Professional Documents
Culture Documents
Early Mobility in The Intensive Care Unit Standard Equipment VS A Mobility Platform
Uploaded by
Bapak Sunaryo SPBUOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Early Mobility in The Intensive Care Unit Standard Equipment VS A Mobility Platform
Uploaded by
Bapak Sunaryo SPBUCopyright:
Available Formats
Early Mobility in Critical Care
E MOBILITY IN THE
ARLY
INTENSIVE CARE UNIT:
STANDARD EQUIPMENT VS
A MOBILITY PLATFORM
By Melanie Roberts, MS, APRN, CCRN, CCNS, Laura Adele Johnson, RN, BSN, CCRN,
and Trent L. Lalonde, PhD
Background Despite the general belief that mobility and exercise
play an important role in the recovery of functional status, mobil-
ity is difficult to implement in patients in intensive care units.
Objectives To compare a mobility platform with standard
equipment, assessing efficiency (decreased time and staff
required to prepare patient), effectiveness (increased activity
time), and safety (no falls, unplanned tube removals, or emer-
gency situations) for intensive care patients.
Methods This observational study was approved by the insti-
tutional review board, and informed consent was obtained
from the patient or the medical decision maker. Intensive care
patients were assigned to a room in the usual manner, with
platforms in odd-numbered rooms and standard equipment in
even-numbered rooms. Standardized data collection tools
were designed to collect data for 24 hours for each patient.
The nurses caring for the patients completed the data collec-
tion tools in real time during the activity. The stages of activity
and the physiological states that would preclude mobility were
very specifically defined for the research study.
Results Data were collected for a total of 71 patients and 238
activities. Important (although not significant) descriptive sta-
tistics regarding early mobility in the intensive care unit were
discovered. The unintended result of the research study was a
change in the culture and practice regarding early mobility in
the intensive care unit.
EBR
Evidence-Based Review on pp 458-459
Conclusions Early mobility can be implemented in intensive
care units. Standard equipment can be used to mobilize such
patients safely; however, for patients who ambulate, a plat-
form may increase efficiency and effectiveness. (American
©2014 American Association of Critical-Care Nurses Journal of Critical Care. 2014;23:451-457)
doi: http://dx.doi.org/10.4037/ajcc2014878
www.ajcconline.org AMERICAN JOURNAL OF CRITICAL CARE, November 2014, Volume 23, No. 6 451
Downloaded from http://ajcc.aacnjournals.org/ by AACN on September 1, 2019
D
espite the general belief that mobility and exercise play an important role in
the recovery of functional status, mobility is difficult to implement in patients
in intensive care units (ICUs). Several studies1-4 in the past 2 decades have
documented the outcomes of early mobility in critical care. Early and frequent
mobilization of ICU patients decreases hospital length of stay, ICU length
of stay, and ventilator days.1-4 Common critical care complications, neuromuscular weakness,
deconditioning, and delirium are decreased with early mobility.2,5-8 Morris et al9 demonstrated
that the lack of early mobility therapy in ICUs was 1 of the 4 variables associated with readmis-
sion or death during the first year for ICU survivors of acute respiratory failure.
Hospitals nationwide are attempting to develop Methods
mobility programs, but actualizing the goal is diffi- Setting
cult. Lack of resources, a lack of established proto- The study was completed at Medical Center of
cols, and staff resistance prevent many facilities the Rockies, a 136-bed nonprofit, tertiary care hos-
from implementing a successful mobility program.10 pital. Clinical areas involved in the research study
Numerous articles exist indicating the importance included a 12-bed cardiac/cardiovascular surgery ICU
of mobilization; however, little detail can be found (CICU) and a 12-bed surgical/trauma ICU (SICU).
to explain how to implement a successful mobility Mobility stages had been implemented in the ICUs
program. Published reports demon- before the study but were not integrated into practice.
Lack of early strate the importance of mobility A research protocol was designed to identify human
protocols in determining individual resources required for early mobility in the ICU, to
mobility is patients’ appropriateness for mobil- compare standard equipment with a platform, and
ity and to define progression of
associated with mobility, but few such protocols
to validate the safety of the protocol.
readmission to the have been published.11 Sample
The culture of the ICU must be The study included all intensive care patients
intensive care unit addressed early in any initiative to who were at least 18 years old and spoke English.
or death during implement a mobility program. Critical care patients are a vulnerable population of
Successful implementation of early patients; many are unable to make decisions because
the first year. mobility requires a change in ICU of cognitive impairment from medications and criti-
culture, nurses’ personal percep- cal illness. To protect the patients, informed consent
tions, and teamwork.10 This article describes how a was obtained from individual patients if their results
community-based hospital developed a mobility on the Confusion Assessment Method12 were nor-
program despite limited resources and changed the mal and the patient was not receiving any sedatives
culture of the ICU to accept the challenge of mobi- or pain medication. If the patient did not meet
lizing patients. both criteria, the patient’s medical decision maker
provided consent. Consent was obtained by spe-
cially trained ICU nurses at an appropriate time
after the patient had been admitted to the ICU,
About the Authors depending on the patient’s condition and planned
Melanie Roberts is a critical care Clinical Nurse Specialist mobility. For planned ICU admissions, consent was
at Medical Center of the Rockies in Loveland, Colorado. obtained before admission.
Laura Adele Johnson is a student registered nurse anes-
thetist at Westminster College in Salt Lake City, Utah. Data were collected for 4 months, with a total
Trent L. Lalonde is an associate professor of applied sta- of 71 patients enrolled in the study and 238 total
tistics at the University of Northern Colorado and a sta- mobility events. Of the 71 patients, 26 (37%) were
tistical consultant at the Medical Center of the Rockies.
