Professional Documents
Culture Documents
Blood Bank Report
Uploaded by
salamon2tOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Blood Bank Report
Uploaded by
salamon2tCopyright:
Available Formats
By :
FAISAL ALMUTAIRI
SAMPLE RECEIVING:
• Plain tube (red cap): SERUM for cross matching
and ICT, Reverse ABO
• EDTA tube ( lavender tube ): whole
blood for ABO, cross matching, DCT
Test in blood bank lab :
• ABO (BLOOD GROUP ) TEST
• Weak D Testing (Du) Testing
• direct coombs test (DCT)
• indirect coombs test (ICT)
• cross matching
• antibody identification
1. ABO (BLOOD GROUP ) TEST
There are four major blood groups and eight different blood types. Doctors call this the ABO
Blood Group System.
https://uc1055decf6fe522be8da6b149ac.dl.dropboxusercon…4mRhDKFVLkuAzhvsrkNqARhU72amtusMHx1alLzXA/file?dl=1 14/07/2019, 2T10 AM
Page 1 of 15
The groups are based on whether or not you have two specific antigens -- A and B:
• Group A has the A antigen and B antibody.
• Group B has the B antigen and the A antibody.
• Group AB has A and B antigens but neither A nor B antibodies.
• Group O doesn’t have A or B antigens but has both A and B antibodies.
There’s also a third kind of antigen called the Rh factor. You either have this antigen (meaning
your blood type is “Rh+” or “positive”), or you don’t (meaning your blood type is “Rh-” or
“negative”). So, from the four blood groups, there are eight blood types:
• A positive or A negative
• B positive or B negative
• AB positive or AB negative
• O positive or O negative
Method to identify ABO grouping:
• Full Automated by machine ( tango machine , ortho autovue)
• Semi-Automated by Gel card
• Manual method by tube method or slide method
A- Full Automated by machine ( tango machine , ortho autovue)
Ortho autovue innova machine :
Principle :
The ORTHO BioVue system column agglutination technology standardizes blood typing
and compatibility testing in a 6-microcolumn cassette preloaded with diluent and/or reagent
and glass beads. Test red cells, with or without serum, are placed in the chamber above the
https://uc1055decf6fe522be8da6b149ac.dl.dropboxusercon…4mRhDKFVLkuAzhvsrkNqARhU72amtusMHx1alLzXA/file?dl=1 14/07/2019, 2T10 AM
Page 2 of 15
column. Upon centrifugation, red cells are forced through the bead column where agglutinated
cells are trapped, while unagglutinated red cells travel to the bottom of the column, forming a
discrete pellet.
B- Semi-Automated by Gel card.
• Prepare cell suspension 200 ul normal saline + 10 ul blood
• Take 10 ul from cell suspension and add to A, B,AB,AND CONTROL
• For Reverse ABO take 10ul from A cell and B cell and 40 ul serum Add to A1 and B1.
• Centrifugation 10 minute
• Read result
Forward Reverse
Ag A Ag B Ag AB A cell B cell
Group A +ve -ve +ve -ve +ve
Group B -ve +ve +ve +ve -ve
Group AB +ve +ve +ve -ve -ve
Group O -ve -ve -ve +ve +ve
C- Manual method by tube method or slide method
• cells Wash three times
• Make cell suspension 3-5 %
• Take four tube for A,B,AB,D add two drops of anti A,B,AB,D and
• two drops of cell suspension
• Centrifugation
• Read result
slide method:
1. On the section of slide labeled anti-A place one drop of antibody A.
2. On the section of slide labeled anti-B place one drop of antibody B.
https://uc1055decf6fe522be8da6b149ac.dl.dropboxusercon…4mRhDKFVLkuAzhvsrkNqARhU72amtusMHx1alLzXA/file?dl=1 14/07/2019, 2T10 AM
Page 3 of 15
3. On the section of slide labeled anti-AB place one drop of antibody AB.
4. On new slide labeled anti-D place one drop of antibody D.
5. Place one drop of cells in each antibody containing circle.
6. Carefully mix each solution with a separate applicator stick.
7. Tilt slowly for one minute, then observe for the agglutination.
Reverse
ABO ;
• Back or reverse
type with A
and B cells
• Commercially
available A
and B cells
are used.
• Patient serum added to the known cells.
• Used as confirmatory for the forward method.
• Reverse should be oppositely forward blood group
A and B cell preparation :
• Take segment from donor bags known blood group A and B
• Add segment to labeled test tube A cell tube and B cell tube
• cells Wash three times
• Make cell suspension
2. Weak D Testing (Du) Testing.
Some red cells possess the D antigen but it is expressed so weakly that the cells are not
agglutinated directly by anti-D sera. An indirect antiglobulin test is necessary to identify
patients with the Weak D (formerly known as Du )phenotype. Weak D testing is done on all
prenatal patients and candidates for Rh immune globulin. Weak D testing is also done on Rh
negative donors to ensure they are truly D negative. It may or may not be done routinely on
Rh negative candidates for transfusion, depending on the policy of the transfusing institution.
If routine weak D testing is done, weak D positive patients should receive Rh positive blood
Procedure of (Du) Testing.
• If the Rh test is negative ?
• Prepare a washed, 3% suspension of patient cells
• In test tube Add one drop of suspension and two drops anti D and two drops bovine albumin
.
• Incubate tube at 37oC for 15 to 30 minutes.
