Professional Documents
Culture Documents
Adult Fallot Mortality in Indonesia
Uploaded by
Luqman AlwiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Adult Fallot Mortality in Indonesia
Uploaded by
Luqman AlwiCopyright:
Available Formats
Jurnal
Kardiologi Indonesia
J Kardiol Ind 2007; 28:197-202
Penelitian Klinik ISSN 0126/3773
Surgical Risk for Adult with Tetralogy of Fallot
Karina V. Wilamarta, Dicky Fakhri, Jusuf Rachmat
Background. The beneficiaries of successful pediatric cardiac surgery and
cardiology increases surgical treatment in the adult population with
congenital heart disease. Adults patient with Tetralogy of Fallot (TOF) will
need surgery either reoperative, palliative or more commonly reparative
by the time they come. Many of them face the prospect of further
operations, arrhythmias, complications and if managed inappropriately will
increase risk of heart failure and premature death. This study presents the
early surgical results of adult TOF.
Methods and results. Data were reviewed retrospectively related to the
hospital course of TOF adult patients (age > 17 years) from June 1, 1998
to December 30, 2006 who require surgical treatment in National Cardiac
Center - Harapan Kita, Indonesia. Most of the operations were corrective
procedures (20 patients, 66.7%), followed by palliative procedures (6
patients, 20%), and reoperations (4 patients, 13.3%). Mean age at surgery
was 20.87+5.49 years. There were no hospital mortality in the primary
corrective group, one death (16.7) in the palliative group related to poor
left ventricular function, and one death (25%) in the reoperation group
related to perioperative bleeding. Follow up data of 11.73+17.68 months
duration were available in 28 of 30 patients (93%) who were discharged
Pediatric Cardiovascular and home. Overall survival probability is higher for corrective procedures than
Congenital Heart Disease Surgery palliative and reoperative procedures.
Unit National Cardiovascular Conclusions. Surgical treatment of TOF in adult patients proved quite
Center, Jakarta, Indonesia. save and beneficial
(J Kardiol Ind 2007;28:197-202)
Keywords: Adult Tetralogy of Fallot, palliative procedures, corrective procedures,
reoperations.
Jurnal Kardiologi Indonesia • Vol. 28, No. 3 • Mei 2007 197
Jurnal
Kardiologi Indonesia
J Kardiol Ind 2007; 28:197-202
ISSN 0126/3773 Clinical Research
Risiko Bedah pada Pasien Dewasa
dengan Tetralogi Fallot
Karina V. Wilamarta, Dicky Fakhri, Jusuf Rachmat
Latar Belakang. Keberhasilan bedah jantung anak telah membawa manfaat besar bagi populasi dewasa dengan penyakit
jatung bawaan. Pasien dewasa dengan Tetralogi Fallot (TF) akan memerlukan tindakan bedah, mungkin reoperasi, bedah
paliatif atau yang paling sering bedah reparatif/korektif. Bila tidak ditangani dengan baik, kebanyakan pasien ini akan menghadapi
masalah bedah berulang, aritmia, gagal jantung dan kematian dini. Penelitian ini mempresentasikan hasil dini bedah pada
pasien dewasa dengan TF.
Metode dan hasil. Data rekam medis pasien dewasa dengan TF (usia 17 tahun atau lebih) yang menjalani pembedahan di
Pusat jantung Nasional – Harapan Kita, Jakarta, Indonesia dalam periode 1 Juni 1998 sampai dengan 30 Desember 2006
dipelajari secara retrospektif. Sebagian terbesar telah dilakukan bedah korektif (20 pasien, 68%), diikuti dengan bedah paliatif
(6 pasien, 20%), dan reoperasi (4 pasien, 13.3%). Usia rerata saat bedah adalah 20.87+5.49 tahun. Tak ada kematian pada
kelompok bedah korektif primer. Satu kematian terjadi pada 6 kasus yang menjalani bedah paliatif (16.7%), dan satu kematian
(25%) terjadi pada 4 kasus yang menjalani reoperasi pasca bedah paliatif sebelumnya. Data evaluasi lebih lanjut didapat dari
28 pasien (93%) yang diikuti selama periode rerata 11.73+17.68 bulan. Probabilitas survival keseluruhan lebih tinggi pada
kelompok bedah korektif dibanding kelompok paliatif dan reoperasi.
Kesimpulan. Pembedahan pada pasien dewasa dengan TF terbukti aman dan bermanfaat.
Kata Kunci: Tetralogi Fallot dewasa, bedah paliatif, bedah korektif, reoperasi.