female with a mean age of 66.00 (SD, 19.76) years,
Corresponding author: Melanie Roberts, MS, APRN, CCRN,
CCNS, Medical Center of the Rockies, 2500 Rocky Mountain
whereas the 45 males (63%) had a mean age of 68.62
Avenue, Loveland, CO 80538 (e-mail: Melanie.Roberts@ (SD, 12.43) years. A total of 49 patients (69%) were
uchealth.org). in the CICU and 22 (31%) were in the SICU. The
452 AJCC AMERICAN JOURNAL OF CRITICAL CARE, November 2014, Volume 23, No. 6 www.ajcconline.org
Downloaded from http://ajcc.aacnjournals.org/ by AACN on September 1, 2019
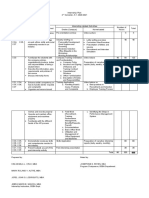
Table 1
Stages of mobility
CICU patients consisted of 15 females (31%) and 34 Stage Activity Research requirement
males (69%), with a mean age of 69.79 (SD, 12.37)
years. The platform was assigned to 23 (47%) of 1 Bed in chair position Not part of the research study
the CICU patients. The SICU patients consisted of 2 Dangle legs at edge of bed Minimum 2 min
11 females (50%) and 11 (50%) males, with a mean
3 Stand upright, weight bearing Minimum 1 min
age of 62.91 (SD, 20.24) years. The platform was
assigned to 12 (55%) of the SICU patients. 4 Chair, stand, pivot/march Minimum 15 min in chair
5 Ambulate Minimum 10 ft (3 m)
Design
A prospective, randomized, controlled, observa-
tional research study was designed to compare a to reeducate themselves on the equipment and the
platform with standard equipment for ICU patients. data collection tool as needed before data collection.
The research hypothesis stated expected improvements During the 2 weeks before the study, the nurses
in efficiency, effectiveness, and safety of ICU mobil- were given instructions by physical therapists on
ity when the platform was used rather than standard the proper method for assisting a patient out of bed
equipment. Effectiveness is defined as the duration to the chair and getting the patient back to bed
of activity performed by the patient. Efficiency is using a gait belt to promote staff and patient safety.
defined as the time to prepare the patient for The data collection sheets were gathered weekly
mobility as well as the number of staff required to and correlated with informed consent. If consent
assist the patient with the activity. Safety is defined had been obtained, the data sheets were entered
by the number of falls or unplanned tube removals. into a data spreadsheet. If consent had not been
The standard equipment used for the study obtained, the data collection sheet was shredded
includes a gait belt, no-slip socks, a walker, and a The ICU nurses determined that it was easier to
wheelchair if the patient was ambulating. The plat- collect the data sheets every day for all patients to
form is a mobile support device that consolidates avoid bias created by their knowledge of who was
equipment (intravenous poles, multiple hooks for enrolled in the study. The nurses were using a mobil-
drainage bags, and a secure location for oxygen) ity protocol with which they were familiar except
into a small area. The patient still requires a gait for the addition of the platform. The mobility pro-
belt and no-slip socks for safety. The design of the tocol used had 5 stages (Table 1), with specific
platform is to allow mobility with the assistance of definitions given for each stage. ICU nurses were
fewer staff. All patients were monitored, had oxy- responsible for determining whether it was safe for
gen, and if the patient was receiving mechanical the patient to mobilize. The expec-
ventilation, a respiratory therapist had to be part tation of the ICU nurse is to use
of the mobility team. the absolute exclusion criteria and Mobility was
The study was approved by the organization’s relative contraindications to deter- defined as
institutional review board. Platforms were placed in mine the patient’s ability to mobi-
odd-numbered rooms. Patients were admitted to lize. Patients start the protocol after purposeful
rooms by the usual process. Data were collected by 24 hours unless they meet 1 of the
the ICU nurses during the activity session, and time exclusion criteria.
movement with
was documented to the nearest minute. Standard- The absolute exclusion criteria the patient’s
ized data collection sheets were used to ensure that are based on the patient’s physiolog-
all appropriate information was recorded. The fol- ical condition: intracranial monitor, participation.
lowing information was collected for each activity: unstable pelvic or spinal fractures,
date, time of day, preparation time (minutes), physician’s order for deep sedation, therapeutic
activity time (minutes), type of activity (chair, dan- hypothermia, vasoactive medication titration, active
gle, stand or march in place, walk), number of staff bleeding, intra-aortic balloon pump or ventricular
required, frequency of activities per patient per day, assist device, comatose, open abdomen, and traction.
and unplanned tube removals or falls. Each patient Relative contraindications such as vasoactive infusions
had a data collection sheet for each day, starting at or changes in respiratory status or vital signs are deter-
midnight with the new ICU flow sheet. Before the mined by the nurse caring for the patient.
beginning of the study, the nurses had 2 weeks to Stage 1 activity, bed in chair position, would not
practice with the platform as well as the data collec- be included in the research study as mobility. Before
tion sheets to ensure that the data collection process the research study, the ICU had determined that
would work as expected. This process allowed nurses mobility would be defined as purposeful movement
www.ajcconline.org AJCC AMERICAN JOURNAL OF CRITICAL CARE, November 2014, Volume 23, No. 6 453
Downloaded from http://ajcc.aacnjournals.org/ by AACN on September 1, 2019
Table 2
Sample size of activities (n) for number of staff,
by activity type
To assess the impact of the platform on activity
No. of staff time, preparation time, number of staff, falls, and
Activity 0 1 2 3 4 5 Total unintended tube removals (endotracheal, gastric,
urinary, chest, and drains), means and standard
Platform deviations are reported for both treatments, by type
Chair 0 9 27 8 1 1 46
Dangle 0 2 14 11 4 0 31
of activity. To evaluate the significance of the dif-
Stand/march 1 2 8 9 3 1 24 ferences in mean activity time, preparation time,
Walk 2 4 9 4 0 0 19 number of staff, falls, and unintended tube removals
Total 3 17 58 32 8 2 120 between treatments, a mixed Poisson log-linear count
Standard regression model is applied.13 This model will account
Chair 0 10 44 8 1 0 63 for the skewness inherent in the strictly positive
Dangle 0 0 17 9 1 2 29 data observed (activity and preparation times; staff,
Stand/march 0 3 8 1 0 0 12
fall, and tube removal counts). The model is mixed
Walk 0 4 6 4 0 0 14
Total 0 17 75 22 2 2 118 with a normal random effect to account for repeated
observation of patients. The independent variables
included are treatment (platform/standard) and
type of activity, along with an interaction between
the 2 variables. Analyses were performed by using
Table 3
Activity time, preparation time, and number of SAS version 9.3.
staff by activity type
Mean (SD)
Results
No unintended tube removals or falls were
Variable Platform Standard
recorded, so safety is not addressed further. The data
Activity time, min set included 118 observations of standard activities
Chair 79.07 (68.53) 62.56 (49.30) and 120 observations of platform activities. Table 2
Dangle 8.97 (4.09) 12.20 (7.40) provides descriptive statistics of the activities observed
Stand/march 9.31 (5.39) 19.64 (20.48) for both treatments. The table shows the number of
Walk 39.53 (36.80) 31.25 (40.63)
activities according to the number of staff required,
Total 39.51 (54.05) 41.87 (45.03)
by activity type.