• Wash three time
• Add coombs reagent
• Centrifugation 30 sec
https://uc1055decf6fe522be8da6b149ac.dl.dropboxusercon…4mRhDKFVLkuAzhvsrkNqARhU72amtusMHx1alLzXA/file?dl=1 14/07/2019, 2T10 AM
Page 4 of 15
• Read result under microscopy
• When result positive Rh+
• When result negative add coombs control cells (CCC) and Centrifugation 30 sec
• After add (CCC) result should be positive
• If result negative repeat test
Other blood group systems
❖ The MNSs System
This system was discovered by injecting animals with human red cells. MNSs genes on
chromosome 4.There are two loci: M/N and S/s. The antigens are M, N, S, and s. There are
naturally occurring (IgM) antibodies to all these antigens. Anti-S and anti-s commonly develop
immune characteristics (IgG class) as a result of pregnancy or transfusion.
❖ The Lewis System
This system was focuses on a single locus with two antigens, Le a and Le b. These antigens do
not form an integral part of the red cell membrane, but are soluble antigens which may be present
in body fluids and secretions. They are adsorbed on to the surface of red cells if they are present
in the plasma in sufficient amounts. There are only three phenotypes: Le(a-b-); Le(a+b-); and
Le(a-b+). Lewis phenotypes may change during pregnancy. Examples of Le(a+b+) are only
transient. Lewis antibodies are only found in Le(a-b-) individuals, and are almost entirely IgM.
They are the only Blood group antibodies which have never been implicated in HDN (hemolytic
disease of the newborn.)
❖ The Kell System
In this system there are four antigens at two loci: K (Kell) and k (cellano), and Kpa and Kpb. The
Kp(a+) phenotype and the Kp(a-b-) phenotype are both rare. The Knull phenotype K- k- Kp(a-b-
) is associated with chronic granulomatus disease (CGD), an inherited defect in the bacterial
capacity of neutrophils. Antibodies to Kell system antigens are IgG. Named for the family of the
antibody producer Mrs. Kellacher.
❖ The Lutheran (Lu) System
This system is a single locus system, with antigens Lua and Lub. The Lu(a) negative phenotype
is very rare. Antibodies to Lutheran antigens are IgG. The genes of the Lutheran group are linked
to the genes responsible for the secretion of ABH substances.
❖ The Duffy System
The Duffy system is also a single locus with two antigens, Fy a and Fy b. The only rare
phenotype is Fy(a-b-), which has a higher frequency in countries where there is a high incidence
of Plasmodium falciparium malaria. This phenotype gives a degree of immunity to the disease
because the malarial parasite requires Duffy antigens to enter the red cells. Duffy antibodies are
almost exclusively IgG. This system is named after the family of the antibody producer, Duffy.
❖ The Kidd (Jk) System
Another single locus system, two antigen system (Jka and Jkb). There are four possible
phenotypes: Jk(a-b-); Jk(a+b-); Jk(a-b+); Jk(a+b+). Jk(a-b-) is a rare phenotype. Antibodies to
the Kidd antigens are almost exclusively IgG.
Incompatible transfusion or pregnancy can lead to the formation of antibodies to all these Blood
groups, if the recipient/mother lacks the relevant antigen. It is possible to detect all red cell
antibodies using an antibody detection panel and different detection techniques. (Some
antibodies, usually IgM class, react best at room temperature or cooler, and some work best at 37
degrees entigrade). If an antibody is detected in a serum the red cells from that patient are tested
for the presence of the antigen. Antigen detection techniques also vary according to the nature of
the antibody-antigen interaction. The presence of a particular antibody specifically excludes the
patient from carrying that antigen.
❖ The P System
This system was also discovered by injecting animals with human red cells. P1 is the most
common antigen which has variable strength of expression. Anti-P1 may be naturally occurring.
It is most often an IgM antibody
❖ The I system
This system found on RBC membranes as well as in plasma, milk, and amniotic fluid These
https://uc1055decf6fe522be8da6b149ac.dl.dropboxusercon…4mRhDKFVLkuAzhvsrkNqARhU72amtusMHx1alLzXA/file?dl=1 14/07/2019, 2T10 AM
Page 5 of 15
antigens may be I or I .They form on the precursor chain of RBC Newborns have strong i antigen
and Adults have strong I antigen
3. direct coombs test (DCT)
What is this test?
This test detects immunoglobulin and/or complement bound to red blood cells surface
antigens in vivo.. Immunoglobulin and complement are involved in the immune system. This test
is used to evaluate for antibody-induced hemolysis (destruction of red blood cells)
You may need this test if you have:
• Autoimmune hemolytic anemia
• Cold autoimmune hemolytic anemia
• Hemolytic disease of fetus OR newborn due to ABO immunization
• HUS - Hemolytic uremic syndrome
• Paroxysmal cold hemoglobinuria
• Transfusion reaction due to blood group antibody-antigen mismatch
Procedure of DCT .
• cells Wash three times
• Make cell suspension 3-5 %
• In test tube add one drops from suspension and two drops bovine albumin
• Centrifugation 30 sec
• Read result .when result negative ? keep tube at room temperature for 10 minute
• Centrifugation 30 sec
• When result negative add coombs control cells (CCC) and Centrifugation 30 sec
• After add (CCC) result should be positive
4. Indirect coombs test (ICT)
The indirect Coombs test (also known as the indirect antiglobulin test or IAT) is used to
detect in-vitro antibody-antigen reactions. It is used to detect very low concentrations of
https://uc1055decf6fe522be8da6b149ac.dl.dropboxusercon…4mRhDKFVLkuAzhvsrkNqARhU72amtusMHx1alLzXA/file?dl=1 14/07/2019, 2T10 AM
Page 6 of 15
antibodies present in a patient’s plasma/serum prior to a blood transfusion. In antenatal care, this
test is used to screen pregnant women for antibodies that may cause hemolytic disease of the
newborn. The IAT can also be used for compatibility testing, antibody identification, RBC
phenotyping, and titration studies.