The number of patients with adult congenital heart surgery, arrhythmia, heart failure and - if managed
disease (ACHD) is expected to increase during this inappropriately – of premature death.2,3
decade.1 Surgery for ACHD as a result of primary repair Surgery for Tetralogy of Fallot (TOF) as a benchmark
of CHD within the pediatric age group is still of cyanotic type congenital cardiac surgery has been chosen
challenging. Although the outlook for patients with to be analyzed. Adult patients with TOF will have had
CHD has been transformed, most early interventions surgery either reoperative, palliative or more commonly
have not been curative. It is estimated that approximately reparative by the time they come. The objective of this
50% of ACHD patients face the prospect of further study is to present the early surgical results of patients who
require surgery for TOF in the adult population.
Alamat korespondensi: Material and Methods
dr. Karina V. Wilamarta
Unit Bedah Jantung Anak dan Penyakit Jantung Bawaan
Pusat Jantung Nasional, Jakarta, Indonesia
We reviewed the medical records of adult patients (aged
17 years or older) who underwent cardiac operations at
198 Jurnal Kardiologi Indonesia • Vol. 28, No. 3 • Mei 2007
Wilamarta K.V. et al: Surgical Risk for Adult with Tetralogy of Fallot
the National Cardiovascular Centre - Harapan Kita anomalies were found in 4 patients. Preoperative
Hospital, Jakarta-indonesia, from June 1, 1998, through diagnosis was achieved by echocardiography and
December 31, 2006. cardiac catheterization.
Cardiac rhythm, preoperative risk factors, extracardiac According to preoperative clinical evaluation, 28
anomalies, and postoperative complications were patients belonged to New York Heart Association
identified as risk factors. For analysis, surgical procedures (NYHA) class I-II, 2 in NYHA class III. Sinus rhythm in
were divided into three categories, including the following: 20 of 30 patients (67%) was revealed in electro-
(1) palliative procedures; (2) corrective procedures; and cardiogram. Arrhythmia were present in the remaining
(3) reoperations. Palliative procedures include all 10 patients and including Right Bundle Branch Block
operations performed to improve the patient’s clinical (RBBB) 7 patients, Ventricular Extra Systole (VES) 3
status. Corrective procedures are operations employed to patients, sinus bradycardia 1 patient. Preoperative variables
achieve an anatomical or physiologic correction with which are commonly associated to an increase hospital
separation of the pulmonary from systemic circulation. morbidity and mortality were identified in 7 patients,
Results are presented as mean and standard deviation being multiple in 2 patients. Preoperative arrhythmia and
(median and range were used if data were not normally preoperative NYHA class III-IV were the only causes
distributed). Comparisons of continuous variables were linked to increasing hospital mortality.
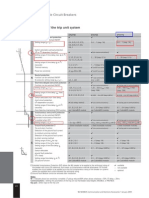
performed by Welch,s t-test. P value greater than 0.05 Major postoperative complications occurred in 10
means that difference between groups is not statistically patients (30%). Seven patients presented multiple
significant. To assess if there was a statistical significance complications (Table 1). Pulmonary insufficiency and
between groups, data were analyzed with analysis of right ventricular dysfunction were measured by
variance. Multiple comparison test was further employed echocardiography following intracardiac repair, with
to assess statistical significance between groups. Overall 10 patients mild pulmonary stenosis (PS), 7 patients
survival probability, as well as survival probability for
different surgical categories (palliative procedures,
corrective procedures, and reoperation), were analyzed Table 1. Postoperative Complications
according to Kaplan–Meier method.
