Professional Documents
Culture Documents
Previous Editions Are All Available At: WWW - Paediatricpearls.co - Uk
Uploaded by
RaoulSusanto Susanto0 ratings0% found this document useful (0 votes)
17 views1 pageOriginal Title
August-2015
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
17 views1 pagePrevious Editions Are All Available At: WWW - Paediatricpearls.co - Uk
Uploaded by
RaoulSusanto SusantoCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 1
Paediatric Pearls
August 2015
Put together by: Dr Julia Thomson, Consultant Paediatrician, julia.thomson@bartshealth.nhs.uk
Previous editions are all available at www.paediatricpearls.co.uk
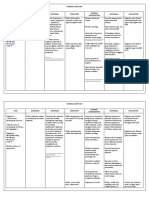
Henoch Schönlein purpura (HSP)
a disease involving inflammation of small blood vessels
cause unknown but probably an abnormal immune response
to a viral or bacterial infection
most commonly occurs in children aged 2-11 (M>F)
if adults get it, disease is usually more severe than in children
inflammation leaky blood vessels in the skin, intestines,
kidneys (and rarely in heart, lungs and brain). The main
symptom is a purpuric rash classically over the legs or buttocks.
patients also get joint pain (in 75% of cases and usually only
lasts a few days), abdominal pain (risk of intussusception (2-3%
incidence)) and haematuria (50% get nephritis which needs
monitoring as 5% go on to get progressive kidney disease).
lasts 4-6 weeks - sometimes with recurrence of symptoms
(about one third), but usually with no long-term consequences
if kidneys and/or intestines are affected, treatment with
steroids may be (rarely) needed
paracetamol and ibuprofen are appropriate for management
of joint pain
see algorithm for follow up recommendations:
no proteinuria? for blood pressure checking and urinalysis at
days 7 and 14 and at 1, 3, 6 and 12 months
with proteinuria, follow-up should be at days 7 and 14, monthly
from 1-6 months and then at 12 months
more information at
http://patient.info/doctor/henoch-
schonlein-purpura-pro
good parent information leaflet:
http://kidshealth.org/parent/medical/h
eart/hsp.html
Bronchiolitis in children. NICE guidelines [NG9]
Reference: Published date: June 2015
E J Tizard and M J J Hamilton-Ayres Henoch−Schönlein purpura Arch Dis Child Educ Pract Ed 2008 93: 1-8
The bronchiolitis season will soon be upon us again
here in the UK. I have summarised Assessment and
Dr Locke’s dermatology slot: Think “PVL” in young, ENT with Mr Sunil diagnosis, When to refer/admit here. Part 2 of this
healthy people with recurrent and painful spots/red areas Sharma topic on Management and Discharge next month.
on the skin (boils, folliculitis, carbuncles, cellulitis), often at Paediatric acute
multiple sites which can persist despite appropriate Mastoiditis Assessment and diagnosis
antibiotic treatment. The affected area is often more Picture taken from occurs in children < 2 years of age, most commonly
painful than the size of the lesion would suggest. http://emedicine.medscape.com
Mastoiditis = inflammation of mastoid air cells < 1 year, peaking around 3 - 6 months
/article/966099-clinical#b2
(fairly common)
Panton-Valentine Leukocidin (PVL) is a toxin produced symptoms usually peak day 3-5: 1-3 day coryzal
Mastoiditis = acute inflammation of mastoid air
by some strains of Staphylococcus aureus (PVL-SA) cells (fairly common) prodrome, persistent cough (resolves in 90% by 3
PVL can be produced by MSSA (methicillin sensitive) However, clinical presentation of acute mastoiditis weeks), respiratory distress, wheeze and/or crackles
(ENT emergency) is when there is pus in the on auscultation
and MRSA (methicillin resistant) mastoid cavity secondary to an acute otitis media
PVL-SA usually causes pyogenic skin infections e.g. boils only 30% have a fever and it is usually < 39°C
Acute mastoiditis less common now with the
and abscesses, but can also cause invasive disease such as advent of antibiotic treatment for otitis media (consider a diagnosis of pneumonia if the fever is high
(AOM). Usually occurs in children <2yrs of age or there are persistently focal crackles
osteomyelitis, and should be suspected with:
due to immature immune system viral induced wheeze is a differential in older infants
- recurrent boils, folliculitis or cellulitis
- clustering of skin infections within a household or social group Most common bacterial causes: Strep. (multiple recurrent episodes? Family history of
- necrotic skin infections pneumoniae, followed by Haemophilus influenzae atopy?). Asthma is not normally diagnosed in infants.
and Strep. pyogenes poor feeding (typically after 3 to 5 days of illness).