Procedure of ICT .
• Label 3 tubes as cell 1, cell 2 and cell 3.
• In the tube labeled as cell 1, take 2 drops of serum. And 1 drops of cell 1
• In the tube labeled as cell 2, take 2 drops of serum. And 1 drops of cell 2
• In the tube labeled as cell 3, take 2 drops of serum. And 1 drops of cell 3
• Add 2 drops of bovine albumin to each tube.
• Incubate all the tubes at 37°C for 45 – 60 min
• Wash the cells 3 times with normal saline
• Add 2 drops of Anti Human Globulin to each tube
• Centrifugation 30 sec
• When result negative add coombs control cells (CCC) and Centrifugation 30 sec
• After add (CCC) result should be positive
5. Cross Matching (Compatibility test).
Cross Matching is a procedure performed prior to a blood transfusion to determine whether
donor blood is compatible (or incompatible) with recipient blood. Compatibility is determined
through matching of different blood group systems, the most important of which are the ABO
and Rh system, and/or by directly testing for the presence of antibodies against a sample of
donor tissues or blood.
Cross-matching will detect incompatibilities between the donor and recipient that will not be
evident on blood typing. There are two types of cross-matches: Major cross-match and Minor
cross-match.
The major cross match involves testing the patient’s serum with donor cells to determine
whether the patient has an antibody which may cause a hemolytic transfusion reaction or
decreased cell survival of donor cells. This is the most important cross-match.
The minor cross match involves testing the patients cells with donor plasma to determine
https://uc1055decf6fe522be8da6b149ac.dl.dropboxusercon…4mRhDKFVLkuAzhvsrkNqARhU72amtusMHx1alLzXA/file?dl=1 14/07/2019, 2T10 AM
Page 7 of 15
whether there is an antibody in the donor’s plasma directed against an antigen on the patient’s
cells.
• Selection of Appropriate Donor Units.
Red cell compatibility.
It is a general principle that red cell components of identical ABO group and RhD type as the
recipient should be used for transfusion. O Rh negative is the universal red cell donor blood that
can be given to all patients. This is common practice when a patient’s blood group is unknown
and in emergency situations especially for women of child-bearing age.
Plasma compatibility
Plasma contains anti-A and anti-B antibodies depending upon the blood group. Our body also
has antibodies to A and/or B antigens according to our blood group. Patients should only receive
plasma that does not contain an antibody which could attack the antigens present on their own
red cells.
Group A recipients have A antigen on their red cells, so they can’t receive group O or group B
plasma as the anti-A will attack their red cells. Group B recipients have B antigen on their red
cells, so they can’t receive group O or group A plasma as the anti-B will attack their red cells.
Group AB recipients can only receive group AB plasma. Group O recipients do not have either A
or B antigen, so can safely receive plasma of any blood group type.
https://uc1055decf6fe522be8da6b149ac.dl.dropboxusercon…4mRhDKFVLkuAzhvsrkNqARhU72amtusMHx1alLzXA/file?dl=1 14/07/2019, 2T10 AM
Page 8 of 15
Platelet Compatibility
ABO identical platelets are usually preferred. However, in some circumstances, the need for
other special requirements may be more important than providing the same ABO group.
Cross Matching procedure.
Tube method
• Prepare a washed, 3% suspension of donor cell
• Label a test tube. Add two drops from the patient serum and two drops from the
appropriate donor cell suspension.
• Mix the tubes and incubate at 37°C for about 45 minutes.
• Wash the cells 3 times with normal saline
• Add two drops of AHG (Antihuman globulin) and mix.
• Centrifugation 30 sec
• Read macroscopically and microscopically and record the results
• If result compatible “no reaction” add CCC and Centrifugation 30 sec to confirm
your result
• After add (CCC) result should be positive.
Gel card method
• prepare a donor cell suspension 200 ul normal saline + 10 ul blood
• take 40 ul serum and 10 ul donor cell suspension and 50ul Bliss (normal saline)
• incubation for 15 min
• Centrifugation 5-10 min
• Read result
Immediate-spin cross-matching (ISCM)
Immediate-spin cross-matching is an abbreviated form of cross-matching that is faster, less
expensive but also less sensitive. It is an immediate test that combines the patient's serum and
donor's red blood cells at room temperature. No agglutination indicates a negative test reaction,
or compatible match. Indications for ISCM are dependent on the circumstances of the patient and
it can be used in place of a full cross-match or performed as a preliminary test.
6. antibody identification
principle:
Patient serum/plasma is tested against an Identification panel of reagent red cells that are
fully antigrammed for the antigens of the major and minor B.G systems using the same technique
with which Ab detected in screening or cross matching (for eluate from DCT positive cells
additive techniques are held). The positive and negative reactions should be compared with the
panel profile in conjunction with the screening results. Determining the specificity of an
unexpected alloantibody is important in pre-transfusion and prenatal testing. If the antibody
specificity is known, it is possible to test donor blood for the absence of the corresponding
antigen. Antibodies should also be identified in donor blood so that this blood is not transfused to
antigen-positive recipients.
PROCEDURE
The patient's sample should first be tested with Screening Cells I and II. If one or both of these
show agglutination, proceed with the antibody identification.
1. Select a cell panel and the corresponding antigen matrix. Be sure the lot number on the cell
panel matches the lot number on the antigen matrix.