Complication n
Arrhythmias 6
Results Bleeding 3
Low output syndrome 2
Thirty patients (>17 years of age) requiring surgical Pericardial effusion requiring drainage 1
treatment for TOF were included in this study which Pleural effusion 1
is consist of 13 males and 17 females. Mean age at Cardiac arrest 1
surgery was 20.87+5.49 years. Extra cardiac anomalies Neurological deficit persisting at discharge 1
were identified in 5 patients and other intracardiac Other postoperative complication 1
Table 2. Surgical Categories
Variables Analyzed Corrective Palliative Reoperations p Value
Procedures Procedures
Number of procedures 20(66.7%) 6 (20.0%) 4(13.3%)
Sex M/F 5/15 6/0 2/2 0.05
Mean age in years (SD) 20.35(5.81) 21.8 (4.02) 22.0(6.78) 0.78
Preoperative sinus rhythm 12(60%) 4 (66.7%) 2(50%) 0.87
Postoperative complications 3(15%) 6 (100.0%) 1(25%) 0.01
Sinus rhythm at discharge 18(90%) 4 (66.7%) 4(100%) 0.24
Mean ICU stay/days (SD) 0.78(0.55) 1.22(1.71) 0.62(0.44) 0.49
Mean hospital stay/days (SD) 15.40(8.93) 9.67(6.97) 9.75(6.40) 0.23
Hospital mortality (%) 0(0%) 1(16.5%) 1(25%) 0.10
Jurnal Kardiologi Indonesia • Vol. 28, No. 3 • Mei 2007 199
Jurnal Kardiologi Indonesia
mild pulmonary insuffisiensi (PI) and 2 patients with Follow up data were available in 28 of 30 patients
severe PI. Two patients with moderate to severe right (93%) who were discharge from hospital. Reoperation
heart failure. was necessary in 2 of 30 patients (6%) within a mean
There were 2 hospital deaths (6.4%), one in the time 3 months after hospital discharge. At a mean
palliative surgery group and one in the reoperation follow-up time of 11.73+17.68 months 28 patients
group; no hospital death in the corrective group. The (93%) were in NYHA I-II. Late death occurred in 1
most common causes of death were pump failure and patient (3%). Survival probability according to
perioperative bleeding. Patients who underwent Kaplan–Meier showed an overall survival of 87.8% at
corrective procedures presented with lower mortality 60 months (Figure 1). A follow-up analysis shows an
rate, requiring also less time in the intensive care unit overall survival probability of 87.8% at 60 months,
and a shorter total hospital stay, although is was not which is higher for corrective procedures (92.3%) if
significant (Table 2). compared with reoperations (75%) and palliations
(83.3%) (Figure 2).
The significant p value is postoperative
1.00
complications (p<0.05), and there are no statistically
significantly different in the multiple comparison
(Bonferroni) test for mean comparison.
0.75 Overall survival
Probability of survival
0.50 Discussion
Patients with CHD who reach the adult age usually
0.25
remain in good or mildly decreased functional status
for several years and are eventually referred to surgical
0.00 treatment because of increasing symptoms not
0 20 40 60 80 controlled by medical therapy. The majority of these
Figure 1. Overall survival probability according to Kaplan- patients survived into adult age in good functional
Meier function with 95% confidence bands. Overall survival status, considering that 93.3 % of them were
in 60 months probability is 87.84% with 95% confidence preoperative NYHA class I or II. They are a selected
bands (0.66-0.96) group of patients mainly composed by individuals who
have survived into adult age without irreversible
1.00
Correction
damage to their heart and lung. Our data suggest that
adult TOF patient with good functional capacity
Palliattion
(NYHA class I-II), the hospital outcome can be better
0.75
Probability of survival
Reoperation
when compared to that of patients who presented with
worse functional status (NYHA class III-IV).
0.50 The overall hospital mortality for TOF repairs in
our centre during three years period (2003-2005,
0.25 N=273) was 6.23%, comparable to the 5% mortality
rate from the European Congenital Database. In our
0.00
series, there is no hospital mortality for TOF repair
0 20 40 60 80 in adult. Palliative procedure was offered to our adult
TOF patient with poor left ventricular function, to
Figure 2. Kaplan-Meier survival function by type of surgery improve the clinical condition at least temporarily.
(palliations , corrections, reoperation). Survival in 60 In our series there were 6 cases who had palliative
months probability in total correction type is 92.31% with procedure, with hospital mortality of 16.7% (1
95% confidence bands (0.57-0.99), in reoperation type is patient). Although the operations achieved a decrease
75% with 95% confidence bands (0.13-0.96) and in on cyanosis, we have no long-term functional results
palliation type is 83.33% with 95% confidence bands (0.27- of these patients. Reoperation after a previous
0.97) palliative procedure to enlarge pulmonary artery,
200 Jurnal Kardiologi Indonesia • Vol. 28, No. 3 • Mei 2007
Wilamarta K.V. et al: Surgical Risk for Adult with Tetralogy of Fallot
carried a high mortality rate (one out of 4 patients, Continuous evaluation of the quality of care
25%). The cause of death was related to perioperative become one of the highest priorities in modern surgical
bleeding. We have no reoperation related to conduit practice.7 Especially, in the field of Congenital Heart
placement or pulmonary valve replacement after Surgery (CHS), where adverse outcomes can be
initial correction. The better outcome in the frequent due to the wide spectrum of congenital cardiac
corrective group possibly related to the better conditions and severity of pathologies, as well as high
condition of the patients. proportion of palliations.8,9 It is obvious that 30 days
Deterioration of RV function and exercise capacity mortality measure carries important limitation for
correlate with a longer interval since repair, but these assessment of residual pulmonary regurgitation or
moderate associations can not be used to predict the stenosis, arrhythmia and ventricular failure.
pace of decline in the individual patients. Improvement According to the Good Clinical Practice
of clinical condition may be obtained by improving guidelines defined and recommended by World
right ventricle outflow tract (RVOT) function Health Organization (WHO), all database contents
preservation during surgery, and by reducing the effect should be verified by comparison with the original
of electrical inhomogenicity for long term outcome of records at the site of their origin-Source Data
TOF.5 The oldest patient in our series is a 42 years Verification (SDV).10,11 Two patients, out of thirty
old patient with poor right ventricular function and after verification, have been missed. There have been
arrhythmia, the long term outcome in this particular no statistically significant differences between
patient is also poor. preoperative sinus rhythm and rhythm at discharge.