PVL-SA infections spread more easily among close contact Signs and symptoms: Babies < 6 weeks of age may present with apnoea
communities, such as families, nurseries and care homes, ® Recent AOM ® Fever without other clinical signs
but also can be identified in gym groups or those playing ® Unilateral otalgia ® Hearing loss
® Non-specific symptoms (poor feeding,
close contact sports irritability) When to refer (1o care) / admit (2o care):
Clear summary of clinical features, investigations, and treatment at ® Bulging erythematous tympanic membrane Immediately if apnoea, child looks seriously unwell,
https://www.gov.uk/government/uploads/system/uploads/attachment_data/ ® Tender, erythematous, swollen post auricular
file/391168/PVL_guidance_in_primary_care_quick_reference_guide.pdf region, leading to protusion of auricle
severe respiratory distress (RR > 70bpm, grunting,
® Loss of postauricular skin crease (see picture) severe recession, cyanosed), persistent O2
British Association of Dermatologists patient information leaflet:
http://www.bad.org.uk/shared/get-file.ashx?id=179&itemtype=document
® Sagging of posterior superior canal wall saturations < 92% in air (measure if correct paediatric
Management: Refer urgently to ENT (some can equipment and training available)
Public Health England advice on how to use the decolonisation treatments:
http://www.iph.cam.ac.uk/files/2014/03/C20-PVL-SA-decolonisation-
be managed medically with IV antibiotics but Consider referral/admission if:
factsheet-Jun-2013.pdf
some will need incision and drainage of abscess + respiratory rate (RR) > 60 breaths/minute
cortical mastoidectomy and grommet insertion).
Reference (Royal College of Nursing, a more informative document): If untreated, can lead to facial nerve palsy, ,
inadequate oral fluid intake (50–75% of usual
https://www.rcn.org.uk/__data/assets/pdf_file/0008/400787/004128.pdf Bezold abscess (a deep abscess in the soft tissues volume) +/- clinical dehydration
Pictures? See the PCDS article on folliculitis and boils: of the neck), labyrinthitis, petrositis leading to take following risk factors for severe bronchiolitis
http://www.pcds.org.uk/clinical-guidance/folliculitis-an-overview Gradenigo syndrome (triad of abducens nerve into account: chronic lung disease, congenital heart
palsy, deep facial pain from trigeminal nerve disease, age < 3 months), premature birth < 32/40,
involvement, and suppurative otitis media),
intracranial complications. neuromuscular disorders, immunodeficiency
Last month I mentioned some services for families struggling with addiction and
Excellent review paper on the topic - Glynn F, Osman L,
consider other factors: social circumstances, skill
substance abuse. Lifeline Waltham Forest is a free, safe and confidential drug
and alcohol service for any adult over the age of 18 using any kind of drug or Colreavy M, Rowley H, Dwyer TP, Blayney A. Acute and confidence of the carer, distance to healthcare in
mastoiditis in children: presentation and long term case of deterioration
alcohol and living in the London Borough of Waltham Forest. Parenting support consequences. J Laryngol Otol 2008 122(3):233-7.
offered. URL: www.lifelinewalthamforest.org.uk or click here for flyer.