Preparation time, min Activities involved between 0 and 5 staff, with
4.85 (4.51) 3.75 (2.81)
Chair
5.00 (3.39) 4.60 (3.39) 2 staff the most common (133 activities with 2
Dangle
4.39 (2.97) 3.00 (4.22) staff). The type of staff was not included in the study.
Stand/march
3.95 (3.34) 6.31 (5.50)
Walk The ICU nurse is responsible for determining if
4.65 (3.75) 4.17 (3.55)
Total the patient is safe for mobility and to ensure that
No. of staff 2.08 (0.81) 2.00 (0.60) mobility occurs. Of the 238 activities, 60 involved
Chair 2.55 (0.81) 2.59 (0.87) a dangle, 109 progressed to the chair, 38 involved
Dangle 2.58 (1.10) 1.83 (0.58) standing/marching in place, and 33 involved walk-
Stand/march 1.79 (0.92) 2.00 (0.78)
ing. The number of stand/walk activities was greater
Walk 2.26 (0.93) 2.13 (0.73)
Total for the platform (24 activities) than for standard
equipment (12 activities). Similarly, the number
of walking activities was greater for the platform
with the patient’s participation. Bed in chair posi- (19 activities) than for standard equipment (14
tion did not require patients to use their muscles or activities).
actively participate. This stage is a safety check to To assess the effectiveness of the platform,
see if the patient can tolerate mobility without sig- means and standard deviations of activity times by
nificant changes in their vital signs. type of activity, for both treatments, are reported in
Table 3. Both treatments showed large amounts of
Statistical Analysis variation in activity time. Although the standard
Analysis includes a description of the activities equipment showed longer mean activity times for a
observed. The total numbers of activities (activity dangle or a stand/march in place, the mean activity
sample size) for both treatments are reported. Activ- times for a walk was greater for platform patients
ity sample size is further classified according to the (39.53 minutes) than for standard patients (31.25
type of activity and the number of staff required for minutes). Thus the platform may be more effective
each activity. in terms of activity time when patients walk. Using
454 AJCC AMERICAN JOURNAL OF CRITICAL CARE, November 2014, Volume 23, No. 6 www.ajcconline.org
Downloaded from http://ajcc.aacnjournals.org/ by AACN on September 1, 2019
a mixed Poisson count regression (MPCR) model, and workflow in the ICU. The study did not show
accounting for repeated observation of patients and any significantly improved efficiency, effectiveness,
controlling for the effect of different activity types, or safety with the platform compared with standard
no significant difference was found in mean activity equipment, proving to ICU nurses that they can mobi-
time between the platform and standard treatments lize ICU patients with the equipment they have avail-
(P = .62). able. New equipment may be less efficient for the
To assess the efficiency of the platform in terms nurses to use than equipment with which they are
of time, means and standard deviations of prepara- familiar. That possibility, coupled with the low sam-
tion times by type of activity, for both treatments, ple size, could have affected statistical significance.
are reported in Table 3. Although the standard equip- The preparation for the research study provided
ment showed faster preparation times for a sit, dan- training to the ICU nurses in using gait belts to assist
gle, or stand/march, the mean preparation time with mobilizing patients out of bed, thus improving
was shorter for platform patients (3.95 minutes) safety for both staff and patients. The safety check-
than for standard patients (6.31 minutes) who walk. list provided for the nurses to use before activity to
Therefore, the platform may be more efficient in ensure a standard process during the research study
terms of preparation time with patients who walk. could be used in other mobility protocols.
Using another MPCR model, no significant differ- The study validated that the mobility protocol
ence was found in mean activity time between the is safe; there were no falls, unplanned tube removals,
platform and standard treatments (P = .19). or emergency events. Two other studies15,16 report
To assess the efficiency of the platform in terms similar results, an unplanned tube removal rate of
of staff, means and standard deviations of number 0.8% in 1 study,15 and 1 unplanned
of staff by type of activity, for both treatments, are tube removal and no falls in a dif-
reported in Table 3. Use of the platform allowed 3 ferent study of 75 patients.16 Allow- Activity time did
patients to be active without the help of any staff ing the nurses to prove that the not differ signifi-
(1 stand/march, 2 walk), whereas no standard mobility protocol was safe had a
patients were active without the help of any staff. huge impact in changing the cul- cantly between
For patients involved in walking, use of the plat- ture of the ICU. In order to change
form allowed fewer staff to be involved on average culture, the nurses’ perceptions and
the platform
(1.79) than was possible with standard treatment teamwork must be addressed. Dur- and standard
(2.00). This result suggests that the platform may be ing the research study, the nurses
more efficient in terms of required staff with had the opportunity to change their equipment.
patients who walk and in terms of encouraging perception as they witnessed suc-
individual activity. Using another MPCR model, a cessful mobility. A study done by Thomsen et al17 in
marginally significant difference was found in mean 2008 illustrated the importance of culture; the
activity time between the platform and standard strongest predictor of a patient ambulating was the
treatments (P = .08), with the platform showing ICU to which they were admitted. Patients admitted
lower mean staff expected after the differences in to the respiratory ICU, where mobility is a key clini-
mean staff across activity types were accounted for. cal intervention, had a statistically significant increase
in ambulation. Mobilizing ICU patients is demand-
Discussion ing: the ICU nurses must be committed to coordi-
Although the study findings were not statistically nation of care and teamwork. The nurses need to
significant, several very important descriptive statis- see the connection between mobilizing their ICU
tics were discovered. No information documenting patients and the patients’ outcomes.