2. Fill in all known patient information on the cell panel worksheet.
3. Number as many tubes as there are cells in the panel. Include the patient's initials on each
tube.
4. Using a controlled drop dispo pipette held at a consistent angle, add 2 drops of patient
https://uc1055decf6fe522be8da6b149ac.dl.dropboxusercon…4mRhDKFVLkuAzhvsrkNqARhU72amtusMHx1alLzXA/file?dl=1 14/07/2019, 2T10 AM
Page 9 of 15
serum to each tube.
5. Gently invert the panel cells several times to resuspend.
6. Add one drop of the appropriate panel cells to each corresponding numbered tube.
7. Set up an autologous control, if none was run with the antibody screen:
8. To a tube labeled with the patient's initials and "auto", add 2 drops patient serum and one
drop of a washed 3% suspension of patient cells.
9. If the Screening Cells were negative at the Immediate Spin phase, proceed directly to step
11. If they were positive at Immediate Spin, centrifuge the tubes the calibrated time for saline
and continue with step 10.
10. Gently resuspend and examine for agglutination using the lighted agglutination viewer.
11. Record all reactions under a column headed IS (for Immediate Spin) on the panel
worksheet.
o
12. Add 2 drops PEG to all tubes, shake to mix, and incubate 10 - 30 minutes at 37 C. Note
that you must incubate at least 15 minutes if using a dry heat block. (or add 2 drops of
LISS & incubate for 15 - 20 min)
13. Wash all tubes three or four times with physiologic saline and add one
drop of Polyspecific Anti-Human Globulin to each tube.
14. Shake to mix and centrifuge the time appropriate to the Coombs spin calibration in
the serofuge (if using gel system).
15. Gently resuspend and examine for agglutination using the lighted agglutination viewer.
16. Record all reactions under a column headed AHG on the panel worksheet.
17. The auto control may be positive or negative. If it is positive, do a DAT and get a recent
transfusion history and medications list.
18. Confirm all negative reactions with Coombs Control Cells. No agglutination after
centrifugation following the addition of Coombs Control Cells invalidates the cell panel
results
Autocontrol.
Patient RBCs + Patient serum
INTERPRETATION
• To determine antibody specificity, use the following protocol:
• Look at each negative cell and cross off all antigens that are present (positive) on that cell.
Use X for homozygous cells, and / for heterozygous cells.
• Eliminate antigens along the top of the cell panel by crossing off all that have been crossed
off at least three times in the antigen matrix, ideally with at least one of them
homozygous for the antigen. Do not eliminate antigens based on only one or two
heterozygous cells crossed off, especially if you are getting different strength reactions on
different cells.
https://uc1055decf6fe522be8da6b149ac.dl.dropboxusercon…4mRhDKFVLkuAzhvsrkNqARhU72amtusMHx1alLzXA/file?dl=1 14/07/2019, 2T10 AM
Page 10 of 15
• Exceptions to the above policy include:
• you may rule out Kell based on 3 heterozygous cells - no need for a homozygous cross-off
• you may rule out low frequency antigens (Cw, V, VS, Kpa, Jsa, Lua) based on only one
cross-off, whether homozygous or heterozygous
• you may also rule out low-frequency antigens if there are no cells positive for them on the
panel
• if anti-D is present, you may rule out anti-C or anti-E based on three heterozygous cells
(r'r for C and r"r for E)
• From the antigens not crossed off, look for a pattern of agglutination matching the pattern
you got in the test. This should identify the antibody specificity.
• At this point there still may be one or more low-frequency antigens not crossed off. If the
cell that has the low-frequency antigen also has the antigen that corresponds to the
antibody you believe you have identified, you may now cross off this low frequency
antigen, because the positive reaction on this cell is most likely due to the antibody you
have identified.
• Often you are unable to rule out the possibility of a second or third antibody because the
corresponding antigens are all present on the same cells. For example, you have
identified Anti-Jka but can't eliminate Anti-Kell because all Kell positive cells are
also Jka positive. Check other cell panels and find 3 other cells that are Kell positive
and Jka negative. A negative result when testing these cells with the patient's serum
eliminates that antibody; a positive result confirms the second antibody.
• When the antibody(ies) have been identified, be sure there are at least 3 cells that are
possess that antigen and give a positive reaction, and at least 3 cells that are lack that
antigen and give a negative reaction. Always check the results of the screening cells. You
may have to test more cells from other panels.
• As a final confirmation of the antibody specificity, if the autocontrol is negative or only
weakly positive, type the patient's cells for the antigen. The result should be negative,
unless the patient has been recently transfused. The result will then be a mixed field.
• If you get different reactions at different phases of testing; if you get different strengths of
reactions on different cells, or if your results don't form a pattern corresponding to one of
the antigens on the matrix, consider multiple antibodies. See (6) above.
• If you get a pattern of reactivity not matching any of the antigens on the matrix, the
antibody may be showing dosage and reacting only with homozygous cells. This is most
often seen in the MNS and Kidd systems, but can be seen in other systems.
Eliminate only the non-reactive homozygous cells; the pattern of reaction may then
match an antigen present only on the remaining homozygous cells.
Confirmation:
Q: how to confirm such a situation?
Sample antibody ID problems
1-A 27-year-old female comes in for a tonsillectomy. She’s never been transfused or pregnant.