You might also like
- Abpmr Moc100Document43 pagesAbpmr Moc100Zeeshan Siddiqui100% (4)
- (Nelsons 21st) Acute GastroenteritisDocument21 pages(Nelsons 21st) Acute GastroenteritisLara Patricia TamsiNo ratings yet
- GEC 103 Week 8 Activity and Home StudyDocument6 pagesGEC 103 Week 8 Activity and Home StudyLorenz Joy Ogatis BertoNo ratings yet
- Clinical Review - FullDocument6 pagesClinical Review - FullKevinTevesYupanquiNo ratings yet
- Peptic Ulcer and Other Conditions of The Stomach: EpidemiologyDocument11 pagesPeptic Ulcer and Other Conditions of The Stomach: Epidemiologynarulitta rianNo ratings yet
- Antireflux Surgery Lich-GregoirDocument16 pagesAntireflux Surgery Lich-GregoircristiangelsNo ratings yet
- Acute Infectious Diarrhea in Children: Continuing Medical EducationDocument11 pagesAcute Infectious Diarrhea in Children: Continuing Medical EducationkhorikNo ratings yet
- Neutering Is Not Associated With Early-Onset Urethral Obstruction in CatsDocument7 pagesNeutering Is Not Associated With Early-Onset Urethral Obstruction in CatsRifia FaniNo ratings yet
- Maldonado 2013Document33 pagesMaldonado 2013martin najeraNo ratings yet
- p1319 PDFDocument4 pagesp1319 PDFSyairodhiNo ratings yet
- Lay Language GlossaryDocument16 pagesLay Language GlossaryqubiivanNo ratings yet
- Kitten WholeDocument5 pagesKitten WholeAlexander GintingNo ratings yet
- Chronic Pelvic PainDocument18 pagesChronic Pelvic PainWilliam Alfonso Parada VecinoNo ratings yet
- CELLE DismenorreaDocument7 pagesCELLE DismenorreaJose Vergara GNo ratings yet
- Reye S SyndromDocument6 pagesReye S SyndromVlada SpatarNo ratings yet
- Cognitive and Psychopathological Aspects of Ehlers DanlosDocument5 pagesCognitive and Psychopathological Aspects of Ehlers DanlosKarel GuevaraNo ratings yet
- Dysphagia in Older AdultsDocument10 pagesDysphagia in Older Adultsconstanza duran cordovaNo ratings yet
- Ijerph 18 04787Document14 pagesIjerph 18 04787Bruno FernandesNo ratings yet
- Peptic Ulcer in Children 1995Document11 pagesPeptic Ulcer in Children 1995kadekapiklestariNo ratings yet
- Gout Obat HosppharmDocument8 pagesGout Obat HosppharmnandaNo ratings yet
- The Laboratory Diagnosis of Feline Kidney DiseaseDocument7 pagesThe Laboratory Diagnosis of Feline Kidney DiseaseCabinet VeterinarNo ratings yet
- ManagementDocument9 pagesManagementanka_mihaelaNo ratings yet
- IsbelDocument7 pagesIsbelCaity YoungNo ratings yet
- Clinical Practice Diagnosis and Management of HenoDocument9 pagesClinical Practice Diagnosis and Management of HenoHosne araNo ratings yet
- VaricoceleDocument6 pagesVaricoceleHemylle Suzane - MEDNo ratings yet
- Managing Psoriasis in The Elderly: Dermatology 19Document4 pagesManaging Psoriasis in The Elderly: Dermatology 19septinNo ratings yet
- Jama 268 6 030Document6 pagesJama 268 6 030Thiago Scharth MontenegroNo ratings yet
- Diagnosis of Pancreatitis in Dogs and Cats: ReviewDocument14 pagesDiagnosis of Pancreatitis in Dogs and Cats: ReviewMiruna ChiriacNo ratings yet
- DS - Mod9Document2 pagesDS - Mod9designericlelynsoronioNo ratings yet
- PottDocument2 pagesPottkimNo ratings yet
- My Approach To Interstitial Lung Disease Usingclinical, Radiological and Histopathological PatternsDocument15 pagesMy Approach To Interstitial Lung Disease Usingclinical, Radiological and Histopathological PatternsMarcelle FreireNo ratings yet
- Jurnal Rheumatoid Arthritis - 6 PDFDocument4 pagesJurnal Rheumatoid Arthritis - 6 PDFJeanstepanisaragihNo ratings yet
- 571 FullDocument2 pages571 FullJauhari JoNo ratings yet
- Neurodegeneration and Medicinal Mushroom PDFDocument5 pagesNeurodegeneration and Medicinal Mushroom PDFjason farmanNo ratings yet
