectDocument8 pagesVentricular Septal DefectWidelmark FarrelNo ratings yet
- Normal Flora of the Respiratory TractDocument6 pagesNormal Flora of the Respiratory TractWidelmark FarrelNo ratings yet
- Tugas Individu-Case 3: Widelmark Farrel Y S - 130110180176Document4 pagesTugas Individu-Case 3: Widelmark Farrel Y S - 130110180176Widelmark FarrelNo ratings yet
- Tugas Tutorial Case 5&6 - IndividuDocument13 pagesTugas Tutorial Case 5&6 - IndividuWidelmark FarrelNo ratings yet
- Tugas Individu-Case 2: Widelmark Farrel Y S - 130110180176Document5 pagesTugas Individu-Case 2: Widelmark Farrel Y S - 130110180176Widelmark FarrelNo ratings yet
- Case 4 FM - Post StrokeDocument168 pagesCase 4 FM - Post StrokeWidelmark FarrelNo ratings yet
- Tetralogy of FallotDocument7 pagesTetralogy of FallotWidelmark FarrelNo ratings yet
- Tugas Individu-Case 1: Widelmark Farrel Y S - 130110180176Document4 pagesTugas Individu-Case 1: Widelmark Farrel Y S - 130110180176Widelmark FarrelNo ratings yet
- Atrial Septal DefectDocument8 pagesAtrial Septal DefectWidelmark FarrelNo ratings yet
- Embryology of HeartDocument6 pagesEmbryology of HeartWidelmark FarrelNo ratings yet
- BHP PHOP CRP Case 5Document9 pagesBHP PHOP CRP Case 5Widelmark FarrelNo ratings yet
- Anatomy of Male GenitaliaDocument24 pagesAnatomy of Male GenitaliaWidelmark FarrelNo ratings yet
- Histology of UreterDocument1 pageHistology of UreterWidelmark FarrelNo ratings yet
- High-Risk Pregnancy: The Internet Journal of Gynecology and ObstetricsDocument16 pagesHigh-Risk Pregnancy: The Internet Journal of Gynecology and ObstetricsWidelmark FarrelNo ratings yet
- Width of The QRS Complex: - Wide VT, SVT With Aberrant Conduction - Narrrow SVTDocument11 pagesWidth of The QRS Complex: - Wide VT, SVT With Aberrant Conduction - Narrrow SVTWidelmark FarrelNo ratings yet
- Nutition in PregnancyDocument11 pagesNutition in PregnancyWidelmark FarrelNo ratings yet
- Embryo 21-29 Weeks: 0the Main Factors That, Status, and Daily Energ y IntakeDocument8 pagesEmbryo 21-29 Weeks: 0the Main Factors That, Status, and Daily Energ y IntakeWidelmark FarrelNo ratings yet
- The Mental Status ExaminationDocument16 pagesThe Mental Status Examinationeloisa.abcedeNo ratings yet
- Chronic PCMDocument29 pagesChronic PCMNur NajminaNo ratings yet
- Clarendonz QN Bank Final pdf-1 PDFDocument69 pagesClarendonz QN Bank Final pdf-1 PDFMayank Jain100% (6)
- PEDIA - Acquired Heart DiseaseDocument5 pagesPEDIA - Acquired Heart DiseaseStephen Pilar PortilloNo ratings yet
- Alcoholic KetoacidosisDocument19 pagesAlcoholic KetoacidosisPraveenya NunnaNo ratings yet
- Urine Analysis FinalDocument112 pagesUrine Analysis FinalNischita JayarajNo ratings yet
- Atheroma - Wikipedia, The Free EncyclopediaDocument9 pagesAtheroma - Wikipedia, The Free EncyclopediaBhadresh MangukiyaNo ratings yet
- 1-Anatomy of The Female Genital OrgansDocument83 pages1-Anatomy of The Female Genital OrganssahrNo ratings yet
- PDF Mcqs in Forensic Medicine and Toxicology 6e by ReddpdfDocument41 pagesPDF Mcqs in Forensic Medicine and Toxicology 6e by ReddpdfIhtisham aliNo ratings yet
- اسئلة الهيئة السعودية- تمريضDocument39 pagesاسئلة الهيئة السعودية- تمريضlolo trabNo ratings yet
- Gastroentrology LastDocument48 pagesGastroentrology LastAbdallah K. RamadanNo ratings yet
- Case Conference: Mrs - Kudasih, 47 Y.o, CM: C 927936Document18 pagesCase Conference: Mrs - Kudasih, 47 Y.o, CM: C 927936bayuNo ratings yet