The above panel is performed. What is the antibody and what should you do?
https://uc1055decf6fe522be8da6b149ac.dl.dropboxusercon…4mRhDKFVLkuAzhvsrkNqARhU72amtusMHx1alLzXA/file?dl=1 14/07/2019, 2T10 AM
Page 11 of 15
Answers to Panels
1. Anti-Leb
Single cold-reacting antibody. Anti-Leb reacting at these temperatures is not clinically
significant, so no specific interventions will be necessary. You might consider using prewarmed
crossmatches to eliminate the antibody activity.
2-A 19-year-old G3P1Ab1 female comes in at 28 weeks for routine prenatal exam.
2. Anti-D
Note that this is likely a gel or solid-phase panel (though it could be a liquid panel only recording
the IAT reactions). Single warm-reacting antibody. Fairly straight-forward identification. Check
the clinical situation (and don’t forget to ask about recent RhIG injection or infusion!).
3. A 45-year-old male with a myelodysplastic syndrome and history of multiple transfusions.
https://uc1055decf6fe522be8da6b149ac.dl.dropboxusercon…4mRhDKFVLkuAzhvsrkNqARhU72amtusMHx1alLzXA/file?dl=1 14/07/2019, 2T10 AM
Page 12 of 15
3. Anti-K and anti-E
After your cross-offs, no single antibody explains all of the reactions, so you should try to fit two
antibodies (again, this panel only shows IAT results, so no concern about different “phases”
here). Anti-K and anti-E is the best fit. Note the slightly weaker reactions in cell 6 due to dosage.
➢ Preservation and storage of Blood component
Blood Storage Shelf life
component temperature
Red 2–6 Red cells: 42 days
cells ºC Paediatric red cells: 35 days
Washed red cells: 28 days
Platelets 20– 5
24 ºC days
Fresh frozen plasma. At or 12
cryoprecipitate below –25 ºC months
➢ Anticoagulant used in blood bank
https://uc1055decf6fe522be8da6b149ac.dl.dropboxusercon…4mRhDKFVLkuAzhvsrkNqARhU72amtusMHx1alLzXA/file?dl=1 14/07/2019, 2T10 AM
Page 13 of 15
➢ CPD AND CPD-A1
Citrate-phosphate-dextrose (CPD) and citratephosphate-dextrose-dextrose (CP2D). Allows 21
days of RBC/Whole Blood storage.
Citrate-phosphate-dextrose-adenine (CPDA-1) has extra adenine compare to CPD or CP2D as a
source of ATP, which allows 35 days of RBC/Whole Blood storage.
➢ SAGM
SAGM is a combination of constituents as additive solution to give the red cell optimum
viability. It actually stands for
- Sodium Chloride: provides isotonicity
- Adenine: maintains ATP for red cell viability
- Glucose: supports red cell metabolism
- Mannitol: helps reduce red cell lysis
Preservation of red cells in SAGM solution can keep the life of red cells to up to 42 days, longer
than using CPD Solution and CPDA solution alone.
➢ Sample rejection slip
o Specimen hemolyzed
o Specimen clotted
o Quantity not sufficient (QNS)
o Incomplete request form
• No doctor sign or stamp
• No diagnosis
• Test not recommended
o Mismatched file name, number on request and tube
• Specimen unlabeled
https://uc1055decf6fe522be8da6b149ac.dl.dropboxusercon…4mRhDKFVLkuAzhvsrkNqARhU72amtusMHx1alLzXA/file?dl=1 14/07/2019, 2T10 AM
Page 14 of 15
• Specimen mislabeled
• Specimen inadequately labeled
o Wrong collection tube
: ❖ مجهود شخصي
" "كل ما احتاجه دعواتكم... وإن اخطأت فمن نفسي والشيطانF❖ إن أصبت فمن ا
https://uc1055decf6fe522be8da6b149ac.dl.dropboxusercon…4mRhDKFVLkuAzhvsrkNqARhU72amtusMHx1alLzXA/file?dl=1 14/07/2019, 2T10 AM
Page 15 of 15
You might also like
- Essentials of ABO -Rh Grouping and Compatibility Testing: Theoretical Aspects and Practical ApplicationFrom EverandEssentials of ABO -Rh Grouping and Compatibility Testing: Theoretical Aspects and Practical ApplicationRating: 5 out of 5 stars5/5 (1)
- Blood BankDocument20 pagesBlood BankSurendar KesavanNo ratings yet
- Blood Typing and Crossmatching ProceduresDocument11 pagesBlood Typing and Crossmatching ProceduresLecture NotesNo ratings yet
- Blood Banking: Revision PracticalDocument36 pagesBlood Banking: Revision PracticalPeaceNo ratings yet
- Compatibility TestingDocument45 pagesCompatibility TestingkatieNo ratings yet
- BB - Abo Blood Group SystemDocument7 pagesBB - Abo Blood Group SystemWayne VillalunaNo ratings yet
- Blood GroupingDocument84 pagesBlood GroupingUday KolheNo ratings yet
- 1 MK Imunohematologi015Document37 pages1 MK Imunohematologi015Putri Sari WardaniNo ratings yet
- Laboratory ManualDocument17 pagesLaboratory ManualSumaira JunaidNo ratings yet
- Pretransfusion Testing BB Lec FinalsDocument3 pagesPretransfusion Testing BB Lec FinalsAndrei PusungNo ratings yet
- Abo Grouping Cell and Serum GroupingDocument33 pagesAbo Grouping Cell and Serum GroupingArslan ArshadNo ratings yet