the resources required to mobilize ICU patients has The research study allowed the ICU nurses to
been published; this study documents the human test the protocol, determine it was safe, define how
resources needed. Most of the time, 2 staff members they would implement the practice, and ultimately
were required to mobilize the patient, with a prepa- to see the difference it made for their patients. Six
ration time of 5 minutes. The most frequent activity months before the research study, the mobility
is getting up and into the chair, and the patient protocol used in the research study had been
stays up approximately 40 minutes. implemented in the ICU; however, practice had
Mobilizing patients to the chair was also the not changed. The goal of the research study was to
most frequent activity in a study conducted by compare equipment needs for mobility, but the
Bourdin et al14 published in 2010. Nurses can use unintended result of the study was a change in the
this information when planning a mobility program individual nurses’ perceptions and beliefs regarding
www.ajcconline.org AJCC AMERICAN JOURNAL OF CRITICAL CARE, November 2014, Volume 23, No. 6 455
Downloaded from http://ajcc.aacnjournals.org/ by AACN on September 1, 2019
mobility. It is unclear what part of the research study as well as recent publications that early mobil-
process created this change: increased education, ity is both safe and feasible. Actualizing a mobility
changes in equipment, the rigor of a research study, protocol does require interruption in sedation or
or a combination of factors. The net result was an nonsedated ICU patients, so that the patient can
improvement in mobility of ICU patients. Although participate. Further research is needed to determine
not reported as part of this research study but tracked the optimal amount of activity for ICU patients.
for quality purposes, the percentage of patients who
FINANCIAL DISCLOSURES
are mobilized in the ICUs has increased fourfold. None reported.
Similar results were found in a study published by
Drolet et al18: implementation of a nurse-driven
protocol increased ambulation of ICU patients from eLetters
Now that you’ve read the article, create or contribute to an
6.2% to 20.2%, and even bigger increases were seen online discussion on this topic. Visit www.ajcconline.org
in the intermediate unit. The nurses proved to them- and click “Responses” in the second column of either the
full-text or PDF view of the article.
selves the value of early mobility and the value of
bedside research in changing clinical practice. It has
changed the culture not just with mobility but also REFERENCES
1. Bailey P, Thomsen GE, Spuhler VJ, et al. Early activity is
with sedation. Patients have to be awake to partici- feasible and safe in respiratory failure patients. Crit Care
pate in mobility. Numerous recently published Med. 2007;35(1):139-145. doi: 10.1097/01.CCM.0000251130
.69568.87
studies5,19-24 have documented the value of lighter 2. Needham DM, Korupolu R, Zanni JM, et al. Early physical
sedation of patients undergoing mechanical ventila- medicine and rehabilitation for patients with acute respira-
tory failure: a quality improvement project. Arch Phys Med
tion. This experience has empowered the nurses to Rehabil. 2010;91:536-542. doi:10.1016/j.apmr.2010.01.002.
make other decisions about changing their practice 3. Schweickert WD, Pohlman MC, Pohlman AS, et al. Early
physical and occupational therapy in mechanically ventilated,
to improve patient care. critically ill patients: a randomized controlled trial. Lancet.
2009;373:1874-1882. doi:10.1016/S0140-6736(09)60658-9.
4. Winkelman C, Johnson KD, Hejal R, et al. Examining the
Limitations and Strengths positive effects of exercise in intubated adults in ICU: a
Our study had several limitations. It was a sin- prospective repeated measure clinical study. Intensive Crit
Care Nurs. 2012;28:307-320.
gle-site study; however, both medical and surgical 5. Morandi A, Brummel NE, Ely EW. Sedation, delirium and
patients were included in the sample. The study mechanical ventilation: the ‘ABCDE’ approach. Curr Opin
Crit Care. 2011;17:43-49.
lacked a sample size large enough to establish sta- doi:10.1097/MCC.0b013e3283427243.
tistical significance, but the number was adequate 6. Morris PE. Moving our critically ill patients: mobility barriers
and benefits. Crit Care Clin. 2007;23(1):1-14. doi:10.1016
for descriptive statistics. The activity times of selected /j.ccc.2006.11.003.
patients varied, reducing the power of associated 7. Needham DM. Mobilizing patients in the intensive care
unit: improving neuromuscular weakness and physical
tests. Mobility was not correlated with severity of function. JAMA. 2008;300(14):1685-1690. doi:10.1001/jama
illness, use of mechanical ventilation, or sedation .300.14.1685.
8. Truong AD, Fan E, Brower RG, Needham DM. Bench-to-
levels. The sample includes patients receiving mechan- bedside review: mobilizing patients in the intensive care
ical ventilation and patients who were not. Results unit: from pathophysiology to clinical trials. Crit Care
Forum. 2009;13:216-224. doi:10.1186/cc7885.
are not stratified on the basis of severity of illness, 9. Morris PE, Griffin L, Berry M, et al. Receiving early mobility
mechanical ventilation, or sedation levels. Adding during an ICU admission is a predictor of improved outcomes
in acute respiratory failure. Am J Med Sci. 2011;341(5):
this information to future studies would be impor- 373-377. doi:10.1097/MAJ.0b013e31820ab4f6.
tant for ICU practice. The study did not address 10. Bailey PP, Miller RR, Clemmer TP. Culture of early mobility
in mechanically ventilated patients. Crit Care Med. 2009;37:
evaluation of patients’ participation or effort. The S429-S435. doi:10.1097/CCM.0b013e3181b6e227.
scope of the study did not include collection of data 11. Zomorodi M, Topley D, McAnaw M. Developing a mobility
protocol for early mobilization of patients in a surgical/
regarding readmission or post-ICU outcomes. The trauma ICU. Crit Care Res Pract. 2012:1-10. doi:10.1155/2012
study results were not correlated with ICU length /964547.
12. Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP,
of stay, days of mechanical ventilation, delirium Horwitz RI. Clarifying confusion: the confusion assessment
rates, or hospital length of stay. These outcomes are method—a new method for detection of delirium. Ann
Intern Med. 1990;113(12):941-948.
already well established in published reports, so our 13. Lee Y, Nelder JA, Pawitan Y. Generalized Linear Models With
limited resources were not used for this correlation. Random Effects. Boca Raton, FL: Chapman & Hall/CRC:2006.
14. Bourdin G, Barbier J, Burle J-F. The feasibility of early
physical activity in intensive care unit patients: a prospec-
Conclusion tive observational one-center study. Respir Care. 2010;55(4):
400-407.
