Professional Documents
Culture Documents
13 Neonatal Fact Sheet
Uploaded by
Walaa EldesoukeyCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
13 Neonatal Fact Sheet
Uploaded by
Walaa EldesoukeyCopyright:
Available Formats
Neonatal Physical Therapy Practice:
Roles and Training
The Section on Pediatrics of the American Physical Therapy Association and the American Board of
Physical Therapy Residency and Fellowship Education have recognized neonatal physical therapy as a
subspecialty area of practice requiring advanced expertise.
Rationale
Neonates are infants (birth to 12 months of age) with medical fragility. They require specialized care due
to physiologic, behavioral, and developmental vulnerabilities. Neonatal physical therapists play
important roles in the interdisciplinary neonatal care team.
Guidelines outlining neonatal physical therapy roles, competencies, and scope of practice have been
published.1-2 Suggestions are made below for mentored, sequential, competency-based training in
preparation for providing physical therapy services for this vulnerable population.
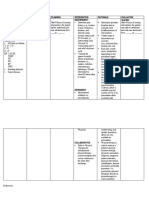
Recommendations for Developing Expertise in Neonatal Physical Therapy
The vulnerability of neonates born prematurely or with complex medical conditions requires physical
therapy services by physical therapists with specialized training to meet the complex needs of this
population. Clinicians seeking to practice in this unique area should participate in continuing education,
mentorship, and supervised experience before providing neonatal physical therapy services. To gain
experience in preparation for mentored training in the neonatal intensive care unit (NICU), pediatric
therapists will benefit from initially working with NICU graduates in early intervention, hospitals, or
follow-up programs. Participation in examination and intervention with older, less fragile infants is
advised prior to working with young neonates.
Preceded, competency-based experience is the preferred method of obtaining expertise in neonatal
physical therapy. Neonatal physical therapy mentoring should be conducted by teams, which may
include neonatal nurses, neonatologists, and neonatal therapists (physical, occupational, or speech) to
cover the core principles guiding care for this vulnerable population. Specific mentoring in physical
therapy roles and competencies is essential.
1 | Academy of Pediatric Physical Therapy Fact Sheet/Resource
The Physical Therapist’s Roles and Responsibilities in Neonatal Physical Therapy:
• Screen neonates to determine needs for physical therapy referral.
• Examine neonates and interpret findings.
• Develop and implement a plan to prevent neurobehavioral disorganization and complications of
prematurity in multiple systems.
• Design, implement, and evaluate the efficacy of intervention plans in collaboration with the
family and medical team.
• Develop and implement discharge plans in collaboration with the family, medical team, and
community resources.
• Consult with providers of specialized equipment or services in preparation for community-based
care.
• Consult and collaborate with health care professionals, families, policy makers, and community
organizations to advocate for services to support the development of neonates.
• Incorporate evidence-based literature into neonatal practice.
• Communicate, demonstrate, and evaluate neonatal physical therapy care procedures with NICU
professionals and other caregivers.
• Develop a physical therapy risk management plan.
• Evaluate the effectiveness of a neonatal physical therapy program.
Knowledge and Skills Required
Knowledge
• Theoretical Principles that guide physical therapy practice in the NICU:
o Family-centered care
o Synactive theory of development¤ Dynamic systems theory
o Theory of neuronal group selection¤ International Classification of Functioning, Disability
and Health (ICF)
• Typical development of:
o Central nervous system and musculoskeletal system
o Behavioral state regulation and behavioral stress cues
o Motor and sensory skills
o Social development and infant/parent interaction
o Early cognitive development and learning opportunities in infancy
• Developmental outcomes of neonatal at developmental risk:
o Infants born preterm
o Infants born at low birth weight
o Infants with genetic conditions
o Infants with cardiovascular and pulmonary conditions
o Infants with neonatal brain injury
• Evidence for neonatal assessments and interventions
• Effective strategies for communication:
o Teaming
o Consulting with other professionals
o Providing family education on a culturally sensitive manner
2 | Academy of Pediatric Physical Therapy Fact Sheet/Resource
Skills
• Examination procedures for neonates:
o Determining physiologic and behavioral readiness for neonatal physical therapy
examination
o Monitoring autonomic, behavioral state, and motor stability throughout an examination
o Conducting observational examination techniques
o Administrating minimal contact examination techniques
o Determining when standardized assessment is safe to perform and clinically warranted
o Providing standardized assessments developed for neonates born preterm or at term
gestation
o Determining the need for and completing oral motor or feeding readiness assessments
• Safe and effective interventions:
o Positioning to support alignment and movement
o Handling to support development and daily activities
o Splinting to provide support for alignment and manage atypical postures or tone
o Providing oral motor intervention in preparation for oral feeding
o Developing and implementing parent/caregiver education programs for adult learners
with diverse backgrounds
o Developing and implementing environmental modification to support behavioral state
regulation
• Educating/consulting others:
o Collaborating as part of an interdisciplinary development team
o Communicating with physicians, occupational therapists, speech language pathologists,
respiratory therapists, child life, social workers, and other professionals
o Planning for discharge, including community resources, car seats, and other equipment
or therapy needs
o Communicating with family members form diverse backgrounds
3 | Academy of Pediatric Physical Therapy Fact Sheet/Resource
References
1. Sweeney JK, Heriza CB, Blanchard Y. Neonatal physical therapy; part I: clinical competencies and
neonatal inten-sive care unit clinical training models. Pediatr Phys Ther. 2009;21(4):296-307.