- Correlation Between Hba1c Level and Epicardial Fat Thickness in Acute Coronary Syndrome PatientDocument5 pagesCorrelation Between Hba1c Level and Epicardial Fat Thickness in Acute Coronary Syndrome PatientIJAR JOURNALNo ratings yet
- Pharma ExamDocument5 pagesPharma ExamMclavin LoveNo ratings yet
- Revision Notes in Anaesthesia and ICUDocument69 pagesRevision Notes in Anaesthesia and ICUlim sjNo ratings yet
- Marfella NEJM 2024Document11 pagesMarfella NEJM 2024tristan_raoultNo ratings yet
- Drug Class Brand or Label Name Generic Name Strength Dosage Form Limits Generic Available? (Y / N)Document4 pagesDrug Class Brand or Label Name Generic Name Strength Dosage Form Limits Generic Available? (Y / N)Al MozahidNo ratings yet
- Acute Appendicitis and PeritonitisDocument8 pagesAcute Appendicitis and PeritonitisYosuaNo ratings yet
- Clinical ECG RoundsDocument2 pagesClinical ECG RoundsKai Siang ChanNo ratings yet
- RosuvastatinDocument2 pagesRosuvastatinShaira Richelle OmagapNo ratings yet
- C P P C P P: Ardiology Atient AGE Ardiology Atient AGEDocument3 pagesC P P C P P: Ardiology Atient AGE Ardiology Atient AGEBBA MaryamNo ratings yet
- Clinical Questions of Combined Liver Kidney TransplantationDocument46 pagesClinical Questions of Combined Liver Kidney TransplantationHermann HernandezNo ratings yet
- Úlcera Arterial e VenosaDocument8 pagesÚlcera Arterial e VenosaRaianna SoaresNo ratings yet
- ECG QuestionsDocument2 pagesECG QuestionsSidd Sharma71% (7)
- Egan's Fundamentals of Respiratory Care Chapter 31 Test BankDocument13 pagesEgan's Fundamentals of Respiratory Care Chapter 31 Test BankZahra Margrette SchuckNo ratings yet
- Muscle and MovementDocument5 pagesMuscle and MovementRabiaNo ratings yet
- Textbook of Veterinary Internal Medicine, 8th Edition-4693-4728 (1) - 1-18Document19 pagesTextbook of Veterinary Internal Medicine, 8th Edition-4693-4728 (1) - 1-18Kevin Andres Trujillo CastroNo ratings yet
- Anatomy of The CVSDocument6 pagesAnatomy of The CVSMercyNo ratings yet
- Guideline For HPT Audit 2019, v1.1 15Document1 pageGuideline For HPT Audit 2019, v1.1 15siti nur aishah jalilNo ratings yet
- Tintinalli Shock PDFDocument13 pagesTintinalli Shock PDFfueny8gmailNo ratings yet
- The Urinary System: Anatomy, Physiology and Common DiseasesDocument8 pagesThe Urinary System: Anatomy, Physiology and Common DiseasesMelany LtrNo ratings yet
- Is That a Fact?: Frauds, Quacks, and the Real Science of Everyday LifeFrom EverandIs That a Fact?: Frauds, Quacks, and the Real Science of Everyday LifeRating: 4.5 out of 5 stars4.5/5 (3)
- Periodic Tales: A Cultural History of the Elements, from Arsenic to ZincFrom EverandPeriodic Tales: A Cultural History of the Elements, from Arsenic to ZincRating: 3.5 out of 5 stars3.5/5 (137)
- The Disappearing Spoon: And Other True Tales of Madness, Love, and the History of the World from the Periodic Table of the ElementsFrom EverandThe Disappearing Spoon: And Other True Tales of Madness, Love, and the History of the World from the Periodic Table of the ElementsRating: 4 out of 5 stars4/5 (146)
- Coating and Drying Defects: Troubleshooting Operating ProblemsFrom EverandCoating and Drying Defects: Troubleshooting Operating ProblemsRating: 5 out of 5 stars5/5 (1)