Optimal timing for reoperation pulmonary valve Undoubtedly, modern intensive care technology
replacement seems crucial, as the children became an extends critical patients survival time what does not
adult, the criteria so far have not been established. We necessarily mean increase in long-term survival and
have seen this problem in a 26 years of age patient improvement of the quality of life. All congenital
with absent pulmonary valve. Shimazaki et.al6 showed cardiac surgery 30 days mortality was 3.58%12.
that in his series, beyond the age 30 to 40 progressively
more patients become symptomatic, with onset of right
heart failure. Conclusions.
A follow-up analysis shows an overall survival
probability of 87.8% at 60 months, which is higher Surgical treatment for Tetralogy of Fallot in adult
for corrective procedures (92.3%) if compared with patients at the National cardiovascular Centre Jakarta-
reoperations (75%) and palliations (83.3%). Although Indonesia is quite save and beneficial; a well organized
palliative operations in these kinds of patients did long term follow up is needed. The care of adult
achieve a decrease cyanosis at low risk, but we have no patients with corrected or uncorrected CHD is growing
long-term functional results of these patients to allow and become a challenging new field for the cardiologist
definitive conclusions. Reoperation after a palliative in Indonesia
procedures or previous corrective procedure includes
patients with either a residual lesion after correction
or patients who acquired secondary complications after References
their initial correction. These group of patients show
the most difficult challenging, who need the premium 1. Vladimiro L. Vida, Hakan berggren, William J. Brawn, Willem
hands of congenital adult cardiac surgeon. It is Daenen, et.al. Risk of surgery for congenital heart disease in
important to know the long term post-operative the adult: A multicentered European study. Ann Thorac Surg
functional results of these patients. Unfortunately we 2006; 83:161-8.
were able to collect follow-up information only in 67% 2. Michael A. Gatzoulis. Adult congenital heart disease: education,
of the patients, and limited to 60 months after the education, education. Nature Clinical Practice cardiovascular
operation (mean of 11.73 + 17.68 months). The reason Medicine 2006 vol 3 No.1.
for this limitation is related to the patients social 3. Joseph W. Rossano, E. O. Brian Smith, CharlesD. Fraser, E.
economy condition, most of them were referred from Dean McKenzie et al. Adults undergoing cardiac surgery at
peripheral suburban area, no proper follow up could Children’s Hospital: An analysis of perioperative morbidity. Ann
be performed. Thorac Surg 2007; 83:606-612.
Jurnal Kardiologi Indonesia • Vol. 28, No. 3 • Mei 2007 201
Jurnal Kardiologi Indonesia
4. Presbitero P, Prever SB, Contrafatto I, Morea M. Results of Annu 2002; 5(1):132.
total correction of TOF performed in adults: updated in 1996. 9. Mavroudis C (Chairman) and Congenital Database
Ann Thorac Surg. Subcommittee: Backer CL, Bove E, Burke RP, Cameron D,
5. M. Elizabeth Brickner, L. David Hillis, Richard A. Lange. Drinkwater DC, Edwards FH, Grover FL, Hammon JW Jr,
Congenital hearts disease in adults. 2o of two parts.New England Jacobs JP, Kron IL, Mayer JE, Myers JL, Ring WS, Siewers
J of Med. Feb 3 2000 No.5 Vol 342:334-342. RD, Szarnicki RJ, Watson DC Jr, Data analyses of the society
6. Shimazaki Y, Blackstone EH, Kirklin JW: The natural history of Thoracic Surgeons National Congenital Cardiac Surgery
of isolated congenital pulmonary valve incompetence; surgical Database 1994-1997. Summit Medical, Minnetonka, MN;
implications. J Thorac Cardiovasc Surg 32;257,1984 September 1998.