Conducting the mobility research study promoted 15. Pohlman MC, Schweichert WD, Pohlman AS, et al. Feasibil-
both earlier initiation and progression of mobility ity of physical and occupational therapy beginning from
initiation of mechanical ventilation. Crit Care Med. 2010;
in the ICU. The study demonstrated that a nurse- 38(11):2089-2094. doi:10.1097/CCM.0b013e3181f270c3.
driven protocol can be effective. It is clear from this 16. Winkelman C, Johnson KD, Hejal R, et al. Examining the
456 AJCC AMERICAN JOURNAL OF CRITICAL CARE, November 2014, Volume 23, No. 6 www.ajcconline.org
Downloaded from http://ajcc.aacnjournals.org/ by AACN on September 1, 2019
positive effects of exercise in intubated adults in ICU: a 22. Barr J, Gilles FL, Puntillo K, et al. Clinical practice guidelines
prospective repeated measures clinical study. Intensive for the management of pain, agitation, and delirium in
Crit Care Nurs. 2012;28:307-320. adult patients in the intensive care unit. Crit Care Med.
17. Thomsen GE, Snow GL, Rodriquez L, Hopkins RO. Patients 2013;41:263-306. doi:10.1097/CCM.0b013e3182783b72.
with respiratory failure increase ambulation after transfer 23. Skrobik Y, Ahern S, Leblanc M, et al. Protocolized intensive
to an intensive care unit where early activity is a priority. care unit management of analgesia, sedation, and delirium
Crit Care Med. 2008;36(4):1119-1124. improves analgesia and subsyndromal delirium rates.
18. Drolet A, Dejuilio P, Harkless S, et al. Move to improve: the Anesth Analg. 2010;111(2):451-463.
feasibility of using an early mobility protocol to increase 24. Salgado DR, Favory R, Goulart M, Brimiolle S, Vincent JL.
ambulation in the intensive and intermediate care setting. Toward less sedation in the intensive care unit: a prospec-
Phys Ther J. 2012;93(2). doi:10.2522/ptj.20110400. tive observational study. J Crit Care. 2011;26(2):113-121.
19. Kress JP. Sedation and mobility: changing the paradigm. doi:10.1016/j.jcrc.2010.11.003.
Crit Care Clin. 2013;29:67-75. doi:10.1016/j.ccc.2012.10.001.
20. Strom T, Martinussen T, Toft P. A protocol of no sedation
for critically ill patients receiving mechanical ventilation: a
randomized controlled trial. Lancet. 2010;375(9713):475-480.
21. Girard TD, Kress JP, Fuchs BD, et al. Efficacy and safety of To purchase electronic or print reprints, contact the
a paired sedation and ventilator weaning protocol for American Association of Critical-Care Nurses, 101
mechanically ventilated patients in intensive care (awaken- Columbia, Aliso Viejo, CA 92656. Phone, (800) 899-1712
ing and breathing controlled trial): a randomized controlled or (949) 362-2050 (ext 532); fax, (949) 362-2049; e-mail,
trial. Lancet. 2008;371(9607):126-134. reprints@aacn.org.
www.ajcconline.org AJCC AMERICAN JOURNAL OF CRITICAL CARE, November 2014, Volume 23, No. 6 457
Downloaded from http://ajcc.aacnjournals.org/ by AACN on September 1, 2019
Early Mobility in the Intensive Care Unit: Standard Equipment vs a Mobility Platform
Melanie Roberts, Laura Adele Johnson and Trent L. Lalonde
Am J Crit Care 2014;23 451-457 10.4037/ajcc2014878
©2014 American Association of Critical-Care Nurses
Published online http://ajcc.aacnjournals.org/
Personal use only. For copyright permission information:
http://ajcc.aacnjournals.org/cgi/external_ref?link_type=PERMISSIONDIRECT
Subscription Information
http://ajcc.aacnjournals.org/subscriptions/
Information for authors
http://ajcc.aacnjournals.org/misc/ifora.xhtml
Submit a manuscript
http://www.editorialmanager.com/ajcc
Email alerts
http://ajcc.aacnjournals.org/subscriptions/etoc.xhtml
The American Journal of Critical Care is an official peer-reviewed journal of the American Association of Critical-Care Nurses
(AACN) published bimonthly by AACN, 101 Columbia, Aliso Viejo, CA 92656. Telephone: (800) 899-1712, (949) 362-2050, ext.