2. Sweeney JK, Heriza CB, Blanchard Y, Dusing SC. Neonatal physical therapy; part II: practice
frameworks and evi-dence-based practice guidelines [erratum in: Pediatr Phys Ther. 2010;22(4):377].
Pediatr Phys Ther. 2010;22(1):2-16.
Resources
Neonatology Special Interest Group, Section on Pediatrics, American Physical Therapy Association:
http://www.pediatricapta.org/special-interest-groups/neonatol-ogy/index.cfm
Physical Therapy Neonatology Fellowship Programs:
http://www.abptrfe.org/FellowshipPrograms/ProgramsDirectory/
Rapport MJ, Sweeney JK, Dannemiller L, Heriza CB. Student experiences in the neonatal intensive care
unit: addendum to neonatal physical therapy competencies and clinical training models. Pediatr Phys
Ther. 2010;22(4):439-440.
There are numerous Web sites and publications available on this subject; this list is not meant to be
all inclusive. Many of the listed sites have links to additional resources.
©2013 by the Academy of Pediatric Physical Therapy, American Physical Therapy Association, 1111 N
Fairfax Street, Alexandria, VA 22314-1488, www.pediatricapta.org.
Developed by the Practice Committee of APPT, with expert contributors Stacey Dusing, PT, PhD, Jane
Sweeney, PT, PhD, PCS, FAPTA, Sheree York, PT, DPT, PCS, and Kim Nixon Cave, PT, PhD, PCS.
The Academy of Pediatric Physical Therapy provides access to these member-produced fact sheets
and resources for informational purposes only. They are not intended to represent the position of
APPT or of the American Physical Therapy Association.
4 | Academy of Pediatric Physical Therapy Fact Sheet/Resource
You might also like
- 09 ABCs of Ped PTDocument3 pages09 ABCs of Ped PTGabriela MarinNo ratings yet
- OT - Neonatal - Intensive - Care - IJOT - ENDocument6 pagesOT - Neonatal - Intensive - Care - IJOT - ENSara Gomes CastroNo ratings yet
- Introduction To Pedi PTDocument36 pagesIntroduction To Pedi PTTitanium TssNo ratings yet
- Therapist's Guide to Pediatric Affect and Behavior RegulationFrom EverandTherapist's Guide to Pediatric Affect and Behavior RegulationNo ratings yet
- Principles of Pediatric Nursing Caring For Children 6th Edition Ball Solutions Manual 1Document36 pagesPrinciples of Pediatric Nursing Caring For Children 6th Edition Ball Solutions Manual 1kevinmichaelgwzmxiyrts100% (23)
- Brueryosefcv 2022Document6 pagesBrueryosefcv 2022api-595108452No ratings yet
- Changing Trends in Pediatrics and Pediatric NursingDocument18 pagesChanging Trends in Pediatrics and Pediatric NursingSakshi AsthanaNo ratings yet
- Follow Up High Risk NBDocument36 pagesFollow Up High Risk NBinggrit anggrainiNo ratings yet
- 1.1, 1.2, 1.3, 1.5 Paediatric Nursing Presentation - 1-1Document54 pages1.1, 1.2, 1.3, 1.5 Paediatric Nursing Presentation - 1-1Christina YounasNo ratings yet
- Principles of Pediatric Nursing Caring For Children 6Th Edition Ball Solutions Manual Full Chapter PDFDocument25 pagesPrinciples of Pediatric Nursing Caring For Children 6Th Edition Ball Solutions Manual Full Chapter PDFJasonMoralesykcx100% (9)
- FINAL-PSYCHE Without TranscribeDocument42 pagesFINAL-PSYCHE Without TranscribeGino B. BulanaNo ratings yet
- Ethical Issues in NeonateDocument11 pagesEthical Issues in Neonatethilaga880% (1)
- Nursing As A ProfessionDocument29 pagesNursing As A ProfessionKenn NuydaNo ratings yet
- Nidcap Poster Final Edited For Research DayDocument1 pageNidcap Poster Final Edited For Research Dayapi-262531856No ratings yet