7. Daenen W, Lacour-Gayet F, Abert T, Comas JV, Daebritz SH, 10. Khodla R, Verna DD, Kapur A, Khosla S. Efficient source data
DiDonato R, Hamilton JR, Lindberg H, Maruszewski B, Monro verification. Indian Journal of Pharmacology 2000; 32:180-6
J. EACTS congenital heart disease committee. Optimal structure 11. WHO guidelines for Good Clinical Practice for Trial on
of a congenital heart surgery department in Europe. Eur J Pharmacoceutical Products; 1994
Cardiothorac Surg 2003; 24(3):343-51. 12. Bohdan Maruszewski, Francois Lacour-Gayet, James L. Monro,
8. Williams WG, McCrindle BW. Practical experience with Bruce E. Keogh, Zdislaw Tobota, Andrzej Kansy. An attempt
databases for congenital heat disease: a registry versus academic at data verification in the EACTS Congenital Database. Eur J
database. Semin Thorac Cardiovasc Surg Pediatr Card Surg of Cardiothorac Surg 2005; 28(3):400-6
202 Jurnal Kardiologi Indonesia • Vol. 28, No. 3 • Mei 2007
You might also like
- How To Start Calisthenics Workout - The Beginners Ultimate Calisthenics Workout Plan and Body Building Routine For A Healthy Lifestyle. - D, Fryer (2021)Document33 pagesHow To Start Calisthenics Workout - The Beginners Ultimate Calisthenics Workout Plan and Body Building Routine For A Healthy Lifestyle. - D, Fryer (2021)Gustavo Gonzalez ServaNo ratings yet
- Ucm 423806Document69 pagesUcm 423806Rahman Mukti AjiNo ratings yet
- ETU 776 TripDocument1 pageETU 776 TripbhaskarinvuNo ratings yet
- Standard Operating Procedure: Validation of Heating Ventilation and Air Conditioning (Hvac) SystemDocument20 pagesStandard Operating Procedure: Validation of Heating Ventilation and Air Conditioning (Hvac) SystemMaryanthony Namyalo100% (3)
- Unit 4 - Site PlanningDocument22 pagesUnit 4 - Site PlanningvgdarchNo ratings yet
- Bojar PediatricDocument123 pagesBojar PediatricLuqman AlwiNo ratings yet
- Filter Integrity Test MachineDocument4 pagesFilter Integrity Test MachineAtul SharmaNo ratings yet
- Quality Operating Process: Manual of Operations Care of PatientsDocument4 pagesQuality Operating Process: Manual of Operations Care of PatientsPrabhat KumarNo ratings yet
- ADAB Member List Provides Contact Details for Development OrganizationsDocument8 pagesADAB Member List Provides Contact Details for Development OrganizationsShipon GhoshNo ratings yet
- Water SprayDocument2 pagesWater SpraySaba SamankanNo ratings yet
- Endocarditis in The Elderly: Clinical, Echocardiographic, and Prognostic FeaturesDocument8 pagesEndocarditis in The Elderly: Clinical, Echocardiographic, and Prognostic FeaturesMehdi285858No ratings yet
- OkeeaeDocument6 pagesOkeeaeZulqi SusiloNo ratings yet
- Khan 2023 Outcomes of Surgical Repair of Tetralogy of Fallot child and adultDocument6 pagesKhan 2023 Outcomes of Surgical Repair of Tetralogy of Fallot child and adultElfrida AuliaNo ratings yet
- Prediktor Kegagalan Intervensi Koroner Perkutan Pada Oklusi Total Di Pusat Jantung Nasional, IndonesiaDocument9 pagesPrediktor Kegagalan Intervensi Koroner Perkutan Pada Oklusi Total Di Pusat Jantung Nasional, IndonesiaNining AnjarwatiNo ratings yet
- JET4Document8 pagesJET4fufuka fukalifuNo ratings yet
- Bernard D. Prendergast and Pilar Tornos: Surgery For Infective Endocarditis: Who and When?Document26 pagesBernard D. Prendergast and Pilar Tornos: Surgery For Infective Endocarditis: Who and When?om mkNo ratings yet
- 10 3389@fsurg 2020 00047Document9 pages10 3389@fsurg 2020 00047Hana Nuraisa BasyaNo ratings yet
- Study 3Document7 pagesStudy 3OstazNo ratings yet
- PIIS1078588419310755Document7 pagesPIIS1078588419310755zeeshan qurbanNo ratings yet
- Surgical Outcomes of DVAPTRepairDocument11 pagesSurgical Outcomes of DVAPTRepairJose YoveraNo ratings yet
- Brief Reports: Outcome of Chest Pain Patients Discharged From A French Emergency Department: A 60-Day Prospective StudyDocument4 pagesBrief Reports: Outcome of Chest Pain Patients Discharged From A French Emergency Department: A 60-Day Prospective StudyDiana LoloiuNo ratings yet