- PDF 5Document25 pagesPDF 5Dhruv Raj 9 B 24100% (1)
- CCN Midterm SkillsDocument37 pagesCCN Midterm SkillsSTEFFANIE VALE BORJANo ratings yet
- PDF 4Document26 pagesPDF 4Dhruv Raj 9 B 24No ratings yet
- Blood BankDocument77 pagesBlood BankSandeep PoudelNo ratings yet
- ABO Grouping.....Document9 pagesABO Grouping.....phisantelaboratoryNo ratings yet
- ImmunologyDocument12 pagesImmunologyNoven Brix DeguitNo ratings yet
- Blood Bank TypingDocument34 pagesBlood Bank TypingSkylarNo ratings yet
- ABO and D Typing-1 PDFDocument16 pagesABO and D Typing-1 PDFmarneabdNo ratings yet
- HEMATOTRANSFUSDocument164 pagesHEMATOTRANSFUSJoe2805No ratings yet
- Week 9 Slide Agglutination TestDocument14 pagesWeek 9 Slide Agglutination TestJae TNo ratings yet
- Clinical Blood TransfusionDocument13 pagesClinical Blood TransfusionAdeniran CharlesNo ratings yet
- Reagent Red Blood Cells IH Cell I II III IH Cell I II IH Cell PoolDocument5 pagesReagent Red Blood Cells IH Cell I II III IH Cell I II IH Cell PoolAbdullahNo ratings yet
- Compatibility Testing - BloodDocument5 pagesCompatibility Testing - BloodMunish DograNo ratings yet
- Blood GroupingDocument27 pagesBlood Groupingcontact.elsen31No ratings yet
- Blood GroupingDocument16 pagesBlood Groupinglubna aloshibiNo ratings yet
- 6BBK Lec6 - Blood Group Serology MQA 2019-09-26 08-14-44Document26 pages6BBK Lec6 - Blood Group Serology MQA 2019-09-26 08-14-44gothai sivapragasamNo ratings yet
- ABO Forward and Reverse Tube MethodDocument4 pagesABO Forward and Reverse Tube Method''Rochelle Mylene ﭢ Ygoña100% (1)
- Blood Grouping TecheniquesDocument19 pagesBlood Grouping TecheniquesLIBIN PALLUPPETTAYIL JOSE93% (15)
- Compatibility TestingDocument70 pagesCompatibility TestingHazel100% (1)
- Blood Typing PresentationDocument39 pagesBlood Typing PresentationNezzeh Clair D. BermejoNo ratings yet
- Blood Bank - Pretransfusion Compatibility TestingDocument4 pagesBlood Bank - Pretransfusion Compatibility TestingWayne VillalunaNo ratings yet
- 5 IhDocument61 pages5 IhGennelyn Ross Delos Reyes0% (1)
- ASCP Review Course: Review Questions: Blood Banking and Transfusion MedicineDocument18 pagesASCP Review Course: Review Questions: Blood Banking and Transfusion MedicineMarl EstradaNo ratings yet
- Blood Group Compatbility TestDocument46 pagesBlood Group Compatbility TestArslan ArshadNo ratings yet
- ABO and RH Blood Group SystemDocument31 pagesABO and RH Blood Group SystemKaab Ishaq100% (1)
- Kursus IH ABO GROUPING v19082015 PDFDocument84 pagesKursus IH ABO GROUPING v19082015 PDFIlyasHasanNo ratings yet
- Abo and MN Blood Group SystemDocument54 pagesAbo and MN Blood Group SystemAkram chaudaryNo ratings yet
- 4 IhDocument59 pages4 IhGennelyn Ross Delos ReyesNo ratings yet
- Blood Typing Worksheet - KFDocument2 pagesBlood Typing Worksheet - KFfrommeyerjamesNo ratings yet
- Type & Screen: What Does The Blood Bank Do With That Tube?Document25 pagesType & Screen: What Does The Blood Bank Do With That Tube?mue1010No ratings yet
- ABO and RH Blood Typing: AB ActsDocument4 pagesABO and RH Blood Typing: AB ActsRaja SharmaNo ratings yet
- Blood Blank 1 PDFDocument6 pagesBlood Blank 1 PDFRajkumar RoderickNo ratings yet
- AABB 2021 Blood Bank Fundamentals Course SBB/BB Exam Review: Supplemental HandoutDocument51 pagesAABB 2021 Blood Bank Fundamentals Course SBB/BB Exam Review: Supplemental HandoutDyne Sabijon100% (1)
- MLAB 2361 Clinical II Immunohematology Assignment Activity 6: ABO Discrepancies Case StudiesDocument7 pagesMLAB 2361 Clinical II Immunohematology Assignment Activity 6: ABO Discrepancies Case Studiespikachu0% (1)
- BMS 201 (Lab) : Blood Grouping and Transfusion: Noha Nooh Lasheen Associate Professor of PhysiologyDocument25 pagesBMS 201 (Lab) : Blood Grouping and Transfusion: Noha Nooh Lasheen Associate Professor of PhysiologyRowaa SamehNo ratings yet
- Transfusion of Apheresis Platelets and Abo Groups 2005Document15 pagesTransfusion of Apheresis Platelets and Abo Groups 2005my accountNo ratings yet
- Pretransfusion or Compatibility Testing: NotesDocument7 pagesPretransfusion or Compatibility Testing: NotesABHINABA GUPTANo ratings yet
- Blood TX & Bone MarrowDocument12 pagesBlood TX & Bone Marrowqueen TinaNo ratings yet
- ABO Blood GroupDocument42 pagesABO Blood Groupjong188No ratings yet
- Blood GroupingDocument47 pagesBlood Groupinggacruz1010No ratings yet
- ABO Discrepancies - RahulDocument47 pagesABO Discrepancies - RahulNyxa AbdullaNo ratings yet
- Immunohematology-Lab MidtermsDocument9 pagesImmunohematology-Lab MidtermsRachel PlanillaNo ratings yet