- Health Career PathwaysDocument72 pagesHealth Career PathwaysRaleigh Marvin PadillaNo ratings yet
- Mental Retardation Treatment and ManagementDocument12 pagesMental Retardation Treatment and ManagementMelchoniza CalagoNo ratings yet
- 1.pengantar FT PediatrikDocument46 pages1.pengantar FT PediatrikrizabNo ratings yet
- Guide Fact SheetDocument4 pagesGuide Fact SheetRodrigo CavalcanteNo ratings yet
- Parent-Child Interaction Therapy with Toddlers: Improving Attachment and Emotion RegulationFrom EverandParent-Child Interaction Therapy with Toddlers: Improving Attachment and Emotion RegulationNo ratings yet
- Knowledge For Graduate Practice 527197: Chronic ConditionsDocument36 pagesKnowledge For Graduate Practice 527197: Chronic ConditionsSofia Krylova-SmithNo ratings yet
- Competency Based Training Programme: Dnb-NeonatologyDocument62 pagesCompetency Based Training Programme: Dnb-NeonatologySonu AntonyNo ratings yet
- 01 NL Trong Tam Va 6 NL Cot Loi - Sinh VienDocument130 pages01 NL Trong Tam Va 6 NL Cot Loi - Sinh VienTrang BùiNo ratings yet
- Running Head: PRACTICE SUMMARY 1Document11 pagesRunning Head: PRACTICE SUMMARY 1api-466983597No ratings yet
- NCLEX-RN Exam Prep 2024-2025: 500 NCLEX-RN Test Prep Questions and Answers with ExplanationsFrom EverandNCLEX-RN Exam Prep 2024-2025: 500 NCLEX-RN Test Prep Questions and Answers with ExplanationsNo ratings yet
- Recreation Therapy: Evidence In-SightDocument14 pagesRecreation Therapy: Evidence In-SightΔΗΜΗΤΡΗΣ ΝΑΝΗΣ100% (1)
- Education SeminarDocument88 pagesEducation SeminarsallycynthiaNo ratings yet
- NCM 0114 Module 4 Audio PowerpointDocument20 pagesNCM 0114 Module 4 Audio PowerpointKristine KimNo ratings yet
- Quality Activities in Center-Based Programs for Adults with Autism: Moving from Nonmeaningful to MeaningfulFrom EverandQuality Activities in Center-Based Programs for Adults with Autism: Moving from Nonmeaningful to MeaningfulNo ratings yet
- 10 y 11 UciDocument51 pages10 y 11 UciBePe DenisseNo ratings yet
- Faye Glenn AbdellahDocument31 pagesFaye Glenn AbdellahMikz JocomNo ratings yet
- Care of Mother, Child, and Adolescent: Prepared by Donna Belle Sumugat RN ManDocument26 pagesCare of Mother, Child, and Adolescent: Prepared by Donna Belle Sumugat RN ManLaurence Docog100% (1)
- NIDCAPDocument38 pagesNIDCAPShahpb100% (3)
- Care of The Older Adult in WellnessDocument67 pagesCare of The Older Adult in WellnessShazich Keith Lacbay100% (1)
- Finding the Path in Alzheimer’s Disease: Early Diagnosis to Ongoing Collaborative CareFrom EverandFinding the Path in Alzheimer’s Disease: Early Diagnosis to Ongoing Collaborative CareNo ratings yet
- Health10 Q4 M7Document12 pagesHealth10 Q4 M7memnochmangubat1104No ratings yet
- PediatricsDocument48 pagesPediatricsNeha OberoiNo ratings yet
- Neonate: Presented By: Sheikh Maria Tabassum and Sharin Robinson Dot (Batch:1)Document14 pagesNeonate: Presented By: Sheikh Maria Tabassum and Sharin Robinson Dot (Batch:1)NABEELA WALINo ratings yet
- Parents With Challenging Children PDFDocument145 pagesParents With Challenging Children PDFAnonymous Ax12P2srNo ratings yet
- O Applies Appropriate Knowledge of Major Health Problems To Guide Nursing PracticeDocument5 pagesO Applies Appropriate Knowledge of Major Health Problems To Guide Nursing Practiceapi-529216367No ratings yet