- High Lactate Levels Are Predictors of Major Complications After Cardiac SurgeryDocument6 pagesHigh Lactate Levels Are Predictors of Major Complications After Cardiac SurgeryMuhammad RizqiNo ratings yet
- Short - and Long-Term Outcomes at A Single InstitutionDocument7 pagesShort - and Long-Term Outcomes at A Single InstitutionJonathan Frimpong AnsahNo ratings yet
- Atm 08 23 1626Document12 pagesAtm 08 23 1626Susana MalleaNo ratings yet
- 70-Article Text-127-2-10-20200403Document7 pages70-Article Text-127-2-10-20200403rifalNo ratings yet
- Diagnostic Value of Three Dimensional EchocardiogrDocument3 pagesDiagnostic Value of Three Dimensional EchocardiogrAmilkar VazquezNo ratings yet
- DownloadDocument6 pagesDownloadDoraNo ratings yet
- Total Anomalous Pulmonary Venous Drainage Repair: Redefining The Long-Term ExpectationsDocument4 pagesTotal Anomalous Pulmonary Venous Drainage Repair: Redefining The Long-Term Expectationswiyay34652ceoshubcomNo ratings yet
- cimitarraDocument7 pagescimitarracindy beltranNo ratings yet
- Late Surgical Treatment of Tetralogy of FallotDocument3 pagesLate Surgical Treatment of Tetralogy of FallotBryan NguyenNo ratings yet
- Article - Surgical Management of Infective Endocarditis - Early Predictors of Short-Term Morbidity and MortalityDocument6 pagesArticle - Surgical Management of Infective Endocarditis - Early Predictors of Short-Term Morbidity and Mortalityfluid_man_brazilNo ratings yet
- Castle AfDocument11 pagesCastle AfgustavoNo ratings yet
- Improvement After Surgical Closure of Secundum Atrial Septal Defects in Adults 2155 9880 1000493Document7 pagesImprovement After Surgical Closure of Secundum Atrial Septal Defects in Adults 2155 9880 1000493Riani NazilaNo ratings yet
- Jurnal THTDocument3 pagesJurnal THTValentina AdindaNo ratings yet
- Mawaqit Makani, Ndaru Setyaningrum : Corresponding Author. Email: Ndaru - Setyaningrum@uii - Ac.idDocument12 pagesMawaqit Makani, Ndaru Setyaningrum : Corresponding Author. Email: Ndaru - Setyaningrum@uii - Ac.idGita wulandariNo ratings yet
- Articulo Referencia CX EndovadcularDocument7 pagesArticulo Referencia CX EndovadcularGabriel Santiago Cano PerdomoNo ratings yet
- Tga Jurnal NcbiDocument30 pagesTga Jurnal NcbiMYMANo ratings yet
- Catheter Ablationin in AF With CHFDocument11 pagesCatheter Ablationin in AF With CHFKristian Sudana HartantoNo ratings yet
- DIAB10.1002@ccd.28194 4Document9 pagesDIAB10.1002@ccd.28194 4marsim92No ratings yet
- Elaxim ResearchDocument6 pagesElaxim ResearchMayukh BanerjeeNo ratings yet
- Early and Late Results of The Modified Fontan Operation For Heterotaxy SyndromeDocument5 pagesEarly and Late Results of The Modified Fontan Operation For Heterotaxy SyndromeJacob Trisusilo SaleanNo ratings yet
- Long-Term Outcomes of Patients With Tetralogy of Fallot Repaired in Young Infants and ToddlersDocument8 pagesLong-Term Outcomes of Patients With Tetralogy of Fallot Repaired in Young Infants and ToddlersResiden KardiologiNo ratings yet
- Articulo VMDocument8 pagesArticulo VMapi-629928343No ratings yet
- Carotid UltrasoundDocument9 pagesCarotid UltrasoundLora LefterovaNo ratings yet
- Early and Late Postoperative Tachyarrhythmias in Children and Young Adults Undergoing Congenital Heart Disease SurgeryDocument13 pagesEarly and Late Postoperative Tachyarrhythmias in Children and Young Adults Undergoing Congenital Heart Disease SurgeryYar ZepolNo ratings yet
- Pediatr Transplant 2016 Pundi - 1Document6 pagesPediatr Transplant 2016 Pundi - 1bm1No ratings yet
- TurkeyGMJ 62 200 enDocument6 pagesTurkeyGMJ 62 200 enCocoNo ratings yet
- Hema Gayathri Arunachalam, Et AlDocument8 pagesHema Gayathri Arunachalam, Et Aluswatun khasanahNo ratings yet