- Dunkel 2012Document2 pagesDunkel 2012Claudia LópezNo ratings yet
- Hirschsprung's Disease: (Congenital Aganglionic Megacolon)Document16 pagesHirschsprung's Disease: (Congenital Aganglionic Megacolon)umiNo ratings yet
- Etanercept in Psoriasis: The Evidence of Its Therapeutic ImpactDocument12 pagesEtanercept in Psoriasis: The Evidence of Its Therapeutic ImpactArlha DebintaNo ratings yet
- Women With Epilepsy: Clinically Relevant Issues: A B C D, E, FDocument8 pagesWomen With Epilepsy: Clinically Relevant Issues: A B C D, E, FAnum SasmitaNo ratings yet
- Rheumatoid ArthritisDocument11 pagesRheumatoid Arthritismelinda tannousNo ratings yet
- Predictive Homeopathy Course Review, Part I: Susanne Saltzman, MDDocument5 pagesPredictive Homeopathy Course Review, Part I: Susanne Saltzman, MDdr TotoNo ratings yet
- España Boulevard, Sampaloc, Manila, Philippines 1015 Tel. No. 406-1611 Loc. 8241 Telefax: 731-5738 Website: WWW - Ust.edu - PHDocument4 pagesEspaña Boulevard, Sampaloc, Manila, Philippines 1015 Tel. No. 406-1611 Loc. 8241 Telefax: 731-5738 Website: WWW - Ust.edu - PHsteffiNo ratings yet
- Sample Chapter 9780323399562Document23 pagesSample Chapter 9780323399562TaeyomiNo ratings yet
- Vomiting: Compendium (Yardley, PA) February 2009Document10 pagesVomiting: Compendium (Yardley, PA) February 2009Vini SasmitaNo ratings yet
- Recurrent Seizures in Cats: 1. Diagnostic Approach - When Is It Idiopathic Epilepsy?Document13 pagesRecurrent Seizures in Cats: 1. Diagnostic Approach - When Is It Idiopathic Epilepsy?Rifia FaniNo ratings yet
- Ibs JurnalDocument11 pagesIbs JurnalimuhammadfahmiNo ratings yet
- Systemic Lupus ErythematosusDocument28 pagesSystemic Lupus ErythematosusLuiz Fernando Alves FerreiraNo ratings yet
- Clinical Features of Benign Paroxysmal Positional VertigoDocument5 pagesClinical Features of Benign Paroxysmal Positional VertigoEko SaputraNo ratings yet
- Post2018 Neuroprogressao TBDocument2 pagesPost2018 Neuroprogressao TBJoão Paulo AtidioNo ratings yet
- Abdominopelvic Pain Syndromes - CeaDocument6 pagesAbdominopelvic Pain Syndromes - CeaLucas CabreraNo ratings yet
- Pertussis Not Only A Disease of ChildhoodDocument7 pagesPertussis Not Only A Disease of ChildhoodRiris Arizka Wahyu KumalaNo ratings yet
- Diagnosis and Management of Polymyalgia Rheumatica: Clinical IntelligenceDocument2 pagesDiagnosis and Management of Polymyalgia Rheumatica: Clinical IntelligenceAbdulAzizNo ratings yet
- Polyneuropathy: ClinicalDocument33 pagesPolyneuropathy: ClinicalIzabella MihályNo ratings yet
- Sensory Processing Issues in Young Children.10Document5 pagesSensory Processing Issues in Young Children.10Itala Campos NeryNo ratings yet
- Evaluation of ConstipationDocument8 pagesEvaluation of ConstipationAndrea GallegoNo ratings yet
- Management of Prosthetic Valve Endocarditis: A Clinical ChallengeDocument2 pagesManagement of Prosthetic Valve Endocarditis: A Clinical Challengedr yasminNo ratings yet
- Nepharites Lesson PlanDocument21 pagesNepharites Lesson Plansaritha Oruganti100% (1)
- p778 PDFDocument11 pagesp778 PDFThivyaroobiniNo ratings yet
- Advancements and Updates in The Field of EnuresisDocument7 pagesAdvancements and Updates in The Field of EnuresisMOHAMED ABDİKADİR KENYNo ratings yet
- Nursing Management Protocol For Mothers of Children Having Ventricular Peritoneal ShuntDocument9 pagesNursing Management Protocol For Mothers of Children Having Ventricular Peritoneal ShuntZikrina RamadhaniNo ratings yet
- Natural History and Spectrum of DiseaseDocument3 pagesNatural History and Spectrum of DiseaseEvans MogakaNo ratings yet
- 14 - Fertilization To Implantation-MbbsDocument52 pages14 - Fertilization To Implantation-MbbsRaoulSusanto SusantoNo ratings yet