532. Fax: (949) 362-2049. Copyright ©2016 by AACN. All rights reserved.
Downloaded from http://ajcc.aacnjournals.org/ by AACN on September 1, 2019
You might also like
- Early Mobilisation in Intensive Care During Renal Replacement TherapyDocument6 pagesEarly Mobilisation in Intensive Care During Renal Replacement TherapyPERALTA MONTILLA LAURANo ratings yet
- Escala PermeDocument9 pagesEscala PermeMileniNo ratings yet
- JBM 2018051810335812Document7 pagesJBM 2018051810335812ARUN VNo ratings yet
- LS 1134 Rev A Early Mobility and Walking Program PDFDocument10 pagesLS 1134 Rev A Early Mobility and Walking Program PDFYANNo ratings yet
- Early Mobilization in The ICU: A Collaborative, Integrated ApproachDocument8 pagesEarly Mobilization in The ICU: A Collaborative, Integrated ApproachJohn LemonNo ratings yet
- Alarms in The Icu: A Study Investigating How Icu Nurses Respond To Clinical Alarms For Patient Safety in A Selected Hospital in Kwazulu-Natal Province, South AfricaDocument6 pagesAlarms in The Icu: A Study Investigating How Icu Nurses Respond To Clinical Alarms For Patient Safety in A Selected Hospital in Kwazulu-Natal Province, South AfricaPASANTIA UAONo ratings yet
- Barriers and Facilitators To Early Mobilisation in Intensive Care A Qualitative StudyDocument6 pagesBarriers and Facilitators To Early Mobilisation in Intensive Care A Qualitative StudyNatalia Tabares EcheverriNo ratings yet
- 436 2003 1 PBDocument7 pages436 2003 1 PBPASANTIA UAONo ratings yet
- Aorn 12423Document14 pagesAorn 12423Ghassan KhairallahNo ratings yet
- ICU Without WallDocument6 pagesICU Without WallFahmi AuliaNo ratings yet
- Evaluating A Case Study Using Bloom's Taxonomy of Education: ASE TudyDocument10 pagesEvaluating A Case Study Using Bloom's Taxonomy of Education: ASE TudyAli RaufNo ratings yet
- ICU Registered Nurses 3Document9 pagesICU Registered Nurses 311 - JEMELYN LOTERTENo ratings yet
- Movilización y Recuperación Precoces en Pacientes Con Ventilación Mecánica en La UCI Un Estudio de Cohorte Prospectivo Binacional, MulticéntricoDocument10 pagesMovilización y Recuperación Precoces en Pacientes Con Ventilación Mecánica en La UCI Un Estudio de Cohorte Prospectivo Binacional, MulticéntricoByron VarasNo ratings yet
- Early Mobility in The Intensive Care Unit: Evidence, Barriers, and Future DirectionsDocument12 pagesEarly Mobility in The Intensive Care Unit: Evidence, Barriers, and Future DirectionsRaka dewiNo ratings yet
- APA 7th Edition Template Student VersionDocument14 pagesAPA 7th Edition Template Student VersionAndrei ArtiedaNo ratings yet
- Standardised Handover Protocol 2014 PDFDocument7 pagesStandardised Handover Protocol 2014 PDFNikkae AngobNo ratings yet
- Elliott 2011Document12 pagesElliott 2011oscar eduardo mateus ariasNo ratings yet
- Duffy 2023 Oi 230251 1680623455.50534Document10 pagesDuffy 2023 Oi 230251 1680623455.50534Hamilton CeballosNo ratings yet
- Jop 2016 016857Document9 pagesJop 2016 016857andrei vladNo ratings yet
- Betters 2017 Development and Implementation of An Early Mobility Program For Mechanically Ventilated Pediatric PatientsDocument6 pagesBetters 2017 Development and Implementation of An Early Mobility Program For Mechanically Ventilated Pediatric PatientsEvelyn_D_az_Ha_8434No ratings yet
- Spooner 2018Document9 pagesSpooner 2018andremNo ratings yet
- Early Postoperative Ambulation Back To Basics A Quality Improvement Project PDFDocument7 pagesEarly Postoperative Ambulation Back To Basics A Quality Improvement Project PDFIndra MulianiNo ratings yet
- What Are The Barriers To Mobilizing Intensive Care Patients?Document4 pagesWhat Are The Barriers To Mobilizing Intensive Care Patients?Tote Cifuentes AmigoNo ratings yet
- J Ijnurstu 2017 12 012Document8 pagesJ Ijnurstu 2017 12 012Osborn KhasabuliNo ratings yet
- Handling Article 1Document10 pagesHandling Article 1Dusabeyezu PacifiqueNo ratings yet
- Paediatric Ambulatory Surgery - Perioperative Concerns: Dr. Pramila Chari Dr. Indu SenDocument7 pagesPaediatric Ambulatory Surgery - Perioperative Concerns: Dr. Pramila Chari Dr. Indu SenT RonaskyNo ratings yet
- A Simple DeviceDocument6 pagesA Simple DeviceErna TamiziNo ratings yet
- Iwashyna 2016Document2 pagesIwashyna 2016febrian rahmatNo ratings yet
- Early Mobilitation For Critically Ill Patients in ICUDocument34 pagesEarly Mobilitation For Critically Ill Patients in ICUririNo ratings yet
- Journal Ortho RequirementDocument13 pagesJournal Ortho RequirementKenn yahweexNo ratings yet
- A Descriptive Study To Assess The Knowledge Regarding Venipuncture Among Staff Nurses in A Selected Hospital, Lucknow With A View To Develop An Information BookletDocument7 pagesA Descriptive Study To Assess The Knowledge Regarding Venipuncture Among Staff Nurses in A Selected Hospital, Lucknow With A View To Develop An Information BookletEditor IJTSRDNo ratings yet
- Jurnal Mobilitas 5Document8 pagesJurnal Mobilitas 5abdul muisNo ratings yet
- International Emergency Nursing: SciencedirectDocument24 pagesInternational Emergency Nursing: SciencedirectRazak AbdullahNo ratings yet
- Early Post Op. MobillizationDocument21 pagesEarly Post Op. MobillizationGenyNo ratings yet
- The Effect of Early Ambulation On Patient Outcomes For Total Joint ReplacementDocument4 pagesThe Effect of Early Ambulation On Patient Outcomes For Total Joint ReplacementAris PurnomoNo ratings yet
- Intensive & Critical Care Nursing: Research ArticleDocument7 pagesIntensive & Critical Care Nursing: Research ArticleEviNo ratings yet
- Semana 1-Paper, Fundamentals of US in Clinical PracticeDocument14 pagesSemana 1-Paper, Fundamentals of US in Clinical PracticeRudy AravenaNo ratings yet