- Korean QX Total Pulm Veins 2010Document5 pagesKorean QX Total Pulm Veins 2010Dr. LicónNo ratings yet
- CIRCULATIONAHA. Incidence, Management, and Immediate- and Long-Term Outcomes After Iatrogenic Aortic Dissection DuringDocument6 pagesCIRCULATIONAHA. Incidence, Management, and Immediate- and Long-Term Outcomes After Iatrogenic Aortic Dissection DuringSajjad HussainNo ratings yet
- IE New 1Document5 pagesIE New 1Kelik WagiyantoNo ratings yet
- Red Cell Distribution Width Is Associated With Acute Myocardial Infarction in Young PatientsDocument6 pagesRed Cell Distribution Width Is Associated With Acute Myocardial Infarction in Young PatientsMentari FaisalNo ratings yet
- Nejmoa 2026141Document14 pagesNejmoa 2026141Matheus FelipeNo ratings yet
- PreventDocument14 pagesPreventfelipeNo ratings yet
- Anesthesia For Major Surgery in NeonatesDocument18 pagesAnesthesia For Major Surgery in NeonatesfulkifadhilaNo ratings yet
- Cardiac Interventions in Neonates WiDocument11 pagesCardiac Interventions in Neonates WiimNo ratings yet
- Nihms 979441Document33 pagesNihms 979441infatuatingsweetserenadeNo ratings yet
- Pi Is 0007091217540015Document10 pagesPi Is 0007091217540015Yoga WibowoNo ratings yet
- Art TaaDocument7 pagesArt TaaCristinaNo ratings yet
- Nennyelyaniginting,+7 +Yoani+Maria+Vianney+Bita+AtyDocument10 pagesNennyelyaniginting,+7 +Yoani+Maria+Vianney+Bita+AtyBayu IsmoyoNo ratings yet
- CourageDocument14 pagesCourageSuryaNo ratings yet
- Outcomes of Cardiopulmonary Resuscitation in The Emergency DepartmentDocument4 pagesOutcomes of Cardiopulmonary Resuscitation in The Emergency DepartmentSteve aokiNo ratings yet
- Management of Penetrating Wounds of The HeartDocument2 pagesManagement of Penetrating Wounds of The HeartInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- E2 Journal of Hypertension Vol 35, E-Supplement 3, November 2017Document1 pageE2 Journal of Hypertension Vol 35, E-Supplement 3, November 2017Sadam_fasterNo ratings yet
- Follow-Up Transcatheter Closure of Atrial Septal Defect in Young Children: Results andDocument7 pagesFollow-Up Transcatheter Closure of Atrial Septal Defect in Young Children: Results andKholid KuNo ratings yet
- A Minimalistic Approach of Device Closure of Atrial Septal Defect: Analysis of Cases Over Five YearsDocument10 pagesA Minimalistic Approach of Device Closure of Atrial Septal Defect: Analysis of Cases Over Five YearsajmrdNo ratings yet
- New Prognostic Classification and Managements in Infants With Esophageal AtresiaDocument8 pagesNew Prognostic Classification and Managements in Infants With Esophageal AtresiaAnisa GayatriNo ratings yet
- Cardaic ResynchronizationDocument11 pagesCardaic ResynchronizationSamatha BiotechNo ratings yet
- HHS Public Access: The Use of Del Nido Cardioplegia in Adult Cardiac Surgery: A Prospective Randomized TrialDocument18 pagesHHS Public Access: The Use of Del Nido Cardioplegia in Adult Cardiac Surgery: A Prospective Randomized Trialcem berkay duranNo ratings yet
- Critical Care for Potential Liver Transplant CandidatesFrom EverandCritical Care for Potential Liver Transplant CandidatesDmitri BezinoverNo ratings yet
- 03 TOEFL ITP BYOP Test Taker Procedures FinalDocument20 pages03 TOEFL ITP BYOP Test Taker Procedures FinalAmilia DeviNo ratings yet
- Pulmonary Function TestDocument39 pagesPulmonary Function TestLuqman AlwiNo ratings yet
- Pulmonary Function TestDocument39 pagesPulmonary Function TestLuqman AlwiNo ratings yet
- Adult Fallot Mortality in IndonesiaDocument6 pagesAdult Fallot Mortality in IndonesiaLuqman AlwiNo ratings yet
- Mitral Valve Repair, How I Teach ItDocument5 pagesMitral Valve Repair, How I Teach ItLuqman AlwiNo ratings yet
- Suture Material LectureDocument35 pagesSuture Material LectureLuqman AlwiNo ratings yet
- Management Arteriosclerosis and ClaudicationDocument41 pagesManagement Arteriosclerosis and ClaudicationLuqman AlwiNo ratings yet