- Blood Bank ProceduresDocument33 pagesBlood Bank Procedures99noname100% (1)
- Antibody PanelDocument5 pagesAntibody PanelCarl Dominic GasconNo ratings yet
- Blood Grouping and RH TypingDocument4 pagesBlood Grouping and RH TypingJeevs MusicNo ratings yet
- Blood Group SystemDocument33 pagesBlood Group SystemAJETUNMOBI IBRAHEEM AYODEJINo ratings yet
- Applied Immunology Practical 2 Um BiomedDocument16 pagesApplied Immunology Practical 2 Um Biomedkiedd_04100% (1)
- خطة الكوارث الداخلية FinalDocument25 pagesخطة الكوارث الداخلية Finalsalamon2tNo ratings yet
- Neonatal BilirubinDocument5 pagesNeonatal Bilirubinsalamon2tNo ratings yet
- HIV Point of Care Test (INSTI ™) Quality Control Log: PHSA LaboratoriesDocument1 pageHIV Point of Care Test (INSTI ™) Quality Control Log: PHSA Laboratoriessalamon2tNo ratings yet
- Procedure Manual Test Name: Wet Mounts/KOH Preps Method or PrincipleDocument3 pagesProcedure Manual Test Name: Wet Mounts/KOH Preps Method or Principlesalamon2tNo ratings yet
- Pediatric Reference Ranges Endocrinology 0981 PDFDocument14 pagesPediatric Reference Ranges Endocrinology 0981 PDFMMCSTORENo ratings yet
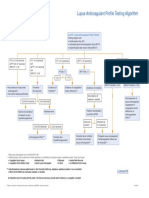
- Lupus Anticoagulant Profile Testing AlgorithmDocument1 pageLupus Anticoagulant Profile Testing Algorithmsalamon2tNo ratings yet
- Parallel Testing and Implementing New QC MaterialDocument14 pagesParallel Testing and Implementing New QC Materialsalamon2tNo ratings yet
- Blank 12Document15 pagesBlank 12salamon2tNo ratings yet
- Kidney Disease Acute and Chronic 2019Document60 pagesKidney Disease Acute and Chronic 2019salamon2tNo ratings yet
- Insturoments Maintenance 2Document6 pagesInsturoments Maintenance 2salamon2tNo ratings yet
- C-Peptide to Glucose Ratio as a Marker of β Cell FunctionDocument9 pagesC-Peptide to Glucose Ratio as a Marker of β Cell Functionsalamon2tNo ratings yet
- Bio-Rad A1C: For Hba, Hba and HBFDocument4 pagesBio-Rad A1C: For Hba, Hba and HBFsalamon2tNo ratings yet
- Equipment Maintenance Log Template 06Document1 pageEquipment Maintenance Log Template 06salamon2tNo ratings yet
- Bio-Rad A1C: For Hba, Hba and HBFDocument4 pagesBio-Rad A1C: For Hba, Hba and HBFsalamon2tNo ratings yet
- Lecciones Basicas en Control de Calidad.2008 Bio-Rad InglesDocument62 pagesLecciones Basicas en Control de Calidad.2008 Bio-Rad InglesPili Gabriel67% (3)
- The Most Advanced Electrolyte AnalyzerDocument2 pagesThe Most Advanced Electrolyte Analyzersalamon2tNo ratings yet
- Laboratory Specimen Collection Guidelines: Ministry of National Guard Health AffairsDocument40 pagesLaboratory Specimen Collection Guidelines: Ministry of National Guard Health Affairssalamon2tNo ratings yet
- QualitativeQC Paulo Pereira SampleDocument62 pagesQualitativeQC Paulo Pereira Samplesalamon2tNo ratings yet
- In The Name of God FG: ABO Discrepancy ABO DiscrepancyDocument27 pagesIn The Name of God FG: ABO Discrepancy ABO Discrepancysalamon2tNo ratings yet
- Transaction ReceiptDocument1 pageTransaction Receiptsalamon2tNo ratings yet
- Practical Bacteriology Laboratory Manual: Prepared byDocument37 pagesPractical Bacteriology Laboratory Manual: Prepared bysalamon2tNo ratings yet
- Customer Service: Pipettes Tips Tubes & Plastics Lab Equipment Accessories Calibration & RepairDocument22 pagesCustomer Service: Pipettes Tips Tubes & Plastics Lab Equipment Accessories Calibration & Repairsalamon2tNo ratings yet
- Pregnant Healthcare Personnel - Infection Prevention For Occupational Health - Table of Contents - APICDocument35 pagesPregnant Healthcare Personnel - Infection Prevention For Occupational Health - Table of Contents - APICsalamon2tNo ratings yet
- Neisseria Meningitidis - Healthcare-Associated Pathogens and Diseases - Table of Contents - APICDocument17 pagesNeisseria Meningitidis - Healthcare-Associated Pathogens and Diseases - Table of Contents - APICsalamon2tNo ratings yet
- Sexually Transmitted Diseases - Healthcare-Associated Pathogens and Diseases - Table of Contents - APICDocument73 pagesSexually Transmitted Diseases - Healthcare-Associated Pathogens and Diseases - Table of Contents - APICsalamon2tNo ratings yet
- Nutrition Services - Infection Prevention For Support Services and The Care Environment - Table of Contents - APICDocument48 pagesNutrition Services - Infection Prevention For Support Services and The Care Environment - Table of Contents - APICsalamon2tNo ratings yet