- Irtual Reality in Research and Rehabilitation of Gait and Balance in Parkinson DiseaseDocument17 pagesIrtual Reality in Research and Rehabilitation of Gait and Balance in Parkinson DiseasePaula EmyNo ratings yet
- Effects of Virtual Reality Training On Functional Reaching Movements in People With Parkinson's Disease: A Randomized Controlled Pilot TrialDocument12 pagesEffects of Virtual Reality Training On Functional Reaching Movements in People With Parkinson's Disease: A Randomized Controlled Pilot TrialVivis Yuvi SamarNo ratings yet
- Original PaperDocument11 pagesOriginal PaperAsmaa GamalNo ratings yet
- Point of Care Ultrasound: The Critical Imaging Tool For The Critically UnwellDocument10 pagesPoint of Care Ultrasound: The Critical Imaging Tool For The Critically UnwellOswaldo OrtizNo ratings yet
- Johnson 2017Document4 pagesJohnson 2017febrian rahmatNo ratings yet
- Tabel AjaDocument7 pagesTabel AjaRainbow DashieNo ratings yet
- PTJ 1636Document10 pagesPTJ 1636Pamela DíazNo ratings yet
- Protocol-Based Mobilization On Intensive Care Units: Stepped-Wedge, Cluster-Randomized Pilot Study (Pro-Motion)Document7 pagesProtocol-Based Mobilization On Intensive Care Units: Stepped-Wedge, Cluster-Randomized Pilot Study (Pro-Motion)Lee Li Nou OkhmachNo ratings yet
- Effectiveness Mobility Protocol Towards Intensive Care Unit PatientsDocument10 pagesEffectiveness Mobility Protocol Towards Intensive Care Unit PatientsMhar IcelNo ratings yet
- Tii 2021 3069470Document9 pagesTii 2021 3069470Gautham SgNo ratings yet
- Critical Care: Queuing Theory Accurately Models The Need For Critical Care ResourcesDocument6 pagesCritical Care: Queuing Theory Accurately Models The Need For Critical Care ResourcesAngela SaoNo ratings yet
- Reviews: Virtual Reality in Research and Rehabilitation of Gait and Balance in Parkinson DiseaseDocument17 pagesReviews: Virtual Reality in Research and Rehabilitation of Gait and Balance in Parkinson DiseaseDuda ShiraiwaNo ratings yet
- Fluid Administration For Acute Circulatory Dysfunction Using Basic Monitoring Narrative Review and Expert Panel Recommendations From An ESICM Task Force Maurizio CecconDocument12 pagesFluid Administration For Acute Circulatory Dysfunction Using Basic Monitoring Narrative Review and Expert Panel Recommendations From An ESICM Task Force Maurizio CecconEllys Macías PeraltaNo ratings yet
- Artigo 2 CinhalDocument7 pagesArtigo 2 CinhalSara PereiraNo ratings yet
- 4-8-1-989 Format For SynopsisDocument7 pages4-8-1-989 Format For SynopsisYashoda SatputeNo ratings yet
- Anesthetic Management of Geriatric Patients: Review ArticleDocument22 pagesAnesthetic Management of Geriatric Patients: Review Articleagita kartika sariNo ratings yet
- Identify: Candidates CareDocument10 pagesIdentify: Candidates CareJHNo ratings yet
- Delirium UciDocument6 pagesDelirium UciHernando CastrillónNo ratings yet
- Implementing Early Mobilisation in The Intensive Care Unit - An Integrative ReviewDocument15 pagesImplementing Early Mobilisation in The Intensive Care Unit - An Integrative ReviewfabianneassisNo ratings yet
- Care Unit PDFDocument9 pagesCare Unit PDFsitinafisahNo ratings yet
- Pa Shik Anti 2012Document8 pagesPa Shik Anti 2012Irfan FauziNo ratings yet
- Monitoring the Nervous System for Anesthesiologists and Other Health Care ProfessionalsFrom EverandMonitoring the Nervous System for Anesthesiologists and Other Health Care ProfessionalsNo ratings yet
- Keys to Successful Orthotopic Bladder SubstitutionFrom EverandKeys to Successful Orthotopic Bladder SubstitutionUrs E. StuderNo ratings yet
- Evaluating Care in Ed Fast TracksDocument7 pagesEvaluating Care in Ed Fast TracksBapak Sunaryo SPBUNo ratings yet
- Prognostic Accuracy of Sepsis-3 Criteria For In-Hospital Mortality Among Patients With Suspected Infection Presenting To The Emergency DepartmentDocument8 pagesPrognostic Accuracy of Sepsis-3 Criteria For In-Hospital Mortality Among Patients With Suspected Infection Presenting To The Emergency DepartmentBapak Sunaryo SPBUNo ratings yet
- Turkish Journal of Emergency MedicineDocument4 pagesTurkish Journal of Emergency MedicineBapak Sunaryo SPBUNo ratings yet
- Improving Emergency Department Patient FlowDocument6 pagesImproving Emergency Department Patient FlowBapak Sunaryo SPBUNo ratings yet
- Efficacy of Bladder Irrigation in Preventing Urinary Tract Infections Associated With Short-Term Catheterization in Comatose PatientsDocument6 pagesEfficacy of Bladder Irrigation in Preventing Urinary Tract Infections Associated With Short-Term Catheterization in Comatose PatientsBapak Sunaryo SPBUNo ratings yet
- Evaluating The Quality of Care Delivered by An Emergency Department Fast Track Unit With Both Nurse Practitioners and DoctorsDocument7 pagesEvaluating The Quality of Care Delivered by An Emergency Department Fast Track Unit With Both Nurse Practitioners and DoctorspoppyNo ratings yet
- Impact of A Planned Workflow ChangeDocument12 pagesImpact of A Planned Workflow ChangeBapak Sunaryo SPBUNo ratings yet
- Prognostic Accuracy of Sepsis-3 Criteria For In-Hospital Mortality Among Patients With Suspected Infection Presenting To The Emergency DepartmentDocument8 pagesPrognostic Accuracy of Sepsis-3 Criteria For In-Hospital Mortality Among Patients With Suspected Infection Presenting To The Emergency DepartmentBapak Sunaryo SPBUNo ratings yet
- Effect of Music On Pain, Anxiety, and Patient Satisfaction inDocument10 pagesEffect of Music On Pain, Anxiety, and Patient Satisfaction inDewi Ji YongNo ratings yet
- Intensive & Critical Care Nursing: Research ArticleDocument7 pagesIntensive & Critical Care Nursing: Research ArticleEviNo ratings yet
- Music in Emergency DepartmentDocument24 pagesMusic in Emergency DepartmentWiryawan AlamNo ratings yet
- 89 452 1 PB PDFDocument19 pages89 452 1 PB PDFpra sethyaNo ratings yet