- Children's Mental Heath PolicyDocument28 pagesChildren's Mental Heath PolicyMarina MeloNo ratings yet
- Child Obesity Service Provision A Cross-Sectional Survey of Physiotherapy Practice Trends and Professional NeedsDocument8 pagesChild Obesity Service Provision A Cross-Sectional Survey of Physiotherapy Practice Trends and Professional Needsanggie mosqueraNo ratings yet
- PAPER WORKPaediatricsDocument22 pagesPAPER WORKPaediatricsIzzati OthmanNo ratings yet
- Physical Therapy Clinical ManagementDocument24 pagesPhysical Therapy Clinical ManagementClaudia MicuNo ratings yet
- Physical Therapy Clinical Management.9 PDFDocument24 pagesPhysical Therapy Clinical Management.9 PDFClaudia MicuNo ratings yet
- Research Day-Nidcap - Goddard & Noss 2015Document16 pagesResearch Day-Nidcap - Goddard & Noss 2015api-262531856No ratings yet
- Assessing Neuromotor Readiness for Learning: The INPP Developmental Screening Test and School Intervention ProgrammeFrom EverandAssessing Neuromotor Readiness for Learning: The INPP Developmental Screening Test and School Intervention ProgrammeRating: 5 out of 5 stars5/5 (1)
- Gerontological Nursing: Scope and Standards of Practice, 2nd EditionFrom EverandGerontological Nursing: Scope and Standards of Practice, 2nd EditionNo ratings yet
- Information Education CommunicationDocument41 pagesInformation Education Communicationhiral mistry100% (2)
- 2022 NMC DM NeonatologyDocument30 pages2022 NMC DM NeonatologySutirtha RoyNo ratings yet
- Palliative Care Needs Assessment GuidanceDocument13 pagesPalliative Care Needs Assessment Guidancenovia100% (1)
- Perinatal Palliative Care: A Clinical GuideFrom EverandPerinatal Palliative Care: A Clinical GuideErin M. Denney-KoelschNo ratings yet
- Health10 q4 Week6 v4Document12 pagesHealth10 q4 Week6 v4Maria Rose Tariga AquinoNo ratings yet
- CBT for Psychological Well-Being in Cancer: A Skills Training Manual Integrating DBT, ACT, Behavioral Activation and Motivational InterviewingFrom EverandCBT for Psychological Well-Being in Cancer: A Skills Training Manual Integrating DBT, ACT, Behavioral Activation and Motivational InterviewingNo ratings yet
- Perineal CareDocument5 pagesPerineal CareTomi AbrahamNo ratings yet
- Nursing As A ProfessionDocument38 pagesNursing As A ProfessionFranco Razon100% (1)
- Cahpater 10 ManagementofcerebralpalsyDocument71 pagesCahpater 10 Managementofcerebralpalsyashlyn granthamNo ratings yet
- 314 NCMB - M2-Cu7Document7 pages314 NCMB - M2-Cu7Roby Roi De GuzmanNo ratings yet
- Management of Children With Cerebral PalsyDocument45 pagesManagement of Children With Cerebral PalsyNamakau MuliloNo ratings yet
- Ankle and Foot Injuries in The Young AthleteDocument14 pagesAnkle and Foot Injuries in The Young AthleteWalaa EldesoukeyNo ratings yet
- The Cumberland Ankle Instability Tool CAIT in TheDocument10 pagesThe Cumberland Ankle Instability Tool CAIT in TheWalaa EldesoukeyNo ratings yet
- The Effects of Wii Fit Plus Training On FunctionalDocument9 pagesThe Effects of Wii Fit Plus Training On FunctionalWalaa EldesoukeyNo ratings yet
- Systematic Review of Chronic Ankle Instability in ChildrenDocument19 pagesSystematic Review of Chronic Ankle Instability in ChildrenWalaa EldesoukeyNo ratings yet
- 2 - Comparison of Supervised Physiotherapy Program VersesDocument8 pages2 - Comparison of Supervised Physiotherapy Program VersesWalaa EldesoukeyNo ratings yet