- Essential Oil Chemistry Formulating Essential Oil Blends that Heal - Aldehyde - Ketone - Lactone: Healing with Essential OilFrom EverandEssential Oil Chemistry Formulating Essential Oil Blends that Heal - Aldehyde - Ketone - Lactone: Healing with Essential OilRating: 5 out of 5 stars5/5 (1)
- Guidelines for Asset Integrity ManagementFrom EverandGuidelines for Asset Integrity ManagementRating: 5 out of 5 stars5/5 (1)
- Organic Chemistry for Schools: Advanced Level and Senior High SchoolFrom EverandOrganic Chemistry for Schools: Advanced Level and Senior High SchoolNo ratings yet
- Meltdown: Nuclear disaster and the human cost of going criticalFrom EverandMeltdown: Nuclear disaster and the human cost of going criticalRating: 5 out of 5 stars5/5 (5)
- An Introduction to the Periodic Table of Elements : Chemistry Textbook Grade 8 | Children's Chemistry BooksFrom EverandAn Introduction to the Periodic Table of Elements : Chemistry Textbook Grade 8 | Children's Chemistry BooksRating: 5 out of 5 stars5/5 (1)
- The Periodic Table of Elements - Post-Transition Metals, Metalloids and Nonmetals | Children's Chemistry BookFrom EverandThe Periodic Table of Elements - Post-Transition Metals, Metalloids and Nonmetals | Children's Chemistry BookNo ratings yet
- Chemistry at Home - A Collection of Experiments and Formulas for the Chemistry EnthusiastFrom EverandChemistry at Home - A Collection of Experiments and Formulas for the Chemistry EnthusiastNo ratings yet
- The Regenerative Grower's Guide to Garden Amendments: Using Locally Sourced Materials to Make Mineral and Biological Extracts and FermentsFrom EverandThe Regenerative Grower's Guide to Garden Amendments: Using Locally Sourced Materials to Make Mineral and Biological Extracts and FermentsRating: 5 out of 5 stars5/5 (3)
- Chemistry: a QuickStudy Laminated Reference GuideFrom EverandChemistry: a QuickStudy Laminated Reference GuideRating: 5 out of 5 stars5/5 (1)
- The Elements We Live By: How Iron Helps Us Breathe, Potassium Lets Us See, and Other Surprising Superpowers of the Periodic TableFrom EverandThe Elements We Live By: How Iron Helps Us Breathe, Potassium Lets Us See, and Other Surprising Superpowers of the Periodic TableRating: 3.5 out of 5 stars3.5/5 (22)
- The Periodic Table: A Very Short IntroductionFrom EverandThe Periodic Table: A Very Short IntroductionRating: 4.5 out of 5 stars4.5/5 (3)
- Science Goes Viral: Captivating Accounts of Science in Everyday LifeFrom EverandScience Goes Viral: Captivating Accounts of Science in Everyday LifeRating: 5 out of 5 stars5/5 (1)
- Stuff Matters: Exploring the Marvelous Materials That Shape Our Man-Made WorldFrom EverandStuff Matters: Exploring the Marvelous Materials That Shape Our Man-Made WorldRating: 4 out of 5 stars4/5 (289)
- Chemistry for Breakfast: The Amazing Science of Everyday LifeFrom EverandChemistry for Breakfast: The Amazing Science of Everyday LifeRating: 4.5 out of 5 stars4.5/5 (14)
- Gas-Liquid And Liquid-Liquid SeparatorsFrom EverandGas-Liquid And Liquid-Liquid SeparatorsRating: 3.5 out of 5 stars3.5/5 (3)
- Monkeys, Myths, and Molecules: Separating Fact from Fiction in the Science of Everyday LifeFrom EverandMonkeys, Myths, and Molecules: Separating Fact from Fiction in the Science of Everyday LifeRating: 4 out of 5 stars4/5 (9)
- Taste: Surprising Stories and Science About Why Food Tastes GoodFrom EverandTaste: Surprising Stories and Science About Why Food Tastes GoodRating: 3 out of 5 stars3/5 (20)