- APACHEIIDocument1 pageAPACHEIIFailasuf WibisonoNo ratings yet
- Manouguian Technique PDFDocument6 pagesManouguian Technique PDFLuqman AlwiNo ratings yet
- Jurnal Mba Sari 1Document44 pagesJurnal Mba Sari 1PitoAdhiNo ratings yet
- AKUT ABDOMEN Rev2Document77 pagesAKUT ABDOMEN Rev2Luqman AlwiNo ratings yet
- VaricoceleDocument14 pagesVaricoceleLuqman AlwiNo ratings yet
- IpssDocument1 pageIpssIka FairuzaNo ratings yet
- Abdominal Wall Defects GuideDocument42 pagesAbdominal Wall Defects GuideLuqman AlwiNo ratings yet
- Surat Perjanjian Non HumanDocument1 pageSurat Perjanjian Non HumanLuqman AlwiNo ratings yet
- Skin Graft and Flap GuideDocument11 pagesSkin Graft and Flap GuideLuqman AlwiNo ratings yet
- The Effect Administration of Phaleria Macrocarpa To Cell Proliferation - JoseDocument19 pagesThe Effect Administration of Phaleria Macrocarpa To Cell Proliferation - JoseLuqman AlwiNo ratings yet
- Hernia of Umbilical Cord: Report of Three Unusual Cases: Ase SeriesDocument4 pagesHernia of Umbilical Cord: Report of Three Unusual Cases: Ase SeriesLuqman AlwiNo ratings yet
- Ethnomusicology in Times of TroubleDocument15 pagesEthnomusicology in Times of TroubleLéo Corrêa BomfimNo ratings yet
- Text CDocument1,100 pagesText CAli NofalNo ratings yet
- Common Admission Test (CAT) 2020 Admit Card: BarcodeDocument2 pagesCommon Admission Test (CAT) 2020 Admit Card: BarcodeViraaj ThakurNo ratings yet
- Journal Review - Philosophical and Contextual Issue in Nursing Theory DevelopmentDocument4 pagesJournal Review - Philosophical and Contextual Issue in Nursing Theory DevelopmentJULIE ANN PARANo ratings yet
- Argumentative Essay-Nursing HomesDocument1 pageArgumentative Essay-Nursing HomesHM TanNo ratings yet
- Observation of Unknown SpectrumDocument3 pagesObservation of Unknown SpectrumOmar HusseinNo ratings yet
- Concrete Exposures ClassesDocument4 pagesConcrete Exposures ClasseshamidkarimpourNo ratings yet
- UG TRB Physical Education Study MaterialDocument17 pagesUG TRB Physical Education Study Materialசண்முக சுந்தரம் குருசாமி100% (2)
- Comparative Study of Soaps of Hul P Amp G Godrej Nirma and Johnson Amp Johnson 130410234307 Phpapp01 PDFDocument71 pagesComparative Study of Soaps of Hul P Amp G Godrej Nirma and Johnson Amp Johnson 130410234307 Phpapp01 PDFdheeraj agarwalNo ratings yet
- Product Data Sheet GC 120 LDocument5 pagesProduct Data Sheet GC 120 LYohanes Meinata PermanaNo ratings yet
- Breast CancerDocument1 pageBreast CancerAdang FirmansyahNo ratings yet
- Chapter 1 F&B ManagementDocument59 pagesChapter 1 F&B ManagementMohd Faizal Bin AyobNo ratings yet
- Instructional Materials: For K12Document17 pagesInstructional Materials: For K12Ram Jacob LevitaNo ratings yet
- Effects of Restorative Materials On Dental PulpDocument32 pagesEffects of Restorative Materials On Dental PulpUpasana BhandariNo ratings yet
- Match Jobs Pictures Sentences Verbs Phrases HobbiesDocument4 pagesMatch Jobs Pictures Sentences Verbs Phrases HobbiesJose ArreagaNo ratings yet
- Predictor PlatesDocument40 pagesPredictor PlatesrambabuNo ratings yet
- De Thi Thu Vao 10 Mon Tieng Anh Quan Dong Da Ha NoiDocument5 pagesDe Thi Thu Vao 10 Mon Tieng Anh Quan Dong Da Ha NoiTrang VuongNo ratings yet
- NCM 120Document5 pagesNCM 120Tiffany AdriasNo ratings yet
- Solutions: Key Words and ConceptsDocument4 pagesSolutions: Key Words and ConceptsSamuel Enrique Cano PatocNo ratings yet
- Quality Management System at Pharmaceutical IndustryDocument85 pagesQuality Management System at Pharmaceutical IndustryTissa Novida Aulia ZahraNo ratings yet
- Can You Distinguish Neutral, Formal and Informal Among The Following Groups of WordsDocument3 pagesCan You Distinguish Neutral, Formal and Informal Among The Following Groups of WordsВікторія РудаNo ratings yet
- Joshua Gonzalez - ResumeDocument2 pagesJoshua Gonzalez - Resumeapi-483760707No ratings yet