- The Effectof Xbox Kinect Intervention On Balance Ability For Previously Injured Young Competitive Male Athletes A Preliminary StudyDocument10 pagesThe Effectof Xbox Kinect Intervention On Balance Ability For Previously Injured Young Competitive Male Athletes A Preliminary StudyWalaa EldesoukeyNo ratings yet
- The Effects of Stable and Unstable Training Surfaces On Dynamic PDocument89 pagesThe Effects of Stable and Unstable Training Surfaces On Dynamic PWalaa EldesoukeyNo ratings yet
- Is Virtual Reality Effective in Orthopedic Rehabilitation A Systematic Review and Meta-AnalysiDocument22 pagesIs Virtual Reality Effective in Orthopedic Rehabilitation A Systematic Review and Meta-AnalysiWalaa EldesoukeyNo ratings yet
- Effects of Nintendo Wii Fit Plus Training On Ankle Strength With Functional Ankle InstabilityDocument5 pagesEffects of Nintendo Wii Fit Plus Training On Ankle Strength With Functional Ankle InstabilityWalaa EldesoukeyNo ratings yet
- Effect of Wii FitTM Exercise Therapy On Gait Parameters in Ankle Sprain Patients A Randomised Controlled TrialDocument23 pagesEffect of Wii FitTM Exercise Therapy On Gait Parameters in Ankle Sprain Patients A Randomised Controlled TrialWalaa EldesoukeyNo ratings yet
- OT Models PratciceDocument30 pagesOT Models PratciceWalaa Eldesoukey100% (1)
- Evaluation of Ankle Instability Using The Biodex Stability SystemDocument6 pagesEvaluation of Ankle Instability Using The Biodex Stability SystemWalaa EldesoukeyNo ratings yet
- Efficacy of Virtual Reality-Based Balance Training Versus The Biodex Balance System Training On The Body Balance of AdultsDocument7 pagesEfficacy of Virtual Reality-Based Balance Training Versus The Biodex Balance System Training On The Body Balance of AdultsWalaa EldesoukeyNo ratings yet
- Review: Is Virtual Reality Effective in Orthopedic Rehabilitation? A Systematic Review and Meta-AnalysisDocument22 pagesReview: Is Virtual Reality Effective in Orthopedic Rehabilitation? A Systematic Review and Meta-AnalysisWalaa EldesoukeyNo ratings yet
- Ankle InstabilityDocument10 pagesAnkle InstabilityWalaa EldesoukeyNo ratings yet
- Orthopedic Manual TherapyDocument56 pagesOrthopedic Manual TherapyWalaa EldesoukeyNo ratings yet
- Appendix A. Fear of Falling Avoidance Behavior QuestionnaireDocument5 pagesAppendix A. Fear of Falling Avoidance Behavior QuestionnaireWalaa EldesoukeyNo ratings yet
- National Academic Reference Standards (NARS) : Physical TherapyDocument19 pagesNational Academic Reference Standards (NARS) : Physical TherapyWalaa EldesoukeyNo ratings yet
- Neck Pain Revision 2017Document83 pagesNeck Pain Revision 2017Iana VieiraNo ratings yet
- Neuromuscular and Nervous System Q OnlyDocument11 pagesNeuromuscular and Nervous System Q OnlyWenzy CruzNo ratings yet
- Curriculum Framework Guidance FINALDocument78 pagesCurriculum Framework Guidance FINALSamuel Iñiguez JiménezNo ratings yet
- Health, Safety and Social Welfare Benefits ReviewerDocument10 pagesHealth, Safety and Social Welfare Benefits ReviewerNovi Mari Noble100% (2)
- Code of Ethical ConductDocument19 pagesCode of Ethical ConductNeha VermaNo ratings yet
- Kmi Profile 2019Document71 pagesKmi Profile 2019VOIIedu成於靈感國際教育No ratings yet
- Tratat de Medicina - Neurologie GifDocument13 pagesTratat de Medicina - Neurologie GifAmi MarcuNo ratings yet