- Sterile Processing - Infection Prevention For Support Services and The Care Environment - Table of Contents - APICDocument74 pagesSterile Processing - Infection Prevention For Support Services and The Care Environment - Table of Contents - APICsalamon2tNo ratings yet
- Immunization of Healthcare Personnel - Infection Prevention For Occupational Health - Table of Contents - APICDocument98 pagesImmunization of Healthcare Personnel - Infection Prevention For Occupational Health - Table of Contents - APICsalamon2tNo ratings yet
- Waste Management - Infection Prevention For Support Services and The Care Environment - Table of Contents - APICDocument35 pagesWaste Management - Infection Prevention For Support Services and The Care Environment - Table of Contents - APICsalamon2tNo ratings yet
- Scheuermanns DiseaseDocument26 pagesScheuermanns DiseaseMihnea VulpeNo ratings yet
- Multiple Organ Dysfunction Syndrome: HistoryDocument6 pagesMultiple Organ Dysfunction Syndrome: HistoryJasmine BaduaNo ratings yet
- Risk Assessment Envirn Mad Cow Disease-2Document9 pagesRisk Assessment Envirn Mad Cow Disease-2api-436969344No ratings yet
- Pediatric Case 9: Charlie Snow (Core) : Guided Reflection QuestionsDocument3 pagesPediatric Case 9: Charlie Snow (Core) : Guided Reflection QuestionsDai NguyenNo ratings yet
- ENDOMETRIOSISDocument33 pagesENDOMETRIOSISpriyanka bhowmikNo ratings yet
- Ayushi SinghDocument2 pagesAyushi SinghAayushi SinghNo ratings yet
- Bells Palsy Handbook Facial Nerve Palsy or Bells Palsy Facial Paralysis Causes, Symptoms, Treatment, Face Exercises ... (Alan MC Donald DR Alexa Smith) (Z-Library)Document94 pagesBells Palsy Handbook Facial Nerve Palsy or Bells Palsy Facial Paralysis Causes, Symptoms, Treatment, Face Exercises ... (Alan MC Donald DR Alexa Smith) (Z-Library)mayakhoNo ratings yet
- Stages of Gingival InflammationDocument13 pagesStages of Gingival Inflammationvisi thiriyanNo ratings yet
- Nursing Care Plan: Cues Objectives Interventions Rationale EvaluationDocument1 pageNursing Care Plan: Cues Objectives Interventions Rationale EvaluationAkiraMamoNo ratings yet
- What Is High Blood PressureDocument2 pagesWhat Is High Blood PressureTariqNo ratings yet
- Zabrina Joana DDocument4 pagesZabrina Joana DEmman BalidoNo ratings yet
- Water Deprivation TestDocument7 pagesWater Deprivation Testsanham100% (2)
- BioFire BrochureDocument3 pagesBioFire BrochureETNo ratings yet
- Immunologic and Allergic DiseaseDocument49 pagesImmunologic and Allergic DiseaseFidz LiankoNo ratings yet
- Case Presentation SiliconomaDocument24 pagesCase Presentation Siliconomaentgo8282No ratings yet
- Ultraformer Info After CareDocument2 pagesUltraformer Info After CareFruity FruitcakeNo ratings yet
- Jonathan C. Lubag Unintentional Injuries Q3M1 W1-3Document26 pagesJonathan C. Lubag Unintentional Injuries Q3M1 W1-3Jonathan LubagNo ratings yet
- Non Invasive Diagnostic Instruments: By. Kailash - Pandey Aditya - MayekarDocument32 pagesNon Invasive Diagnostic Instruments: By. Kailash - Pandey Aditya - MayekarkrupalithakkerNo ratings yet
- Memorandum: Rule 198 of WBSR, PTDocument2 pagesMemorandum: Rule 198 of WBSR, PTMd. Sahir KhanNo ratings yet
- PSYC 210 Abnormal Psychology: Introduction To Psychology (PSYC 101) or Equivalent Is Strongly Recommended. StudentsDocument8 pagesPSYC 210 Abnormal Psychology: Introduction To Psychology (PSYC 101) or Equivalent Is Strongly Recommended. StudentsAriadne MangondatoNo ratings yet
- How We Conquered SmallpoxDocument4 pagesHow We Conquered SmallpoxNadir BaghdadNo ratings yet
- Trastuzumab MonographDocument11 pagesTrastuzumab MonographAmeliaNo ratings yet
- A Case Report On Symptomatic Primary Herpetic Gingivostomatitis (New)Document4 pagesA Case Report On Symptomatic Primary Herpetic Gingivostomatitis (New)Annisa MardhatillahNo ratings yet
- (Hepatoportoenterostomy) : Anna M. Banc-Husu, MDDocument1 page(Hepatoportoenterostomy) : Anna M. Banc-Husu, MDwatimelawatiNo ratings yet
- NCP Proper CholecystectomyDocument2 pagesNCP Proper CholecystectomyGail Lian SantosNo ratings yet
- Afib NCPDocument3 pagesAfib NCPGen RodriguezNo ratings yet
- Obsessive-Compulsive Disorder SectionDocument19 pagesObsessive-Compulsive Disorder Sectionark1974No ratings yet
- Defense Medical Epidemiology Database Report - Jan 26, 2022Document41 pagesDefense Medical Epidemiology Database Report - Jan 26, 2022adan_infowars100% (2)
- Health Certificate: Personal Details: Section ADocument3 pagesHealth Certificate: Personal Details: Section APrashob SugathanNo ratings yet
- 16 OdtDocument2 pages16 OdtKHYATI PARMARNo ratings yet