- Endocrinology: Version 2 (2020)Document89 pagesEndocrinology: Version 2 (2020)RaoulSusanto SusantoNo ratings yet
- 3RD To 8TH Week (I)Document31 pages3RD To 8TH Week (I)RaoulSusanto SusantoNo ratings yet
- Adult Invig Inf TableDocument6 pagesAdult Invig Inf TableRaoulSusanto SusantoNo ratings yet
- 187 FullDocument8 pages187 FullRaoulSusanto SusantoNo ratings yet
- Plasma Cell DisordersDocument20 pagesPlasma Cell Disordersalihos93No ratings yet
- Algorithm 1: Initial Evaluation and Management: Symptoms of Possible ACSDocument6 pagesAlgorithm 1: Initial Evaluation and Management: Symptoms of Possible ACSNenyNo ratings yet
- Document PDFDocument17 pagesDocument PDFlilisNo ratings yet
- American Medical Association - ICD-10-CM Documentation - Essential Charting Guidance To Support Medical Necessity 2019-American Medical Association (2018)Document1,229 pagesAmerican Medical Association - ICD-10-CM Documentation - Essential Charting Guidance To Support Medical Necessity 2019-American Medical Association (2018)johnharnsberryNo ratings yet
- BPH PpsDocument26 pagesBPH PpsDita Putri ShafiraNo ratings yet
- Matriks EkstraselulerDocument75 pagesMatriks EkstraselulerRenaldy PamungkasNo ratings yet
- A Case of Patient AI, Who Came in Due To Sore ThroatDocument16 pagesA Case of Patient AI, Who Came in Due To Sore ThroatLovelle LopezNo ratings yet
- AMOEBADocument74 pagesAMOEBAhuyenthanh1807No ratings yet
- Drug Study For VaccinesDocument6 pagesDrug Study For VaccinesMarion RebolledoNo ratings yet
- Depression in Older Adults: A Treatable Medical ConditionDocument12 pagesDepression in Older Adults: A Treatable Medical ConditionJose Alonso Aguilar Valera100% (1)
- Lec 8 Ulcerative Vesicular & Bullous LesionsDocument6 pagesLec 8 Ulcerative Vesicular & Bullous LesionsAbd 9961No ratings yet
- Carpal Tunnel SyndromeDocument13 pagesCarpal Tunnel SyndromeMmaNo ratings yet
- ArchRheumatol 32 21Document5 pagesArchRheumatol 32 21indriNo ratings yet
- NBDHE Board Review 2013 Oral Pathology Flashcards - QuizletDocument15 pagesNBDHE Board Review 2013 Oral Pathology Flashcards - QuizletDENTAL REVIEWER ONLY100% (1)
- Post-Traumatic Subarachnoid Hemorrhage: A ReviewDocument8 pagesPost-Traumatic Subarachnoid Hemorrhage: A ReviewdeslitaNo ratings yet
- Oncovet 2008Document18 pagesOncovet 2008Frederico VelascoNo ratings yet
- I. INTRODUCTION Cesarean Section Is A SurgicalDocument62 pagesI. INTRODUCTION Cesarean Section Is A SurgicalLuis R. Dela Cruz86% (7)
- The Blue BookDocument53 pagesThe Blue BookTammy BoudNo ratings yet
- NCP Karl Jacon M. FerolinoDocument4 pagesNCP Karl Jacon M. FerolinoWhyng CabugayanNo ratings yet
- Noac Prescribing Tips For NoacsDocument4 pagesNoac Prescribing Tips For NoacsBudiono WijayaNo ratings yet
- Autoimmune DiseasesDocument14 pagesAutoimmune Diseasesdr_swaralipiNo ratings yet
- Crion NeuritisDocument9 pagesCrion NeuritisffffffffffnnvNo ratings yet
- Surgical Anatomy of Salivary GlandsDocument41 pagesSurgical Anatomy of Salivary GlandsBikram Choudhury100% (1)
- Crohn Vs ColitisDocument5 pagesCrohn Vs Colitiswbarnes7No ratings yet
- LithiumDocument4 pagesLithiumapi-3797941100% (1)
- Shake It OffDocument106 pagesShake It OffViolet VioletNo ratings yet
- Orthopedic One Liners Mci ImpDocument15 pagesOrthopedic One Liners Mci ImpadiNo ratings yet
- Unit SHC21 From The Level 2 Diploma in Health and Social Care Candidate HandbookDocument33 pagesUnit SHC21 From The Level 2 Diploma in Health and Social Care Candidate HandbookVaso Te AmargoNo ratings yet
- Autoimmune Autonomic GanglionopathyDocument14 pagesAutoimmune Autonomic Ganglionopathyveerraju tvNo ratings yet