- Marketing Hospital IIPMDocument108 pagesMarketing Hospital IIPMAnil Kumar SinghNo ratings yet
- Professionalism in Physical Therapy: Core Values Bod P05-04-02-03 (Amended BodDocument6 pagesProfessionalism in Physical Therapy: Core Values Bod P05-04-02-03 (Amended BodJay PatelNo ratings yet
- Su4152208medical CertificateDocument4 pagesSu4152208medical CertificateTobias PriceNo ratings yet
- Effect of Kinesio Taping On Knee Symptoms in Patients With HemophiliaDocument10 pagesEffect of Kinesio Taping On Knee Symptoms in Patients With HemophiliaFrankChenNo ratings yet
- NCM 114 Care of The Older Adult Emelie Jalandoni Tan, RN., DnsDocument7 pagesNCM 114 Care of The Older Adult Emelie Jalandoni Tan, RN., DnsPatricia Vasquez100% (4)
- 2017 Anthem GHIP Benefits Booklet (Final)Document119 pages2017 Anthem GHIP Benefits Booklet (Final)Alexander NewberryNo ratings yet
- SH Onishin: Japanese-Style Acupuncture For Pediatric PatientsDocument8 pagesSH Onishin: Japanese-Style Acupuncture For Pediatric Patientsyan92120No ratings yet
- Shoulder Impingement SyndromeDocument21 pagesShoulder Impingement SyndromeivannaOctavianiNo ratings yet
- HiMAS National Trainers' Profile May 2012Document6 pagesHiMAS National Trainers' Profile May 2012Benjie EugenioNo ratings yet
- 320 PDFDocument4 pages320 PDFilona ilincaNo ratings yet
- Horn International University College: Colleege of Health ScienceDocument27 pagesHorn International University College: Colleege of Health Sciencekaise AbdiNo ratings yet
- NCP Multple MyelomaDocument2 pagesNCP Multple Myelomavia macarioNo ratings yet
- Does The Addition of Visceral Manipulation Alter Outcomes For Patients With Low Back Pain? A Randomized Placebo Controlled TrialDocument9 pagesDoes The Addition of Visceral Manipulation Alter Outcomes For Patients With Low Back Pain? A Randomized Placebo Controlled TrialQuiroprácticaParaTodosNo ratings yet
- Scribd Version of The CalendarDocument1 pageScribd Version of The CalendarCEO_OsthéopathieNo ratings yet
- Torii U.S. Army Garrison Japan Weekly Newspaper, Jun. 10, 2010 EditionDocument8 pagesTorii U.S. Army Garrison Japan Weekly Newspaper, Jun. 10, 2010 EditionCamp ZamaNo ratings yet
- Definitions of Quality of Life: What Has Happened and How To Move OnDocument14 pagesDefinitions of Quality of Life: What Has Happened and How To Move OnLeticia Dos SantosNo ratings yet
- Vojta at Cerebra - Org.uk PDFDocument12 pagesVojta at Cerebra - Org.uk PDFGavriela CostachiNo ratings yet
- RPN ResumeDocument2 pagesRPN Resumeapi-353367728No ratings yet
- Between Session Reliability of Four Hop Tests And.40Document8 pagesBetween Session Reliability of Four Hop Tests And.40Jorge Rubio LopezNo ratings yet
- Karen Barker - Developing and Leading An Evidence Based Orthopaedic Physiotherapy ServiceDocument24 pagesKaren Barker - Developing and Leading An Evidence Based Orthopaedic Physiotherapy ServiceManisha KarnaniNo ratings yet
- 2 TAHPI Service PlaningDocument32 pages2 TAHPI Service PlaningMuhammad Ali TariqNo ratings yet
- Assessment of The Visual Status of Older Adults On An Orthopedic UnitDocument7 pagesAssessment of The Visual Status of Older Adults On An Orthopedic UnitSebastian CheungNo ratings yet
- Instant Download Ebook PDF Essentials of Athletic Injury Management 10th Edition PDF ScribdDocument41 pagesInstant Download Ebook PDF Essentials of Athletic Injury Management 10th Edition PDF Scribdjune.thompson131100% (45)