- Patient Satisfaction and Benefts of Music Therapy Services To Manage Stress and Pain in The Hospital Emergency DepartmentDocument25 pagesPatient Satisfaction and Benefts of Music Therapy Services To Manage Stress and Pain in The Hospital Emergency DepartmentBapak Sunaryo SPBU100% (1)
- Mobilization of Intensive Care Patients A Multidisciplinary Practical Guide For CliniciansDocument10 pagesMobilization of Intensive Care Patients A Multidisciplinary Practical Guide For CliniciansBapak Sunaryo SPBUNo ratings yet
- 1495 PDFDocument8 pages1495 PDFSusan Wulandari ApriLiaNo ratings yet
- Patient Early Mobilization A Malaysias Study of Nursing Practices PDFDocument7 pagesPatient Early Mobilization A Malaysias Study of Nursing Practices PDFNuraien LapaleoNo ratings yet
- Working With Art in A Case of SchizophreniaDocument5 pagesWorking With Art in A Case of SchizophreniaBapak Sunaryo SPBUNo ratings yet
- Working With Art in A Case of SchizophreniaDocument5 pagesWorking With Art in A Case of SchizophreniaBapak Sunaryo SPBUNo ratings yet
- Acceptance and Commitment Therapy For The Treatment of Adolescent Depression (Hayes, 2011)Document9 pagesAcceptance and Commitment Therapy For The Treatment of Adolescent Depression (Hayes, 2011)Bapak Sunaryo SPBUNo ratings yet
- Visual Hallucination For Computational CreationDocument8 pagesVisual Hallucination For Computational CreationBapak Sunaryo SPBUNo ratings yet
- Working With Art in A Case of SchizophreniaDocument5 pagesWorking With Art in A Case of SchizophreniaBapak Sunaryo SPBUNo ratings yet
- Visual Hallucination For Computational CreationDocument8 pagesVisual Hallucination For Computational CreationBapak Sunaryo SPBUNo ratings yet
- A Review of Acceptance and Commitment Therapy (Act) Empirical EvidenceDocument39 pagesA Review of Acceptance and Commitment Therapy (Act) Empirical EvidenceBapak Sunaryo SPBUNo ratings yet
- Art Therapy May Reduce Psychopathology in Schizophrenia by Strengthening The Patients' Sense of SelfDocument6 pagesArt Therapy May Reduce Psychopathology in Schizophrenia by Strengthening The Patients' Sense of SelfBapak Sunaryo SPBUNo ratings yet
- Comparative Study For Determination of Atracurium Besilate in Presence of Its Toxic Degradant (Laudanosine) by Reversed Phase HPLC and by TLC DensitometryDocument11 pagesComparative Study For Determination of Atracurium Besilate in Presence of Its Toxic Degradant (Laudanosine) by Reversed Phase HPLC and by TLC DensitometrySabrina JonesNo ratings yet
- MSDS TSHDocument8 pagesMSDS TSHdwiNo ratings yet
- Know Your Customer BrochureDocument4 pagesKnow Your Customer BrochureTEL COMENo ratings yet
- Manufacturing ProcessesDocument6 pagesManufacturing ProcessesSudalai MadanNo ratings yet
- Jeremiah's Law, Introduced by Assemblywoman Rodneyse BichotteDocument2 pagesJeremiah's Law, Introduced by Assemblywoman Rodneyse BichotteCity & State NYNo ratings yet
- Awsum BrandingDocument18 pagesAwsum Brandingdharam123_904062105No ratings yet
- Compact Water Treatment 200 m3Document3 pagesCompact Water Treatment 200 m3civil eng915No ratings yet
- 1978 - Behavior Analysis and Behavior Modification - Mallot, Tillema & Glenn PDFDocument499 pages1978 - Behavior Analysis and Behavior Modification - Mallot, Tillema & Glenn PDFKrusovice15No ratings yet
- SEI BasicDocument146 pagesSEI BasicYuthia Aulia Riani100% (1)
- Karen Horney's Theories of PersonalityDocument8 pagesKaren Horney's Theories of PersonalityGeorge BaywongNo ratings yet
- Syntheis Writing 2 How Do Fear and Desire For Personal Acceptance Influence Human BehaviorDocument2 pagesSyntheis Writing 2 How Do Fear and Desire For Personal Acceptance Influence Human Behaviorapi-463684021No ratings yet
- To: Head of Sea Training Department PT Gemilang Bina Lintas Tirta Ship ManagementDocument1 pageTo: Head of Sea Training Department PT Gemilang Bina Lintas Tirta Ship ManagementtarNo ratings yet
- Internship-Plan BSBA FInalDocument2 pagesInternship-Plan BSBA FInalMark Altre100% (1)
- Aaos PDFDocument4 pagesAaos PDFWisnu CahyoNo ratings yet
- QTR-2 2023 Meeting Format Nov.23Document45 pagesQTR-2 2023 Meeting Format Nov.23skumar31397No ratings yet
- Blood Stasis and What Does That MeanDocument2 pagesBlood Stasis and What Does That MeanCarl MacCordNo ratings yet
- Formulating A Dental Treatment Plan: DR Tashnim BagusDocument33 pagesFormulating A Dental Treatment Plan: DR Tashnim BagustarekrabiNo ratings yet
- Midterm Requirement-Green BuildingDocument7 pagesMidterm Requirement-Green BuildingJo-anne RiveraNo ratings yet
- Zinc Silicate or Zinc Epoxy As The Preferred High Performance PrimerDocument10 pagesZinc Silicate or Zinc Epoxy As The Preferred High Performance Primerbabis1980100% (1)
- Bio 2Document3 pagesBio 2ganchimeg gankhuuNo ratings yet
- ISO 9001 - 14001 - 2015 enDocument2 pagesISO 9001 - 14001 - 2015 enVĂN THÀNH TRƯƠNGNo ratings yet
- Problems SetDocument10 pagesProblems SetSajith KurianNo ratings yet
- Rozdział 12 Słownictwo Grupa BDocument1 pageRozdział 12 Słownictwo Grupa BBartas YTNo ratings yet
- Executive Compensation: A Presentation OnDocument9 pagesExecutive Compensation: A Presentation On9986212378No ratings yet
- PSV Sizing For Two Phase FlowDocument28 pagesPSV Sizing For Two Phase FlowSyed Haideri100% (1)
- Eisenmenger SyndromeDocument6 pagesEisenmenger SyndromeWarkah SanjayaNo ratings yet
- Access To JusticeDocument9 pagesAccess To JusticeprimeNo ratings yet
- Name of Learner: Section: Subject Teacher: Date:: Practical Research 2Document4 pagesName of Learner: Section: Subject Teacher: Date:: Practical Research 2J-heart Basabas Malpal100% (6)
- Paper 4 Nov 2000Document2 pagesPaper 4 Nov 2000MSHNo ratings yet
- Manual Fritadeira PDFDocument136 pagesManual Fritadeira PDFtherasiaNo ratings yet